Multifaceted Exercise Prescription in the Management of an Overhead Athlete with Suspected Distal Biceps Tendinopathy: A Case Report
Abstract
1. Introduction
2. Case Presentation
2.1. Case Description
2.2. Clinical Impression #1
2.3. Examination
2.4. Outcome Measures Used
2.5. Clinical Impression #2
2.6. Biceps Brachii Biomechanical Considerations for Baseball Pitching
2.7. Intervention
2.8. Outcomes
3. Discussion
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Kelly, M.P.; Perkinson, S.G.; Ablove, R.H.; Tueting, J.L. Distal Biceps Tendon Ruptures. Am. J. Sports Med. 2015, 43, 2012–2017. [Google Scholar] [CrossRef]
- Festa, A.; Mulieri, P.J.; Newman, J.S.; Spitz, D.J.; Leslie, B.M. Effectiveness of Magnetic Resonance Imaging in Detecting Partial and Complete Distal Biceps Tendon Rupture. J. Hand Surg. 2010, 35, 77–83. [Google Scholar] [CrossRef]
- Friedmann, E. Rupture of the Distal Biceps Brachii Tendon. JAMA 1963, 184, 60–63. [Google Scholar] [CrossRef] [PubMed]
- Ramsey, M.L. Distal Biceps Tendon Injuries: Diagnosis and Management. J. Am. Acad. Orthop. Surg. 1999, 7, 199–207. [Google Scholar] [CrossRef] [PubMed]
- Le Huec, J.C.; Moinard, M.; Liquois, F.; Zipoli, B.; Chauveaux, D.; Le Rebeller, A. Distal rupture of the tendon of biceps brachii. J. Bone Jt. Surgery. Br. Vol. 1996, 78, 767–770. [Google Scholar] [CrossRef]
- Safran, M.R.; Graham, S.M. Distal Biceps Tendon Ruptures. Clin. Orthop. Relat. Res. 2002, 404, 275–283. [Google Scholar] [CrossRef]
- Mazzocca, A.D.; Cohen, M.; Berkson, E.; Nicholson, G.; Carofino, B.C.; Arciero, R.; Romeo, A.A. The anatomy of the bicipital tuberosity and distal biceps tendon. J. Shoulder Elb. Surg. 2007, 16, 122–127. [Google Scholar] [CrossRef]
- Idler, C.S.; Montgomery, W.H.; Lindsey, D.P.; Badua, P.A.; Wynne, G.F.; Yerby, S.A. Distal Biceps Tendon Repair. Am. J. Sports Med. 2006, 34, 968–974. [Google Scholar] [CrossRef]
- Bekerom, M.P.J.V.D.; Kodde, I.F.; Aster, A.; Bleys, R.L.A.W.; Eygendaal, D. Clinical relevance of distal biceps insertional and footprint anatomy. Knee Surgery Sports Traumatol. Arthrosc. 2014, 24, 2300–2307. [Google Scholar] [CrossRef]
- Scott, A.; Docking, S.I.; Vicenzino, B.; Alfredson, H.; Zwerver, J.; Lundgreen, K.; Finlay, O.; Pollock, N.; Cook, J.L.; Fearon, A.; et al. Sports and exercise-related tendinopathies: A review of selected topical issues by participants of the second International Scientific Tendinopathy Symposium (ISTS) Vancouver 2012. Br. J. Sports Med. 2013, 47, 536–544. [Google Scholar] [CrossRef]
- Irby, A.; Gutierrez, J.; Chamberlin, C.; Thomas, S.J.; Rosen, A.B. Clinical management of tendinopathy: A systematic review of systematic reviews evaluating the effectiveness of tendinopathy treatments. Scand. J. Med. Sci. Sports 2020. [Google Scholar] [CrossRef] [PubMed]
- Cook, J.L.; Khan, K.M.; Harcourt, P.R.; Grant, M.; A Young, D.; Bonar, S.F. A cross sectional study of 100 athletes with jumper’s knee managed conservatively and surgically. The Victorian Institute of Sport Tendon Study Group. Br. J. Sports Med. 1997, 31, 332–336. [Google Scholar] [CrossRef]
- Kettunen, J.A.; Kvist, M.; Alanen, E.; Kujala, U. Long-Term Prognosis for Jumper’s Knee in Male Athletes: Prospective Follow-up Study. Am. J. Sports Med. 2002, 30, 689–692. [Google Scholar] [CrossRef] [PubMed]
- Beyer, R.; Kongsgaard, M.; Kjær, B.H.; Øhlenschlæger, T.; Kjaer, M.; Magnusson, S.P. Heavy Slow Resistance Versus Eccentric Training as Treatment for Achilles Tendinopathy. Am. J. Sports Med. 2015, 43, 1704–1711. [Google Scholar] [CrossRef]
- Couppe, C.; Svensson, R.B.; Silbernagel, K.G.; Langberg, H.; Magnusson, S.P. Eccentric or Concentric Exercises for the Treatment of Tendinopathies? J. Orthop. Sports Phys. Ther. 2015, 45, 853–863. [Google Scholar] [CrossRef]
- Jayaseelan, D.J.; Mischke, J.J.; Strazzulla, R.L. Eccentric Exercise for Achilles Tendinopathy: A Narrative Review and Clinical Decision-Making Considerations. J. Funct. Morphol. Kinesiol. 2019, 4, 34. [Google Scholar] [CrossRef]
- Rio, E.; Van Ark, M.; Docking, S.I.; Moseley, G.L.; Kidgell, D.J.; Gaida, J.E.; Akker-Scheek, I.V.D.; Zwerver, J.; Cook, J. Isometric Contractions Are More Analgesic Than Isotonic Contractions for Patellar Tendon Pain. Clin. J. Sport Med. 2017, 27, 253–259. [Google Scholar] [CrossRef] [PubMed]
- Van Ark, M.; Cook, J.L.; Docking, S.I.; Zwerver, J.; Gaida, J.E.; Akker-Scheek, I.V.D.; Rio, E.; Information, P.E.K.F.C. Do isometric and isotonic exercise programs reduce pain in athletes with patellar tendinopathy in-season? A randomised clinical trial. J. Sci. Med. Sport 2016, 19, 702–706. [Google Scholar] [CrossRef]
- Silbernagel, K.G.; Vicenzino, B.T.; Rathleff, M.S.; Thorborg, K. Isometric exercise for acute pain relief: Is it relevant in tendinopathy management? Br. J. Sports Med. 2019, 53, 1330–1331. [Google Scholar] [CrossRef]
- Hart, D.L.; Wang, Y.-C.; Cook, K.F.; Mioduski, J.E. A Computerized Adaptive Test for Patients with Shoulder Impairments Produced Responsive Measures of Function. Phys. Ther. 2010, 90, 928–938. [Google Scholar] [CrossRef] [PubMed]
- Hart, D.L.; Tepper, S.; Lieberman, D. Changes in health status for persons with wrist or hand impairments receiving occupational therapy or physical therapy. Am. J. Occup. Ther. 2001, 55, 68–74. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Resnik, L.; Liu, D.; Mor, V.; Hart, D.L. Predictors of Physical Therapy Clinic Performance in the Treatment of Patients with Low Back Pain Syndromes. Phys. Ther. 2008, 88, 989–1004. [Google Scholar] [CrossRef]
- Wang, Y.-C.; Hart, D.L.; Stratford, P.W.; Mioduski, J.E. Baseline Dependency of Minimal Clinically Important Improvement. Phys. Ther. 2011, 91, 675–688. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.-C.; Hart, D.L.; Cook, K.F.; Mioduski, J.E. Translating Shoulder Computerized Adaptive Testing Generated Outcome Measures into Clinical Practice. J. Hand Ther. 2010, 23, 372–383. [Google Scholar] [CrossRef] [PubMed]
- Kamper, S.J.; Maher, C.G.; Mackay, G. Global Rating of Change Scales: A Review of Strengths and Weaknesses and Considerations for Design. J. Man. Manip. Ther. 2009, 17, 163–170. [Google Scholar] [CrossRef] [PubMed]
- Cook, J.L.; Purdam, C.R. Is tendon pathology a continuum? A pathology model to explain the clinical presentation of load-induced tendinopathy. Br. J. Sports Med. 2008, 43, 409–416. [Google Scholar] [CrossRef]
- Cook, J.L.; Rio, E.; Purdam, C.R.; Docking, S.I. Revisiting the continuum model of tendon pathology: What is its merit in clinical practice and research? Br. J. Sports Med. 2016, 50, 1187–1191. [Google Scholar] [CrossRef]
- Seroyer, S.T.; Nho, S.J.; Bach, B.R.; Bush-Joseph, C.A.; Nicholson, G.P.; Romeo, A.A. The Kinetic Chain in Overhand Pitching. Sports Health A Multidiscip. Approach 2010, 2, 135–146. [Google Scholar] [CrossRef]
- Itoi, E.; Kuechle, D.; Newman, S.R.; Morrey, B.; An, K. Stabilising function of the biceps in stable and unstable shoulders. J. Bone Jt. Surgery. Br. Vol. 1993, 75, 546–550. [Google Scholar] [CrossRef]
- Dillman, C.J.; Fleisig, G.S.; Andrews, J.R. Biomechanics of Pitching With Emphasis Upon Shoulder Kinematics. J. Orthop. Sports Phys. Ther. 1993, 18, 402–408. [Google Scholar] [CrossRef]
- Pappas, A.M.; Zawacki, R.M.; Sullivan, T.J. Biomechanics of baseball pitching. Am. J. Sports Med. 1985, 13, 216–222. [Google Scholar] [CrossRef] [PubMed]
- Stodden, D.F.; Fleisig, G.S.; McLean, S.P.; Andrews, J.R. Relationship of Biomechanical Factors to Baseball Pitching Velocity: Within Pitcher Variation. J. Appl. Biomech. 2005, 21, 44–56. [Google Scholar] [CrossRef] [PubMed]
- Fleisig, G.S.; Andrews, J.R.; Dillman, C.J.; Escamilla, R.F. Kinetics of Baseball Pitching with Implications About Injury Mechanisms. Am. J. Sports Med. 1995, 23, 233–239. [Google Scholar] [CrossRef]
- Matsuo, T.; Escamilla, R.F.; Fleisig, G.S.; Barrentine, S.W.; Andrews, J.R. Comparison of Kinematic and Temporal Parameters between Different Pitch Velocity Groups. J. Appl. Biomech. 2001, 17, 1–13. [Google Scholar] [CrossRef]
- Werner, S.L.; Suri, M.; Guido, J.A.; Meister, K.; Jones, D.G. Relationships between ball velocity and throwing mechanics in collegiate baseball pitchers. J. Shoulder Elb. Surg. 2008, 17, 905–908. [Google Scholar] [CrossRef] [PubMed]
- Gowan, I.D.; Jobe, F.W.; Tibone, J.E.; Perry, J.; Moynes, D.R. A comparative electromyographic analysis of the shoulder during pitching. Am. J. Sports Med. 1987, 15, 586–590. [Google Scholar] [CrossRef]
- Escamilla, R.F.; Fleisig, G.S.; Barrentine, S.W.; Zheng, N.; Andrews, J.R. Kinematic Comparisons of Throwing Different Types of Baseball Pitches. J. Appl. Biomech. 1998, 14, 1–23. [Google Scholar] [CrossRef]
- Special Interest Report Abstracts. Physiotherapy 2011, 97, eS1416–eS1638. [CrossRef]
- Torstensen, T.A.; Meen, H.D.; Stiris, M. The Effect of Medical Exercise Therapy on a Patient With Chronic Supraspinatus Tendinitis. Diagnostic Ultrasound—Tissue Regeneration: A Case Study. J. Orthop. Sports Phys. Ther. 1994, 20, 319–327. [Google Scholar] [CrossRef]
- Østerås, H.; Torstensen, T.A.; Østerås, B. High-dosage medical exercise therapy in patients with long-term subacromial shoulder pain: A randomized controlled trial. Physiother. Res. Int. 2010, 15, 232–242. [Google Scholar] [CrossRef]
- Østerås, B.; Østerås, H.; Torstensen, T.A.; Vasseljen, O. Dose–response effects of medical exercise therapy in patients with patellofemoral pain syndrome: A randomised controlled clinical trial. Physiotherapy 2013, 99, 126–131. [Google Scholar] [CrossRef] [PubMed]
- Coviello, J.P.; Kakar, R.S.; Reynolds, T.J. Short-term effects of instrument-assisted soft tissue mobilization on pain free range of motion in a weightlifter with subacromial pain syndrome. Int. J. Sports Phys. Ther. 2017, 12, 144–154. [Google Scholar] [PubMed]
- Kim, J.; Sung, N.J.; Lee, J. Therapeutic effectiveness of instrument-assisted soft tissue mobilization for soft tissue injury: Mechanisms and practical application. J. Exerc. Rehabilitation 2017, 13, 12–22. [Google Scholar] [CrossRef] [PubMed]
- Cheatham, S.W.; Baker, R.; Kreiswirth, E. Instrument assisted soft-tissue mobilization: A commentary on clinical practice guidelines for rehabilitation professionals. Int. J. Sports Phys. Ther. 2019, 14, 670–682. [Google Scholar] [CrossRef] [PubMed]
- Jayaseelan, D.J.; Magrum, E.M. Eccentric training for the rehabilitation of a high level wrestler with distal biceps tendinosis: A case report. Int. J. Sports Phys. Ther. 2012, 7, 413–424. [Google Scholar]
- Chalmers, P.N.; Wimmer, M.A.; Verma, N.N.; Cole, B.J.; Romeo, A.A.; Cvetanovich, G.L.; Pearl, M.L. The Relationship Between Pitching Mechanics and Injury: A Review of Current Concepts. Sports Health A Multidiscip. Approach 2017, 9, 216–221. [Google Scholar] [CrossRef]
- Norton, R.; Honstad, C.; Joshi, R.; Silvis, M.; Chinchilli, V.; Dhawan, A. Risk Factors for Elbow and Shoulder Injuries in Adolescent Baseball Players: A Systematic Review. Am. J. Sports Med. 2018, 47, 982–990. [Google Scholar] [CrossRef]
- Noreski, M.A.; Cohen, S.B. Epidemiology of Shoulder Injuries in Overhead Athletes. Sports Injuries to the Shoulder and Elbow; Park, J., Ed.; Springer: Berlin, Germany, 2015; pp. 23–34. [Google Scholar]
- Gandhi, J.; ElAttrache, N.S.; Kaufman, K.R.; Hurd, W.J. Voluntary activation deficits of the infraspinatus present as a consequence of pitching-induced fatigue. J. Shoulder Elb. Surg. 2012, 21, 625–630. [Google Scholar] [CrossRef]
- Kelly, J.D., IV. Identifying and managing scapular problems in overhead athletes. J Musculoskelet Med. 2007, 24, 228. [Google Scholar]
- Kisner, C.; Colby, L.A. Therapeutic Exercise Foundations and Techniques, 6th ed.; F.A. Davis: Philadelphia, PA, USA, 2012; pp. 157–240. [Google Scholar]
- Silbernagel, K.G.; Brorsson, A.; Lundberg, M. The Majority of Patients with Achilles Tendinopathy Recover Fully When Treated With Exercise Alone. Am. J. Sports Med. 2010, 39, 607–613. [Google Scholar] [CrossRef]

| Type of Assessment | Test(s) Performed | Result | |
|---|---|---|---|
| Observation | Postural assessment | Rounded shoulders, increased thoracic kyphosis | |
| Visual inspection | No local ecchymosis, edema, atrophy, or deformity | ||
| Neurological examination | Deep tendon reflexes, dermatome, and myotomes of UE | Normal, symmetrical | |
| Proximal joint screening | Cervical, shoulder, scapulothoracic A/PROM | Normal, pain free | |
| Range of motion | Elbow A/PROM: Flexion Extension | WNL, biceps stretch * WNL | |
| Wrist/Hand A/PROM: Supination Pronation Flexion Extension | WNL | ||
| Manual muscle testing | Shoulder: | L | R |
| External rotation | 4/5 | 5/5 | |
| Internal rotation | 5/5 | 5/5 | |
| Flexion | 4/5 | 5/5 | |
| Elbow: | L | R | |
| Flexion: 90° at side | 4/5 * | 5/5 | |
| 0°, shoulder flexion to 90° | 3/5 * | 5/5 | |
| Extension | 5/5 | 5/5 | |
| Wrist/Hand: | L | R | |
| Grip strength | WNL | WNL | |
| Supination: at side | 4/5 * | 5/5 | |
| 0°, shoulder flexion to 90° | 3/5 * | 5/5 | |
| Pronation | WNL | WNL | |
| Flexion | WNL | WNL | |
| Extension | WNL | WNL | |
| Tissue differentiation | Palpation | (+) pain at DBBT (−) defect/discontinuity | |
| Speed’s and Yergason’s tests | (+) | ||
| Hook and biceps squeeze | (−) | ||
| Elbow valgus stress | (−) | ||
| Biceps load II | (−) | ||
| Intervention | Visit 1 (Evaluation) | Visit 2 | Visit 3 | Visit 4 | Visit 5 (Discharge) |
|---|---|---|---|---|---|
| Manual therapy | Pronator/flexor soft tissue restriction - Manual and IASTM anterior/medial forearm - Wrist/pronator stretch 3 × 30” | Pronator/flexor soft tissue restriction - Manual and IASTM anterior/medial forearm - Wrist/pronator stretch 3 × 30” | Pronator/flexor soft tissue restriction - Manual and IASTM anterior/medial forearm - Wrist/pronator stretch 3 × 30” | Pronator/flexor soft tissue restriction - Manual and IASTM anterior/medial forearm - Wrist/pronator stretch 1′ | Not performed, no mobility restrictions noted |
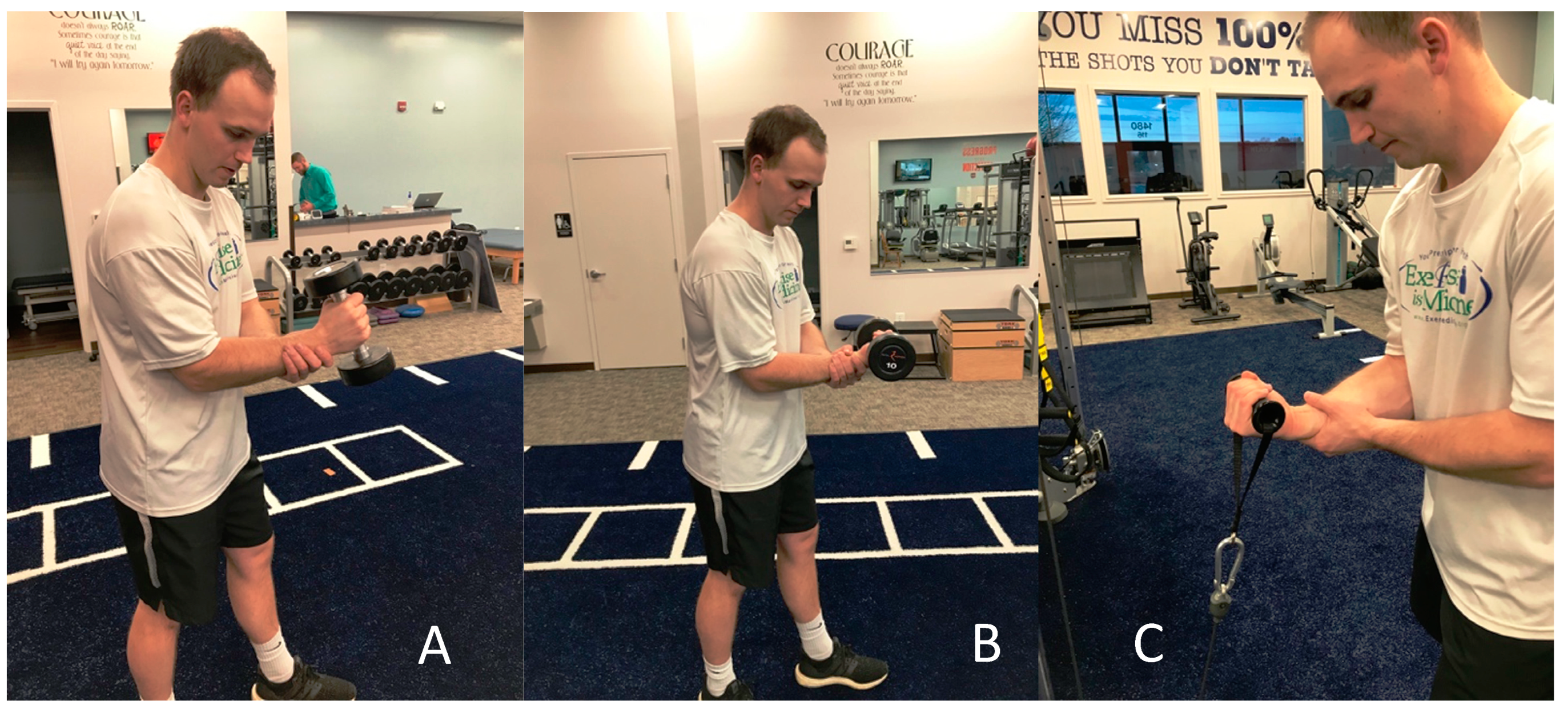
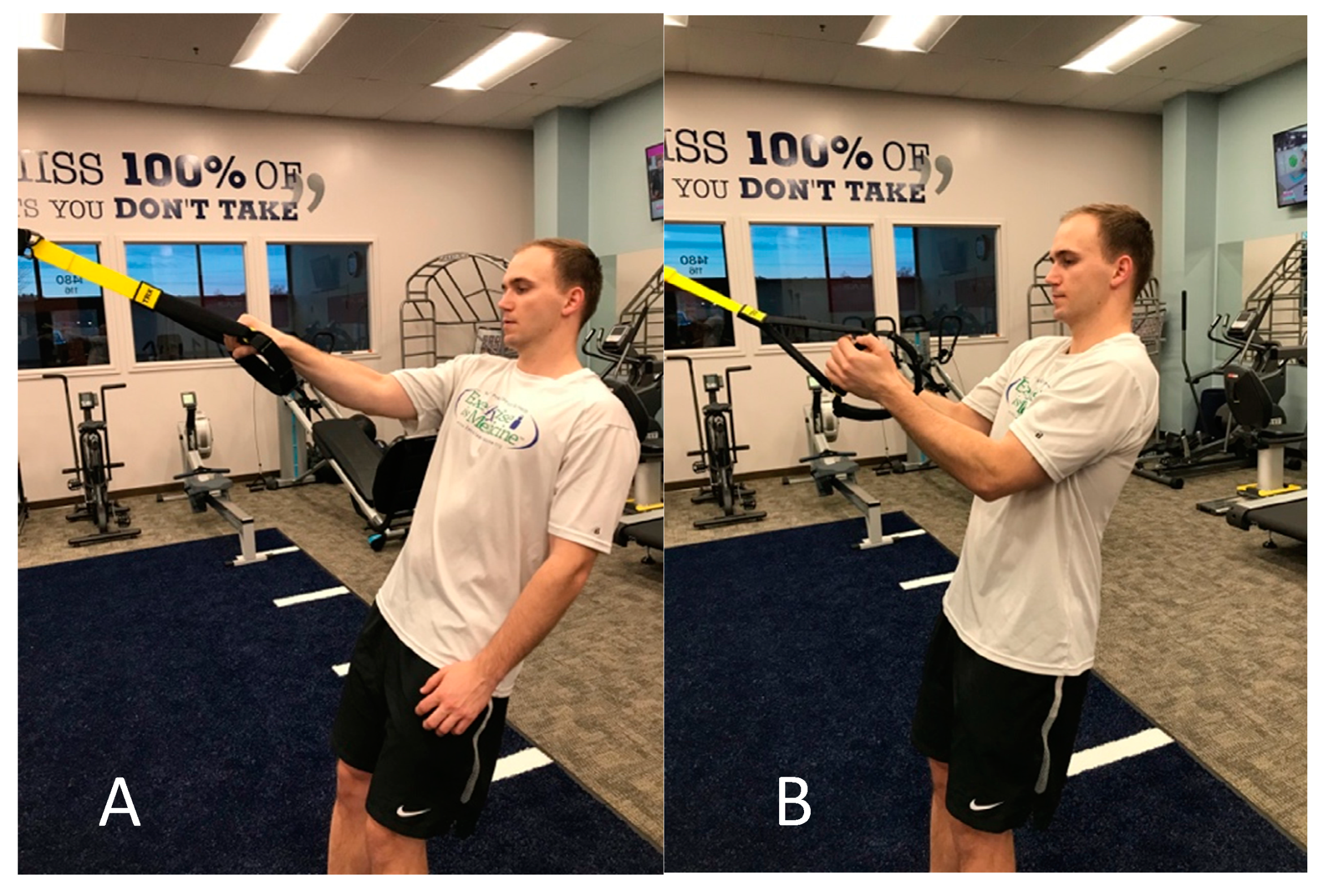
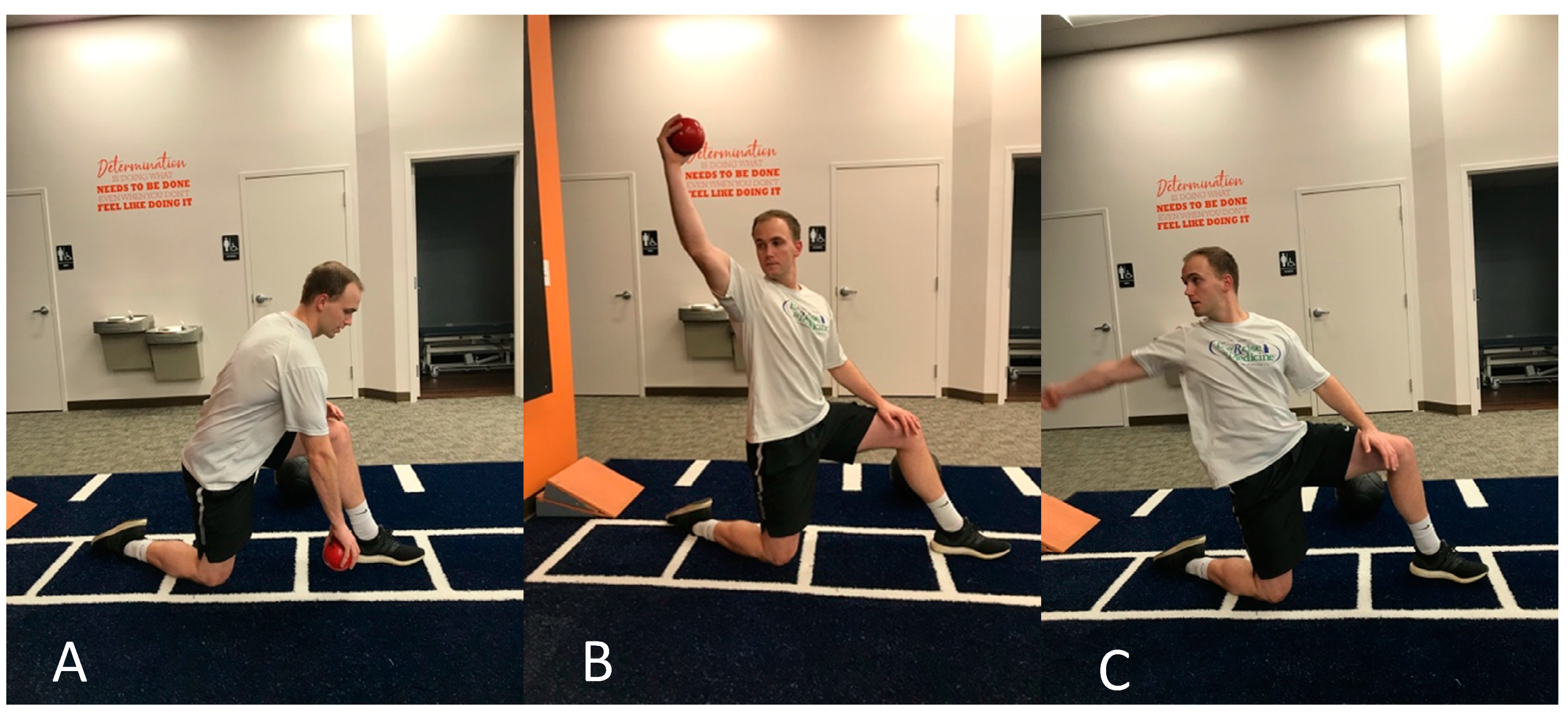
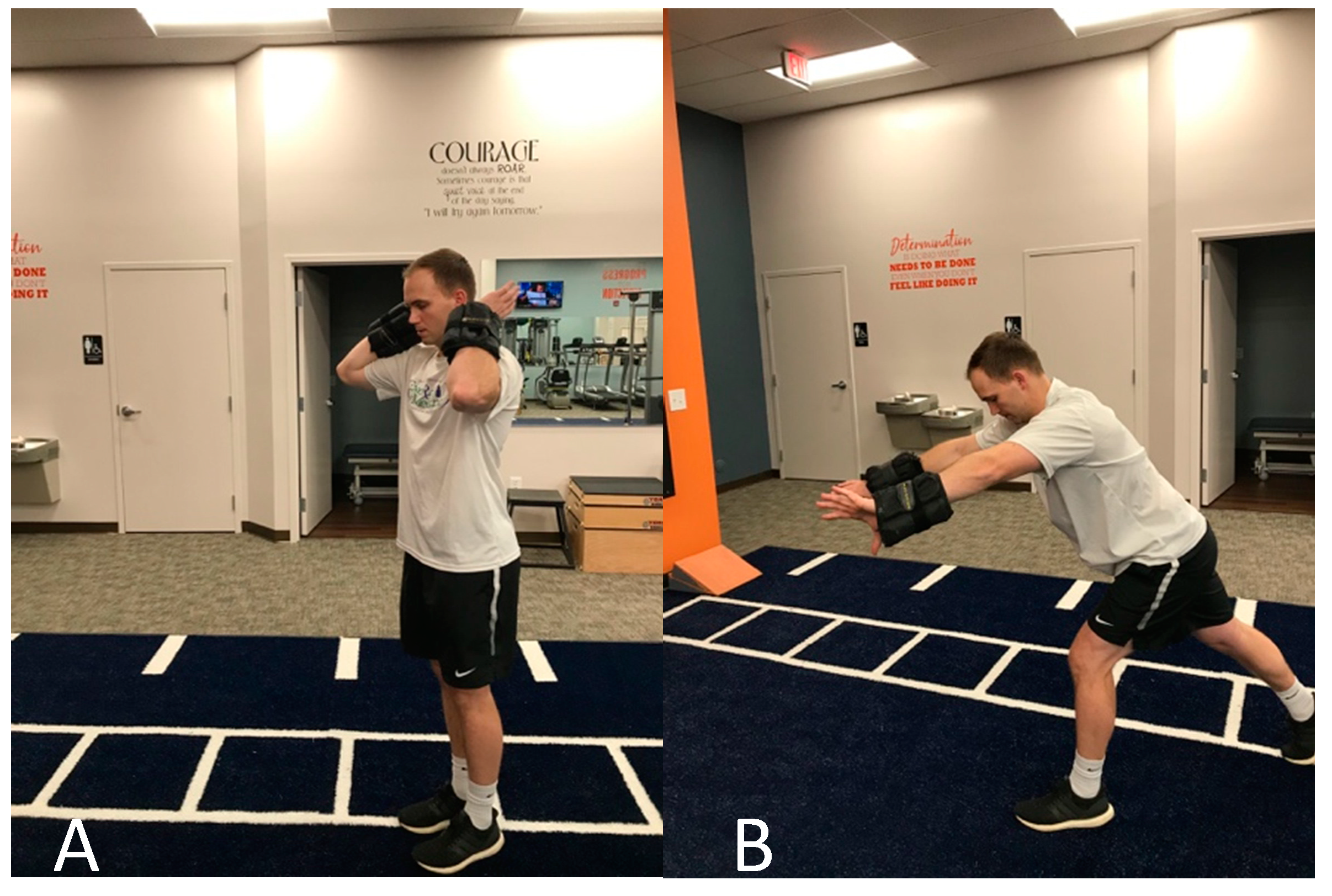
| Exercise | Pain-Free AROM - Dowel elbow flexion/extension 60× - Supination pronation 60× @ 90 deg. elbow flexion Eccentric training - Eccentric biceps curl 3 × 10, 3# DB - TRX eccentric elbow biceps with neutral grip 2 × 10 Baseball specific - Standing ER @ 0 abduction, 3 × 20, red band | Pain-Free AROM - Rows with shoulder pulleys 2′ - Dowel elbow flexion/extension 60× - Supination pronation 60× @ 90 deg. elbow flexion - Assault bike UE and LE, light 5′ Eccentric training - 3 × 7 cable pulley eccentric on painful side 12.5#, supinated grip - 3 × 7 neutral grip curl, 10# DB - 3 × 7 TRX Eccentric biceps on left, pronated grip Baseball specific - ER/IR @ 0 Abduction 30× ea. red band - ER/IR @ 45 deg. in stride position, 30× ea. red band - ER/IR @ 90/90 in stride position, 30× ea. red band - Plank shoulder taps 3 × 10 - Prone I, W, T, I 20× ea. | Pain-Free AROM - Assault bike UE and LE, light 8′ - Dowel elbow flexion/extension 60× Eccentric training - 3 × 7 cable pulley eccentric on painful side 17.5#, supinated grip - 3 × 7 neutral grip curl, 15# DB - 3 × 7 TRX Eccentric biceps on left, pronated grip - Bent over eccentric row 20# KB Baseball specific - ER/IR @ 0 Abduction 2 × 30 ea. red band - ER/IR @ 45 deg. in stride position, 2 × 30 ea. red band - ER/IR @ 90/90 in stride position, 2 × 30 ea. red band - Plank shoulder taps 3 × 10 - Prone I, W, T, I 2 × 20 ea. | Pain-Free AROM - Assault bike UE and LE, 8′ Eccentric training - 3 × 7 cable pulley eccentric on painful side 17.5#, supinated grip - 3 × 7 neutral grip curl, 20# DB - 3 × 7 TRX Eccentric biceps on left, pronated grip Concentric training - Neutral grip DB: 3 × 10, 5# - Supinated grip cable, 3 × 10, 2.5# - Pronated grip, 3# DB 3 × 10 - Lunge follow-through position concentric cable rows 2 × 10 each leg, 7.5# Baseball specific - ER/IR @ 0 Abduction 60× ea., red, quick - ER/IR @ 90/90 2 × 20 red, quick - Push-ups 20× | Pain-Free AROM - Assault bike UE and LE, 8′ Concentric Training - Neutral grip DB: 3 × 10, 10# - Supinated grip cable, 2 × 20, 5# Baseball specific - Elbow flexion/supination to elbow extension/pronation –quick 5# wrist weight 3 × 7 - Overhead biceps flexion to elbow extension/pronation- quick 5# weights weight 3 × 7 - Reverse throw with red ball against wall (faster eccentric) 2 × 7 - Single leg kettlebell shot put throw 4# med ball 2 × 7 - Overhead med ball throw 2 × 7 - Elbow extended ball flips 2 × 15, red ball - Tennis ball throwing 2 × 20 - Pronated ball catches in flexion - Single-arm underhand toss 2 × 7 |
| Education | - Limiting amount of heavy lifting with elbow flexion - Limiting end-range shoulder or elbow motions with quick and forceful stress on biceps tendon especially when combined with supination - No throwing | - AROM elbow flex/ext., wrist sup/pro – active pain free 2×/day 60 reps ea. - Forearm and distal biceps self-massage with hand - Wrist flexor stretch 3×/day, 2 × 30” | - AROM elbow flex/ext., wrist sup/pro – active pain free 2×/day 60 reps ea. - Forearm and distal biceps self-massage with hand - Wrist flexor stretch 3×/day, 2 × 30” - Eccentric training every day at gym with supinated, neutral, pronated grip 3 × 7 each, “heavy as tolerated, uncomfortable but not disabling, good form; pulley supinated, DB neutral, kettlebell pronated” | HEP: Eccentric training - 3×/week - Same intensity, progressing if easy add light concentric training | Return to throwing program, no curveballs for 2 weeks, should be able to perform flat ground prior to mound throwing, continue HEP, stretch and self-soft tissue massage between innings or sessions |
| Outcome Measure | Initial Evaluation | Discharge (4 weeks) |
|---|---|---|
| NPRS (average over past 24 h) | 4/10 | 0/10 |
| Patient Physical Functional Status (FOTO) | 83/100 | 98/100 |
| Participating in recreational activities in which you take some force or impact through your elbow, wrist, or hand (FOTO) | With Mild Difficulty | With No Difficulty |
| Severity of any weakness (FOTO) | Mild | None |
| Global Rating of Change (FOTO) | N/A | +5 |
| Resisted biceps brachii testing | Elbow flexed: 4/5 * Elbow extended: 3/5 with pain | Elbow flexed: 5/5 Elbow extended: 5/5 |
| Tenderness to palpation | (+) distal biceps tendon | (−) |
| Tissue differentiation tests | Speed’s: (+) Yergason’s (+) | Speed’s: (−) Yergason’s: (−) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Holshouser, C.; Jayaseelan, D.J. Multifaceted Exercise Prescription in the Management of an Overhead Athlete with Suspected Distal Biceps Tendinopathy: A Case Report. J. Funct. Morphol. Kinesiol. 2020, 5, 56. https://doi.org/10.3390/jfmk5030056
Holshouser C, Jayaseelan DJ. Multifaceted Exercise Prescription in the Management of an Overhead Athlete with Suspected Distal Biceps Tendinopathy: A Case Report. Journal of Functional Morphology and Kinesiology. 2020; 5(3):56. https://doi.org/10.3390/jfmk5030056
Chicago/Turabian StyleHolshouser, Cameron, and Dhinu J. Jayaseelan. 2020. "Multifaceted Exercise Prescription in the Management of an Overhead Athlete with Suspected Distal Biceps Tendinopathy: A Case Report" Journal of Functional Morphology and Kinesiology 5, no. 3: 56. https://doi.org/10.3390/jfmk5030056
APA StyleHolshouser, C., & Jayaseelan, D. J. (2020). Multifaceted Exercise Prescription in the Management of an Overhead Athlete with Suspected Distal Biceps Tendinopathy: A Case Report. Journal of Functional Morphology and Kinesiology, 5(3), 56. https://doi.org/10.3390/jfmk5030056





