Performance of Dental Cements Used for Bonding Zirconia Crowns with Titanium Implants Embedded in an Innovative Bi-Layered Artificial Bone
Abstract
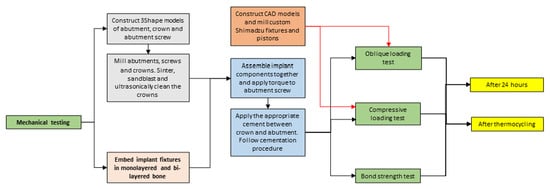
1. Introduction
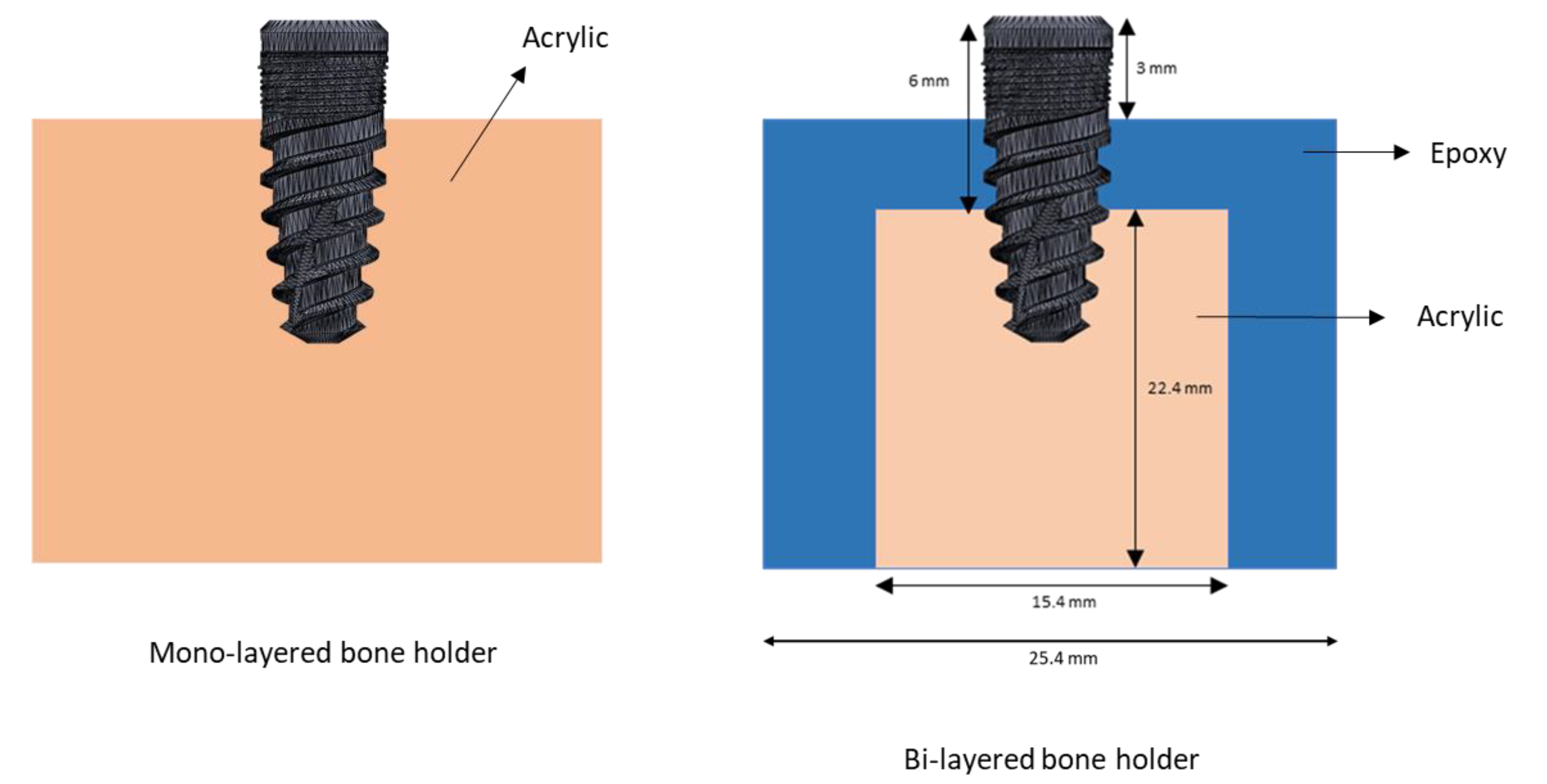
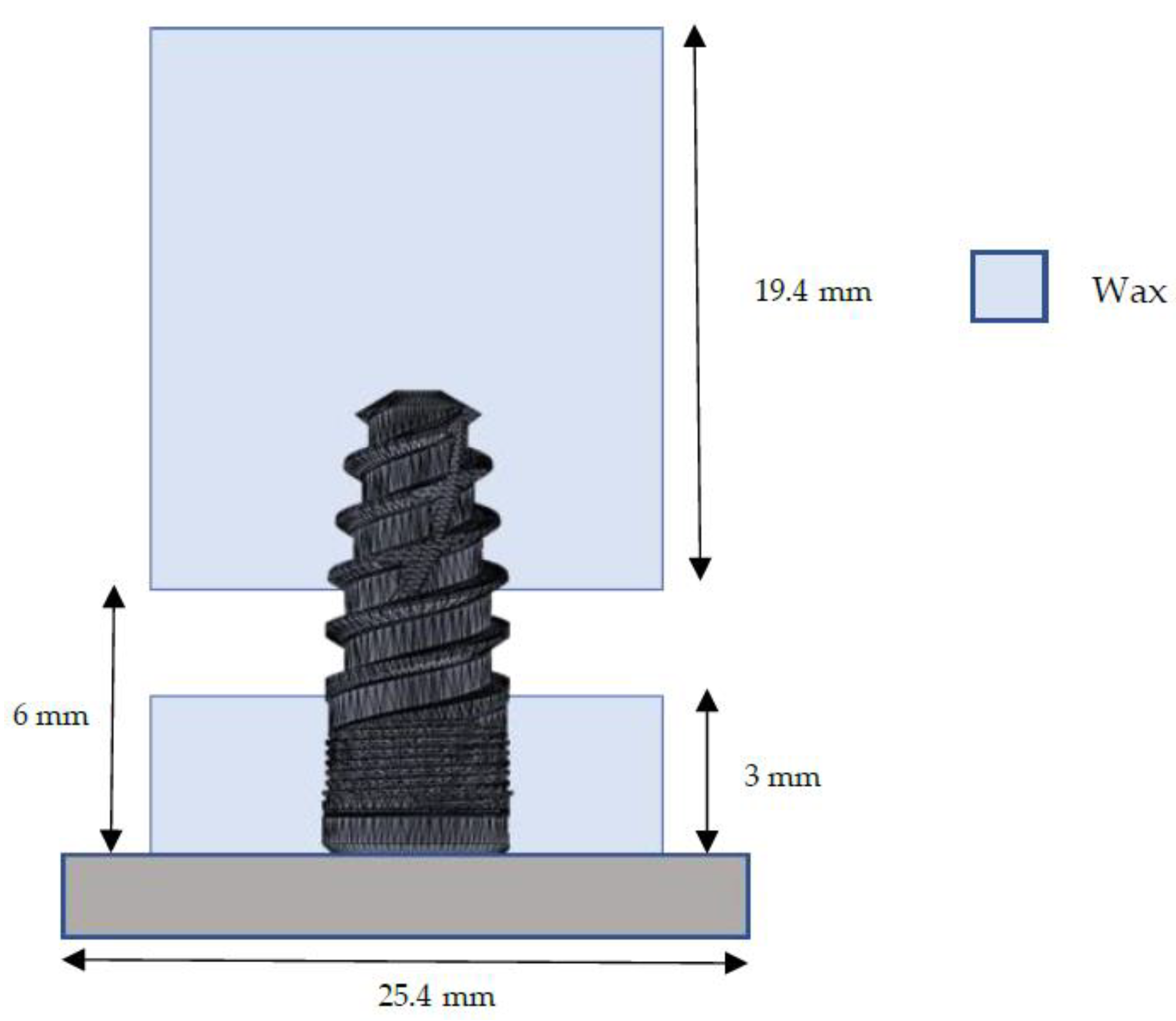
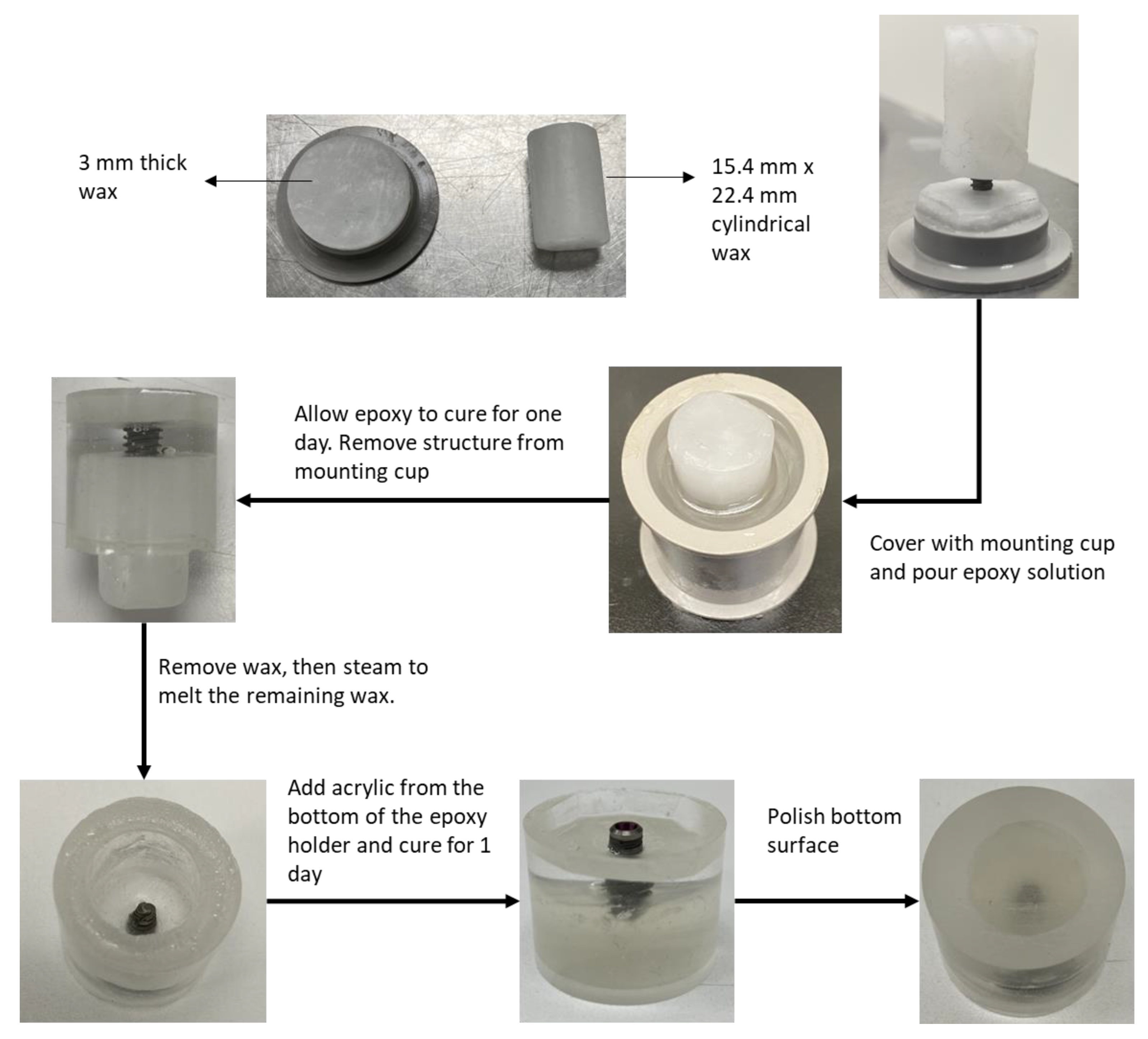
- To construct an artificial bi-layered bone holder to mimic the natural structure of the jawbone.
- To perform a tensile bond strength test, a compressive load test, and an oblique load test on cement-retained crowns in titanium dental implant assemblies with different cement materials, before and after thermocycling.
2. Materials and Methods
2.1. Mimicking the Bone Holder
- Tensile bond strength test (after 24 h): 10 implants/cement × 4 cements = 40 implants
- Tensile bond strength test (after thermocycling): 10 implants/cement × 4 cements = 40 implants
- Compressive load test (after 24 h): 4 implants/cement × 4 cements = 16 implants
- Compressive load test (after thermocycling): 4 implants/cement × 4 cements = 16 implants
- Oblique load test (after 24 h): 4 implants/cement × 4 cements = 16 implants
- Oblique load test (after thermocycling): 4 implants/cement × 4 cements = 16 implants
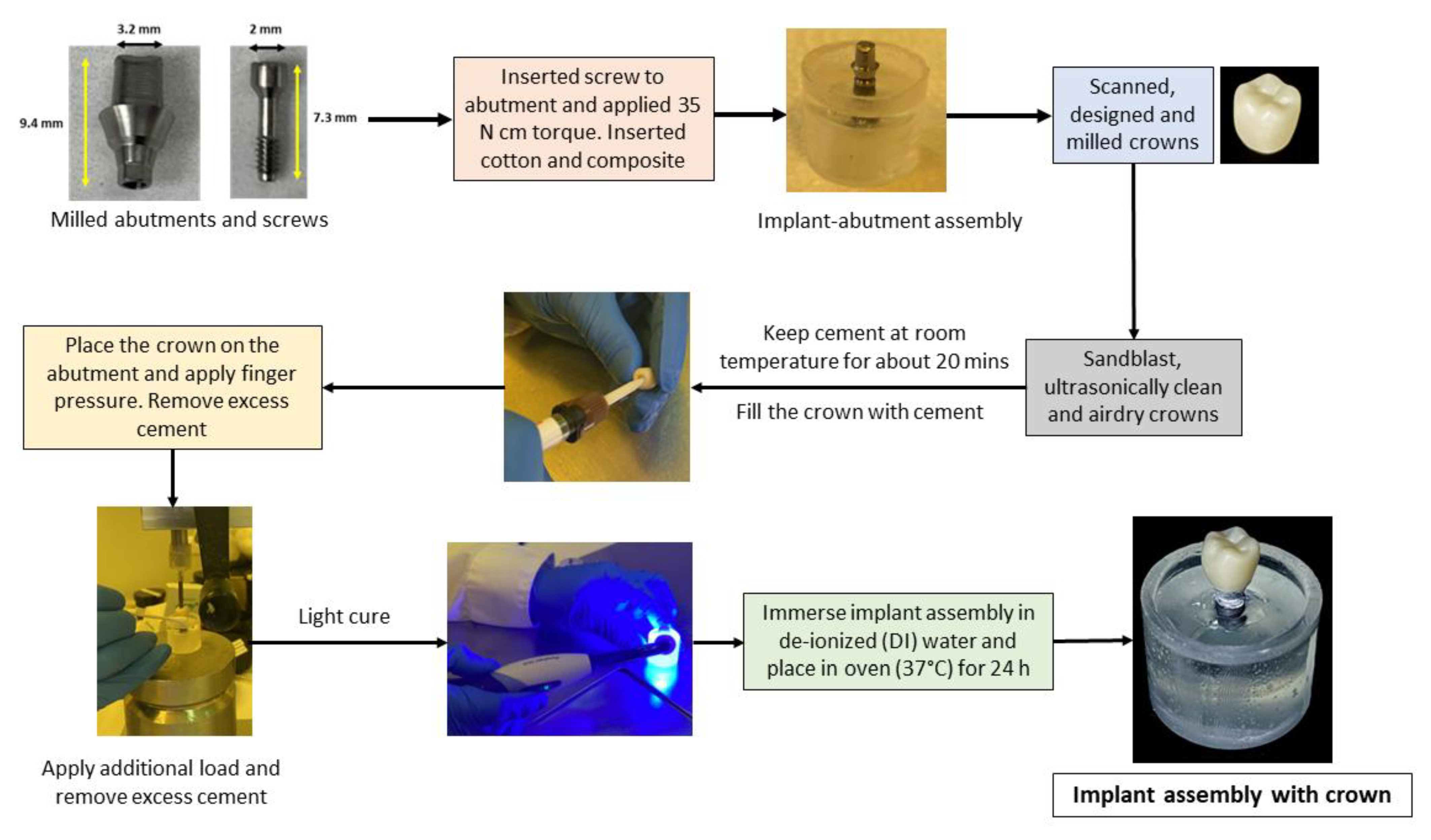
2.2. Cementation Procedure
2.3. Mechanical Tests
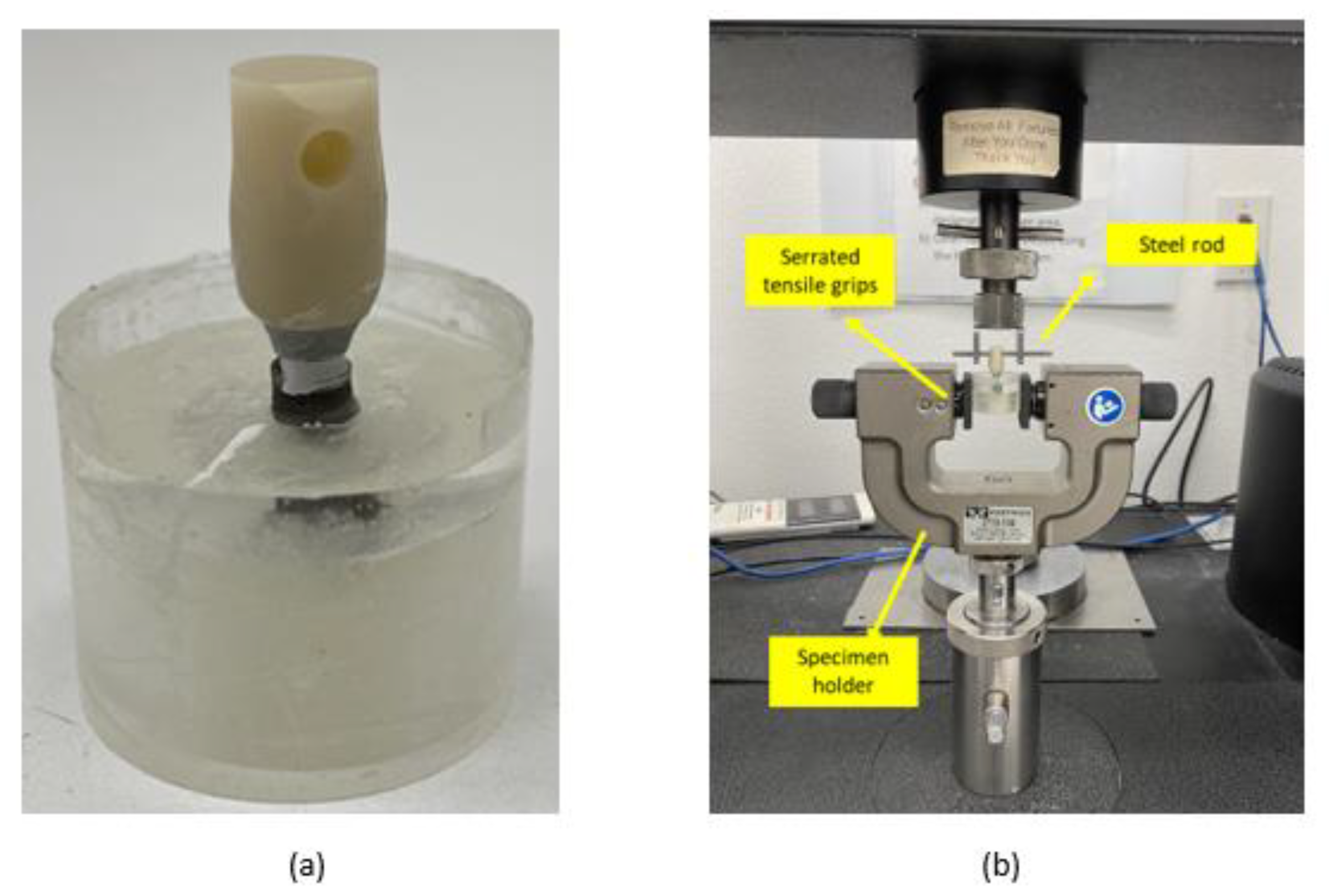
2.3.1. Tensile Bond Strength Test
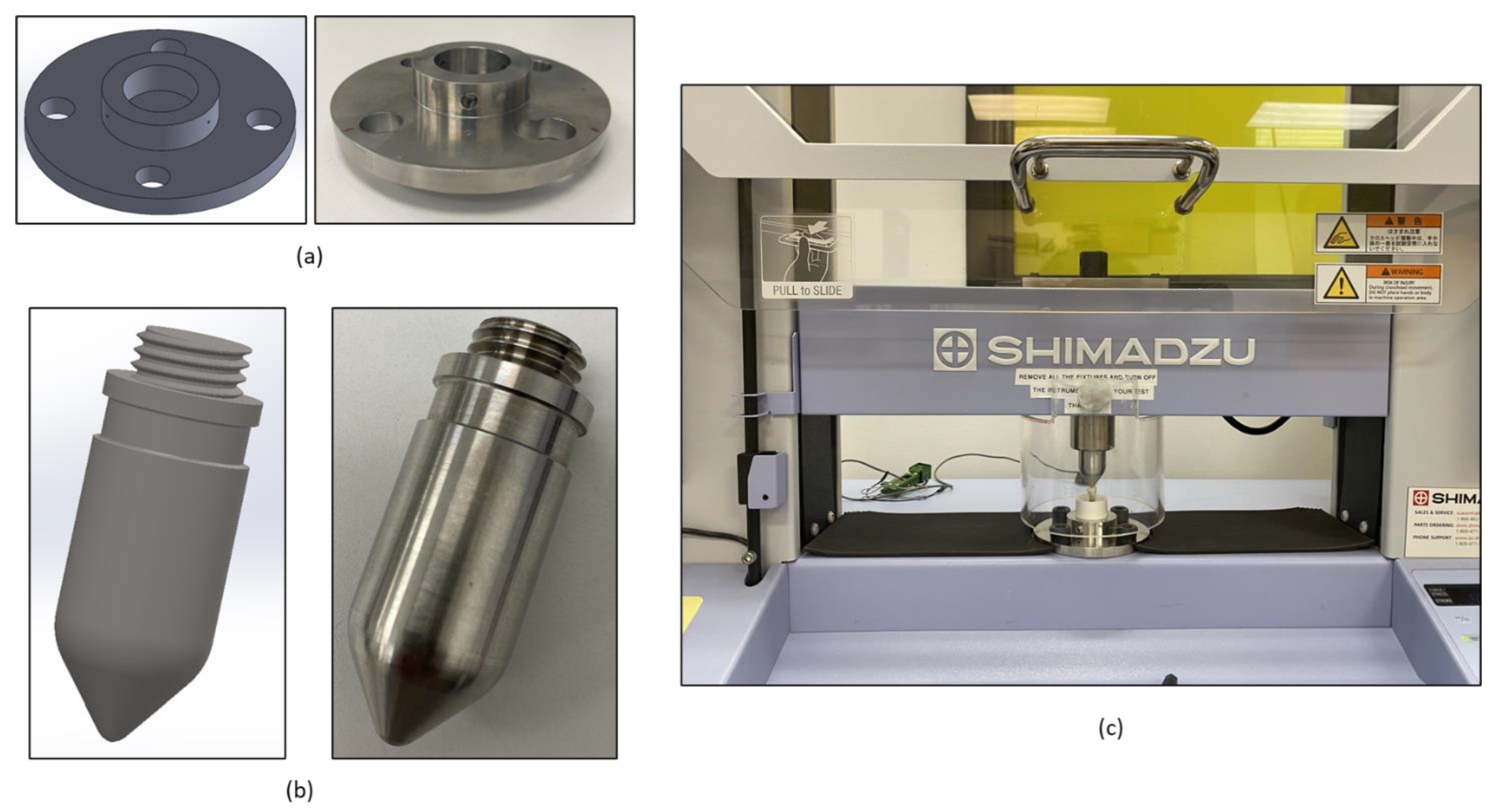
2.3.2. Compressive Load Test
2.3.3. Oblique Load Test
2.4. Statistical Analysis
3. Results
3.1. Mechanical Tests
3.1.1. Tensile Bond Strength Test
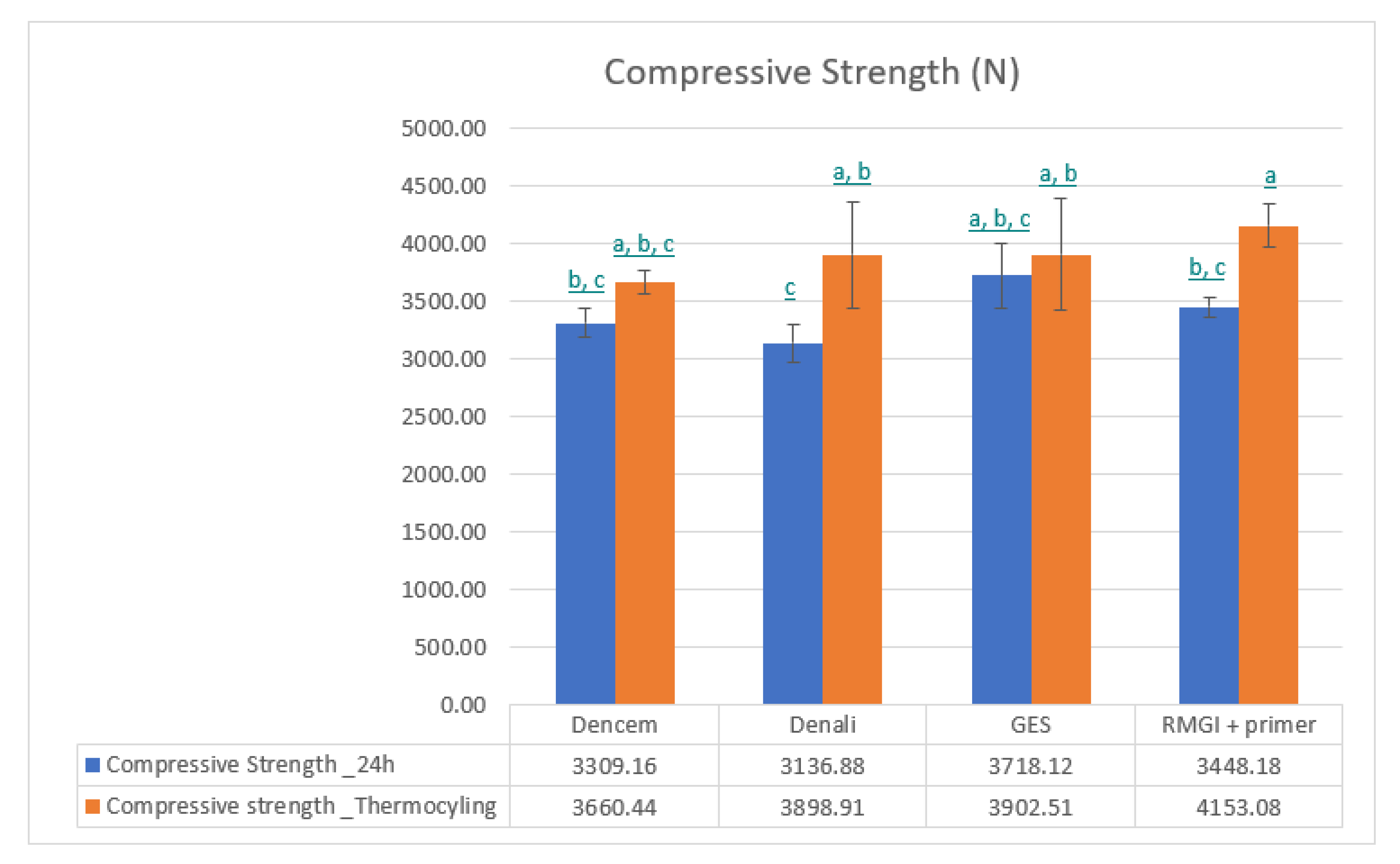
3.1.2. Compressive Load Test
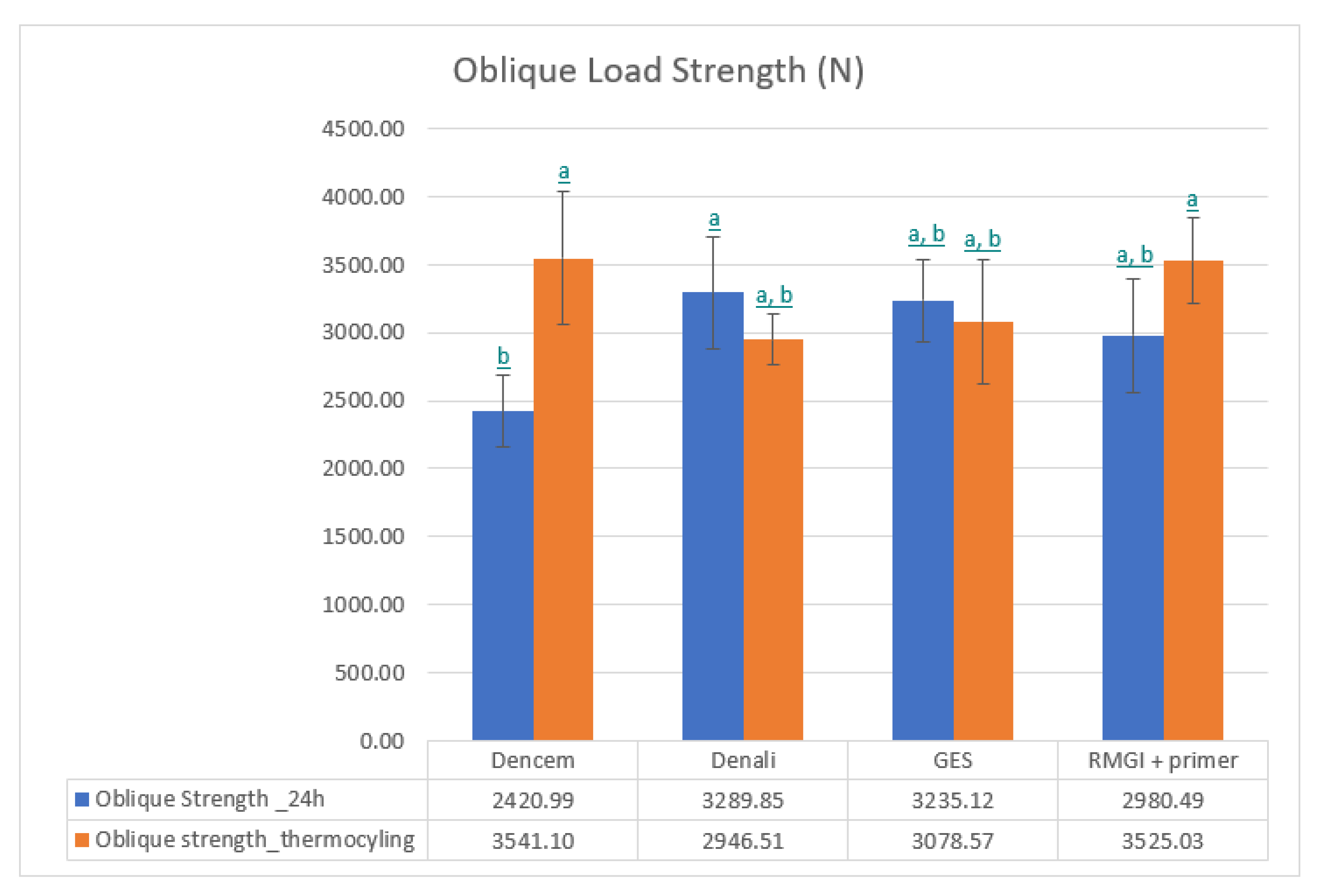
3.1.3. Oblique Load Test
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sailer, I.; Sailer, T.; Stawarczyk, B.; Jung, R.E.; Hämmerle, C.H.F. In vitro study of the influence of the type of connection on the fracture load of zirconia abutments with internal and external implant-abutment connections. Int. J. Oral Maxillofac. Implants 2009, 245, 850–858. [Google Scholar]
- Griggs, J.A. Dental Implants. Dent. Clin. N. Am. 2017, 614, 857–871. [Google Scholar] [CrossRef] [PubMed]
- Alghamdi, H.S.; Jansen, J.A. The development and future of dental implants. Dent. Mater. J. 2020, 392, 167–172. [Google Scholar] [CrossRef] [PubMed]
- Kalluri, L.; Seale, B.; Satpathy, M.; Esquivel-Upshaw, J.F.; Duan, Y. Three-Dimensional Finite Element Analysis of the Veneer—Framework Thickness in an All-Ceramic Implant Supported Fixed Partial Denture. Ceramics 2021, 42, 199–207. [Google Scholar] [CrossRef]
- Leo, S.; Tan, M.; Yee, S.; Lee, F.; Tan, K. Rotational Load Fatigue Performance of Titanium vs Titanium-Zirconium Implant-Abutment Connections. Int. J. Oral Maxillofac. Implants 2022, 374, 740–747. [Google Scholar] [CrossRef]
- Parzham, V.; Judge, R.; Bailey, D. A Five-Year Retrospective Assay of Implant Treatments and Complications in Private Practice: Restorative Treatment Profiles of Long-Span, Implant-Supported Fixed and Removable Dental Prostheses. Int. J. Prosthodont. 2018, 313, 211–222. [Google Scholar] [CrossRef]
- Hamed, M.T.; Abdullah Mously, H.; Khalid Alamoudi, S.; Hossam Hashem, A.B.; Hussein Naguib, G. A Systematic Review of Screw versus Cement-Retained Fixed Implant Supported Reconstructions. Clin. Cosmet. Investig. Dent. 2020, 12, 9–16. [Google Scholar] [CrossRef]
- Hebel, K.S.; Gajjar, R.C. Cement-retained versus screw-retained implant restorations: Achieving optimal occlusion and esthetics in implant dentistry. J. Prosthet. Dent. 1997, 771, 28–35. [Google Scholar] [CrossRef]
- Karl, M.; Graef, F.; Taylor, T.D.; Heckmann, S.M. In vitro effect of load cycling on metal-ceramic cement- and screw-retained implant restorations. J. Prosthet. Dent. 2007, 973, 137–140. [Google Scholar] [CrossRef]
- Lee, J.H.; Jang, H.Y.; Lee, S.Y. Finite Element Analysis of Dental Implants with Zirconia Crown Restorations: Conventional Cement-Retained vs. Cementless Screw-Retained. Materials 2021, 14, 2666. [Google Scholar] [CrossRef]
- Michalakis, K.X.; Hirayama, H.; Garefis, P.D. Cement-retained versus screw-retained implant restorations: A critical review. Int. J. Oral Maxillofac. Implants 2003, 185, 719–728. [Google Scholar]
- Agarwal, S.; Ashok, V.; Maiti, S.; Agarwal, V. Dentists’ Preference toward Fixed Versus Removable Implant Prosthesis on Edentulous Jaws to Improve Quality of Life. J. Long Term Eff. Med. Implants 2023, 331, 83–89. [Google Scholar] [CrossRef] [PubMed]
- Wittneben, J.G.; Millen, C.; Brägger, U. Clinical Performance of Screw- Versus Cement-Retained Fixed Implant-Supported Reconstructions—A Systematic Review. Int. J. Oral Maxillofac. Implants 2014, 29, 84–98. [Google Scholar] [CrossRef] [PubMed]
- Kern, J.; Kern, T.; Wolfart, S.; Heussen, N. A systematic review and meta-analysis of removable and fixed implant-supported prostheses in edentulous jaws: Post-loading implant loss. Clin. Oral Implants Res. 2016, 272, 174–195. [Google Scholar] [CrossRef]
- Gundogdu, M.; Aladag, L.I. Effect of adhesive resin cements on bond strength of ceramic core materials to dentin. Niger. J. Clin. Pract. 2018, 213, 367–374. [Google Scholar] [CrossRef]
- Johnson, G.H.; Lepe, X.; Patterson, A.; Schäfer, O. Simplified cementation of lithium disilicate crowns: Retention with various adhesive resin cement combinations. J. Prosthet. Dent. 2018, 1195, 826–832. [Google Scholar] [CrossRef]
- Dressano, D.; Salvador, M.V.; Oliveira, M.T.; Marchi, G.M.; Fronza, B.M.; Hadis, M.; Palin, W.M.; Lima, A.F. Chemistry of novel and contemporary resin-based dental adhesives. J. Mech. Behav. Biomed. Mater. 2020, 110, 103875. [Google Scholar] [CrossRef]
- Carville, R.; Quinn, F. The selection of adhesive systems for resin-based luting agents. J. Ir. Dent. Assoc. 2008, 545, 218–222. [Google Scholar]
- Wilson, A.D. Glass-ionomer cement origins, development and future. Clin. Mater. 1991, 74, 275–282. [Google Scholar] [CrossRef]
- Ansari, S.; Moshaverinia, M.; Roohpour, N.; Chee, W.W.L.; Schricker, S.R.; Moshaverinia, A. Properties of a proline-containing glass ionomer dental cement. J. Prosthet. Dent. 2013, 1105, 408–413. [Google Scholar] [CrossRef]
- Bahsi, E.; Sagmak, S.; Dayi, B.; Cellik, O.; Akkus, Z. The evaluation of microleakage and fluoride release of different types of glass ionomer cements. Niger. J. Clin. Pract. 2019, 227, 961. [Google Scholar] [CrossRef] [PubMed]
- Berg, J.H.; Croll, T.P. Glass ionomer restorative cement systems: An update. Pediatr. Dent. 2015, 372, 116–124. [Google Scholar]
- Smith, D.C. Dental cements. Curr. Opin. Dent. 1991, 12, 228–234. [Google Scholar]
- Prasanth, B.K.; Prakasam, S.; Bharadwaj, P.; Loganathan, S. A comparative evaluation of compressive strength of Portland cement with zinc oxide eugenol and Polymer-reinforced cement: An in vitro analysis. Indian J. Dent. Res. 2014, 251, 73. [Google Scholar] [CrossRef] [PubMed]
- Bra¨nnstro¨m, M.; Nyborg, H. Pulp reaction to a temporary zinc oxide/eugenol cement. J. Prosthet. Dent. 1976, 352, 185–191. [Google Scholar] [CrossRef]
- Powers, J.M. Self-adhesive Resin Cements: Characteristics, Properties, and Manipulation. AEGIS Dental Network. Funct. Esthet. Restor. Dent. 2008, 1, 34–40. [Google Scholar]
- Weiser, F.; Behr, M. Self-Adhesive Resin Cements: A Clinical Review. J. Prosthodont. 2015, 242, 100–108. [Google Scholar] [CrossRef]
- Makkar, S.; Malhotra, N. Self-adhesive resin cements: A new perspective in luting technology. Dent. Update 2013, 409, 758–768. [Google Scholar] [CrossRef]
- Marghalani, H.Y. Sorption and solubility characteristics of self-adhesive resin cements. Dent. Mater. 2012, 2810, e187–e198. [Google Scholar] [CrossRef]
- Sidhu, S.K. Glass-ionomer cement restorative materials: A sticky subject? Aust. Dent. J. 2011, 56 (Suppl. S1), 23–30. [Google Scholar] [CrossRef]
- Walia, T.; Brigi, C.; Ziadkhani, M.M.; Khayat, A.A.; Tabibzadeh, Z. Retention Force of Glass Ionomer Based Luting Cements with Posterior Primary Zirconium Crowns—A Comparative in Vitro Study. J. Clin. Pediatr. Dent. 2021, 454, 259–264. [Google Scholar] [CrossRef] [PubMed]
- Satpathy, M.; Duan, Y.; Betts, L.; Priddy, M.; Griggs, J.A. Effect of Bone Remodeling on Dental Implant Fatigue Limit Predicted Using 3D Finite Element Analysis. J. Dent. Oral Epidemiol. 2022, 2. [Google Scholar] [CrossRef]
- ISO 14801; Dentistry—Implants—Dynamic Loading Test for Endosseous Dental Implants. ISO: London, UK, 2016.
- Satpathy, M.; Jose, R.M.; Duan, Y.; Griggs, J.A. Effects of abutment screw preload and preload simulation techniques on dental implant lifetime. JADA Found. Sci. 2022, 1, 100010. [Google Scholar] [CrossRef] [PubMed]
- ISO/TS 11405; Dentistry—Testing of Adhesion to Tooth Structure. ISO: London, UK, 2015.
- ISO/TR 11405; Dental Materials—Guidance on Testing on Adhesion to Tooth Structure. ISO: London, UK, 1994.
- Saghiri, M.A.; Asatourian, A.; Garcia-Godoy, F.; Gutmann, J.L.; Sheibani, N. The Impact of Thermocycling Process on the Dislodgement Force of Different Endodontic Cements. BioMed Res. Int. 2013, 2013, 317185. [Google Scholar] [CrossRef] [PubMed]
- Luthy, H.; Loeffel, O.; Hammerle, C. Effect of thermocycling on bond strength of luting cements to zirconia ceramic. Dent. Mater. 2006, 222, 195–200. [Google Scholar] [CrossRef]
- Bitter, K.; Meyer-Lueckel, H.; Priehn, K.; Kanjuparambil, J.P.; Neumann, K.; Kielbassa, A.M. Effects of luting agent and thermocycling on bond strengths to root canal dentine. Int. Endod. J. 2006, 3910, 809–818. [Google Scholar] [CrossRef]
- Miyazaki, M.; Sato, M.; Onose, H.; Moore, B.K. Influence of thermal cycling on dentin bond strength of two-step bonding systems. Am. J. Dent. 1998, 113, 118–122. [Google Scholar]
- Helvatjoglu-Antoniades, M.; Koliniotou-Kubia, E.; Dionyssopoulos, P. The effect of thermal cycling on the bovine dentine shear bond strength of current adhesive systems. J. Oral Rehabil. 2004, 319, 911–917. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Satpathy, M.; Pham, H.; Shah, S. Performance of Dental Cements Used for Bonding Zirconia Crowns with Titanium Implants Embedded in an Innovative Bi-Layered Artificial Bone. Ceramics 2023, 6, 651-663. https://doi.org/10.3390/ceramics6010039
Satpathy M, Pham H, Shah S. Performance of Dental Cements Used for Bonding Zirconia Crowns with Titanium Implants Embedded in an Innovative Bi-Layered Artificial Bone. Ceramics. 2023; 6(1):651-663. https://doi.org/10.3390/ceramics6010039
Chicago/Turabian StyleSatpathy, Megha, Hai Pham, and Shreya Shah. 2023. "Performance of Dental Cements Used for Bonding Zirconia Crowns with Titanium Implants Embedded in an Innovative Bi-Layered Artificial Bone" Ceramics 6, no. 1: 651-663. https://doi.org/10.3390/ceramics6010039
APA StyleSatpathy, M., Pham, H., & Shah, S. (2023). Performance of Dental Cements Used for Bonding Zirconia Crowns with Titanium Implants Embedded in an Innovative Bi-Layered Artificial Bone. Ceramics, 6(1), 651-663. https://doi.org/10.3390/ceramics6010039