1. Introduction
Urban tree canopy is endorsed as a key element of sustainable city planning due to its public health and environmental benefits [
1]. Urban trees improve air quality, alleviate urban heat, and promote psychological well-being [
2,
3]. These benefits support the hypothesis that improving tree canopy cover should reduce asthma morbidity overall by reducing exposure to air pollutants such as particulate matter and nitrogen dioxide [
4]. However, the association between tree canopy coverage and asthma prevalence remains inconclusive [
5]. Prior studies have reported both protective and adverse associations, suggesting that the relationship may be more complex than traditionally assumed [
6].
The relationship between tree canopy cover and asthma prevalence is complex: while some studies report that greater canopy reduces asthma risk [
7,
8], others suggest that allergenic pollen or pollutant trapping under dense canopies may increase prevalence [
9,
10]. Other confounding variables include the composition of tree species, seasonality, and local air quality. Urban trees can influence asthma through opposing mechanisms: canopy improves air quality and reduces heat-related pollutant formation, but certain species release allergenic pollen, and dense vegetation can trap pollutants at street level. These effects may differ by age because children are more geographically localized and have developing lungs, whereas adults may experience cumulative allergen exposure or greater exposure during commuting. Thus, tree canopy may not confer the same respiratory benefit across age groups.
Understanding whether the canopy–asthma association differs between children and adults is critical, as exposure patterns, and sensitivity may vary across the lifespan. Most prior research has focused on pediatric asthma, leaving the link with adult asthma less clear [
11]. Adults may have different exposure patterns, cumulative sensitivities, and unique risk profiles that could influence how urban greening affects respiratory health [
12].
This study examines whether the association between tree canopy cover and asthma prevalence differs between children and adults in Los Angeles County. We also assess whether neighborhood racial and ethnic composition modifies this relationship.
2. Materials and Methods
Study Design and Setting:
This study used a cross-sectional, geospatial design to examine the association between urban tree canopy cover and asthma prevalence by ZIP code in Los Angeles County, California. The county spans about 4753 square miles and has a population of nearly 10 million residents, the largest of any U.S. county. It includes more than 200 ZIP codes that range from densely urbanized areas to suburban neighborhoods and less developed peripheries. Longstanding problems with air pollution, urban heat, and asthma disparities make the county a relevant setting to study the impact of urban tree canopy on respiratory health in children and adults.
Data Sources:
We analyzed ZIP code-level data on both adult and pediatric asthma prevalence and tree canopy coverage across 210 municipalities in Los Angeles County [
13,
14]. Tree Canopy Coverage: ZIP code-level data on tree canopy coverage were obtained from the Los Angeles County Open Data Portal, which provides canopy estimates weighted by population size [
14]. Complete tree canopy and asthma prevalence data were available for 75 municipalities. The tree canopy coverage metric represents the percentage of land area covered by tree canopy relative to total ZIP code area, accounting for population density to better reflect canopy exposure relevant to residents. The data are derived from high-resolution aerial imagery analysis and remote sensing datasets collected by Los Angeles County’s Geographic Information Systems (GISs) division. Unlike NDVI or general greenness indices that capture any vegetation—including grass, shrubs, or undeveloped land—this dataset measures true tree canopy structure. Canopy coverage is a more targeted indicator of usable, shade-producing green infrastructure relevant to residents’ exposure.
Asthma Prevalence:
ZIP code-level asthma prevalence estimates for both adults and children were sourced from the Los Angeles GeoHub, updated in 2023 and 2024, respectively [
13,
15]. Adult asthma prevalence represents the proportion of adults diagnosed with asthma within each ZIP code, based on California Health Interview Survey (CHIS) self-reported responses and modeled using small area estimation techniques [
13]. Pediatric asthma prevalence was compiled from multiple CHIS-based regional datasets and consolidated into a single ZIP code-level estimate. The pediatric prevalence represents the proportion of children diagnosed with asthma within each ZIP code, based on self-reported or parent-reported survey responses and similarly modeled using small area estimation techniques to ensure data stability at the ZIP code level [
15]. Because ZIP codes in Los Angeles County differ widely in population size and density, we restricted the analytic sample to ZIP codes with complete small-area asthma estimates to avoid unstable rates from sparsely populated areas. These CHIS-derived ZIP code rates incorporate small-area smoothing, which improves statistical stability and reduces noise from low-population ZIP codes.
Population and Demographic Data: Population sizes and ZIP code-level demographic characteristics, including percentage of minority population, were obtained from the 2022 ACS 5-year estimates [
16]. For the purposes of this study, minority population was defined as all residents who identify with a racial or ethnic group other than non-Hispanic White. In Los Angeles, higher minority population percentages are strongly associated with socioeconomic disadvantage and historical underinvestment, so we treat minority composition as a proxy for structural inequities rather than an inherent risk factor.
Population by ZIP code was used for population weighting and population density as an adjusted model covariate.
Data Inclusion Criteria: All 210 ZIP codes within Los Angeles County were initially evaluated. ZIP codes were included in the final analytic dataset if they had complete data for tree canopy coverage and asthma prevalence for either adults or children. ZIP codes with missing or incomplete data for both adult and pediatric asthma prevalence were excluded. The final sample included 75 ZIP codes with complete case data for tree canopy coverage and asthma prevalence in at least one population group.
Variable Definitions:
Exposure: Tree canopy cover (%), as the proportion of tree canopy land cover area per ZIP code.
Outcomes: Adult prevalence of asthma (%), defined as the proportion of adults with a current asthma diagnosis per ZIP code.
Pediatric prevalence of asthma (%), defined as the proportion of children with a current asthma diagnosis per ZIP code.
Covariates: Population density (total population per area of ZIP code) was used as a covariate to control for possible confounding by urban intensity and socioeconomic stressors.
Statistical Analysis:
Descriptive Statistics: Means, standard deviations, and ranges were calculated for tree canopy cover, adult asthma incidence, children’s asthma incidence, and percentage of minority population by ZIP code. Tree canopy cover was also categorized into tertiles (low, medium, and high) for facilitating group comparisons.
Bivariate Analysis: Pearson correlation was employed to compare the linear association between asthma prevalence and tree canopy coverage for children and adults separately. Independent-samples t-tests were applied to check whether mean asthma prevalence varied among ZIP codes in the highest and lowest tree canopy tertiles for each group.
Multivariate Regression: We employed multivariate linear regression to model the relationship between tree canopy cover and the prevalence of asthma among adults and children, adjusting for population density as a proxy for urbanization and possible socioeconomic confounding. Regression coefficients (β) and p-values were reported to determine the magnitude and significance of associations.
Stratified and Interaction Analyses: ZIP codes were stratified into tertiles based on tree canopy coverage to explore potential differences in asthma prevalence across canopy density groups. Mean asthma prevalence was compared across tertiles using bar plots to visually illustrate group-level patterns.
We also conducted interaction analyses to assess whether the relationship between tree canopy coverage and pediatric asthma prevalence varied by community racial and ethnic composition, using an 80% minority population cutoff to evaluate differential effects.
Sensitivity Analyses: Although minority composition was considered as a potential effect modifier in the adult asthma analysis, the interaction findings were not significant and were excluded from final reporting to maintain focus on the primary research question.
Statistical Software:
All the data cleaning, the descriptive statistics, and regression tests were performed in Python (3.9), using the pandas, statsmodels, seaborn, and matplotlib libraries. Geospatial plotting was not included due to limitations in available ZIP code geolocation data.
Ethical Considerations:
De-identified, publicly available, aggregate data were utilized in this work. This analysis did not constitute human subjects research and did not require institutional review board (IRB) approval.
3. Results
Baseline Characteristics:
Seventy-five Los Angeles County ZIP codes were included in the final analysis following the elimination of missing tree canopy or asthma prevalence ZIP codes.
Table 1 provides thorough descriptive statistics for the key study variables, including tree canopy cover distributions, pediatric and adult asthma prevalence distributions, and minority mix.
Tree canopy cover was right-skewed, while both asthma prevalence measures were more approximately normally distributed [
Figure 1].
Bivariate Associations:
Pediatric Asthma:
Tree canopy cover was moderately to strongly inversely correlated with pediatric asthma prevalence (r = −0.56,
p < 0.001) [
Table 1]. ZIP code areas with higher tree canopy cover consistently reported lower rates of pediatric asthma [
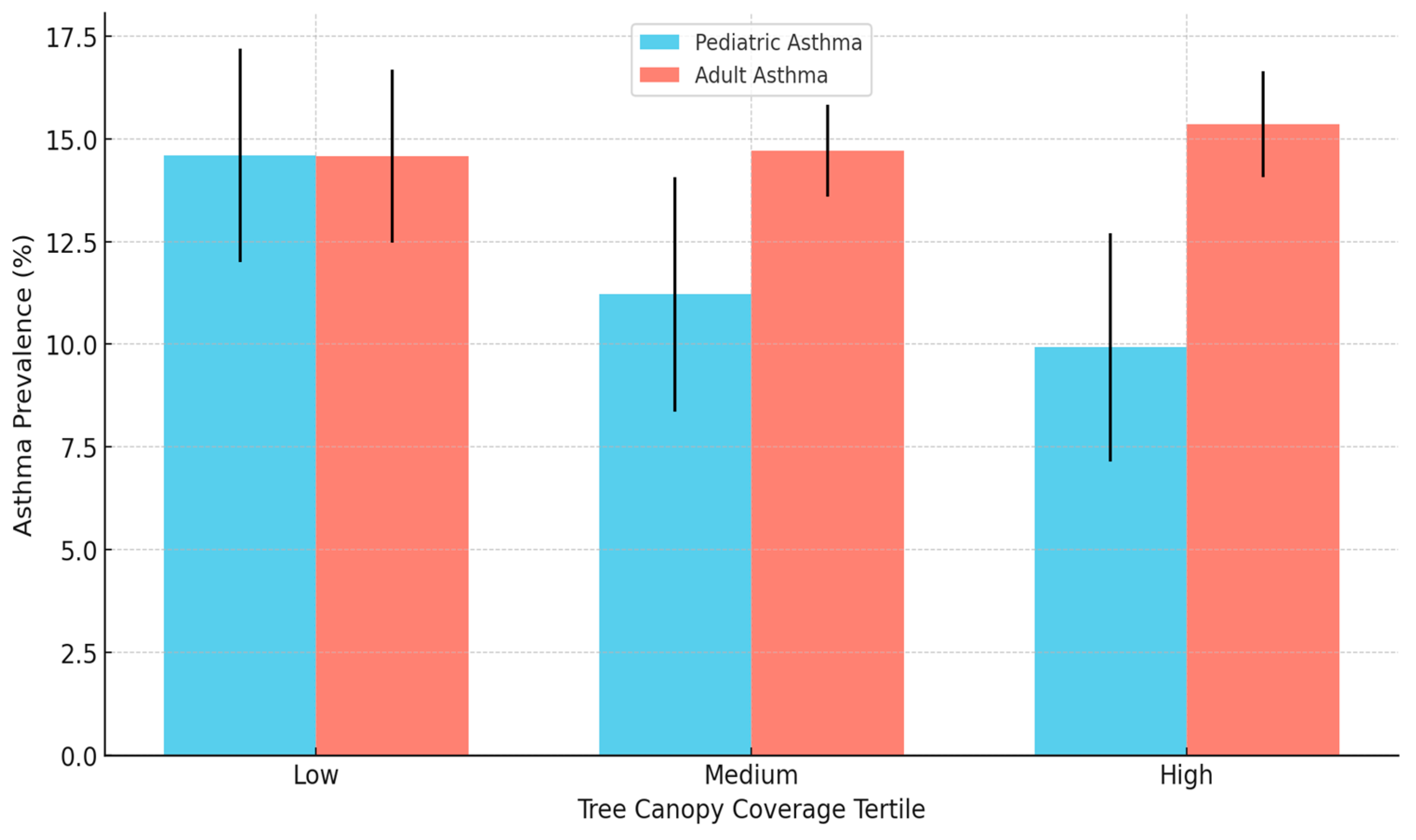
Figure 2]. When stratified by canopy cover tertile, pediatric asthma prevalence decreased significantly in all groups [
Figure 2]. ZIP codes in the lowest canopy tertile had an average pediatric asthma prevalence of 12.7% (SD: 0.7%), whereas the highest tertile had an average of 10.5% (SD: 0.9%) (t = 6.07,
p < 0.001).
Adult Asthma:
In contrast, tree canopy cover was weakly but significantly positively associated with adult asthma prevalence (r = 0.32, p = 0.005). ZIP codes in the lower canopy tertile (mean canopy: 2.4%) had a mean adult asthma prevalence of 14.7% (SD: 1.5%), and those in the upper tertile (mean canopy: 9.3%) averaged 15.2% (SD: 1.6%), though without statistical significance (p = 0.197).
Multivariate Regression Results:
Pediatric Asthma:
Multivariate regression confirmed that tree canopy cover remained strongly inversely associated with the prevalence of pediatric asthma when adjusted for minority composition (β = −0.625,
p < 0.001) (
Table 2). The model explained a substantial portion of the variance (adjusted R
2 = 0.32) and indicates a clinically significant protective effect of the urban canopy on children [
Figure 3].
Adult Asthma:
In adults, tree canopy cover was weakly positively correlated with asthma prevalence (β = 0.33,
p < 0.001), though the effect size was small and the model explained only a moderate percentage of the variance (adjusted R
2 = 0.10) [
Figure 3 and
Figure 4].
Stratified and Interaction Analyses:
Pediatric Asthma:
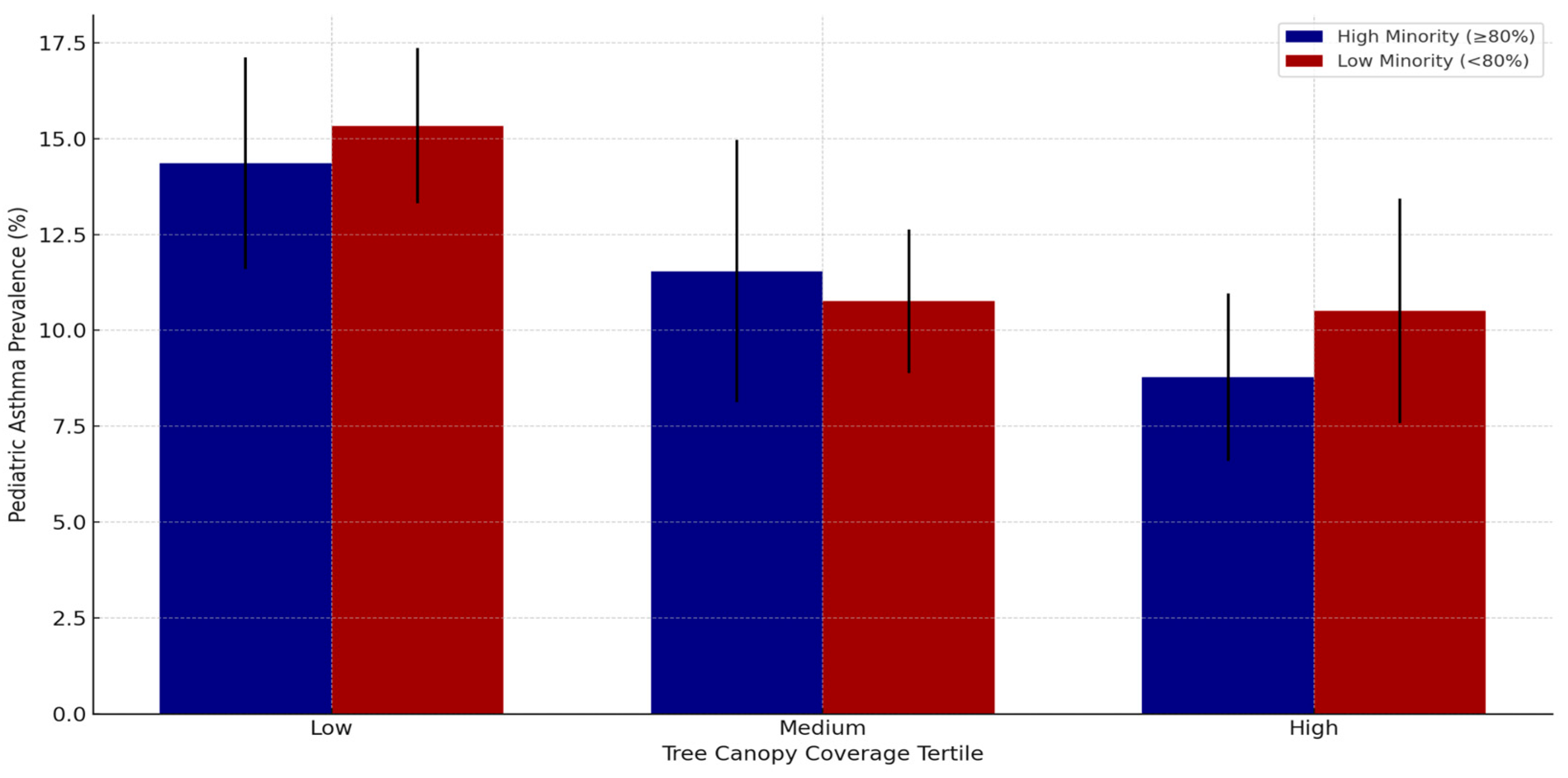
Stratified analysis revealed a clear, statistically significant decline in pediatric asthma incidence with increasing canopy tertiles [
Figure 2]. In addition, the interaction analysis revealed that the protective association was stronger for high-minority ZIP codes (interaction β = −0.0145,
p = 0.006), suggesting urban greening could yield increased respiratory health benefits in these populations [
Figure 5].
Adult Asthma:
Stratified analysis of adult asthma showed minor, non-significant differences across canopy tertiles, consistent with the weak positive association [
Figure 2 and
Figure 3]. No significant interaction with minority composition was observed for adult asthma. The distribution of ZIP Codes Across Tree Canopy Coverage Tertiles in Los Angeles County is shown in
Figure 6. Tertiles were defined as follows: Low: ≤3.5% canopy coverage; Medium: 3.6% to 5.9% canopy coverage; High: ≥6.0% canopy coverage.
Summary:
Tree canopy cover was strongly associated with lower pediatric asthma prevalence in Los Angeles County ZIP codes, and higher canopy coverage was associated with significantly lower prevalence of pediatric asthma. This protective relationship was more pronounced in high-minority ZIP codes. In contrast, higher tree canopy cover was weakly associated with higher adult asthma prevalence, and the strength of the effect was modest and likely of limited clinical relevance.
These age-specific convergent trends emphasize the need to consider population subgroups when evaluating the public health impacts of urban greenery initiatives.
4. Discussion
In this cross-sectional geospatial analysis of 75 Los Angeles County ZIP codes, we observed a strong, statistically significant inverse association between urban tree canopy cover and pediatric asthma prevalence. Those ZIP codes with greater tree canopy cover consistently had lower rates of pediatric asthma, with a moderate effect size that remained after adjustment for population density and minority composition. This finding contributes to a growing body of literature showing that green space exposure, particularly during early life, can have respiratory health protective effects [
17]. Unlike NDVI-based greenness measures, which capture all vegetated surfaces, our canopy metric reflects actual tree canopy structure, making it more relevant to shade, heat reduction, and usable green space.
Several pioneering studies revealed urban green space to have protective effects on pediatric respiratory health outcomes. In New York City, street tree density was inversely associated with asthma prevalence among preschool children [
7]. Similarly, increased exposure to green spaces in Shanghai was linked with reduced incidence of asthma and wheezing among children [
8]. Our findings align with this literature, providing further evidence of the public health value of urban greening for the protection of pediatric respiratory health in a vast, heterogeneous, and highly urbanized region like Los Angeles County.
Interestingly, we found that tree canopy’s protective impact on pediatric asthma was most robust in ZIP codes with higher minority populations, suggesting that urban greening can be an equity-enhancing strategy for respiratory health improvement. In this study, minority population composition served as a proxy for structural and historical inequities, including disproportionate exposure to environmental hazards and chronic underinvestment in green infrastructure. Thus, the interaction between canopy and minority composition reflects not only demographic variation, but embedded patterns of environmental injustice. This is a contribution to existing calls for greening initiatives to be targeted in historically marginalized communities where asthma burden and environmental exposures are often concentrated [
18].
In contrast, we observed a weak but statistically significant positive association between tree canopy coverage and adult asthma prevalence, echoing more recent studies that challenge the uniformly protective narrative surrounding urban greening [
19]. Notably, this positive association was not present in the unadjusted quartile comparison, suggesting that the relationship emerges only after accounting for population density and demographic composition, which may indicate that canopy coverage is spatially clustered in denser neighborhoods where other respiratory stressors are present. This pattern likely reflects methodological differences: treating canopy cover as a continuous variable in the regression preserves variability and statistical power, whereas categorizing it into quartiles reduces information and may obscure weak trends. A study in New York City demonstrated that greater tree cover was associated with greater numbers of asthma-related emergency department visits during high pollen seasons [
20]. An investigation of high-traffic areas raised additional concerns about the possibility of dense canopies trapping particulate matter and volatile organic compounds at street level [
21]. These mechanisms may disproportionately impact adults, whose cumulative exposures and long-term environmental sensitizations could render them more vulnerable to the complex interplay of pollen, pollution, and urban vegetation [
22].
The contrasting age-specific trends that we identified—protection in children but a weakly positive association in adults—highlight the importance of age-stratified analyses in urban health research. It is emerging that the respiratory impact of urban greening is not universally beneficial or harmful but instead is dependent on life stage, environmental context, and local urban design. Pediatric age groups are expected to benefit from reduced exposure to air pollutants and increased physical activity opportunity associated with green spaces, while adults, and particularly those with chronic allergic sensitizations, are more likely to be affected by allergenic pollen or pollutant entrapment under dense canopies.
Our findings are consistent with emerging research emphasizing the context-dependent, species-dependent, and seasonally dependent nature of green space impacts on respiratory health. A comprehensive review of different studies reported that green space may offer respiratory protection in some seasons but increase risk during periods of high allergenic pollen exposure [
23]. A study in Toronto found that tree species diversity, rather than canopy coverage alone, was more consistently associated with positive respiratory outcomes [
24]. Another study further emphasized this complexity, noting that adult airway obstruction decreased with greater residential greenness, while pediatric respiratory symptoms increased, underscoring the need for more nuanced, population-specific analyses [
25].
Additional pediatric-focused research reinforces this idea. A Connecticut ecological study found that higher tree canopy coverage was associated with fewer pediatric asthma emergency visits, particularly in socially vulnerable communities, suggesting that urban greening may offer the greatest respiratory protection where asthma burdens are highest [
6]. A large Montreal cohort study added seasonal nuance, reporting that deciduous tree canopy reduced asthma development during leaf-on seasons but that these benefits were diminished during peak pollen periods [
26]. A multi-neighborhood study in Shanghai similarly confirmed that increased residential greenspace was linked to lower pediatric asthma risk [
8]. However, recent work in Ontario demonstrated that pollen from both trees and weeds can attenuate respiratory benefits, emphasizing that protective effects may erode in areas with high allergenic pollen loads [
27]. A Philadelphia study also noted that tree canopy reduced children’s asthma-related emergency department visits on high pollution days, but not on low pollution days, suggesting that the respiratory benefits of urban greening may be most potent in environmentally disadvantaged communities [
28]. These studies are highly consistent with our results, particularly our finding that the children’s protective effect was strongest in high-minority, high-density ZIP codes where environmental stressors are more likely to cluster.
Collectively, these results uphold the conclusion that urban greening is not a one-size-fits-all intervention. Tree canopy’s respiratory health benefit is potentially enhanced in pediatric age groups and in environmentally disadvantaged groups, yet tree species choice, seasonal allergen load, and the urban microenvironment need to be carefully taken into account to avoid trade-offs, particularly for adults.
Limitations:
There are several limitations to our study. The cross-sectional design precludes causal inference, and ZIP code-level aggregation may mask significant within-area variability, a concern about ecological fallacy. Our analysis was limited to 75 of the county’s 210 ZIP codes because complete canopy and asthma prevalence data were only available for this subset. As a result, additional associations may have been missed if countywide data were available. ZIP codes with missing asthma estimates were typically those with small populations, where rates are statistically unstable; therefore, these ZIP codes are excluded from the CHIS-derived dataset. Because we did not have demographic or canopy data for the excluded ZIP codes, we were unable to compare included versus excluded areas, which introduces the possibility of selection bias. We did not have species-specific canopy data to differentiate between allergenic and non-allergenic trees or directly quantify pollen exposure. Although we adjusted for population density, residual confounding by neighborhood-level socioeconomic factors, access to health care, and local pollution sources remains possible. This includes traffic-related exposures, which are highly relevant in Los Angeles but were not directly captured in our dataset. Additionally, we were unable to include socioeconomic variables such as median household income or poverty rate (ACS), which limits our ability to fully account for socioeconomic confounding. Also, we were unable to include socioeconomic covariates (e.g., income, poverty rate) without further reducing the dataset, and residual socioeconomic confounding remains possible.
Implications and Future Directions:
Despite these restrictions, our study contributes nuance to the literature on urban greening. The shielding relationship between tree canopy cover and children’s asthma supports continued investment in context-sensitive urban forestry initiatives, particularly in high-minority and high-density communities. Our findings also complicate the assumption that increases in canopy cover will have an across-the-board respiratory health benefit for all populations.
Species selection, pollen management, and meticulous spatial design balancing ecological and public health objectives should be prioritized in upcoming urban greening endeavors. Future research including long-term investigations that track changes in respiratory outcomes following greening interventions will be needed to strengthen causal inference. Incorporation of species-level canopy mapping, dense pollen monitoring, and high-resolution air quality measurement will be essential in disentangling the competing respiratory effects of urban vegetation. Future studies should incorporate raw satellite NDVI data and geospatial methods such as Geographically Weighted Regression (GWR) to assess spatial heterogeneity and vegetation structure beyond canopy percentage. Studies integrating individual-level exposure assessment with socio-demographic and built environment studies will lead the field forward and facilitate the development of equitable, evidence-driven urban health policy.
5. Conclusions
In conclusion, our results show that greater tree canopy cover in Los Angeles County is strongly associated with lower prevalence of pediatric asthma but is weakly associated with a higher prevalence of adult asthma. These findings emphasize the importance of going beyond simplistic metrics of canopy cover and pursuing a more focused, age-specific, and community-sensitive approach of urban greening. Thoughtfully designed, species-rich, and strategically placed urban forestry remains essential for building healthier, more equitable, and more livable cities. In practice, this means prioritizing canopy expansion in low-canopy, high-asthma-burden neighborhoods and selecting low-allergenic, pollution-tolerant species to avoid introducing new respiratory risks. Designing greening projects with explicit public health criteria—rather than simply increasing tree counts—allows urban forestry to function as a targeted health equity strategy, not just an environmental intervention.