Echocardiographic Strain Evaluation Shows Persistent Echocardiographic Changes at 1 Year after Diagnosis of Multisystem Inflammatory Syndrome in Children
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Echocardiography
2.3. Statistical Analysis
3. Results
3.1. Analysis of Echocardiographic Parameters at MIS-C Diagnosis
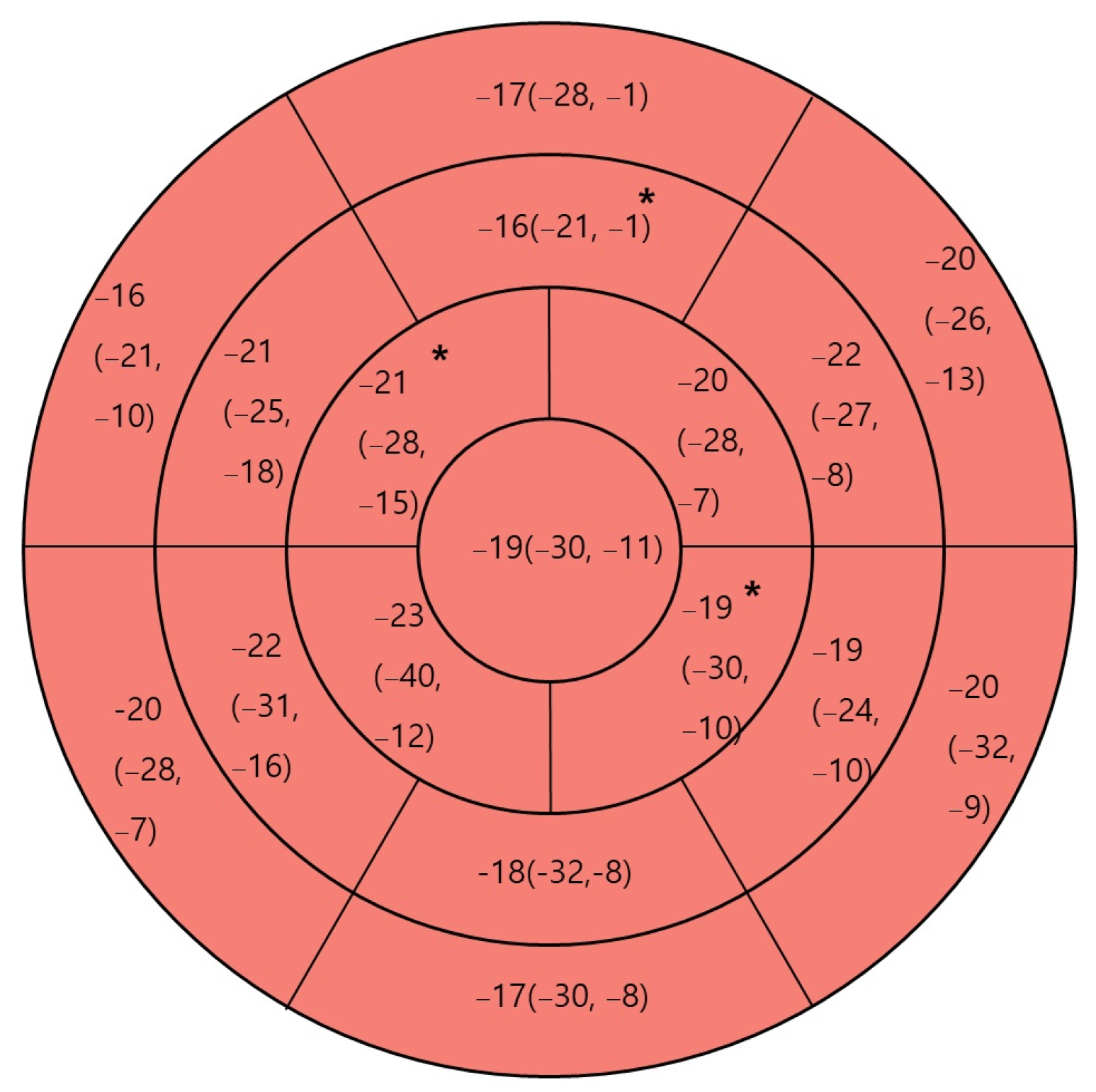
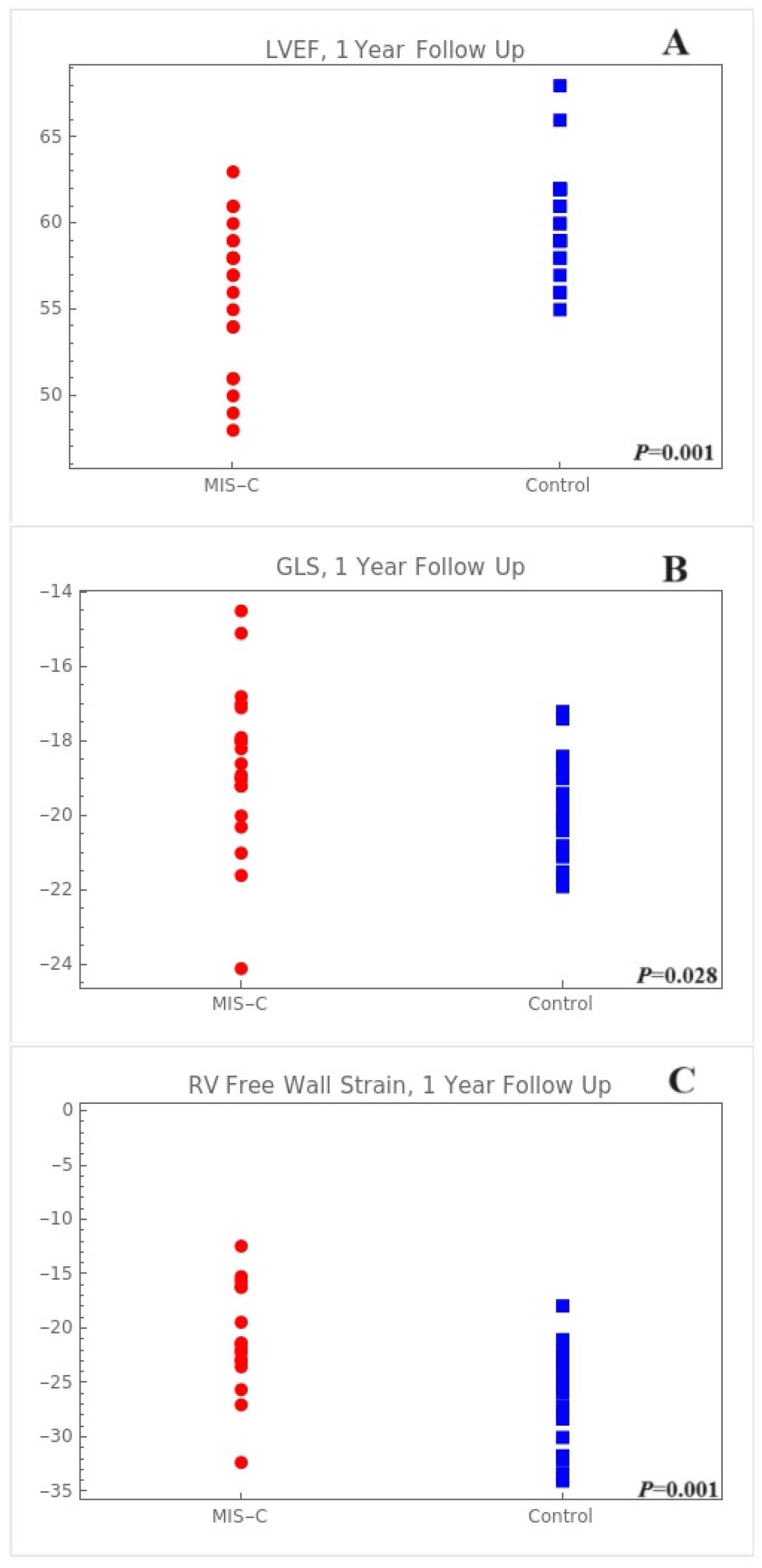
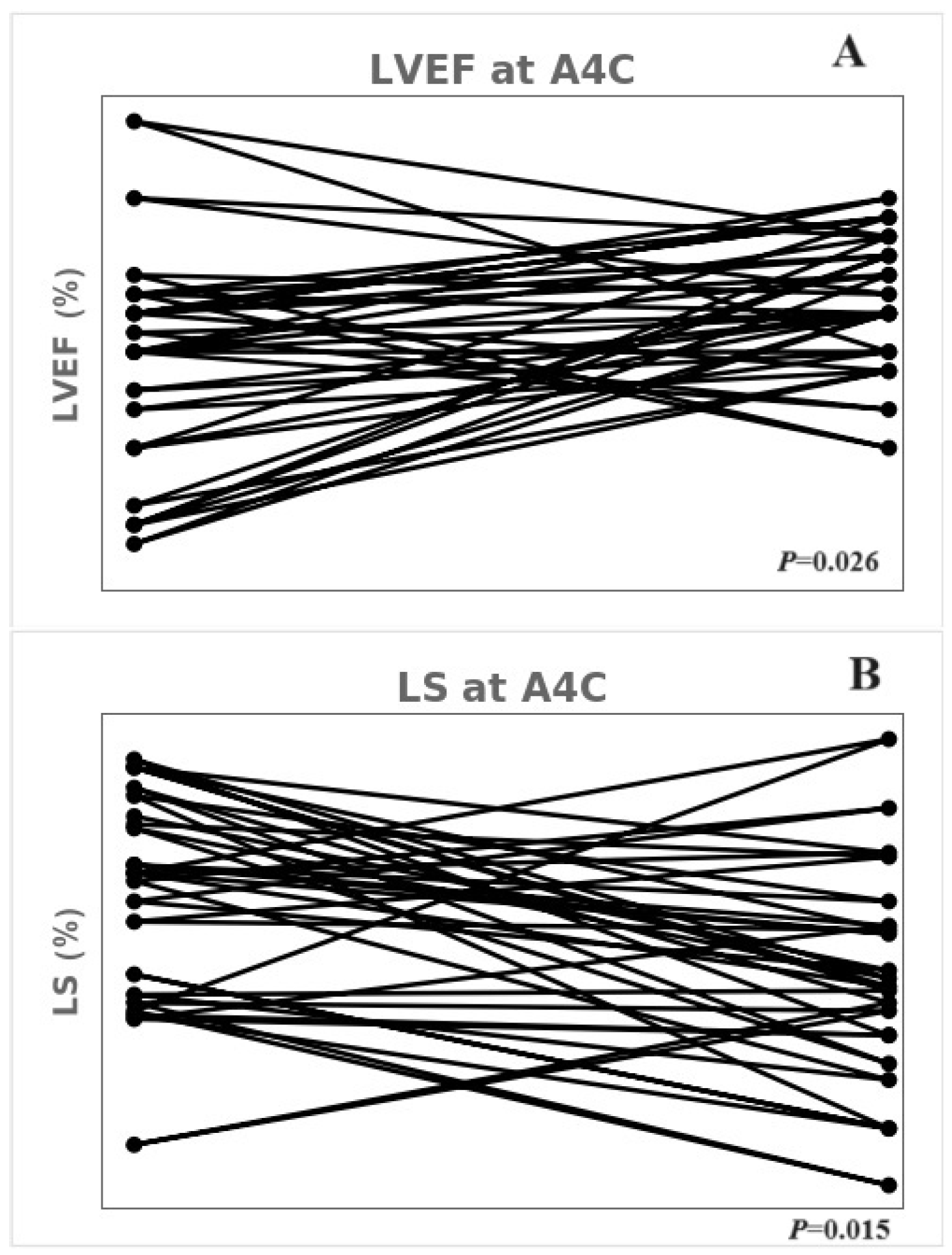
3.2. Echocardiographic Findings of the 1-Year Follow-Up in Patients with MIS-C
3.3. Treatment Outcomes in Patients with MIS-C
3.4. Reproducibility Testing
4. Discussion
Limitations
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sharma, A.; Tiwari, S.; Deb, M.K.; Marty, J.L. Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2): A global pandemic and treatment strategies. Int. J. Antimicrob. Agents 2020, 56, 106054. [Google Scholar] [CrossRef]
- Rafferty, M.S.; Burrows, H.; Joseph, J.P.; Leveille, J.; Nihtianova, S.; Amirian, E.S. Multisystem inflammatory syndrome in children (MIS-C) and the coronavirus pandemic: Current knowledge and implications for public health. J. Infect. Public Health 2021, 14, 484–494. [Google Scholar] [CrossRef]
- Lee, P.Y.; Day-Lewis, M.; Henderson, L.A.; Friedman, K.G.; Lo, J.; Roberts, J.E.; Lo, M.S.; Platt, C.D.; Chou, J.; Hoyt, K.J.; et al. Distinct clinical and immunological features of SARS-CoV-2-induced multisystem inflammatory syndrome in children. J. Clin. Investig. 2020, 130, 5942–5950. [Google Scholar] [CrossRef] [PubMed]
- Feldstein, L.R.; Rose, E.B.; Horwitz, S.M.; Collins, J.P.; Newhams, M.M.; Son, M.B.F.; Newburger, J.W.; Kleinman, L.C.; Heidemann, S.M.; Martin, A.A.; et al. Multisystem inflammatory syndrome in U.S. Children and adolescents. N. Engl. J. Med. 2020, 383, 334–346. [Google Scholar] [CrossRef] [PubMed]
- Perrone, S.; Cannavò, L.; Manti, S.; Rullo, I.; Buonocore, G.; Esposito, S.M.R.; Gitto, E. Pediatric multisystem syndrome associated with SARS-CoV-2 (MIS-C): The interplay of oxidative stress and inflammation. Int. J. Mol. Sci. 2022, 23, 12836. [Google Scholar] [CrossRef]
- Nakra, N.A.; Blumberg, D.A.; Herrera-Guerra, A.; Lakshminrusimha, S. Multi-system inflammatory syndrome in children (MIS-C) following SARS-CoV-2 infection: Review of clinical presentation, hypothetical pathogenesis, and proposed management. Children 2020, 7, 69. [Google Scholar] [CrossRef]
- Wu, E.Y.; Campbell, M.J. Cardiac manifestations of multisystem inflammatory syndrome in children (MIS-C) following COVID-19. Curr. Cardiol. Rep. 2021, 23, 168. [Google Scholar] [CrossRef]
- Alsaied, T.; Tremoulet, A.H.; Burns, J.C.; Saidi, A.; Dionne, A.; Lang, S.M.; Newburger, J.W.; de Ferranti, S.; Friedman, K.G. Review of cardiac involvement in multisystem inflammatory syndrome in children. Circulation 2021, 143, 78–88. [Google Scholar] [CrossRef]
- Henderson, L.A.; Canna, S.W.; Friedman, K.G.; Gorelik, M.; Lapidus, S.K.; Bassiri, H.; Behrens, E.M.; Ferris, A.; Kernan, K.F.; Schulert, G.S.; et al. American College of Rheumatology clinical guidance for multisystem inflammatory syndrome in children associated with SARS-CoV-2 and hyperinflammation in pediatric COVID-19. version 1. Arthritis Rheumatol. 2020, 72, 1791–1805. [Google Scholar] [CrossRef]
- Mahmoud, S.; El-Kalliny, M.; Kotby, A.; El-Ganzoury, M.; Fouda, E.; Ibrahim, H. Treatment of MIS-C in children and adolescents. Curr. Pediatr. Rep. 2022, 10, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Garbin, M.; Raso, I.; Piersanti, A.; Gianolio, L.; De Silvestri, A.; Calcaterra, V.; Corti, C.G.; Nespoli, L.F.; Santacesaria, S.; Fini, G.; et al. Advanced echocardiographic analysis in medium-term follow-up of children with previous multisystem inflammatory syndrome. Children 2022, 9, 917. [Google Scholar] [CrossRef]
- Matsubara, D.; Kauffman, H.L.; Wang, Y.; Calderon-Anyosa, R.; Nadaraj, S.; Elias, M.D.; White, T.J.; Torowicz, D.L.; Yubbu, P.; Giglia, T.M.; et al. Echocardiographic findings in pediatric multisystem inflammatory syndrome associated with COVID-19 in the United States. J. Am. Coll. Cardiol. 2020, 76, 1947–1961. [Google Scholar] [CrossRef]
- Fremed, M.A.; Farooqi, K.M. Longitudinal outcomes and monitoring of patients with multisystem inflammatory syndrome in children. Front. Pediatr. 2022, 10, 820229. [Google Scholar] [CrossRef]
- Capone, C.A.; Misra, N.; Ganigara, M.; Epstein, S.; Rajan, S.; Acharya, S.S.; Hayes, D.A.; Kearney, M.B.; Romano, A.; Friedman, R.A.; et al. Six month follow-up of patients with multi-system inflammatory syndrome in children. Pediatrics 2021, 148, e2021050973. [Google Scholar] [CrossRef] [PubMed]
- Collier, P.; Phelan, D.; Klein, A. A test in context: Myocardial strain measured by speckle-tracking echocardiography. J. Am. Coll. Cardiol. 2017, 69, 1043–1056. [Google Scholar] [CrossRef] [PubMed]
- Mouton, S.; Ridon, H.; Fertin, M.; Pentiah, A.D.; Goémine, C.; Petyt, G.; Lamblin, N.; Coisne, A.; Foucher-Hossein, C.; Montaigne, D.; et al. 2D-speckle tracking right ventricular strain to assess right ventricular systolic function in systolic heart failure. Analysis of the right ventricular free and posterolateral walls. Int. J. Cardiol. 2017, 245, 190–195. [Google Scholar] [CrossRef] [PubMed]
- Di Nardo, M.; Franceschini, A.; Tissieres, P.; Chinali, M. What is new on paediatric echocardiography for the diagnosis, management and follow-up of the multisystem inflammatory syndrome associated with COVID-19? Children 2022, 9, 146. [Google Scholar] [CrossRef] [PubMed]
- Wong, J.; Theocharis, P.; Regan, W.; Pushparajah, K.; Stephenson, N.; Pascall, E.; Cleary, A.; O’Byrne, L.; Savis, A.; Miller, O. Medium-term cardiac outcomes in young people with multi-system inflammatory syndrome: The era of COVID-19. Pediatr. Cardiol. 2022, 43, 1728–1736. [Google Scholar] [CrossRef] [PubMed]
- He, M.; Leone, D.M.; Frye, R.; Ferdman, D.J.; Shabanova, V.; Kosiv, K.A.; Sugeng, L.; Faherty, E.; Karnik, R. Longitudinal assessment of global and regional left ventricular strain in patients with multisystem inflammatory syndrome in children (MIS-C). Pediatr. Cardiol. 2022, 43, 844–854. [Google Scholar] [CrossRef] [PubMed]
- Başar, E.Z.; Usta, E.; Akgün, G.; Güngör, H.S.; Sönmez, H.E.; Babaoğlu, K. Is strain echocardiography a more sensitive indicator of myocardial involvement in patients with multisystem inflammatory syndrome in children (MIS-C) associated with SARS-CoV-2? Cardiol. Young 2022, 32, 1657–1667. [Google Scholar] [CrossRef] [PubMed]
- Melgar, M.; Lee, E.H.; Miller, A.D.; Lim, S.; Brown, C.M.; Yousaf, A.R.; Zambrano, L.D.; Belay, E.D.; Godfred-Cato, S.; Abrams, J.Y.; et al. Council of State and Territorial Epidemiologists/CDC Surveillance Case Definition for Multisystem Inflammatory Syndrome in Children Associated with SARS-CoV-2 Infection—United States. MMWR Recomm. Rep. 2022, 71, 1–14. [Google Scholar] [CrossRef] [PubMed]
- You, S.D.; Kim, J.H.; You, J. Clinical characteristics and short-term outcomes of multisystem inflammatory syndrome in a country with a high prevalence of KD. Front. Pediatr. 2023, 11, 1088529. [Google Scholar] [CrossRef] [PubMed]
- Pettersen, M.D.; Du, W.; Skeens, M.E.; Humes, R.A. Regression equations for calculation of z scores of cardiac structures in a large cohort of healthy infants, children, and adolescents: An echocardiographic study. J. Am. Soc. Echocardiogr. 2008, 21, 922–934. [Google Scholar] [CrossRef]
- Choi, S.H.; Eun, L.Y.; Kim, N.K.; Jung, J.W.; Choi, J.Y. Myocardial tissue doppler velocity in child growth. J. Cardiovasc. Ultrasound 2016, 24, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Levy, P.T.; Machefsky, A.; Sanchez, A.A.; Patel, M.D.; Rogal, S.; Fowler, S.; Yaeger, L.; Hardi, A.; Holland, M.R.; Hamvas, A.; et al. Reference ranges of left ventricular strain measures by two-dimensional speckle-tracking echocardiography in children: A systematic review and meta-analysis. J. Am. Soc. Echocardiogr. 2016, 29, 209–225.e6. [Google Scholar] [CrossRef]
- Chang, J.C.; Matsubara, D.; Morgan, R.W.; Diorio, C.; Nadaraj, S.; Teachey, D.T.; Bassiri, H.; Behrens, E.M.; Banerjee, A. Skewed cytokine responses rather than the magnitude of the cytokine storm may drive cardiac dysfunction in multisystem inflammatory syndrome in children. J. Am. Heart Assoc. 2021, 10, e021428. [Google Scholar] [CrossRef]
- McAree, D.; Griffith, G.J.; Husain, N.; Koenig, P.; Carr, M.; Ward, K. Multisystem inflammatory syndrome in children (MIS-C): Reduced exercise duration and capacity at six month follow-up. Pediatr. Cardiol. 2023, 44, 1605–1612. [Google Scholar] [CrossRef]
- Mainzer, G.; Zucker-Toledano, M.; Hanna, M.; Bar-Yoseph, R.; Kodesh, E. Significant exercise limitations after recovery from MIS-C related myocarditis. World J. Pediatr. 2023, 19, 1149–1154. [Google Scholar] [CrossRef]
| MIS-C (N = 22) | Control (N = 22) | p-Value | |
|---|---|---|---|
| Age at diagnosis (year) | 8.0 (6.0 to 10.8) | 5.5 (5.0 to 8.8) | 0.326 |
| Age at 1 year f/u (year) | 9.0 (6.0 to 13.0) | 0.066 | |
| Male (%) | 45.5 | 54.5 | 0.763 |
| Height (cm) | 133.0 (121.1 to 155.8) | 117.8 (110.8 to 138.3) | 0.286 |
| Height at 1 year f/u (cm) | 133.4 (124.5 to 159.0) | 0.148 | |
| Weight (kg) | 30.5 (22.8 to 45.2) | 22.2 (18.8 to 31.8) | 0.231 |
| Weight at 1 year f/u (kg) | 35.4 (25.0 to 52.0) | 0.084 | |
| Organ involvement (N, %) | |||
| Cardiac involvement | 21 (95.5) | ||
| Troponin-T (ng/mL) | |||
| N-terminal prohormone of brain natriuretic peptide (pg/mL) | |||
| Renal involvement | 7 (31.8) | ||
| Respiratory involvement | 4 (18.2) | ||
| Hematologic involvement | 18 (81.8) | ||
| Gastrointestinal involvement | 19 (86.4) | ||
| Neurologic involvement | 6 (27.3) |
| MIS-C | Control | p-Value | |
|---|---|---|---|
| LVIDd z score | −0.1 (−0.3 to 0.6) | −0.0 (−0.6 to 0.2) | 0.164 |
| FS (%) | 36.5 (30.8 to 40.0) | 38.2 (33.6 to 40.2) | 0.336 |
| EF (%) | 67.2 (59.7 to 71.1) | 66.4 (62.6 to 71.7) | 0.656 |
| LVMI (g/m2) | 72.2 (69.2 to 78.5) | 70.8 (58.2 to 76.0) | 0.330 |
| TAPSE (mm) | 18.4 (16.7 to 22.5) | 20.1 (18.2 to 21.5) | 0.627 |
| RV s’ (cm/s) | 12.0 (10.2 to 12.8) | 12.0 (11.0 to 13.0) | 0.380 |
| Mitral E/A | 1.6 (1.4 to 1.8) | 1.7 (1.6 to 1.8) | 0.211 |
| Mitral E/e’ | 10.0 (7.7 to 10.7) | 7.6 (6.6 to 8.5) | 0.050 |
| LVEF (apical 4-chamber, %) | 51.0 (46.0 to 53.0) | 58.5 (55.0 to 60.0) | <0.001 |
| LVEF (apical 2-chamber, %) | 53.0 (47.0 to 60.0) | 61.0 (59.0 to 63.8) | 0.010 |
| LVEF (total, %) | 52.0 (47.0 to 59.0) | 59.5 (58.2 to 62.0) | 0.002 |
| LS at apical 4-chamber (%) | −16.1 (−19.0 to −14.8) | −20.8 (−21.9 to −18.9) | <0.001 |
| LS at apical 3-chamber (%) | −17.3 (−18.3 to −14.1) | −17.7 (−20.2 to −16.4) | 0.218 |
| LS at apical 2-chamber (%) | −18.4 (−20.1 to −16.9) | −21.1 (−22.7 to −19.8) | 0.006 |
| GLS (%) | −17.5 (−18.7 to −15.9) | −20.1 (−20.9 to −19.1) | 0.001 |
| MIS-C | Control | p-Value | |
|---|---|---|---|
| LVIDd z score | −0.2 (−0.7 to 0.3) | −0.0 (−0.6 to 0.2) | 0.952 |
| FS (%) | 36.6 (33.6 to 38.8) | 38.2 (33.6 to 40.2) | 0.535 |
| EF (%) | 68.9 (63.0 to 70.9) | 66.4 (62.6 to 71.7) | 0.913 |
| LVMI (g/m2) | 63.2 (56.3 to 72.6) | 70.8 (58.2 to 76.0) | 0.239 |
| TAPSE (mm) | 20.1 (18.0 to 21.7) | 20.1 (18.2 to 21.5) | 0.743 |
| RV s’ (cm/s) | 12.0 (10.0 to 12.0) | 12.0 (11.0 to 13.0) | 0.154 |
| Mitral E/A | 1.7 (1.5 to 1.9) | 1.7 (1.6 to 1.8) | 0.660 |
| Mitral E/e’ | 7.7 (6.7 to 8.4) | 7.6 (6.6 to 8.5) | 0.989 |
| LVEF (apical 4-chamber, %) | 54.0 (51.0 to 57.0) | 58.5 (55.0 to 60.0) | 0.003 |
| LVEF (apical 2-chamber, %) | 59.0 (56.0 to 64.0) | 61.0 (59.0 to 63.8) | 0.124 |
| LVEF (total, %) | 57.0 (54.0 to 59.0) | 59.5 (58.2 to 62.0) | 0.002 |
| LS at apical 4-chamber (%) | −18.9 (−20.1 to −17.4) | −20.8 (−21.9 to −18.9) | 0.025 |
| LS at apical 3-chamber (%) | −17.3 (−18.5 to −15.1) | −17.7 (−20.2 to −16.4) | 0.314 |
| LS at apical 2-chamber (%) | −19.9 (−21.3 to −17.8) | −21.0 (−22.7 to −19.8) | 0.148 |
| GLS (%) | −18.8 (−19.4 to −17.7) | −20.1 (−20.9 to −19.1) | 0.015 |
| SRIVR (s−1) | 0.3 (0.2 to 0.3) | 0.2 (0.2 to 0.3) | 0.300 |
| E/SRIVR (cm) | 389.7 (335.2 to 450.0) | 420.6 (340.5 to 466.0) | 0.375 |
| 4-chamber reservoir strain (%) | 38.0 (35.0 to 40.0) | 38.0 (34.5 to 41.8) | 1.000 |
| 2-chamber reservoir strain (%) | 40.0 (33.0 to 43.0) | 43.0 (36.2 to 47.5) | 0.202 |
| Global LA reservoir strain (%) | 37.0 (35.0 to 43.0) | 40.0 (36.0 to 43.8) | 0.551 |
| RV free wall strain (%) | −20.0 (−21.7 to −17.5) | −23.6 (−25.7 to −22.0) | 0.001 |
| RV global strain (%) | −21.6 (−23.1 to −16.2) | −25.9 (−31.7 to −23.5) | 0.001 |
| At Diagnosis | 1-Year Follow-Up | p-Value | |
|---|---|---|---|
| LVIDd z score | −0.2 (−0.3 to 0.6) | −0.2 (−0.7 to 0.3) | 0.111 |
| FS (%) | 36.4 (30.7 to 40.0) | 36.6 (33.6 to 38.8 | 0.609 |
| EF (%) | 66.8 (59.6 to 71.2) | 68.9 (63.0 to 70.9) | 0.191 |
| LVMI (g/m2) | 72.2 (69.2 to 78.5 | 63.2 (55.9 to 74.5) | 0.278 |
| TAPSE (mm) | 18.2 (16.4 to 22.9) | 20.1 (18.0 to 21.7) | 0.475 |
| RV s’ (cm/s) | 12.0 (10.0 to 13.0) | 11.0 (10.0 to 12.0) | 0.427 |
| Mitral E/A | 1.6 (1.4 to 1.8) | 1.66 (1.5 to 1.9) | 0.050 |
| Mitral E/e’ | 9.9 (7.6 to 10.7) | 7.9 (6.9 to 8.5) | 0.005 |
| LVEF (apical 4-chamber, %) | 51.0 (46.0 to 53.2) | 53.5 (51.0 to 56.2) | 0.030 |
| LVEF (apical 2-chamber, %) | 53.5 (47.75 to 61.5) | 59.0 (54.5 to 61.0) | 0.298 |
| LVEF (total, %) | 52.0 (47.0 to 59.2) | 56.5 (53.25 to 58.2) | 0.175 |
| LS at apical 4-chamber (%) | −16.1 (−19.1 to −14.9) | −18.9 (−20.1 to −17.4) | 0.009 |
| LS at apical 3-chamber (%) | −17.3 (−18.25 to −14.5) | −16.9 (−18.45 to −14.7) | 0.978 |
| LS at apical 2-chamber (%) | −18.4 (−20.1 to −17.0) | −19.7 (−20.9 to −17.6) | 0.860 |
| GLS (%) | −17.5 (−19.0 to −16.2) | −18.6 (−19.1 to −17.6) | 0.330 |
| At Diagnosis | 1-Year Follow-Up | p-Value | |
|---|---|---|---|
| LMCA | 1.76 (1.11 to 2.35) | −0.04 (−0.43 to 0.70) | <0.001 |
| LAD | 1.46 (0.34 to 1.96) | 0.14 (−0.36 to 0.89) | <0.001 |
| LCx | 0.76 (0.05 to 1.70) | −0.27 (−0.79 to 0.35) | 0.004 |
| RCA | 0.80 (0.17 to 1.29) | −0.08 (−0.49 to 0.16) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
You, J. Echocardiographic Strain Evaluation Shows Persistent Echocardiographic Changes at 1 Year after Diagnosis of Multisystem Inflammatory Syndrome in Children. Children 2024, 11, 308. https://doi.org/10.3390/children11030308
You J. Echocardiographic Strain Evaluation Shows Persistent Echocardiographic Changes at 1 Year after Diagnosis of Multisystem Inflammatory Syndrome in Children. Children. 2024; 11(3):308. https://doi.org/10.3390/children11030308
Chicago/Turabian StyleYou, Jihye. 2024. "Echocardiographic Strain Evaluation Shows Persistent Echocardiographic Changes at 1 Year after Diagnosis of Multisystem Inflammatory Syndrome in Children" Children 11, no. 3: 308. https://doi.org/10.3390/children11030308
APA StyleYou, J. (2024). Echocardiographic Strain Evaluation Shows Persistent Echocardiographic Changes at 1 Year after Diagnosis of Multisystem Inflammatory Syndrome in Children. Children, 11(3), 308. https://doi.org/10.3390/children11030308







