A Rapid Assessment of Health Literacy and Health Status of Rohingya Refugees Living in Cox’s Bazar, Bangladesh Following the August 2017 Exodus from Myanmar: A Cross-Sectional Study
Abstract
1. Introduction
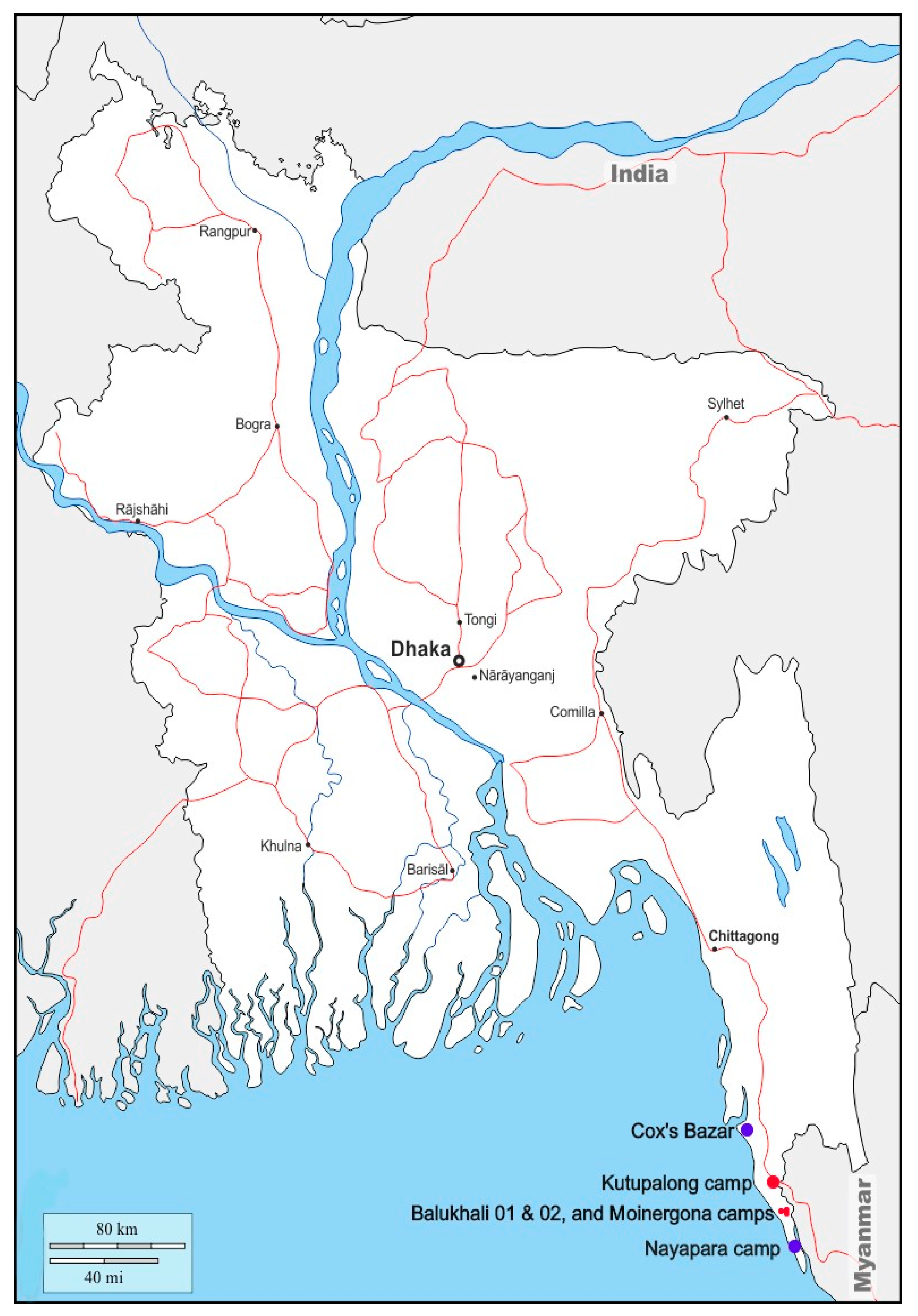
2. Materials and Methods
3. Results
3.1. Demographics
3.2. Health Literacy and Health Status
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Mahmood, S.S.; Wroe, E.; Fuller, A.; Leaning, J. The Rohingya people of Myanmar: Health, human rights, and identity. Lancet 2017, 389, 1841–1850. [Google Scholar] [CrossRef]
- Bhatia, A.; Mahmud, A.; Fuller, A.; Shin, R.; Rahman, A.; Shatil, T.; Sultana, M.; Morshed, K.A.M.; Leaning, J.; Balsari, S. The Rohingya in Cox’s Bazar: When the Stateless Seek Refuge. Health Hum. Rights 2018, 20, 105–122. [Google Scholar] [PubMed]
- Lancet. Recognising the Rohingya people. Lancet 2016, 388, 2714. [Google Scholar] [CrossRef]
- Lancet. Last days of the Rohingya of Rakhine. Lancet 2017, 390, 1466. [Google Scholar] [CrossRef][Green Version]
- Villasana, D. Picturing health: Rohingya refugees in Bangladesh. Lancet 2017, 390, 2233–2242. [Google Scholar] [CrossRef]
- White, K. Rohingya in Bangladesh: An unfolding public health emergency. Lancet 2017, 390, 1947. [Google Scholar] [CrossRef]
- Karo, B.; Haskew, C.; Khan, A.S.; Polonsky, J.A.; Mazhar, M.K.A.; Buddha, N. World Health Organization Early Warning, Alert and Response System in the Rohingya Crisis, Bangladesh, 2017–2018. Emerg. Infect. Dis. 2018, 24, 2074–2076. [Google Scholar] [CrossRef] [PubMed]
- Cousins, S. Rohingya threatened by infectious diseases. Lancet Infect. Dis. 2018, 18, 609–610. [Google Scholar] [CrossRef]
- Chan, E.Y.Y.; Chiu, C.P.; Chan, G.K.W. Medical and health risks associated with communicable diseases of Rohingya refugees in Bangladesh 2017. Int. J. Infect. Dis. 2018, 68, 39–43. [Google Scholar] [CrossRef] [PubMed]
- Medicins Sans Frontiers (MSF). Health Survey in Kutupalong and Balukhali Refugee Settlements, Cox’s Bazar, Bangladesh; Médecins Sans Frontières: Geneva, Switzerland, 2017; Available online: https://www.msf.org/sites/msf.org/files/coxsbazar_healthsurveyreport_dec2017_final1.pdf (accessed on 1 July 2020).
- Leidman, E.; Humphreys, A.; Greene Cramer, B.; Toroitich-Van Mil, L.; Wilkinson, C.; Narayan, A.; Bilukha, O. Acute Malnutrition and Anemia Among Rohingya Children in Kutupalong Camp, Bangladesh. JAMA 2018, 319, 1505–1506. [Google Scholar] [CrossRef]
- Hsan, K.; Naher, S.; Gozal, D.; Griffiths, M.D.; Furkan Siddique, M.R. Varicella outbreak among the Rohingya refugees in Bangladesh: Lessons learned and potential prevention strategies. Travel Med. Infect. Dis. 2019, 31, 101465. [Google Scholar] [CrossRef] [PubMed]
- Rahman, M.R.; Islam, K. Massive diphtheria outbreak among Rohingya refugees: Lessons learnt. J. Travel Med. 2019, 26, tay122. [Google Scholar] [CrossRef]
- Summers, A.; Humphreys, A.; Leidman, E.; Van Mil, L.T.; Wilkinson, C.; Narayan, A.; Miah, M.L.; Cramer, B.G.; Bilukha, O. Notes from the Field: Diarrhea and Acute Respiratory Infection, Oral Cholera Vaccination Coverage, and Care-Seeking Behaviors of Rohingya Refugees—Cox’s Bazar, Bangladesh, October–November 2017. Morb. Mortal. Wkly. Rep. 2018, 67, 533–535. [Google Scholar] [CrossRef] [PubMed]
- Lancet. Our responsibility to protect the Rohingya. Lancet 2018, 390, 2740. [Google Scholar]
- Riley, A.; Varner, A.; Ventevogel, P.; Taimur Hasan, M.M.; Welton-Mitchell, C. Daily stressors, trauma exposure, and mental health among stateless Rohingya refugees in Bangladesh. Transcult. Psychiatry 2017, 54, 304–331. [Google Scholar] [CrossRef] [PubMed]
- Landry, M.D.; Tupetz, A. Disability and the Rohingya Displacement Crisis: A Humanitarian Priority. Arch. Phys. Med. Rehabil. 2018, 99, 2122–2124. [Google Scholar] [CrossRef]
- Tay, A.K.; Riley, A.; Islam, R.; Welton-Mitchell, C.; Duchesne, B.; Waters, V.; Varner, A.; Moussa, B.; Mahmudul Alam, A.N.M.; Elshazly, M.A.; et al. The culture, mental health and psychosocial wellbeing of Rohingya refugees: A systematic review. Epidemiol. Psychiatr. Sci. 2019, 28, 489–494. [Google Scholar] [CrossRef]
- Parmar, P.K.; Leigh, J.; Venters, H.; Nelson, T. Violence and mortality in the Northern Rakhine State of Myanmar, 2017: Results of a quantitative survey of surviving community leaders in Bangladesh. Lancet Planet Health 2019, 3, e144–e153. [Google Scholar] [CrossRef]
- Physicians for Human Rights. The Chut Pyin Massacre: Forensic Evidence of Violence against the Rohingya in Myanmar. Available online: https://rohingya.phr.org/resources/chutpyin/?ms=homepagebanner (accessed on 31 May 2020).
- World Health Organization (WHO). Health Literacy: The Solid Facts; World Health Organization: Geneva, Switzerland, 2013; Available online: https://apps.who.int/iris/bitstream/handle/10665/128703/e96854.pdf (accessed on 1 July 2020).
- World Bank. Poverty. Available online: https://www.worldbank.org/en/topic/poverty (accessed on 31 May 2020).
- Peters, D.H.; Garg, A.; Bloom, G.; Walker, D.G.; Brieger, W.R.; Rahman, M.H. Poverty and access to health care in developing countries. Ann. NY Acad. Sci. 2008, 1136, 161–171. [Google Scholar] [CrossRef]
- World Health Organization (WHO). WHO Traditional Medicine Strategy: 2014–2023. Available online: https://www.who.int/medicines/publications/traditional/trm_strategy14_23/en/ (accessed on 31 May 2020).
- Khan, M.U.; Munshi, M.H. Clinical illnesses and causes of death in a Burmese refugee camp in Bangladesh. Int. J. Epidemiol. 1983, 12, 460–464. [Google Scholar] [CrossRef]
- Han, A.M.; Myint, T.M. Knowledge, attitudes and behaviour in relation to diarrhoea in a rural community in Burma. Southeast Asian J. Trop Med. Public Health 1986, 17, 59–62. [Google Scholar] [PubMed]
- Knoema Myanmar—Assault Rate. Available online: https://knoema.com/atlas/Myanmar/topics/Crime-Statistics/Assaults-Kidnapping-Robbery-Sexual-Rape/Assault-rate (accessed on 31 May 2020).
- Friedrich, M.J. High Rates of Violent Death Among Rohingya Refugees. JAMA 2018, 319, 648. [Google Scholar] [CrossRef] [PubMed]
- Mahmood, M.A.; Halliday, D.; Cumming, R.; Thwin, K.T.; Kyaw, M.M.Z.; White, J.; Alfred, S.; Warrell, D.; Bacon, D.; Naing, W.; et al. Snakebite incidence in two townships in Mandalay Division, Myanmar. PLoS Negl. Trop. Dis. 2018, 12, e0006643. [Google Scholar] [CrossRef] [PubMed]
- Mu, T.T.; Sein, A.A.; Soe, C.; Phyu Aung, N.P.; Kyi, T.T.; Hanson, J. Rabies in Myanmar: Prevalent, Preventable but not Prioritized. Am. J. Trop. Med. Hyg. 2017, 97, 989–991. [Google Scholar] [CrossRef][Green Version]
- Khan, N.Z.; Shilpi, A.B.; Sultana, R.; Sarker, S.; Razia, S.; Roy, B.; Arif, A.; Ahmed, M.U.; Saha, S.C.; McConachie, H. Displaced Rohingya children at high risk for mental health problems: Findings from refugee camps within Bangladesh. Child. Care Health Dev. 2019, 45, 28–35. [Google Scholar] [CrossRef]
- Tay, A.K.; Rees, S.; Miah, M.A.A.; Khan, S.; Badrudduza, M.; Morgan, K.; Fadil Azim, D.; Balasundaram, S.; Silove, D. Functional impairment as a proxy measure indicating high rates of trauma exposure, post-migration living difficulties, common mental disorders, and poor health amongst Rohingya refugees in Malaysia. Transl. Psychiatry 2019, 9, 213. [Google Scholar] [CrossRef]
- ABC News. A Coronavirus Crisis is Building Inside Cox’s Bazar, the World’s Largest Refugee Camp. Available online: https://www.abc.net.au/news/2020-06-16/rohingya-refugees-coxs-bazar-coronavirus/12356046 (accessed on 22 June 2020).
- Jalloh, M.F.; Bennett, S.D.; Alam, D.; Kouta, P.; Lourenco, D.; Alamgir, M.; Feldstein, L.R.; Ehlman, D.C.; Abad, N.; Kapil, N.; et al. Rapid behavioral assessment of barriers and opportunities to improve vaccination coverage among displaced Rohingyas in Bangladesh, January 2018. Vaccine 2019, 37, 833–838. [Google Scholar] [CrossRef]
| Particulars (N = 1634) | Overall n (%) | Male n (%) | Female n (%) | p Value |
|---|---|---|---|---|
| Number of participants | 1634 | 913 (55.9) | 721 (44.1) | |
| Age in years (median, mean ± SD) | 10–90 (32, 36.3 ± 13.8) | 10–90 (35, 37.7 ± 14.6) | 10–80 (30, 34.4 ± 12.5) | <0.01 |
| Children (aged < 18 years) | 9 (0.6) | 7 (0.8) | 2 (0.3) | 0.19 |
| Occupation in Myanmar | ||||
| Farmer | 423 (25.9) | 393 (43.0) | 30 (4.2) | <0.01 |
| Homemaker | 629 (38.5) | 5 (0.5) | 624 (86.5) | <0.01 |
| Grocery businessman | 211 (12.9) | 199 (21.8) | 12 (1.7) | <0.01 |
| Sedentary workers | 58 (3.5) | 56 (6.1) | 2 (0.3) | <0.01 |
| Fisherman | 32 (2) | 32 (3.5) | 0 (0) | <0.01 |
| Student | 32 (2) | 24 (2.6) | 8 (1.1) | 0.03 |
| Labourer | 108 (6.6) | 97 (10.6) | 11 (1.5) | <0.01 |
| Others | 95 (5.8) | 77 (8.4) | 18 (2.5) | <0.01 |
| Retired | 32 (2.0) | 25 (2.7) | 7 (0.8) | 0.01 |
| Unemployed | 14 (0.9) | 5 (0.5) | 9 (1.2) | 0.13 |
| Years of education received | ||||
| No education | 389 (23.8) | 241 (26.4) | 148 (20.5) | 0.01 |
| 1–5 years | 834 (51.1) | 403 (44.1) | 431 (59.8) | <0.01 |
| 6–10 years | 340 (20.7) | 208 (22.8) | 132 (18.3) | 0.03 |
| 11–12 years | 51 (3.2) | 41 (4.5) | 10 (1.4) | <0.01 |
| >12 years | 20 (1.3) | 20 (2.2) | 0 (0) | <0.01 |
| Particulars (N = 1634) | Overall n (%) |
|---|---|
| Owned lands in Rakhine | 1278 (78.2) |
| Total arable land in acres, range (median; IQR) | 0.4–144 (2; 0.8–4.0) |
| Own gold/jewelleries | 1310 (80.2) |
| Total amount of gold in grams, range (median) | 1–478 (23.3) |
| Family income per month in US$ before migration, range (median; IQR) | 0–5200 (65; 65–195) |
| Have money deposited in a bank | 12 (0.7) |
| Roof of your Myanmar house built with | |
| Leaves | 909 (55.6) |
| Thatched | 597 (36.5) |
| Corrugated iron sheets | 111 (6.8) |
| Others | 17 (1) |
| At home, where did you usually get your drinking water from? | |
| Tube well | 1316 (80.5) |
| Pond | 174 (10.6) |
| Deep well | 105 (6.4) |
| Other sources | 39 (2.4) |
| Have sanitary latrine for the family in Myanmar | 1583 (96.9) |
| One latrine | 1267 (77.5) |
| More than one latrine | 316 (19.3) |
| Particulars | Overall n (%) | Male n (%) | Female n (%) | p Value |
|---|---|---|---|---|
| Total number of participants | 6268 | 2973 (47.4) | 3295 (52.6) | |
| Age in years range (median, mean ± SD) | 0.1–120 (12, 15.9 ± 14.6) | 0.1–98 (11, 15.1 ± 14.7) | 0.1–120 (13, 16.5 ± 14.4) | <0.01 |
| Children (aged < 18 years) | 4163 (66.4) | 2114 (71.1) | 2049 (62.2) | <0.01 |
| Occupation in Myanmar | ||||
| Student | 2217 (35.4) | 1129 (38.0) | 1088 (33.0) | <0.01 |
| Homemaker | 1111 (17.7) | 19 (0.6) | 1092 (33.1) | <0.01 |
| Farmer | 363 (5.8) | 339 (11.4) | 24 (0.7) | <0.01 |
| Grocery businessman | 198 (3.2) | 189 (6.4) | 9 (0.3) | <0.01 |
| Labourer | 150 (2.4) | 145 (4.9) | 5 (0.2) | <0.01 |
| Others | 334 (5.3) | 182 (6.1) | 152 (4.6) | 0.01 |
| Unemployed or too young to be employed | 1832 (29.2) | 940 (31.6) | 892 (27.1) | <0.01 |
| Retired | 63 (1) | 30 (1) | 33 (1) | 0.98 |
| Years of education received | ||||
| No education | 2064 (32.9) | 1057 (35.6) | 1007 (30.6) | <0.01 |
| 1–5 years | 3322 (52.9) | 1434 (48.2) | 1888 (57.3) | <0.01 |
| 6–10 years | 810 (13) | 423 (14.2) | 387 (11.7) | <0.01 |
| 11–12 years | 51 (0.8) | 39 (1.3) | 12 (0.4) | <0.01 |
| >12 years | 21 (0.3) | 20 (0.7) | 1 (0.03) | <0.01 |
| Ever received a vaccine | 5255 (83.8) | 2475 (83.2) | 2780 (84.4) | 0.23 |
| BCG vaccination in children < 5 years (N = 1264) | 764 (60.4) | 381 (12.8) | 383 (11.6) | 0.15 |
| Are they ill now? (Yes) | 778 (12.4) | 318 () | 460 (14) | <0.01 |
| Questions | Number (%) (Total N = 1634) |
|---|---|
| How do you treat if someone at home suffers from diarrhoea? | |
| With oral rehydration salt | 736 (45) |
| With medicine | 247 (15.1) |
| Other | 54 (3.3) |
| No response provided | 597 (36.5) |
| Do you wash your hands with soap after the toilet? (Yes) | 1092 (66.8) |
| Where do you go first when a family member is ill? | |
| Unqualified village doctor | 882 (54) |
| Pharmacy/dispensary | 449 (27.5) |
| Government hospital | 274 (16.8) |
| Other | 29 (1.7) |
| Any babies born in the family in the last one year? (Yes) | 397 (24.3) |
| Did a pregnant woman in your family ever receive a vaccine? (Yes) | 1102 (67.4) |
| Did a pregnant woman in the family ever receive antenatal care? (Yes) | 562 (34.4) |
| Place of delivery of the last baby born to the family | |
| At home | 1464 (89.6) |
| In hospital | 63 (3.9) |
| Other places | 107 (6.5) |
| Who delivered (or helped deliver) the last baby born in the family? | |
| A traditional birth attendant | 1178 (72.1) |
| A relative | 291 (17.8) |
| A nurse/mid-wife or doctor | 71 (4.3) |
| Other | 94 (5.8) |
| Particulars | Number (%) |
|---|---|
| Any injury among family members in the last six months (N = 1634)? (Yes) | 547 (33.5) |
| Injury type (N = 547) | |
| Assault | 286 (52.3) |
| Accident | 128 (23.4) |
| Occupational | 51 (9.3) |
| Domestic task | 41 (7.5) |
| Other | 41 (7.5) |
| Assault caused by (N = 276) | |
| Stick | 128 (46.4) |
| Bullet | 65 (23.6) |
| Knife | 16 (5.8) |
| Burn | 4 (1.4) |
| Other | 63 (22.8) |
| Treatment received (N = 547) | |
| From pharmacy | 211 (38.6) |
| From hospital | 158 (28.9) |
| From primary care centre | 47 (8.6) |
| No treatment received | 108 (19.7) |
| Consequence of injuries (N = 547) | |
| Complete resolution | 195 (35.6) |
| Ongoing complaint or disability | 310 (56.7) |
| Death | 42 (7.6) |
| Any snake bitesamong family members in the last six months (N = 1634)? (Yes) | 48 (2.9) |
| Fatalities from snake bites (N = 48) | 0 (0) |
| Any dog bitesamong family members in the last six months (N = 1634)? (Yes) | 104 (6.3) |
| Fatalities from dog bites (N = 104) | 5 (5%) |
| At least one death among family members in the last one year (N = 1634) | 192 (11.8) |
| Two deaths in the family | 25 (1.5) |
| Three deaths in the family | 2 (0.1) |
| Gender of deceased (N = 192) | |
| Male | 134 (69.8) |
| Female | 54 (28.1) |
| Unspecified | 4 (2.1) |
| Age of deceased in years, range (median) | 0.1–113 (31) |
| Deceased aged≤50 years | 116 (60.4) |
| When did the individual die? (N = 192) | |
| Within the preceding 4 months | 114 (59.4) |
| 4–12 months prior | 78 (40.6) |
| Cause of death (N = 192) | |
| Homicide | 85 (44.2) |
| Sudden unexpected death | 34 (17.7) |
| Febrile illness | 19 (9.9) |
| Paralytic illness | 11 (5.7) |
| Accident | 9 (4.7) |
| Maternal death | 8 (4.2) |
| Coma | 4 (2.1) |
| Other | 18 (9.4) |
| Unknown | 4 (2.1) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rahman, M.R.; Faiz, M.A.; Nu, M.Y.; Hassan, M.R.; Chakrabarty, A.K.; Kabir, I.; Islam, K.; Jafarullah, A.K.M.; Alakabawy, M.; Khatami, A.; et al. A Rapid Assessment of Health Literacy and Health Status of Rohingya Refugees Living in Cox’s Bazar, Bangladesh Following the August 2017 Exodus from Myanmar: A Cross-Sectional Study. Trop. Med. Infect. Dis. 2020, 5, 110. https://doi.org/10.3390/tropicalmed5030110
Rahman MR, Faiz MA, Nu MY, Hassan MR, Chakrabarty AK, Kabir I, Islam K, Jafarullah AKM, Alakabawy M, Khatami A, et al. A Rapid Assessment of Health Literacy and Health Status of Rohingya Refugees Living in Cox’s Bazar, Bangladesh Following the August 2017 Exodus from Myanmar: A Cross-Sectional Study. Tropical Medicine and Infectious Disease. 2020; 5(3):110. https://doi.org/10.3390/tropicalmed5030110
Chicago/Turabian StyleRahman, Md Ridwanur, Mohammad Abul Faiz, Ma Yin Nu, Md Rafiqul Hassan, Ashish Kumar Chakrabarty, Iqbal Kabir, Khaleda Islam, Abul Kashem Mohammad Jafarullah, Mariam Alakabawy, Ameneh Khatami, and et al. 2020. "A Rapid Assessment of Health Literacy and Health Status of Rohingya Refugees Living in Cox’s Bazar, Bangladesh Following the August 2017 Exodus from Myanmar: A Cross-Sectional Study" Tropical Medicine and Infectious Disease 5, no. 3: 110. https://doi.org/10.3390/tropicalmed5030110
APA StyleRahman, M. R., Faiz, M. A., Nu, M. Y., Hassan, M. R., Chakrabarty, A. K., Kabir, I., Islam, K., Jafarullah, A. K. M., Alakabawy, M., Khatami, A., & Rashid, H. (2020). A Rapid Assessment of Health Literacy and Health Status of Rohingya Refugees Living in Cox’s Bazar, Bangladesh Following the August 2017 Exodus from Myanmar: A Cross-Sectional Study. Tropical Medicine and Infectious Disease, 5(3), 110. https://doi.org/10.3390/tropicalmed5030110






