A Systematic Review of Randomized Controlled Trials of Telehealth and Digital Technology Use by Community Pharmacists to Improve Public Health
Abstract
1. Introduction
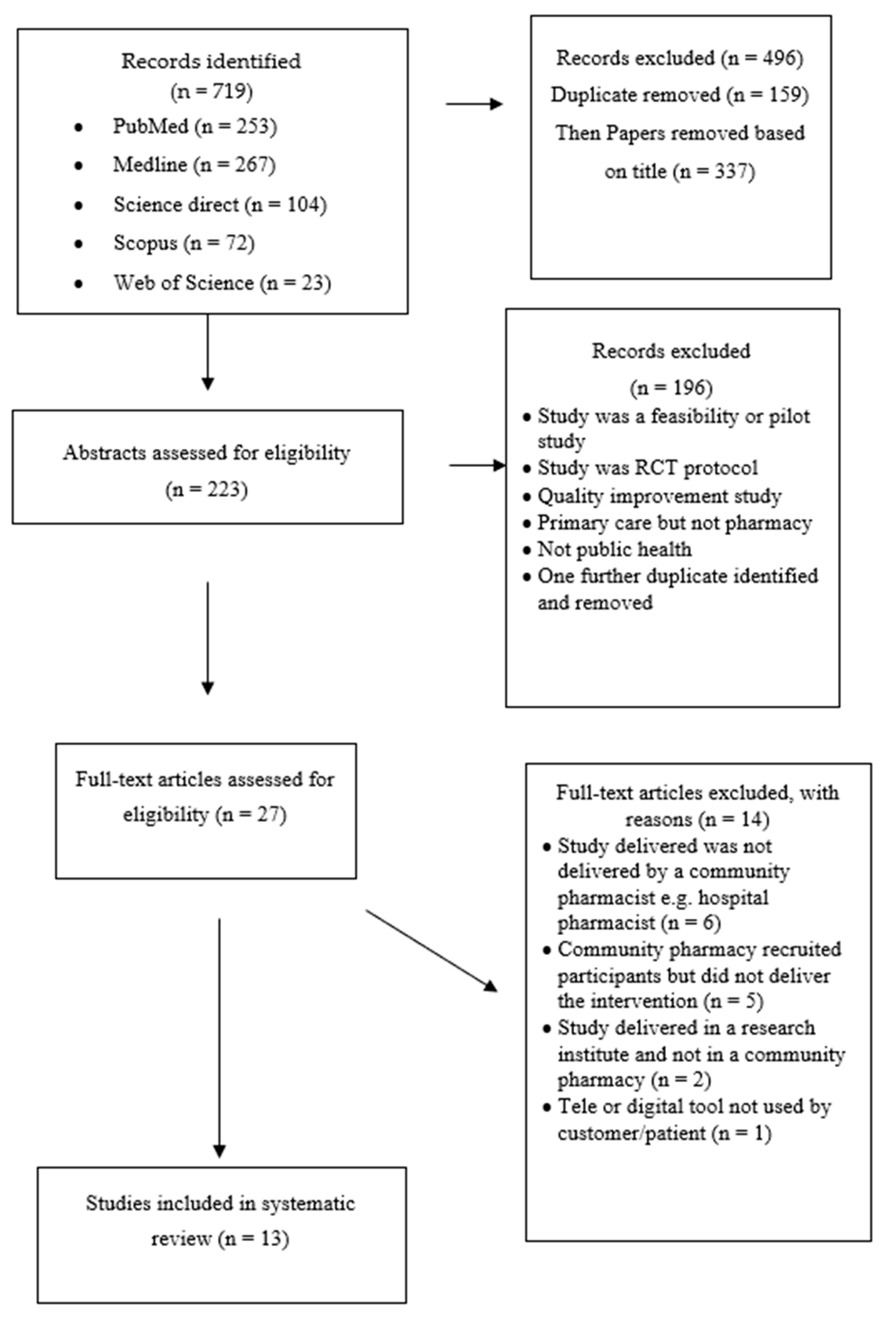
2. Materials and Methods
2.1. Design of the Study
2.2. Data Sources and Search Terms
2.3. Study Selection and Definitions
2.4. Data Extraction
2.5. Methodological Quality of RCTs and Risk of Study Bias
3. Results
3.1. Public Health Topics
3.1.1. Vaccination Uptake
3.1.2. Smoking Cessation
3.1.3. Medication Adherence
3.1.4. Medication Counseling
3.1.5. Hypertension Management
3.2. Methodological Quality of RCTs and Risk of Study Bias
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- WHO. Coronavirus Disease 2019. WHO Website. 2020. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed on 1 August 2020).
- Ung, C.O.L. Community pharmacist in public health emergencies: Quick to action against the coronavirus 2019-nCoV outbreak. In Research in Social and Administrative Pharmacy; Elsevier: Amsterdam, The Netherlands, 2020; Volume 16, pp. 583–586. [Google Scholar]
- Liu, S.; Luo, P.; Tang, M.; Hu, Q.; Polidoro, J.P.; Sun, S.; Gong, Z. Providing pharmacy services during the coronavirus pandemic. Int. J. Clin. Pharm. 2020, 42, 299–304. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Disease Burden and Mortality Estimates. WHO, 2018; pp. 1–65. Available online: https://www.who.int/healthinfo/global_burden_disease/estimates/en/ (accessed on 1 August 2020).
- World Health Organization. Noncommunicable Diseases [Internet]. WHO, 2018. Available online: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases (accessed on 1 August 2020).
- World Health Organization. Global Action Plan for the Prevention and Control of Noncommunicable diseases 2013–2020 [Internet]. Available online: www.who.int (accessed on 29 May 2020).
- Chaloupka, F.J.; Yurekli, A.; Fong, G.T. Tobacco taxes as a tobacco control strategy. Tob. Control 2012, 21, 172–180. [Google Scholar] [CrossRef] [PubMed]
- Cabrera Escobar, M.A.; Veerman, J.L.; Tollman, S.M.; Bertram, M.Y.; Hofman, K.J. Evidence that a tax on sugar sweetened beverages reduces the obesity rate: A meta-analysis. BMC Public Health 2013, 13, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Blanchette, J.G.; Lira, M.C.; Heeren, T.C.; Naimi, T.S. Alcohol Policies in U.S. States, 1999–2018. J. Stud. Alcohol Drugs 2020, 81, 58–67. [Google Scholar] [CrossRef]
- Cappelli, D.P.; Mobley, C.C. Association between Sugar Intake, Oral Health, and the Impact on Overall Health: Raising Public Awareness. Curr. Oral Health Rep. 2017, 4, 176–183. [Google Scholar] [CrossRef]
- Gudka, S.; Afuwape, F.E.; Wong, B.; Yow, X.L.; Anderson, C.; Clifford, R.M. Chlamydia screening interventions from community pharmacies: A systematic review. Sex Health 2013, 10, 229. [Google Scholar] [CrossRef]
- Kirkdale, C.L.; Nebout, G.; Megerlin, F.; Thornley, T. Benefits of pharmacist-led flu vaccination services in community pharmacy. Ann. Pharm Françaises 2017, 75, 3–8. [Google Scholar] [CrossRef]
- Essack, S.; Bell, J.; Shephard, A. Community pharmacists-Leaders for antibiotic stewardship in respiratory tract infection. J. Clin. Pharm. Ther. 2018, 43, 302–307. [Google Scholar] [CrossRef]
- Krass, I.; Hourihan, F.; Chen, T. Health promotion and screening for cardiovascular risk factors in NSW: A community pharmacy model. Health Promot. J. Aust. 2003, 14, 101–107. [Google Scholar] [CrossRef]
- Crilly, P.; Hassanali, W.; Khanna, G.; Matharu, K.; Patel, D.; Patel, D.; Rahman, F.; Kayyali, R. Community pharmacist perceptions of their role and the use of social media and mobile health applications as tools in public health. Res. Soc. Adm. Pharm. 2018. [Google Scholar] [CrossRef]
- Zomahoun, H.T.V.; Guénette, L.; Grégoire, J.P.; Lauzier, S.; Lawani, A.M.; Ferdynus, C.; Huiart, L.; Moisan, J. Effectiveness of motivational interviewing interventions on medication adherence in adults with chronic diseases: A systematic review and meta-analysis. Int. J. Epidemiol. 2017, 46, 589–602. [Google Scholar] [CrossRef] [PubMed]
- Dhital, R.; Norman, I.; Whittlesea, C.; Murrells, T.; Mccambridge, J. The effectiveness of brief alcohol interventions delivered by community pharmacists: Randomized controlled trial. Addiction 2015, 110, 1586–1594. [Google Scholar] [CrossRef] [PubMed]
- Boardman, H.F.; Avery, A.J. Effectiveness of a community pharmacy weight management programme. Int. J. Clin. Pharm. 2014, 36, 800–806. [Google Scholar] [CrossRef] [PubMed]
- Saba, M.; Diep, J.; Saini, B.; Dhippayom, T. Meta-analysis of the effectiveness of smoking cessation interventions in community pharmacy. J. Clin. Pharm. Ther. 2014, 39, 240–247. [Google Scholar] [CrossRef]
- Michie, L.; Cameron, S.T.; Glasier, A.; Chen, Z.E.; Milne, D.; Wilson, S. Provision of contraception after emergency contraception from the pharmacy: Evaluating the acceptability of pharmacy for providing sexual and reproductive health services. Public Health 2016, 135, 97–103. [Google Scholar] [CrossRef]
- Twigg, M.J.; Wright, D.J.; Thornley, T.; Haynes, L. Community pharmacy type 2 diabetes risk assessment: Demographics and risk results. Int. J. Pharm. Pract. 2015, 23, 80–82. [Google Scholar] [CrossRef]
- Rai, G.K.; Wood, A. Effectiveness of community pharmacies in improving seasonal influenza uptake-an evaluation using the Donabedian framework. J. Public Health 2018, 40, 359–365. [Google Scholar] [CrossRef]
- Kovačević, M.; Ćulafić, M.; Jovanović, M.; Vučićević, K.; Kovačević, S.V.; Miljković, B. Impact of community pharmacists’ interventions on asthma self-management care. Res. Soc. Adm. Pharm. 2018, 14, 603–611. [Google Scholar] [CrossRef]
- Presley, B.; Groot, W.; Pavlova, M. Pharmacy-led interventions to improve medication adherence among adults with diabetes: A systematic review and meta-analysis. In Research in Social and Administrative Pharmacy; Elsevier: Amsterdam, The Netherlands, 2019; Volume 15, pp. 1057–1067. [Google Scholar]
- Rupp, M.T. Improving medication delivery and counseling in community pharmacy. J. Am. Pharm. Assoc. 2009, 49, 585. [Google Scholar] [CrossRef]
- Crilly, P.; Jair, S.; Mahmood, Z.; Khan, A.M.; Munir, A.; Osei-bediako, I.; Samir, M.; Kayyli, R. Public views of different sources of health advice: Pharmacists, social media and mobile health applications. Int. J. Pharm. Pract. 2018, 27, 88–95. [Google Scholar] [CrossRef]
- Kayyali, R.; Hesso, I.; Mahdi, A.; Hamzat, O.; Adu, A.; Nabhani Gebara, S. Telehealth: Misconceptions and experiences of healthcare professionals in England. Int. J. Pharm. Pract. 2017, 25, 203–209. [Google Scholar] [CrossRef] [PubMed]
- Jeminiwa, R.; Hohmann, L.; Qian, J.; Garza, K.; Hansen, R.; Fox, B.I. Impact of eHealth on medication adherence among patients with asthma: A systematic review and meta-analysis. Respir. Med. 2019, 149, 59–68. [Google Scholar] [CrossRef] [PubMed]
- Dumit, E.M.; Novillo-Ortiz, D.; Contreras, M.; Velandia, M.; Danovaro-Holliday, M.C. The use of eHealth with immunizations: An overview of systematic reviews. Vaccine 2018, 36, 7923–7928. [Google Scholar] [CrossRef] [PubMed]
- McCarroll, R.; Eyles, H.; Ni Mhurchu, C. Effectiveness of mobile health (mHealth) interventions for promoting healthy eating in adults: A systematic review. Prev. Med. 2017, 105, 156–168. [Google Scholar] [CrossRef]
- Greenwood, D.A.; Gee, P.M.; Fatkin, K.J.; Peeples, M. A Systematic Review of Reviews Evaluating Technology-Enabled Diabetes Self-Management Education and Support. J. Diabetes Sci. Tech. 2017, 11, 1015–1027. [Google Scholar] [CrossRef]
- McIntosh, J.R.D.; Jay, S.; Hadden, N.; Whittaker, P.J. Do E-health interventions improve physical activity in young people: A systematic review. Public Health 2017, 148, 140–148. [Google Scholar] [CrossRef]
- Baskerville, N.B.; Azagba, S.; Norman, C.; McKeown, K.; Brown, K.S. Effect of a Digital Social Media Campaign on Young Adult Smoking Cessation. Nicotine Tob. Res. 2016, 18, 351–360. [Google Scholar] [CrossRef]
- Benetoli, A.; Chen, T.F.; Aslani, P. The use of social media in pharmacy practice and education. Res. Soc. Adm. Pharm. 2015, 11, 1–46. [Google Scholar] [CrossRef]
- Chang, T.; Chopra, V.; Zhang, C.; Woolford, S.J. The role of social media in online weight management: Systematic review. J. Med. Internet Res. 2013, 15, e262. [Google Scholar] [CrossRef]
- Crilly, P.; Jair, S.; Mahmood, Z.; Moin Khan, A.; Munir, A.; Osei-Bediako, I.; Samir, M.; Kayyli, R. A survey to establish Greater London public perceptions of the use of digital technology and the role of the pharmacist when looking for health information. Int. J. Pharm. Pract. 2017, 25, 4–39. [Google Scholar]
- Napolitano, M.A.; Hayes, S.; Bennett, G.G.; Ives, A.K.; Foster, G.D. Using facebook and text messaging to deliver a weight loss program to college students. Obesity 2013, 21, 25–31. [Google Scholar] [CrossRef] [PubMed]
- Turner-McGrievy, G.; Tate, D. Tweets, Apps, and Pods: Results of the 6-month Mobile Pounds Off Digitally (Mobile POD) randomized weight-loss intervention among adults. J. Med. Internet Res. 2011, 13, e120. [Google Scholar] [CrossRef] [PubMed]
- Ratzan, S.; Parker, R. Introduction. In National Library of Medicine Current Bibliographies in Medicine: Health Literacy; Seldon, C., Zorn, M., Ratzan, S., Parker, R., Eds.; National Institutes of Health: Bethesda, MD, USA, 2000. [Google Scholar]
- Gilster, P. Digital Literacy; Glister, P., Ed.; Wiley Computer Publisher: New York, NY, USA, 1997. [Google Scholar]
- Mackert, M.; Mabry-Flynn, A.; Champlin, S.; Donovan, E.E.; Pounders, K. Health Literacy and Health Information Technology Adoption: The Potential for a New Digital Divide. J. Med. Internet Res. 2016, 18, e264. [Google Scholar] [CrossRef] [PubMed]
- MacLure, K.; Stewart, D. Digital literacy knowledge and needs of pharmacy staff: A systematic review. J. Innov. Health Inform. 2016, 23, 560. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Jadad, A.R.; Moore, R.A.; Carroll, D.; Jenkinson, C.; Reynolds, D.J.M.; Gavaghan, D.J.; McQuay, H.J. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control Clin. Trials 1996, 17, 1–12. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbet, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366. [Google Scholar] [CrossRef]
- Stolpe, S.; Choudhry, N.K. Effect of Automated Immunization Registry-Based Telephonic Interventions on Adult Vaccination Rates in Community Pharmacies: A Randomized Controlled Trial. J. Manag. Care Spec. Pharm. 2019, 25, 989–994. [Google Scholar] [CrossRef]
- Hess, R. Impact of automated telephone messaging on zoster vaccination rates in community pharmacies. J. Am. Pharm. Assoc. 2013, 53, 182–187. [Google Scholar] [CrossRef]
- Rickles, N.M.; Svarstad, B.L.; Statz-Paynter, J.L.; Taylor, L.V.; Kobak, K.A. Pharmacist telemonitoring of antidepressant use: Effects on pharmacist-patient collaboration. J. Am. Pharm. Assoc. 2005, 45, 344–353. [Google Scholar] [CrossRef]
- Odegard, P.S.; Christensen, D.B. MAP study: RCT of a medication adherence program for patients with type 2 diabetes. J. Am. Pharm. Assoc. 2012, 52, 753–762. [Google Scholar] [CrossRef] [PubMed]
- Margolis, K.L.; Asche, S.E.; Dehmer, S.P.; Bergdall, A.R.; Green, B.B.; Sperl-Hillen, J.A.M.; Nyboer, R.A.; Pawloski, P.A.; Maciosek, M.V.; Trower, N.K.; et al. Long-term Outcomes of the Effects of Home Blood Pressure Telemonitoring and Pharmacist Management on Blood Pressure Among Adults With Uncontrolled Hypertension: Follow-up of a Cluster Randomized Clinical Trial. JAMA Netw. Open 2018, 1, e181617. [Google Scholar] [CrossRef] [PubMed]
- Margolis, K.L.; Asche, S.E.; Bergdall, A.R.; Dehmer, S.P.; Groen, S.E.; Kadrmas, H.M.; Kerby, T.J.; Klotzle, K.J.; Maciosek, M.V.; Michels, R.D.; et al. Effect of home blood pressure telemonitoring and pharmacist management on blood pressure control a cluster randomized clinical trial. JAMA J. Am. Med. Assoc. 2013, 310, 46–56. [Google Scholar] [CrossRef] [PubMed]
- Nietert, P.J.; Tilley, B.C.; Zhao, W.; Edwards, P.F.; Wessell, A.M.; Mauldin, P.D.; Polk, P.P. Two pharmacy interventions to improve refill persistence for chronic disease medications a randomized, controlled trial. Med. Care 2008, 47, 32–40. [Google Scholar] [CrossRef]
- Elliott, R.A.; Boyd, M.J.; Tanajewski, L.; Barber, N.; Gkountouras, G.; Avery, A.J.; Mehta, R.; Davies, J.E.; Salema, N.-E.; Craig, C.; et al. “New Medicine Service”: Supporting adherence in people starting a new medication for a long-term condition: 26-week follow-up of a pragmatic randomised controlled trial. BMJ Qual. Saf. 2020, 29, 286–295. [Google Scholar] [CrossRef]
- Burford, O.; Jiwa, M.; Carter, O.; Parsons, R.; Hendrie, D. Internet-based photoaging within australian pharmacies to promote smoking cessation: Randomized controlled trial. J. Med. Internet Res. 2013, 15, e64. [Google Scholar] [CrossRef]
- Kosse, R.C.; Bouvy, M.L.; de Vries, T.W.; Koster, E.S. Effect of a mHealth intervention on adherence in adolescents with asthma: A randomized controlled trial. Respir. Med. 2019, 149, 45–51. [Google Scholar] [CrossRef]
- Kooy, M.J.; van Geffen, E.C.G.; Heerdink, E.R.; van Dijk, L.; Bouvy, M.L. Patients’ general satisfaction with telephone counseling by pharmacists and effects on satisfaction with information and beliefs about medicines: Results from a cluster randomized trial. Patient Educ. Couns. 2015, 98, 797–804. [Google Scholar] [CrossRef]
- Kooij, M.J.; Heerdink, E.R.; van Dijk, L.; van Geffen, E.C.G.; Belitser, S.V.; Bouvy, M.L. Effects of telephone counseling intervention by pharmacists (TelCIP) on medication adherence; Results of a cluster randomized trial. Front. Pharmacol. 2016, 7, 269. [Google Scholar] [CrossRef]
- Beaucage, K.; Lachance-Demers, H.; Ngo, T.T.-T.; Vachon, C.; Lamarre, D.; Guévin, J.-F.; Pharm, M.B.A.; Martineau, A.; Desroches, D.; Brassard, J.; et al. Telephone follow-up of patients receiving antibiotic prescriptions from community pharmacies. Am. J. Heal Pharm. 2006, 63, 557–563. [Google Scholar] [CrossRef]
- Pharmaceutical Services Negotiating Committee. New Medicine Service (NMS) [Internet]. PSNC Webpage. 2020. Available online: https://psnc.org.uk/services-commissioning/advanced-services/nms/ (accessed on 29 May 2020).
- Elliott, R.A.; Barber, N.; Clifford, S.; Horne, R.; Hartley, E. The cost effectiveness of a telephone-based pharmacy advisory service to improve adherence to newly prescribed medicines. Pharm. World Sci. 2008, 8, 17–23. [Google Scholar] [CrossRef]
- Cain, J.; Romanelli, F.; Fox, B. Pharmacy, social media, and health: Opportunity for impact. J. Am. Pharm. Assoc. 2010, 50, 745–751. [Google Scholar] [CrossRef] [PubMed]
- Kayyali, R.; Crilly, P. Digital Media in Pharmacy Public Health. Pharm. Pharmacol. Int. J. 2016, 4, 00069. [Google Scholar] [CrossRef]
- Shcherbakova, N.; Shepherd, M. Community pharmacists, Internet and social media: An empirical investigation. Res. Soc. Adm. Pharm. 2014, 10, 75–85. [Google Scholar] [CrossRef]
- Lam, A. Practice innovations: Delivering medication therapy management services via videoconference interviews. Consult. Pharm. 2011, 26, 764–773. [Google Scholar] [CrossRef] [PubMed]
- Crilly, P.; Zein, M.; Kayyali, R. The digital literacy skills of the community pharmacy workforce. Int. J. Pharm. Pract. 2019, 27, 6–31. [Google Scholar]
| Study Author and Year Research Completed | Intervention Design and Study Population (I = Intervention and C = Control) | Primary Outcome | Results | Risk of Bias (RoB-2) | |||||
| Study Location | Duration | Tele or Digital Medium Used | N | Mean Age (Years) | % Female | ||||
| Vaccination Uptake | |||||||||
| Hess (2013) [47] | USA | 14-months | Automated telephonic prompt | I = 5599 C = 6383 | I = 72.9 C = 71.8 | Not stated | The number of HZ vaccines administererd to study participants (adults 60 years and over) during the time period of March to May 2007 | In the intervention group, 146 vaccinations were administered to the study participants. In the control group, 46 vaccinations were administered. This accounted for HZ vaccination rates of 2.6% vs 0.72% for intervention and control groups, respectively, representing a significant improvement in vaccination rates. | Some concerns |
| Participants: Adults over 60 years who were not vaccinated for herpes zoster (HZ) Intervention: Participants received a 30-s automated telephone prompt advertising that they should speak to their pharamcist about their risks of HZ and the availability of the vaccine. Control: Did not receive a telephone prompt | |||||||||
| Stolpe and Choudhry (2019) [46] | USA | 10-months | Automated telephonic prompt | I = 11,009 C = 10,962 | I = 63.2 C = 63.3 | I = 56.9 C = 57.7 | The proportion of study participants who were administered at least one of their missed vaccines between the time period of March 2015 and January 2016. | In the intervention group, 236 vaccinations were administered to the study participants. In the control group, 225 vaccinations were administered. This accounted for vaccination rates of 2.14% and 2.05% for intervention and control groups respecitvely. This was not a significant differrence. Only 33.3% of intervention participants listened to the full telephone call. Of those who did, they were more likely to get vaccinated than controls. | Some concerns |
| Participants: Adults aged over 19 years old who were scheduled to have an automated telephone call from their community pharmay, e.g., to remind them to refill their medication Intervention: Participants received an additional prompt within the call and were offered either pneumococcal or HZ vaccine or both, depending on their vaccination record. Three call attempts were made in total. Control: Received their scheduled automated telephone call but without the additional vaccination offer. | |||||||||
| Study Author and Year Research Completed | Intervention Design and Study Population (I = Intervention and C = Control) | Primary Outcome | Results | Risk of Bias (RoB-2) | |||||
| Study Location | Duration | Tele or Digital Medium Used | N | Mean Age (Years) | % Female | ||||
| Smoking Cessation | |||||||||
| Burford et al. (2013) [54] | Australia | 12-months | Internet-based photo-aging software | I = 80 C = 80 | I = 24.2 C = 25.1 | I = 55 C = 45 | The number of successful smoking quit attempts, confirmed by carbon monoxide (CO) breath test, measured at 1, 3 and 6 month follow-ups. In addition, nicotine dependence was measured via the Fagerström scale | 11 (13.8%) of intervention group were non-smokers at 6 months vs 1 (1.3%) of control group (p = 0.003). This was significant and confirmed by CO monitor. Change in Fagerström score from baseline at 6 months was −0.26 for control group and −1.88 for intervention group. 14% of the control group moved to a lower category of the Fagerström score versus 51% of the intervention group (p < 0.001) | Some concerns |
| Participants: Adults aged 18–30 years old, who were smokers, without facial hair, who did not suffer from body dysmorphia and who did not take nicotine replacement therapy or medication for nicotine dependence. Intervention: Participants received 2 min of smoking cessation advice from a pharmacist. In addition, Face aging software, APRIL, was used to create aged images of faces from a digital photograph. In addition to the using the normal wrinkling algorithm, the images were also adjusted to compare how participants would age as a smoker versus as a non-smoker. Control: Participants received 2 min of smoking cessation advice from a pharmacist | |||||||||
| Medication Adherence | |||||||||
| Rickles et al. (2005) [48] | USA | 12-months | Telephone call | I = 31 C = 32 | I = 37.8 C = 37.5 | I = 80.6 C = 87.5 | The number of times study patients spoke to their pharmacist about their new medication (whether during intervention call or when visiting the pharmacy). In addition, changes in patient knowledge, beliefs, adherence, and depression symptoms at 3 and 6 months. | The intervention had a significant and positive effect on the number of times patients spoke to their pharmacist about their new medication (p < 0.001). In addition, patient knowledge, medication beliefs, and perceptions of progress were significantly better in the intervention group (p < 0.05). No significant difference was noted in adherence, however, fewer doses were missed in the intervention group. No significant difference was noted in depressive symptoms. | Some concerns |
| Participants: Adults aged over 18 years old on a newly prescribed antidepressant (within the previous 4 months before recruitment). Intervention: Participants were telephoned by their pharmacist and taken through Pharmacist-Guided Education and Monitoring (PGEM). This involved three phone calls at monthly intervals, the first lasted 20 min and assessed medication related issues and education. The second and third calls lasted 10 min each and checked progress with medication and helped with problem management. Control: Usual care that pharmacists typically provide for patients on new medications. | |||||||||
| Study Author and Year Research Completed | Intervention Design and Study Population (I = Intervention and C = Control) | Primary Outcome | Results | Risk of Bias (RoB-2) | |||||
| Study Location | Duration | Tele or Digital Medium Used | N | Mean Age (Years) | % Female | ||||
| Medication Adherence continued… | |||||||||
| Beaucage et al. (2006) [58] | Canada | 2-months | Telephone call | I = 126 C = 129 | I = 47 C = 49 | I = 55 C = 60 | The number of drug-related problems participants reported. In addition, the number and severity of infection symptoms following start of antibiotic treatment. Patient adherence to treatment, as well as patient satisfaction. | 53% of intervention participants reported drug related problems versus only 8% in the control arm (p < 0.001). These were mostly noted on the phone call and included adverse drug reactions and drug interactions. Differences in the number of infectious symptoms and severity of symptoms between control and intervention group were small and not significant. Adherence to treatment and satisfaction did not differ across the groups. | Some concerns |
| Participants: Adult patients with a new prescription for oral antibiotic treatment, whose treatment would last between 5 and 14 days, and who had access to a telephone. Participants had a private consultation with the pharmacist about their antibiotic, potential side effects, and adherence to treatment. Intervention: Referred to the pharmacist telephone follow-up intervention (PTFI). Patient received a phone call from their pharmacist on day 3 of antibiotic treatment to discuss treatment, side effects, adherence and any questions they had. Control: Usual care. Afer intial private consultation patients were invited to contact pharmacist, if needed. | |||||||||
| Nietert et al. (2009) [52] | USA | 7 months | Telephone call | PI = 1018 FI = 1016 C = 1014 | PI = 59.9 FI = 60.6 C = 59.7 | Not stated | The primary outcome was the number of days from the date that a patient was declared at least 7 days overdue to the date of the next prescription refill. | There were no significant differences in primary outcomes by treatment arm. Pharmacists contacted 81% of those patients in the phone patient intervention. Of those, 19.2% stated that they were waiting to switch to another medication and 4.1% stated that they were planning to stop the medication. | Some concerns |
| Participants: Patients who were at least 7 days overdue for a medication used to treat a chronic disease (diabetes, hypertension, hyperlipidaemia, heart failure, depression, and psychosis). Usual care: Prescriptions were filled when requested by patients. Phone patient (P) intervention: Pharmacist reminded patient that they were overdue picking up medications, asked why they were overdue, reminded the patient of the importance of taking medications regularly and helped the patient to overcome barriers. Fax physician (F) intervention: Pharmacist faxed prescriber with information about patients overdue collecting medication and asked them to return patient disposition codes via fax to the pharmacy. | |||||||||
| Study Author and Year Research Completed | Intervention Design and Study Population (I = Intervention and C = Control) | Primary Outcome | Results | Risk of Bias (RoB-2) | |||||
| Study Location | Duration | Tele or Digital Medium Used | N | Mean Age (Years) | % Female | ||||
| Medication Adherence continued… | |||||||||
| Odegard and Christensen (2012) [49] | USA | 18 months | Telephone call | I = 120 C = 145 | I = 65 C = 61 | I = 53.8 C = 50.3 | Determination of medication adherence to type 2 diabetes medication (days late at refill, percentage with a refill gap at 6 days, medication possession ratio (MPR) at 6 and 12 months | Significant improvement in medication adherence in intervention group, based on MPR ratio. The impact was particularly noticed in those participants who had a baseline MPR of 0.80 or less. MPR significantly improved in intervention group at 12 months (p = 0.001) | Some concerns |
| Participants: Adults over 18-years old on at least one oral prescription diabetes medication who were late for refills. Intervention: Participants were contacted by their pharmacist by telephone and guided through the 4 A’s (ask, advise, assist and arrange), a model used successfully for changing behaviour in smoking cessation. The pharmacist asked if the patient’s medication had run out, why they had been late to order their medication, if they were having any challenges with their medication, and to discuss a self-management plan. A follow-up call occurred between 1 week and 1 month later. Control: Pharmacist discussed ahderence and ordering medication on time at in-person medication refill collections. | |||||||||
| Kooij et al. (2016) [57] | Netherlands | 30 months | Telephone call | I = 3094 C = 3627 | I = 56.9 C = 59.0 | I = 57.7 C = 54.6 | The primary outcome was patients’ refill adherence measured using the Medication Possession Ratio modified (MPRm) in the year following start of medication therapy. MPRm > 80% considered adherent. | 3094 patients were in the intervention arm, however, only 1054 (34%) received a telephone call. Reasons why patients did not receive a telephone call included: no telephone number available, patient not interested, and patient could not be reached. The analysis of the primary outcome was based on those in the intervention arm who received the phone call. The mean MPRm was 74.7% in intervention arm and 74.5% in the control arm. The proportion of patients who had an MPRm >80% was 69.0% in the intevention arm and 69.9% in the control arm. Patients taking RAS inhibitors were more likely to be adherent in the intervention arm compared to the control arm. The intervention had no benefit to adherence to patients on antidepressants. | Low risk |
| Participants: Adults over 18-years old, who speak Dutch or same language as pharmacist and taking an antidepressant, a bisphosphonate, a statin, or a Renin-Angiotensin-System (RAS) inhibitor for the first time. Usual care: Patients receive both or and written information about medication from a pharmacy technician. Patients are given two weeks of new medication and at first refill are asked about their experience. Further counseling given if needed. Intervention: Usual care plus pharmacist telephoned patient between 7 and 21 days after first prescription. The call addressed need for information, medication intake behaviour, barriers including side effects and concerns or beliefs about the medication. | |||||||||
| Study Author and Year Research Completed | Intervention Design and Study Population (I = Intervention and C = Control) | Primary Outcome | Results | Risk of Bias (RoB-2) | |||||
| Study Location | Duration | Tele or Digital Medium Used | N | Mean Age (Years) | % Female | ||||
| Medication Adherence continued… | |||||||||
| Kosse et al. (2019) [55] | Netherlands | 10 months | mHealth app | I = 87 C = 147 | I = 15.0 C = 15.2 | I = 55.2 C = 51.0 | To deteremine patient self-reported adherence to asthma medication, measured with the Medicine Adherence Report Scales (MARS) tool. Higher scores indicate higher adherence. Secondary outcomes asthma control and quality of life | Adherence of patients who previously had poor adherence increased in intervention group; adherence rates in control group decreased (p = 0.04). No significant difference observed between intervention and control groups on asthma control (p > 0.05) or quality of life (p > 0.05). | Some concerns |
| Participants: Asthma patients aged between 12–18 years old, who own a smartphone and have filled at least two prescriptions for inhaled corticosteroids or combination steroid with bronchodilator inhaler in the previous 12 months Intervention: Usual care (as described in the control) plus 6 months access to the ADAPT intervention. ADAPT is a smartphone application connected to software in the patients community pharmacy. The application targeted non-adherent behaviours. The pharmacist could control its settings, review patient use of the application and chat with the patient. Control: Usual care, meaning that patients received instruction on how to use inhaler at first dispensing, and automated system to detect underuse of inhaled corticosteroid or overuse of bronchodilator. | |||||||||
| Elliott et al. (2020) [53] | UK | 14 months | Telephone call | I = 251 C = 253 | I = 59.5 C = 59.3 | I = 49.8 C = 53.4 | To determine the self-reported adherence or non-adherence to medication at 10 weeks and 26 weeks follow-up. Adherence was assessed by telephone and was defined as missing medication without agreement with a medical professional in the previous 7 days. | 133 (70.7%) out of the 188 who could be contacted at 10 weeks were adherent in the intervention arm versus 60.5% (115/190 who could be contacted) in the control arm (p = 0.037)—significant difference. At week 26, 65.6% in the intervention group were adherentas compared with the 57.1% in the control group (p = 0.113)—no significant difference. Therefore, statistical difference in adherence between groups was lost after week 10. | Low risk |
| Participants: Patients aged 14 years old and over who phsyically present in the pharmacy with a prescription for a new medicine for a predefined long-term medical condition. Intervention: The intervention comprises of a two parts that can be carried out either face-to-face or over the telephone. The first “intervention” happens 7–14 days after the first one-to-one consulation. The “follow-up” then happens 14–21 days after that. The pharmacist will ask about adherence at these meetings. The whole process should be covered within a maximum of 5 weeks. Control: The pharmacists usual advice when a patient presents with a prescription for a new medicine. No follow-up was offered. | |||||||||
| Study Author and Year Research Completed | Intervention Design and Study Population (I = Intervention and C = Control) | Primary Outcome | Results | Risk of Bias (RoB-2) | |||||
| Study Location | Duration | Tele or Digital Medium Used | N | Mean Age (Years) | % Female | ||||
| Medication Counseling | |||||||||
| Kooy et al. (2015) [56] | Netherlands | 16 months | Telephone call | I = 94 C = 117 | I = 59.9 C = 62.2 | I = 52 C = 62 | 1. Patient satisfaction with pharmacist counseling (using the Consumer Quality Index (CQI) plus additional quesitons for intervention arm); 2. Satisfaction with information provided (using Satisfaction with Information about Medicine Scale (SIMS); 3. Beliefs about medicine. | Only 56 of the 94 patients in the intervention arm actually received telephone counseling. Some reasons for not providing counseling included: patient could not be contacted and patient refusal. Usual care participants’ satisfaction with counseling was 31% versus 63% in intervention group who received counseling. Men were more likely to prefer telephone counseling than women (p < 0.05). 74% said telephone counseling had an added value. | Some concerns |
| Particiapnts: Adults aged 18 years or older who filled a first time prescription for an antidepressant, a bisphosphonate, an antilipaemic, or a Renin-Angiotensin-System (RAS) inhibitor. Intervention: Usual care (as defined below) plus telephone counseling by a pharmacist. Telephone call covered actual intake of medication, barriers to medication use, and information needs about medication. Pharmacist used the Health Belief Model (HBM) to direct the counseling. Usual care: Dutch guidelines on counselling for a first prescription of a new medication. Covers an exploration of the patient’s needs and experiences with medication. | |||||||||
| Study Author and Year Research Completed | Intervention Design and Study Population (I = Intervention and C = Control) | Primary Outcome | Results | Risk of Bias (RoB-2) | |||||
| Study Location | Duration | Tele or Digital Medium Used | N | Mean Age (Years) | % Female | ||||
| Hypertension Management | |||||||||
| Margolis et al. (2013) [51] | USA | 25 months; | Blood pressure telemonitor | I = 228 C = 222 | I = 62.0 C = 60.2 | I = 45.2 C = 44.1 | The number of participants who had controlled BP at 6, 12, and 18 months. Change in SBP and DBP were also monitored, as were patient satisfaction with care. | At 6 months, BP was controlled in 71.8% of intervention group versus 45.2% of control arm (p < 0.001). At 12 months BP was controlled in 71.2% of intervention group versus 52.8% of control arm (p = 0.005). At 18 months, BP was controlled in 71.8% of intervention arm versus 57.1% in control arm (p = 0.003). SBP was significantly lower in the intervention group versus control group at 6, 12, and 18 months. | Some concerns |
| Participants: Adult patients with elevated blood pressure (BP) (systolic BP > 140 mmHg or diastolic BP > 90 mmHg) at their two most recent primary care visits. Patients had to have uncontrolled BP based on 3 BP measurements. Intervention: Patients receievd a home BP monitor that stored and transmitted their readings to a website accessible by pharmacist. Pharmacists met them for 1 h initially to discuss BP management and goal setting. Patients submitted at least 6 weekly BP measurements. During the first 6 months, pharmacists and patients had telephone calls every two weeks until BP controlled for 6 weeks, then calls became monthly. From months 7–12 the phone calls were every two months. After 12 months, the BP monitor was returned. Pharmacist telephone calls discussed lifestyle, medication adherence, and goal setting. Treatment intensification recommended in some instances. Control: Management of BP by a physician and referral to pharmacist for medication therapy management when needed. | |||||||||
| Margolis et al. (2018) [50] | USA | 81 months | Blood pressure telemonitor | I = 162 C = 164 | I = 62.0 C = 60.0 | I = 45.1 C = 42.7 | Changes in SMP and DBP from baseline to 54 months | Mean SBP in intervention group reduced by 2.5 mmHg versus 1.0 mmHg in the control group. The intervention group sustained significanttly lower SBP and DBP versus control group for 24 months from baseline. | Some concerns |
| A follow-up study to the research described above by Margolis et al. [52] in 2013. | |||||||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Crilly, P.; Kayyali, R. A Systematic Review of Randomized Controlled Trials of Telehealth and Digital Technology Use by Community Pharmacists to Improve Public Health. Pharmacy 2020, 8, 137. https://doi.org/10.3390/pharmacy8030137
Crilly P, Kayyali R. A Systematic Review of Randomized Controlled Trials of Telehealth and Digital Technology Use by Community Pharmacists to Improve Public Health. Pharmacy. 2020; 8(3):137. https://doi.org/10.3390/pharmacy8030137
Chicago/Turabian StyleCrilly, Philip, and Reem Kayyali. 2020. "A Systematic Review of Randomized Controlled Trials of Telehealth and Digital Technology Use by Community Pharmacists to Improve Public Health" Pharmacy 8, no. 3: 137. https://doi.org/10.3390/pharmacy8030137
APA StyleCrilly, P., & Kayyali, R. (2020). A Systematic Review of Randomized Controlled Trials of Telehealth and Digital Technology Use by Community Pharmacists to Improve Public Health. Pharmacy, 8(3), 137. https://doi.org/10.3390/pharmacy8030137






