Actual vs. Perceived Competency Development—How Can Virtual Patients Impact Pharmacist Pre-Registration Training?
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Demographic Results
3.2. Pre–Post MCQ Results
3.3. Likert Scale Analysis
3.4. Qualitative Analysis
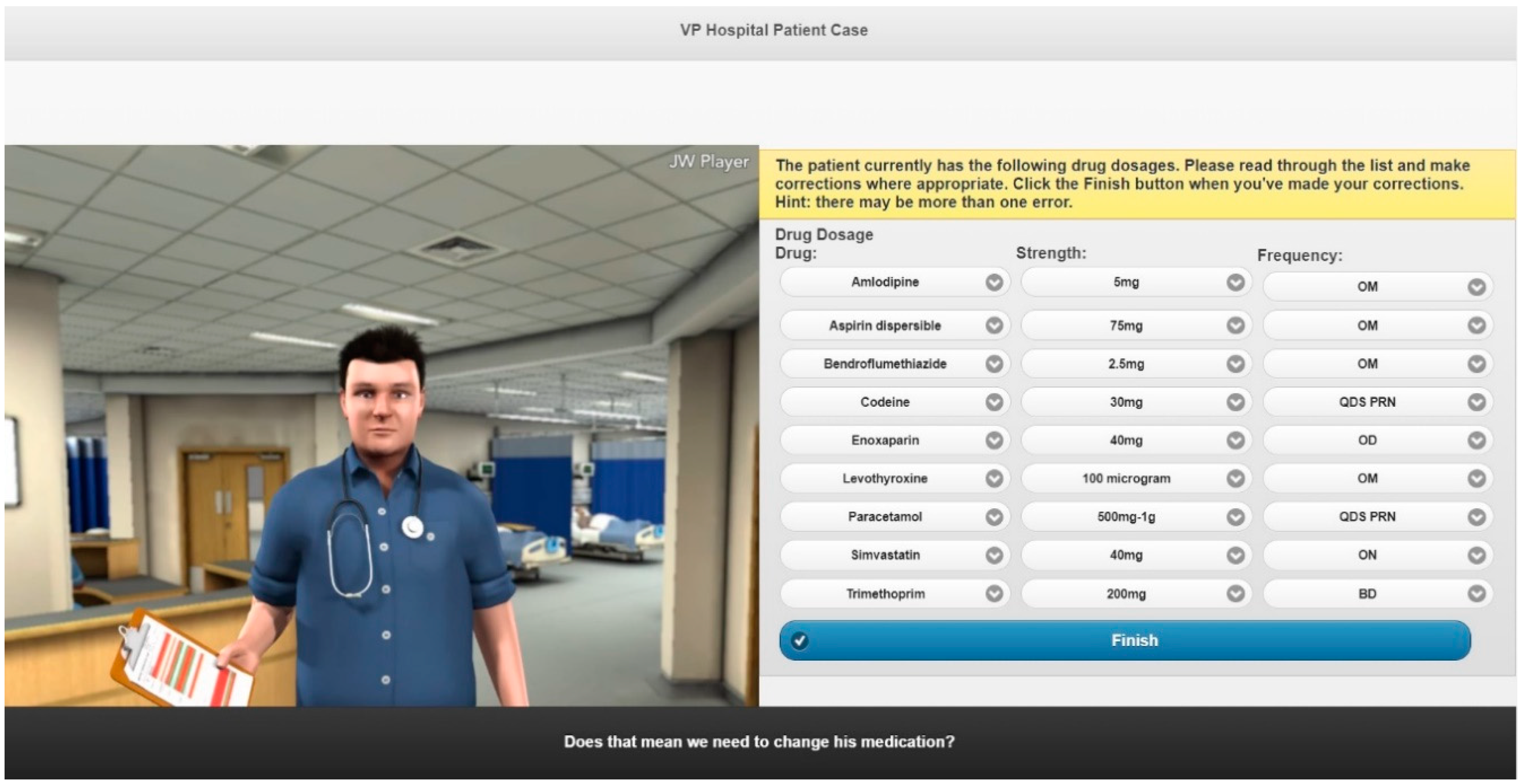
3.4.1. Features of the Learning Tools
3.4.2. Ease of Use of the Learning Tools
3.4.3. Trainee Development
3.4.4. Integration of the Learning Tools
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Blenkinsopp, A.; Marshall, K.; Roberts, G.; Wisher, S.; McNair, K. General Pharmaceutical Council Survey of 2013/2014 Pre-Registration Trainees; The General Pharmaceutical Council: London, UK, 2015. [Google Scholar]
- John, C. The changing role of the pharmacists in the 21st century. Pharm. J. 2018, 300. Available online: https://www.pharmaceutical-journal.com/your-rps/the-changing-role-of-the-pharmacist-in-the-21st-century/20204131.article?firstPass=false (accessed on 25 May 2020). [CrossRef]
- Ker, J.; Bradley, P. Simulation in medical education. In Understanding Medical Education: Evidence, Theory and Practice, 1st ed; Swanwick, T., Ed.; Wiley-Blackwell: London, UK, 2010; pp. 164–180. [Google Scholar] [CrossRef]
- Rosen, K.R. The history of medical simulation. J. Crit. Care 2008, 23, 157–166. [Google Scholar] [CrossRef] [PubMed]
- Seropian, M.A.; Brown, K.; Gavilanes, J.S.; Driggers, B. Simulation: Not just a manikin. J. Nurs. Educ. 2004, 43, 164–170. [Google Scholar] [CrossRef] [PubMed]
- Association of American Medical Colleges (AAMC). Effective Use of Educational Technology in Medical Education. Colloquium on Educational Technology: Recommendations and Guideline for Medical Educators. 2007. Available online: https://store.aamc.org/downloadable/download/sample/sample_id/111/ (accessed on 25 May 2020).
- Cook, D.A.; Triola, M.M. Virtual patients: A critical literature review and proposed next steps. Med. Educ. 2009, 43, 303–311. [Google Scholar] [CrossRef]
- Mori, M.; Macdorman, K.F.; Kageki, N. The uncanny valley [from the field]. IEEE Robot Autom. Mag. 2012, 19, 98–100. [Google Scholar] [CrossRef]
- Poulton, T.; Ellaway, R.H.; Round, J.; Jivram, T.; Kavia, S.; Hilton, S. Exploring the efficacy of replacing linear paper-based patient cases in problem-based learning with dynamic web-based virtual patients: Randomized controlled trial. J. Med. Internet Res. 2014, 16, e240. [Google Scholar] [CrossRef]
- Ellaway, R.H.; Poulton, T.; Smothers, V.; Greene, P. Virtual patients come of age. Med. Teach. 2009, 31, 683–684. [Google Scholar] [CrossRef]
- Cook, D.A.; Erwin, P.J.; Triola, M.M. Computerized virtual patients in health professions education: A systematic review and meta-analysis. Acad. Med. 2010, 85, 1589–1602. [Google Scholar] [CrossRef]
- Kononowicz, A.A.; Woodham, L.A.; Edelbring, S.; Stathakarou, N.; Davies, D.; Saxena, N.; Car, L.T.; Carlstedt-Duke, J.; Car, J.; Zary, N. Virtual patient simulations in health professions education: Systematic review and meta-analysis by the Digital Health Education Collaboration. J. Med. Internet Res. 2019, 21, e14676. [Google Scholar] [CrossRef]
- Issenberg, S.B.; McGaghie, W.C.; Petrusa, E.R.; Lee, G.D.; Scalese, R.J. Features and uses of high-fidelity medical simulations that lead to effective learning: A BEME systematic review. Med. Teach. 2005, 27, 10–28. [Google Scholar] [CrossRef]
- Jabbur-lopes, M.O.; Mesquita, A.R.; Silva, L.M.; De Almeida Neto, A.D.; Lyra, D.P. Virtual patients in pharmacy education. Am. J. Pharm. Educ. 2012, 76, 92. [Google Scholar] [CrossRef] [PubMed]
- Richardson, C.L.; White, S.; Chapman, S. Virtual patient technology to educate pharmacists and pharmacy students on patient communication: A systematic review. BMJ Simul. Technol. Enhanc. Learn. 2019, 5, A39. [Google Scholar] [CrossRef]
- Thompson, J.F.; White, S.; Chapman, S. An evaluation into the effectiveness of virtual patients compared with non-interactive learning techniques in pre-registration training. Int. J. Pharm. Pract. 2016, 24 (Suppl. 1), 27. [Google Scholar] [CrossRef]
- Thompson, J.F.; White, S.; Chapman, S. Can interactive clinical avatars improve pre-registration pharmacists’ knowledge base? Int. J. Pharm. Pract. 2019, 27 (Suppl. 2), 34. [Google Scholar] [CrossRef]
- Taglieri, C.A.; Crosby, S.J.; Zimmerman, K.; Schneider, T.; Patel, D.K. Evaluation of the use of a virtual patient on student competence and confidence in performing simulated clinic visits. Am. J. Pharm. Educ. 2017, 81, 5. [Google Scholar] [CrossRef]
- McDowell, J.; Styles, K.; Sewell, K.; Trinder, P.; Marriott, J.; Maher, S.; Naidu, S. A simulated learning environment for teaching medicine dispensing skills. Am. J. Pharm. Educ. 2016, 80, 1. [Google Scholar] [CrossRef]
- Ferrone, M.; Kebodeaux, C.; Fitzgerald, J.; Holle, L. Implementation of a virtual dispensing simulator to support US pharmacy education. Curr. Pharm. Teach. Learn 2017, 9, 511–520. [Google Scholar] [CrossRef] [PubMed]
- Cláudio, A.P.; Carmo, M.B.; Pinto, V.; Cavaco, A. Virtual humans for training and assessment of self-medication consultation skills in pharmacy students. In Proceedings of the 10th International Conference on Computer Science & Education (ICCSE 2015), Cambridge, UK, 22–24 July 2015; IEEE: Piscataway, NJ, USA, 2015; pp. 175–180. [Google Scholar] [CrossRef]
- Bindoff, I.; Ling, T.; Bereznicki, L.; Westbury, J.; Chalmers, L.; Peterson, G.; Ollington, R. A computer simulation of community pharmacy practice for educational use. Am. J. Pharm. Educ. 2014, 78, 9. [Google Scholar] [CrossRef]
- McFalls, M. Integration of problem-based learning and innovative technology into a self-care course. Am. J. Pharm. Educ. 2013, 77, 6. [Google Scholar] [CrossRef]
- The Accreditation Council for Pharmacy Education (ACPE). Accreditation Standards and Key Elements for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree; ACPE: Chicago, IL, USA, 2015; Available online: https://www.acpe-accredit.org/pdf/Standards2016FINAL.pdf (accessed on 10 July 2020).
- Zlotos, L.; Power, A.; Hill, D.; Chapman, P. A scenario-based virtual patient program to support substance misuse education. Am. J. Pharm. Educ. 2016, 80, 48. [Google Scholar] [CrossRef] [PubMed]
- Thompson, J. Clinical Simulations Using Virtual Patient Avatars for Pre-Registration Pharmacist Training: A Mixed Methods Evaluation. Ph.D. Thesis, Keele University, Keele, UK, June 2018. [Google Scholar]
- Thompson, J.; White, S.; Chapman, S. Validation of a questionnaire to evaluate the design of interactive clinical avatars for pre-registration pharmacist training. J. Med. Internet Res. 2019. [Google Scholar] [CrossRef]
- Shadish, W.R.; Clark, M.H.; Steiner, P.M. Can nonrandomized experiments yield accurate answers? A randomized experiment comparing random and nonrandom assignments. J. Am. Stat. Assoc. 2008, 103, 1334–1344. [Google Scholar] [CrossRef]
- Wilkinson, S. Women with breast cancer talking causes: Comparing content, biographical and discursive analyses. Fem. Psychol. 2000, 10, 431–460. [Google Scholar] [CrossRef]
- Elo, S.; Kyngäs, H. The qualitative content analysis process. J. Adv. Nurs. 2008, 62, 107–115. [Google Scholar] [CrossRef] [PubMed]
- Royal Pharmaceutical Council (RPS). Transforming the Pharmacy Workforce in Great Britain: The RPS Vision. 2015. Available online: https://www.rpharms.com/Portals/0/RPS%20document%20library/Open%20access/Support/Workforce%20and%20Education/transforming-the-pharmacy-workforce-in-great-britain.pdf (accessed on 25 May 2020).
- NHS England. General Practice Forward View. 2016. Available online: https://www.england.nhs.uk/wp-content/uploads/2016/04/gpfv.pdf (accessed on 25 May 2020).
- Rosenthal, M.; Austin, Z.; Tsuyuki, R.T. Are pharmacists the ultimate barrier to pharmacy practice change? Can. Pharm. J. 2010, 143, 37–42. [Google Scholar] [CrossRef]
- Miller, G.E. The assessment of clinical skills/competence/performance. Acad. Med. 1990, 65, 63–67. [Google Scholar] [CrossRef]
- Kolb, A.Y.; Kolb, D.A. Learning styles and learning spaces: Enhancing experiential learning in higher education. Acad. Learn. Educ. 2005, 4, 193–212. [Google Scholar] [CrossRef]
- McGaghie, W.C.; Issenberg, S.B.; Petrusa, E.R.; Scalese, R.J. A critical review of simulation-based medical education research: 2003–2009. Med. Educ. 2010, 44, 50–63. [Google Scholar] [CrossRef]
- Ellaway, R.; Poulton, T.; Fors, U.; McGee, J.B.; Albright, S. Building a virtual patient commons. Med. Teach. 2008, 30, 170–174. [Google Scholar] [CrossRef]
- Kelley, K.W.; Fowlin, J.M.; Tawfik, A.A.; Anderson, M.C. The role of using formative assessments in problem-based learning: A health sciences education perspective. Interdiscip. J. Probl. Based Learn. 2019, 13, 6. [Google Scholar] [CrossRef]
- Salinitri, F.D.; O’Connell, M.B.; Garwood, C.L.; Lehr, V.T.; Abdallah, K. An Objective Structured Clinical Examination to assess problem-based learning. Am. J. Pharm. Educ. 2012, 76, 44. [Google Scholar] [CrossRef] [PubMed]
- Krathwohl, D.R. A revision of Bloom’s taxonomy: An overview. Theory Pract. 2002, 41, 212–218. [Google Scholar] [CrossRef]
- Huang, G.; Reynolds, R.; Candler, C. Virtual patient simulation at U.S. and Canadian medical schools. Acad. Med. 2007, 82, 446–451. [Google Scholar] [CrossRef]
- Farrell, B.; Ward, N.; Jennings, B.; Jones, C.; Jorgenson, D.; Gubbels-Smith, A.; Dolovich, L.; Kennie, N. Participation in online continuing education. Int. J. Pharm. Pract. 2016, 24, 60–71. [Google Scholar] [CrossRef]
- Hassell, K. GPhC Register Analysis 2011; General Pharmaceutical Council: London, UK, 2011. [Google Scholar]


| Stage of Research | No. of Participants (% RR) | ||
|---|---|---|---|
| VP Group | NI Group | Overall | |
| Consented | 83 | 82 | 165 |
| Case 1 Completion | 60 (72%) | 66 (80%) | 126 (76%) |
| Case 2 Completion | 42 (51%) | 47 (57%) | 89 (54%) |
| Case 3 Completion | 27 (33%) | 36 (44%) | 63 (38%) |
| Questionnaire Completion | 24 (29%) | 32 (39%) | 56 (34%) |
| Case Study | Mean (SD) Knowledge Improvement VP Group (Pre–Post) | Mean (SD) Knowledge Improvement NI Group (Pre–Post) | Independent t-Test VP vs. NI Knowledge Improvement | Independent t-Test Hospital vs. Community Knowledge Improvement |
|---|---|---|---|---|
| 1 | 2.18 (1.92) a | 2.11 (1.96) a | t (100) = 0.183 | t (72) = 1.898 b |
| 2 | 1.37 (1.67) b | 1.54 (1.63) b | t (63) = −0.429 | t (63) = −0.249 a |
| 3 | 1.17 (1.44) b | 1.24 (2.21) | t (46) = −1.665 | t (46) = −1.824 b |
| Likert Statement | VP Median Score (IQR) | NI Median Score (IQR) | Percentage Agree/Strongly Agree | Percentage Disagree/Strongly Disagree | ||
|---|---|---|---|---|---|---|
| VP | NI | VP | NI | |||
| The case studies provided a realistic patient simulation | 4 (3–4) | 3 (3–4) | 58.3% | 46.9% | 4.2% | 12.5% |
| When completing the case studies I felt as if I were the pharmacist caring for this patient | 4 (3–5) | 4 (3–4) | 66.7% | 53.1% | 16.7% | 15.6% |
| When completing the case studies I felt I had to make the same decisions as a pharmacist would in real life | 4 (4–5) | 4 (3–5) | 79.2% | 56.3% | 8.3% | 6.3% |
| The case studies were interesting | 4 (4–5) | 4 (3–5) | 83.3% | 68.8% | 0% | 6.3% |
| The case studies were enjoyable | 4 (4–5) | 4 (3–4) | 79.2% | 62.5% | 8.3% | 9.4% |
| The difficulty of the case studies were appropriate for my level of training | 4 (4–5) | 4 (4–5) | 87.5% | 78.1% | 8.3% | 6.3% |
| The feedback I received was adequate for my needs | 4 (3–4.25) | 4 (3–4.25) | 66.7% | 68.8% | 8.3% | 9.4% |
| The objectives for the case studies were clear and easy to understand | 4 (3–4.25) | 4 (4–5) | 62.5% | 78.1% | 16.7% | 6.3% |
| I was able to access the case studies at my convenience | 4.5 (3.75–5) | 4.5 (4–5) | 75% | 78.1% | 8.3% | 3.1% |
| The case studies helped develop my clinical reasoning skills | 4 (4–5) | 4 (3–4) | 79.2% | 65.6% | 16.7% | 6.3% |
| The case studies helped develop my problem-solving and decision-making skills | 4 (3–5) | 4 (3–4) | 66.7% | 65.6% | 12.5% | 6.3% |
| The case studies have helped me to put theory into practice | 4 (3.75–5) | 4 (3–5) | 75% | 56.3% | 8.3% | 6.3% |
| I am confident I am developing skills from the case studies that will be required in practice | 4 (3–4) | 4 (3–5) | 66.7% | 59.4% | 12.5% | 6.3% |
| I am confident I am gaining knowledge from the case studies that will be required in practice | 4 (4–5) | 4 (3–5) | 87.5% | 65.6% | 0% | 6.3% |
| It is my responsibility to learn what I need to know from the case studies | 5 (4–5) | 4.5 (3.75–5) | 91.7% | 75% | 0% | 3.1% |
| Completing the case studies has improved my confidence for the pre-registration exam | 3 (3–4) | 3 (3–4) | 45.83% | 46.9% | 16.7% | 15.6% |
| I feel better prepared to care for real-life patients | 4 (3–4) | 3 (3–4) | 62.5% | 40.6% | 16.7% | 12.5% |
| I feel more confident about collaborating with patients and other healthcare professionals | 3 (2–4) | 3 (3–4) | 41.7% | 34.4% | 37.4% | 18.8% |
| The case studies have increased my confidence about practicing as a pharmacist | 3 (3–4) | 3 (3–4) | 45.8% | 43.8% | 16.7% | 6.3% |
| Overall, the experience has enhanced my learning | 4 (3–5) | 4 (4–5) | 70.8% | 78.1% | 8.3% | 3.1% |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thompson, J.; White, S.; Chapman, S. Actual vs. Perceived Competency Development—How Can Virtual Patients Impact Pharmacist Pre-Registration Training? Pharmacy 2020, 8, 138. https://doi.org/10.3390/pharmacy8030138
Thompson J, White S, Chapman S. Actual vs. Perceived Competency Development—How Can Virtual Patients Impact Pharmacist Pre-Registration Training? Pharmacy. 2020; 8(3):138. https://doi.org/10.3390/pharmacy8030138
Chicago/Turabian StyleThompson, Jessica, Simon White, and Stephen Chapman. 2020. "Actual vs. Perceived Competency Development—How Can Virtual Patients Impact Pharmacist Pre-Registration Training?" Pharmacy 8, no. 3: 138. https://doi.org/10.3390/pharmacy8030138
APA StyleThompson, J., White, S., & Chapman, S. (2020). Actual vs. Perceived Competency Development—How Can Virtual Patients Impact Pharmacist Pre-Registration Training? Pharmacy, 8(3), 138. https://doi.org/10.3390/pharmacy8030138







