Abstract
This study builds on Davis’ TAM by integrating environmental and psychological variables relevant to AI medical diagnostics. This study developed a mathematical theoretical model called the “AI medical diagnosis-acceptance evaluation model” (AMD-AEM) to better understand acceptance behavior intention. Using mathematical modeling, we established reflective measurement model indicators and structural equation relationships, where linear structural equations illustrate the interactions among latent variables. In 2025, we collected empirical data from 2380 patients and medical staff who have experience with AI diagnostic systems in teaching hospitals in central Taiwan. Smart PLS 3 was employed to validate the AMD-AEM model. The results reveal that perceived usefulness (PU) and information quality (IQ) are the primary predictors of acceptance behavior intention (ABI). Additionally, perceived ease of use (PE) indirectly influences ABI through PU and attitude toward use (ATU). AI emotional perception (AEP) notably shows a significant positive relationship with ATU, highlighting that warm and positive human–AI interactions are crucial for user acceptance. IQ was identified as a mediating variable, with variance accounted for (VAF) coefficient analysis confirming its complete mediation effect on the path from ATU to ABI. This indicates that information quality enhances user attitudes and directly increases acceptance behavior intention. The AMD-AEM model demonstrates an excellent fit, providing valuable insights for academia and the healthcare industry.
MSC:
62-02; 62P25
1. Introduction
1.1. Research Background and Motivation
With the rapid advancement of artificial intelligence (AI) technology in the medical field, intelligent health information systems have become essential components of modern healthcare [1]. The applications of AI are expanding quickly, including clinical decision support systems (CDSSs), disease prediction models, electronic health record analysis, and personalized health recommendation platforms [2]. According to Bajwa et al. (2021) [3] and Varnosfaderani & Forouzanfar (2024) [4], AI has considerable potential to improve diagnostic accuracy, enhance patient monitoring efficiency, and reduce healthcare costs, making it a crucial technology for the future transformation of innovative healthcare. However, despite its growing maturity, AI medical diagnostic systems encounter several implementation challenges, such as low user acceptance, trust issues, insufficient transparency, privacy concerns, and poor human–machine interaction [5,6]. The “black-box nature” of AI diagnostic systems, which is marked by limited explainability and emotional detachment, can intensify psychological resistance among patients and medical staff, posing a significant barrier to practical adoption [7].
Developing a predictive and theoretically grounded model to analyze user acceptance of AI diagnostic systems has become a crucial priority in academic and practical contexts. This study takes an integrative approach by combining the widely recognized technology acceptance model (TAM) with two specific contextual variables relevant to AI medical diagnostics: 1. information quality (IQ): this refers to the accuracy, completeness, and comprehensibility of the information generated by the system. These factors are essential for building user trust and supporting effective decision-making [8]. 2. AI emotion perception (AEP): this encompasses user perceptions of an AI system’s empathy, responsiveness that mimics human interaction, and overall warmth [9]. Together, these components form the mathematically rigorous dual-A model (AI medical diagnosis-acceptance evaluation modeling: AMD-AEM). This model is designed to explain the intention of patients to accept behavior toward AI medical diagnostic systems.
Using partial least squares structural equation modeling (PLS-SEM), we developed the dual-A (AMD-AEM) model framework to analyze user acceptance behavior intention. Our empirical data analysis confirmed the relationships among latent variables, demonstrating the model’s validity. This research establishes a mathematical and statistical theoretical foundation for the application of AI in the health industry and provides quantitative evidence to support implementation strategies. Notably, this study is the first to quantify information quality (IQ) as a mediating variable and to validate its significant mediation effect on the relationship between attitude (ATU) and acceptance behavioral intention (ABI). It addresses a critical gap in the research on acceptance of AI in medical diagnostics.
1.2. Research Significance
This study presents three key academic and practical contributions:
- Mathematical modeling contribution: we convert abstract psychological constructs and acceptance behavior intentions into the dual-A (AMD-AEM) mathematical model using PLS-SEM. It quantifies the structural relationships among latent variables. This approach addresses the gap in the mathematical and statistical foundations for user acceptance behavior intention in existing AI medical diagnostics research. It showcases the potential for integrating methodologies from information science and social sciences.
- Theoretical innovation: this study expands on Davis’s (1989) [10] oversimplified technology acceptance model (TAM) by introducing two exogenous variables: information quality (IQ) and AI emotion perception (AEP). It addresses TAM’s limitations in accounting for environmental and contextual variables while tackling critical challenges in AI diagnostics, such as information transparency and emotional recognition in human–AI interactions. The enhancements to the model increase its explanatory power for real-world applications, helping to fill research gaps in innovative healthcare, human–computer interaction, and medical trust.
- Practical implications: the findings provide actionable insights for governments and healthcare institutions, offering strategies to enhance the usability of AI systems and improve the credibility of information. Additionally, the validated model provides concrete guidance for optimizing the implementation of AI medical diagnostics. The dual-A (AMD-AEM) model proposed in this study combines theoretical innovation, mathematical rigor, and empirical validation, serving as a foundational framework for deploying AI medical diagnostic systems in regional medical centers and advancing health informatics.
1.3. Research Objectives
(1) To construct a mathematical model for understanding AI medical diagnostic acceptance behavior.
By integrating Davis’s (1989) [10] technology acceptance model (TAM) framework with key contextual variables in AI healthcare, we develop a model called “AI medical diagnosis-acceptance evaluation model” (AMD-AEM). This model uses structural equation modeling and mathematical formalization, focusing on six latent constructs: perceived ease of use (PE), perceived usefulness (PU), information quality (IQ), AI emotion perception (AEP), attitude toward use (ATU), and acceptance behavior intention (ABI). The mathematical model represents the linear structural equations between these latent variables.
(2) To validate the relationships between the variables and the influence paths using partial least squares structural equation modeling (PLS-SEM) for data analysis and model estimation.
We test the statistical significance of all hypothesized paths for the AMD-AEM latent variables by checking reliability (Cronbach’s α and composite reliability), validity (average variance extracted (AVE) and discriminant validity), model fit (standardized root mean square residual: SRMR), and the significance of structural coefficients via Smart PLS 3.
(3) To examine the mediating effect of information quality (IQ).
We specifically analyze IQ’s mediating role between the independent variables—perceived ease of use (PE), perceived usefulness (PU), AI emotion perception (AEP), and attitude toward use (ATU)—and the dependent variable, acceptance behavior intention (ABI). This analysis utilizes the bootstrapping method (5000 iterations) approach in Smart PLS 3 to uncover the underlying psychological mechanisms.
2. Literature Review
To establish the theoretical foundation of this study, the researchers conducted a comprehensive review of the relevant journal articles, conference papers, and monographs. This section is organized into four parts: (1) applications and challenges of AI medical diagnostic systems; (2) the technology acceptance model and key variables that influence acceptance behavior intention towards AI medical diagnostic systems; (3) the historical background and development of mathematical modeling theory; and (4) the construction of a theoretical model that applies PLS-SEM to understand acceptance behavioral intention towards AI medical diagnostics.
2.1. Applications and Challenges of AI Medical Diagnostic Systems
Artificial intelligence (AI) technology has rapidly advanced in the healthcare industry in recent years, becoming a key driver of the transformation toward competent healthcare. Through technologies such as machine learning, natural language processing (NLP), and clinical decision support systems (CDSSs), AI effectively assists medical institutions in various tasks, including disease diagnosis, case management, image interpretation, medical record analysis, health risk prediction, and remote care [3,11]. For instance, AI algorithms can analyze vast amounts of structured and unstructured medical data to predict specific disease risk indices and provide personalized health recommendations and care plans, helping specialists make accurate decisions quickly under high-pressure conditions [4,12].
In terms of efficiency and accuracy, AI systems show clear advantages. Studies indicate that well-designed AI diagnostic tools can improve healthcare quality, reduce human errors, lower treatment costs, enhance patient management, and realize long-term care [8]. However, despite these significant technological advances, practical implementation faces multiple challenges related to user acceptance [7]. Therefore, this study incorporates two key exogenous variables, information quality (IQ) and AI emotion perception (AEP), to further explore their effects on user acceptance behavior intention. First, information quality is crucial in influencing user trust and decision-making. AI medical diagnostic systems that fail to provide accurate, timely, and easily understandable information struggle to gain user confidence. The “black-box” nature of their computational logic and the lack of explainability in medical diagnostic results often prevent users from understanding AI’s reasoning, thereby diminishing system credibility [7,13]. Second, AI emotion perception (AEP) refers to whether AI systems can perceive and appropriately respond to users’ emotional states during interactions. AI interfaces that appear cold, unresponsive, or lack humanized communication weaken users’ psychological connection and willingness to use the system [14].
Furthermore, users’ concerns about privacy and information security are closely linked to information quality. AI healthcare systems process large amounts of personal data; without robust encryption and data protection policies, perceived information quality diminishes, further undermining user confidence [15]. Furthermore, AI emotion perception fails to address healthcare professionals’ occupational emotions and role identity adequately. In that case, it may lead to anxiety and resistance due to fears of AI replacing human roles, creating barriers to adoption. In summary, while AI medical diagnostic systems possess great potential and significant technological advantages, their practical implementation must consider user trust, psychological acceptance, information quality, and privacy security [6,15].
This study aims to comprehensively understand users’ acceptance psychology and behavioral responses while promoting AI healthcare systems by incorporating the exogenous variables of information quality and AI emotion perception. This approach enhances theoretical models’ explanatory power and predictive accuracy within practical settings. Therefore, an in-depth exploration of the behavioral variables and psychological mechanisms influencing user acceptance behavior intention holds significant theoretical and practical value for promoting the widespread and sustainable development of AI medical diagnostic systems.
2.2. Technology Acceptance Model (TAM) and Key Variables Influencing Acceptance Behavior Intention to AI Medical Diagnostic Systems
Davis (1989) [10] proposed the technology acceptance model (TAM) to understand user adoption behavior toward emerging technologies. This model emphasizes key variables such as perceived ease of use (PE), perceived usefulness (PU), and behavioral intention (BI). PE refers to users’ perception of how easily the system operates, while PU indicates whether the system enhances decision-making and efficiency. Both of these variables can influence acceptance behavior intention (ABI) directly or indirectly through attitude toward use (ATU) [16]. Over the past three decades, TAM has evolved with numerous extensions, including TAM2 [17] and the unified theory of acceptance and use of technology (UTAUT). These extensions introduce social influence, facilitating conditions, and cognitive motivation, which broaden TAM’s applicability across diverse technological contexts [18,19]. Given its concise framework and stable measurement properties, ref. [20] suggests leveraging the strengths of TAM while incorporating environmental variables to enhance its explanatory power and practicality, particularly in the context of AI, mobile health (mHealth), and electronic health record systems.
Based on this foundational understanding, the researchers argue that applying the traditional TAM to AI medical diagnostics requires consideration of more complex usage contexts and psychological factors. Therefore, building on Davis’ (1989) [10] TAM, we introduce two new latent variables—information quality (IQ) and AI emotion perception (AEP)—to create a dual-A (AMD-AEM) mathematical model. This model aims to explain the factors influencing patients’ acceptance behavior intention toward AI diagnostic systems. It comprises six primary constructs:
- Perceived ease of use (PE): intuitive and simple system operation enhances user confidence and acceptance [16].
- Perceived usefulness (PU): users’ belief that AI improves diagnostic accuracy and efficiency increases motivation to use [16].
- Information quality (IQ): provision of timely, accurate, secure, and understandable information by AI systems strengthens trust and satisfaction [8,21].
- AI emotion perception (AEP): AI systems capable of perceiving and responding to human emotions improve acceptance behavior intention (ABI) and positively influence ATU [9].
- Attitude toward use (ATU): an overall evaluation formed by the combined effects of the above constructs, serving as a mediator predicting acceptance behavior intention [20].
- Acceptance behavior intention (ABI): The dependent variable representing patients’ willingness to accept AI medical diagnostic behavior intention.
In summary, PE, PU, IQ, and AEP interact as influencing factors, with ATU as a critical bridge linking these variables to ABI. This study integrates the traditional TAM with contemporary environmental and psychological variables (IQ and AEP) relevant to AI medical diagnostics, constructing a novel dual-A (AMD-AEM) mathematical model. The model is validated using PLS-SEM, contributing to a deeper understanding of user acceptance behavior intention in AI health information systems.
2.3. Background and Development of Mathematical Modeling Theory
Mathematical modeling transforms complex real-world problems into mathematical expressions to enable systematic analysis and predictive reasoning [22]. Hochmuth et al. (2025) [23] emphasize that modeling is a methodological tool and has significant educational, psychological, and cultural value. Kaiser and Sriraman (2006) [24] identified three main orientations in mathematical modeling: practical (focused on solving real-world problems), educational (facilitating mathematical learning), and critical (promoting civic and reflective thinking).
Mathematical modeling in healthcare and AI systems helps conceptualize and quantify users’ perceptions, attitudes, and behavioral responses to AI-based diagnostic technologies [25]. With the growing integration of AI into clinical and health management settings, understanding patient acceptance of AI diagnostic systems has become a critical issue [15]. Developing a mathematical model that captures the psychological and cognitive mechanisms underlying acceptance behavior provides a valuable empirical and analytical tool for system designers and policymakers [26].
This study proposes an extended mathematical framework—the AMD-AEM model—based on Davis’ (1989) [10] technology acceptance model (TAM), incorporating two additional constructs: information quality (IQ) and AI emotion perception (AEP). These additions better reflect the complexity of AI-driven healthcare environments, including information transparency and human–machine emotional interaction. Methodologically, the study applies partial least squares structural equation modeling (PLS-SEM) as the inferential basis for the model.
The mathematical expression for the acceptance behavior intention (ABI) is formulated as:
ABI = β8 · ATU + β9 · IQ + ε4
ABI represents the behavioral intention to accept AI diagnostics, ATU denotes attitude toward use, IQ is information quality, β indicates path coefficients, and ε is the structural error term.
A reflective measurement model is adopted in this study. Following Hair et al. (2021) [27], factor loadings (λ), composite reliability (CR), and average variance extracted (AVE) are used to test the reliability and validity of the latent variables. This modeling framework enables the quantification of abstract psychological constructs and effectively explains and predicts user acceptance of AI diagnostic systems. It highlights the practical and empirical value of mathematical modeling in advancing research on behavioral intention in intelligent healthcare systems.
2.4. Construction of Theoretical Model for AI Medical Diagnostic Acceptance Behavior Intention Using PLS-SEM
With the increasing prevalence of AI and clinical diagnostic systems, users’ acceptance behavior intention decision mechanisms involve multiple latent psychological variables and may exhibit nonlinear relationships [28]. Traditional statistical methods, such as multiple regression and factor analysis, struggle to effectively explain these complex causal structures and relationships among multiple latent variables, especially in analyzing mediation and moderation effects [29]. To address these challenges, structural equation modeling (SEM), which can handle latent variables and complex path relationships, has become the mainstream method for theoretical verification in related fields. Among SEM techniques, PLS-SEM estimates parameters based on maximizing variance and offers several advantages [27,29,30]: (1) it can handle complex multivariable models; (2) it is suitable for small samples, many variables, or non-normally distributed data; and (3) it is prediction-oriented, emphasizing explanatory power and practical utility, making it effective for hypothesis testing [31]. According to [32], compared to covariance-based SEM (CB-SEM), PLS-SEM is more prediction-driven and flexible in model construction, thus widely applied in information systems, health education, and the acceptance behavior intention research.
In healthcare information system studies, PLS-SEM provides a comprehensive analysis process that tests the TAM path hypotheses and examines mediation effects. For example, ref. [33] explored how technology influences nurses’ willingness to improve performance using medical applications and how technology facilitates hospital system improvements. Their results showed statistically significant relationships among technology complexity, perceived usefulness, perceived ease of use, and acceptance behavior intention. Similarly, Saihi et al. (2024) [34] applied PLS-SEM to validate model robustness and identify key factors influencing users’ decisions to adopt chatbots.
To enhance TAM’s generalizability in AI medical diagnostic contexts, this study incorporates two cognitive–psychological and environmental constructs: AI emotion perception (AEP) and information quality (IQ). Emotion is a dynamic cognitive and physiological state responding to inputs such as experiences, thoughts, or interactions [9,35]. Research on human emotions is crucial for human–computer interaction and brain–machine evaluation; thus, detailed study and safe automated recognition of human emotions by AI are vital. Emotion recognition is key in human–computer interaction, healthcare, mental health monitoring, and security [8]. Recent studies highlight that AI systems with human-like emotional recognition capabilities hold promise and risks, with potential constructive applications in education, patient self-awareness, conversational therapy, and diagnosis [36,37,38]. In addition, the information quality emphasizes the accuracy, completeness, and comprehensibility of information provided by AI medical diagnostic systems. High-quality information enhances user trust and sense of security and strengthens perceived usefulness, thereby improving attitude toward use and acceptance behavior intention [3,37].
Previous AI-related studies have largely overlooked the importance of AEP and IQ and have not integrated them into the TAM framework, especially in AI clinical diagnostics research, where such integration remains scarce. Therefore, this study employs PLS-SEM to construct and validate an integrated model for examining patients’ acceptance behavior intention to AI medical diagnostic systems (AMD-AEM). This model addresses TAM’s risk perception and information trust limitations and enhances explanatory depth and predictive power for high-tech acceptance behavior intention.
3. Research Methodology
3.1. Composition of the Dual-A Mathematical Model (AMD-AEM)
3.1.1. Theoretical Logic of Model Construction
This study is based on the technology acceptance model (TAM). It introduces two key extended variables related to the characteristics of AI medical diagnostic systems: IQ: information quality, emphasizing the accuracy and transparency of information provided by the AI system; AEP: AI emotion perception, highlighting the system’s humanized interaction and warmth in response. Therefore, the constructed dual-A mathematical model (AMD-AEM) includes six latent variables: PE: perceived ease of use; PU: perceived usefulness; IQ: information quality; AEP: AI emotion perception; ATU: attitude toward use; and ABI: acceptance behavior intention.
The mathematical and statistical foundations for constructing this dual-A mathematical model (AMD-AEM) are analyzed as follows.
3.1.2. Overall Mathematical Model Form
The following system of simultaneous structural equations can represent the overall behavioral performance of the AMD-AEM:
3.1.3. Reflective Measurement Model
For each latent variable ηj, the measurement equation for the observed variable Xij is as follows:
Xij = λij · ηj + εij
For example, perceived ease of use (PE) is reflected by three items: PE1, PE2, and PE3.
PE1 = λ11 · PE + ε11
PE2 = λ12 · PE + ε12
PE3 = λ13 · PE + ε13
3.1.4. Hypotheses and Mathematical Formulations
Based on the hypothesis methodology, the model establishes 16 research hypotheses (H1–H16), which can be mathematically expressed as follows:
(1) Structural function of PU: predicted by PE and IQ: PU = β1 · PE + β7 · IQ + ε1
Corresponding hypotheses:
(2) Structural function of AEP: predicted by PU: AEP = β2 · PU + ε5
Corresponding hypothesis:
(3) Structural function of ATU: predicted by PU, PE, AEP, IQ: ATU = β4 · PU + β6 · PE + β8 · AEP + β10 · IQ + ε3
Corresponding hypotheses:
(4) Structural function of ABI: predicted by ATU and IQ: ABI = β11 · ATU + β9 · IQ + ε4
Corresponding hypotheses:
(5) Mediating hypotheses analysis
The significance testing (p-values, t-values, confidence intervals) and variance accounted for (VAF) classification are conducted using the Bootstrapping method with 5000 iterations:
- (1)
- VAF > 80%: full mediation;
- (2)
- 20% < VAF < 80%: partial mediation;
- (3)
- VAF < 20%: no or weak mediation.
This study designs the following mediation effect hypotheses to verify the internal psychological process links within the model, as shown in Table 1.

Table 1.
Indirect effects define mathematical expressions of mediation hypotheses.
In summary, based on the analytical framework of the dual-A mathematical model (AMD-AEM), this study targets individuals and healthcare professionals in central Taiwan who have experience using an AI medical diagnostic system to explore their acceptance behavior intention toward the system. Using a stratified sampling technique, 2380 valid questionnaires were collected from public and private medical institutions. To validate this “hypothetical theoretical model” framework, the study proposes the following mathematical hypotheses, as shown in Table 2:

Table 2.
Mathematical hypotheses of this study.
3.2. Advantages of the Dual-A Mathematical Model (AMD-AEM)
This study is based on Davis’ (1989) [10] TAM and extends the theoretical framework by incorporating two core AI medical diagnostic variables: IQ and AEP. This extension addresses and overcomes TAM’s limitations in covering medical information transparency and human–computer emotional interaction, enhancing the model’s explanatory power in the practical AI medical diagnosis healthcare sector.
We then compared this AMD-AEM model constructed in this study with previously established extended models (TAM, TAM2, UTAUT). The advantages of the dual-A mathematical model (AMD-AEM) include the following: (1) the addition of two AI medical-specific external variables, IQ and AEP; (2) emphasis on preserving explanatory power for human–computer emotional interaction and information transparency while simplifying computation and modeling processes; (3) linear computability, supporting PLS-SEM; (4) specific explanatory power regarding emotional aspects and information credibility tailored to AI medical characteristics. Table 3 summarizes the comparison and differences between the AMD-AEM and previously developed models.

Table 3.
Comparison of AMD-AEM with TAM, TAM2, and UTAUT models.
3.3. Implementation Steps for Constructing the Dual-A Mathematical Model (AMD-AEM)
The implementation steps for constructing the dual-A mathematical model (AMD-AEM) proposed in this study are based on mathematical modeling and the PLS-SEM analysis process. Following a logical sequence, six significant steps are organized:
- (1)
- Theoretical model construction;
- (2)
- Questionnaire design and pilot testing;
- (3)
- Data collection and sample planning;
- (4)
- Measurement model evaluation;
- (5)
- Structural model analysis;
- (6)
- Model fit and mediation effect verification.
3.3.1. Research Process of Implementation Steps
The research process of the implementation steps organized by this study is illustrated in Figure 1.
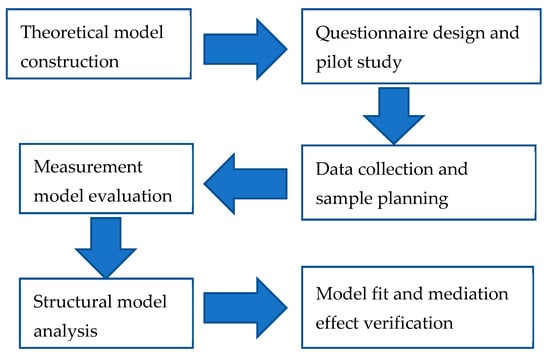
Figure 1.
Implementation process steps of the dual-A mathematical model (AMD-AEM). Source: this study.
3.3.2. Questionnaire Development, Reliability and Validity
This study targeted individuals and central Taiwan healthcare personnel with experience using AI medical diagnostic systems. A stratified sampling technique was employed, collecting 2380 valid questionnaires from public and private medical institutions. The sample size ensured representativeness across demographic variables such as age, occupation, and system familiarity.
The questionnaire data collected consisted of two parts: 1. basic information, including gender, age, and prior experience with AI medical diagnosis; 2. questionnaire contents, covering five key research dimensions: perceived usefulness, perceived ease of use, information quality, AI emotion perception, attitude toward use, and acceptance behavior intention. Each item in the questionnaire was measured using a 7-point Likert scale ranging from (1) strongly disagree, (2) disagree, (3) somewhat disagree, (4) neutral, (5) somewhat agree, and (6) agree to (7) strongly agree.
After completing the initial draft of the questionnaire, a pilot study was conducted with 50 randomly selected participants. The results were analyzed using SPSS 22.0 software to assess split-half reliability, yielding a reliability coefficient of 0.91. Additionally, three professors specializing in medical management in Taiwan reviewed and revised the questionnaire, ensuring strong expert validity.
Based on the mathematical modeling foundation from the literature review and referencing studies by Khare et al. (2024), Elyoseph et al. (2023, 2024), and Hadar-Shoval et al. (2023) [9,36,37,38], the researchers developed the survey instrument. The variables and corresponding contents of this questionnaire are displayed in Table 4.

Table 4.
Questionnaire variables and item correspondence.
3.3.3. Hypothetical Theoretical Research Framework
The dual-A mathematical model (AMD-AEM) for AI medical diagnostic systems constructed in this study integrates the latent variables AEP and IQ, expanding the core variables of Davis’ (1989) [10] TAM model. These variables include perceived ease of use (PE), perceived usefulness (PU), information quality (IQ), AI emotion perception (AEP), attitude toward use (ATU), and acceptance behavior intention (ABI) for AI medical diagnosis. The hypothetical theoretical research framework is illustrated in Figure 2.
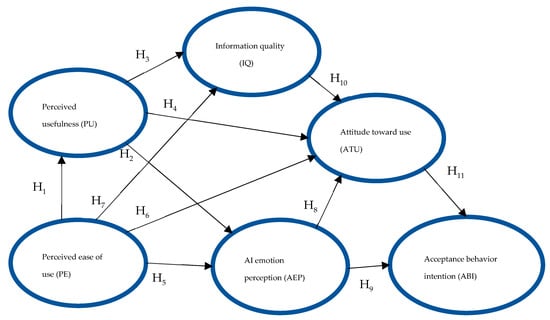
Figure 2.
Hypothetical theoretical research framework of the dual-A mathematical model (AMD-AEM). Source: this study.
4. Analysis and Discussion
The tool used in this study’s dual-A mathematical model (AMD-AEM) is a survey questionnaire, with the contents and items designed based on the latent variables of the hypothetical theoretical framework.
4.1. Research Data Analysis Tools
After collecting the survey questionnaires, this study employed SPSS 22.0 and Smart PLS 3 to construct and analyze the structural equation model. The authors chose partial least squares structural equation modeling (PLS-SEM) for data analysis due to the moderate sample size obtained and the possibility of non-normal data distribution. Additionally, the model construction involved six latent variables, adding a certain level of complexity. Therefore, PLS-SEM was selected for its robustness and suitability in model construction and analysis.
Between March and June 2025, the study targeted individuals and healthcare personnel in central Taiwan with experience using AI medical diagnostic systems. Using a stratified sampling technique, 2380 valid questionnaires were collected from public and private medical institutions. Among the respondents, 1166 were male and 1214 female; ages ranged from 18 to 65, with the largest group (46%) aged 26 to 45. The data were analyzed using Smart PLS 3 to test the hypothetical theoretical model. All participants signed a consent form titled “Study on Acceptance Behavior Intention of AI Medical Diagnostic Systems Based on AMD-AEM.”
4.2. Mathematical and Statistical Foundation Analysis of the AMD-AEM Model
This study integrates IQ and AEP to construct a dual-A mathematical model (AMD-AEM) for AI medical diagnostic systems based on the TAM. We select partial least squares structural equation modeling (PLS-SEM) for the mathematical and statistical foundation analysis. The detailed explanation and discussion are as follows.
4.2.1. Latent Variable Matrix η
PLS-SEM consists of two main components: the measurement and structural models. The latent variable matrix η is expressed as in Equation (1):
In the 6 × 1 matrix, PE: perceived ease of use; PU: perceived usefulness; IQ: information quality; AEP: AI emotion perception; ATU: attitude toward use; and ABI: acceptance behavior intention.
4.2.2. Structural Model
Based on the path coefficients and the PLS-SEM model settings, the structural equation of the model is as follows:
- (1)
- PU is a function of PE and IQ: PU = β1 · PE + β2 · IQ + ε1;Path coefficient: β1 = 0.688, β2 = 0.178;
- (2)
- AEP is a function of PE: AEP = β3 · PE + ε2;Path coefficient: β3 = 0.037;
- (3)
- ATU is a function of PU, PE, AEP, IQ;ATU = β4 · PU + β5 · PE + β6 · AEP + β7 · IQ + ε3;Path coefficient: β4 = 0.422, β5 = 0.042, β6 = 0.033, β7 = 0.258;
- (4)
- ABI is a function of ATU and IQ: ABI = β8 · ATU + β9 · IQ + ε4;Path coefficient: β8 = 0.212, β9 = 0.862.
4.2.3. Coefficients of Determination R2 (Model Explanatory Power)
Using PLS-SEM for mathematical analysis, the coefficients of determination R2 for the latent variables in the AMD-AEM model are PU = 0.178, AEP = 0.608, ATU = 0.818, IQ = 0.167, and ABI = 0.128, respectively. The coefficients of determination R2 indicate that these latent variables demonstrate the model’s moderate to high explanatory power, as shown in Table 5.

Table 5.
Mathematical analysis of coefficients of determination R2 (model explanatory power).
4.2.4. Effect Size f2
Based on the TAM, this study integrates IQ and AEP to construct the AI medical diagnostic AMD-AEM model. We then conducted a mathematical analysis using PLS-SEM to represent individual path contributions to the model’s explanatory power. According to Cohen’s (1988) [39] criteria, f2 = 0.02 (small); f2 = 0.15 (medium); f2 = 0.35 (large).
The effect sizes (f2) representing the contribution of the individual path of the AMD-AEM model are as follows:
- IQ to ATU: f2 = 3.373 (extremely large contribution);
- PE to AEP: f2 = 0.991 (very large contribution);
- PE to PU: f2 = 0.216 (moderately large contribution).
The results of explanatory power and contribution of individual paths in the AMD-AEM model (effect size f2) are shown in Table 6.

Table 6.
Explanatory power and contribution of individual paths in the AMD-AEM model (effect size f2).
4.2.5. Measurement Model Validity Criteria
PLS-SEM (partial least squares structural equation model) estimates model parameters through an iterative calculation procedure, and its core goal is to maximize the explained variance among latent variables. The mathematical model validity criteria are described as follows:
1. Indicator factor loadings
After the AI medical diagnostic AMD-AEM model is constructed, we use PLS-SEM for mathematical analysis. Assuming each latent variable (PU, PE, IQ, AEP, ATU, ABI) is reflected by several observed indicators. Indicator factor loadings can be expressed by the following Formula (2):
χij = λij ηj + εij
Symbol descriptions:
- χij: the jth observed indicator (questionnaire item) of the ith latent variable;
- λij: the factor loading of that indicator on the latent variable;
- ηj: the latent variable (latent construct);
- εij: measurement error.
- λij ≥ 0.7 (or the minimum value shall not be less than 0.6).
For example, “perceived ease of use” (PE) can be represented by three observed indicators, PE1 to PE3, as:
- PEi = λi · PE + εi, i = 1, 2, 3
2. Average variance extracted (AVE)
The AVE of each potential variable ηj is defined as follows: the convergence condition is AVEj ≥ 0.5.
Symbol descriptions:
- AVEj: average variance extracted of latent variable j;
- λij: factor loading of the ith observed indicator on latent variable j;
- k: number of observed indicators for the latent variable;
- Var(εij): variance of the measurement error for indicator ij.
3. Composite reliability (CR)
The composite reliability is defined as follows: the convergence condition is CRj ≥ 0.7.
Symbol descriptions:
- CRj: composite reliability of latent variable j;
- ij: factor loading of the ith indicator on latent variable j;
- k: number of indicators measuring latent variable j;
- Var(εij): variance of the measurement error for indicator ij.
4. Cronbach’s α reliability coefficient
The convergence condition of Cronbach’s alpha is: α ≥ 0.7.
Symbol descriptions:
- α: Cronbach’s alpha coefficient;
- k: number of items (indicators) in the latent construct;
- variance of the ith item;
- variance of the total score (sum of all items under the same latent construct).
4.2.6. Model Analysis
After the AI medical diagnostic AMD-AEM model is constructed, we use PLS-SEM for mathematical analysis. The structural model can be mathematically represented by linear equations that simulate the hypothesized relationships among latent variables. Its general form is shown in Equation (3), where Y is the dependent variable (ABI); Xi are the independent variables (PU, PE, IQ, AEP, ATU); βi are the estimated path coefficients; and ε is the error term:
Y = β0 + ∑βi Xi + ε
The measurement model is evaluated through reflective indicators to ensure that the model has convergent validity and discriminant validity before analyzing the structural paths. The causal relationships among latent variables can be expressed by the linear structural equation (Equation (4)) as follows:
H = β · η + ζ
In this study, the specific structural relationships among the latent variables are detailed as follows:
where βi: path coefficient between latent variables, and ζi: error term of the structural model. All variables were standardized (mean = 0, variance = 1). According to the PLS-SEM mathematical analysis, all latent variables in this study have CR > 0.8 and AVE > 0.6, indicating good reliability and convergent validity.
PU = β1 PE + β2 IQ + ζ1; AEP = β3 PE + ζ2; ATU = β4 PU + β5 PE + β6 AEP + β7 IQ + ζ3; ABI = β8 ATU + β9 IQ + ζ4
4.3. Case Study Analysis of the Dual-A Mathematical Model (AMD-AEM)
This study employs confirmatory factor analysis (CFA) to examine the convergent validity and discriminant validity of the measurement structure of the AMD-AEM model. According to the statistical principles of the least squares method, before conducting structural model analysis, it is necessary to establish an optimal fitting measurement model [39]. To verify whether there are influential relationships among the six constructs proposed in this study—PE, PU, IQ, AEP, ATU, and ABI—SmartPLS 3 was used to test the associations among these latent variables and to assess whether the null hypotheses hold or are rejected.
4.3.1. Convergent Validity Test of the Dual-A Mathematical Model (AMD-AEM)
This study conducted a mathematical analysis using PLS-SEM. It tested convergent validity based on the criteria proposed by Kline (2019) [40], analyzing factor loadings (CFR), average variance extracted (AVE), and composite reliability (CR) of the survey items. Hair et al. (2019) [41] suggest that an ideal “hypothetic theoretical model” should have factor loadings for all latent variables’ corresponding items greater than the critical value of 0.60, AVE values for each latent variable should exceed 0.5, and Cronbach’s α and composite reliability (CR) should be above the threshold of 0.7. Additionally, the square root of each latent variable’s AVE should be greater than its correlations with any other latent variables in the model [27]. Furthermore, Fornell and Larcker (1981) [42] state that an ideal “hypothetical theoretical model” should meet the following three criteria for convergent validity: (1) standardized factor loadings greater than 0.5; (2) AVE greater than 0.5; and (3) CR greater than 0.6.
The data analysis results of this study are shown in Table 7. For all latent variables in the dual-A mathematical model (AMD-AEM), the factor loadings of their corresponding items ranged from 0.738 to 0.927, Cronbach’s α values ranged from 0.722 to 0.893, CR values ranged from 0.843 to 0.934, and AVE values ranged from 0.643 to 0.855. These results meet the recommended thresholds [41]. According to Fornell and Larcker’s (1981) [42] convergent validity criteria, the factor loadings of all items corresponding to the latent variables exceed the 0.5 threshold, AVE values for each latent variable are greater than 0.5, Cronbach’s α are above 0.7, CR values are far above 0.6, and the square root of each latent variable’s AVE is greater than its correlations with any other latent variables in the model. The empirical results demonstrate that all latent variables (constructs) in the dual-A mathematical model (AMD-AEM) proposed by this study meet convergent validity and internal reliability criteria.

Table 7.
Confirmatory factor analysis of items corresponding to latent variables (convergent validity).
4.3.2. Discriminant Validity Test of the Dual-A Mathematical Model (AMD-AEM)
This study verifies the correlations between constructs and their extracted average variance extracted (AVE). The survey questionnaire data analysis results indicate that all latent variables in this study demonstrated satisfactory discriminant validity (Fornell & Larcker, 1981) [42]. Specifically, the square root of the AVE for each construct is greater than all the correlations with other constructs outside the main diagonal of the reflective structure. These results indicate that all latent variables in the dual-A mathematical model (AMD-AEM) possess adequate discriminant validity, as shown in Table 8.

Table 8.
Correlations between constructs and extracted average variance of latent variables (discriminant validity).
4.3.3. Goodness of Fit (GOF) Analysis of the Dual-A Mathematical Model (AMD-AEM)
This study evaluated the goodness of fit for the “hypothetical theoretical model”—the dual-A mathematical model (AMD-AEM). When the four parameters SRMR, d_ULS, d_G, and NFI are all satisfied (as shown in Table 4), the “hypothetical theoretical model” can be considered a good-fitting model [41]. The data analysis in this study found that SRMR = 0.06, below the threshold of 0.08, indicating a moderate fit. According to [43], an NFI value greater than 0.9 indicates an optimal model fit, while an NFI value greater than 0.8 is considered acceptable. As shown in Table 8, the NFI value ranges from 0 to 1 and is derived by comparing a given independent theoretical model. A higher value, especially one close to 1, is considered ideal, meaning the model fits well [44]. The empirical data analysis in this study shows an NFI of 0.79, close to the optimal acceptance threshold (>0.9). Therefore, this study’s proposed dual-A mathematical model (AMD-AEM) is believed to be an accepted fit model, as shown in Table 9.

Table 9.
Goodness of fit comparison table for the dual-A mathematical model (AMD-AEM).
4.3.4. Mathematical Analysis of Mediation Effects
After the AI medical diagnostic AMD-AEM model is constructed, we use PLS-SEM for the mathematical analysis. To verify whether the model path coefficients and mediation effects reach statistical significance, this study employs the bootstrapping resampling method (5000 iterations) for estimation. The summary of the calculation formula is as follows:
- (1)
- Indirect effect estimation:Indirect Effect = β1 × β2
- (2)
- The t-value estimation:
- (3)
- Proportion of variance explained (VAF):
During model analysis, this study utilized the SmartPLS 3 software, the “bootstrapping” module (5000 iterations), and a two-tailed test to calculate the significance of mediation effects and the path coefficients among latent variables. This method effectively overcomes issues related to non-normal data distribution and small sample sizes, making it a commonly used inferential approach in PLS-SEM. The study employed the VAF method to analyze the strength of mediation effects within the model. VAF measures the proportion of the total effect that is mediated.
(1) Information quality influences acceptance behavior intention through the mediation of attitude toward use.
IQ → ATU = 0.862;
ATU → ABI = 0.219;
IQ → ABI (direct effect) = 0.042;
Indirect effect = 0.862 × 0.219 = 0.18888;
Total effect = 0.18888 (indirect) + 0.042 (direct) = 0.23088.
Conclusion: After incorporating the empirical data into the theoretical model analysis, this study found that information quality influences acceptance behavior intention through the mediation of attitude toward use, representing a “partial mediation.” According to the VAF value, it is close to full mediation (greater than 80%).
(2) Perceived ease of use influences attitude toward use by mediating perceived usefulness.
PE → PU = 0.422;
PU → ATU = 0.226;
PE → ATU (direct) = 0.178;
Indirect effect = 0.422 × 0.226 = 0.095372;
Total effect = 0.095372 (indirect) + 0.178 (direct) = 0.273372.
Conclusion: after incorporating the empirical data into the theoretical model analysis, this study found that perceived ease of use influences attitude toward use through the mediation of perceived usefulness. According to the VAF value, this represents a typical “partial mediation” effect (between 20% and 80%).
(3) Perceived usefulness influences acceptance behavior intention by mediating attitude toward use.
PU → ATU = 0.226;
ATU → ABI = 0.219;
PU → ABI (direct) = 0.037;
Indirect effect = 0.226 × 0.219 = 0.049494;
Total effect = 0.049494 (indirect) + 0.037 (direct) = 0.086494.
Conclusion: after incorporating the empirical data into the theoretical model analysis, this study found that perceived usefulness influences acceptance behavior intention through the mediation of attitude toward use, representing a “partial mediation” effect according to the VAF value.
This study used the VAF method to analyze the strength of mediation effects within the model. The results are summarized in Table 10.

Table 10.
Summary of mediation effect analysis using VAF.
4.3.5. Path Analysis
Path analysis is an advanced application of regression analysis. The results of the path coefficient analysis conducted in this study are shown in Table 9. After compiling the t-values and their statistical significance among the latent variables of the dual-A mathematical model (AMD-AEM), it was found that there are mutual influences among the six research constructs: perceived ease of use (PE), perceived usefulness (PU), information quality (IQ), AI emotion perception (AEP), attitude toward use (ATU), and acceptance behavior intention (ABI). The summary of these findings is presented in Table 11.

Table 11.
Analysis of t-values and statistical significance among latent variables in the AMD-AEM model.
Based on the data in Table 11, for hypothesis H1, “perceived ease of use” predicting “perceived usefulness,” the regression coefficient is t = 17.744 *** (p < 0.001); for H2, “perceived usefulness” predicting “AI emotion perception,” the regression coefficient is t = 9.561 *** (p < 0.001); for H3, “perceived usefulness” predicting “information quality,” the regression coefficient is t = 9.40 *** (p < 0.001); for H4, “perceived usefulness” predicting “attitude toward use,” the regression coefficient is t = 3.319 ** (p < 0.01); for H5, “perceived ease of use” predicting “AI emotion perception,” the regression coefficient is t = 48.897 *** (p < 0.001); for H6, “perceived ease of use” predicting “attitude toward use,” the regression coefficient is t = 2.154 * (p < 0.05); for H7, “perceived ease of use” predicting “information quality,” the regression coefficient is t = 9.011 *** (p < 0.001); for H8, “AI emotion perception” predicting “attitude toward use,” the regression coefficient is t = 2.044 * (p < 0.05); for H9, “AI emotion perception“ predicting “acceptance behavior intention,” the regression coefficient is t = 8.730 *** (p < 0.001); for H10, “information quality” predicting “attitude toward use,” the regression coefficient is t = 84.799 *** (p < 0.001); and for H11, “attitude toward use” predicting “acceptance behavior intention,” the regression coefficient is t = 8.921 *** (p < 0.001). These results indicate that all the above paths are significant and effective predictors.
To further explore the relationships among the factors in the “hypothetical theoretical model”—the dual-A mathematical model (AMD-AEM), we used SmartPLS 3 with bootstrapping to analyze and verify the paths among the dimensions, adopting p < 0.05 as the criterion for statistical significance. The analysis provides data on patients’ acceptance behavior intention to use AI medical diagnosis. The results are presented in Figure 3.
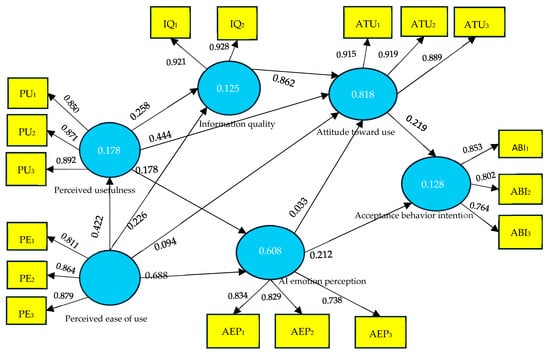
Figure 3.
Acceptance behavior intention toward AI medical diagnosis using mathematical model (AMD-AEM). Source: this study.
4.4. Case Discussion
This section examines the empirical analysis results of the dual-A mathematical model (AMD-AEM). Using survey data, the AMD-AEM model is validated across its six dimensions. The discussion follows this logical sequence: (1) analysis of key predictive factors; (2) exploration of mediation mechanisms; (3) role of AI emotion and information quality; (4) comprehensive evaluation of model explanatory power and goodness-of-fit; and (5) integration of theoretical and practical implications.
4.4.1. Verification and Analysis of Key Predictive Factors
The PLS-SEM model results indicate that both IQ and PU have significant positive effects on the ultimate acceptance behavior intention (ABI) (IQ → ABI, β = 0.862; PU → ABI, β = 0.037), with IQ showing the most significant contribution. This finding supports the importance of PU within the TAM framework. It highlights the central role of information accuracy, transparency, and timeliness in building user trust and behavioral intention in AI medical systems.
From the mathematical model perspective, the structural equation for ABI is:
ABI = β8 · ATU + β9 · IQ + ε4
Empirical data show that β9 = 0.862, the highest among all path coefficients, indicating that IQ has the strongest direct predictive power on ABI. This reflects that the core value of AI medical systems lies in functional benefits (PU), and critically in IQ, information quality (IQ) is not only a source of diagnostic accuracy, which fosters user confidence, it is also a key mechanism for trust and acceptance behavior [8,15].
4.4.2. Logical Linkage and Mathematical Verification of Mediation Mechanisms
This study further examined the mediation effects using bootstrapping and quantified the mediation strength with VAF. We then significantly verified three mediation paths as follows:
IQ → ATU → ABI: indirect effect = 0.1889, VAF = 81.8%, classified as “close to full mediation”;
PU → ATU → ABI: indirect effect = 0.0774, VAF = 57.2%, classified as “moderate partial mediation”;
PE → PU → ATU: indirect effect = 0.149, VAF = 34.9%, classified as “partial mediation.”
These three indirect effects can be expressed mathematically as:
Indirect effect = βi × βj
For example, for IQ → ATU → ABI:
Indirect = βIQ → ATU × βATU → ABI = 0.862 × 0.219 = 0.1889
The results indicate that in addition to directly influencing ABI, information quality (IQ) indirectly strengthens acceptance behavior intention (ABI) by enhancing attitude toward use (ATU), making it an important variable with a dual-path effect.
4.4.3. Dual-Axis Driving Effects of AI Emotion Perception and Information Quality
This study’s model incorporates two exogenous variables not initially included in TAM: AEP and IQ, enhancing the model’s fit to the real medical context. The results are shown below:
Although AEP → ATU (β = 0.033) has a modest contribution, its t-value reaches statistical significance (t = 8.633), indicating a meaningful influence;
PE → AEP (β = 0.037, f2 = 0.991) demonstrates a strong predictive power of PE on AEP.
This suggests that users’ perception of the humanization of AI systems is deeply affected by their system operation experience, influencing their positive attitude toward the system. Particularly in the medical field, “warmth” and “emotional understanding” have become important psychological factors for patients and healthcare providers in accepting AI interfaces. In mathematical modeling, AEP is a function of PE:
AEP = β3 · PE + ε2
This path represents the psychological process explaining how the ease of human–computer interaction transforms into an emotional response, meaning the acceptance threshold of AEP is PE [35,38].
4.4.4. Overall Model Explanatory Power and Goodness-of-Fit Evaluation
By examining the R2 values of the structural model, the R2 for ATU in this study’s model reaches 0.818, indicating very high explanatory power and demonstrating that the model effectively captures the main factors influencing ATU. Additionally, the R2 values for AEP and PU are 0.608 and 0.178, respectively, considered moderate to high.
Moreover, the model fit indices (SRMR = 0.059, NFI = 0.79) indicate that this model is acceptable and even excellent [41], confirming that the dual-A mathematical model (AMD-AEM) not only offers theoretical innovation but also possesses statistical validity.
4.4.5. Theoretical Extension and Practical Implications
Theoretically, this study successfully integrates the core framework of TAM and, through mathematical modeling logic, extends it by introducing two significant external variables—AEP and IQ—to propose an acceptance behavior intention model closely aligned with the healthcare information environment. This fills the gap in TAM research regarding patients’ AEP and IQ transparency in AI medical diagnosis and confirms that the “acceptance behavior intention (ABI)” toward AI medical diagnosis systems involves a multi-level psychological decision-making structure.
From a practical perspective, the model results indicate that enhancing the responsiveness of AEP in AI medical diagnosis system interfaces and improving IQ will help increase healthcare professionals’ and patients’ overall acceptance behavior intention. Therefore, it is recommended that regional medical centers and AI system developers focus on “emotional design” and “information credibility” as strategic directions for system optimization [3,7].
In summary, the construction and empirical validation of the dual-A mathematical model (AMD-AEM) sufficiently demonstrate its effectiveness in explaining the “acceptance behavior intention (ABI)” toward AI medical diagnosis systems. Through the interplay of mathematical and statistical modeling with empirical data interpretation, this study provides a logically rigorous and practical framework linking theory and practice, which is worthy of reference for future innovative healthcare system promotion and policy formulation.
5. Conclusions, Theoretical Contributions, Practical Recommendations, Limitations, and Future Research Suggestions
5.1. Conclusions
This study constructed a novel AMD-AEM mathematical model to explore the acceptance behavior intention of AI-driven medical diagnosis systems. It integrates the core constructs of the TAM and introduces two extended variables: information quality (IQ) and AI emotion perception (AEP). Using partial least squares structural equation modeling (PLS-SEM) combined with bootstrapping iterations analysis (n = 5000), this study rigorously tested the structural validity of the model and the statistical significance of each path coefficient.
The results show that information quality (IQ) is the most critical mediating variable, successfully linking cognitive constructs such as perceived usefulness (PU), perceived ease of use (PE), and AI emotion perception (AEP), thereby influencing acceptance behavior intention (ABI). This study found that when IQ is a mediator between ATU as the independent variable and ABI as the dependent variable, it produces a “close to full mediation” effect (VAF = 81.8%). Additionally, although AEP has a relatively small direct effect on ABI, it remains statistically significant, highlighting the emotional dimension embedded in human–computer interaction.
The overall model fit index, SRMR = 0.083, falls within an acceptable range, confirming that the proposed theoretical model structure is sound. These findings further strengthen the explanatory power of the mathematical model regarding psychological and behavioral science variables.
The theoretical contribution of this study lies in demonstrating how the “cognitive–information” and “emotional–perception” dimensions influence the user’s ABI to the artificial intelligence medical system through the mediating variable of ATU. It also provides a replicable PLS-SEM mathematical modeling analysis procedure for future researchers to quantitatively model behavioral mechanisms in complex and emotionally sensitive technology usage domains.
5.2. Theoretical Contributions
Based on the TAM, this study incorporates two key variables—IQ and AEP—to construct the dual-A mathematical model (AMD-AEM), successfully extending the TAM, TAM2, and UTAUT frameworks. Using empirical survey data, we verified the AMD-AEM model fit. The study found that IQ is a critical mediating variable, producing a “close to full mediation” effect on the path where ATU influences ABI. This result validates the theory that the psychological pathway of “quality–attitude–intention” is a reality. Furthermore, this study employed the variance accounted for (VAF) method to analyze the strength and type of different mediation paths, reinforcing the rigor of mediation inference in PLS-SEM and enhancing the explanatory power of AI medical diagnosis system usage intention, thus contributing to theoretical innovation.
5.3. Practical Recommendations
Through observation and analysis of empirical data from 2380 samples in central Taiwan, we understand that functional factors and emotional conditions influence users’ acceptance of AI medical diagnosis systems. AI medical diagnosis systems that provide trustworthy information quality and establish interactive emotional connections with users are more likely to break down the human–machine barrier and become trusted partners in healthcare. The findings of this study can also be extended to AI agent systems in education and social welfare fields, enhancing human-centered technology acceptance models.
From a practical perspective, this study found that IQ is the most critical predictor influencing the ABI to AI medical diagnosis systems. The results indicate that the “accuracy,” “transparency,” and “reliability” of AI medical diagnosis systems are the primary conditions for fostering public trust and usage. Although AEP has a smaller effect size on ATU and ABI, it remains statistically significant, indicating its potential psychological influence.
Therefore, it is recommended that system designers and development teams focus on creating “emotional interaction interfaces” by developing more humanized feedback and emotion recognition mechanisms to enhance users’ sense of engagement and belonging. From a policy standpoint, regional medical centers are advised to promote AI medical diagnosis strategies centered on “information transparency,” “user-friendly interfaces,” and “harmonization of human–machine emotions.”
5.4. Limitations and Future Research Suggestions
Although the overall model fit of this study is good (SRMR = 0.083), there are three limitations: (1) the data are cross-sectional, which limits the ability to observe the dynamic process of usage intention changes over time; (2) the sample is concentrated in central Taiwan, so caution should be exercised when generalizing the findings to other cultures or regions; (3) user experience data were primarily self-reported due to practical research environment constraints, lacking actual operational logs or interaction data for validation.
Future research can be strengthened in the following areas: (1) employ longitudinal designs to track changes in usage attitudes and intentions over a more extended period; (2) expand samples to multicultural communities to validate the model’s cross-cultural generalizability; (3) integrate backend log data from AI medical diagnosis systems and emotion detection devices to improve consistency between subjective feedback and objective behavior; (4) incorporate variables such as AI ethics, data bias, and transparency mechanisms to shift from human–computer interaction toward a more comprehensive “human–technology–society” systems perspective.
Author Contributions
Conceptualization, K.-C.Y. and S.C.; data curation, S.C.; formal analysis, S.C.; funding acquisition, S.C.; investigation, S.C.; methodology, S.C. and K.-C.Y.; project administration, K.-C.Y.; resources, S.C.; software, S.C.; supervision, K.-C.Y.; validation, S.C.; writing—original draft, S.C.; writing—review and editing, K.-C.Y. and S.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Before conducting the experiments, this research project was submitted to and approved by the Academic Ethics Review Committee of the first author’s affiliated university, National Changhua University of Education.
Informed Consent Statement
We obtained informed consent from all participants involved in the study. The authors informed the participants before the experiment about the voluntary nature of their participation and the confidentiality of the collected information.
Data Availability Statement
The data supporting this study’s findings are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Gou, F.; Liu, J.; Xiao, C.; Wu, J. Research on artificial-intelligence-assisted medicine: A survey on medical artificial intelligence. Diagnostics 2024, 14, 1472. [Google Scholar] [CrossRef] [PubMed]
- Elhaddad, M.; Hamam, S. AI-driven clinical decision support systems: An ongoing pursuit of potential. Cureus 2024, 16, e57728. [Google Scholar] [CrossRef] [PubMed]
- Bajwa, J.; Munir, U.; Nori, A.; Williams, B. Artificial intelligence in healthcare: Transforming the practice of medicine. Future Healthc. J. 2021, 8, e188–e194. [Google Scholar] [CrossRef] [PubMed]
- Varnosfaderani, S.M.; Forouzanfar, M. The role of AI in hospitals and clinics: Transforming healthcare in the 21st century. Bioengineering 2024, 11, 337. [Google Scholar] [CrossRef] [PubMed]
- Jiang, F.; Jiang, Y.; Zhi, H.; Dong, Y.; Li, H.; Ma, S.; Wang, Y.; Dong, Q.; Shen, H.; Wang, Y. Artificial intelligence in healthcare: Past, present and future. Stroke Vasc. Neurol. 2017, 2, 230–243. [Google Scholar] [CrossRef] [PubMed]
- Topol, E.J. High-performance medicine: The convergence of human and artificial intelligence. Nat. Med. 2019, 25, 44–56. [Google Scholar] [CrossRef] [PubMed]
- Sobaih, A.E.E.; Chaibi, A.; Brini, R.; Ibrahim, T.M.A. Unlocking patient resistance to AI in healthcare: A psychological exploration. Eur. J. Investig. Health Psychol. Educ. 2025, 15, 6. [Google Scholar] [CrossRef] [PubMed]
- Miller, R.; Chan, S.H.M.; Whelan, H.; Gregório, J. A comparison of data quality frameworks: A review. Big Data Cogn. Comput. 2025, 9, 93. [Google Scholar] [CrossRef]
- Khare, S.K.; Blanes-Vidal, V.; Nadimi, E.S.; Acharya, U.R. Emotion recognition and artificial intelligence: A systematic review (2014–2023) and research recommendations. Inf. Fusion 2024, 102, 102019. [Google Scholar] [CrossRef]
- Davis, F.D. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q. 1989, 13, 319–340. [Google Scholar] [CrossRef]
- Alowais, S.A.; Alghamdi, S.S.; Alsuhebany, N.; Alqahtani, T.; Alshaya, A.I.; Almohareb, S.N.; Aldairem, A.; Alrashed, M.; Bin Saleh, K.; Badreldin, H.A.; et al. Revolutionizing healthcare: The role of artificial intelligence in clinical practice. BMC Med. Educ. 2023, 23, 689. [Google Scholar] [CrossRef] [PubMed]
- Tsvetanov, F. Integrating AI technologies into remote monitoring patient systems. Eng. Proc. 2024, 70, 54. [Google Scholar] [CrossRef]
- Saklaki, A.; Gardikiotis, A. Exploring Greek students’ attitudes toward artificial intelligence: Relationships with AI ethics, media, and digital literacy. Societies 2024, 14, 248. [Google Scholar] [CrossRef]
- Gomez-Cabello, C.A.; Borna, S.; Pressman, S.; Haider, S.A.; Haider, C.R.; Forte, A.J. Artificial-intelligence-based clinical decision support systems in primary care: A scoping review of current clinical implementations. Eur. J. Investig. Health Psychol. Educ. 2024, 14, 685–698. [Google Scholar] [CrossRef] [PubMed]
- Williamson, S.M.; Prybutok, V. Balancing privacy and progress: A review of privacy challenges, systemic oversight, and patient perceptions in AI-driven healthcare. Appl. Sci. 2024, 14, 675. [Google Scholar] [CrossRef]
- Aksakallı, C.; Daşer, Z. Unlocking EFL learners’ insights into ChatGPT use for L2 writing: The impacts of usage frequency and gender variations. Curr. Psychol. 2025, 44, 7957–7977. [Google Scholar] [CrossRef]
- Venkatesh, V.; Davis, F. A theoretical extension of the technology acceptance model: Four longitudinal field studies. Manag. Sci. 2000, 46, 186–204. [Google Scholar] [CrossRef]
- Ajzen, I. The theory of planned behavior. Organ. Behav. Hum. Decis. Process. 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Holden, R.J.; Karsh, B.T. The technology acceptance model: Its past and its future in health care. J. Biomed. Inform. 2010, 43, 159–172. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.T.; Ramasamy, R.K.; Subbarao, A. Understanding psychosocial barriers to healthcare technology adoption: A review of TAM technology acceptance model and unified theory of acceptance and use of technology and UTAUT frameworks. Healthcare 2025, 13, 250. [Google Scholar] [CrossRef] [PubMed]
- Delone, W.H.; McLean, E.R. The DeLone and McLean model of information systems success: A ten-year update. J. Manag. Inf. Syst. 2003, 19, 9–30. [Google Scholar] [CrossRef]
- Kaiser, G.; Bracke, M.; Göttlich, S.; Kaland, C. Authentic complex modelling problems in mathematics education. In Educational Interfaces Between Mathematics and Industry; Damlamian, A., Rodrigues, J.F., Sträßer, R., Eds.; New ICMI Study Series; Springer International Publishing: Berlin/Heidelberg, Germany, 2013; Volume 16, pp. 287–297. [Google Scholar]
- Hochmuth, R.; Peters, J.; Rønning, F. Modelling mathematics for educational research and practice: A comparison of two theoretical approaches. Educ. Stud. Math. 2025, 118, 153–168. [Google Scholar] [CrossRef]
- Kaiser, G.; Sriraman, B. A global survey of international perspectives on modelling in mathematics education. ZDM Math. Educ. 2006, 38, 302–310. [Google Scholar] [CrossRef]
- Spreitzer, C.; Straser, O.; Zehetmeier, S.; Maaß, K. Mathematical modelling abilities of artificial intelligence tools: The case of ChatGPT. Educ. Sci. 2024, 14, 698. [Google Scholar] [CrossRef]
- Cruz-Gonzalez, P.; He, A.W.-J.; Lam, E.P.; Ng, I.M.C.; Li, M.W.; Hou, R.; Chan, J.N.; Sahni, Y.; Guasch, N.V.; Millwe, T.; et al. Artificial intelligence in mental health care: A systematic review of diagnosis, monitoring, and intervention applications. Psychol. Med. 2025, 55, e18. [Google Scholar] [CrossRef] [PubMed]
- Hair, J.F.; Hult, G.T.M.; Ringle, C.M.; Sarstedt, M.; Danks, N.P.; Ray, S. An introduction to structural equation modeling. In Partial Least Squares Structural Equation Modeling (PLS-SEM) Using R. Classroom Companion: Business; Springer: Cham, Switzerland, 2021. [Google Scholar] [CrossRef]
- Karalis, V.D. The integration of artificial intelligence into clinical practice. Appl. Biosci. 2024, 3, 14–44. [Google Scholar] [CrossRef]
- Schuler, M.S.; Coffman, D.L.; Stuart, E.A. Practical challenges in mediation analysis: A guide for applied researchers. Health Serv. Outcomes Res. Methodol. 2025, 25, 57–84. [Google Scholar] [CrossRef] [PubMed]
- Chang, S.H. Structural Equation Modeling by the Least Squares Method (PLS-SEM): Applying Intelligent PLS; Wunan Publishing House: Taiwan, China, 2021. [Google Scholar]
- Hair, J.; Alamer, A. Partial least squares structural equation modeling (PLS-SEM) in second language and education research: Guidelines using an applied example. Res. Methods Appl. Linguist. 2022, 1, 100027. [Google Scholar] [CrossRef]
- Hair, J.F., Jr.; Black, W.C.; Babin, B.J.; Anderson, R.E. Multivariate Data Analysis, 7th ed.; Prentice Hall Book Co., Ltd.: Saddle River, NJ, USA, 2009. [Google Scholar]
- Edo, O.C.; Ang, D.; Etu, E.E.; Tenebe, I.; Edo, S.; Diekola, O.A. Why do healthcare workers adopt digital health technologies—A cross-sectional study integrating the TAM and UTAUT model in a developing economy. Int. J. Inf. Manag. Data Insights 2023, 3, 100186. [Google Scholar] [CrossRef]
- Saihi, A.; Ben-Daya, M.; Monser, H.; As’ad, R. A structural equation modeling analysis of generative AI chatbots adoption among students and educators in higher education. Comput. Educ. Artif. Intell. 2024, 7, 100274. [Google Scholar] [CrossRef]
- Šimić, G.; Tkalčić, M.; Vukić, V.; Mulc, D.; Španić, E.; Šagud, M.; Olucha-Bordonau, F.E.; Vukšić, M.; R. Hof, P. Understanding emotions: Origins and roles of the amygdala. Biomolecules 2021, 11, 823. [Google Scholar] [CrossRef] [PubMed]
- Elyoseph, Z.; Hadar-Shoval, D.; Asraf, K.; Lvovsky, M. ChatGPT outperforms humans in emotional awareness evaluations. Front. Psychol. 2023, 14, 1199058. [Google Scholar] [CrossRef] [PubMed]
- Elyoseph, Z.; Refoua, E.; Asraf, K.; Lvovsky, M.; Shimoni, Y.; Hadar-Shoval, D. Capacity of generative AI to interpret human emotions from visual and textual data: Pilot evaluation study. JMIR Ment. Health 2024, 11, e54369. [Google Scholar] [CrossRef] [PubMed]
- Hadar-Shoval, D.; Elyoseph, Z.; Lvovsky, M. The plasticity of ChatGPT’s mentalizing abilities: Personalization for personality structures. Front. Psychiatry 2023, 14, 1234397. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Routledge: New York, NY, USA, 1988. [Google Scholar] [CrossRef]
- Kline, R.B. Principles and Practice of Structural Equation Modeling, 4th ed.; The Guilford Press: New York, NY, USA, 2016. [Google Scholar]
- Hair, J.F.; Risher, J.J.; Sarstedt, M.; Ringle, C.M. When to use and how to report the results of PLS-SEM. Eur. Bus. Rev. 2019, 31, 2–24. [Google Scholar] [CrossRef]
- Fornell, C.; Larcker, D.F. Structural equation models with unobservable variables and measurement error: Algebra and statistics. J. Mark. Res. 1981, 18, 382–388. [Google Scholar] [CrossRef]
- Segars, A.; Grover, V. Re-examining perceived ease of use and usefulness: A confirmatory factor analysis. MIS Q. 1993, 17, 517–525. [Google Scholar] [CrossRef]
- Ghozali, I.; Latan, H. Partial Least Squares: Konsep, Teknik dan Aplikasi Menggunakan SmartPLS 3.0 (edisi ke-2); Universitas Diponegoro: Semarang, Indonesia, 2014. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).