ESBL-Producing Enterobacterales at the Human–Domestic Animal–Wildlife Interface: A One Health Approach to Antimicrobial Resistance in Piauí, Northeastern Brazil
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Method
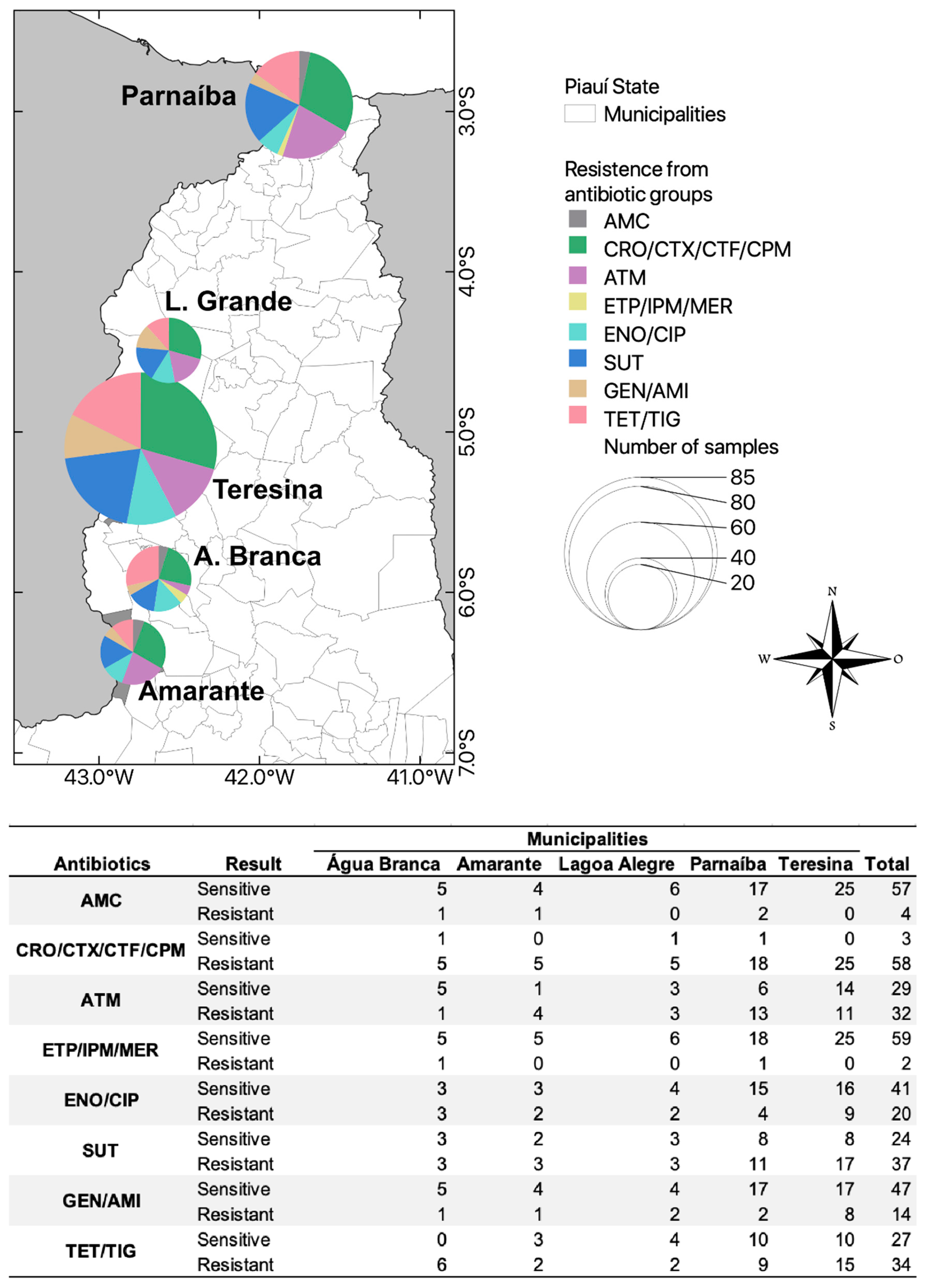
2.1. Study Area
2.2. Study Period and Group
2.3. Bird and Domestic Sampling
2.4. Laboratory Analysis
2.4.1. Antimicrobial Susceptibility Testing and Molecular Analysis
2.4.2. Bacterial Identification
3. Ethics Statement
4. Statistical Analysis
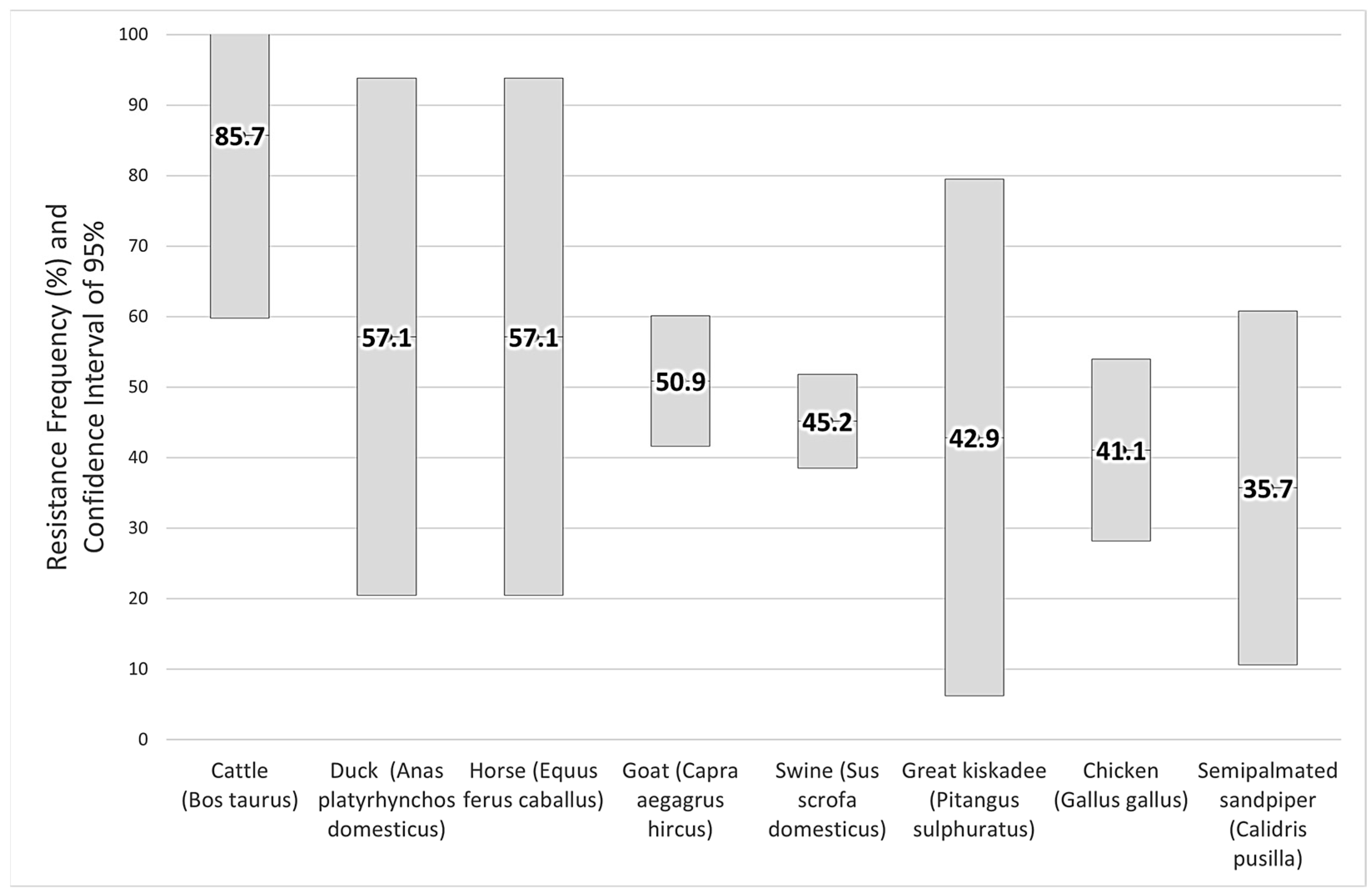
5. Results
6. Discussion
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Primer | Sequence (5′-3′) | Bp * | T (°C) ** | Reference |
|---|---|---|---|---|
| TEM-1 | F: GAGTATTCAACATTTCCGTGTC R: TAATCAGTGAGGCACCTATCT | 851 | 51 | [32] |
| SHV-1 | F: ATGCGTTATATTCGCCTGTG R: GTTAGCGTTGCCAGTGCTCG | 573 | 53 | [34] |
| CTX-M | F: CGCTTTGCGATGTGCAG R: ACCCGCGATATCGTTGGT | 550 | 49 | [31] |
| CTX-M-8 | F: GATGAGACATCGCGTTAAG R: GGTGACGATTTTCGCGGCA | 861 | 60 | [35] |
| CTX=M-15 | F: CACACGTGGAATTTAGGGACT R: GCCGTCTAAGGCGATAAACA | 995 | 56 | [33] |
References
- World Health Organization (WHO). Integrated Surveillance of Antimicrobial Resistance in Foodborne Bacteria: Application of a One Health Approach; World Health Organization: Geneva, Switzerland, 2017; p. 88. [Google Scholar]
- Ait Ouakrim, D.; Cassini, A.; Cecchini, M.; Plauchoras, D. The Health and Economic Burden of Antimicrobial Resistance. Eur. J. Public Health 2020, 30, ckaa165.1201. [Google Scholar] [CrossRef]
- Barrocas, A. Epidemiologia Das Beta-Lactamases CTX-M, Em Bactérias Gram Negativo, Em Portugal; Universidade de Coimbra: Lisbon, Portugal, 2016. [Google Scholar]
- Murray, P.R.; Rosenthal, K.S.; Pfaller, M.A. Medical Microbiology, 8th ed.; Elsevier Sander: Amsterdam, The Netherlands, 2016; Volume 8, ISBN 9780323299565. [Google Scholar]
- Carvalho, I.; Silva, N.; Carrola, J.; Silva, V.; Currie, C.; Igrejas, G.; Poeta, P. Immunity-Acquired Resistance: Evolution of Antimicrobial Resistance Among Extended-Spectrum Β-Lactamases and Carbapenemases in Klebsiella Pneumoniae and Escherichia coli. Antibiot. Drug Resist. 2020, 239–259. [Google Scholar] [CrossRef]
- Caudell, M.A.; Mair, C.; Subbiah, M.; Matthews, L.; Quinlan, R.J.; Quinlan, M.B.; Zadoks, R.; Keyyu, J.; Call, D.R.; Hernando-Amado, S.; et al. Identification of Risk Factors Associated with Carriage of Resistant Escherichia coli in Three Culturally Diverse Ethnic Groups in Tanzania: A Biological and Socioeconomic Analysis. Lancet Planet. Health 2018, 2, e489–e497. [Google Scholar] [CrossRef] [PubMed]
- Hernando-Amado, S.; Coque, T.M.; Baquero, F.; Martínez, J.L. Defining and Combating Antibiotic Resistance from One Health and Global Health Perspectives. Nat. Microbiol. 2019, 4, 1432–1442. [Google Scholar] [CrossRef]
- Tazerji, S.S.; Nardini, R.; Safdar, M.; Shehata, A.A.; Duarte, P.M. An Overview of Anthropogenic Actions as Drivers for Emerging and Re-Emerging Zoonotic Diseases. Pathogens 2022, 11, 1376. [Google Scholar] [CrossRef]
- Bonnedahl, J.; Järhult, J.D. Antibiotic Resistance in Wild Birds. Ups. J. Med. Sci. 2014, 119, 113–116. [Google Scholar] [CrossRef]
- Lin, Y.; Dong, X.; Sun, R.; Wu, J.; Tian, L.; Rao, D.; Zhang, L.; Yang, K. Migratory Birds-One Major Source of Environmental Antibiotic Resistance around Qinghai Lake, China. Sci. Total Environ. 2020, 739, 139758. [Google Scholar] [CrossRef]
- Carignan, V.; Villard, M. Selecting Indicator Species to Monitor Ecological Integrity: A Review. Environ. Monit. Assess. 2002, 78, 45–61. [Google Scholar] [CrossRef] [PubMed]
- Kaesbohrer, A.; Schroeter, A.; Tenhagen, B.A.; Alt, K.; Guerra, B.; Appel, B. Emerging Antimicrobial Resistance in Commensal Escherichia coli with Public Health Relevance. Zoonoses Public Health 2012, 59, 158–165. [Google Scholar] [CrossRef]
- Robinson, T.P.; Bu, D.P.; Carrique-Mas, J.; Fèvre, E.M.; Gilbert, M.; Grace, D.; Hay, S.I.; Jiwakanon, J.; Kakkar, M.; Kariuki, S.; et al. Antibiotic Resistance Is the Quintessential One Health Issue. Trans. R. Soc. Trop. Med. Hyg. 2016, 110, 377–380. [Google Scholar] [CrossRef]
- Ahmed, N.A.; Gulhan, T. Determination of Antibiotic Resistance Patterns and Genotypes of Escherichia coli Isolated from Wild Birds. Microbiome 2024, 12, 8. [Google Scholar] [CrossRef] [PubMed]
- McEwen, S.A.; Collignon, P.J. Antimicrobial Resistance: A One Health Perspective. Microbiol. Spectr. 2018, 6, 521–547. [Google Scholar] [CrossRef] [PubMed]
- Ministério da Saúde. Plano de Ação Nacional de Prevenção e Controle Da Resistência Aos Antimicrobianos No Âmbito Da Saúde Única 2018–2022. Diário da República, 1.a Série—N.o 96, 18 May 2018; p. 23. [Google Scholar]
- Rabello, R.F.; Bonelli, R.R.; Penna, B.A.; Albuquerque, J.P.; Souza, R.M.; Cerqueira, A.M.F. Antimicrobial Resistance in Farm Animals in Brazil: An Update Overview. Animals 2020, 10, 552. [Google Scholar] [CrossRef] [PubMed]
- Leal, I.R.; Tabarelli, M.; Silva, J.M.C. Da Ecologia e Conservação Da Caatinga. Ecol. Conserv. Caatinga 2003, 1, 822. [Google Scholar]
- Schmid, B.; Bernal, R.; Silva, N.N. Automedicação Em Adultos de Baixa Renda No Município de São Paulo. Rev. Saude Publica 2010, 44, 1039–1045. [Google Scholar] [CrossRef] [PubMed]
- Rossi, F. The Challenges of Antimicrobial Resistance in Brazil. Clin. Infect. Dis. 2011, 52, 1138–1143. [Google Scholar] [CrossRef]
- Bonelli, R.R.; Moreira, B.M.; Picão, R.C. Antimicrobial Resistance among Enterobacteriaceae in South America: History, Current Dissemination Status and Associated Socioeconomic Factors. Drug Resist. Updates 2014, 17, 24–36. [Google Scholar] [CrossRef] [PubMed]
- CEMAVE/ICMBio. Relatório de Rotas e Áreas de Concentração de Aves Migratórias No Brasil, 3rd ed.; ICMBio: Cabedelo, Parnaíba, Brazil, 2020; ISSN 2446-9750. (Online version). Available online: https://www.gov.br/icmbio/pt-br/centrais-de-conteudo/publicacoes/relatorios/relatorio_de_rotas_e_areas_de_concentracao_de_aves_migratorias_brasil_3edicao_2019.pdf (accessed on 17 March 2024).
- de Lima, M.G.; de Moraes, A.M.; Nunes, L.A.P.L.; de Andrade Júnior, A.S. Climas Do Piauí: Interações Com o Ambiente; Ribeiro, R.A., Ed.; EDUFPI: Piauí, Brazil, 2020; ISBN 978-65-86171-80-8. [Google Scholar]
- Tolsá, M.J.; García-Peña, G.E.; Rico-Chávez, O.; Roche, B.; Suzán, G. Macroecology of Birds Potentially Susceptible to West Nile Virus. Proc. R. Soc. B Biol. Sci. 2018, 285, 20182178. [Google Scholar] [CrossRef] [PubMed]
- Jacob, M.E.; Keelara, S.; Aidara-Kane, A.; Matheu Alvarez, J.R.; Fedorka-Cray, P.J. Optimizing a Screening Protocol for Potential Extended-Spectrum β-Lactamase Escherichia coli on MacConkey Agar for Use in a Global Surveillance Program. J. Clin. Microbiol. 2020, 58, e01039-19. [Google Scholar] [CrossRef]
- Clinical and Laboratory Standards Institute (CLSI). Performance Standards for Antimicrobial Susceptibility Testing, 28th ed.; CSLI supplement M100; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2018; ISBN 1-56238-839-8. (Electronic). [Google Scholar]
- Clinical and Laboratory Standards Institute (CLSI). Performance Standards for Antimicrobial Susceptibility Testing, 30th ed.; CLSI supplement M100; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2020; ISBN 978-1-68440-067-6. (Electronic). [Google Scholar]
- Jarlier, V.; Nicolas, M.H.; Fournier, G.; Philippon, A. Extended Broad-Spectrum β-Lactamases Conferring Transferable Resistance to Newer β-Lactam Agents in Enterobacteriaceae: Hospital Prevalence and Susceptibility Patterns. Clin. Infect. Dis. 1988, 10, 867–878. [Google Scholar] [CrossRef]
- Magiorakos, A.P.; Srinivasan, A.; Carey, R.B.; Carmeli, Y.; Falagas, M.E.; Giske, C.G.; Harbarth, S.; Hindler, J.F.; Kahlmeter, G.; Olsson-Liljequist, B.; et al. Multidrug-Resistant, Extensively Drug-Resistant and Pandrug-Resistant Bacteria: An International Expert Proposal for Interim Standard Definitions for Acquired Resistance. Clin. Microbiol. Infect. 2012, 18, 268–281. [Google Scholar] [CrossRef] [PubMed]
- da Silva, Q.M. Resistência Bacteriana a Antimicrobianos Em Uma Comunidade Remota Da Floresta Amazônica; Universidade de São Paulo: São Paulo, Brazil, 2017. [Google Scholar]
- Bonnet, R.; Dutour, C.; Sampaio, J.L.M.; Chanal, C.; Sirot, D.; Labia, R.; De Champs, C.; Sirot, J. Novel Cefotaximase (CTX-M-16) with Increased Catalytic Efficiency Due to Substitution Asp-240→Gly. Antimicrob. Agents Chemother. 2001, 45, 2269–2275. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Baraniak, A.; Fiett, J.; Mrówka, A.; Walory, J.; Hryniewicz, W.; Gniadkowski, M. Evolution of TEM-Type Extended-Spectrum β-Lactamases in Clinical Enterobacteriaceae Strains in Poland. Antimicrob. Agents Chemother. 2005, 49, 1872–1880. [Google Scholar] [CrossRef] [PubMed]
- Muzaheed, D.Y.; Adams-Haduch, J.M.; Endimiani, A.; Sidjabat, H.E.; Gaddad, S.M.; Paterson, D.L. High Prevalence of CTX-M-15-Producing Klebsiella Pneumoniae among Inpatients and Outpatients with Urinary Tract Infection in Southern India. J. Antimicrob. Chemother. 2008, 61, 1393–1394. [Google Scholar] [CrossRef] [PubMed]
- Tollentino, F.M.; Polotto, M.; Nogueira, M.L.; Lincopan, N.; Neves, P.; Mamizuka, E.M.; Remeli, G.A.; De Almeida, M.T.G.; Rúbio, F.G.; Nogueira, M.C.L. High Prevalence of BlaCTX-M Extended Spectrum Beta-Lactamase Genes in Klebsiella Pneumoniae Isolates from a Tertiary Care Hospital: First Report of BlaSHV-12, BlaSHV-31, BlaSHV-38, and BlaCTX-M-15 in Brazil. Microb. Drug Resist. 2011, 17, 7–16. [Google Scholar] [CrossRef] [PubMed]
- Dropa, M.; Balsalobre, L.C.; Lincopan, N.; Matté, G.R.; Matté, M.H. Complex Class 1 Integrons Harboring CTX-M-2-Encoding Genes in Clinical Enterobacteriaceae from a Hospital in Brazil. J. Infect. Dev. Ctries. 2015, 9, 890–897. [Google Scholar] [CrossRef] [PubMed]
- Pasternak, J. New Methods of Microbiological Identification Using MALDI-TOF. Einstein 2012, 10, 118–119. [Google Scholar] [CrossRef] [PubMed]
- Ramadan, A.A.; Abdelaziz, N.A.; Amin, M.A.; Aziz, R.K. Novel BlaCTX-M Variants and Genotype-Phenotype Correlations among Clinical Isolates of Extended Spectrum Beta Lactamase-Producing Escherichia coli. Sci. Rep. 2019, 9, 1–12. [Google Scholar] [CrossRef] [PubMed]
- da Silva, K.C.; Lincopan, N. Epidemiologia Das Betalactamases de Espectro Estendido No Brasil: Impacto Clínico e Implicações Para o Agronegócio. J. Bras. Patol. Med. Lab. 2012, 48, 91–99. [Google Scholar] [CrossRef]
- D’Andrea, M.M.; Arena, F.; Pallecchi, L.; Rossolini, G.M. CTX-M-Type β-Lactamases: A Successful Story of Antibiotic Resistance. Int. J. Med. Microbiol. 2013, 303, 305–317. [Google Scholar] [CrossRef]
- Dalmarco, E.M.; Blatt, S.L.; de Córdova, C.M.M. Identificação Laboratorial de β-Lactamases De\r\nEspectro Estendido (ESBLs)—Revisão. Rbac 2006, 38, 171–177. [Google Scholar]
- De Oliveira, P.A.; Moura, R.A.; Rodrigues, G.V.; Lopes, K.F.C.; Zaniolo, M.M.; Rubio, K.A.J.; Dias, E.H.; De Oliveira, L.A.; Chideroli, R.T.; Gonçalves, D.D. Detection of Extended Spectrum Beta-Lactamases and Resistance in Members of the Enterobacteriaceae Family Isolated from Healthy Sheep and Dogs in Umuarama, Paraná, Brazil. Semin. Agrar. 2016, 37, 829–840. [Google Scholar] [CrossRef][Green Version]
- Pissetti, C.; Werlang, G.O.; Kich, J.D.; Cardoso, M. Genotyping and Antimicrobial Resistance in Escherichia coli from Pig Carcasses. Pesqui. Vet. Bras. 2017, 37, 1253–1260. [Google Scholar] [CrossRef]
- Hoepers, P.G.; Silva, P.L.; Rossi, D.A.; Valadares Júnior, E.C.; Ferreira, B.C.; Zuffo, J.P.; Koerich, P.K.; Fonseca, B.B. The Association between Extended Spectrum Beta-Lactamase (ESBL) and Ampicillin C (AmpC) Beta-Lactamase Genes with Multidrug Resistance in Escherichia coli Isolates Recovered from Turkeys in Brazil. Br. Poult. Sci. 2018, 59, 396–401. [Google Scholar] [CrossRef] [PubMed]
- Mezalira, T.S.; Gonçalves, D.D.; Dias, E.H.; da Silva, F.M.; dos Santos, I.C.; Gerônimo, E.; Dias, J.C.P.; Otutumi, L.K. Extended-Spectrum β-Lactamase (ESBL)-Producing Enterobacteria Isolated from Broiler Breeder Chickens. Biotemas 2019, 32, 1–10. [Google Scholar] [CrossRef]
- Brisola, M.C.; Crecencio, R.B.; Bitner, D.S.; Frigo, A.; Rampazzo, L.; Stefani, L.M.; Faria, G.A. Escherichia coli Used as a Biomarker of Antimicrobial Resistance in Pig Farms of Southern Brazil. Sci. Total Environ. 2019, 647, 362–368. [Google Scholar] [CrossRef] [PubMed]
- de Paiva Anciens Ramos Ramos, G.L.; dos Santos Nascimento, J. Characterization of Acinetobacter spp. from Raw Goat Milk. Cienc. Rural 2019, 49, 8–11. [Google Scholar] [CrossRef]
- de Souza Gazal, L.E.; Medeiros, L.P.; Dibo, M.; Nishio, E.K.; Koga, V.L.; Gonçalves, B.C.; Grassotti, T.T.; de Camargo, T.C.L.; Pinheiro, J.J.; Vespero, E.C.; et al. Detection of ESBL/AmpC-Producing and Fosfomycin-Resistant Escherichia coli From Different Sources in Poultry Production in Southern Brazil. Front. Microbiol. 2021, 11, 604544. [Google Scholar] [CrossRef] [PubMed]
- Ewbank, A.C.; Esperón, F.; Sacristán, C.; Sacristán, I.; Neves, E.; Costa-Silva, S.; Antonelli, M.; Rocha Lorenço, J.; Kolesnikovas, C.K.M.; Catão-Dias, J.L. Occurrence and Quantification of Antimicrobial Resistance Genes in the Gastrointestinal Microbiome of Two Wild Seabird Species with Contrasting Behaviors. Front. Vet. Sci. 2021, 8, 651781. [Google Scholar] [CrossRef]
- da Silva, C.R. Resistência Antimicrobiana De Enterobactérias De Aves Migratórias No Litoral Paraibano; Universidade Federal da Paraíba: João Pessoa, Brazil, 2019. [Google Scholar]
- Ewbank, A.C.; Esperón, F.; Sacristán, C.; Sacristán, I.; Krul, R.; Macedo Cavalcanti, E.; Calatayud, O.; Bueno, I.; de Francisco Strefezzi, R.; Catão-Dias, J.L. Seabirds as Anthropization Indicators in Two Different Tropical Biotopes: A One Health Approach to the Issue of Antimicrobial Resistance Genes Pollution in Oceanic Islands. Sci. Total Environ. 2021, 754, 142141. [Google Scholar] [CrossRef]
- Davies, Y.M.; Cunha, M.P.V.; Oliveira, M.G.X.; Oliveira, M.C.V.; Philadelpho, N.; Romero, D.C.; Milanelo, L.; Guimarães, M.B.; Ferreira, A.J.P.; Moreno, A.M.; et al. Virulence and Antimicrobial Resistance of Klebsiella Pneumoniae Isolated from Passerine and Psittacine Birds. Avian Pathol. 2016, 45, 194–201. [Google Scholar] [CrossRef] [PubMed]
- Walther-Rasmussen, J.; Høiby, N. Cefotaximases (CTX-M-Ases), an Expanding Family of Extended-Spectrum β-Lactamases. Can. J. Microbiol. 2004, 50, 137–165. [Google Scholar] [CrossRef] [PubMed]
- Rocha, F.R.; Pinto, V.P.T.; Barbosa, F.C.B. The Spread of CTX-M-Type Extended-Spectrum β-Lactamases in Brazil: A Systematic Review. Microb. Drug Resist. 2016, 22, 301–311. [Google Scholar] [CrossRef] [PubMed]
- IBGE. Censo Demográgico. 2010. Available online: https://www.ibge.gov.br/pt/inicio.html (accessed on 12 August 2021).
- Bengtsson-Palme, J.; Kristiansson, E.; Larsson, D.G.J. Environmental Factors Influencing the Development and Spread of Antibiotic Resistance. Fed. Eur. Microbiol. Soc. 2018, 42, 68–80. [Google Scholar] [CrossRef] [PubMed]
- Mattner, F.; Bange, F.; Meyer, E.; Seifert, H.; Wichelhaus, T.A.; Chaberny, I.F. Preventing the Spread of Multidrug- Resistant Gram-Negative Pathogens. Dtsch. Ärzteblatt Int. 2012, 109, 39–45. [Google Scholar] [CrossRef]
- Skarzynska, M.; Leekitcharoenphon, P.; Hendriksen, R.S.; Aarestrup, F.M.; Wasyl, D. A Metagenomic Glimpse into the Gut of Wild and Domestic Animals: Quantification of Antimicrobial Resistance and More. PLoS ONE 2020, 15, e0242987. [Google Scholar] [CrossRef]
- Cardoso, M. Antimicrobial Use, Resistance and Economic Benefits and Costs to Livestock Producers in Brazil. Food Agric. Fish. Pap. 2019, 135, 1–44. [Google Scholar] [CrossRef]
- De Jesus, A.A.B.; Freitas, A.A.R.; De Souza, J.C.; Martins, N.; Botelho, L.A.B.; Girão, V.B.C.; Teixeira, L.M.; Riley, L.W.; Moreira, B.M. High-Level Multidrug-Resistant Escherichia coli Isolates from Wild Birds in a Large Urban Environment. Microb. Drug Resist. 2018, 25, 167–172. [Google Scholar] [CrossRef]
- Ewbank, A.C.; Fuentes-Castillo, D.; Sacristán, C.; Esposito, F.; Fuga, B.; Cardoso, B.; Godoy, S.N.; Zamana, R.R.; Gattamorta, M.A.; Catão-Dias, J.L.; et al. World Health Organization Critical Priority Escherichia coli Clone ST648 in Magnificent Frigatebird (Fregata magnificens) of an Uninhabited Insular Environment. Front. Microbiol. 2022, 13, 940600. [Google Scholar] [CrossRef]
- Gralha, R.E.F. Métodos de Pesquisa de Beta-Lactamases Em Amostras Clínicas—Estudo de Revisão; Universidade Fernando Pessoa: Porto, Portugal, 2011. [Google Scholar]
- Nobre, M.L.M.; Santos, L.S.; Silva, D.R.P.; Oliveira, F.A.A.; Araújo, A.R.; Campos, M.A.S.; Sousa, B.C.; Figueirêdo, A.V.; Muratori, M.C.S.; Soares, M.J.S. Multiresistance and Virulence Factors of Staphylococcus Aureus Isolated from Pigs. Arq. Bras. Medicima Veterinária Zootec. 2021, 73, 343–351. [Google Scholar] [CrossRef]
- Dhanji, H.; Murphy, N.M.; Doumith, M.; Durmus, S.; Lee, S.S.; Hope, R.; Woodford, N.; Livermore, D.M. Cephalosporin Resistance Mechanisms in Escherichia coli Isolated from Raw Chicken Imported into the UK. J. Antimicrob. Chemother. 2010, 65, 2534–2537. [Google Scholar] [CrossRef] [PubMed]
- Abhilash, K.P.P.; Veeraraghavan, B.; Abraham, O.C. Epidemiology and Outcome of Bacteremia Caused by Extended Spectrum Beta-Lactamase (ESBL)-Producing Escherichia coli and Klebsiella Spp. in a Tertiary Care Teaching Hospital in South India. J. Assoc. Physicians India 2010, 58, 13–17. [Google Scholar] [PubMed]
- Lee, C.R.; Cho, I.H.; Jeong, B.C.; Lee, S.H. Strategies to Minimize Antibiotic Resistance. Int. J. Environ. Res. Public Health 2013, 10, 4274–4305. [Google Scholar] [CrossRef]
- Mezhoud, H.; Chantziaras, I.; Iguer-Ouada, M.; Moula, N.; Garmyn, A.; Martel, A.; Touati, A.; Smet, A.; Haesebrouck, F.; Boyen, F. Presence of Antimicrobial Resistance in Coliform Bacteria from Hatching Broiler Eggs with Emphasis on ESBL/AmpC-Producing Bacteria. Avian Pathol. 2016, 45, 493–500. [Google Scholar] [CrossRef] [PubMed]
- Lee, N.Y.; Huang, W.H.; Tsui, K.C.; Hsueh, P.R.; Ko, W.C. Carbapenem Therapy for Bacteremia Due to Extended-Spectrum β-Lactamase-Producing Escherichia coli or Klebsiella Pneumoniae. Diagn. Microbiol. Infect. Dis. 2011, 70, 150–153. [Google Scholar] [CrossRef] [PubMed]
- Bryan, A.; Shapir, N.; Sadowsky, M.J. Frequency and Distribution of Tetracycline Resistance Genes in Genetically Diverse, Nonselected, and Nonclinical Escherichia coli Strains Isolated from Diverse Human and Animal Sources. Appl. Environ. Microbiol. 2004, 70, 2503–2507. [Google Scholar] [CrossRef]
- Da Costa, M.M.; E Silva, M.S.; Spricigo, D.A.; Witt, N.M.; Marchioro, S.B.; Kolling, L.; De Vargas, A.P.C. Epidemiology, Molecular Characterization and Resistance to Antimicrobials of Escherichia coli Isolated from South-Brazilian Pig Herds. Pesqui. Vet. Bras. 2006, 26, 5–8. [Google Scholar] [CrossRef][Green Version]


| Classes | Antibiotics | Abbreviation | Concentration |
|---|---|---|---|
| β-lactam + β-lactamase Inhibitor Combination | Amoxicillin + clavulanic acid | AMC | 30 μg |
| Cephems | Ceftriaxone | CRO | 30 μg |
| Cefotaxime | CTX | 30 μg | |
| Ceftiofur | CTF | 30 μg | |
| Cefepime | CPM | 30 μg | |
| Monobactams | Aztreonam | ATM | 30 μg |
| Carbapenems | Ertapenem | ETP | 10 μg |
| Imipenem | IPM | 10 μg | |
| Meropenem | MER | 10 μg | |
| Fluoroquinolones | Enrofloxacin | ENO | 5 μg |
| Ciprofloxacin | CIP | 5 μg | |
| Sulfonamides | Sulfamethoxazole/ trimethoprim | SUT | 25 μg |
| Aminoglycosides | Gentamicin | GEN | 10 μg |
| Amikacin | AMI | 30 μg | |
| Tetracyclines | Tetracycline | TET | 30 μg |
| Glycylcycline | Tigecycline | TIG | 15 μg |
| Municipalities | Animal Group | n° of Samples | Positive Samples (n) | Resistance Genes | Prevalence/ Municipality (%) | Confidence Interval (95%) |
|---|---|---|---|---|---|---|
| Água Branca | Wild birds | 17 | 1 | blaSHV-1 | 5.88 | 0–17.07 |
| Domestic birds | 13 | 1 | blaCTX-M | 7.69 | 0–22.18 | |
| Equine | 18 | 0 | - | 0 | 0 | |
| Swine | 16 | 2 | blaCTX-M (1) Not identified (1) | 12.5 | 0–28.71 | |
| Ruminants | 15 | 1 | blaCTX-M-15 | 6.67 | 0–19.29 | |
| Total | 79 | 5 | - | 6.33 | 0.96–11.70 | |
| Amarante | Wild birds | 18 | 0 | - | 0 | 0 |
| Domestic birds | 12 | 3 | blaCTX-M (3) | 25.0 | 0.50–49.50 | |
| Equine | 16 | 0 | - | 0 | 0 | |
| Swine | 16 | 2 | blaCTX-M (2) | 12.5 | 0–28.71 | |
| Ruminants | 23 | 0 | - | 0 | 0 | |
| Total | 85 | 5 | - | 5.88 | 0.88–10.88 | |
| Lagoa Alegre | Wild birds | 15 | 0 | - | 0 | 0 |
| Domestic birds | 15 | 1 | blaCTX-M-8 | 6.67 | 0–19.29 | |
| Equine | 15 | 1 | blaCTX-M | 6.67 | 0–19.29 | |
| Swine | 15 | 1 | blaCTX-M | 6.67 | 0–19.29 | |
| Ruminants | 15 | 2 | blaCTX-M (2) | 13.33 | 0–30.54 | |
| Total | 75 | 5 | - | 6.67 | 1.02–12.31 | |
| Parnaíba | Wild birds | 14 | 2 | blaCTX-M (2) | 14.29 | 0–32.62 |
| Domestic birds | 12 | 4 | blaCTX-M (2) | 33.33 | 6.66–60.01 | |
| Equine | 15 | 0 | - | 0 | 0 | |
| Swine | 14 | 11 | blaCTX-M (9) blaCTX-M-15 (2) | 78.57 | 57.08–100 | |
| Ruminants | 15 | 2 | blaCTX-M (1) blaCTX-M-15 (1) | 13.33 | 0–30.54 | |
| Total | 70 | 19 | 27.14 | 16.73–37.56 | ||
| Teresina | Wild birds | 25 | 0 | - | 0 | 0 |
| Domestic birds | 8 | 0 | - | 0 | 0 | |
| Equine | 16 | 0 | - | 0 | 0 | |
| Swine | 15 | 14 | blaCTX-M (12) blaCTX-M-8 (1) blaTEM-1 (1) | 93.33 | 80.71–100 | |
| Ruminants | 14 | 11 | blaCTX-M (7) blaCTX-M-8 (2) blaCTX-M-15 (1) Not identified (1) | 78.57 | 57.08–100 | |
| Total | 78 | 25 | - | 32.05 | 21.69–42.41 | |
| All municipalities | Total | 387 | 59 | - | 15.25 | 11.66–18.83 |
| ESBL Positive | ESBL Negative | IC 95% | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | Total | Analyze | OR | Lower | Higher | p Value | ||
| Sex | Male | 14 | 10.8 | 116 | 89.2 | 130 | univariate | 0.44 | 0.23 | 0.84 | 0.001 |
| Female | 41 | 21.6 | 149 | 78.4 | 190 | Ref | |||||
| No Information | 4 | 6.0 | 63 | 94.0 | 67 | - | |||||
| Age Group | Cub | 2 | 6.9 | 27 | 93.1 | 29 | univariate | 0.46 | 0.11 | 2.02 | 0.306 |
| Young | 17 | 30.4 | 39 | 69.6 | 56 | 2.72 | 1.41 | 5.27 | 0.003 | ||
| Adult | 40 | 13.8 | 250 | 86.2 | 290 | Ref | |||||
| Geriatric | 0 | 0.0 | 3 | 100.0 | 3 | 0 | 0 | Inf | 0.987 | ||
| No Information | 0 | 0.0 | 9 | 100.0 | 9 | - | |||||
| Municipality | Água Branca | 5 | 6.3 | 74 | 93.7 | 79 | multivariate | 1.11 | 0.29 | 4.24 | 0.874 |
| Amarante | 5 | 5.9 | 80 | 94.1 | 85 | Ref | |||||
| Lagoa Alegre | 5 | 6.7 | 70 | 93.3 | 75 | 1.15 | 0.30 | 4.36 | 0.842 | ||
| Parnaíba | 19 | 27.1 | 51 | 72.9 | 70 | 8.58 | 2.75 | 26.80 | <0.001 | ||
| Teresina | 25 | 32.1 | 53 | 67.9 | 78 | 16.06 | 5.07 | 50.85 | <0.001 | ||
| Animal Group | Wild Birds | 3 | 3.4 | 86 | 96.6 | 89 | multivariate | ref | |||
| Domestic Birds | 9 | 15.0 | 51 | 85.0 | 60 | 8.63 | 2.06 | 36.18 | 0.003 | ||
| Equine | 1 | 1.3 | 79 | 98.8 | 80 | 0.42 | 0.04 | 4.22 | 0.460 | ||
| Ruminants | 16 | 19.5 | 66 | 80.5 | 82 | 11.66 | 3.03 | 44.86 | 0.000 | ||
| Swine | 30 | 39.5 | 46 | 60.5 | 76 | 39.68 | 10.26 | 153.54 | 0.000 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
da Silva, S.K.S.M.; Fuentes-Castillo, D.A.; Ewbank, A.C.; Sacristán, C.; Catão-Dias, J.L.; Sevá, A.P.; Lincopan, N.; Deem, S.L.; Feitosa, L.C.S.; Catenacci, L.S. ESBL-Producing Enterobacterales at the Human–Domestic Animal–Wildlife Interface: A One Health Approach to Antimicrobial Resistance in Piauí, Northeastern Brazil. Vet. Sci. 2024, 11, 195. https://doi.org/10.3390/vetsci11050195
da Silva SKSM, Fuentes-Castillo DA, Ewbank AC, Sacristán C, Catão-Dias JL, Sevá AP, Lincopan N, Deem SL, Feitosa LCS, Catenacci LS. ESBL-Producing Enterobacterales at the Human–Domestic Animal–Wildlife Interface: A One Health Approach to Antimicrobial Resistance in Piauí, Northeastern Brazil. Veterinary Sciences. 2024; 11(5):195. https://doi.org/10.3390/vetsci11050195
Chicago/Turabian Styleda Silva, Sandy Kelly S. M., Danny A. Fuentes-Castillo, Ana Carolina Ewbank, Carlos Sacristán, José L. Catão-Dias, Anaiá P. Sevá, Nilton Lincopan, Sharon L. Deem, Lauro C. S. Feitosa, and Lilian S. Catenacci. 2024. "ESBL-Producing Enterobacterales at the Human–Domestic Animal–Wildlife Interface: A One Health Approach to Antimicrobial Resistance in Piauí, Northeastern Brazil" Veterinary Sciences 11, no. 5: 195. https://doi.org/10.3390/vetsci11050195
APA Styleda Silva, S. K. S. M., Fuentes-Castillo, D. A., Ewbank, A. C., Sacristán, C., Catão-Dias, J. L., Sevá, A. P., Lincopan, N., Deem, S. L., Feitosa, L. C. S., & Catenacci, L. S. (2024). ESBL-Producing Enterobacterales at the Human–Domestic Animal–Wildlife Interface: A One Health Approach to Antimicrobial Resistance in Piauí, Northeastern Brazil. Veterinary Sciences, 11(5), 195. https://doi.org/10.3390/vetsci11050195









