Discovery of A Novel Series of Quinazoline–Thiazole Hybrids as Potential Antiproliferative and Anti-Angiogenic Agents
Abstract
1. Introduction
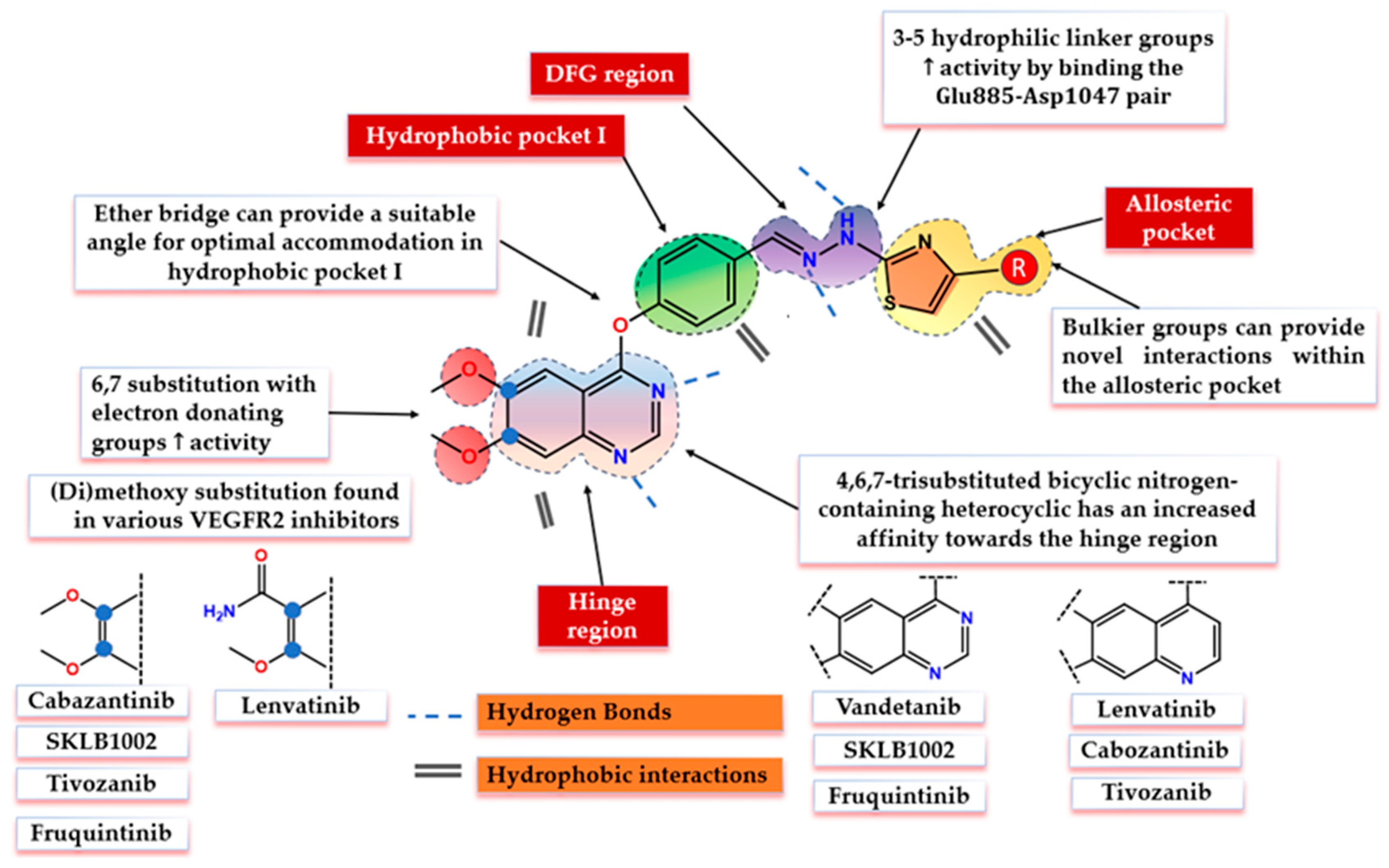
2. Structural Design and Rationale
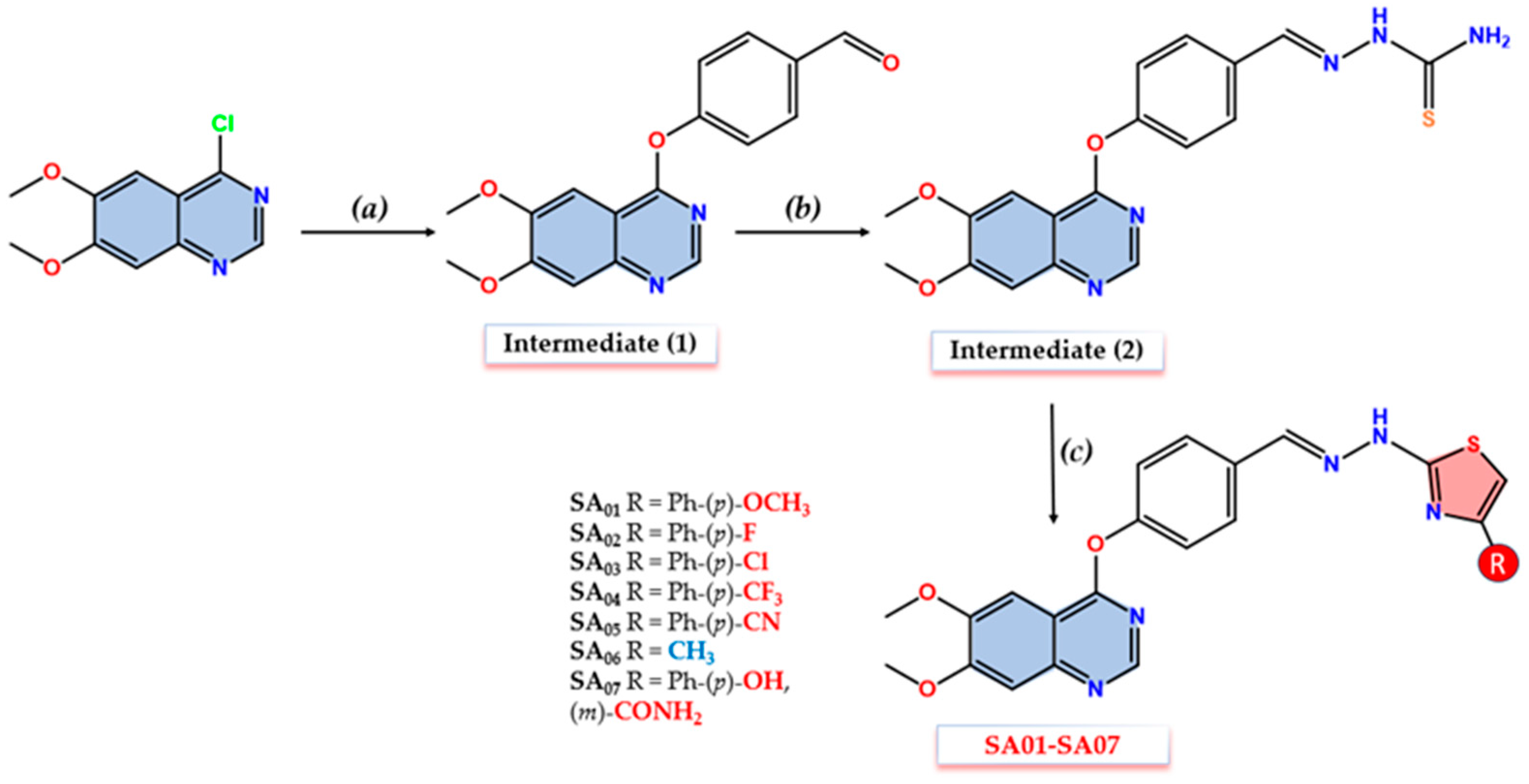
3. Materials and Methods
3.1. Materials and Measurements
3.2. Chemistry
3.2.1. Synthesis of Intermediate (1)
3.2.2. Synthesis of Intermediate (2)
3.2.3. Synthesis of Compounds SA01–SA07
3.3. In Vitro Cytotoxicity Evaluation
3.4. Molecular Docking Studies
3.5. Molecular Dynamics Studies
3.6. MM-PBSA Free Energy Calculation
3.7. Density Function Theory (DFT) Calculations
3.8. Wound Healing (Scratch) Assay
3.9. Chorioallantoic Egg Membrane (CAM) Assay
3.10. In Silico Physicochemical and Pharmacokinetics Predictions
4. Results and Discussion
4.1. Chemistry
4.2. In Vitro Cytotoxicity Evaluation
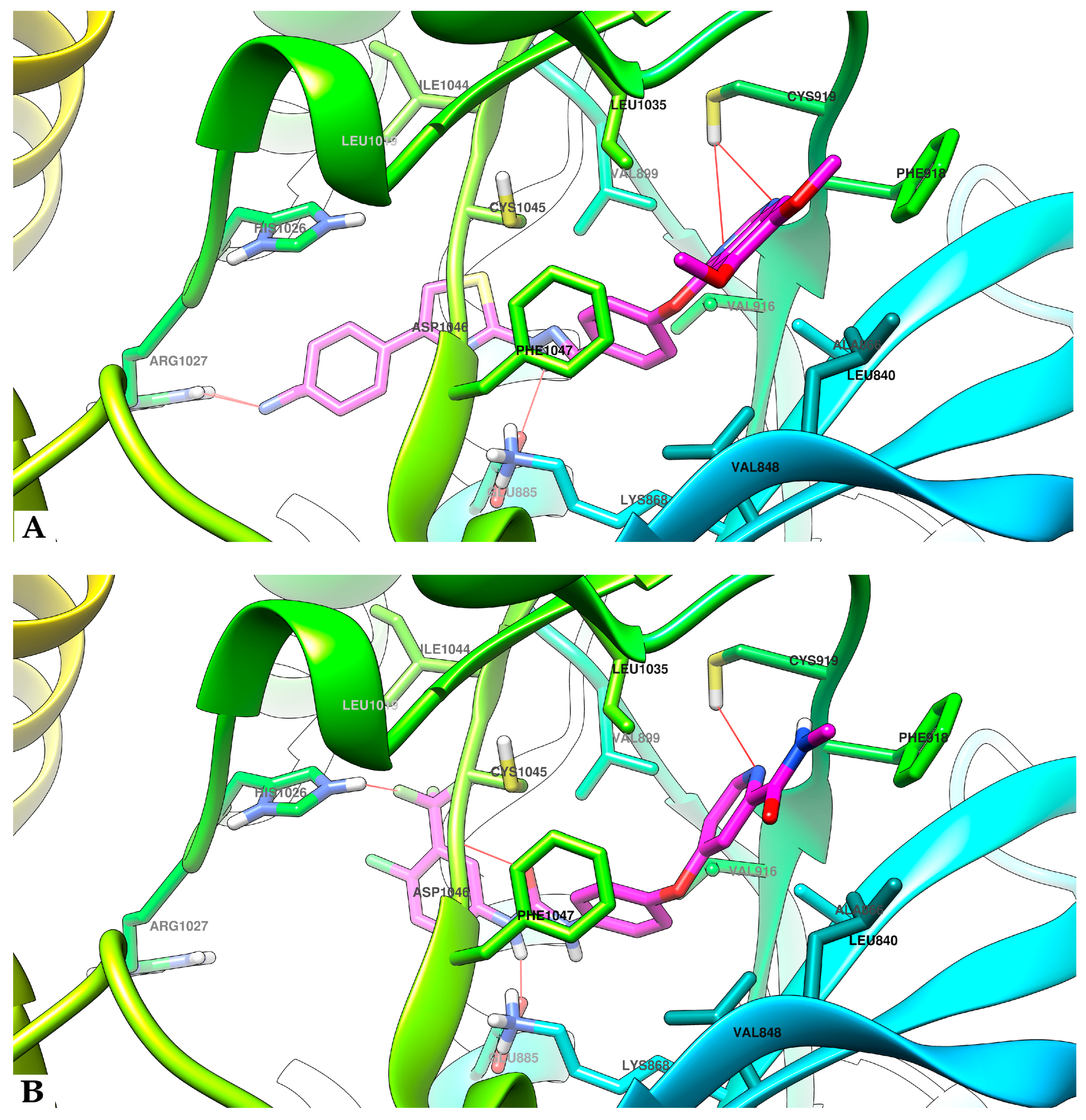
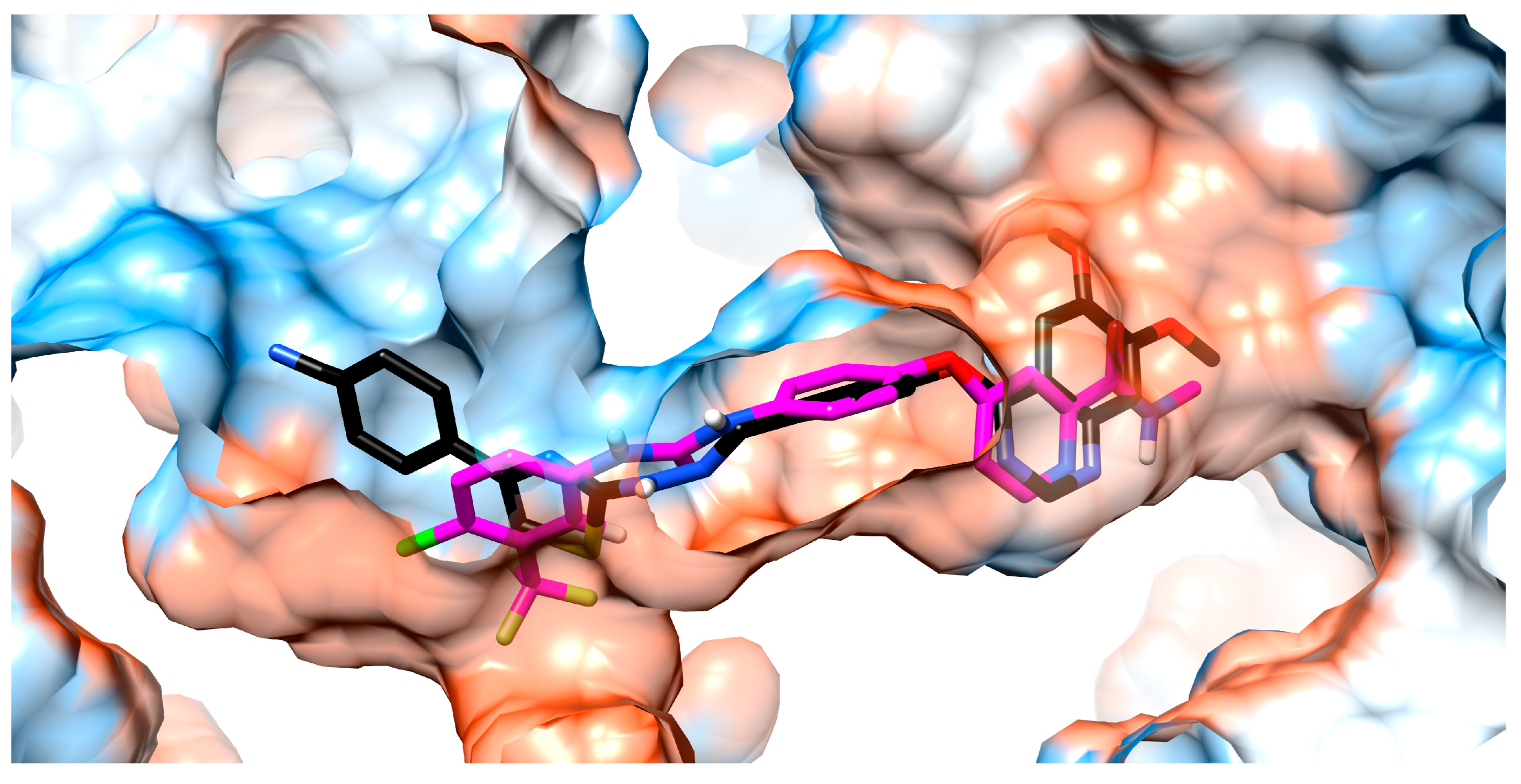
4.3. Molecular Docking Studies
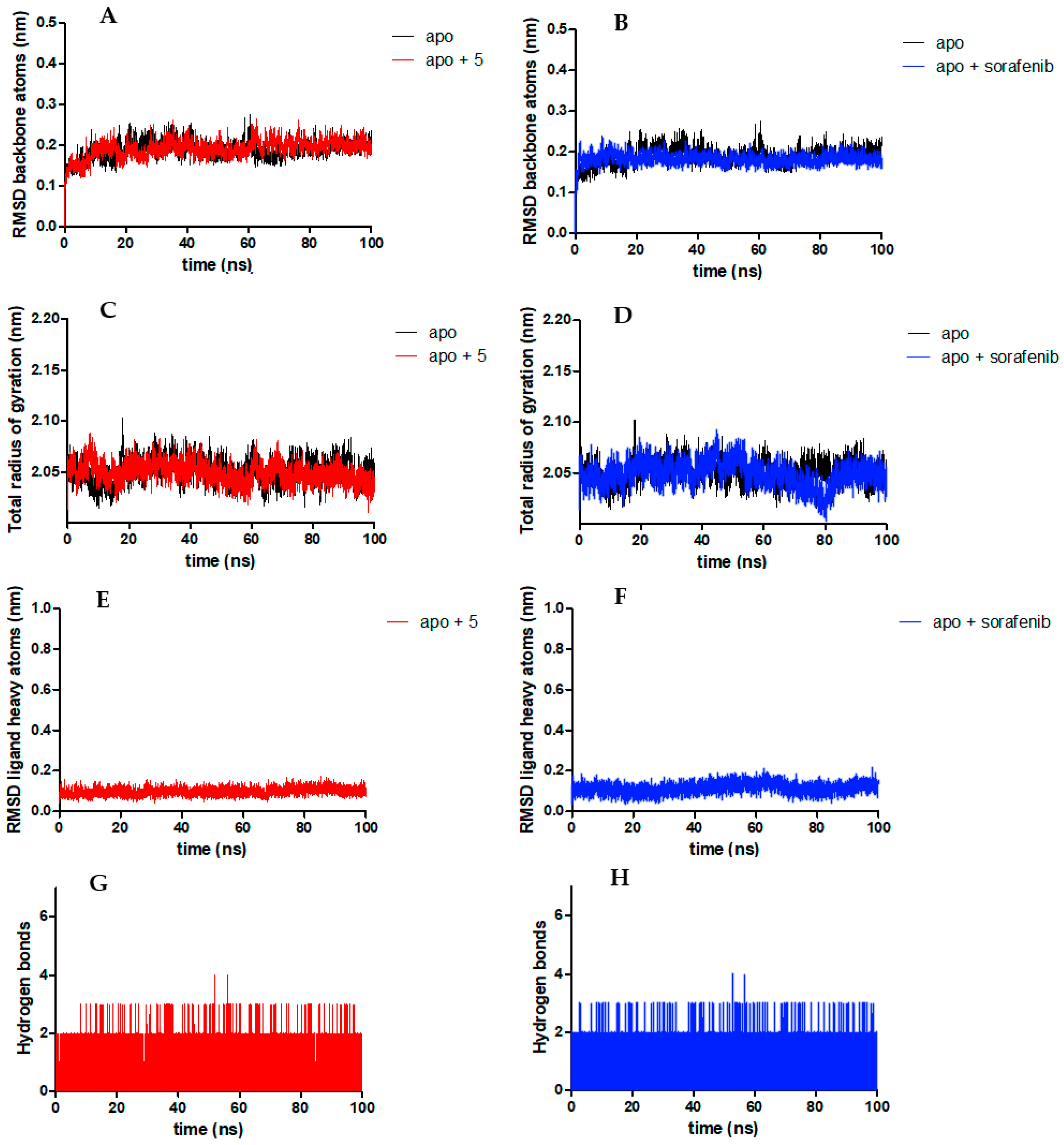
4.4. Molecular Dynamics Studies
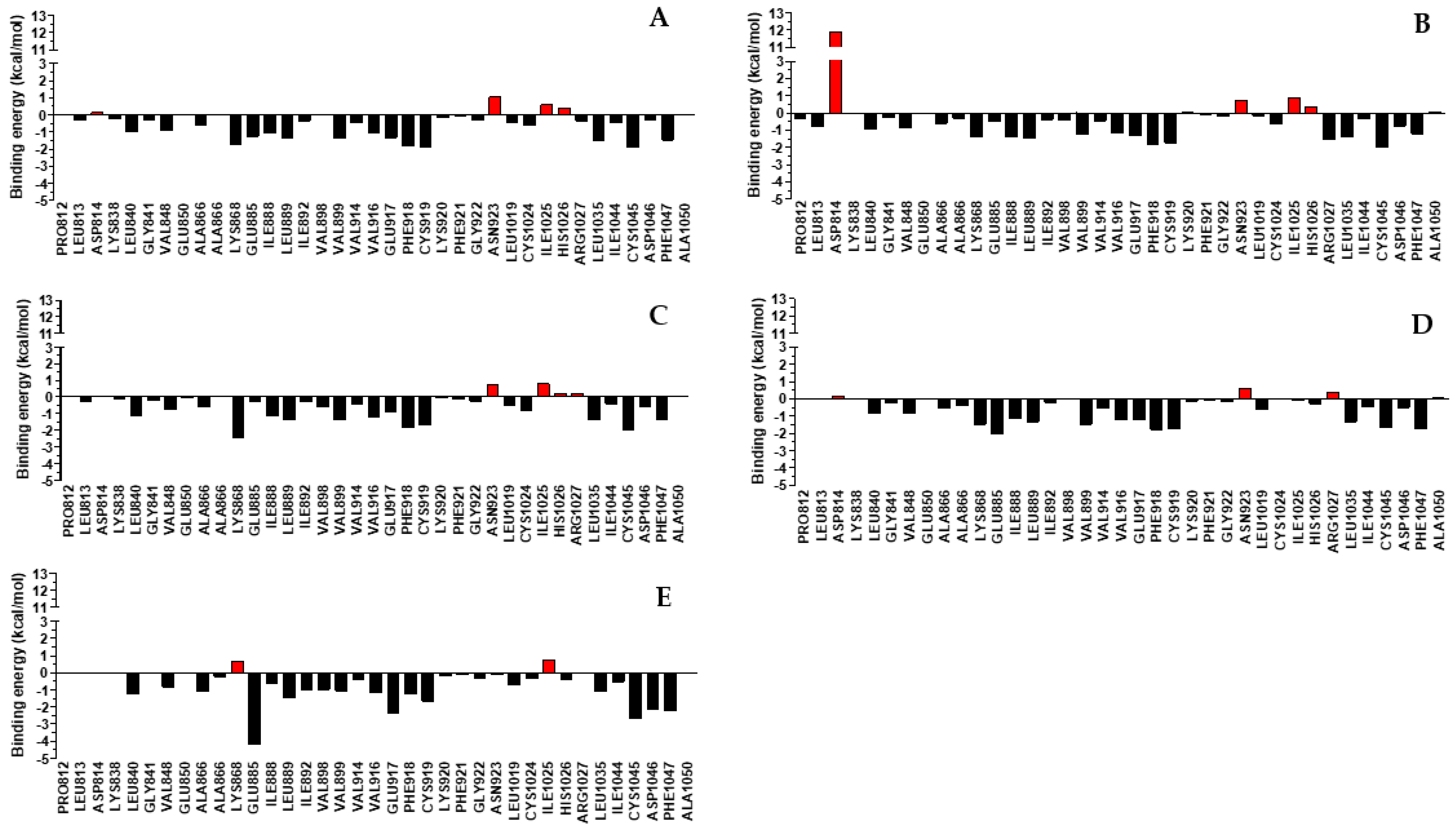
4.5. MM-PBSA Free Energy Calculation
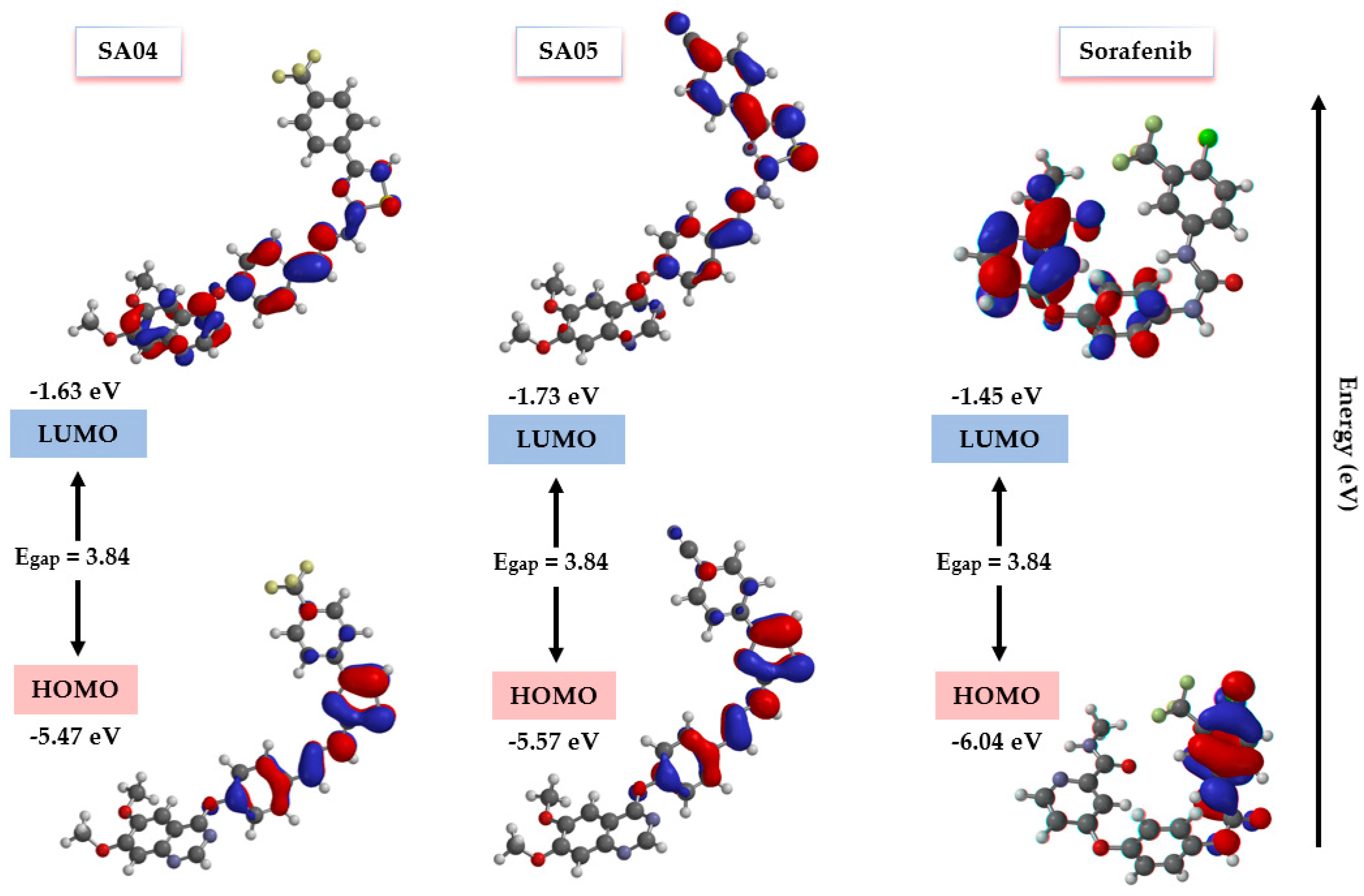
4.6. FMO Analysis and Chemical Reactivity Descriptors
4.7. Wound Healing (Scratch) Assay
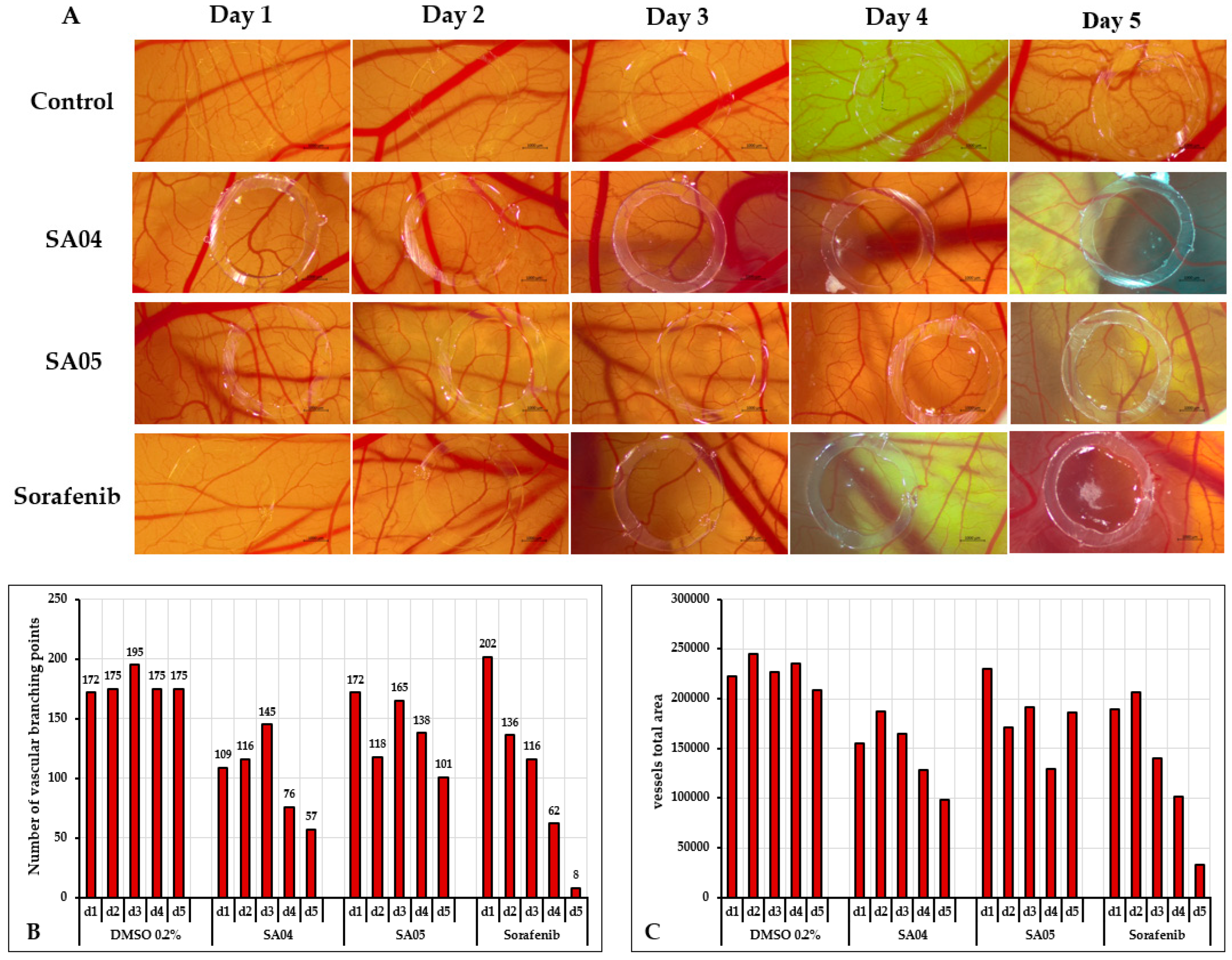
4.8. Chorioallantoic Egg Membrane (CAM) Assay
4.9. In Silico Physicochemical and Pharmacokinetics Prediction
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hanahan, D.; Weinberg, R.A. The Hallmarks of Cancer. Cell 2000, 100, 57–70. [Google Scholar] [CrossRef] [PubMed]
- Hanahan, D.; Weinberg, R.A. Hallmarks of Cancer: The next Generation. Cell 2011, 144, 646–674. [Google Scholar] [CrossRef] [PubMed]
- Hanahan, D. Hallmarks of Cancer: New Dimensions. Cancer Discov. 2022, 12, 31–46. [Google Scholar] [CrossRef]
- Lugano, R.; Ramachandran, M.; Dimberg, A. Tumor Angiogenesis: Causes, Consequences, Challenges and Opportunities. Cell. Mol. Life Sci. 2020, 77, 1745–1770. [Google Scholar] [CrossRef]
- Carmeliet, P.; Jain, R.K. Molecular Mechanisms and Clinical Applications of Angiogenesis. Nature 2011, 473, 298–307. [Google Scholar] [CrossRef] [PubMed]
- Majidpoor, J.; Mortezaee, K. Angiogenesis as a Hallmark of Solid Tumors—Clinical Perspectives. Cell. Oncol. 2021, 44, 715–737. [Google Scholar] [CrossRef]
- Hanahan, D.; Folkman, J. Patterns and Emerging Mechanisms of the Angiogenic Switch during Tumorigenesis. Cell 1996, 86, 353–364. [Google Scholar] [CrossRef]
- Herbert, S.P.; Stainier, D.Y.R. Molecular Control of Endothelial Cell Behaviour during Blood Vessel Morphogenesis. Nat. Rev. Mol. Cell Biol. 2011, 12, 551–564. [Google Scholar] [CrossRef]
- Sengupta, S.; Eavarone, D.; Capila, I.; Zhao, G.; Watson, N.; Kiziltepe, T.; Sasisekharan, R. Temporal Targeting of Tumour Cells and Neovasculature with a Nanoscale Delivery System. Nature 2005, 436, 568–572. [Google Scholar] [CrossRef] [PubMed]
- Chauhan, V.P.; Stylianopoulos, T.; Boucher, Y.; Jain, R.K. Delivery of Molecular and Nanoscale Medicine to Tumors: Transport Barriers and Strategies. Annu. Rev. Chem. Biomol. Eng. 2011, 2, 281–298. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Bove, A.M.; Simone, G.; Ma, B. Molecular Bases of VEGFR-2-Mediated Physiological Function and Pathological Role. Front. Cell Dev. Biol. 2020, 8, 599281. [Google Scholar] [CrossRef]
- Weis, S.M.; Cheresh, D.A. Tumor Angiogenesis: Molecular Pathways and Therapeutic Targets. Nat. Med. 2011, 17, 1359–1370. [Google Scholar] [CrossRef]
- Ivy, S.P.; Wick, J.Y.; Kaufman, B.M. An Overview of Small-Molecule Inhibitors of VEGFR Signaling. Nat. Rev. Clin. Oncol. 2009, 6, 569–579. [Google Scholar] [CrossRef] [PubMed]
- Modi, S.J.; Kulkarni, V.M. Vascular Endothelial Growth Factor Receptor (VEGFR-2)/KDR Inhibitors: Medicinal Chemistry Perspective. Med. Drug Discov. 2019, 2, 100009. [Google Scholar] [CrossRef]
- Wu, P.; Nielsen, T.E.; Clausen, M.H. FDA-Approved Small-Molecule Kinase Inhibitors. Trends Pharmacol. Sci. 2015, 36, 422–439. [Google Scholar] [CrossRef] [PubMed]
- Gauthier, A.; Ho, M. Role of Sorafenib in the Treatment of Advanced Hepatocellular Carcinoma: An Update. Hepatol. Res. 2013, 43, 147–154. [Google Scholar] [CrossRef] [PubMed]
- Hansen, C.R.; Grimm, D.; Bauer, J.; Wehland, M.; Magnusson, N.E. Effects and Side Effects of Using Sorafenib and Sunitinib in the Treatment of Metastatic Renal Cell Carcinoma. Int. J. Mol. Sci. 2017, 18, 461. [Google Scholar] [CrossRef] [PubMed]
- Højer Wang, L.; Wehland, M.; Wise, P.M.; Infanger, M.; Grimm, D.; Kreissl, M.C. Cabozantinib, Vandetanib, Pralsetinib and Selpercatinib as Treatment for Progressed Medullary Thyroid Cancer with a Main Focus on Hypertension as Adverse Effect. Int. J. Mol. Sci. 2023, 24, 2312. [Google Scholar] [CrossRef]
- Vallilas, C.; Sarantis, P.; Kyriazoglou, A.; Koustas, E.; Theocharis, S.; Papavassiliou, A.G.; Karamouzis, M.V. Gastrointestinal Stromal Tumors (GISTs): Novel Therapeutic Strategies with Immunotherapy and Small Molecules. Int. J. Mol. Sci. 2021, 22, 493. [Google Scholar] [CrossRef]
- Molhoek, K.R.; Erdag, G.; Rasamny, J.; Murphy, C.; Deacon, D.; Patterson, J.W.; Slingluff, C.L.; Brautigan, D.L. VEGFR-2 Expression in Human Melanoma: Revised Assessment. Int. J. Cancer 2011, 129, 2807–2815. [Google Scholar] [CrossRef]
- Pfeiffer, P.; Liposits, G.; Taarpgaard, L.S. Angiogenesis Inhibitors for Metastatic Colorectal Cancer. Transl. Cancer Res. 2023, 12, 3241. [Google Scholar] [CrossRef]
- Zhai, B.; Sun, X.Y. Mechanisms of Resistance to Sorafenib and the Corresponding Strategies in Hepatocellular Carcinoma. World J. Hepatol. 2013, 5, 345. [Google Scholar] [CrossRef]
- Li, Y.; Gao, Z.H.; Qu, X.J. The Adverse Effects of Sorafenib in Patients with Advanced Cancers. Basic Clin. Pharmacol. Toxicol. 2015, 116, 216–221. [Google Scholar] [CrossRef] [PubMed]
- Hayman, S.R.; Leung, N.; Grande, J.P.; Garovic, V.D. Vegf Inhibition, Hypertension, and Renal Toxicity. Curr. Oncol. Rep. 2012, 14, 285–294. [Google Scholar] [CrossRef]
- Jiang, L.; Li, L.; Liu, Y.; Lu, L.; Zhan, M.; Yuan, S.; Liu, Y. Drug Resistance Mechanism of Kinase Inhibitors in the Treatment of Hepatocellular Carcinoma. Front. Pharmacol. 2023, 14, 1097277. [Google Scholar] [CrossRef] [PubMed]
- Berman, H.M.; Westbrook, J.; Feng, Z.; Gilliland, G.; Bhat, T.N.; Weissig, H.; Shindyalov, I.N.; Bourne, P.E. The Protein Data Bank. Nucleic Acids Res. 2000, 28, 235–242. [Google Scholar] [CrossRef]
- Kettle, J.G.; Anjum, R.; Barry, E.; Bhavsar, D.; Brown, C.; Boyd, S.; Campbell, A.; Goldberg, K.; Grondine, M.; Guichard, S.; et al. Discovery of N-(4-{[5-Fluoro-7-(2-Methoxyethoxy)Quinazolin-4-Yl]Amino}phenyl)-2-[4-(Propan-2-Yl)-1 H-1,2,3-Triazol-1-Yl]Acetamide (AZD3229), a Potent Pan-KIT Mutant Inhibitor for the Treatment of Gastrointestinal Stromal Tumors. J. Med. Chem. 2018, 61, 8797–8810. [Google Scholar] [CrossRef]
- Okamoto, K.; Ikemori-Kawada, M.; Jestel, A.; Von König, K.; Funahashi, Y.; Matsushima, T.; Tsuruoka, A.; Inoue, A.; Matsui, J. Distinct Binding Mode of Multikinase Inhibitor Lenvatinib Revealed by Biochemical Characterization. ACS Med. Chem. Lett. 2015, 6, 89–94. [Google Scholar] [CrossRef]
- McTigue, M.; Murray, B.W.; Chen, J.H.; Deng, Y.-L.; Solowiej, J.; Kania, R.S. Molecular Conformations, Interactions, and Properties Associated with Drug Efficiency and Clinical Performance among VEGFR TK Inhibitors. Proc. Natl. Acad. Sci. USA 2012, 109, 18281–18289. [Google Scholar] [CrossRef] [PubMed]
- Eldehna, W.M.; Abou-Seri, S.M.; El Kerdawy, A.M.; Ayyad, R.R.; Hamdy, A.M.; Ghabbour, H.A.; Ali, M.M.; Abou El Ella, D.A. Increasing the Binding Affinity of VEGFR-2 Inhibitors by Extending Their Hydrophobic Interaction with the Active Site: Design, Synthesis and Biological Evaluation of 1-Substituted-4-(4-Methoxybenzyl)Phthalazine Derivatives. Eur. J. Med. Chem. 2016, 113, 50–62. [Google Scholar] [CrossRef]
- Zhao, Z.; Wu, H.; Wang, L.; Liu, Y.; Knapp, S.; Liu, Q.; Gray, N.S. Exploration of Type II Binding Mode: A Privileged Approach for Kinase Inhibitor Focused Drug Discovery? ACS Chem. Biol. 2014, 9, 1230–1241. [Google Scholar] [CrossRef]
- Modi, S.J.; Kulkarni, V.M. Exploration of Structural Requirements for the Inhibition of VEGFR-2 Tyrosine Kinase: Binding Site Analysis of Type II, ‘DFG-out’ Inhibitors. J. Biomol. Struct. Dyn. 2022, 40, 5712–5727. [Google Scholar] [CrossRef] [PubMed]
- Moradi, M.; Mousavi, A.; Emamgholipour, Z.; Giovannini, J.; Moghimi, S.; Peytam, F.; Honarmand, A.; Bach, S.; Foroumadi, A. Quinazoline-Based VEGFR-2 Inhibitors as Potential Anti-Angiogenic Agents: A Contemporary Perspective of SAR and Molecular Docking Studies. Eur. J. Med. Chem. 2023, 259, 115626. [Google Scholar] [CrossRef] [PubMed]
- Șandor, A.; Ionuț, I.; Marc, G.; Oniga, I.; Eniu, D.; Oniga, O. Structure–Activity Relationship Studies Based on Quinazoline Derivatives as EGFR Kinase Inhibitors (2017–Present). Pharmaceuticals 2023, 16, 534. [Google Scholar] [CrossRef] [PubMed]
- Marc, G.; Stana, A.; Franchini, A.H.; Vodnar, D.C.; Barta, G.; Tertiş, M.; Şanta, I.; Cristea, C.; Pîrnau, A.; Ciorîta, A.; et al. Phenolic Thiazoles with Antioxidant and Antiradical Activity. Synthesis, in Vitro Evaluation, Toxicity, Electrochemical Behavior, Quantum Studies and Antimicrobial Screening. Antioxidants 2021, 10, 1707. [Google Scholar] [CrossRef]
- Hassan, A.; Badr, M.; Hassan, H.A.; Abdelhamid, D.; Abuo-Rahma, G.E.A. Novel 4-(Piperazin-1-Yl)Quinolin-2(1H)-One Bearing Thiazoles with Antiproliferative Activity through VEGFR-2-TK Inhibition. Bioorg. Med. Chem. 2021, 40, 116168. [Google Scholar] [CrossRef] [PubMed]
- Iacovita, C.; Fizeșan, I.; Pop, A.; Scorus, L.; Dudric, R.; Stiufiuc, G.; Vedeanu, N.; Tetean, R.; Loghin, F.; Stiufiuc, R.; et al. In Vitro Intracellular Hyperthermia of Iron Oxide Magnetic Nanoparticles, Synthesized at High Temperature by a Polyol Process. Pharmaceutics 2020, 12, 424. [Google Scholar] [CrossRef]
- Waterhouse, A.; Bertoni, M.; Bienert, S.; Studer, G.; Tauriello, G.; Gumienny, R.; Heer, F.T.; De Beer, T.A.P.; Rempfer, C.; Bordoli, L.; et al. SWISS-MODEL: Homology Modelling of Protein Structures and Complexes. Nucleic Acids Res. 2018, 46, W296–W303. [Google Scholar] [CrossRef]
- Trott, O.; Olson, A.J. AutoDock Vina: Improving the Speed and Accuracy of Docking with a New Scoring Function, Efficient Optimization, and Multithreading. J. Comput. Chem. 2010, 31, 455–461. [Google Scholar] [CrossRef]
- Stoica, C.I.; Marc, G.; Pîrnău, A.; Vlase, L.; Araniciu, C.; Oniga, S.; Palage, M.; Oniga, O. Thiazolyl-Oxadiazole Derivatives Targeting Lanosterol 14α-Demethylase as Potential Antifungal Agents: Design, Synthesis and Molecular Docking Studies. Farmacia 2016, 64, 390–397. [Google Scholar]
- Morris, G.M.; Huey, R.; Lindstrom, W.; Sanner, M.F.; Belew, R.K.; Goodsell, D.S.; Olson, A.J. AutoDock4 and AutoDockTools4: Automated Docking with Selective Receptor Flexibility. J. Comput. Chem. 2009, 30, 2785–2791. [Google Scholar] [CrossRef]
- Baammi, S.; El Allali, A.; Daoud, R. Unleashing Nature’s Potential: A Computational Approach to Discovering Novel VEGFR-2 Inhibitors from African Natural Compound Using Virtual Screening, ADMET Analysis, Molecular Dynamics, and MMPBSA Calculations. Front. Mol. Biosci. 2023, 10, 1227643. [Google Scholar] [CrossRef]
- Altschul, S.F.; Madden, T.L.; Schaffer, A.A.; Zhang, J.; Zhang, Z.; Miller, W.; Lipman, D.J. Gapped BLAST and PSI-BLAST: A New Generation of Protein Database Search Programs. Nucleic Acids Res. 1997, 25, 3389–3402. [Google Scholar] [CrossRef]
- O’Boyle, N.M.; Banck, M.; James, C.A.; Morley, C.; Vandermeersch, T.; Hutchison, G.R. Open Babel: An Open Chemical Toolbox. J. Cheminform. 2011, 3, 33. [Google Scholar] [CrossRef]
- Velázquez-Libera, J.L.; Durán-Verdugo, F.; Valdés-Jiménez, A.; Núñez-Vivanco, G.; Caballero, J. LigRMSD: A Web Server for Automatic Structure Matching and RMSD Calculations among Identical and Similar Compounds in Protein-Ligand Docking. Bioinformatics 2020, 36, 2912–2914. [Google Scholar] [CrossRef]
- Pettersen, E.F.; Goddard, T.D.; Huang, C.C.; Couch, G.S.; Greenblatt, D.M.; Meng, E.C.; Ferrin, T.E. UCSF Chimera—A Visualization System for Exploratory Research and Analysis. J. Comput. Chem. 2004, 25, 1605–1612. [Google Scholar] [CrossRef]
- Vanommeslaeghe, K.; Hatcher, E.; Acharya, C.; Kundu, S.; Zhong, S.; Shim, J.; Darian, E.; Guvench, O.; Lopes, P.; Vorobyov, I.; et al. CHARMM General Force Field: A Force Field for Drug-like Molecules Compatible with the CHARMM All-Atom Additive Biological Force Fields. J. Comput. Chem. 2009, 31, 671–690. [Google Scholar] [CrossRef]
- Abraham, M.J.; Murtola, T.; Schulz, R.; Páll, S.; Smith, J.C.; Hess, B.; Lindahl, E. GROMACS: High Performance Molecular Simulations through Multi-Level Parallelism from Laptops to Supercomputers. SoftwareX 2015, 1–2, 19–25. [Google Scholar] [CrossRef]
- Revankar, A.G.; Bagewadi, Z.K.; Shaikh, I.A.; Mannasaheb, B.A.; Ghoneim, M.M.; Khan, A.A.; Asdaq, S.M.B. In-Vitro and Computational Analysis of Urolithin-A for Anti-Inflammatory Activity on Cyclooxygenase 2 (COX-2). Saudi J. Biol. Sci. 2023, 30, 103804. [Google Scholar] [CrossRef] [PubMed]
- Shadakshari, A.J.; Suresha Kumara, T.H.; Kumar, N.; Jagadeep Chandra, S.; Anil Kumar, K.M.; Ramu, R. Synthesis, Characterization, and Biocomputational Assessment of the Novel 3-Hydroxy-4-(Phenyl(Pyridin-2-Ylamino) Methyl)-2-Naphthoic Acid Derivatives as Potential Dual Inhibitors of α-Glucosidase and α-Amylase Enzymes. Results Chem. 2023, 5, 100745. [Google Scholar] [CrossRef]
- Ahmad Mir, S.; Meher, R.K.; Baitharu, I.; Nayak, B. Molecular Dynamic Simulation, Free Binding Energy Calculation of Thiazolo-[2,3-b]Quinazolinone Derivatives against EGFR-TKD and Their Anticancer Activity. Results Chem. 2022, 4, 100418. [Google Scholar] [CrossRef]
- Lv, Z.; Wang, H.S.; Niu, X.D. Molecular Dynamics Simulations Reveal Insight into Key Structural Elements of Aaptamines as Sortase Inhibitors with Free Energy Calculations. Chem. Phys. Lett. 2013, 585, 171–177. [Google Scholar] [CrossRef]
- Jin, H.; Zhou, Z.; Wang, D.; Guan, S.; Han, W. Molecular Dynamics Simulations of Acylpeptide Hydrolase Bound to Chlorpyrifosmethyl Oxon and Dichlorvos. Int. J. Mol. Sci. 2015, 16, 6217–6234. [Google Scholar] [CrossRef] [PubMed]
- Crișan, O. Synthesis and in silico approaches of new symmetric bis-thiazolidine-2,4-diones as Ras and Raf oncoproteins inhibitors. Farmacia 2023, 71, 254–263. [Google Scholar] [CrossRef]
- Bussi, G.; Donadio, D.; Parrinello, M. Canonical Sampling through Velocity Rescaling. J. Chem. Phys. 2007, 126, 014101. [Google Scholar] [CrossRef] [PubMed]
- Parrinello, M.; Rahman, A. Polymorphic Transitions in Single Crystals: A New Molecular Dynamics Method. J. Appl. Phys. 1981, 52, 7182–7190. [Google Scholar] [CrossRef]
- Meng, F. Molecular Dynamics Simulation of VEGFR2 with Sorafenib and Other Urea-Substituted Aryloxy Compounds. J. Theor. Chem. 2013, 2013, 739574. [Google Scholar] [CrossRef]
- Elrazaz, E.Z.; Serya, R.A.T.; Ismail, N.S.M.; Albohy, A.; Abou El Ella, D.A.; Abouzid, K.A.M. Discovery of Potent Thieno [2,3-d]Pyrimidine VEGFR-2 Inhibitors: Design, Synthesis and Enzyme Inhibitory Evaluation Supported by Molecular Dynamics Simulations. Bioorg. Chem. 2021, 113, 105019. [Google Scholar] [CrossRef]
- Valdés-Tresanco, M.S.; Valdés-Tresanco, M.E.; Valiente, P.A.; Moreno, E. Gmx_MMPBSA: A New Tool to Perform End-State Free Energy Calculations with GROMACS. J. Chem. Theory Comput. 2021, 17, 6281–6291. [Google Scholar] [CrossRef]
- Case, D.A.; Cheatham, T.E.; Darden, T.; Gohlke, H.; Luo, R.; Merz, K.M.; Onufriev, A.; Simmerling, C.; Wang, B.; Woods, R.J. The Amber Biomolecular Simulation Programs. J. Comput. Chem. 2005, 26, 1668–1688. [Google Scholar] [CrossRef] [PubMed]
- Ahmad Mir, S.; Paramita Mohanta, P.; Kumar Meher, R.; Baitharu, I.; Kumar Raval, M.; Kumar Behera, A.; Nayak, B. Structural Insights into Conformational Stability and Binding of Thiazolo-[2,3-b] Quinazolinone Derivatives with EGFR-TKD and in-Vitro Study. Saudi J. Biol. Sci. 2022, 29, 103478. [Google Scholar] [CrossRef] [PubMed]
- Janani, S.; Rajagopal, H.; Muthu, S.; Aayisha, S.; Raja, M. Molecular Structure, Spectroscopic (FT-IR, FT-Raman, NMR), HOMO-LUMO, Chemical Reactivity, AIM, ELF, LOL and Molecular Docking Studies on 1-Benzyl-4-(N-Boc-Amino)Piperidine. J. Mol. Struct. 2021, 1230, 129657. [Google Scholar] [CrossRef]
- Yue, P.Y.K.; Leung, E.P.Y.; Mak, N.K.; Wong, R.N.S. A Simplified Method for Quantifying Cell Migration/Wound Healing in 96-Well Plates. J. Biomol. Screen. 2010, 15, 427–433. [Google Scholar] [CrossRef] [PubMed]
- IKOSA Prisma Application Wound Healing (Scratch) Assay (v2.2.0). Available online: https://www.kmlvision.com/ (accessed on 14 January 2024).
- Annese, T.; Tamma, R.; Ribatti, D. IKOSA® CAM Assay Application to Quantify Blood Vessels on Chick Chorioallantoic Membrane (CAM). Methods Mol. Biol. 2023, 2572, 129–139. [Google Scholar] [CrossRef] [PubMed]
- Daina, A.; Michielin, O.; Zoete, V. SwissADME: A Free Web Tool to Evaluate Pharmacokinetics, Drug-Likeness and Medicinal Chemistry Friendliness of Small Molecules. Sci. Rep. 2017, 7, 42717. [Google Scholar] [CrossRef] [PubMed]
- Ronald, H.; Klaus, K. WO2020140001A1—Quinazoline Derivatives as Ectonucleotide Pyrophosphatase Phosphodiesterase 1 Inhibitors. U.S. Patent Application No. 17/415,584, 27 December 2019. [Google Scholar]
- Pingaew, R.; Prachayasittikul, S.; Ruchirawat, S. Synthesis, Cytotoxic and Antimalarial Activities of Benzoyl Thiosemicarbazone Analogs of Isoquinoline and Related Compounds. Molecules 2010, 15, 988–996. [Google Scholar] [CrossRef]
- De Moraes Gomes, P.A.T.; Oliveira, A.R.; De Oliveira Cardoso, M.V.; De Farias Santiago, E.; De Oliveira Barbosa, M.; De Siqueira, L.R.P.; Moreira, D.R.M.; Bastos, T.M.; Brayner, F.A.; Soares, M.B.P.; et al. Phthalimido-Thiazoles as Building Blocks and Their Effects on the Growth and Morphology of Trypanosoma Cruzi. Eur. J. Med. Chem. 2016, 111, 46–57. [Google Scholar] [CrossRef] [PubMed]
- El-Adl, K.; Ibrahim, M.K.; Khedr, F.; Abulkhair, H.S.; Eissa, I.H. Design, Synthesis, Docking, and Anticancer Evaluations of Phthalazines as VEGFR-2 Inhibitors. Arch. Pharm. 2022, 355, 2100278. [Google Scholar] [CrossRef]
- Liu, L.; Qin, S.; Zheng, Y.; Han, L.; Zhang, M.; Luo, N.; Liu, Z.; Gu, N.; Gu, X.; Yin, X. Molecular Targeting of VEGF/VEGFR Signaling by the Anti-VEGF Monoclonal Antibody BD0801 Inhibits the Growth and Induces Apoptosis of Human Hepatocellular Carcinoma Cells in Vitro and in Vivo. Cancer Biol. Ther. 2017, 18, 166–176. [Google Scholar] [CrossRef]
- Huang, A.; Yang, X.R.; Chung, W.Y.; Dennison, A.R.; Zhou, J. Targeted Therapy for Hepatocellular Carcinoma. Signal Transduct. Target. Ther. 2020, 5, 143. [Google Scholar] [CrossRef]
- Aranda, E.; Owen, G.I. A Semi-Quantitative Assay to Screen for Angiogenic Compounds and Compounds with Angiogenic Potential Using the EA.Hy926 Endothelial Cell Line. Biol. Res. 2009, 42, 377–389. [Google Scholar] [CrossRef] [PubMed]
- Stolbovaya, A.Y.; Smirnov, I.V.; Pinevich, A.A.; Vartanyan, N.L.; Krutetskaya, I.Y.; Terekhina, L.A.; Markova, K.L.; Malashicheva, A.B.; Samoilovich, M.P. Comparative Analysis of HUVEC and EA.Hy926 Functional Characteristics under the Influence of Anti-Endoglin Antibodies. Cell Tissue Biol. 2021, 15, 503–517. [Google Scholar] [CrossRef]
- Ishak, R.S.; Aad, S.A.; Kyei, A.; Farhat, F.S. Cutaneous Manifestations of Anti-Angiogenic Therapy in Oncology: Review with Focus on VEGF Inhibitors. Crit. Rev. Oncol. Hematol. 2014, 90, 152–164. [Google Scholar] [CrossRef]
- Wang, Y.; Peng, C.; Wang, G.; Xu, Z.; Luo, Y.; Wang, J.; Zhu, W. Exploring Binding Mechanisms of VEGFR2 with Three Drugs Lenvatinib, Sorafenib, and Sunitinib by Molecular Dynamics Simulation and Free Energy Calculation. Chem. Biol. Drug Des. 2019, 93, 934–948. [Google Scholar] [CrossRef]
- Fathima Rizwana, B.; Prasana, J.C.; Abraham, C.S.; Muthu, S. Spectroscopic Investigation, Hirshfeld Surface Analysis and Molecular Docking Studies on Anti-Viral Drug Entecavir. J. Mol. Struct. 2018, 1164, 447–458. [Google Scholar] [CrossRef]
- Banavath, H.N.; Sharma, O.P.; Kumar, M.S.; Baskaran, R. Identification of Novel Tyrosine Kinase Inhibitors for Drug Resistant T315I Mutant BCR-ABL: A Virtual Screening and Molecular Dynamics Simulations Study. Sci. Rep. 2014, 4, 6948. [Google Scholar] [CrossRef]
- Maluleka, M.M.; Mokoena, T.P.; Mampa, R.R. Synthesis, Crystal, and Hirschfeld Surface, DFT and Molecular Docking Studies of 6-(3-chloro-4-Fluorophenyl)-4-Ethoxy-2-(4-Methoxyphenyl)Quinazoline Derivative. J. Mol. Struct. 2022, 1255, 132439. [Google Scholar] [CrossRef]
- Balogun, T.A.; Ipinloju, N.; Abdullateef, O.T.; Moses, S.I.; Omoboyowa, D.A.; James, A.C.; Saibu, O.A.; Akinyemi, W.F.; Oni, E.A. Computational Evaluation of Bioactive Compounds from Colocasia Affinis Schott as a Novel EGFR Inhibitor for Cancer Treatment. Cancer Inform. 2021, 20, 11769351211049244. [Google Scholar] [CrossRef] [PubMed]
- Thirumurugan, K.; Lakshmanan, S.; Govindaraj, D.; Daniel Prabu, D.S.; Ramalakshmi, N.; Arul Antony, S. Design, Synthesis and Anti-Inflammatory Activity of Pyrimidine Scaffold Benzamide Derivatives as Epidermal Growth Factor Receptor Tyrosine Kinase Inhibitors. J. Mol. Struct. 2018, 1171, 541–550. [Google Scholar] [CrossRef]
- Venugopal, P.P.; Das, B.K.; Soorya, E.; Chakraborty, D. Effect of Hydrophobic and Hydrogen Bonding Interactions on the Potency of SS-Alanine Analogs of G-Protein Coupled Glucagon Receptor Inhibitors. Proteins Struct. Funct. Bioinforma. 2020, 88, 327–344. [Google Scholar] [CrossRef]
- Padmaja, L.; Ravikumar, C.; Sajan, D.; Joe, I.H.; Jayakumar, V.S.; Pettit, G.R.; Nielsen, O.F. Density Functional Study on the Structural Conformations and Intramolecular Charge Transfer from the Vibrational Spectra of the Anticancer Drug Combretastatin-A2. J. Raman Spectrosc. 2009, 40, 419–428. [Google Scholar] [CrossRef]
- Alnoman, R.B.; Parveen, S.; Khan, A.; Knight, J.G.; Hagar, M. New Quinoline-Based BODIPYs as EGFR/VEGFR-2 Inhibitors: Molecular Docking, DFT and in Vitro Cytotoxicity on HeLa Cells. J. Mol. Struct. 2022, 1247, 131312. [Google Scholar] [CrossRef]
- Parthasarathi, R.; Subramanian, V.; Roy, D.R.; Chattaraj, P.K. Electrophilicity Index as a Possible Descriptor of Biological Activity. Bioorg. Med. Chem. 2004, 12, 5533–5543. [Google Scholar] [CrossRef]
- Jaramillo, P.; Domingo, L.R.; Chamorro, E.; Pérez, P. A Further Exploration of a Nucleophilicity Index Based on the Gas-Phase Ionization Potentials. J. Mol. Struct. Theochem. 2008, 865, 68–72. [Google Scholar] [CrossRef]
- Eissa, I.H.; Yousef, R.G.; Elkady, H.; Elkaeed, E.B.; Alsfouk, B.A.; Husein, D.Z.; Asmaey, M.A.; Ibrahim, I.M.; Metwaly, A.M. Anti-Breast Cancer Potential of a New Xanthine Derivative: In Silico, Antiproliferative, Selectivity, VEGFR-2 Inhibition, Apoptosis Induction and Migration Inhibition Studies. Pathol. Res. Pract. 2023, 251, 154894. [Google Scholar] [CrossRef]
- Lauffenburger, D.A.; Horwitz, A.F. Cell Migration: A Physically Integrated Molecular Process. Cell 1996, 84, 359–369. [Google Scholar] [CrossRef]
- Lipinski, C.A.; Lombardo, F.; Dominy, B.W.; Feeney, P.J. Experimental and Computational Approaches to Estimate Solubility and Permeability in Drug Discovery and Development Settings. Adv. Drug Deliv. Rev. 1997, 23, 3–25. [Google Scholar] [CrossRef]
- Veber, D.F.; Johnson, S.R.; Cheng, H.Y.; Smith, B.R.; Ward, K.W.; Kopple, K.D. Molecular Properties That Influence the Oral Bioavailability of Drug Candidates. J. Med. Chem. 2002, 45, 2615–2623. [Google Scholar] [CrossRef]
- Khan, M.A.; Raza, A.; Ovais, M.; Sohail, M.F.; Ali, S. Current State and Prospects of Nano-Delivery Systems for Sorafenib. Int. J. Polym. Mater. Polym. Biomater. 2018, 67, 1105–1115. [Google Scholar] [CrossRef]
- Elder, D.P.; Delaney, E.; Teasdale, A.; Eyley, S.; Reif, V.D.; Jacq, K.; Facchine, K.L.; Oestrich, R.S.; Sandra, P.; David, F. The Utility of Sulfonate Salts in Drug Development. J. Pharm. Sci. 2010, 99, 2948–2961. [Google Scholar] [CrossRef]


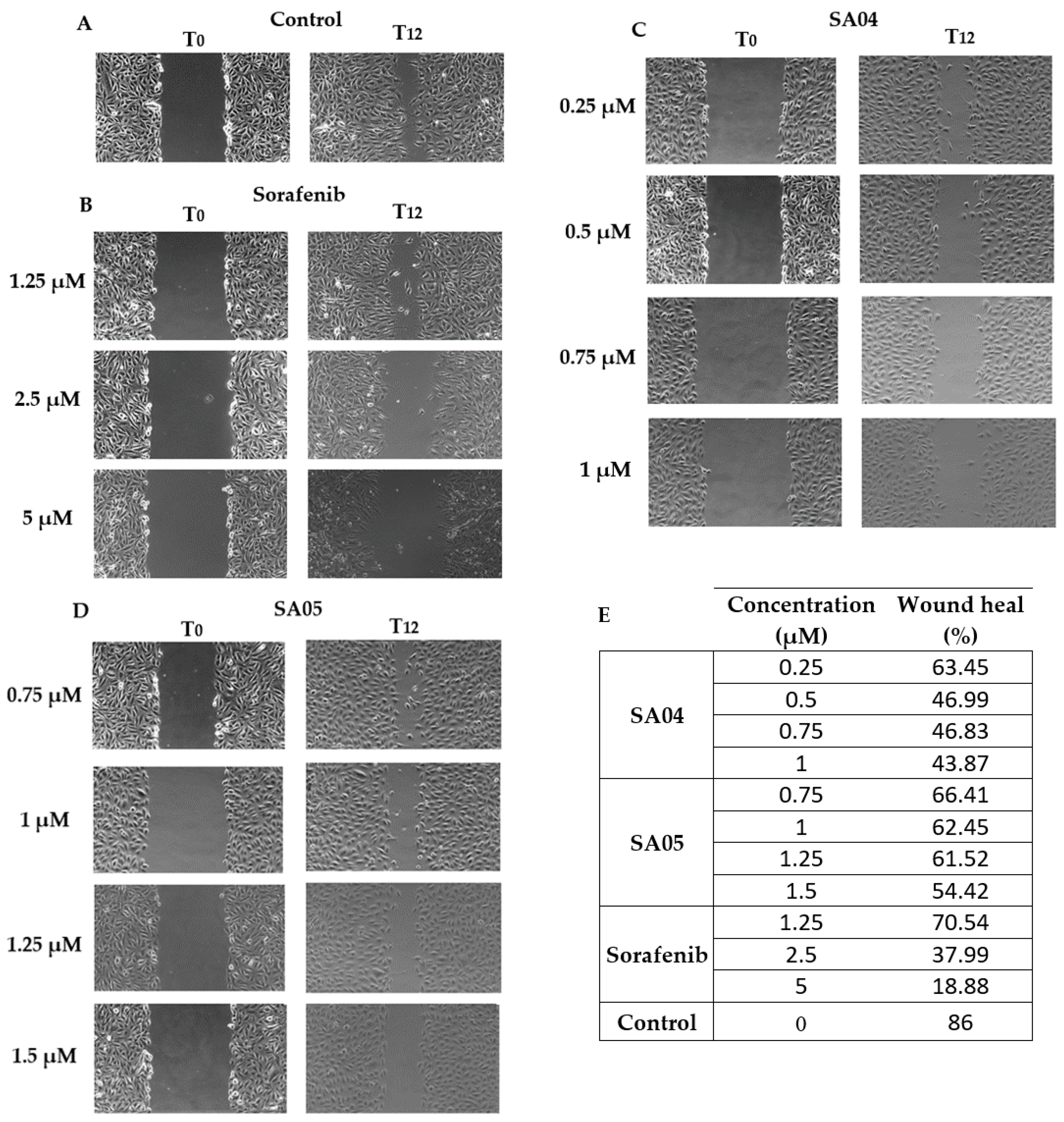
| Comp. | Evaluated Cell Lines | Selectivity Index | |||
|---|---|---|---|---|---|
| EA.hy926 | HepG2 | BJ | 1 SIa | 2 SIb | |
| SA01 | 3.64 | 31.20 | 36.25 | 9.96 | 1.16 |
| SA02 | 0.93 | 2.34 | 2.35 | 2.53 | 1.00 |
| SA03 | 0.79 | 4.24 | 2.84 | 3.59 | 0.67 |
| SA04 | 0.98 | 2.72 | 6.79 | 6.93 | 2.50 |
| SA05 | 1.40 | 1.83 | 2.67 | 1.91 | 1.46 |
| SA06 | >10 | >100 | >100 | - | - |
| SA07 | 5.85 | 27.30 | 23.76 | 4.06 | 0.87 |
| Sorafenib | 6.62 | 6.28 | 13.24 | 2.00 | 2.11 |
| System Evaluated | RMSD—Protein (nm) 1 | RMSF Amino Acid αCarbons (nm) 2 | RMSF Amino Acid Sidechains (nm) 3 | RMSD—Ligand (nm) 4 | Rg Protein(nm) 5 | NoHB Protein–Ligand (no/ns) 6 |
|---|---|---|---|---|---|---|
| apo VEGFR2 receptor + SA01 | 0.22 | 0.11 | 0.17 | 0.17 | 2.07 | 0.98 |
| apo VEGFR2 receptor + SA02 | 0.21 | 0.12 | 0.17 | 0.10 | 2.06 | 0.91 |
| apo VEGFR2 receptor + SA03 | 0.16 | 0.10 | 0.15 | 0.13 | 2.04 | 0.94 |
| apo VEGFR2 receptor + SA04 | 0.23 | 0.11 | 0.16 | 0.10 | 2.06 | 0.98 |
| apo VEGFR2 receptor + SA05 | 0.19 | 0.10 | 0.16 | 0.10 | 2.05 | 0.99 |
| apo VEGFR2 receptor + SA06 | 0.31 | 0.09 | 0.14 | 0.19 | 2.07 | 0.98 |
| apo VEGFR2 receptor + SA07 | 0.23 | 0.16 | 0.21 | 0.15 | 2.03 | 1.60 |
| apo VEGFR2 receptor + SFN | 0.18 | 0.13 | 0.17 | 0.12 | 2.05 | 1.00 |
| Number of H-Bond Interactions (% of Total Interactions) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Lys868 | Glu885 | Cys919 | Cys1024 | Ile1025 | His1026 | Arg1027 | Asp1046 | Total H-Bonds | |
| SA01 | 18 (0.18%) | 6959 (69.59%) | 1762 (17.62%) | - | 194 (1.94%) | - | - | 882 (8.82%) | 9815 |
| SA02 | 18 (0.20%) | 6605 (66.05%) | 1525 (15.25%) | - | - | - | 2 (0.02%) | 946 (9.46%) | 9096 |
| SA03 | 20 (0.21%) | 7066 (70.66%) | 1300 (13.00%) | - | 1 (0.01%) | - | 137 (1.37%) | 839 (8.39%) | 9363 |
| SA04 | 3 (0.03%) | 7556 (75.56%) | 1275 (12.75%) | 3 (0.03%) | 20 (0.20%) | - | 10 (0.10%) | 876 (8.76%) | 9743 |
| SA05 | 5 (0.05%) | 7329 (73.29%) | 1389 (13.75%) | - | 88 (0.88%) | - | 11 (0.11%) | 1082 (10.82%) | 9904 |
| SA06 | 56 (0.57%) | 7493 (74.93%) | 1590 (15.75%) | - | - | - | - | 669 (6.69%) | 9808 |
| SA07 | 4 (0.02%) | 7355 (73.55%) | 1886 (18.86%) | - | 5288 (52.88%) | - | 495 (4.95%) | 1011 (10.11%) | 16039 |
| Sorafenib | - | 3825 (38.25%) | 178 (1.78%) | 13 (0.13%) | - | 13 (0.13%) | - | 5833 (58.33%) | 9866 |
| Compound | ΔG (±SD *) | van der Waals (±SD *) | Electrostatic (±SD *) | Solvation (±SD *) |
|---|---|---|---|---|
| SA02 | −65.38 ± 4.13 | −58.48 ± 3.26 | −32.95 ± 3.93 | 26.06 ± 3.24 |
| SA03 | −47.20 ± 11.74 | −46.68 ± 10.66 | −24.37 ± 3.94 | 23.84 ± 3.65 |
| SA04 | −64.21 ± 4.18 | −58.87 ± 3.29 | −27.99 ± 4.33 | 22.66 ± 3.45 |
| SA05 | −71.23 ± 5.29 | −64.37 ± 3.33 | −33.84 ± 4.39 | 26.97 ± 3.58 |
| sorafenib | −69.39 ± 3.63 | −59.19 ± 2.81 | −39.67 ± 3.76 | 29.47 ± 2.65 |
| FMO Analysis | SA01 | SA02 | SA03 | SA04 | SA05 | SA06 | SA07 | Sorafenib |
|---|---|---|---|---|---|---|---|---|
| HOMO (eV) | −5.08 | −5.3 | −5.37 | −5.47 | −5.57 | −5.26 | −5.22 | −6.04 |
| LUMO (eV) | −1.5 | −1.55 | −1.95 | −1.63 | −1.73 | −1.49 | −1.54 | −1.45 |
| Energy gap (eV) | 3.58 | 3.75 | 3.42 | 3.84 | 3.84 | 3.77 | 3.68 | 4.59 |
| Chemical reactivity descriptors | ||||||||
| Ionization potential (I) (eV) | 5.08 | 5.3 | 5.37 | 5.47 | 5.57 | 5.26 | 5.22 | 6.04 |
| Electronic affinity (A) (eV) | 1.5 | 1.55 | 1.95 | 1.63 | 1.73 | 1.49 | 1.54 | 1.45 |
| Chemical potential (μ) (eV) | −3.29 | −3.42 | −3.66 | −3.55 | −3.65 | −3.37 | −3.38 | −3.74 |
| Chemical hardness (η) (eV) | 1.79 | 1.87 | 1.71 | 1.92 | 1.92 | 1.88 | 1.84 | 2.29 |
| Global softness (S) (eV) | 0.89 | 0.93 | 0.85 | 0.96 | 0.96 | 0.94 | 0.92 | 1.14 |
| Electrophilicity index (ω)(eV) | 9.68 | 10.99 | 11.45 | 12.09 | 12.79 | 10.73 | 10.51 | 16.09 |
| Nucleophilicity index (N) (eV−1) | 0.10 | 0.09 | 0.08 | 0.08 | 0.07 | 0.09 | 0.09 | 0.06 |
| Additional electronic charges (∆N) | 1.83 | 1.82 | 2.14 | 1.84 | 1.90 | 1.79 | 1.83 | 1.63 |
| Dipole moment (Debye) | 2.96 | 2.71 | 3.06 | 3.74 | 5.59 | 2.84 | 5.35 | 6.68 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Șandor, A.; Fizeșan, I.; Ionuț, I.; Marc, G.; Moldovan, C.; Oniga, I.; Pîrnău, A.; Vlase, L.; Petru, A.-E.; Macasoi, I.; et al. Discovery of A Novel Series of Quinazoline–Thiazole Hybrids as Potential Antiproliferative and Anti-Angiogenic Agents. Biomolecules 2024, 14, 218. https://doi.org/10.3390/biom14020218
Șandor A, Fizeșan I, Ionuț I, Marc G, Moldovan C, Oniga I, Pîrnău A, Vlase L, Petru A-E, Macasoi I, et al. Discovery of A Novel Series of Quinazoline–Thiazole Hybrids as Potential Antiproliferative and Anti-Angiogenic Agents. Biomolecules. 2024; 14(2):218. https://doi.org/10.3390/biom14020218
Chicago/Turabian StyleȘandor, Alexandru, Ionel Fizeșan, Ioana Ionuț, Gabriel Marc, Cristina Moldovan, Ilioara Oniga, Adrian Pîrnău, Laurian Vlase, Andreea-Elena Petru, Ioana Macasoi, and et al. 2024. "Discovery of A Novel Series of Quinazoline–Thiazole Hybrids as Potential Antiproliferative and Anti-Angiogenic Agents" Biomolecules 14, no. 2: 218. https://doi.org/10.3390/biom14020218
APA StyleȘandor, A., Fizeșan, I., Ionuț, I., Marc, G., Moldovan, C., Oniga, I., Pîrnău, A., Vlase, L., Petru, A.-E., Macasoi, I., & Oniga, O. (2024). Discovery of A Novel Series of Quinazoline–Thiazole Hybrids as Potential Antiproliferative and Anti-Angiogenic Agents. Biomolecules, 14(2), 218. https://doi.org/10.3390/biom14020218










