Association Between Coffee Consumption and Metabolic Syndrome Components Among Saudi Adults
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population and Design
2.2. Anthropometric Measurements and Definition of MetS
2.3. Assessment of Other Covariates
2.4. Data Analysis
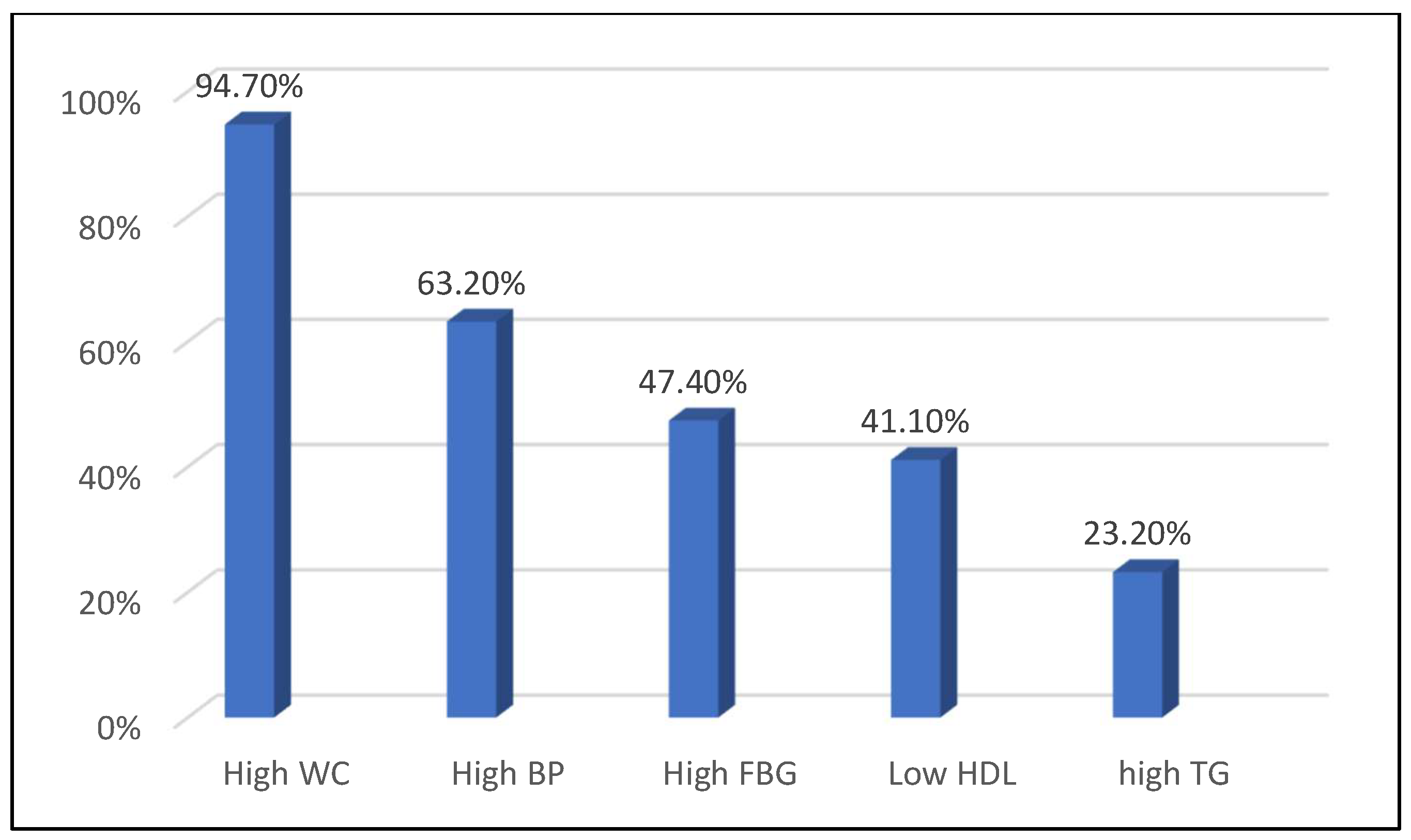
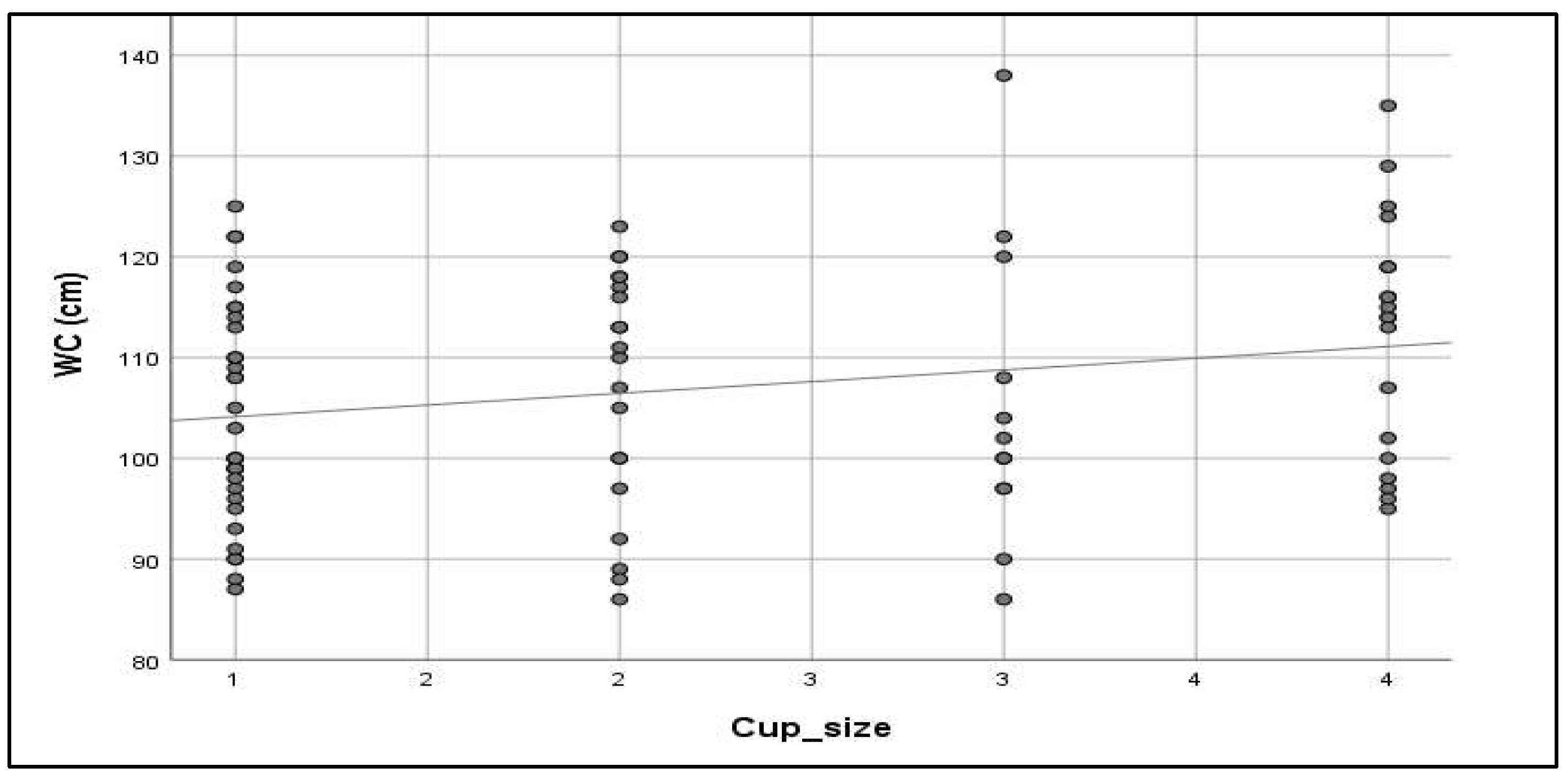
3. Results
4. Discussion
4.1. Study Strengths
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| HDL-C | High-density lipoprotein cholesterol |
| LDL-C | Low-density lipoprotein cholesterol |
| TC | Total cholesterol |
| TG | Triglyceride |
| HbA1c | Hemoglobin A1c |
| FBG | Fasting blood glucose |
| WC | Waist circumference |
| BP | Blood glucose |
References
- Islam, M.S.; Wei, P.; Suzauddula, M.; Nime, I.; Feroz, F.; Acharjee, M.; Pan, F. The interplay of factors in metabolic syndrome: Understanding its roots and complexity. Mol. Med. 2024, 30, 279. [Google Scholar] [CrossRef]
- Al-Rubeaan, K.; Bawazeer, N.; Al Farsi, Y.; Youssef, A.M.; Al-Yahya, A.A.; AlQumaidi, H.; Al-Malki, B.M.; Naji, K.A.; Al-Shehri, K.; Al Rumaih, F.I. Prevalence of metabolic syndrome in Saudi Arabia—A cross-sectional study. BMC Endocr. Disord. 2018, 18, 16–25. [Google Scholar] [CrossRef] [PubMed]
- Yesil, A.; Yilmaz, Y. Review article: Coffee consumption, the metabolic syndrome and non-alcoholic fatty liver disease. Aliment. Pharmacol. Ther. 2013, 38, 1038–1044. [Google Scholar] [CrossRef] [PubMed]
- SPA Saudi Coffee: Optimal Investment in Promising Sector with 400,000 Trees Enhancing Local Production Chains. Spa.gov.sa. 2023. Available online: https://www.spa.gov.sa/w1881434 (accessed on 20 February 2025).
- Baspinar, B.; Eskici, G.; Ozcelik, A.O. How coffee affects metabolic syndrome and its components. Food Funct. 2017, 8, 2089–2101. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Lee, E.T.; Cowan, L.D.; Fabsitz, R.R.; Howard, B.V. Coffee consumption and the incidence of type 2 diabetes in men and women with normal glucose tolerance: The Strong Heart Study. Nutr. Metab. Cardiovasc. Dis. 2011, 21, 418–423. [Google Scholar] [CrossRef] [PubMed]
- Sarriá, B.; Martínez-López, S.; Sierra-Cinos, J.L.; García-Diz, L.; Mateos, R.; Bravo-Clemente, L. Regularly consuming a green/roasted coffee blend reduces the risk of metabolic syndrome. Eur. J. Nutr. 2018, 57, 269–278. [Google Scholar] [CrossRef]
- Jalal, S.; Alsebeiy, S.; Aleid, H.; Alhamad, S. Effect of Arabic Qahwa on Blood Pressure in Patients with Stage One Hypertension in the Eastern Region of Saudi Arabia. J. Pers. Med. 2023, 13, 1011. [Google Scholar] [CrossRef]
- Takami, H.; Nakamoto, M.; Uemura, H.; Katsuura, S.; Yamaguchi, M.; Hiyoshi, M.; Sawachika, F.; Juta, T.; Arisawa, K. Inverse Correlation Between Coffee Consumption and Prevalence of Metabolic Syndrome: Baseline Survey of the Japan Multi-Institutional Collaborative Cohort (J-MICC) Study in Tokushima, Japan. J. Epidemiol. 2013, 23, 12–20. [Google Scholar] [CrossRef]
- Kempf, K.; Herder, C.; Erlund, I.; Kolb, H.; Martin, S.; Carstensen, M.; Koenig, W.; Sundvall, J.; Bidel, S.; Kuha, S.; et al. Effects of coffee consumption on subclinical inflammation and other risk factors for type 2 diabetes: A clinical trial. Am. J. Clin. Nutr. 2010, 91, 950–957. [Google Scholar] [CrossRef]
- Miranda, A.M.; Steluti, J.; Fisberg, R.M.; Marchioni, D.M. Association between Coffee Consumption and Its Polyphenols with Cardiovascular Risk Factors: A Population-Based Study. Nutrients 2017, 9, 276. [Google Scholar] [CrossRef]
- Lu, M.-Y.; Cheng, H.-Y.; Lai, J.C.-Y.; Chen, S.-J. The Relationship between Habitual Coffee Drinking and the Prevalence of Metabolic Syndrome in Taiwanese Adults: Evidence from the Taiwan Biobank Database. Nutrients 2022, 14, 1867. [Google Scholar] [CrossRef] [PubMed]
- Shin, H.; Linton, J.A.; Kwon, Y.; Jung, Y.; Oh, B.; Oh, S. Relationship between Coffee Consumption and Metabolic Syndrome in Korean Adults: Data from the 2013–2014 Korea National Health and Nutrition Examination Survey. Korean J. Fam. Med. 2017, 38, 346–351. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Kim, H.; Kim, J. Coffee Consumption and the Risk of Obesity in Korean Women. Nutrients 2017, 9, 1340. [Google Scholar] [CrossRef] [PubMed]
- Alshahrani, S.H.; Atia, Y.A.; Badir, R.A.; Almalki, S.G.; Tayyib, N.A.; Shahab, S.; Romero-Parra, R.M.; Abid, M.K.; Hussien, B.M.; Ramaiah, P. Dietary caffeine intake is associated with favorable metabolic profile among apparently healthy overweight and obese individuals. BMC Endocr. Disord. 2023, 23, 227. [Google Scholar] [CrossRef]
- Enani, S.; Bahijri, S.; Malibary, M.; Jambi, H.; Eldakhakhny, B.; Al-Ahmadi, J.; Al Raddadi, R.; Ajabnoor, G.; Boraie, A.; Tuomilehto, J. The Association between Dyslipidemia, Dietary Habits and Other Lifestyle Indicators among Non-Diabetic Attendees of Primary Health Care Centers in Jeddah, Saudi Arabia. Nutrients 2022, 12, 2441. [Google Scholar] [CrossRef]
- Kalel, A.; Almutairi, A.; Alyahiwi, A.; Jalaluddin, A.; Aljohani, M.; Aloufi, R.; Almatrafi, R. Effect of coffee consumption on serum lipid profile among adult population in Madinah, Saudi Arabia. Int. J. Med. Dev. Countries 2020, 8, 1527–1532. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Cut-Off for BMI According to WHO Standards. 2018. Available online: https://gateway.euro.who.int/en/indicators/mn_survey_19-cut-off-for-bmi-according-to-who-standards/#id=32083 (accessed on 20 February 2025).
- Weir, C.B.; Jan, A. BMI Classification Percentile and Cut off Points. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2025. Available online: https://www.ncbi.nlm.nih.gov/sites/books/NBK541070/ (accessed on 20 February 2025).
- Alberti, K.G. International Diabetes Federation Task Force on Epidemiology and Prevention, Hational Heart, Lung, and Blood Institute, American Heart Association, World Heart Federation, International Atherosclerosis Society, & International Association for the Study of Obesity. Harmonizing the metabolic syndrome: A joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009, 120, 1640–1645. [Google Scholar]
- Sherwani, S.I.; Khan, H.A.; Ekhzaimy, A.; Masood, A.; Sakharkar, M.K. Significance of HbA1c Test in Diagnosis and Prognosis of Diabetic Patients. Biomark. Insights 2016, 11, 95–104. [Google Scholar] [CrossRef]
- Irons, J.G.; Bassett, D.T.; Prendergast, C.O.; Landrum, R.E.; Heinz, A.J. Development and initial validation of the Caffeine Consumption Questionnaire-Revised. J. Caffeine Res. 2016, 6, 20–25. [Google Scholar] [CrossRef]
- Nina, R.; Lingling, H.; Qiushuang, L.; Honglin, G.; Liyuan, S.; Yuting, Z. Association of coffee consumption pattern and metabolic syndrome among middle-aged and older adults: A cross-sectional study. Front. Public Health 2023, 11, 1022616. [Google Scholar] [CrossRef]
- Zhao, H.; Wang, S.; Han, Y.; Yao, M.; Zhang, Y.; Zeng, X. Coffee consumption might be associated with lower potential risk and severity of metabolic syndrome: National health and nutrition examination survey 2003–2018. Eur. J. Nutr. 2024, 63, 1705–1718. [Google Scholar] [CrossRef]
- Balk, L.; Hoekstra, T.; Twisk, J. Relationship between long-term coffee consumption and components of the metabolic syndrome: The Amsterdam Growth and Health Longitudinal Study. Eur. J. Epidemiol. 2009, 24, 203–209. [Google Scholar] [CrossRef] [PubMed]
- Chang, H.C.; Nfor, O.N.; Ho, C.C.; Chen, P.H.; Kung, Y.Y.; Hsu, S.Y.; Tantoh, D.M.; Liaw, Y.C.; Hsieh, C.F.; Liaw, Y.P. Changes in High-Density Lipoprotein Cholesterol Levels in Relation to Coffee Consumption Among Taiwanese Adults. J. Multidiscip. Healthc. 2020, 13, 1427–1432. [Google Scholar] [CrossRef] [PubMed]
- Uto-Kondo, H.; Ayaori, M.; Ogura, M.; Nakaya, K.; Ito, M.; Suzuki, A.; Takiguchi, S.; Yakushiji, E.; Terao, Y.; Ozasa, H.; et al. Coffee consumption enhances high-density lipoprotein-mediated cholesterol efflux in macrophages. Circ. Res. 2010, 106, 779–787. [Google Scholar] [CrossRef] [PubMed]
- Panagiotakos, D.B.; Lionis, C.; Zeimbekis, A.; Makri, K.; Bountziouka, V.; Economou, M.; Vlachou, I.; Micheli, M.; Tsakountakis, N.; Metallinos, G.; et al. Long-term, moderate coffee consumption is associated with lower prevalence of diabetes mellitus among elderly non-tea drinkers from the Mediterranean Islands (MEDIS Study). Rev. Diabet. Stud. 2007, 4, 105–112. [Google Scholar] [CrossRef]
- Larsen, S.C.; Mikkelsen, M.L.; Frederiksen, P.; Heitmann, B.L. Habitual coffee consumption and changes in measures of adiposity: A comprehensive study of longitudinal associations. Sci. Rep. 2018, 42, 880–886. [Google Scholar] [CrossRef]
- Jee, S.H.; He, J.; Appel, L.J.; Whelton, P.K.; Suh, I.; Klag, M.J. Coffee consumption and serum lipids: A meta-analysis of randomized controlled clinical trials. Am. J. Epidemiol. 2001, 153, 353–362. [Google Scholar] [CrossRef]
- Karabudak, E.; Türközü, D.; Köksal, E. Association between coffee consumption and serum lipid profile. Exp. Ther. Med. 2015, 9, 1841–1846. [Google Scholar] [CrossRef]
- Tabrizi, R.; Saneei, P.; Lankarani, K.B.; Akbari, M.; Kolahdooz, F.; Esmaillzadeh, A.; Nadi-Ravandi, S.; Mazoochi, M.; Asemi, Z. The effects of caffeine intake on weight loss: A systematic review and dos-response meta-analysis of randomized controlled trials. Crit. Rev. Food Sci. Nutr. 2018, 59, 2688–2696. [Google Scholar] [CrossRef]
- Freedman, N.D.; Park, Y.; Abnet, C.C.; Hollenbeck, A.R.; Sinha, R. Association of Coffee Drinking with Total and Cause-Specific Mortality. N. Engl. J. Med. 2012, 366, 1891–1904. [Google Scholar] [CrossRef]
- Svatun, Å.L.; Løchen, M.L.; Thelle, D.S.; Wilsgaard, T. Association between espresso coffee and serum total cholesterol: The Tromsø Study 2015–2016. Open Heart 2022, 9, e001946. [Google Scholar] [CrossRef] [PubMed]
- Henn, M.; Glenn, A.J.; Willett, W.C.; Martínez-González, M.A.; Sun, Q.; Hu, F.B. Coffee Consumption, Additive Use, and Risk of Type 2 Diabetes- Results from Three Large Prospective US Cohort Studies. Am. J. Clin. Nutr. 2025. Online ahead of print. [Google Scholar]
- Tan, L.J.; Jeon, H.J.; Park, S.; Kim, S.A.; Lim, K.; Chung, S.; Chang, P.S.; Lee, J.K.; Kang, D.; Shin, S. Association of Coffee Consumption and Its Types According to Addition of Sugar and Creamer with Metabolic Syndrome Incidence in a Korean Population from the Health Examinees (HEXA) Study. Nutrients 2021, 13, 920. [Google Scholar] [CrossRef] [PubMed]
- Stutz, B.; Ahola, A.J.; Harjutsalo, V.; Forsblom, C.; Groop, P.H.; FinnDiane Study Group. Association between habitual coffee consumption and metabolic syndrome in type 1 diabetes. Nutr. Metab. Cardiovasc. Dis. 2018, 28, 470–476. [Google Scholar] [CrossRef] [PubMed]
| Coffee Consumption | ||||
|---|---|---|---|---|
| Variable | Categories | Yes (N = 85) | No (N = 10) | p-Value * |
| High WC | No | 4 (4.7%) | 1 (10%) | 0.478 |
| Yes | 81 (95.3%) | 9 (90%) | ||
| High BP | No | 30 (35.3%) | 5 (50%) | 0.362 |
| Yes | 55 (64.7%) | 5 (50%) | ||
| High FBG | No | 45 (52.9%) | 5 (50%) | 0.860 |
| Yes | 40 (47.1%) | 5 (50%) | ||
| Low HDL | No | 47 (55.3%) | 9 (90%) | 0.035 |
| Yes | 38 (44.7%) | 1 (10%) | ||
| High TGs | No | 64 (75.3%) | 9 (90%) | 0.297 |
| Yes | 21 (24.7%) | 1 (10%) | ||
| High WC | High BP | High TGs | Low HDL | High FBG | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes (n = 81) | No (n = 4) | p-Value | Yes (n = 55) | No (n = 30) | p-Value | Yes (n = 21) | No (n = 64) | p-Value | Yes (n = 38) | No (n = 47) | p-Value | Yes (n = 40) | No (n = 45) | p-Value | ||
| Coffee cup size | S | 31 (38.3%) | 1 (25%) | 0.602 | 23 (41.8%) | 9 (30%) | 0.243 | 10 (47.6%) | 22 (34.4%) | 0.022 | 13 (34.2%) | 19 (40.4%) | 0.488 | 15 (37.5%) | 17 (37.8%) | 0.702 |
| M | 19 (23.5%) | 2 (50%) | 11 (20%) | 10 (33.3%) | 1 (4.8%) | 20 (31.3%) | 12 (31.6%) | 9 (19.1%) | 10 (25%) | 11 (24.4%) | ||||||
| L | 12 (14.8%) | 0 | 6 (10.9%) | 6 (20%) | 6 (28.6%) | 6 (9.4%) | 6 (15.8%) | 6 (12.8%) | 4 (10%) | 8 (17.8%) | ||||||
| XL | 19 (23.5%) | 1 (25%) | 15 (27.3%) | 5 (16.7%) | 4 (19%) | 16 (25%) | 7 (13.4%) | 13 (27.7%) | 11 (27.5%) | 9 (20%) | ||||||
| Coffee cups/day | <1 (once a week) | 6 (7.4%) | 0 | 0.429 | 4 (7.3%) | 2 (6.7%) | 0.373 | 2 (7.4%) | 4 (6.3%) | 0.013 | 2 (5.3%) | 4 (8.5%) | 0.605 | 1 (2.5%) | 5 (11.1%) | 0.491 |
| 1 | 30 (37%) | 0 | 18 (32.7%) | 12 (40%) | 3 (37%) | 27 (42.2%) | 12 (31.6%) | 18 (38.3%) | 15 (37.5%) | 15 (33.3%) | ||||||
| 2 | 15 (18.5%) | 1 (25%) | 8 (14.5%) | 8 (26.7%) | 9 (18.5%) | 7 (10.9%) | 10 (26.3%) | 6 (12.8%) | 7 (17.5%) | 9 (20%) | ||||||
| 3 | 15 (18.5%) | 1 (25%) | 11 (20%) | 5 (31.3%) | 3 (18.5%) | 13 (20.3%) | 7 (18.4%) | 9 (19.1%) | 7 (17.5%) | 9 (20%) | ||||||
| > 3 | 15 (18.5%) | 2 (50%) | 14 (25.5%) | 3 (10%) | 4 (18.5%) | 13 (20.3%) | 7 (18.4%) | 10 (21.3%) | 10 (25%) | 7 (15.6%) | ||||||
| Types of coffee | Arabic | 73 (90.1%) | 3 (75%) | 0.243 | 48 (87.3%) | 28 (93.3%) | 0.822 | 21 (100%) | 55 (85.9%) | 0.496 | 34 (89.5%) | 42 (89.4%) | 0.132 | 28 (84.8%) | 48 (92.3%) | 0.522 |
| Cappuccino | 12 (14.8%) | 1 (25%) | 8 (14.5%) | 5 (16.7%) | 4 (19%) | 9 (14.1%) | 6 (15.8%) | 7 (14.9%) | 4 (12.1%) | 9 (17.3%) | ||||||
| Black | 25 (30.9%) | 2 (50%) | 20 (36.4%) | 7 (23.3%) | 7 (33.3%) | 20 (31.3%) | 13 (34.2%) | 14 (29.8%) | 14 (42.4%) | 13 (25%) | ||||||
| Turkish | 8 (9.9%) | 1 (25%) | 7 (12.7%) | 2 (6.7%) | 2 (9.5%) | 7 (10.9%) | 4 (10.5%) | 5 (10.6%) | 3 (9.1%) | 6 (11.5%) | ||||||
| Instant | 13 (16%) | 0 | 10 (18.2%) | 3 (10%) | 0 | 13 (20.3%) | 6 (15.8%) | 7 (14.9%) | 3 (9.1%) | 10 (19.2%) | ||||||
| Americano | 1 (1.2%) | 0 | 1 (1.8%) | 0 | 0 | 1 (1.6%) | 1 (2.6%) | 0 | 1 (3.0%) | 0 | ||||||
| Cold | 1 (1.2%) | 0 | 1 (1.8%) | 0 | 0 | 1 (1.6%) | 1 (2.6%) | 0 | 1 (3.0%) | 0 | ||||||
| Latte | 1 (1.2%) | 0 | 1 (1.8%) | 0 | 1 (4.8%) | 0 | 1 (2.6%) | 0 | 0 | 1 (1.9%) | ||||||
| Mocha | 2 (2.5%) | 0 | 1 (1.8%) | 1 (3.3%) | 0 | 2 (3.1%) | 1 (2.6%) | 1 (2.1%) | 1 (3.0%) | 1 (1.9%) | ||||||
| Coffee additives | Milk | 13 (16%) | 0 | 0.921 | 11 (20%) | 2 (6.7%) | 0.369 | 5 (23.8%) | 8 (12.5%) | 0.585 | 7 (18.4%) | 6 (12.8%) | 0.137 | 2 (6.1%) | 11 (21.2%) | 0.368 |
| Sugar | 9 (11.1%) | 0 | 6 (10.9%) | 3 (10%) | 3 (14.3%) | 6 (9.4%) | 5 (13.2%) | 4 (8.5%) | 0 | 9 (17.3%) | ||||||
| Sweetener | 3 (3.7%) | 0 | 3 (5.5%) | 0 | 1 (4.8%) | 2 (3.1%) | 0 | 3 (6.4%) | 1 (3.0%) | 2 (3.8%) | ||||||
| Syrup | 1 (1.2%) | 0 | 1 (1.8%) | 0 | 1 (4.8%) | 0 | 0 | 1 (2.1%) | 0 | 1 (1.9%) | ||||||
| Shredded chocolate | 1 (1.2%) | 0 | 0 | 1 (3.3%) | 0 | 1 (1.6%) | 0 | 1 (2.1%) | 0 | 1 (1.9%) | ||||||
| Stevia sugar | 2 (2.5%) | 0 | 0 | 2 (6.7%) | 0 | 2 (3.1%) | 0 | 2 (4.3%) | 1 (3.0%) | 1 (1.9%) | ||||||
| None | 60 (64.1%) | 4 (100%) | 40 (72.7%) | 24 (80%) | 15 (71.4%) | 49 (76.6%) | 28 (73.7%) | 36 (76.6%) | 29 (87.9%) | 35 (67.3%) | ||||||
| Variable | TGs | HDL | FBG | WC | SBP | DBP | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| r * | p-Value | r | p-Value | r | p-Value | r | p-Value | r | p-Value | r | p-Value | |
| Coffee cup size (mL) | −0.020 | 0.855 | 0.122 | 0.275 | 0.104 | 0.322 | 0.299 | 0.038 | 0.033 | 0.765 | −0.034 | 0.757 |
| Coffee cups/day | 0.164 | 0.134 | 0.050 | 0.655 | 0.119 | 0.279 | −0.078 | 0.486 | 0.045 | 0.681 | −0.119 | 0.279 |
| BMI | LDL | TC | |||||
|---|---|---|---|---|---|---|---|
| Mean ± SD | p-Value | Mean ± SD | p-Value | Mean ± SD | p-Value | ||
| Coffee cup size | S | 33.3 ± 7.6 | 0.133 | 3.0 ± 1.0 | 0.578 | 4.7 ± 1.2 | 0.498 |
| M | 32.9 ± 5.3 | 2.8 ± 0.9 | 4.4 ± 1.0 | ||||
| L | 35.0 ± 5.5 | 3.2 ± 1.1 | 5.0 ± 1.2 | ||||
| XL | 37.1 ± 6.0 | 3.2 ± 0.8 | 4.9 ± 1.0 | ||||
| Coffee cups/day | <1 (once a week) | 43.1 ± 11.5 | 0.008 | 4.0 ± 1.6 | 0.052 | 5.7 ± 1.7 | 0.046 |
| 1 | 32.6 ± 4.5 | 2.8 ± 0.8 | 4.4 ± 1.1 | ||||
| 2 | 33.9 ± 5.8 | 3.2 ± 0.9 | 4.9 ± 0.9 | ||||
| 3 | 34.0 ± 4.8 | 2.8 ± 0.7 | 4.4 ± 1.0 | ||||
| >3 | 35.1 ± 6.5 | 3.2 ± 1.0 | 4.9 ± 1.1 | ||||
| Types of coffee | Arabic | 34.8 ± 6.6 | 0.407 | 3.1 ± 1.0 | 0.668 | 4.7 ± 1.1 | 0.469 |
| Cappuccino | 33.9 ± 6.2 | 3.3 ± 0.8 | 4.9 ± 0.9 | ||||
| Black | 35.0 ± 7.6 | 3.2 ± 1.1 | 4.8 ± 1.4 | ||||
| Turkish | 32.7 ± 7.1 | 2.8 ± 1.0 | 4.2 ± 1.2 | ||||
| Instant | 37.8 ± 0.9 | 3.0 ± 1.0 | 4.5 ± 1.1 | ||||
| Americano | 25.2 ± 0.0 | 1.2 ± 0.0 | 2.2 ± 0.0 | ||||
| Cold | 43.2 ± 0.0 | 2.9 ± 0.0 | 4.1 ± 0.0 | ||||
| Latte | 30.0 ± 0.0 | 3.7 ± 0.0 | 5.1 ± 0.0 | ||||
| Mocha | 34.4 ± 6.6 | 2.9 ± 0.1 | 4.7 ± 0.1 | ||||
| Coffee additives | Milk | 35.6 ± 6.4 | 0.515 | 3.3 ± 0.7 | 0.655 | 5.1 ± 0.9 | 0.704 |
| Sugar | 36.0 ± 5.1 | 3.1 ± 0.4 | 4.5 ± 0.8 | ||||
| Sweetener | 33.9 ± 10 | 3.1 ± 1.3 | 4.8 ± 1.3 | ||||
| Syrup | 45.0 ± 0.0 | 4.5 ± 0.0 | 6.3 ± 0.0 | ||||
| Shredded chocolate | 37 ± 0.0 | 3.7 ± 0.0 | 4.7 ± 0.0 | ||||
| Stevia sugar | 40.6 ± 4.9 | 2.8 ± 0.9 | 4.5 ± 1.0 | ||||
| None | 34.0 ± 6.9 | 3.0 ± 1.0 | 4.7 ± 1.2 | ||||
| Variable | BMI | LDL | TC | |||
|---|---|---|---|---|---|---|
| r * | p-Value | r | p-Value | r | p-Value | |
| Coffee cup size (mL) | 0.282 | 0.009 | 0.079 | 0.486 | 0.104 | 0.357 |
| Coffee cups/day | −0.015 | 0.891 | 0.011 | 0.920 | −0.008 | 0.946 |
| β * | 95% CI | p-Value | |||
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Coffee cup size | 0.842 | 0.559 | 1.269 | 0.412 | |
| Number of coffee cups/day | 0.691 | 0.468 | 1.019 | 0.062 | |
| Types of coffee | Arabic | 2.143 | 0.531 | 8.646 | 0.284 |
| Cappuccino | 1.517 | 0.427 | 5.395 | 0.519 | |
| Black | 0.452 | 0.178 | 1.150 | 0.096 | |
| Turkish | 1.304 | 0.303 | 5.618 | 0.721 | |
| Instant | 2.381 | 0.603 | 9.359 | 0.215 | |
| Americano | -- | 0.0 | 0.0 | 1.00 | |
| Cold | -- | 0.0 | 0.0 | 1.00 | |
| Latte | -- | 0.0 | 0.0 | 1.00 | |
| Mocha | 0.627 | 0.038 | 10.389 | 0.745 | |
| Coffee additives | Milk | 4.159 | 0.859 | 20.133 | 0.077 |
| Sugar | -- | 0.0 | 0.0 | 0.999 | |
| Sweetener | 1.280 | 0.111 | 14.702 | 0.843 | |
| Syrup | -- | 0.0 | 0.0 | 1.00 | |
| Shredded chocolate | -- | 0.0 | 0.0 | 1.00 | |
| Stevia sugar | 0.627 | 0.038 | 10.389 | 0.745 | |
| None | 0.284 | 0.086 | 0.938 | 0.039 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alzahrani, W.I.; Alsharif, S.N.; Hafiz, M.S.; Alyoubi, D.A.; Alrizqi, A.M.; Younes, R.A.; Jahlan, A.M.; Yaghmour, K.A. Association Between Coffee Consumption and Metabolic Syndrome Components Among Saudi Adults. Metabolites 2025, 15, 163. https://doi.org/10.3390/metabo15030163
Alzahrani WI, Alsharif SN, Hafiz MS, Alyoubi DA, Alrizqi AM, Younes RA, Jahlan AM, Yaghmour KA. Association Between Coffee Consumption and Metabolic Syndrome Components Among Saudi Adults. Metabolites. 2025; 15(3):163. https://doi.org/10.3390/metabo15030163
Chicago/Turabian StyleAlzahrani, Wala I., Sarah N. Alsharif, Maryam S. Hafiz, Doaa A. Alyoubi, Amal M. Alrizqi, Raneem A. Younes, Alaa M. Jahlan, and Khaled A. Yaghmour. 2025. "Association Between Coffee Consumption and Metabolic Syndrome Components Among Saudi Adults" Metabolites 15, no. 3: 163. https://doi.org/10.3390/metabo15030163
APA StyleAlzahrani, W. I., Alsharif, S. N., Hafiz, M. S., Alyoubi, D. A., Alrizqi, A. M., Younes, R. A., Jahlan, A. M., & Yaghmour, K. A. (2025). Association Between Coffee Consumption and Metabolic Syndrome Components Among Saudi Adults. Metabolites, 15(3), 163. https://doi.org/10.3390/metabo15030163






