A One Health Approach for Guinea Worm Disease Control: Scope and Opportunities
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Epidemiological Data
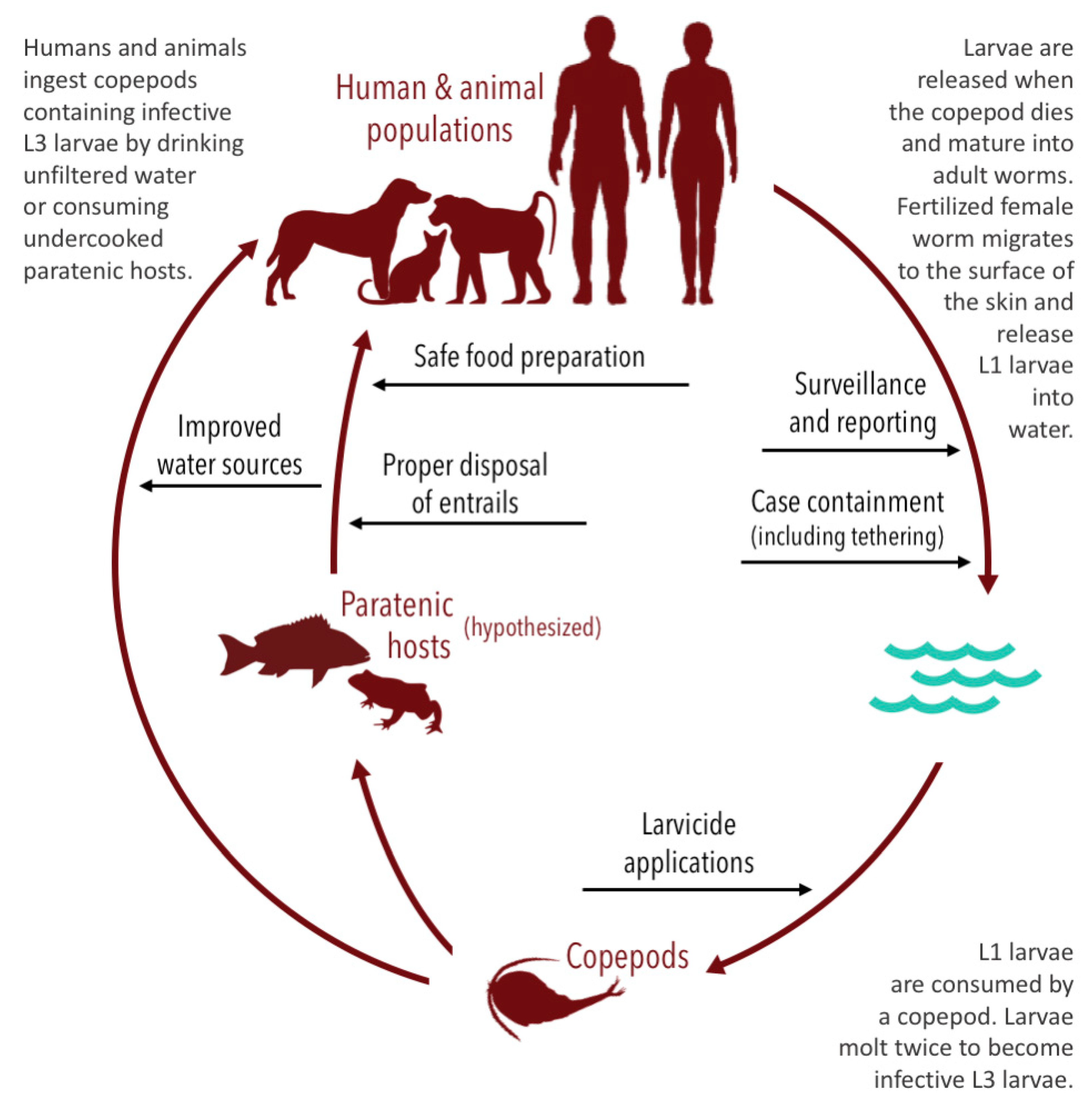
3.2. Interventions Used to Reduce the Burden of Guinea Worm Disease in Humans and Animal Populations
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Greenaway, C. Dracunculiasis (guinea worm disease). CMAJ 2004, 170, 495–500. [Google Scholar]
- Beyene, H.B.; Bekele, A.; Shifara, A.; Ebstie, Y.A.; Desalegn, Z.; Kebede, Z.; Mulugeta, A.; Deribe, K.; Tadesse, Z.; Abebe, T.; et al. Elimination of Guinea Worm Disease in Ethiopia; Current Status of the Disease’s, Eradication Strategies and Challenges to the End Game. Ethiop. Med. J. 2017, 55, 15–31. [Google Scholar] [PubMed]
- Cairncross, S.; Muller, R.; Zagaria, N. Dracunculiasis (Guinea Worm Disease) and the Eradication Initiative. Clin. Microbiol. Rev. 2002, 15, 223–246. [Google Scholar] [CrossRef] [PubMed]
- Biswas, G.; Sankara, D.P.; Agua-Agum, J.; Maiga, A. Dracunculiasis (guinea worm disease): Eradication without a drug or a vaccine. Phil. Trans. R. Soc. B 2013, 368, 20120146. [Google Scholar] [CrossRef] [PubMed]
- Belcher, D. Opportunities for control of dracunculiasis: Transmission and epidemiology. In Workshop on Opportunities for Control of Dracunculiasis; National Academy Press: Washington, DC, USA, 1985; pp. 1–7. [Google Scholar]
- Cook, G.; Zumla, A. Manson’s Tropical Diseases, 22nd ed.; Elsevier: Philadelphia, PA, USA, 2009. [Google Scholar]
- Muller, R. Guinea worm disease: Epidemiology, control, and treatment. Bull. World Health Organ. 1979, 57, 683. [Google Scholar]
- Hopkins, D.R.; Ruiz-Tiben, E.; Eberhard, M.L.; Roy, S.L.; Weiss, A.J. Progress Toward Global Eradication of Dracunculiasis, January 2016–June 2017. MMWR 2017, 66, 1327–1331. [Google Scholar] [CrossRef]
- World Health Organization. Dracunculiasis (Guinea-Worm Disease). Available online: https://www.who.int/dracunculiasis/portal/en/ (accessed on 12 March 2020).
- Roberts, L. Battle to wipe out Guinea worm stumbles. Nature 2019, 574, 157–158. [Google Scholar] [CrossRef]
- Galán-Puchades, M.T. WHO delays guinea-worm disease eradication to 2020: Are dogs the sole culprits? Lancet 2017, 17, 1124–1125. [Google Scholar] [CrossRef]
- Hopkins, D.R.; Ruiz-Tiben, E.; Eberhard, M.L.; Roy, S.L. Progress toward Global Eradication of Dracunculiasis, January 2013–June 2014. MMWR 2014, 63, 1150–1154. [Google Scholar]
- Thiele, E.A.; Eberhard, M.L.; Cotton, J.A.; Durrant, C.; Berg, J.; Hamm, K.; Ruiz-Tiben, E. Population genetic analysis of Chadian Guinea worms reveals that human and non-human hosts share common parasite populations. PLoS Negl. Trop. Dis. 2018, 12, e0006747. [Google Scholar] [CrossRef]
- Callaway, E. Dogs thwart effort to eradicate Guinea worm. Nature 2016, 529, 10–11. [Google Scholar] [CrossRef]
- Eberhard, M.L.; Ruiz-Tiben, E.; Hopkins, D.R.; Farrell, C.; Toe, F.; Weiss, A.; Withers, P.C., Jr.; Jenks, M.H.; Thiele, E.A.; Cotton, J.A.; et al. The Peculiar Epidemiology of Dracunculiasis in Chad. Am. J. Trop. Med. Hyg. 2014, 90, 61–70. [Google Scholar] [CrossRef] [PubMed]
- Eberhard, M.L.; Cleveland, C.A.; Zirimwabagabo, H.; Yabsley, M.J.; Ouakou, P.T.; Ruiz-Tiben, E. Guinea Worm (Dracunculus medinensis) Infection in a Wild-Caught Frog, Chad. Emerg. Infect. Dis. 2016, 22, 1961–1962. [Google Scholar] [CrossRef]
- Galán-Puchades, M.T. Dracunculiasis: Water-borne anthroponosis vs. food-borne zoonosis. J. Helminthol. 2019, 94. [Google Scholar] [CrossRef] [PubMed]
- Hopkins, D.R.; Ruiz-Tiben, E.; Eberhard, M.L.; Weiss, A.; Withers, P.C., Jr.; Roy, S.L.; Sienko, D.G. Dracunculiasis Eradication: Are We There Yet? Am. J. Trop. Med. Hyg. 2018, 99, 388–395. [Google Scholar] [CrossRef]
- McDonald, R.A.; Wilson-Aggarwal, J.K.; Swan, G.J.F.; Goodwin, C.E.D.; Moundai, T.; Sankara, D.; Biswas, G.; Zingeser, J.A. Ecology of domestic dogs Canis familiaris as an emerging reservoir of Guinea worm Dracunculus medinensis infection. PLoS Negl. Trop. Dis. 2020, 14, e0008170. [Google Scholar] [CrossRef]
- Molyneux, D.; Sankara, D.P. Guinea worm eradication: Progress and challenges—Should we beware of the dog? PLoS Negl. Trop. Dis. 2017, 11, e0005495. [Google Scholar] [CrossRef] [PubMed]
- Cleveland, C.A.; Eberhard, M.L.; Thompson, A.T.; Smith, S.J.; Zirimwabagabo, H.; Bringolf, R.; Yabsley, M.J. Possible Role of Fish as Transport Hosts for Dracunculus spp. Larvae. Emerg. Infect. Dis. 2017, 23, 1590–1592. [Google Scholar] [CrossRef]
- Karesh, W.B.; Cook, R.A. The Human-Animal Link. Foreign Aff. 2005, 84, 38–50. [Google Scholar] [CrossRef]
- Lee, K.; Brumme, Z.L. Operationalizing the One Health approach: The global governance challenges. Health Policy Plan. 2013, 28, 778–785. [Google Scholar] [CrossRef]
- The Carter Center. Guinea Worm Wrap-Up. Available online: https://www.cartercenter.org/news/publications/health/guinea_worm_wrapup_english.html (accessed on 12 March 2020).
- The Carter Center. Guinea Worm Wrap-Up, #222; The Carter Center: Atlanta, GA, USA, 2013; pp. 1–20. [Google Scholar]
- The Carter Center. Guinea Worm Wrap-Up, #223; The Carter Center: Atlanta, GA, USA, 2014; pp. 1–8. [Google Scholar]
- The Carter Center. Guinea Worm Wrap-Up, #262; The Carter Center: Atlanta, GA, USA, 2019; pp. 1–10. [Google Scholar]
- The Carter Center. Guinea Worm Wrap-Up, #238; The Carter Center: Atlanta, GA, USA, 2016; pp. 1–12. [Google Scholar]
- Wilson-Aggarwal, J.K.; Goodwin, C.E.D.; Swan, G.J.F.; Fielding, H.; Tadesse, Z.; Getahun, D.; Odiel, A.; Adam, A.; Marshall, H.H.; Bryant, J.; et al. Ecology of domestic dogs (Canis familiaris) as a host for Guinea worm (Dracunculus medinensis) infection in Ethiopia. Transbound. Emerg. Dis. 2020. [Google Scholar] [CrossRef] [PubMed]
- The Carter Center. Guinea Worm Wrap-Up, #265; The Carter Center: Atlanta, GA, USA, 2020; pp. 1–8. [Google Scholar]
- The Carter Center. Guinea Worm Wrap-Up, #263; The Carter Center: Atlanta, GA, USA, 2019; pp. 1–13. [Google Scholar]
- The Carter Center. Guinea Worm Wrap-Up, #231; The Carter Center: Atlanta, GA, USA, 2015; pp. 1–21. [Google Scholar]
- The Carter Center. Guinea Worm Wrap-Up, #235; The Carter Center: Atlanta, GA, USA, 2015; pp. 1–16. [Google Scholar]
- The Carter Center. Guinea Worm Wrap-Up, #246; The Carter Center: Atlanta, GA, USA, 2017; pp. 1–10. [Google Scholar]
- The Carter Center. Guinea Worm Wrap-Up, #252; The Carter Center: Atlanta, GA, USA, 2018; pp. 1–18. [Google Scholar]
- The Carter Center. Guinea Worm Wrap-Up, #256; The Carter Center: Atlanta, GA, USA, 2019; pp. 1–13. [Google Scholar]
- Callahan, K.; Bolton, B.; Hopkins, D.R.; Ruiz-Tiben, E.; Withers, P.C.; Meagley, K. Contributions of the Guinea Worm Disease Eradication Campaign toward Achievement of the Millennium Development Goals. PLoS Negl. Trop. Dis. 2013, 7, e2160. [Google Scholar] [CrossRef]
- The Carter Center. Guinea Worm Wrap-Up, #261; The Carter Center: Atlanta, GA, USA, 2019; pp. 1–9. [Google Scholar]
- Brieger, W.; Otusanya, S.; Adeniyi, D.; Tijani, J.; Banjoko, M. Eradicating guinea worm without wells: Unrealized hopes of the water decade. Health Policy Plan. 1997, 12, 354–362. [Google Scholar] [CrossRef] [PubMed]
- Hopkins, D.R.; Ruiz-Tiben, E. Dracunculiasis (Guinea Worm Disease): Case Study of the Effort to Eradicate Guinea Worm. In Water and Sanitation-Related Diseases and the Environment: Challenges, Interventions, and Preventive Measures, 1st ed.; Selendy, J.M.H., Ed.; Wiley-Blackwell: Hoboken, NJ, USA, 2011; pp. 125–132. [Google Scholar]
- Hopkins, D.R.; Ruiz-Tiben, E.; Eberhard, M.L.; Roy, S.L. Progress toward Global Eradication of Dracunculiasis, January 2014–June 2015. MMWR 2015, 64, 1161–1165. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Garrett, K.B.; Box, E.K.; Cleveland, C.A.; Majewska, A.A.; Yabsley, M.J. Dogs and the classic route of Guinea Worm transmission: An evaluation of copepod ingestion. Sci. Rep. 2020, 10, 1430. [Google Scholar] [CrossRef]
- The Carter Center. Guinea Worm Wrap-Up, #257; The Carter Center: Atlanta, GA, USA, 2018; pp. 1–16. [Google Scholar]
- The Carter Center. Guinea Worm Wrap-Up, #247; The Carter Center: Atlanta, GA, USA, 2017; pp. 1–10. [Google Scholar]
- The Carter Center. Guinea Worm Wrap-Up, #259; The Carter Center: Atlanta, GA, USA, 2019; pp. 1–13. [Google Scholar]
- The Carter Center. Guinea Worm Wrap-Up, #237; The Carter Center: Atlanta, GA, USA, 2015; pp. 1–13. [Google Scholar]
- The Carter Center. Guinea Worm Wrap-Up, #244; The Carter Center: Atlanta, GA, USA, 2016; pp. 1–13. [Google Scholar]
- The Carter Center. Guinea Worm Wrap-Up, #245; The Carter Center: Atlanta, GA, USA, 2017; pp. 1–13. [Google Scholar]
- The Carter Center. Guinea Worm Wrap-Up, #254; The Carter Center: Atlanta, GA, USA, 2018; pp. 1–9. [Google Scholar]
- The Carter Center. Guinea Worm Wrap-Up, #264; The Carter Center: Atlanta, GA, USA, 2019; pp. 1–13. [Google Scholar]
- Woolhouse, M.E.; Gowtage-Sequeria, S. Host range and emerging and reemerging pathogens. Emerg. Infect. Dis. 2005, 11, 1842–1847. [Google Scholar] [CrossRef]
- Dowdle, W.R. The Principles of Disease Elimination and Eradication. MMWR 1999, 48, 23–27. [Google Scholar]
- McGuinness, S.L.; Leder, K. Global burden of Toxocariasis: A common neglected infection of poverty. Curr. Trop. Med. Rep. 2014, 1, 52–61. [Google Scholar] [CrossRef]
- Etheart, M.D.; Kligerman, M.; Augustin, P.D.; Blanton, J.D.; Monroe, B.; Fleurinord, L.; Millien, M.; Crowdis, K.; Fenelon, N.; Wallace, R.M. Effect of counselling on health-care-seeking behaviours and rabies vaccination adherence after dog bites in Haiti, 2014–2015: A retrospective follow-up survey. Lancet Glob. Health 2017, 5, e1017–e1025. [Google Scholar] [CrossRef]
- Lushasi, K.; Steenson, R.; Bernard, J.; Changalucha, J.J.; Govella, N.J.; Haydon, D.T.; Hoffu, H.; Lankester, F.; Magoti, F.; Mpolya, E.A.; et al. One Health in Practice: Using Integrated Bite Case Management to Increase Detection of Rabid Animals in Tanzania. Front. Public Health 2020, 8, 13. [Google Scholar] [CrossRef]
- World Health Organization. Rabies: Rationale for Investing in the Global Elimination of Dog-Mediated Human Rabies; World Health Organization: Geneva, Switzerland, 2015; pp. 1–30. [Google Scholar]
- Cunningham, A.A.; Daszak, P.; Wood, J.L.N. One Health, emerging infectious diseases and wildlife: Two decades of progress? Phil. Trans. R. Soc. B 2017, 372, 20160167. [Google Scholar] [CrossRef] [PubMed]
- Buyon, L.; Slaven, R.; Emerson, P.M.; King, J.; Debrah, O.; Aboe, A.; Ruiz-Tiben, E.; Callahan, E.K. Achieving the endgame: Integrated NTD case searches. PLoS Negl. Trop. Dis. 2018, 12, e0006623. [Google Scholar] [CrossRef]
- The Carter Center. Guinea Worm Wrap-Up, #260; The Carter Center: Atlanta, GA, USA, 2019; pp. 1–12. [Google Scholar]
- The Carter Center. Guinea Worm Wrap-Up, #266; The Carter Center: Atlanta, GA, USA, 2020; pp. 1–8. [Google Scholar]
- Standley, C.; Boyce, M.R.; Klineberg, A.; Essix, G.; Katz, R. Organization of oversight for integrated control of neglected tropical diseases within Ministries of Health. PLoS Negl. Trop. Dis. 2018, 12, e0006929. [Google Scholar] [CrossRef] [PubMed]
- Cleveland, C.A.; Eberhard, M.L.; Thompson, A.T.; Garrett, K.B.; Swanepoel, L.; Zirimwabagabo, H.; Moundai, T.; Ouakou, P.T.; Ruiz-Tiben, E.; Yabsley, M.J. A search for tiny dragons (Dracunculus medinensis third-stage larvae) in aquatic animals in Chad, Africa. Sci. Rep. 2019, 9, 375. [Google Scholar] [CrossRef] [PubMed]
- Boonham, N.; Tomlinson, J.; Ostoja-Starzewska, S.; McDonald, R. A pond-side test for Guinea worm: Development of a loop-mediated isothermal amplification (LAMP) assay for detection of Dracunculiasis medinensis. Exp. Parasitol. 2020, 217, 107960. [Google Scholar] [CrossRef]
- Bardosh, K. Global aspirations, local realities: The role of social science research in controlling neglected tropical diseases. Infect. Dis. Poverty 2014, 3, 35. [Google Scholar] [CrossRef] [PubMed]
- The Carter Center. Guinea Worm Wrap-Up, #268; The Carter Center: Atlanta, GA, USA, 2020; pp. 1–12. [Google Scholar]
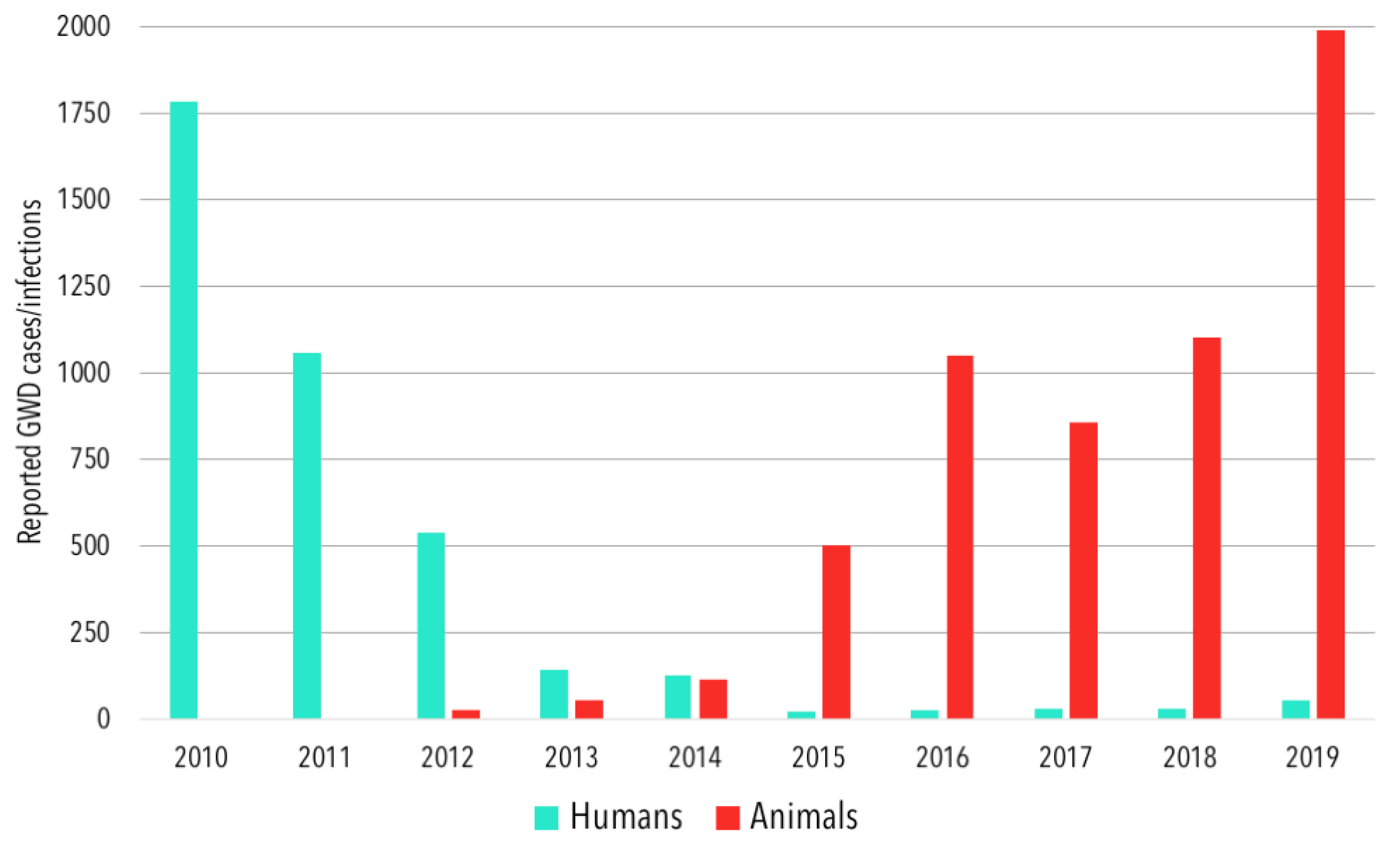
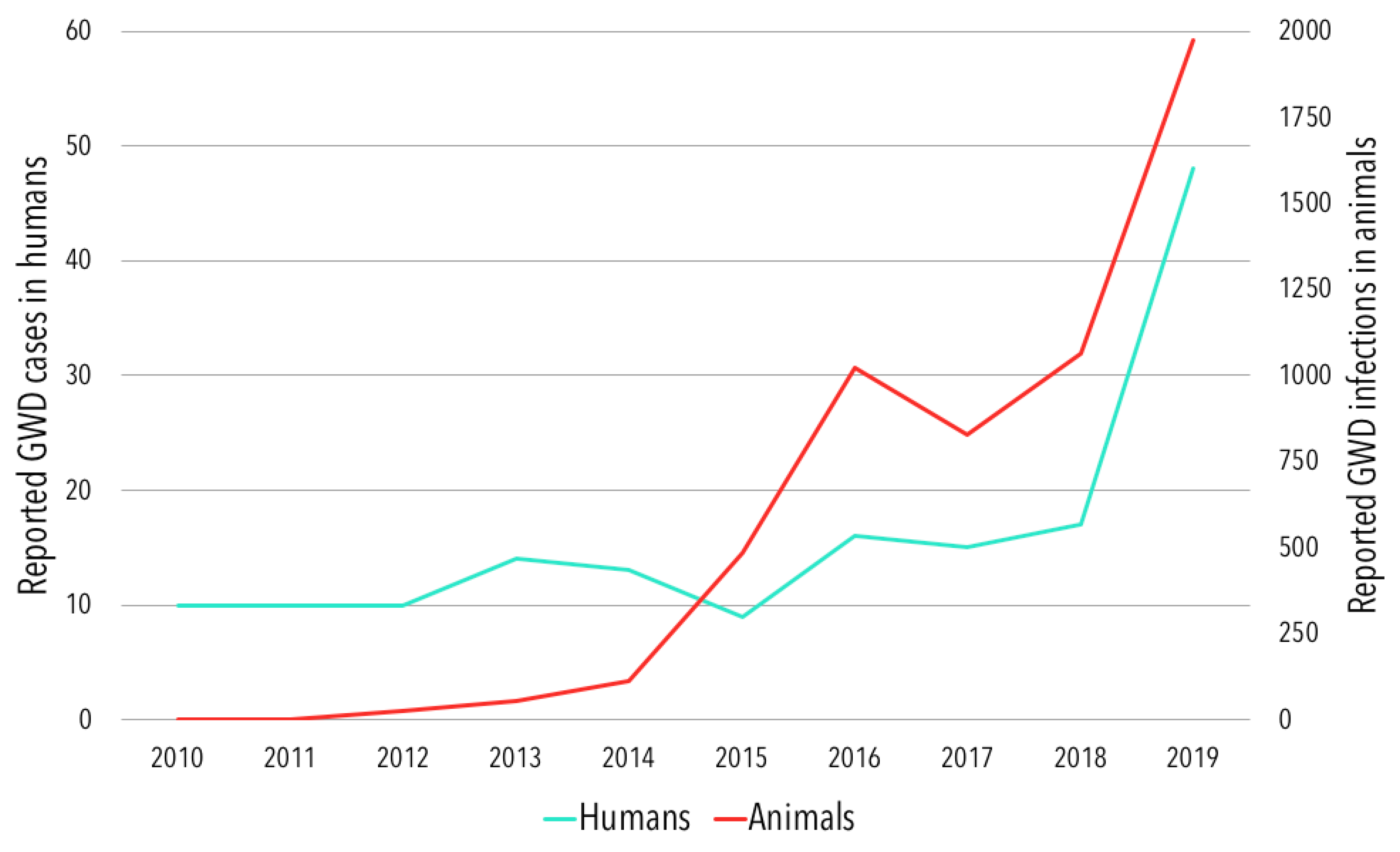
| Year | Country | Total | |||||
|---|---|---|---|---|---|---|---|
| Angola | Cameroon | Chad | Ethiopia | Mali | South Sudan | ||
| 2010 | 0 | 0 | 10 | 21 | 57 | 1698 | 1786 |
| 2011 | 0 | 0 | 10 | 8 | 12 | 1028 | 1058 |
| 2012 | 0 | 0 | 10 | 4 | 4 | 521 | 539 1 |
| 2013 | 0 | 0 | 14 | 7 | 11 | 113 | 145 2 |
| 2014 | 0 | 0 | 13 | 3 | 40 | 70 | 126 |
| 2015 | 0 | 0 | 9 | 3 | 5 | 5 | 22 |
| 2016 | 0 | 0 | 16 | 3 | 0 | 6 | 25 |
| 2017 | 0 | 0 | 15 | 15 | 0 | 0 | 30 |
| 2018 | 1 | 0 | 17 | 0 | 0 | 10 | 28 |
| 2019 | 1 | 1 3 | 47 | 0 | 0 | 4 | 53 |
| Year | Country | Total | |||||
|---|---|---|---|---|---|---|---|
| Angola | Cameroon | Chad | Ethiopia | Mali | South Sudan | ||
| 2015 | 0 | 0 | 487 (483) | 14 (13) | 1 (1) | 1 (1) | 503 (498) |
| 2016 | 0 | 0 | 1022 (1011) | 16 (14) | 11 (11) | 0 | 1049 (1036) |
| 2017 | 0 | 0 | 830 (817) | 15 (11) | 10 (9) | 0 | 855 (837) |
| 2018 | 0 | 1 (1) | 1065 (1040) | 17 (11) | 20 (18) | 0 | 1103 (1070) |
| 2019 | 1 (1) | 5 (5) 1 | 1973 (1927) | 8 (2) | 9 (8) | 0 | 1996 (1943) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Boyce, M.R.; Carlin, E.P.; Schermerhorn, J.; Standley, C.J. A One Health Approach for Guinea Worm Disease Control: Scope and Opportunities. Trop. Med. Infect. Dis. 2020, 5, 159. https://doi.org/10.3390/tropicalmed5040159
Boyce MR, Carlin EP, Schermerhorn J, Standley CJ. A One Health Approach for Guinea Worm Disease Control: Scope and Opportunities. Tropical Medicine and Infectious Disease. 2020; 5(4):159. https://doi.org/10.3390/tropicalmed5040159
Chicago/Turabian StyleBoyce, Matthew R., Ellen P. Carlin, Jordan Schermerhorn, and Claire J. Standley. 2020. "A One Health Approach for Guinea Worm Disease Control: Scope and Opportunities" Tropical Medicine and Infectious Disease 5, no. 4: 159. https://doi.org/10.3390/tropicalmed5040159
APA StyleBoyce, M. R., Carlin, E. P., Schermerhorn, J., & Standley, C. J. (2020). A One Health Approach for Guinea Worm Disease Control: Scope and Opportunities. Tropical Medicine and Infectious Disease, 5(4), 159. https://doi.org/10.3390/tropicalmed5040159







