PrEP Use Awareness and Interest Cascade among MSM and Transgender Women Living in Bali, Indonesia
Abstract
1. Introduction
2. Methods
2.1. Data and Samples
2.2. Procedures
2.3. Variables and Measures
- 1
- Classified as high risk for HIV infection: measured by questions on sexual behavior and STI diagnoses; those who reported any STI diagnoses in the last 6 months, >1 sexual partner in the last 6 months, and/or reported condom-less anal intercourse (CLAI) with MSM/waria partners in the last 6 months were classified as high risk.
- 2
- Self-perceived high risk for HIV infection: measured by the question, “Based on your sexual activities in the last 6 months, how likely do you perceive your risk of being infected with HIV?”; of 4 options provided for the participants (not at all at risk, less risky, risky, and highly risky) those answering “not at all” were classified as not perceiving themselves as high risk.
- 3
- Aware of PrEP: measured by the question, “Have you ever heard of or received information about PrEP?”; those answering “yes” were classified as being aware of PrEP.
- 4
- Interested in using PrEP: measured by the question, “Are you interested in using PrEP to protect yourself from HIV infection?”; those answering “yes” were classified as interested.
- 5
- Willing to do PrEP procedures: measured by the question, “How willing are you to take PrEP if it involves regular consultation visits including voluntary counselling and testing (VCT) and liver function check?”; those answering “yes” were considered to be willing to do PrEP procedures.
- 6
- Willing to pay 500,000 to 600,000 IDR for PrEP (the cost of locally available PrEP at the time): Measured by the question, “How willing are you to use PrEP if it costs 500,000–600,000 IDR per month?”; of the 5 options provided for the participants (highly unwilling, unwilling, slightly willing, willing, and highly willing) those answering “highly unwilling” and “unwilling” were classified as unwilling.
- 7
- Already in PrEP: measured by the question, “Have you ever used ARV as PrEP before any sexual activities?”; those answering “yes” were classified as already on PrEP.
2.4. Analysis
2.5. Ethical Consideration
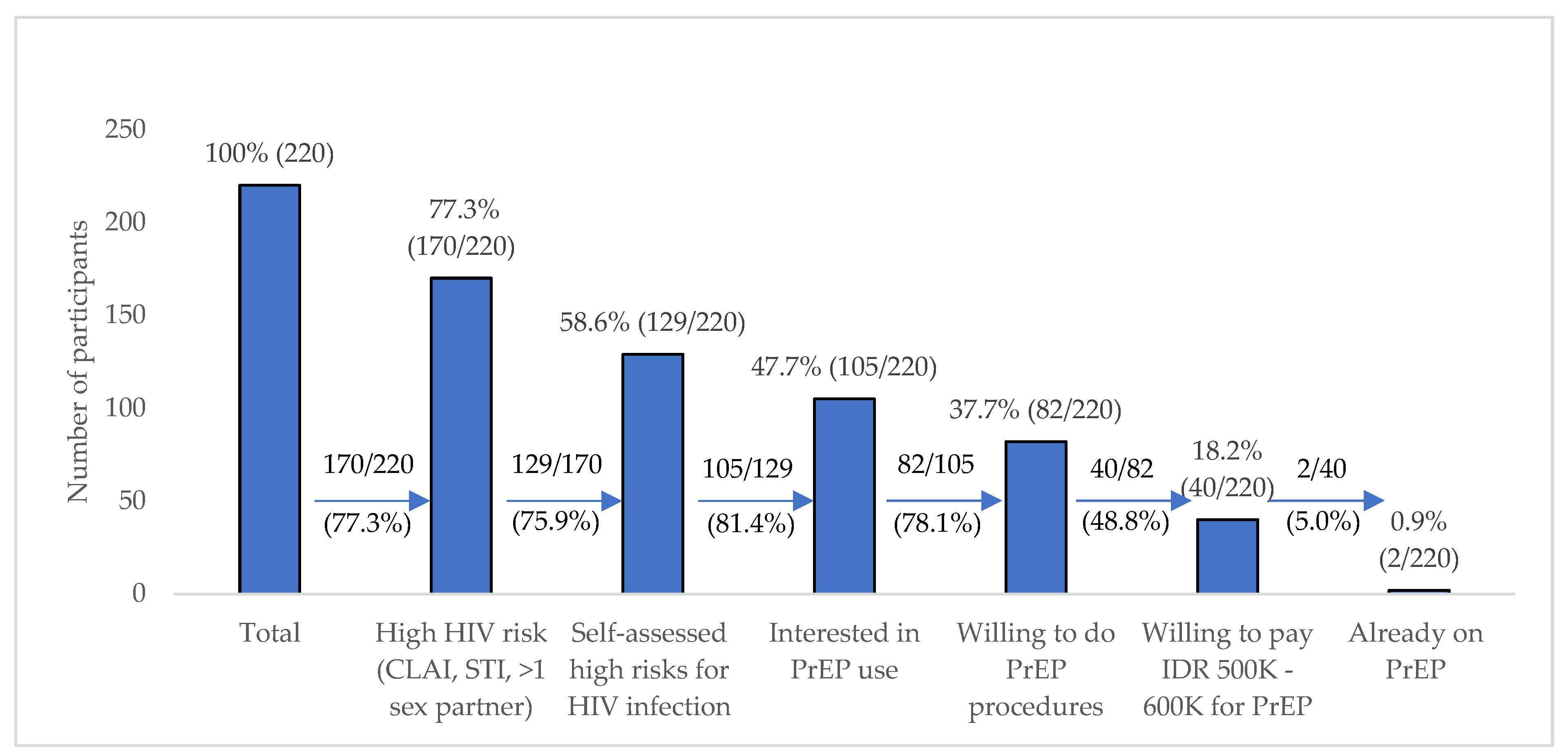
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- UNAIDS. Indonesia Country Data 2018. Available online: https://www.unaids.org/en/regionscountries/countries/indonesia (accessed on 14 April 2020).
- Kementerian Kesehatan Republik Indonesia. Survei Terpadu Biologis dan Perilaku 2018–2019; Kementerian Kesehatan Republik Indonesia: Jakarta, Indonesia, 2019.
- Kementerian Kesehatan Republik Indonesia. Survei Terpadu Biologis dan Perilaku 2015; Kementerian Kesehatan Republik Indonesia: Jakarta, Indonesia, 2016.
- WHO. Consolidated Guidelines on HIV Prevention, Diagnosis, Treatment and Care for Key Populations–2016 Update; World Health Organization: Geneva, Switzerland, 2016. Available online: https://www.who.int/hiv/pub/guidelines/keypopulations-2016/en/ (accessed on 14 April 2020).
- Johnson, W.D.; Hedges, L.V.; Ramirez, G.; Semaan, S.; Norman, L.R.; Sogolow, E.; Sweat, M.D.; Diaz, R.M. HIV prevention research for men who have sex with men: A systematic review and meta-analysis. J. Acquir. Immune Defic. Syndr. 2002, 30, S118–S129. [Google Scholar] [CrossRef] [PubMed]
- WHO. WHO HIV/AIDS Facts Sheet; World Health Organization: Geneva, Switzerland, 2019. Available online: https://www.who.int/news-room/fact-sheets/detail/hiv-aids (accessed on 9 April 2020).
- WHO. WHO Implementation Tool for Pre-Exposure Prophylaxis (PrEP) of HIV Infection: Module 11: PrEP Users; World Health Organization: Geneva, Switzerland, 2017.
- Donnell, D.; Baeten, J.M.; Bumpus, N.N.; Brantley, J.; Bangsberg, D.R.; Haberer, J.E.; Mujugira, A.; Mugo, N.; Ndase, P.; Hendrix, C.; et al. HIV protective efficacy and correlates of tenofovir blood concentrations in a clinical trial of PrEP for HIV prevention. J. Acquir. Immune Defic. Syndr. 2014, 66, 340–348. [Google Scholar] [CrossRef] [PubMed]
- Nicol, M.R.; Adams, J.L.; Kashuba, A.D. HIV PrEP trials: The road to success. Clin. Investig. 2013, 3, 295–308. Available online: https://pubmed.ncbi.nlm.nih.gov/24409341 (accessed on 9 September 2020). [CrossRef]
- Pinto, R.M.; Lacombe-Duncan, A.; Kay, E.S.; Berringer, K.R. Expanding knowledge about implementation of pre-exposure prophylaxis (PrEP): A methodological review. AIDS Behav. 2019, 23, 2761–2778. Available online: https://pubmed.ncbi.nlm.nih.gov/31292825 (accessed on 9 September 2020).
- Mallayasamy, S.; Chaturvedula, A.; Fossler, M.J.; Sale, M.E.; Hendrix, C.W.; Haberer, J.E. Assessment of demographic and socio-behavioral factors on adherence to HIV pre-exposure prophylaxis using a Markov modeling approach. Front. Pharmacol. 2019, 10, 785. Available online: https://www.frontiersin.org/article/10.3389/fphar.2019.00785 (accessed on 9 September 2020).
- Haberer, J.E.; Bangsberg, D.R.; Baeten, J.M.; Curran, K.; Koechlin, F.; Amico, K.R.; Anderson, P.; Mugo, N.; Venter, F.; Goicochea, P.; et al. Defining success with HIV pre-exposure prophylaxis: A prevention-effective adherence paradigm. AIDS 2015, 29, 1277. [Google Scholar] [CrossRef] [PubMed]
- Komisi Penanggulangan AIDS. Strategi Dan Rencana Aksi Nasional 2015–2019 Penanggulangan HIV Dan AIDS di Indonesia; Komisi Penanggulangan AIDS Nasional: Jakarta, Indonesia, 2015.
- Zablotska, I.; Grulich, A.E.; Phanuphak, N.; Anand, T.; Janyam, S.; Poonkasetwattana, M.; Baggaley, R.; van Griensven, F.; Lo, Y.-R. PrEP implementation in the Asia-Pacific region: Opportunities, implementation and barriers. J. Int. AIDS Soc. 2016, 19, 21119. [Google Scholar] [CrossRef] [PubMed]
- UNAIDS. Thailand Brings PrEP to Scale | UNAIDS. 2018. Available online: https://www.unaids.org/en/resources/presscentre/featurestories/2018/august/thailand-brings-prep-to-scale (accessed on 12 April 2020).
- PrePWatch. Thailand—PrEPWatch. PrepWatch.org. 2020. Available online: https://www.prepwatch.org/country/thailand/ (accessed on 5 October 2020).
- Thai National AIDS Committee. Thailand Ending AIDS: 2014 Thailand AIDS Response Progress Report; Ministry of Health: Bangkok, Thailand, 2014.
- WHO. WHO Implementation Tool for Pre-Exposure Prophylaxis (PrEP) of HIV Infection: Module 6: Pharmacist; World Health Organization: Geneva, Switzerland, 2017.
- Kementerian Kesehatan Republik Indonesia. Peraturan Mentri Kesehatan RI No 87 Tahun 2014 tentang Pedoman Pengobatan Antiretrovial; Kementerian Kesehatan RI: Jakarta, Indonesia, 2014; pp. 1–122.
- Jual Prep HIV | Tokopedia. Available online: https://www.tokopedia.com/search?nuq=prep hiv&nuq=prep hiv&ob=23&rf=true&rf=true&st=product&rf=true&nuq=prep hiv&q=prep HIV (accessed on 7 September 2020).
- Jual Truvada Murah—Harga Terbaru. 2020. Available online: https://www.tokopedia.com/find/truvada (accessed on 7 September 2020).
- Pulse-Clinic. PrEP THAILAND ONLINE SHOP—Asia’s Leading Sexual Healthcare Network. Available online: https://www.pulse-clinic.com/buypreponline/ (accessed on 14 April 2020).
- BaliMedika. PrEP—Satu Pil Sehari Mencegah Terinfeksi HIV—Bali Medika. Available online: https://www.balimedika.com/informasi-hiv/prep-satu-pil-sehari-mencegah-terinfeksi-hiv/ (accessed on 14 April 2020).
- Hidayat, R. Mengapa Obat Pencegah HIV Sulit Didapat di Indonesia?—BBC News Indonesia. BBC News Indonesia. 2016. Available online: https://www.bbc.com/indonesia/majalah/2016/10/161007_majalah_obat_pencegah_hiv (accessed on 14 April 2020).
- Adam, A. PrEP Masuk Indonesia, Siapkah Kita?—Tirto.ID [Internet]. Tirto.id. 2019. Available online: https://tirto.id/prep-masuk-indonesia-siapkah-kita-ekzf (accessed on 14 April 2020).
- Gombe, M.M.; Cakouros, B.E.; Ncube, G.; Zwangobani, N.; Mareke, P.; Mkwamba, A.; Prescott, M.R.; Bhatasara, T.; Murwira, M.; Mangwiro, A.Z.; et al. Key barriers and enablers associated with uptake and continuation of oral pre-exposure prophylaxis (PrEP) in the public sector in Zimbabwe: Qualitative perspectives of general population clients at high risk for HIV. PLoS ONE 2020, 15, e0227632. [Google Scholar] [CrossRef] [PubMed]
- Krishnaratne, S.; Hensen, B.; Cordes, J.; Enstone, J.; Hargreaves, J.R. Interventions to strengthen the HIV prevention cascade: A systematic review of reviews. Lancet HIV 2016, 3, e307–e317. [Google Scholar] [CrossRef]
- Hargreaves, J.R.; Delany-Moretlwe, S.; Hallett, T.B.; Johnson, S.; Kapiga, S.; Bhattacharjee, P.; Dallabetta, G.; Garnett, G.P. The HIV prevention cascade: Integrating theories of epidemiological, behavioural, and social science into programme design and monitoring. Lancet HIV 2016, 3, e318–e322. [Google Scholar] [CrossRef]
- Januraga, P.P.; Reekie, J.; Mulyani, T.; Lestari, B.W.; Iskandar, S.; Wisaksana, R.; Kusmayanti, N.A.; Subronto, Y.W.; Widyanthini, D.N.; Wirawan, D.N.; et al. The cascade of HIV care among key populations in Indonesia: A prospective cohort study. Lancet HIV 2018, 5, e560–e568. [Google Scholar] [CrossRef]
- Balitbangkes, K.K.R.I. Riset Kesehatan Dasar; Kementerian Kesehatan Republik Indonesia: Jakarta, Indonesia, 2010.
- Rismawati, N.L. UMP Bali 2020 Disepakati Rp2.494.000—ANTARA News. Antaranews. 2019. Available online: https://www.antaranews.com/berita/1140156/ump-bali-2020-disepakati-rp2494000 (accessed on 15 June 2020).
- Holt, M.; Lee, E.; Lea, T.; Bavinton, B.; Broady, T.; Mao, L.; MacGibbon, J.; Keen, P.; Murphy, D.; Bear, B.; et al. HIV preexposure prophylaxis cascades to assess implementation in Australia: Results from repeated, national behavioral surveillance of gay and bisexual men, 2014–2018. J. Acquir. Immune Defic. Syndr. 2020, 83, e16–e22. [Google Scholar] [CrossRef]
- Liu, A.; Colfax, G.; Cohen, S.; Bacon, O.; Kolber, M.; Amico, K.R.; Mugavero, M.; Grant, R.; Buchbinder, S. The spectrum of engagement in HIV prevention: Proposal for a PrEP cascade. In Proceedings of the International Conference on HIV Treatment and Prevention Adherence, Miami Beach, FL, USA, 3–5 June 2012. [Google Scholar]
- Schneider, K.; Gray, R.T.; Wilson, D.P. A cost-effectiveness analysis of HIV preexposure prophylaxis for men who have sex with men in Australia. Clin. Infect. Dis. 2014, 58, 1027–1034. [Google Scholar] [CrossRef]
- WHO. WHO Implementation Tool for Pre-Exposure Prophylaxis (PrEP) of HIV Infection: Module 5: Monitoring and Evaluation; World Health Organization: Geneva, Switzerland, 2017.
- Umboh, L.; Romyco, I. Awareness, knowledge and willingness to use HIV PrEP among MSM and TG people in Bali, Indonesia. Sex. Transm. Infect. 2019, 95 (Suppl. S1), A213. Available online: http://sti.bmj.com/content/95/Suppl_1/A213.2.abstract (accessed on 9 September 2020).
- Seekaew, P.; Pengnonyang, S.; Jantarapakde, J.; Meksena, R.; Sungsing, T.; Lujintanon, S.; Mingkwanrungruangkit, P.; Sirisakyot, W.; Tongmuang, S.; Panpet, P.; et al. Discordance between self-perceived and actual risk of HIV infection among men who have sex with men and transgender women in Thailand: A cross-sectional assessment. J. Int. AIDS Soc. 2019, 22, e25430. [Google Scholar] [CrossRef] [PubMed]
- Koh, K.C.; Yong, L.S. HIV risk perception, sexual behavior, and HIV prevalence among men-who-have-sex-with-men at a community-based voluntary counseling and testing center in Kuala Lumpur, Malaysia. Interdiscip. Perspect. Infect. Dis. 2014, 2014, 1–6. [Google Scholar] [CrossRef]
- Freeborn, K.; Portillo, C.; Boyer, C.B.; Santos, G.M. Misclassification of sexual health risks in a self-identified low risk cohort of men who have sex with men (MSM) enrolled in a community based PrEP program. AIDS Care 2020, 32, 230–237. [Google Scholar] [CrossRef]
- Frankis, J.S.; Young, I.; Lorimer, K.; Davis, M.; Flowers, P. Towards preparedness for PrEP: PrEP awareness and acceptability among MSM at high risk of HIV transmission who use sociosexual media in four Celtic nations: Scotland, Wales, Northern Ireland and The Republic of Ireland: An online survey. Sex. Transm. Infect. 2016, 92, 279–285. [Google Scholar] [CrossRef][Green Version]
- Thoma, B.C.; Huebner, D.M. HIV pre-exposure prophylaxis engagement among adolescent men who have sex with men: The role of parent-adolescent communication about sex. J. Acquir. Immune Defic. Syndr. 2018, 79, 453. [Google Scholar] [CrossRef] [PubMed]
- Oldenburg, C.E.; Le, B.; Huyen, H.T.; Thien, D.D.; Quan, N.H.; Biello, K.B.; Nunn, A.; Chan, P.A.; Mayer, K.H.; Mimiaga, M.J.; et al. Antiretroviral pre-exposure prophylaxis preferences among men who have sex with men in Vietnam: Results from a nationwide cross-sectional survey. Sex. Health 2016, 13, 465–473. [Google Scholar] [CrossRef]
- Draper, B.L.; Oo, Z.M.; Thein, Z.W.; Aung, P.P.; Veronese, V.; Ryan, C.; Thant, M.; Hughes, C.; Stoové, M. Willingness to use HIV pre-exposure prophylaxis among gay men, other men who have sex with men and transgender women in Myanmar. J. Int. AIDS Soc. 2017, 20, 21885. [Google Scholar] [CrossRef]
- Ren, Y. Awareness and willingness to use pre-exposure prophylaxis (prep) amongst men who have sex with men (MSM) in China: A mini-review. J. HIV AIDS Infect. Dis. 2019, 5, 1–13. [Google Scholar]
- Dubov, A.; Galbo, P., Jr.; Altice, F.L.; Fraenkel, L. Stigma and shame experiences by MSM who take PrEP for HIV prevention: A qualitative study. Am. J. Men’s Health 2018, 12, 1843–1854. [Google Scholar] [CrossRef]
- Plotzker, R.; Seekaew, P.; Jantarapakde, J.; Pengnonyang, S.; Trachunthong, D.; Linjongrat, D.; Janyam, S.; Nakpor, T.; Charoenying, S.; Mills, S.; et al. Importance of risk perception: Predictors of PrEP acceptance among Thai MSM and TG women at a community-based health service. J. Acquir. Immune Defic. Syndr. 2017, 76, 473–481. [Google Scholar] [CrossRef] [PubMed]
- Binfar, D. Pedoman Pelayanan Kefarmasian Untuk Orang Dengan HIV/AIDS (ODHA); Departemen Kesehatan Republik Indonesia: Jakarta, Indonesia, 2006.
- Suharni, M. Integrasi Upaya Penanggulangan HIV dan AIDS ke Dalam Sistem Kesehatan; Pusat Kebijakan & Manajemen Kesehatan, Fakultas Kedokteran Universitas Gadjah Mada: Yogyakarta, Indonesia, 2015.
- Cairns, G. PrEP Use Taking off in Thailand and Vietnam | Aidsmap. Aidsmap. 2018. Available online: http://www.aidsmap.com/news/aug-2018/prep-use-taking-thailand-and-vietnam (accessed on 16 April 2020).
- Cairns, G. Taking PrEP During Acute HIV Infection for More than 2–3 Weeks is Likely to Cause Resistance, Thai Study Finds | Aidsmap. Aidsmap. 2020. Available online: http://www.aidsmap.com/news/mar-2020/taking-prep-during-acute-hiv-infection-more-2–3-weeks-likely-cause-resistance-thai (accessed on 14 April 2020).
| Variable | Number of Participants (n = 220) |
|---|---|
| Demography | |
| Age (years) | |
| <25 | 67 (30.5%) |
| 25–29 | 66 (30.0%) |
| 30–39 | 73 (33.2%) |
| 40 and above | 14 (6.4%) |
| Not married to a woman | 200 (90.9%) |
| Education | |
| Primary education | 26 (11.8%) |
| Senior high school | 128 (58.2%) |
| University | 66 (30.0%) |
| Full-time employee | 163 (74.1%) |
| Income more than Bali minimum wage | 105 (47.7%) |
| High social engagement as MSM/waria | 68 (30.9%) |
| Adequate HIV risks/prevention knowledge | 93 (42.3%) |
| Sexual and HIV Prevention-Related Behavior in the Last 6 Months | |
| Sex with women | 73 (33.2%) |
| Multiple sex partner | 111 (50.5%) |
| Sex with the regular partner/s | 126 (57.3%) |
| Inconsistent condom use | 136 (61.8%) |
| Sex with casual partner/s | 128 (58.2%) |
| Paid for sex | 34 (15.5%) |
| Sexually transmitted infection (STI) diagnoses | 26 (11.8%) |
| Assessed HIV high risk | 170 (77.3%) |
| Self-assessed HIV high risk | 150 (68.2%) |
| PrEP Awareness and Interest | |
| Have heard of PrEP before | 36 (16.4%) |
| Want to use PrEP | 164 (74.5%) |
| Willing to do PrEP procedures | 134 (60.9%) |
| Willing to pay 500K–600K IDR | 84 (38.2%) |
| Have been in PrEP before | 2 (0.9%) |
| Variables | Self-Perception of no HIV Risk | Self-Perception of High HIV Risk | Crude Odds Ratio (OR) | Adjusted OR (aOR) | ||||
|---|---|---|---|---|---|---|---|---|
| n = 41, n (%) | n = 129, n (%) | OR | 95% CI | p-Value | aOR | 95% CI | p-Value | |
| Age | ||||||||
| <25 years | 4 (9.8) | 49 (38.0) | Ref | Ref | Ref | |||
| 25–29 years | 10 (24.4) | 45 (34.9) | 0.37 | 0.11–1.25 | 0.110 * | 0.30 | 0.11–1.30 | 0.0073 |
| 30–39 years | 22 (53.7) | 30 (23.3) | 0.11 | 0.03–0.35 | 0.000 * | 0.07 | 0.03–0.29 | 0.000 ** |
| 40 and above | 5 (12.2) | 5 (3.9) | 0.08 | 0.02–0.41 | 0.002 * | 0.06 | 0.01–0.34 | 0.002 ** |
| Education | ||||||||
| Less than senior high school | 8 (19.6) | 15 (11.6) | Ref | Ref | Ref | Ref | Ref | Ref |
| Senior high school | 23 (56.1) | 72 (55.8) | 1.67 | 0.63–4.44 | 0.304 | 1.43 | 0.44–4.69 | 0.552 |
| University | 10 (24.4) | 42 (32.6) | 2.24 | 0.74–6.74 | 0.151 * | 2.51 | 0.68–9.26 | 0.167 |
| Income more than Bali minimum wage | 22 (53.7) | 59 (45.7) | 0.73 | 0.36–1.47 | 0.377 | |||
| High social engagement as MSM/waria | 13 (31.7) | 42 (32.6) | 1.04 | 0.49–2.21 | 0.919 | |||
| Adequate HIV risk/prevention knowledge | 15 (36.6) | 61 (47.3) | 1.55 | 0.75–3.21 | 0.232 * | 2.10 | 0.89–4.95 | 0.088 |
| Sex with women in the last 6 months | 17 (41.5) | 43 (33.3) | 0.71 | 0.34–1.45 | 0.344 | |||
| >1 MSM/waria sex partner in the last 6 months | 20 (48.8) | 91 (70.5) | 2.51 | 1.22–5.17 | 0.012 * | 3.08 | 1.23–7.72 | 0.016 ** |
| Inconsistent condom use in the last 6 months | 36 (87.8) | 93 (72.1) | 0.36 | 0.13–2.30 | 0.047 * | 0.57 | 0.18–1.83 | 0.348 |
| Paid sex in the last 6 months | 8 (19.5) | 24 (18.6) | 0.94 | 0.39–2.3 | 0.897 | |||
| STI diagnoses in the last 6 months | 3 (7.3) | 23 (17.8) | 2.75 | 0.78–9.68 | 0.115 * | 2.44 | 0.61–9.74 | 0.206 |
| Variables | Not Interested In Prep Use | Interested in PrEP Use | Crude OR (OR) | Adjusted OR (aOR) | ||||
|---|---|---|---|---|---|---|---|---|
| n = 24, n (%) | n = 105, n (%) | OR | 95% CI | p-Value | aOR | 95% CI | p-Value | |
| Age | ||||||||
| <25 years | 12 (50.0) | 37 (35.2) | Ref | Ref | Ref | Ref | Ref | Ref |
| 25–29 years | 4 (16.7) | 41 (39.1) | 3.32 | 0.99–11.21 | 0.053 * | 4.23 | 0.96–18.60 | 0.056 |
| 30–39 years | 6 (25.0) | 24 (22.9) | 1.30 | 0.43–3.92 | 0.645 | 1.59 | 0.40–6.30 | 0.509 |
| 40 and above | 2 (8.3) | 3 (2.9) | 0.49 | 0.07–3.27 | 0.458 | 1.57 | 0.15–16.95 | 0.707 |
| Education | ||||||||
| Less than senior high school | 1 (4.17) | 14 (13.3) | Ref | Ref | Ref | Ref | Ref | Ref |
| Senior high school | 14 (58.3) | 58 (55.2) | 0.30 | 0.04–2.44 | 0.258 | 0.31 | 0.03–3.23 | 0.330 |
| University | 9 (37.5) | 33 (31.4) | 0.26 | 0.03–2.27 | 0.224 * | 0.26 | 0.02–3.41 | 0.303 |
| Income more than Bali minimum wage | 15 (62.5) | 44 (41.9) | 0.43 | 0.17–1.08 | 0.072 * | 0.38 | 0.10–1.43 | 0.151 |
| High social engagement as MSM/waria | 15 (62.5) | 27 (25.7) | 0.21 | 0.08–0.53 | 0.001 * | 0.17 | 0.06–0.51 | 0.002 ** |
| Adequate HIV risk/prevention knowledge | 13 (54.2) | 48 (45.7) | 0.71 | 0.29–1.74 | 0.455 | |||
| Sex with women in the last 6 months | 5 (20.8) | 38 (36.2) | 2.16 | 0.74–6.24 | 0.157 * | 1.37 | 0.38–4.88 | 0.628 |
| >1 MSM/waria sex partner in the last 6 months | 14 (58.3) | 77 (73.3) | 1.96 | 0.78–4.93 | 0.150 * | 4.26 | 1.26–14.45 | 0.020 ** |
| Inconsistent condom use in the last 6 months | 14 (58.3) | 79 (75.2) | 2.17 | 0.86–5.47 | 0.100 * | 4.80 | 1.43–16.09 | 0.011 ** |
| Paid sex in the last 6 months | 3 (12.5) | 21 (20.0) | 1.75 | 0.48–6.43 | 0.399 | |||
| STI diagnoses in the last 6 months | 3 (12.5) | 20 (19.1) | 1.65 | 0.45–6.07 | 0.453 | |||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cempaka, R.; Wardhani, B.; Sawitri, A.A.S.; Januraga, P.P.; Bavinton, B. PrEP Use Awareness and Interest Cascade among MSM and Transgender Women Living in Bali, Indonesia. Trop. Med. Infect. Dis. 2020, 5, 158. https://doi.org/10.3390/tropicalmed5040158
Cempaka R, Wardhani B, Sawitri AAS, Januraga PP, Bavinton B. PrEP Use Awareness and Interest Cascade among MSM and Transgender Women Living in Bali, Indonesia. Tropical Medicine and Infectious Disease. 2020; 5(4):158. https://doi.org/10.3390/tropicalmed5040158
Chicago/Turabian StyleCempaka, Rissa, Brigitta Wardhani, Anak Agung Sagung Sawitri, Pande Putu Januraga, and Benjamin Bavinton. 2020. "PrEP Use Awareness and Interest Cascade among MSM and Transgender Women Living in Bali, Indonesia" Tropical Medicine and Infectious Disease 5, no. 4: 158. https://doi.org/10.3390/tropicalmed5040158
APA StyleCempaka, R., Wardhani, B., Sawitri, A. A. S., Januraga, P. P., & Bavinton, B. (2020). PrEP Use Awareness and Interest Cascade among MSM and Transgender Women Living in Bali, Indonesia. Tropical Medicine and Infectious Disease, 5(4), 158. https://doi.org/10.3390/tropicalmed5040158






