Is Supine Position Superior to Prone Position in the Surgical Pinning of Supracondylar Humerus Fracture in Children?
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample
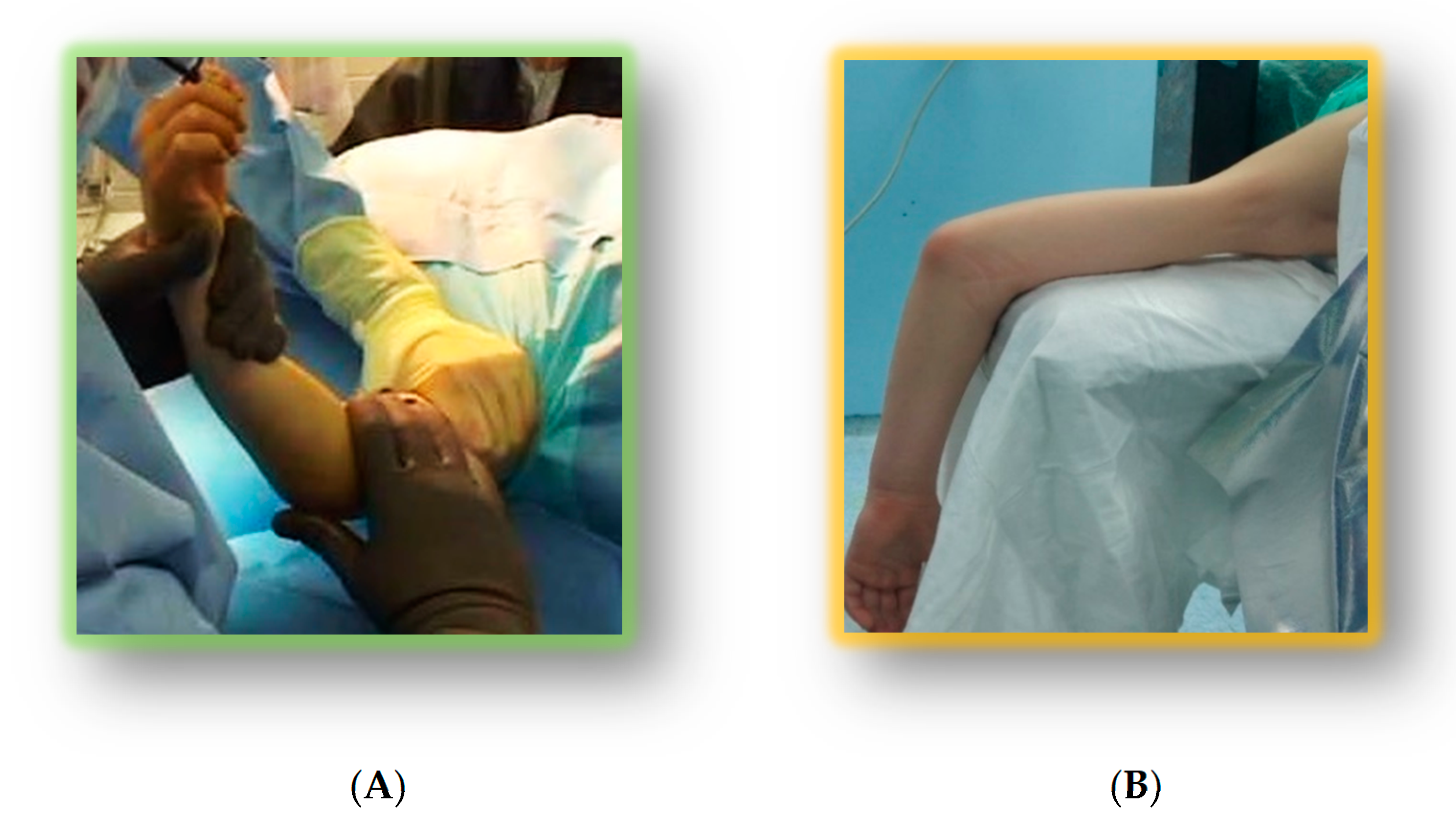
2.2. Treatment Protocol
2.3. Clinical and Radiological Assessments
2.4. Statistical Analysis
3. Results
3.1. Sample
3.2. Clinical and Radiological Assessments
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- de Neira, J.Z.S.; Prada-Cañizares, A.; Marti-Ciruelos, R.; Pretell-Mazzini, J. Supracondylar humeral fractures in children: Current concepts for management and prognosis. Int. Orthop. 2015, 39, 2287–2296. [Google Scholar] [CrossRef]
- Pavone, V.; Riccioli, M.; Testa, G.; Lucenti, L.; De Cristo, C.; Condorelli, G.; Avondo, S.; Sessa, G. Surgical Treatment of Displaced Supracondylar Pediatric Humerus Fractures: Comparison of Two Pinning Techniques. J. Funct. Morphol. Kinesiol. 2016, 1, 39. [Google Scholar] [CrossRef]
- Pavone, V.; Vescio, A.; Lucenti, L.; Chisari, E.; Canavese, F.; Testa, G. Analysis of loss of reduction as risk factor for additional secondary displacement in children with displaced distal radius fractures treated conservatively. Orthop. Traumatol. Surg. Res. 2020, 106, 193–198. [Google Scholar] [CrossRef]
- Barron-Torres, E.A.; Sanchez-Cruz, J.F.; Cruz-Melendez, J.R. Clinical and epidemiological characteristic of humeral supracondylar fractures in pediatric patients in a Regional General Hospital. Cir. Cir. 2015, 83, 29–34. [Google Scholar]
- De Pellegrin, M.; Brivio, A.; Pescatori, E.; Tessari, L. Supracondylar humerus fractures in children: Closed reduction and cross pin fixation in prone position. GIOT 2008, 34, 199–204. [Google Scholar]
- Dua, A.; Eachempati, K.K.; Malhotra, R.; Sharma, L.; Gidaganti, M. Closed reduction and percutaneous pinning of displaced supracondylar fractures of humerus in children with delayed presentation. Chin. J. Traumatol. 2011, 14, 14–19. [Google Scholar]
- Gupta, N.; Kay, R.M.; Leitch, K.; Femino, J.D.; Tolo, V.T.; Skaggs, D.L. Effect of surgical delay on perioperative complications and need for open reduction in supracondylar humerus fractures in children. J. Pediatr. Orthop. 2004, 24, 245–248. [Google Scholar] [CrossRef]
- Mangwani, J.; Nadarajah, R.; Paterson, J.M. Supracondylar humeral fractures in children: Ten years’ experience in a teaching hospital. J. Bone Jt. Surg. Br. 2006, 88, 362–365. [Google Scholar] [CrossRef]
- Mommsen, P.; Zeckey, C.; Hildebrand, F.; Frink, M.; Khaladj, N.; Lange, N.; Krettek, C.; Probst, C. Traumatic extremity arterial injury in children: Epidemiology, diagnostics, treatment and prognostic value of Mangl1ed Extremity Severity Score. J. Orthop. Surg. Res. 2010, 15, 25–35. [Google Scholar] [CrossRef]
- Skaggs, D.L.; Hale, J.M.; Bassett, J.; Kaminsky, C.; Kay, R.M.; Tolo, V.T. Operative treatment of supracondylar fractures of the humerus in children. The consequences of pin placement. J. Bone Jt. Surg. Am. 2001, 83, 735–740. [Google Scholar] [CrossRef]
- Havlas, V.; Trc, T.; Gaheer, R.; Schejbalova, A. Manipulation of pediatric supracondylar fractures of humerus in prone position under general anesthesia. J. Pediatr. Orthop. 2008, 28, 660–664. [Google Scholar] [CrossRef]
- Pescatori, E.; Memeo, A.; Brivio, A.; Trapletti, A.; Camurri, S.; Pedretti, L.; Albisetti, W. Supracondylar humerus fractures in children: Comparison of experiences. J. Pediatr. Orthop. B 2012, 21, 505–513. [Google Scholar] [CrossRef]
- Guler, O.; Mutlu, S.; Isyar, M.; Mutlu, H.; Cerci, H.; Mahirogullari, M. Prone versus supine position during surgery for supracondylar humeral fractures. J. Orthop. Surg. (Hong Kong) 2016, 24, 167–169. [Google Scholar] [CrossRef]
- Flynn, J.C.; Matthews, J.G.; Benoit, R.L. Blind pinning of displaced supracondylar fractures of the humerus in children. Sixteen years’ experience with long-term follow-up. J. Bone Jt. Surg. 1974, 56, 263–272. [Google Scholar] [CrossRef]
- Longo, U.G.; Franceschi, F.; Loppini, M.; Maffulli, N.; Denaro, V. Rating systems for evaluation of the elbow. Br. Med. Bull. 2008, 87, 131–161. [Google Scholar] [CrossRef]
- Mallo, G.; Stanat, S.J.; Gaffney, J. Use of the Gartland classification system for treatment of pediatric supracondylar humerus fractures. Orthopedics 2010, 33, 19. [Google Scholar] [CrossRef]
- Silva, M.; Pandarinath, R.; Farng, E.; Park, S.; Caneda, C.; Fong, Y.J.; Penman, A. Inter- and intra-observer reliability of the Baumann angle of the humerus in children with supracondylar humeral fractures. Int. Orthop. 2010, 34, 553–557. [Google Scholar] [CrossRef]
- Heggeness, M.H.; Sanders, J.O.; Murray, J.; Pezold, R.; Sevarino, K.S. Management of Pediatric Supracondylar Humerus Fractures. J. Am. Acad. Orthop. Surg. 2015, 23, e49–e51. [Google Scholar] [CrossRef]
- Sanders, J.O.; Heggeness, M.H.; Murray, J.N.; Pezold, R.C.; Sevarino, K.S. Management of Pediatric Supracondylar Humerus Fractures with Vascular Injury. J. Am. Acad. Orthop. Surg. 2016, 24, e21–e23. [Google Scholar] [CrossRef]
- Mooney, J.F., III; Hosseinzadeh, P.; Oetgen, M.; Cappello, T. AAOS appropriate use criteria: Management of pediatric supracondylar humerus fractures with vascular injury. J. Am. Acad. Orthop. Surg. 2016, 24, e24–e28. [Google Scholar] [CrossRef]
- Mulpuri, K.; Wilkins, K. The treatment of displaced supracondylar humerus fractures: Evidence-based guideline. J. Pediatr. Orthop. 2012, 32, S143–S152. [Google Scholar] [CrossRef]
- Marengo, L.; Cravino, M.; Origo, C. Practices concerning management of Gartland type III supracondylar humeral fractures among Italian pediatric orthopedic surgeons. J. Pediatr. Orthop. 2019, 28, 267–270. [Google Scholar] [CrossRef]
- Schmid, T.; Joeris, A.; Slongo, T.; Ahmad, S.S.; Ziebarth, K. Displaced supracondylar humeral fractures: Influence of delay of surgery on the incidence of open reduction, complications and outcome. Arch. Orthop. Trauma Surg. 2015, 135, 963–969. [Google Scholar] [CrossRef]
- Flierl, M.A.; Carry, P.M.; Scott, F.; Georgopoulos, G.; Hadley-Miller, N. Rotation and displacement predict adverse events in pediatric supracondylar fractures. Orthopedics 2015, 38, e690–e695. [Google Scholar] [CrossRef]
- Koehler, S.M.; Sakamoto, S.; Abernathie, B.L.; Hausman, M.R. Arthroscopic correction of a supracondylar malunion in a child. Arthorosc. Tech. 2015, 4, e215–e221. [Google Scholar] [CrossRef]
- Brauer, C.A.; Lee, B.M.; Bae, D.S.; Waters, P.M.; Kocher, M.S. A systematic review of medial and lateral entry pinning versus lateral entry pinning for supracondylar fractures of the humerus. J. Pediatr. Orthop. 2007, 27, 181–186. [Google Scholar] [CrossRef]
- Larson, L.; Firoozbakhsh, K.; Passarelli, R.; Bosch, P. Biomechanical analysis of pinning techniques for pediatric supracondylar humerus fractures. J. Pediatr. Orthop. 2006, 26, 573–578. [Google Scholar] [CrossRef]
- Sibinski, M.; Sharma, H.; Sherlock, D.A. Lateral versus crossed wire fixation for displaced extension supracondylar humeral fractures in children. Injury 2006, 37, 961–965. [Google Scholar] [CrossRef] [PubMed]
- Boero, S.; Catena, N.; De Pellegrin, M.; Società Italiana di Ortopedia e Traumatologia Pediatrica (S.I.T.O.P.) Group. Surgical treatment of supracondylar fractures in child. GIOT 2018, 44, 257–263. [Google Scholar]
- Venkatadass, K.; Balachandar, G.; Rajasekaran, S. Is Prone Position Ideal for Manipulation and Pinning of Displaced Pediatric Extension-type Supracondylar Fractures of Humerus? A Randomized Control Trial. J. Pediatr. Orthop. 2015, 35, 672–676. [Google Scholar] [CrossRef] [PubMed]
- Kao, H.K.; Lee, W.C.; Yang, W.E.; Chang, C.H. Treatment of displaced flexion-type pediatric supracondylar humeral fractures in the prone position. J. Orthop. Surg. (Hong Kong) 2017, 25, 2309499016684412. [Google Scholar] [CrossRef] [PubMed]
- De Pellegrin, M.; Fracassetti, D.; Moharamzadeh, D.; Origo, C.; Catena, N. Advantages and disadvantages of the prone position in the surgical treatment of supracondylar humerus fractures in children. A literature review. Injury 2018, 49, S37–S42. [Google Scholar] [CrossRef] [PubMed]
- Catena, N.; Calevo, M.G.; Fracassetti, D.; Moharamzadeh, D.; Origo, C.; De Pellegrin, M. Risk of ulnar nerve injury during cross-pinning in supine and prone position for supracondylar humeral fractures in children: A recent literature review. Eur. J. Orthop. Surg. Traumatol. 2019, 29, 1169–1175. [Google Scholar] [CrossRef] [PubMed]
- Anwar, R.; Rahman, N.; Iqbal, M.J.; Khan, M.A. Comparison of the two methods of percutaneous K-wire fixation in displaced supracondylar fracture of the humerus in children. J. Post. Grad. Med. Instr. 2011, 25, 356–361. [Google Scholar]
- Barlas, K.; George, B.; Hashmi, F.; Bagga, T. Open medial placement of Kirschner wires for supracondylar humeral fractures in children. J. Orthop. Surg. [Hong Kong] 2006, 14, 53–57. [Google Scholar] [CrossRef]
- Lacher, M.; Schaeffer, K.; Boehm, R.; Dietz, H.G. The treatment of supracondylar humeral fractures with elastic stable intramedullary nailing (ESIN) in children. J. Pediatr. Orthop. 2011, 31, 33–38. [Google Scholar] [CrossRef]
- Schaffer, K.; Bohm, R.; Dietz, H.G. Elastic stable intramedullary nailing (ESIN) of supracondylar fractures of the humerus in children. Unfallchirurg 2007, 110, 852–858. [Google Scholar] [CrossRef]
- Prevot, J.; Lascombes, P.; Metaizeau, J.P.; Blanquart, D. Supracondylar fractures of the humerus in children: Treatment by downward nailing. Rev. Chir. Orthop. Reparatrice Appar. Mot. 1990, 76, 191–197. [Google Scholar]
- Wendling-Keim, D.S.; Binder, M.; Dietz, H.G.; Lehner, M. Prognostic Factors for the Outcome of Supracondylar Humeral Fractures in Children. Orthop. Surg. 2019, 11, 690–697. [Google Scholar] [CrossRef]
- Kim, W.Y.; Chandru, R.; Bonshahi, A.; Paton, R.W. Displaced supracondylar humeral fractures in children: Results of a national survey of paediatric orthopaedic consultants. Injury 2003, 34, 274–277. [Google Scholar] [CrossRef]
- Saarinen, A.J.; Helenius, I. Paediatric supracondylar humeral fractures: The effect of the surgical specialty on the outcomes. J. Child. Orthop. 2019, 13, 40–46. [Google Scholar] [CrossRef] [PubMed]
- Tuomilehto, N.; Sommarhem, A.; Nietosvaara, A.Y. 9 years’ follow-up of 168 pin-fixed supracondylar humerus fractures in children. Acta Orthop. 2018, 89, 351–356. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Group 1—Supine Position (n = 34) | Group 2—Prone Position (n = 25) | p-Value |
|---|---|---|---|
| Age (years) | 6.1 ± 2.8 | 5.9 ± 2.3 | 0.77 |
| Gender (Male/Female) | 22/12 (64.7%) | 12/13 (48%) | 0.66 |
| Left Side (Left/Right) | 18/16 | 14/11 | 0.53 |
| Follow up (months) | 59.8 ± 15.8 | 59.9 ± 12.8 | 0.74 |
| Result | Rating | Cosmetic Factor Loss of Carrying Angle (degrees) | Functional Factor Motion Loss (degrees) |
|---|---|---|---|
| Satisfactory | Excellent | 0–5 | 0–5 |
| Good | 5–10 | 5–10 | |
| Fair | 10–15 | 10–15 | |
| Unsatisfactory | Poor | >15 | >15 |
| Feature | Rating | Score |
|---|---|---|
| Pain Intensity | None | 45 |
| Mild | 30 | |
| Moderate | 15 | |
| Severe | 0 | |
| Arc of Motion | >100° | 20 |
| 50°–100° | 15 | |
| <50° | 5 | |
| Stability | Stable | 10 |
| Moderate instability | 5 | |
| Moderate instability | 0 | |
| Function | Can comb hair | 5 |
| Can eat | 5 | |
| Can perform hygiene | 5 | |
| Can put on shirt | 5 | |
| Can lace shoe | 5 | |
| Maximum Score | 100 |
| Group 1 (n = 34) | Group 2 (n = 25) | p-Value | ||
|---|---|---|---|---|
| Excellent | 32 (94.1%) | 25 (100%) | 0.22 | |
| Flynn Criteria | Good | 2 (5.9%) | 0 | |
| Fair | 0 | 0 | ||
| Poor | 0 | 0 | ||
| Extension | 3.4 ± 1.8 | 2.9 ± 2.2 | 0.35 | |
| Flexion | 110.9 ± 14.3 | 113.6 ± 11.2 | 0.44 | |
| Supination-Pronation | 84.9 ± 3.1 | 86.2 ± 2.2 | 0.08 | |
| Mayo Elbow Performance Score | 96.0 ± 3.8 | 97.8 ± 3.3 | 0.06 | |
| Modified Baumann’s Angle (deg) | 5.5 ± 1.0 | 5.1 ± 1.1 | 0.15 | |
| Reoperations | 0 | 0 | ||
| Minor Complications | 4 (11.4%) | 3 (12%) | ||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pavone, V.; Vescio, A.; Riccioli, M.; Culmone, A.; Cosentino, P.; Caponnetto, M.; Dimartino, S.; Testa, G. Is Supine Position Superior to Prone Position in the Surgical Pinning of Supracondylar Humerus Fracture in Children? J. Funct. Morphol. Kinesiol. 2020, 5, 57. https://doi.org/10.3390/jfmk5030057
Pavone V, Vescio A, Riccioli M, Culmone A, Cosentino P, Caponnetto M, Dimartino S, Testa G. Is Supine Position Superior to Prone Position in the Surgical Pinning of Supracondylar Humerus Fracture in Children? Journal of Functional Morphology and Kinesiology. 2020; 5(3):57. https://doi.org/10.3390/jfmk5030057
Chicago/Turabian StylePavone, Vito, Andrea Vescio, Maria Riccioli, Annalisa Culmone, Pierluigi Cosentino, Marco Caponnetto, Sara Dimartino, and Gianluca Testa. 2020. "Is Supine Position Superior to Prone Position in the Surgical Pinning of Supracondylar Humerus Fracture in Children?" Journal of Functional Morphology and Kinesiology 5, no. 3: 57. https://doi.org/10.3390/jfmk5030057
APA StylePavone, V., Vescio, A., Riccioli, M., Culmone, A., Cosentino, P., Caponnetto, M., Dimartino, S., & Testa, G. (2020). Is Supine Position Superior to Prone Position in the Surgical Pinning of Supracondylar Humerus Fracture in Children? Journal of Functional Morphology and Kinesiology, 5(3), 57. https://doi.org/10.3390/jfmk5030057






