Prevalence of Antimicrobial Resistance in Bacterial Isolates from Dogs and Cats in a Veterinary Diagnostic Laboratory in Colombia from 2016–2019
Abstract
1. Introduction
2. Materials and Methods
3. Results
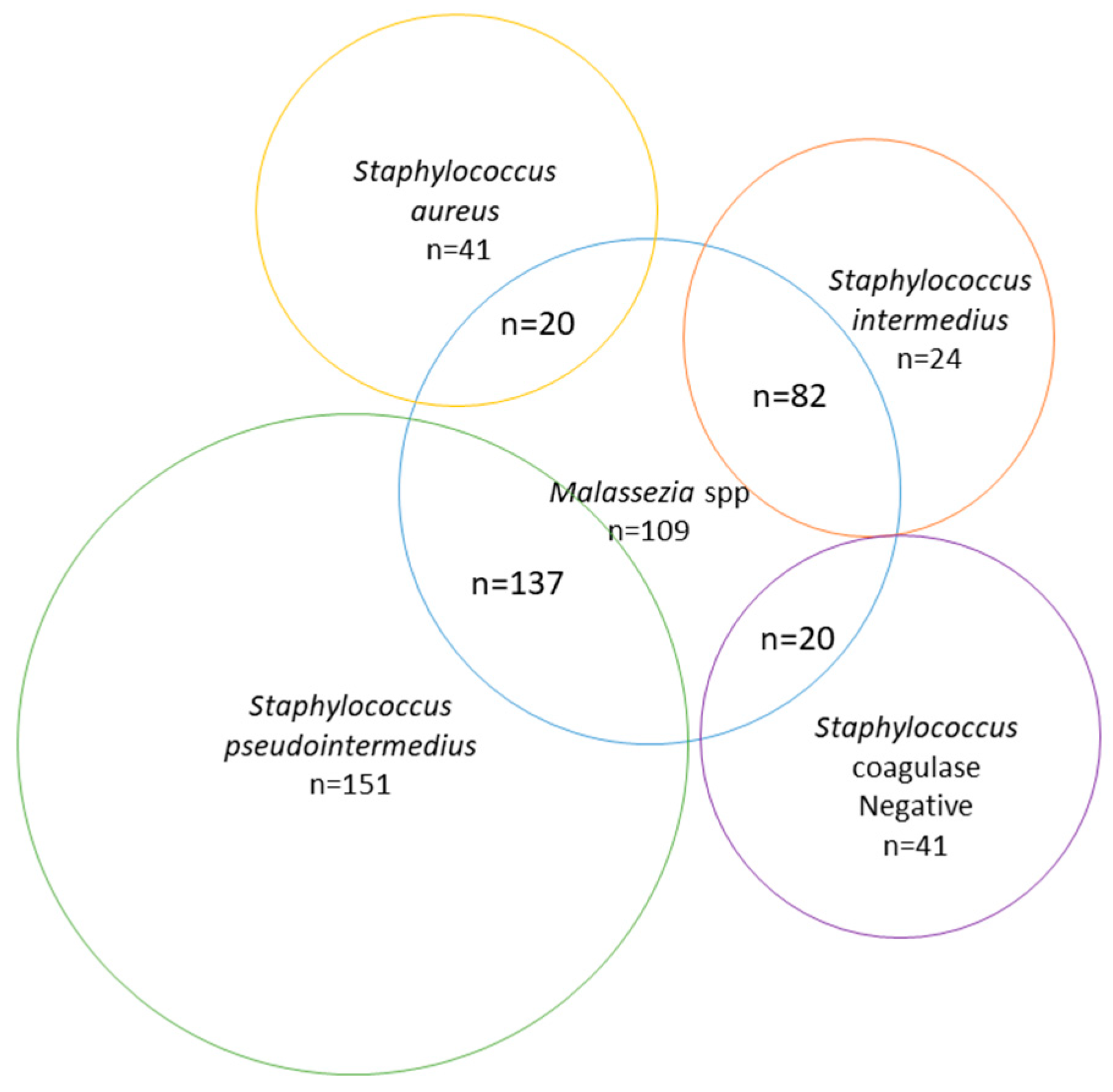
3.1. Dog Isolates and Antimicrobial Susceptibility
3.2. Cat Isolates and Antimicrobial Susceptibility
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Awosile, B.; McClure, J.T.; Saab, M.E.; Heider, L.C. Antimicrobial resistance in bacteria isolated from cats and dogs from the Atlantic Provinces, Canada from 1994–2013. Can. Vet. J. 2018, 59, 885–893. [Google Scholar] [PubMed]
- Authier, S.; Paquette, D.; Labrecque, O.; Messier, S. Comparison of susceptibility to antimicrobials of bacterial isolates from companion animals in a veterinary diagnostic laboratory in Canada between 2 time points 10 years apart. Can. Vet. J. 2006, 47, 774–778. [Google Scholar] [PubMed]
- Donado-Godoy, P.; Castellanos, L.R.; Leon, M.; Arévalo, A.; Clavijo, V.; Bernal, J.; León, D.; Tafur, M.A.; Byrne, B.A.; Smith, W.A.; et al. The Establishment of the Colombian Integrated Program for Antimicrobial Resistance Surveillance (COIPARS): A Pilot Project on Poultry Farms, Slaughterhouses and Retail Market. Zoonoses Public Heal. 2015, 62 (Suppl. 1), 58–69. [Google Scholar] [CrossRef] [PubMed]
- Biemer, J.J. Antimicrobial susceptibility testing by the Kirby-Bauer disc diffusion method. Ann. Clin. Lab. Sci. 1973, 3, 135–140. [Google Scholar]
- Clinical and Laboratory Standards Institute (CLSI). Performance Standards for Antimicrobial Dick and Dilutions Susceptibility Test for Bacteria Isolated from Animals, 4th ed.; CLSI Supplement Vet08; CLSI: Wayne, NY, USA, 2018. [Google Scholar]
- Magiorakos, A.-P.; Srinivasan, A.; Carey, R.; Carmeli, Y.; Falagas, M.; Giske, C.; Harbarth, S.J.; Hindler, J.; Kahlmeter, G.; Olsson-Liljequist, B.; et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: An international expert proposal for interim standard definitions for acquired resistance. Clin. Microbiol. Infect. 2012, 18, 268–281. [Google Scholar] [CrossRef]
- EFSA (European Food Safety Authority) and ECDC (European Centre for Disease Prevention and Control). EU Summary Report on antimicrobial resistance in zoonotic and indicator bacteria from humans, animals and food in 2013. EFSA J. 2015, 13, 4036–4214. [Google Scholar]
- Lee, G.-Y.; Lee, H.-H.; Hwang, S.Y.; Hong, J.; Lyoo, K.-S.; Yang, S.-J. Carriage of Staphylococcus schleiferi from canine otitis externa: Antimicrobial resistance profiles and virulence factors associated with skin infection. J. Vet. Sci. 2019, 20, e6. [Google Scholar] [CrossRef]
- Penna, B.; Varges, R.; Medeiros, L.; Martins, G.; Martins, R.; Lilenbaum, W. In vitro antimicrobial susceptibility of staphylococci isolated from canine pyoderma in Rio de Janeiro, Brazil. Braz. J. Microbiol. 2009, 40, 490–494. [Google Scholar] [CrossRef]
- Ludwig, C.; De Jong, A.; Moyaert, H.; El Garch, F.; Janes, R.; Klein, U.; Morrissey, I.; Thiry, J.; Youala, M. Antimicrobial susceptibility monitoring of dermatological bacterial pathogens isolated from diseased dogs and cats across Europe (ComPath results). J. Appl. Microbiol. 2016, 121, 1254–1267. [Google Scholar] [CrossRef]
- Conner, J.G.; Smith, J.; Erol, E.; Locke, S.; Phillips, E.; Carter, C.N.; Odoi, A. Temporal trends and predictors of antimicrobial resistance among Staphylococcus spp. isolated from canine specimens submitted to a diagnostic laboratory. PLoS ONE 2018, 13, e0200719. [Google Scholar] [CrossRef]
- Schmidt, V.M.; Williams, N.J.; Pinchbeck, G.; Corless, C.; Shaw, S.; McEwan, N.; Dawson, S.; Nuttall, T. Antimicrobial resistance and characterisation of staphylococci isolated from healthy Labrador retrievers in the United Kingdom. BMC Vet. Res. 2014, 10, 17. [Google Scholar] [CrossRef] [PubMed]
- Gandolfi-Decristophoris, P.; Schüpbach-Regula, G.; Petrini, O.; Zinsstag, J.; Schelling, E. Prevalence and risk factors for carriage of multi-drug resistantStaphylococciin healthy cats and dogs. J. Vet. Sci. 2013, 14, 449–456. [Google Scholar] [CrossRef] [PubMed]
- Bourély, C.; Cazeau, G.; Jarrige, N.; Leblond, A.; Madec, J.; Haenni, M.; Gay, E. Antimicrobial resistance patterns of bacteria isolated from dogs with otitis. Epidemiol. Infect. 2019, 147, e121. [Google Scholar] [CrossRef] [PubMed]
- Hillier, A.; Lloyd, D.H.; Weese, J.S.; Blondeau, J.M.; Boothe, D.; Breitschwerdt, E.; Guardabassi, L.; Papich, M.G.; Rankin, S.; Turnidge, J.D.; et al. Guidelines for the diagnosis and antimicrobial therapy of canine superficial bacterial folliculitis (Antimicrobial Guidelines Working Group of the International Society for Companion Animal Infectious Diseases). Vet. Dermatol. 2014, 25, 163-e43. [Google Scholar] [CrossRef]
- Magalhães, R.J.S.; Loeffler, A.; Lindsay, J.; Rich, M.; Roberts, L.; Smith, H.; Lloyd, D.H.; Pfeiffer, D.U. Risk factors for methicillin-resistantStaphylococcus aureus(MRSA) infection in dogs and cats: A case-control study. Vet. Res. 2010, 41, 55. [Google Scholar] [CrossRef]
- Faires, M.C.; Traverse, M.; Tater, K.C.; Pearl, D.L.; Weese, J.S. Methicillin-Resistant and -Susceptible Staphylococcus aureus Infections in Dogs. Emerg. Infect. Dis. 2010, 16, 69–75. [Google Scholar] [CrossRef]
- Eckholm, N.G.; Outerbridge, C.A.; White, S.D.; Sykes, J.E. Prevalence of and risk factors for isolation of meticillin-resistant Staphylococcus spp. from dogs with pyoderma in northern California, USA. Vet. Dermatol. 2013, 24, 154–161.e34. [Google Scholar] [CrossRef]
- Frank, L.A.; Loeffer, L.A. Meticillin-resistant Staphylococcus pseudointermedius: Clinical challenge and treatment options. Vet. Dermatol. 2012, 23, 283–291.e56. [Google Scholar] [CrossRef]
- Weese, J.S.; Faires, M.C.; Frank, L.A.; Reynolds, L.M.; Battisti, A. Factors associated with methicillin-resistant versus methicillin-susceptible Staphylococcus pseudointermedius infection in dogs. J. Am. Vet. Med. Assoc. 2012, 240, 1450–1455. [Google Scholar] [CrossRef]
- Hensel, N.; Zabel, S. Prior antibacterial drug exposure in dogs with meticillin-resistant Staphylococcus pseudintermedius (MRSP) pyoderma. Vet. Dermatol. 2016, 27, 72. [Google Scholar] [CrossRef]
- Loeffler, A.; Linek, M.; Moodley, A.; Guardabassi, L.; Sung, J.M.L.; Winkler, M.; Weiss, R.; Lloyd, D.H. First report of multiresistant, mecA-positive Staphylococcus intermedius in Europe: 12 cases from a veterinary dermatology referral clinic in Germany. Vet. Dermatol. 2007, 18, 412–421. [Google Scholar] [CrossRef] [PubMed]
- Ball, K.R.; Rubin, J.E.; Chirino-Trejo, M.; Dowling, P.M. Antimicrobial resistance and prevalence of canine uropathogens at the Western College of Veterinary Medicine Veterinary Teaching Hospital, 2002–2007. Can. Vet. J. 2008, 49, 985–990. [Google Scholar] [PubMed]
- Roberts, M.; White, J.; Lam, A. Prevalence of bacteria and changes in trends in antimicrobial resistance of Escherichia coli isolated from positive canine urinary samples from an Australian referral hospital over a 5-year period (2013–2017). Vet. Rec. Open 2019, 6, e000345. [Google Scholar] [CrossRef] [PubMed]
- Qekwana, D.N.; Phophi, L.; Naidoo, V.; Oguttu, J.W.; Odoi, A. Antimicrobial resistance among Escherichia coli isolates from dogs presented with urinary tract infections at a veterinary teaching hospital in South Africa. BMC Vet. Res. 2018, 14, 228. [Google Scholar] [CrossRef]
- Marques, C.; Gama, L.T.; Belas, A.; Bergström, K.; Beurlet, S.; Briend-Marchal, A.; Broens, E.M.; Costa, M.; Criel, D.; Damborg, P.; et al. European multicenter study on antimicrobial resistance in bacteria isolated from companion animal urinary tract infections. BMC Vet. Res. 2016, 12, 1–17. [Google Scholar] [CrossRef]
- Thungrat, K.; Price, S.B.; Carpenter, D.M.; Boothe, D. Antimicrobial susceptibility patterns of clinical Escherichia coli isolates from dogs and cats in the United States: January 2008 through January 2013. Vet. Microbiol. 2015, 179, 287–295. [Google Scholar] [CrossRef]
- Weese, J.S.; Blondeau, J.; Boothe, D.; Guardabassi, L.G.; Gumley, N.; Papich, M.; Jessen, L.R.; Lappin, M.; Rankin, S.; Westropp, J.L.; et al. International Society for Companion Animal Infectious Diseases (ISCAID) guidelines for the diagnosis and management of bacterial urinary tract infections in dogs and cats. Vet. J. 2019, 247, 8–25. [Google Scholar] [CrossRef]
- Penna, B.; Varges, R.; Martins, R.; Martins, G.; Lilenbaum, W. In vitro antimicrobial resistance of staphylococci isolated from canine urinary tract infection. Can. Vet. J. 2010, 51, 738–742. [Google Scholar]
- Wong, C.; Epstein, S.E.; Westropp, J. Antimicrobial Susceptibility Patterns in Urinary Tract Infections in Dogs (2010–2013). J. Vet. Intern. Med. 2015, 29, 1045–1052. [Google Scholar] [CrossRef]
| Clinical Samples | n | Enterobacteriaceaea | Enterococcus spp. b | Escherichia coli. | Pseudomonasc | Staphylococcus Coagulase Negative d | Staphylococcus Coagulase Positive e | Streptococcus spp. | Others f |
|---|---|---|---|---|---|---|---|---|---|
| % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | ||
| Ear | 667 | 9.1 (7.2–11.6) | 7.3 (5.6–9.6) | 3.3 (2.2–4.9) | 7.9 (6.1–10.29 | 6.7 (5.0–8.9) | 64.0 (60.3–67.6) | 0.9 (0.4–1.9) | 0.6 (0.2–1.5) |
| Wound | 240 | 8.3 (5.5–12.5) | 5.0 (2.9–8.5) | 4.6 (2.5–8.0) | 4.2 (2.3–7.5) | 10.4 (7.1–14.9) | 65.0 (58.8–70.7) | 1.3 (0.4–3.6) | 1.3 (0.40–3.6) |
| Urine | 226 | 34.1 (28.2–40.5) | 5.3 (3.1–9.0) | 46.5 (40.1–52.9) | 2.2 (0.9–5.0) | 1.8 (0.7–4.5) | 9.7 (6.5–14.3) | 0.4 (0.1–2.5) | 0 (0–1.7) |
| Skin | 45 | 2.2 (0.4–11.6) | 4.4 (1.2–14.8) | 2.2 (0.4–11.6) | 4.4 (1.2–14.8) | 33.3 (21.3–47.9) | 48.9 (35.0–63.0) | 2.2 (0.4–11.6) | 2.2 (0.4–11.6) |
| Nasal cavity | 34 | 17.6 (8.3–33.5) | 11.8 (4.7–26.6) | 14.7 (6.4–30.1) | 0 (0–10.2) | 2.9 (0.52–14.9) | 35.3 (21.5–52.1) | 5.9 (1.6–19.1) | 11.8 (4.7–26.6) |
| Abscess | 18 | 5.6 (1.0–25.7) | 22.2 (9.0–45.2) | 22.2 (5.8–39.2) | 11.1 (3.1–32.8) | 0 (0–17.6) | 38.9 (20.3–61.4) | 0 (0–17.6) | 5.6 (1.0–25.7) |
| Eyes | 15 | 6.7 (1.19–29.8) | 0 (0–20.4) | 20.0 (7.0–45.2) | 6.7 (1.2–29.8) | 26.7 (10.9–51.9) | 33.3 (15.2–58.3) | 6.7 (1.2–29.8) | 0 (0–20.4) |
| Surgical | 11 | 0 (0–25.9) | 9.1 (1.6–37.7) | 27.3 (9.7–56.5) | 27.3 (9.7–56.5) | 18.2 (5.1–47.7) | 18.2 (5.1–47.7) | 0 (0–25.9) | 0 (0–25.9) |
| Bacteria | n | % Susceptible | MDR (%) | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AMK | AMC | AMP | CEX | ENO | GEN | TMS | DOX | TET | CIP | FLO | PEN | AMPS | CET | RIF | CEF | NEO | CHL | ERY | CFP | |||
| Enterobacteriaceae | 183 | 100 | 76.7 | 61.8 | 60.9 | 64.4 | 89 | 83.9 | 38.7 | 52.2 | 84.4 | 100 | - | 75 | - | - | 56.9 | 83.3 | - | - | - | 18.6 |
| Enterococcus spp. | 90 | 66.7 | 89.7 | 84.9 | 28.6 | 24.7 | 64.7 | 36.4 | 38.3 | 50.9 | 66.7 | 96 | 88.2 | 88.2 | - | - | 42.9 | - | 80 | 20 | - | 20.0 |
| Escherichia coli | 163 | 100 | 66.7 | 67.7 | 72.3 | 69.2 | 89.8 | 77.6 | 68.7 | 64.5 | 75 | 100 | - | 83.3 | 57.4 | - | 70.7 | 66.7 | - | - | - | 17.2 |
| Other * | 14 | 87.5 | 90 | 91.7 | 100 | 90.9 | 88.9 | 83.3 | - | - | - | - | - | - | - | - | - | - | - | - | - | 7.1 |
| Pseudomonas spp. | 79 | 93.9 | 14.7 | 16.2 | 8.3 | 31.8 | 86.7 | 21.4 | 17.2 | 12.5 | 91.4 | - | - | 17.2 | - | - | 0% | 33.3 | - | - | - | 49.4 |
| Staphylococcus coagulase Negative | 101 | 78.2 | 96.9 | 77.4 | 83.5 | 82.7 | 73.3 | 65.3 | 100 | 38.5 | 66.7 | - | - | 50 | - | - | 100 | 71.4 | - | - | - | 10.9 |
| Staphylococusaureus | 104 | 100 | 100 | 75.5 | 74.7 | 59.8 | 59.8 | 62.3 | 91.7 | 25 | 92.3 | - | - | - | - | - | - | - | - | - | - | 19.2 |
| Staphylococusintermedius | 160 | - | 84.4 | 74.7 | 73.3 | 58.6 | 80 | 60 | 70 | - | 85.5 | - | - | - | - | 100 | 96.6 | 75.6 | - | - | - | 16.9 |
| Staphylococospseudointermedius | 406 | 96.8 | 93.3 | 77.6 | 81.6 | 82.3 | 63.9 | 57 | 60.9 | 62.8 | 100 | - | - | 76 | - | - | 86.7 | - | - | - | 100 | 16.7 |
| Streptococcus spp. | 16 | 42.9 | 91.7 | 86.7 | 80 | 58.3 | 75 | 100 | - | 25 | - | - | - | - | - | - | 100 | - | - | - | - | 12.5 |
| Clinical Samples | n | Enterobacteriaceaea | Enterococcus spp. b | Escherichia coli. | Pseudomonasc | Staphylococcus Coagulase Negative d | Staphylococcus Coagulase Positive e | Streptococcus spp. f | Others |
|---|---|---|---|---|---|---|---|---|---|
| % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | ||
| Wound | 29 | 17.2 (7.6–34.5) | 10.3 (3.6–26.4) | 6.9 (1.9–21.9) | 6.9 (1.9–21.9) | 6.9 (1.9–22.0) | 44.8 (28.4–62.5) | 3.4 (0.6–17.2) | 3.4 (0.6–17.2) |
| Urine | 29 | 24.1 (12.2–42.1) | 6.9 (1.9–21.9) | 31 (17.3–49.2) | 13.8 (5.5–30.6) | 10.3 (3.6–26.4) | 13.8 (5.5–30.6) | 0 (0–11.7) | 0 (0–11.7) |
| Ear | 18 | 5.6 (1–25.7) | 5.6 (0.9–25.8) | 0 (0–17.6) | 5.6 (0.9–25.7) | 16.7 (5.8–39.2) | 66.7 (43.7–83.7) | 0 (0–17.6) | 0 (0–17.6) |
| Nasal cavity | 10 | 20 (5.7–50.9) | 10 (1.8–40.4) | 0 (0–27.7) | 0 (0–27.7) | 30 (10.8–60.3) | 30 (10.8–60.3) | 0 (0–27.7) | 10 (1.8–40.4) |
| Skin | 3 | 33.3 (6.14–79.23) | 33.3 (6.1–79.2) | 33.3 (6.1–79.2) | 0 (0–56.1) | 0 (0–56.1) | 0 (0–56.1) | 0 (0–56.1) | 0 (0–56.1) |
| Surgical | 2 | 0 (0–65.8) | 50 (9.5–90.5) | 0 (0–65.8) | 0 (0–65.8) | 0 (0–65.8) | 50 (9.5–90.5) | 0 (0–65.8) | 0 (0–65.8) |
| Abscess | 2 | 0 (0–65.8) | 0 (0–65.7) | 0 (0–65.8) | 0 (0–65.8) | 0 (0–65.8) | 50 (9.5–90.5) | 50 (9.5–90.5) | 0 (0–65.8) |
| Eyes | 1 | 0 (0–79.3) | 100 (20.6–100) | 0 (0–79.3) | 0 (0–79.3) | 0 (0–79.3) | 0 (0–79.3) | 0 (0–79.3) | 0 (0–79.3) |
| Bacteria | n | % Susceptible | MDR (%) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AMK | AMC | AMP | CEX | ENO | GEN | TMS | DOX | TET | CIP | FLO | CEF | |||
| Enterobacteriaceae | 18 | - | 72.2 | 46.2 | 66.7 | 26.7 | 66.7 | 63.6 | 61.5 | 80 | 66.7 | - | 50 | 33.3 |
| Staphylococusaureus | 16 | 100 | 85.7 | 83.3 | 64.3 | 93.3 | 100 | 88.9 | - | - | 92.3 | - | - | 6.3 |
| Escherichia coli | 13 | - | 66.7 | 54.5 | 72.3 | 63.6 | 70 | 60 | 62.5 | 64.5 | - | - | 100 | 30.8 |
| Others | 13 | - | - | - | - | - | - | - | - | - | - | - | - | 7.7 |
| Staphylococospseudointermedius | 13 | 100 | 100 | 91.7 | 100 | 92.3 | 100 | 57 | - | - | - | - | - | 0.0 |
| Enterococcus spp. | 11 | - | 63.6 | 75 | - | 37.5 | - | 25 | 25 | 42.9 | - | 87.5 | - | 18.2 |
| Staphylococcus coagulase Negative | 11 | 45.5 | 100 | 90.9 | 80 | 81.7 | 85.7 | 100 | - | - | - | - | - | 18.2 |
| Pseudomonas spp. | 8 | - | - | - | - | 50 | 100 | 50 | 50 | - | - | - | - | 37.5 |
| Staphylococusintermedius | 5 | - | 60 | 40 | 40 | - | - | - | - | - | 50 | - | - | 40.0 |
| Streptococcus spp. | 2 | - | - | - | - | - | - | - | - | - | - | - | - | 0.0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gómez-Beltrán, D.A.; Villar, D.; López-Osorio, S.; Ferguson, D.; Monsalve, L.K.; Chaparro-Gutiérrez, J.J. Prevalence of Antimicrobial Resistance in Bacterial Isolates from Dogs and Cats in a Veterinary Diagnostic Laboratory in Colombia from 2016–2019. Vet. Sci. 2020, 7, 173. https://doi.org/10.3390/vetsci7040173
Gómez-Beltrán DA, Villar D, López-Osorio S, Ferguson D, Monsalve LK, Chaparro-Gutiérrez JJ. Prevalence of Antimicrobial Resistance in Bacterial Isolates from Dogs and Cats in a Veterinary Diagnostic Laboratory in Colombia from 2016–2019. Veterinary Sciences. 2020; 7(4):173. https://doi.org/10.3390/vetsci7040173
Chicago/Turabian StyleGómez-Beltrán, David A., David Villar, Sara López-Osorio, Duncan Ferguson, Laura K. Monsalve, and Jenny J. Chaparro-Gutiérrez. 2020. "Prevalence of Antimicrobial Resistance in Bacterial Isolates from Dogs and Cats in a Veterinary Diagnostic Laboratory in Colombia from 2016–2019" Veterinary Sciences 7, no. 4: 173. https://doi.org/10.3390/vetsci7040173
APA StyleGómez-Beltrán, D. A., Villar, D., López-Osorio, S., Ferguson, D., Monsalve, L. K., & Chaparro-Gutiérrez, J. J. (2020). Prevalence of Antimicrobial Resistance in Bacterial Isolates from Dogs and Cats in a Veterinary Diagnostic Laboratory in Colombia from 2016–2019. Veterinary Sciences, 7(4), 173. https://doi.org/10.3390/vetsci7040173







