Unveiling the Spatial Inequality of Accessibility to High-Quality Healthcare Resources in the Beijing–Tianjin–Hebei Urban Agglomeration of China: A Focus on the Impacts of Intercity Patient Mobility
Abstract
1. Introduction
2. Methods and Data
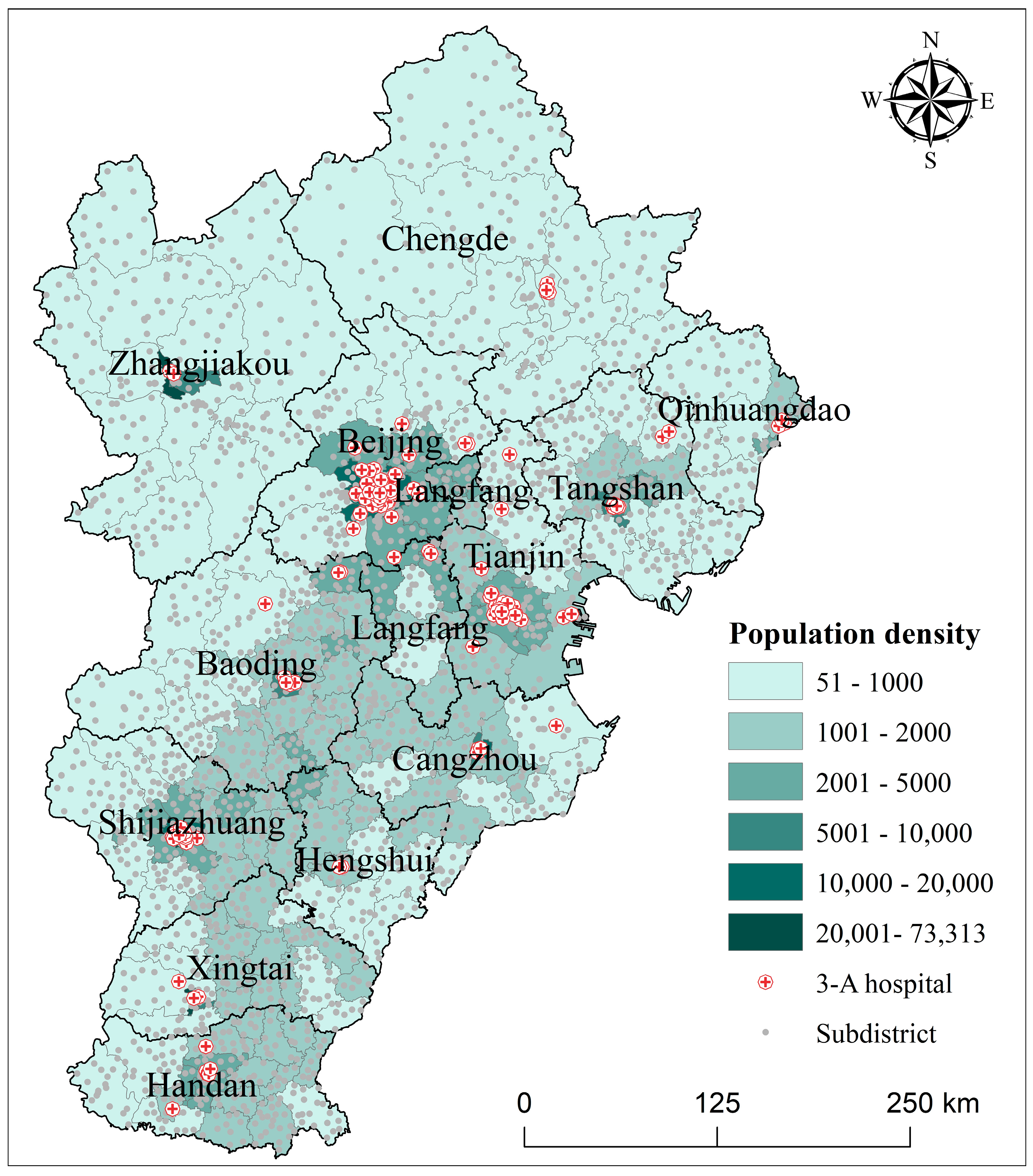
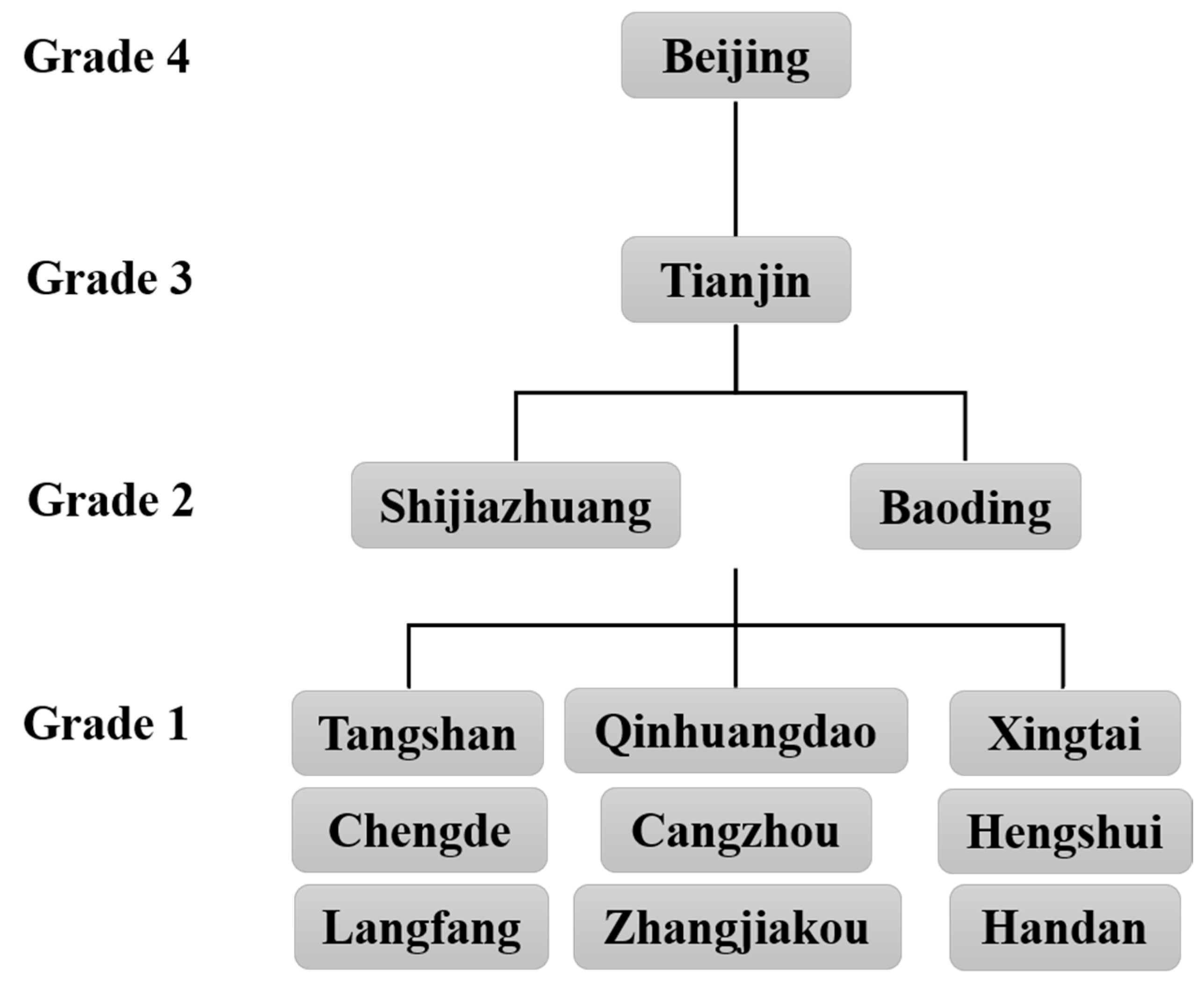
2.1. Study Area and Data Sources
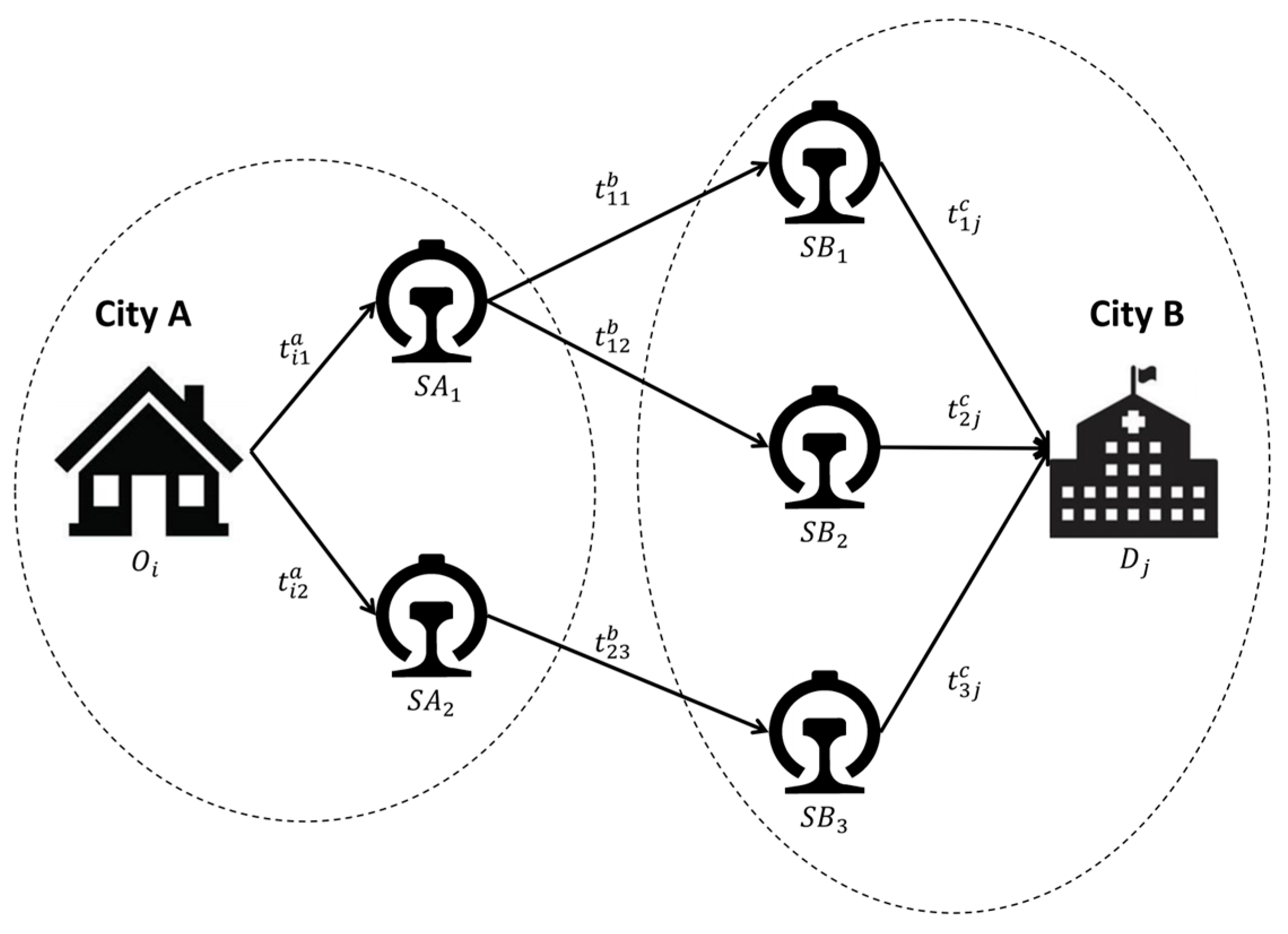
2.2. The Directional Two-Step Floating Catchment Area Method
2.3. Estimating Travel Time via a Multilevel Transportation Network
2.4. Decomposition of Inequality
2.5. Calculation of the Proportions of Intercity and Intracity Travel Times
3. Results
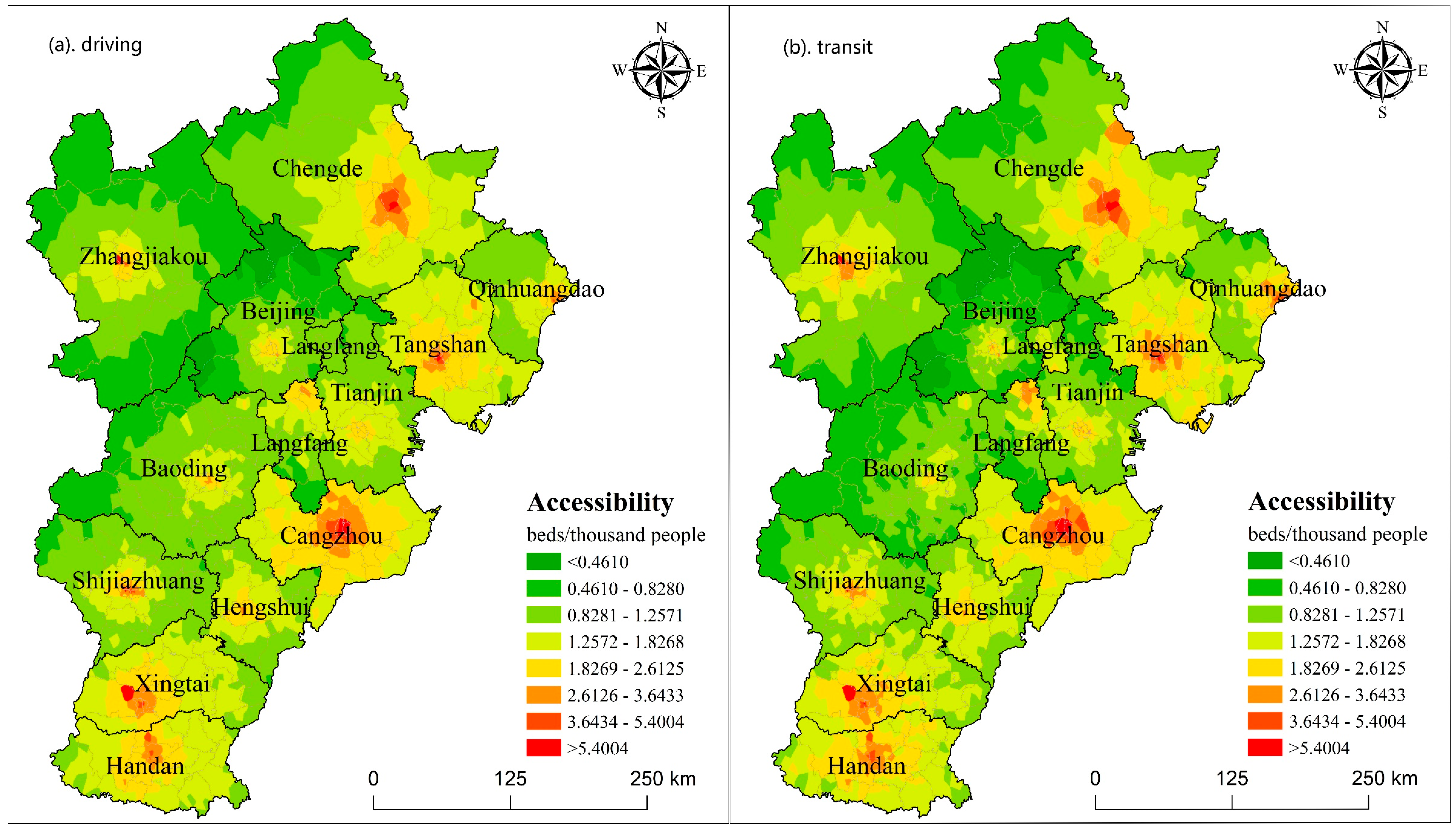
3.1. Spatial Distribution and Equality of Healthcare Accessibility in the Intracity Scenario
3.2. Spatial Distribution and Equality of Healthcare Accessibility in the Intercity Scenario
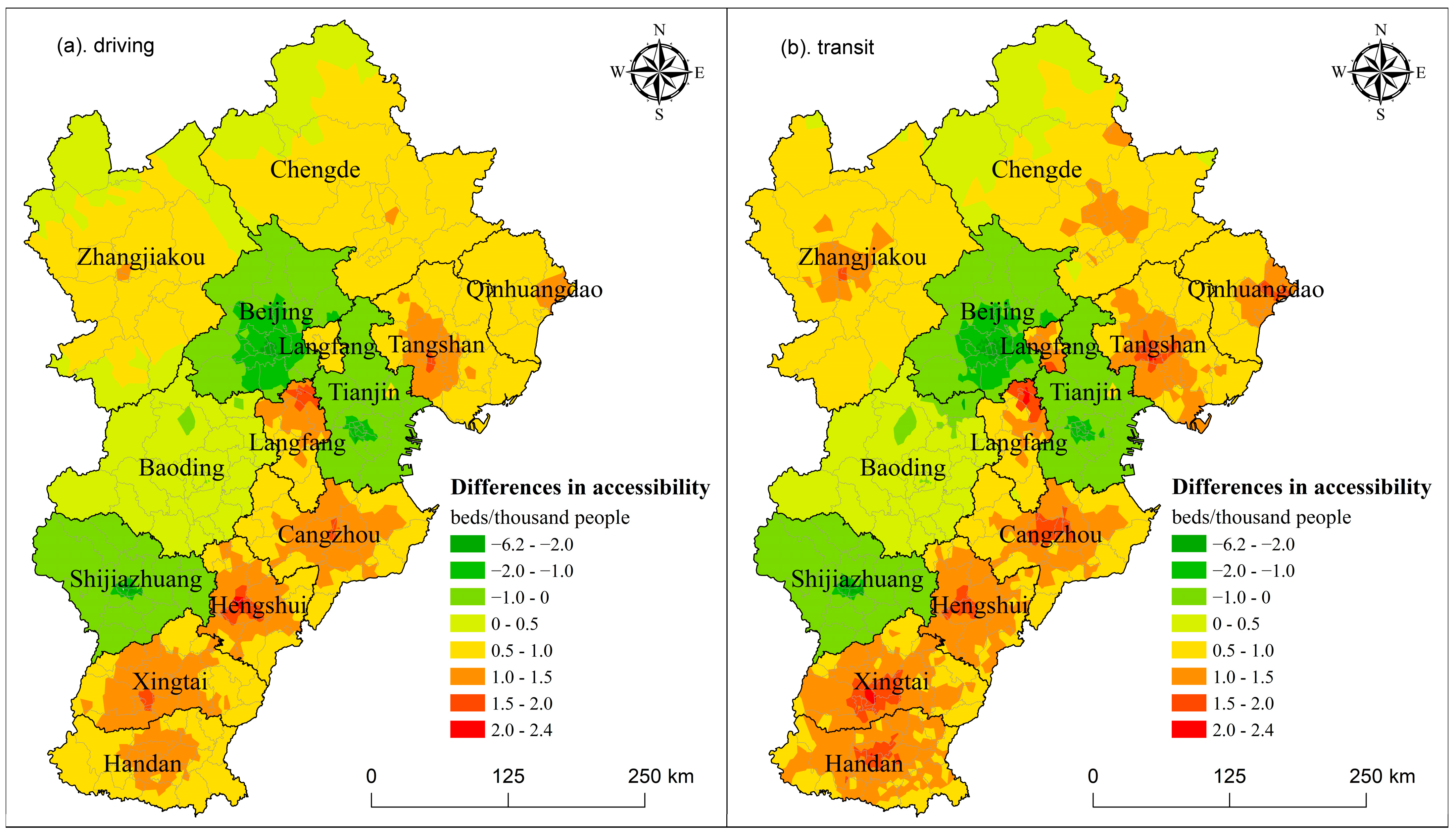
3.3. The Differences Between the Two Scenarios and the Impacts of Intercity Patient Mobility
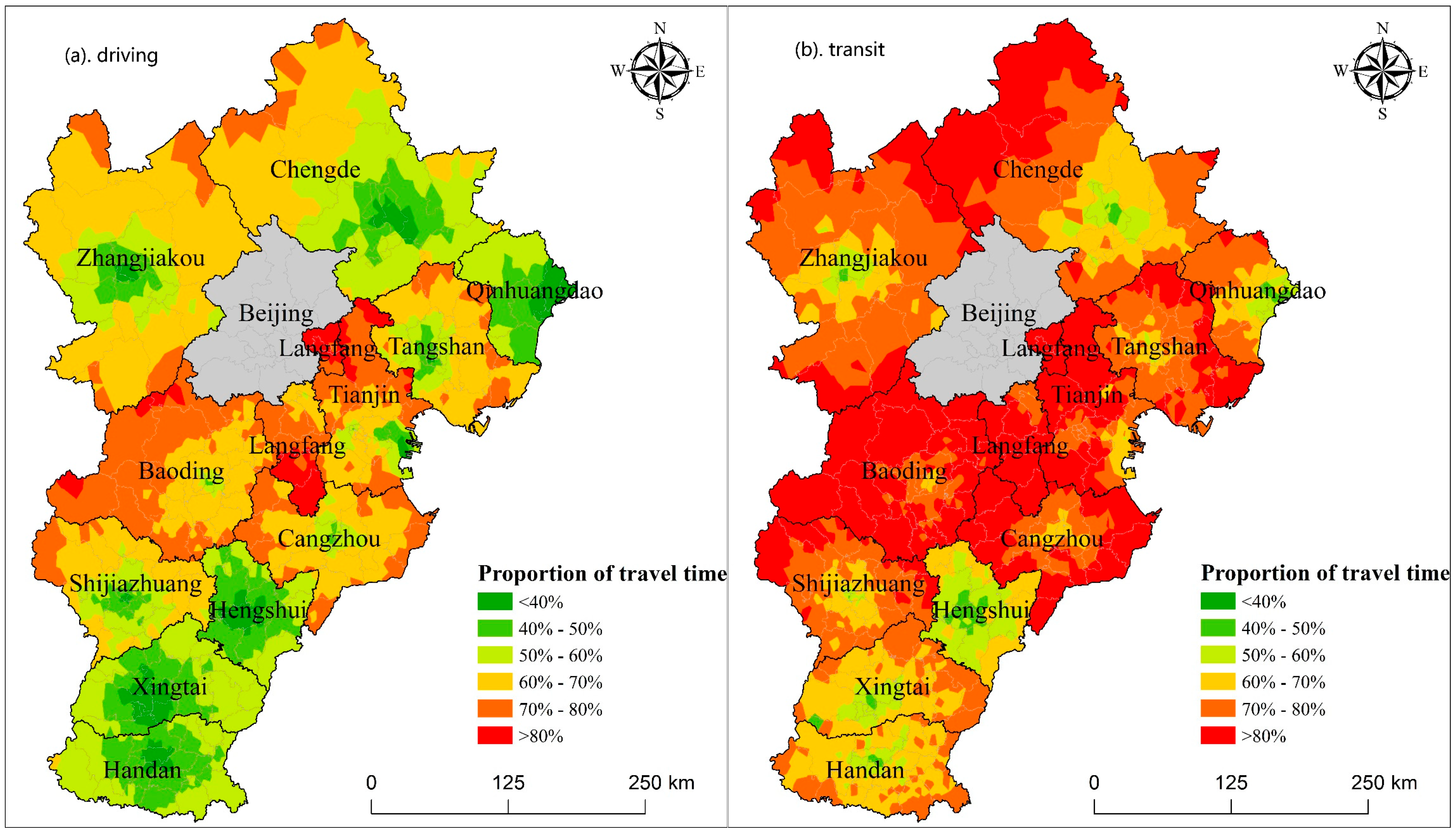
3.4. Proportions of Intercity and Intracity Travel Times
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- The United Nations (UN). Sustainable Development Goals 3; The United Nations (UN): New York, NY, USA, 2015. [Google Scholar]
- Penchansky, R.; Thomas, J.W. The concept of access: Definition and relationship to consumer satisfaction. Med. Care 1981, 19, 127–140. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.A. An integrated approach to measuring potential spatial access to health care services. Socio Econ. Plan. Sci. 1992, 26, 275–287. [Google Scholar] [CrossRef] [PubMed]
- Guagliardo, M.F. Spatial accessibility of primary care: Concepts, methods and challenges. Int. J. Health Geogr. 2004, 3, 3. [Google Scholar] [CrossRef] [PubMed]
- McGrail, M.R. Spatial accessibility of primary health care utilising the two step floating catchment area method: An assessment of recent improvements. Int. J. Health Geogr. 2012, 11, 50. [Google Scholar] [CrossRef]
- Park, Y.; Guldmann, J. Understanding disparities in community green accessibility under alternative green measures: A metropolitan-wide analysis of Columbus, Ohio, and Atlanta, Georgia. Landsc. Urban Plan. 2020, 200, 103806. [Google Scholar] [CrossRef]
- Sharma, G.; Patil, G.R. Spatial and social inequities for educational services accessibility—A case study for schools in Greater Mumbai. Cities 2022, 122, 103543. [Google Scholar] [CrossRef]
- Sharma, G.; Patil, G.R. Urban spatial structure and equity for urban services through the lens of accessibility. Transp. Policy 2024, 146, 72–90. [Google Scholar] [CrossRef]
- Xiong, Q.; Liu, Y.; Xing, L.; Wang, L.; Ding, Y.; Liu, Y. Measuring spatio-temporal disparity of location-based accessibility to emergency medical services. Health Place 2022, 74, 102766. [Google Scholar] [CrossRef]
- Luo, W.; Wang, F. Measures of spatial accessibility to health care in a GIS environment: Synthesis and a case study in the Chicago region. Environ. Plan. B Plan. Des. 2003, 30, 865–884. [Google Scholar] [CrossRef]
- Wang, F. Measurement, optimization and impact of healthcare accessibility: A methodological review. Ann. Assoc. Am. Geogr. 2012, 102, 1104–1112. [Google Scholar] [CrossRef]
- Oliver, A.; Mossialos, E. Equity of access to health care: Outlining the foundations for action. J. Epidemiol. Community Health 2004, 58, 655–658. [Google Scholar] [CrossRef] [PubMed]
- Whitehead, J.; Pearson, A.L.; Lawrenson, R.; Atatoa-Carr, P. How can the spatial equity of health services be defined and measured? A systematic review of spatial equity definitions and methods. J. Health Serv. Res. Policy 2019, 24, 270–278. [Google Scholar] [CrossRef] [PubMed]
- Wang, F.; Tang, Q. Planning toward equal accessibility to services: A quadratic programming approach. Environ. Plan. B Plan. Des. 2013, 40, 195–212. [Google Scholar] [CrossRef]
- Du, X.; Liu, M.; Luo, S. Exploring Equity in a Hierarchical Medical Treatment System: A Focus on Determinants of Spatial Accessibility. ISPRS Int. J. Geo Inf. 2023, 12, 318. [Google Scholar] [CrossRef]
- Vallée, J.; Shareck, M.; Le Roux, G.; Kestens, Y.; Frohlich, K.L. Is accessibility in the eye of the beholder? Social inequalities in spatial accessibility to health-related resources in Montréal, Canada. Soc. Sci. Med. 2020, 245, 112702. [Google Scholar] [CrossRef]
- Tao, Z.; Cheng, Y.; Du, S.; Feng, L.; Wang, S. Accessibility to delivery care in Hubei Province, China. Soc. Sci. Med. 2020, 260, 113186. [Google Scholar] [CrossRef]
- Ghorbanzadeh, M.; Kim, K.; Erman Ozguven, E.; Horner, M.W. Spatial accessibility assessment of COVID-19 patients to healthcare facilities: A case study of Florida. Travel Behav. Soc. 2021, 24, 95–101. [Google Scholar] [CrossRef]
- Yan, X.; He, S.; Webster, C.; Yu, M. Divergent distributions of physicians and healthcare beds in China Changing patterns, driving forces, and policy implications. Appl. Geogr. 2022, 138, 102626. [Google Scholar] [CrossRef]
- Jia, P.; Wang, Y.; Yang, M.; Wang, L.; Yang, X.; Shi, X.; Yang, L.; Wen, J.; Liu, Y.; Yang, M.; et al. Inequalities of spatial primary healthcare accessibility in China. Soc. Sci. Med. 2022, 314, 115458. [Google Scholar] [CrossRef]
- Ye, P.; Ye, Z.; Xia, J.; Zhong, L.; Zhang, M.; Lv, L.; Tu, W.; Yue, Y.; Li, Q. National-scale 1-km maps of hospital travel time and hospital accessibility in China. Sci. Data 2024, 11, 1130. [Google Scholar] [CrossRef]
- Falchetta, G.; Hammad, A.T.; Shayegh, S. Planning universal accessibility to public health care in sub-Saharan Africa. Proc. Natl. Acad. Sci. USA 2020, 117, 31760–31769. [Google Scholar] [CrossRef] [PubMed]
- Juran, S.; Broer, P.N.; Klug, S.J.; Snow, R.C.; Okiro, E.A.; Ouma, P.O.; Snow, R.W.; Tatem, A.J.; Meara, J.G.; Alegana, V.A. Geospatial mapping of access to timely essential surgery in sub-Saharan Africa. BMJ Glob. Health 2018, 3, e000875. [Google Scholar] [CrossRef] [PubMed]
- Weiss, D.J.; Nelson, A.; Vargas-Ruiz, C.A.; Gligorić, K.; Bavadekar, S.; Gabrilovich, E.; Bertozzi-Villa, A.; Rozier, J.; Gibson, H.S.; Shekel, T.; et al. Global maps of travel time to healthcare facilities. Nat. Med. 2020, 26, 1835–1838. [Google Scholar] [CrossRef] [PubMed]
- Hall, P.; Pain, K. The Polycentric Metropolis: Learning from Megacity Regions in Europe; Earthscan: London, UK, 2006. [Google Scholar]
- Gottmann, J. Megalopolis or the Urbanization of the Northeastern Seaboard. Econ. Geogr. 1957, 33, 189–200. [Google Scholar] [CrossRef]
- Scott, A.J. Global City-Regions: Trends, Theory, Policy; Oxford University Press: New York, NY, USA, 2001. [Google Scholar]
- Florida, R.; Gulden, T.; Mellander, C. The rise of the mega-region. Camb. J. Reg. Econ. Soc. 2008, 1, 459–476. [Google Scholar] [CrossRef]
- Kloosterman, R.; Musterd, S. The Polycentric Urban Region: Towards a Research Agenda. Urban Stud. 2001, 38, 623–633. [Google Scholar] [CrossRef]
- McGee, T.G. The Emergence of Desakota Regions in Asia: Expanding a Hypothesis. In The Extended Metropolis: Settlement Transition Is Asia; Ginsburg, N., Koppel, B., McGee, T.G., Eds.; University of Hawaii Press: Honolulu, HI, USA, 1991. [Google Scholar]
- Fang, C.; Yu, D. Urban agglomeration: An evolving concept of an emerging phenomenon. Landsc. Urban Plan. 2017, 162, 126–136. [Google Scholar] [CrossRef]
- The State Council of China. The National New-Type Urbanization Plan; The State Council of China: Beijing, China, 2014. [Google Scholar]
- Dash Nelson, G.; Rae, A. An Economic Geography of the United States: From Commutes to Megaregions. PLoS ONE 2016, 11, e0166083. [Google Scholar] [CrossRef]
- Huang, H.; Xia, T.; Tian, Q.; Liu, T.; Wang, C.; Li, D. Transportation issues in developing China’s urban agglomerations. Transp. Policy 2020, 85, A1–A22. [Google Scholar] [CrossRef]
- Marull, J.; Font, C.; Boix, R. Modelling urban networks at mega-regional scale: Are increasingly complex urban systems sustainable? Land Use Policy 2015, 43, 15–27. [Google Scholar] [CrossRef]
- Zhang, W.; Fang, C.; Zhou, L.; Zhu, J. Measuring megaregional structure in the Pearl River Delta by mobile phone signaling data: A complex network approach. Cities 2020, 104, 102809. [Google Scholar] [CrossRef]
- Lin, X.; Yang, J.; MacLachlan, I. High-speed rail as a solution to metropolitan passenger mobility: The case of Shenzhen-Dongguan-Huizhou metropolitan area. J. Transp. Land Use 2018, 11, 1257–1270. [Google Scholar] [CrossRef]
- Ross, C. Transport and megaregions: High-speed rail in the United States. Town Plan. Rev. 2011, 82, 341–356. [Google Scholar] [CrossRef]
- Harrington, D.W.; Rosenberg, M.W.; Wilson, K. Comparing health status and access to health care in Canada’s largest metropolitan areas. Urban Geogr. 2014, 35, 1156–1170. [Google Scholar] [CrossRef]
- Yu, M.; He, S.; Wu, D.; Zhu, H.; Webster, C. Examining the Multi-Scalar Unevenness of High-Quality Healthcare Resources Distribution in China. Int. J. Environ. Res. Public Health 2019, 16, 2813. [Google Scholar] [CrossRef]
- Brekke, K.R.; Levaggi, R.; Siciliani, L.; Straume, O.R. Patient mobility and health care quality when regions and patients differ in income. J. Health Econ. 2016, 50, 372–387. [Google Scholar] [CrossRef]
- Koylu, C.; Delil, S.; Guo, D.; Celik, R.N. Analysis of big patient mobility data for identifying medical regions, spatio-temporal characteristics and care demands of patients on the move. Int. J. Health Geogr. 2018, 17, 32. [Google Scholar] [CrossRef]
- Beraldo, S.; Collaro, M.; Marino, I. Patient migration as a response to the regulation of subnational healthcare budgets. Reg. Stud. 2023, 57, 2207–2219. [Google Scholar] [CrossRef]
- Ding, J.; Yang, C.; Wang, Y.; Li, P.; Wang, F.; Kang, Y.; Wang, H.; Liang, Z.; Zhang, J.; Han, P.; et al. Influential factors of intercity patient mobility and its network structure in China. Cities 2023, 132, 103975. [Google Scholar] [CrossRef]
- Wang, X.; Nie, X. The uneven distribution of medical resources for severe diseases in China: An analysis of the disparity in inter-city patient mobility. Appl. Geogr. 2024, 165, 103226. [Google Scholar] [CrossRef]
- Zhong, Q.; Wu, J.; Tao, Z. Intercity patient mobility can improve healthcare accessibility and equality in metropolitan areas: A case study of Shenzhen metropolitan area, China. Appl. Geogr. 2024, 171, 103383. [Google Scholar] [CrossRef]
- Li, C.; Wang, J. A hierarchical two-step floating catchment area analysis for high-tier hospital accessibility in an urban agglomeration region. J. Transp. Geogr. 2022, 102, 103369. [Google Scholar] [CrossRef]
- Zhang, H.; Zhou, B.-B.; Liu, S.; Hu, G.; Meng, X.; Liu, X.; Shi, H.; Gao, Y.; Hou, H.; Li, X. Enhancing intercity transportation will improve the equitable distribution of high-quality health care in China. Appl. Geogr. 2023, 152, 102892. [Google Scholar] [CrossRef]
- Yip, W.; Fu, H.; Chen, A.T.; Zhai, T.; Jian, W.; Xu, R.; Pan, J.; Hu, M.; Zhou, Z.; Chen, Q.; et al. 10 years of health-care reform in China: Progress and gaps in Universal Health Coverage. Lancet 2019, 394, 1192–1204. [Google Scholar] [CrossRef]
- Tao, Z.; Yao, Z.; Kong, H.; Duan, F.; Li, G. Spatial accessibility to healthcare services in Shenzhen, China: Improving the multi-modal two-step floating catchment area method by estimating travel time via online map APIs. BMC Health Serv. Res. 2018, 18, 345. [Google Scholar] [CrossRef]
- Chen, K.; Zhao, P.; Qin, K.; Kwan, M.; Wang, N. Towards healthcare access equality: Understanding spatial accessibility to healthcare services for wheelchair users. Comput. Environ. Urban Syst. 2024, 108, 102069. [Google Scholar] [CrossRef]
- Yang, D.; Goerge, R.; Mullner, R. Comparing GIS-based methods of measuring spatial accessibility to health services. J. Med. Syst. 2006, 30, 23–32. [Google Scholar] [CrossRef]
- Stacherl, B.; Sauzet, O. Gravity models for potential spatial healthcare access measurement: A systematic methodological review. Int. J. Health Geogr. 2023, 22, 34. [Google Scholar] [CrossRef]
- Radke, J.; Mu, L. Spatial decomposition, modeling and mapping service regions to predict access to social programs. Geogr. Inf. Sci. 2000, 2, 105–112. [Google Scholar] [CrossRef]
- Dai, D. Black residential segregation, disparities in spatial access to health care facilities, and late-stage breast cancer diagnosis in metropolitan Detroit. Health Place 2010, 16, 1038–1052. [Google Scholar] [CrossRef]
- Luo, W.; Qi, Y. An enhanced two-step floating catchment area (E2SFCA) method for measuring spatial accessibility to primary care physicians. Health Place 2009, 15, 1100–1107. [Google Scholar] [CrossRef] [PubMed]
- McGrail, M.R.; Humphreys, J.S. Measuring spatial accessibility to primary health care services: Utilising dynamic catchment sizes. Appl. Geogr. 2014, 54, 182–188. [Google Scholar] [CrossRef]
- Langford, M.; Higgs, G.; Fry, R. Multi-modal two-step floating catchment area analysis of primary health care accessibility. Health Place 2016, 38, 70–81. [Google Scholar] [CrossRef]
- Mao, L.; Nekorchuk, D. Measuring spatial accessibility to healthcare for populations with multiple transportation modes. Health Place 2013, 24, 115–122. [Google Scholar] [CrossRef] [PubMed]
- Delamater, P.L. Spatial accessibility in suboptimally configured health care systems: A modified two-step floating catchment area (M2SFCA) metric. Health Place 2013, 24, 30–43. [Google Scholar] [CrossRef]
- Luo, J. Integrating the Huff Model and Floating Catchment Area Methods to Analyze Spatial Access to Healthcare Services. Trans. GIS 2014, 18, 436–448. [Google Scholar] [CrossRef]
- Shao, Y.; Luo, W. Supply-demand adjusted two-steps floating catchment area (SDA-2SFCA) model for measuring spatial access to health care. Soc. Sci. Med. 2022, 296, 114727. [Google Scholar] [CrossRef]
- Wang, J.; Du, F.; Huang, J.; Liu, Y. Access to hospitals: Potential vs. observed. Cities 2020, 100, 102671. [Google Scholar] [CrossRef]
- Wei, Z.; Bai, J.; Feng, R. Evaluating the spatial accessibility of medical resources taking into account the residents‘ choice behavior of outpatient and inpatient medical treatment. Socio Econ. Plan. Sci. 2022, 83, 101336. [Google Scholar] [CrossRef]
- Wei, W.; Xiang, B. Spatial pattern of cross-city medical network and supply-demand relationship of medical facilities in China: Based on cross-city medical internet data. Geogr. Res. 2024, 43, 701–717. [Google Scholar]
- Jia, W.; Huang, Z.; Bao, J.; Shen, W. Spatiotemporal differences in the accessibility of scenic spots based on door-to-door travel by high-speed rail: A case study of Shanghai-Nanjing intercity travel. Tour. Trib. 2023, 38, 148–159. [Google Scholar]
- Dai, G.; Li, R.; Ma, S. Research on the equity of health resource allocation in TCM hospitals in China based on the Gini coefficient and agglomeration degree: 2009–2018. Int. J. Equity Health 2022, 21, 145. [Google Scholar] [CrossRef] [PubMed]
- Skaftun, E.K.; Verguet, S.; Norheim, O.F.; Johansson, K.A. Geographic health inequalities in Norway: A Gini analysis of cross-county differences in mortality from 1980 to 2014. Int. J. Equity Health 2018, 17, 64. [Google Scholar] [CrossRef] [PubMed]
- Dagum, C. A New Approach to the Decomposition of the Gini Income Inequality Ratio. Empir. Econ. 1997, 22, 515–531. [Google Scholar] [CrossRef]
- Peng, R.; Huang, J.; Deng, X. Spatiotemporal evolution and influencing factors of the allocation of social care resources for the older adults in China. Int. J. Equity Health 2023, 22, 222. [Google Scholar] [CrossRef]


| Scenario | Overall Gini Coefficient | Intracity Component | Intercity Component | Super-Variable Density Component |
|---|---|---|---|---|
| Intracity—Driving | 0.459 | 0.028 (6.1%) | 0.318 (69.3%) | 0.113 (24.6%) |
| Intracity—Transit | 0.466 | 0.029 (6.3%) | 0.315 (67.5%) | 0.122 (26.2%) |
| Intercity—Driving | 0.265 | 0.019 (7.2%) | 0.131 (49.4%) | 0.116 (43.8%) |
| Intercity—Transit | 0.297 | 0.020 (6.8%) | 0.159 (53.7%) | 0.117 (39.5%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the International Society for Photogrammetry and Remote Sensing. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, Y.; Chen, L.; Liu, B.; Tao, Z. Unveiling the Spatial Inequality of Accessibility to High-Quality Healthcare Resources in the Beijing–Tianjin–Hebei Urban Agglomeration of China: A Focus on the Impacts of Intercity Patient Mobility. ISPRS Int. J. Geo-Inf. 2025, 14, 168. https://doi.org/10.3390/ijgi14040168
Wang Y, Chen L, Liu B, Tao Z. Unveiling the Spatial Inequality of Accessibility to High-Quality Healthcare Resources in the Beijing–Tianjin–Hebei Urban Agglomeration of China: A Focus on the Impacts of Intercity Patient Mobility. ISPRS International Journal of Geo-Information. 2025; 14(4):168. https://doi.org/10.3390/ijgi14040168
Chicago/Turabian StyleWang, Yandi, Lin Chen, Binglin Liu, and Zhuolin Tao. 2025. "Unveiling the Spatial Inequality of Accessibility to High-Quality Healthcare Resources in the Beijing–Tianjin–Hebei Urban Agglomeration of China: A Focus on the Impacts of Intercity Patient Mobility" ISPRS International Journal of Geo-Information 14, no. 4: 168. https://doi.org/10.3390/ijgi14040168
APA StyleWang, Y., Chen, L., Liu, B., & Tao, Z. (2025). Unveiling the Spatial Inequality of Accessibility to High-Quality Healthcare Resources in the Beijing–Tianjin–Hebei Urban Agglomeration of China: A Focus on the Impacts of Intercity Patient Mobility. ISPRS International Journal of Geo-Information, 14(4), 168. https://doi.org/10.3390/ijgi14040168





