Edge-Driven Disability Detection and Outcome Measurement in IoMT Healthcare for Assistive Technology
Abstract
1. Introduction
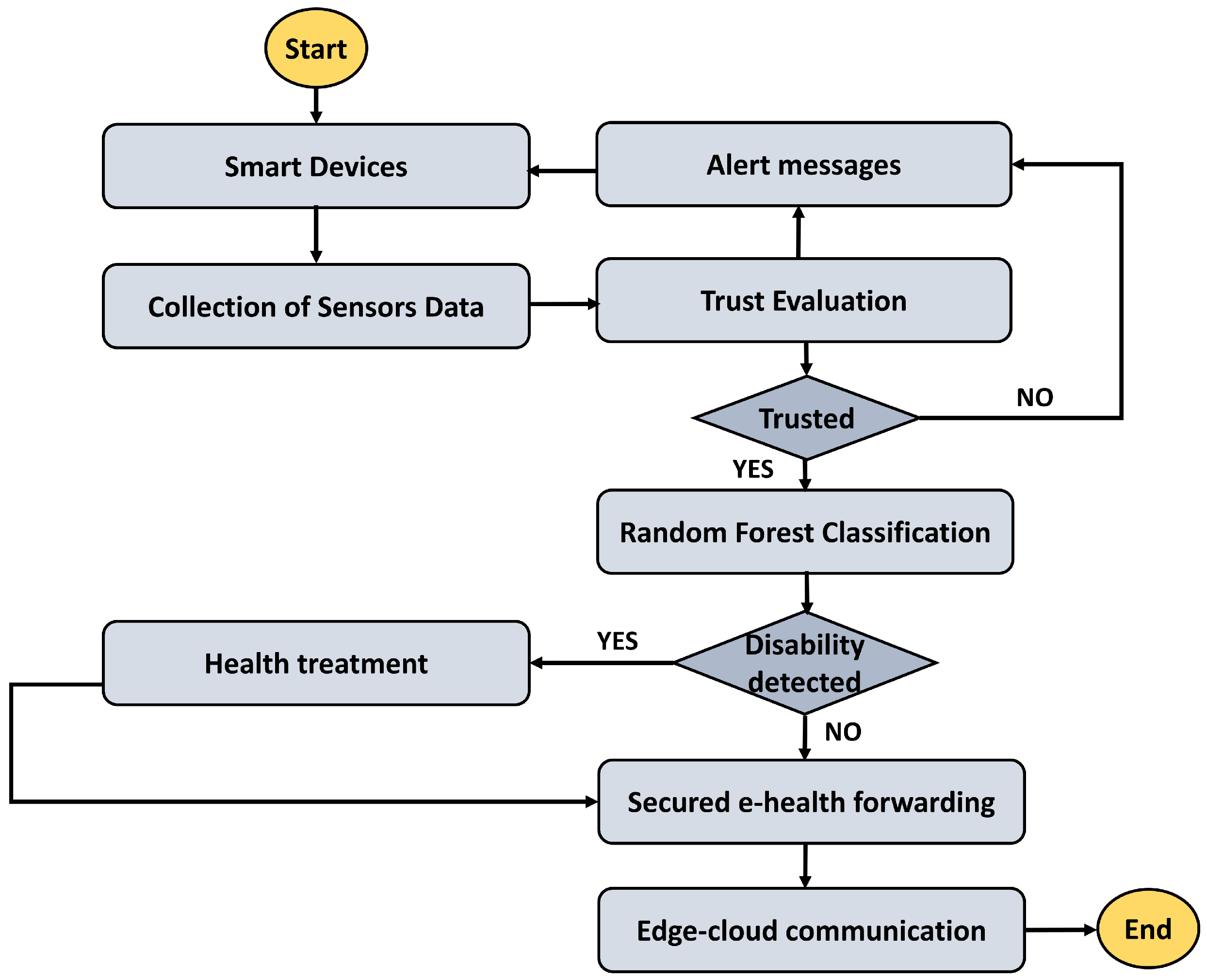
Contributions
- It integrates wearable IoMT sensors with edge computing to develop a timely algorithm for disability detection. By combining motion data and sEMG signals, the Random Forest classifier extracts key features to distinguish between normal and abnormal movement patterns, enhancing the real-time diagnostic capabilities of assistive healthcare systems.
- Trust integration is employed to ensure the reliability of data from IoMT devices, thereby improving the accuracy of disability detection and disease classification. This approach reduces false positives and enhances decision-making strategies by filtering out unreliable data, ensuring that healthcare systems can provide trustworthy assessments for individuals with disabilities.
- The use of edge computing for preprocessing data minimizes computational overhead on IoMT devices, enabling an energy-efficient and low-latency communication system. This optimization is crucial for real-time healthcare applications, particularly in systems designed to monitor and assist individuals with disabilities.
2. Related Work
Problem Formulation
3. Materials and Methods
| Algorithm 1: Edge-Based Data Preprocessing with Trust-Driven Evaluation |
 |
| Algorithm 2: Random Forest-Based Multiple Features-Enabled Disability Detection |
 |
4. Simulation Environment
Results Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- El-Saleh, A.A.; Sheikh, A.M.; Albreem, M.A.; Honnurvali, M.S. The internet of medical things (IoMT): Opportunities and challenges. Wirel. Netw. 2025, 31, 327–344. [Google Scholar] [CrossRef]
- Osama, M.; Ateya, A.A.; Sayed, M.S.; Hammad, M.; Pławiak, P.; Abd El-Latif, A.A.; Elsayed, R.A. Internet of medical things and healthcare 4.0: Trends, requirements, challenges, and research directions. Sensors 2023, 23, 7435. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Amin, O.; Shihada, B. Intelligent wearable systems: Opportunities and challenges in health and sports. ACM Comput. Surv. 2024, 56, 1–42. [Google Scholar] [CrossRef]
- Yuan, Y.; Liu, B.; Li, H.; Li, M.; Song, Y.; Wang, R.; Wang, T.; Zhang, H. Flexible wearable sensors in medical monitoring. Biosensors 2022, 12, 1069. [Google Scholar] [CrossRef]
- Anikwe, C.V.; Nweke, H.F.; Ikegwu, A.C.; Egwuonwu, C.A.; Onu, F.U.; Alo, U.R.; Teh, Y.W. Mobile and wearable sensors for data-driven health monitoring system: State-of-the-art and future prospect. Expert Syst. Appl. 2022, 202, 117362. [Google Scholar] [CrossRef]
- Cicirelli, G.; Impedovo, D.; Dentamaro, V.; Marani, R.; Pirlo, G.; D’Orazio, T.R. Human gait analysis in neurodegenerative diseases: A review. IEEE J. Biomed. Health Inform. 2021, 26, 229–242. [Google Scholar] [CrossRef]
- Buyya, R.; Ilager, S.; Arroba, P. Energy-efficiency and sustainability in new generation cloud computing: A vision and directions for integrated management of data centre resources and workloads. Softw. Pract. Exp. 2024, 54, 24–38. [Google Scholar] [CrossRef]
- Abughazalah, M.; Alsaggaf, W.; Saifuddin, S.; Sarhan, S. Centralized vs. Decentralized Cloud Computing in Healthcare. Appl. Sci. 2024, 14, 7765. [Google Scholar] [CrossRef]
- Shukla, S.; Hassan, M.F.; Tran, D.C.; Akbar, R.; Paputungan, I.V.; Khan, M.K. Improving latency in Internet-of-Things and cloud computing for real-time data transmission: A systematic literature review (SLR). Clust. Comput. 2023, 26, 2657–2680. [Google Scholar] [CrossRef]
- Shahzad, A.; Chen, W.; Shaheen, M.; Zhang, Y.; Ahmad, F. A robust algorithm for authenticated health data access via blockchain and cloud computing. PLoS ONE 2024, 19, e0307039. [Google Scholar] [CrossRef] [PubMed]
- Aminizadeh, S.; Heidari, A.; Dehghan, M.; Toumaj, S.; Rezaei, M.; Navimipour, N.J.; Stroppa, F.; Unal, M. Opportunities and challenges of artificial intelligence and distributed systems to improve the quality of healthcare service. Artif. Intell. Med. 2024, 149, 102779. [Google Scholar] [CrossRef]
- Dhinakaran, D.; Ramani, R.; Edwin Raja, S.; Selvaraj, D. Enhancing security in electronic health records using an adaptive feature-centric polynomial data security model with blockchain integration. Peer-to-Peer Netw. Appl. 2025, 18, 7. [Google Scholar] [CrossRef]
- Adam, M.; Hammoudeh, M.; Alrawashdeh, R.; Alsulaimy, B. A survey on security, privacy, trust, and architectural challenges in IoT systems. IEEE Access 2024, 12, 57128–57149. [Google Scholar] [CrossRef]
- Jaime, F.J.; Muñoz, A.; Rodríguez-Gómez, F.; Jerez-Calero, A. Strengthening privacy and data security in biomedical microelectromechanical systems by IoT communication security and protection in smart healthcare. Sensors 2023, 23, 8944. [Google Scholar] [CrossRef]
- Martínez, A.L.; Pérez, M.G.; Ruiz-Martínez, A. A comprehensive model for securing sensitive patient data in a clinical scenario. IEEE Access 2023, 11, 137083–137098. [Google Scholar] [CrossRef]
- Neto, E.C.P.; Dadkhah, S.; Sadeghi, S.; Molyneaux, H.; Ghorbani, A.A. A review of Machine Learning (ML)-based IoT security in healthcare: A dataset perspective. Comput. Commun. 2024, 213, 61–77. [Google Scholar] [CrossRef]
- Arunprasath, S.; Annamalai, S. Improving patient centric data retrieval and cyber security in healthcare: Privacy preserving solutions for a secure future. Multimed. Tools Appl. 2024, 83, 70289–70319. [Google Scholar] [CrossRef]
- Almalawi, A.; Khan, A.I.; Alsolami, F.; Abushark, Y.B.; Alfakeeh, A.S. Managing security of healthcare data for a modern healthcare system. Sensors 2023, 23, 3612. [Google Scholar] [CrossRef]
- AlZubi, A.A.; Al-Maitah, M.; Alarifi, A. Cyber-attack detection in healthcare using cyber-physical system and machine learning techniques. Soft Comput. 2021, 25, 12319–12332. [Google Scholar] [CrossRef]
- Palimkar, P.; Shaw, R.N.; Ghosh, A. Machine learning technique to prognosis diabetes disease: Random forest classifier approach. In Advanced Computing and Intelligent Technologies: Proceedings of ICACIT 2021; Springer: Singapore, 2021; pp. 219–244. [Google Scholar]
- Hartmann, M.; Hashmi, U.S.; Imran, A. Edge computing in smart health care systems: Review, challenges, and research directions. Trans. Emerg. Telecommun. Technol. 2022, 33, e3710. [Google Scholar] [CrossRef]
- Ray, P.P.; Dash, D.; De, D. Edge computing for Internet of Things: A survey, e-healthcare case study and future direction. J. Netw. Comput. Appl. 2019, 140, 1–22. [Google Scholar] [CrossRef]
- Kamruzzaman, M.M.; Alanazi, S.; Alruwaili, M.; Alrashdi, I.; Alhwaiti, Y.; Alshammari, N. Fuzzy-assisted machine learning framework for the fog-computing system in remote healthcare monitoring. Measurement 2022, 195, 111085. [Google Scholar] [CrossRef]
- Rehman, A.; Saba, T.; Haseeb, K.; Larabi Marie-Sainte, S.; Lloret, J. Energy-efficient IoT e-health using artificial intelligence model with homomorphic secret sharing. Energies 2021, 14, 6414. [Google Scholar] [CrossRef]
- Nawaz Tareen, F.; Alvi, A.N.; Alsamani, B.; Alkhathami, M.; Alsadie, D.; Alosaimi, N. EOTE-FSC: An efficient offloaded task execution for fog enabled smart cities. PLoS ONE 2024, 19, e0298363. [Google Scholar] [CrossRef]
- Jacobs, M.; He, J.; F. Pradier, M.; Lam, B.; Ahn, A.C.; McCoy, T.H.; Perlis, R.H.; Doshi-Velez, F.; Gajos, K.Z. Designing AI for trust and collaboration in time-constrained medical decisions: A sociotechnical lens. In Proceedings of the 2021 CHI Conference on Human Factors in Computing Systems, Yokohama, Japan, 8–13 May 2021; pp. 1–14. [Google Scholar]
- Versaci, M.; Angiulli, G.; Crucitti, P.; De Carlo, D.; Laganà, F.; Pellicanò, D.; Palumbo, A. A fuzzy similarity-based approach to classify numerically simulated and experimentally detected carbon fiber-reinforced polymer plate defects. Sensors 2022, 22, 4232. [Google Scholar] [CrossRef] [PubMed]
- Manimurugan, S.; Almutairi, S.; Aborokbah, M.M.; Narmatha, C.; Ganesan, S.; Chilamkurti, N.; Alzaheb, R.A.; Almoamari, H. Two-stage classification model for the prediction of heart disease using IoMT and artificial intelligence. Sensors 2022, 22, 476. [Google Scholar] [CrossRef]
- Versaci, M.; Laganà, F.; Manin, L.; Angiulli, G. Soft computing and eddy currents to estimate and classify delaminations in biomedical device CFRP plates. J. Electr. Eng. 2025, 76, 72–79. [Google Scholar] [CrossRef]
- Manickam, P.; Mariappan, S.A.; Murugesan, S.M.; Hansda, S.; Kaushik, A.; Shinde, R.; Thipperudraswamy, S.P. Artificial intelligence (AI) and internet of medical things (IoMT) assisted biomedical systems for intelligent healthcare. Biosensors 2022, 12, 562. [Google Scholar] [CrossRef]
- Menniti, M.; Laganà, F.; Oliva, G.; Bianco, M.; Fiorillo, A.S.; Pullano, S.A. Development of Non-Invasive Ventilator for Homecare and Patient Monitoring System. Electronics 2024, 13, 790. [Google Scholar] [CrossRef]
- Mahmmod, B.M.; Naser, M.A.; Al-Sudani, A.H.S.; Alsabah, M.; Mohammed, H.J.; Alaskar, H.; Almarshad, F.; Hussain, A.; Abdulhussain, S.H. Patient monitoring system based on internet of things: A review and related challenges with open research issues. IEEE Access 2024, 12, 132444–132479. [Google Scholar] [CrossRef]
- Rana, B.; Singh, Y.; Singh, P.K.; Hong, W.C. A Priority Based Energy-Efficient Metaheuristic Routing Approach for Smart Healthcare System (SHS). IEEE Access 2024, 12, 85694–85708. [Google Scholar] [CrossRef]
- Lakshmanan, R.; Balakrishnan, S.; Mahendran, A.; Subramanian, A.K. Multimodal healthcare data classification with Tangent Namib Beetle Optimization based routing in blockchain based IoT. Comput. Electr. Eng. 2024, 120, 109614. [Google Scholar] [CrossRef]
- Balakrishnan, D.; Rajkumar, T.D.; Dhanasekaran, S.; Murugan, B.S. Secure and energy-efficient data transmission framework for IoT-based healthcare applications using EMCQLR and EKECC. Clust. Comput. 2024, 27, 2999–3016. [Google Scholar] [CrossRef]
- Gupta, S.; Chithaluru, P.; Stephan, T.; Nafisa, S.; Kumar, S. HSPBCI: A robust framework for secure healthcare data management in blockchain-based IoT systems. Multimed. Tools Appl. 2024, 84, 27695–27719. [Google Scholar] [CrossRef]
- Laganà, F.; Pellicanò, D.; Arruzzo, M.; Pratticò, D.; Pullano, S.A.; Fiorillo, A.S. FEM-Based Modelling and AI-Enhanced Monitoring System for Upper Limb Rehabilitation. Electronics 2025, 14, 2268. [Google Scholar] [CrossRef]
- Kore, A.; Patil, S. Cross layered cryptography based secure routing for IoT-enabled smart healthcare system. Wirel. Netw. 2022, 28, 287–301. [Google Scholar] [CrossRef]
- Anguita, D.; Ghio, A.; Oneto, L.; Parra, X.; Reyes-Ortiz, J.L. A public domain dataset for human activity recognition using smartphones. In Proceedings of the 21st European Symposium on Artificial Neural Networks, Computational Intelligence and Machine Learning, ESANN, Bruges, Belgium, 24–26 April 2013; Volume 3, pp. 3–4. [Google Scholar]



| Existing Approaches | Contribution | Limitation | Significance of TRDD-SRF Model |
|---|---|---|---|
| Wearable IoMT Devices with Edge Computing [21,22] | Integration of wearable IoMT devices with edge computing for healthcare monitoring. | Limited focus on real-time disease detection and data trustworthiness. | Provides real-time disability detection by integrating IoMT sensors with a trust-based framework, improving both accuracy and security of the system. |
| Fault Detection in Biomedical Devices [27,28] | Non-invasive techniques for detecting defects in biomedical devices using edge-based anomaly detection. | Does not incorporate lightweight AI models in real-time patient monitoring. | Combines edge computing with Random Forest for real-time disability detection in healthcare, bridging the gap between structural fault detection and patient health monitoring. |
| Home Care Devices [31,32] | Development of home care devices with IoMT sensors for continuous health monitoring in non-clinical environments. | The focus is on sensor integration, with trustworthiness and real-time disease detection being overlooked. | Improves the system with trust-aware IoMT sensors, ensuring secure and reliable real-time feedback for home-based healthcare. |
| Optimization Techniques for IoT Healthcare Systems [33,34] | ACO-based routing for energy-efficient IoT healthcare systems. | Does not address privacy concerns or integrate AI classification for disease detection. | Enhances energy efficiency and privacy while integrating AI-based classification for disability detection, addressing privacy and trust issues. |
| Hybrid Modeling Approaches for Healthcare Applications [33,37] | Hybrid FEM-AI model for upper limb rehabilitation with real-time feedback. | Focused on rehabilitation, not disability detection in real-time healthcare systems. | Integrates real-time disability detection and edge computing, making it applicable to rehabilitation and home monitoring in healthcare settings. |
| Features | Description | Computing Contributions |
|---|---|---|
| Data Input | Raw sensor data from IoMT devices | Edge-based data collection for preprocessing |
| Preprocessing Techniques | Noise filtering, normalization, segmentation | Data processed at the edge to reduce latency |
| Feature Extraction Methods | Acceleration, angular velocity, postural angle | Real-time processing to minimize transmission |
| Trust Score Computation | Accuracy and freshness weighted sum | Security via trust evaluation for data integrity |
| Classification Method | Random Forest classifier | Edge-based classification reduces response time |
| Trusted Metrics | Normal/Abnormal detection | Trust-driven evaluation for accurate classification |
| Key Features of the Model | Edge preprocessing, trust evaluation, real-time detection | Efficient edge computing for reliable monitoring |
| Performance Metrics | Trust score, accuracy, precision, recall, F1-score | Metrics computed at edge to conserve bandwidth |
| Security Features | Trust score, malicious activity detection, thresholding | Trust-based evaluation of data and devices |
| Edge Device Utilization | Edge-level data processing | Lightweight edge solutions with enhanced security |
| Security Aspect | Description | Impact on Healthcare System |
|---|---|---|
| Data Integrity | Ensures accurate data through noise filtering and preprocessing (). | Protects against corrupted data, ensuring reliable health monitoring. |
| Confidentiality | Trust score computation filters unreliable data (). | Safeguards patient privacy by excluding low-trust data (). |
| Authentication | Edge devices verify data authenticity before processing (). | Prevents unauthorized data or device manipulation, ensuring secure access. |
| Data Freshness | Trust score includes data freshness for timely health information (). | Ensures up-to-date data () is used for timely decisions. |
| Access Control | Low-trust data are excluded based on trust score thresholds (). | Limits classification to trusted data (), reducing false diagnoses. |
| Malicious Activity Detection | Detects discrepancies in data quality during trust evaluation (). | Mitigates risks from data manipulation or faulty sensors. |
| Data Transmission Security | Edge-based processing reduces data transmission (). | Minimizes exposure to breaches by reducing transmitted data volume. |
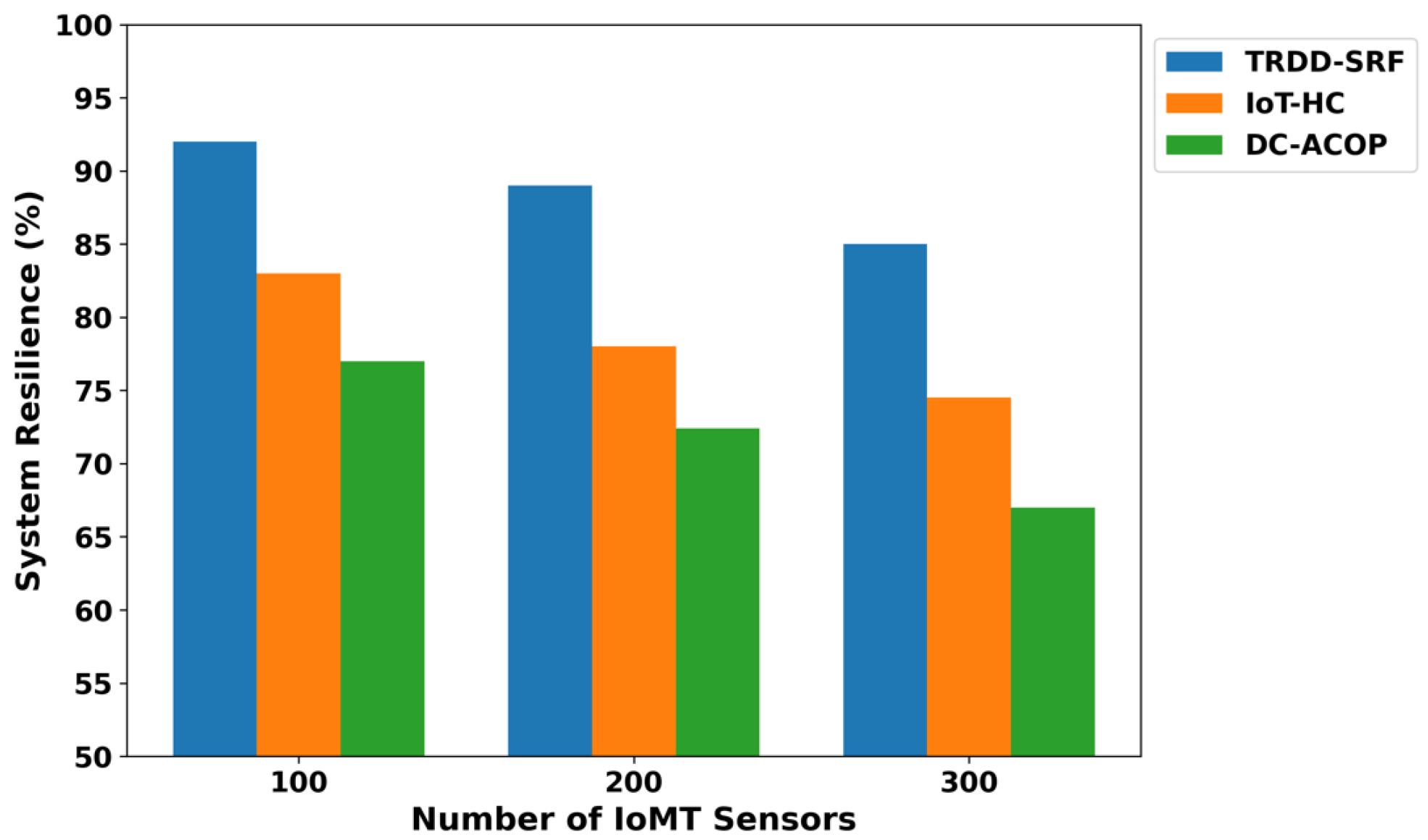
| System Resilience | Edge classification reduces reliance on cloud infrastructure (). | Ensures continuous monitoring, even during network failures (). |
| Parameter | Value |
|---|---|
| Simulation Area | 1000 m × 1000 m |
| Number of Sensors | 100 to 300 |
| Initial Energy per Node | 5J |
| Simulation Run | 70 |
| Edge Devices | 15 |
| Malicious Devices | 10 to 20 |
| Packet Size | 1024 bytes |
| Analyzing Scenarios | varying health devices |
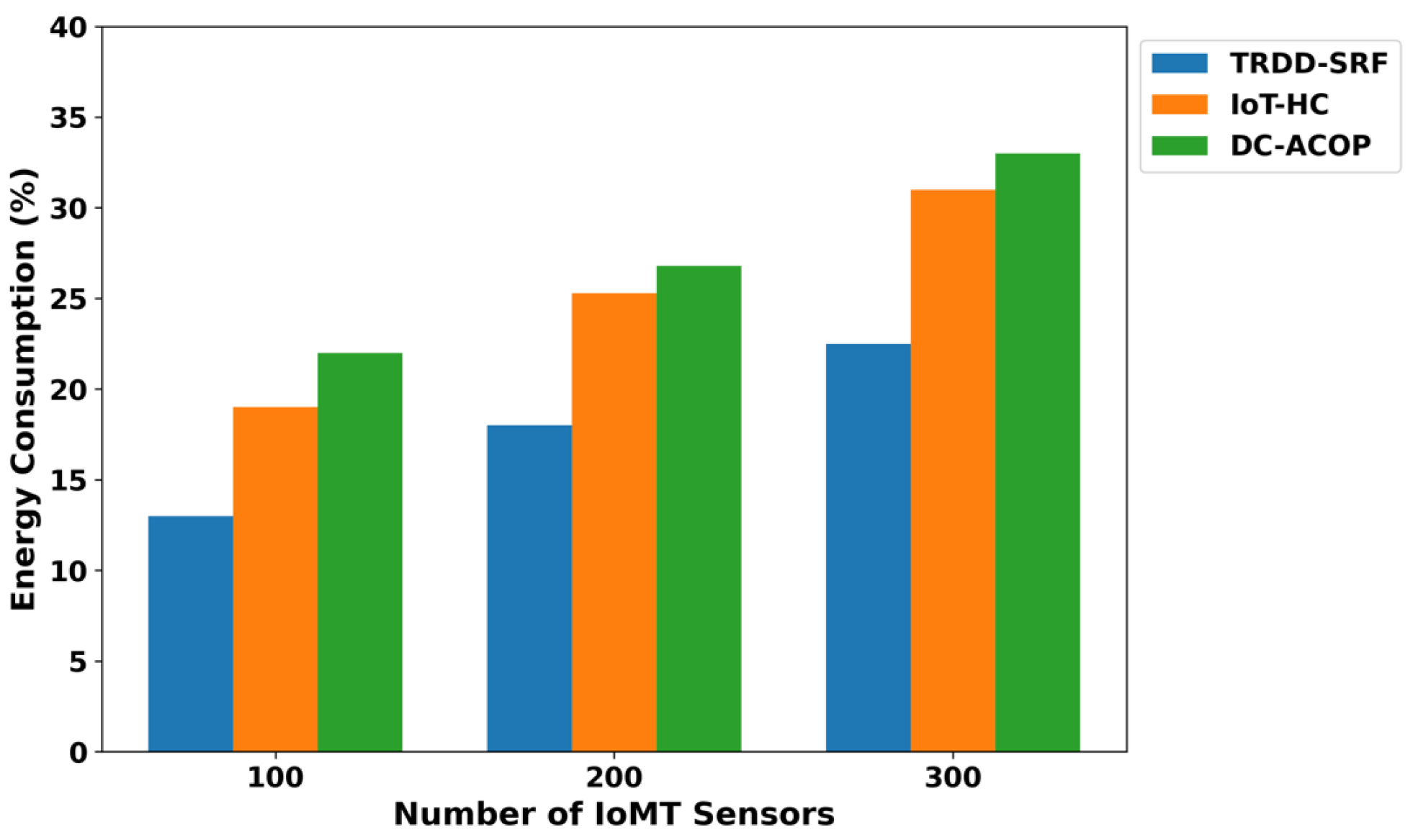
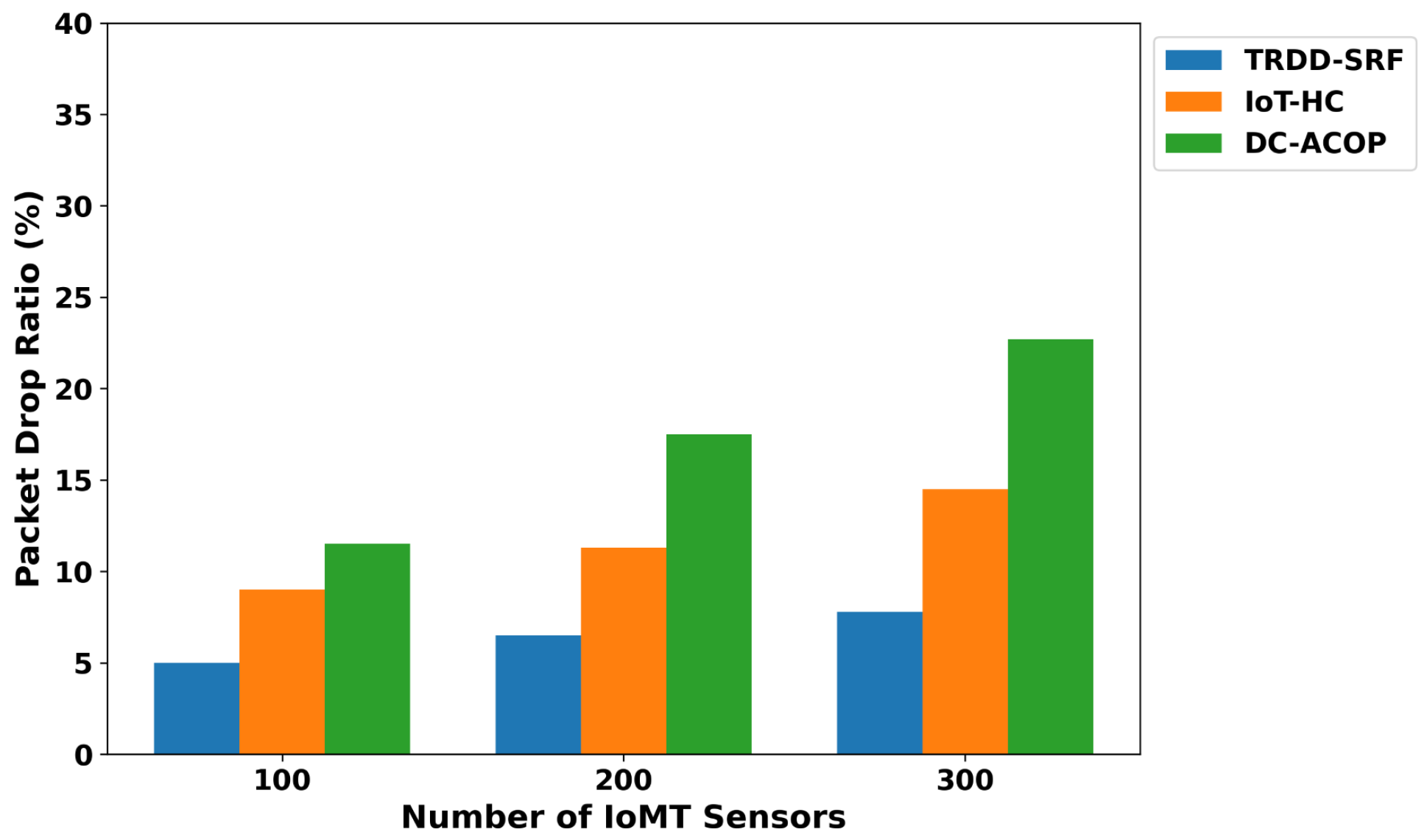
| Performance metrics | energy consumption, packet drop ratio, and system resilience |
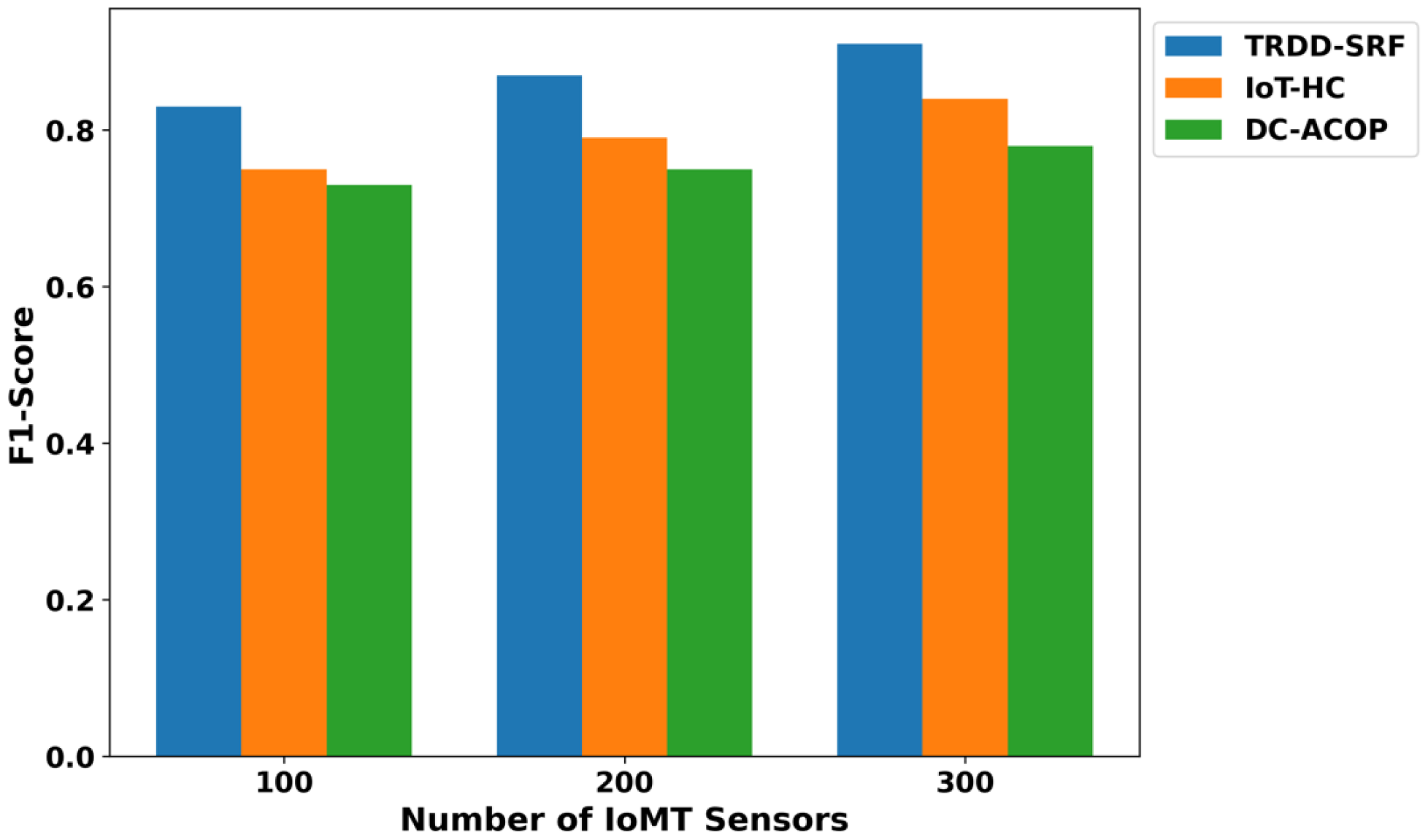
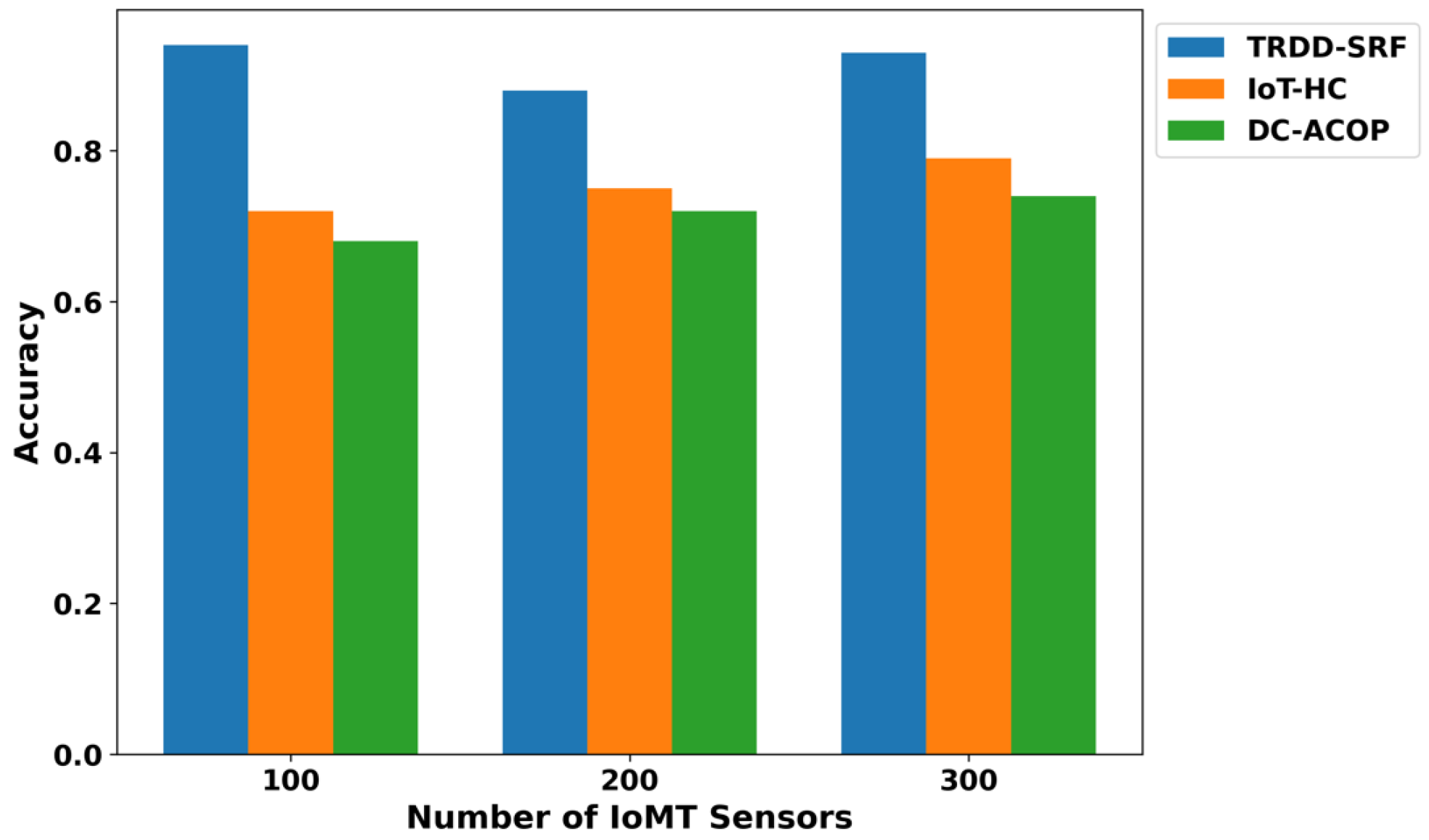
| Classification metrics | accuracy, precision, recall, and F1-score |
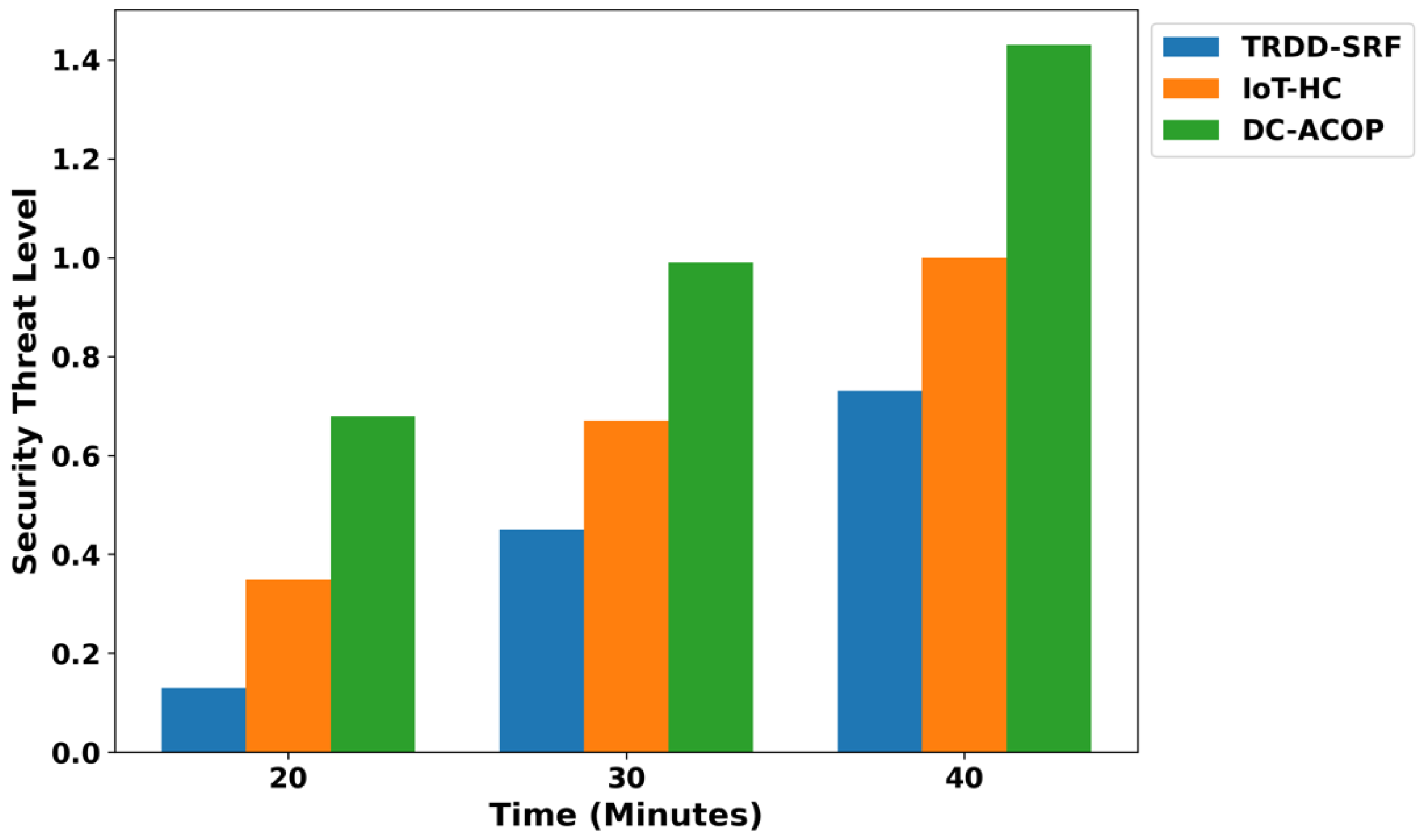
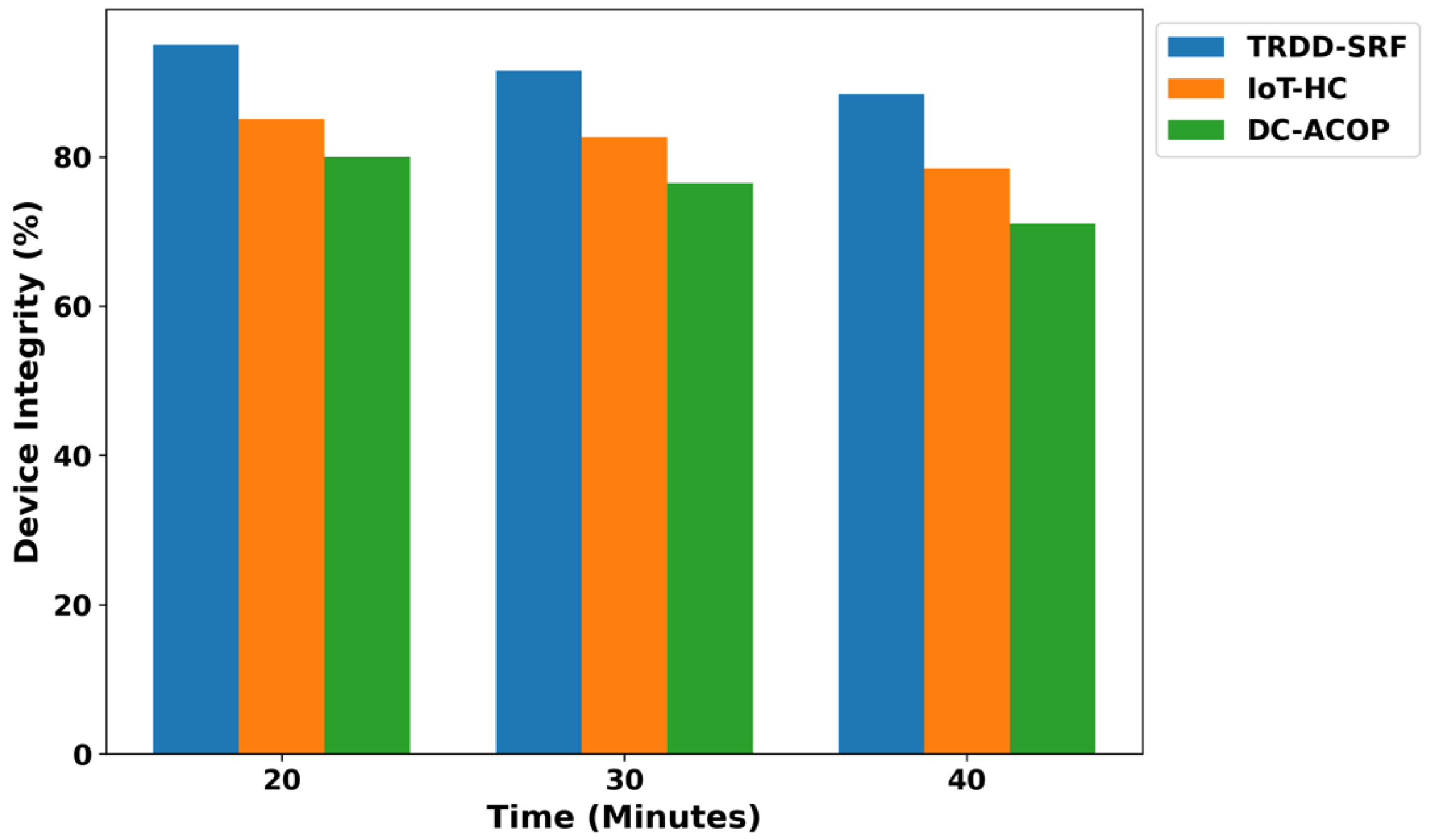
| Security analysis | threat level, malicious activity, and device integrity |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alamri, M.; Haseeb, K.; Humayun, M.; Alshammeri, M.; Alwakid, G.N.; Ramzan, N. Edge-Driven Disability Detection and Outcome Measurement in IoMT Healthcare for Assistive Technology. Bioengineering 2025, 12, 1013. https://doi.org/10.3390/bioengineering12101013
Alamri M, Haseeb K, Humayun M, Alshammeri M, Alwakid GN, Ramzan N. Edge-Driven Disability Detection and Outcome Measurement in IoMT Healthcare for Assistive Technology. Bioengineering. 2025; 12(10):1013. https://doi.org/10.3390/bioengineering12101013
Chicago/Turabian StyleAlamri, Malak, Khalid Haseeb, Mamoona Humayun, Menwa Alshammeri, Ghadah Naif Alwakid, and Naeem Ramzan. 2025. "Edge-Driven Disability Detection and Outcome Measurement in IoMT Healthcare for Assistive Technology" Bioengineering 12, no. 10: 1013. https://doi.org/10.3390/bioengineering12101013
APA StyleAlamri, M., Haseeb, K., Humayun, M., Alshammeri, M., Alwakid, G. N., & Ramzan, N. (2025). Edge-Driven Disability Detection and Outcome Measurement in IoMT Healthcare for Assistive Technology. Bioengineering, 12(10), 1013. https://doi.org/10.3390/bioengineering12101013









