Resting Energy Expenditure of Physically Active Boys in Southeastern Poland—The Accuracy and Validity of Predictive Equations
Abstract
1. Introduction
2. Results
2.1. Characteristics of the Study Group
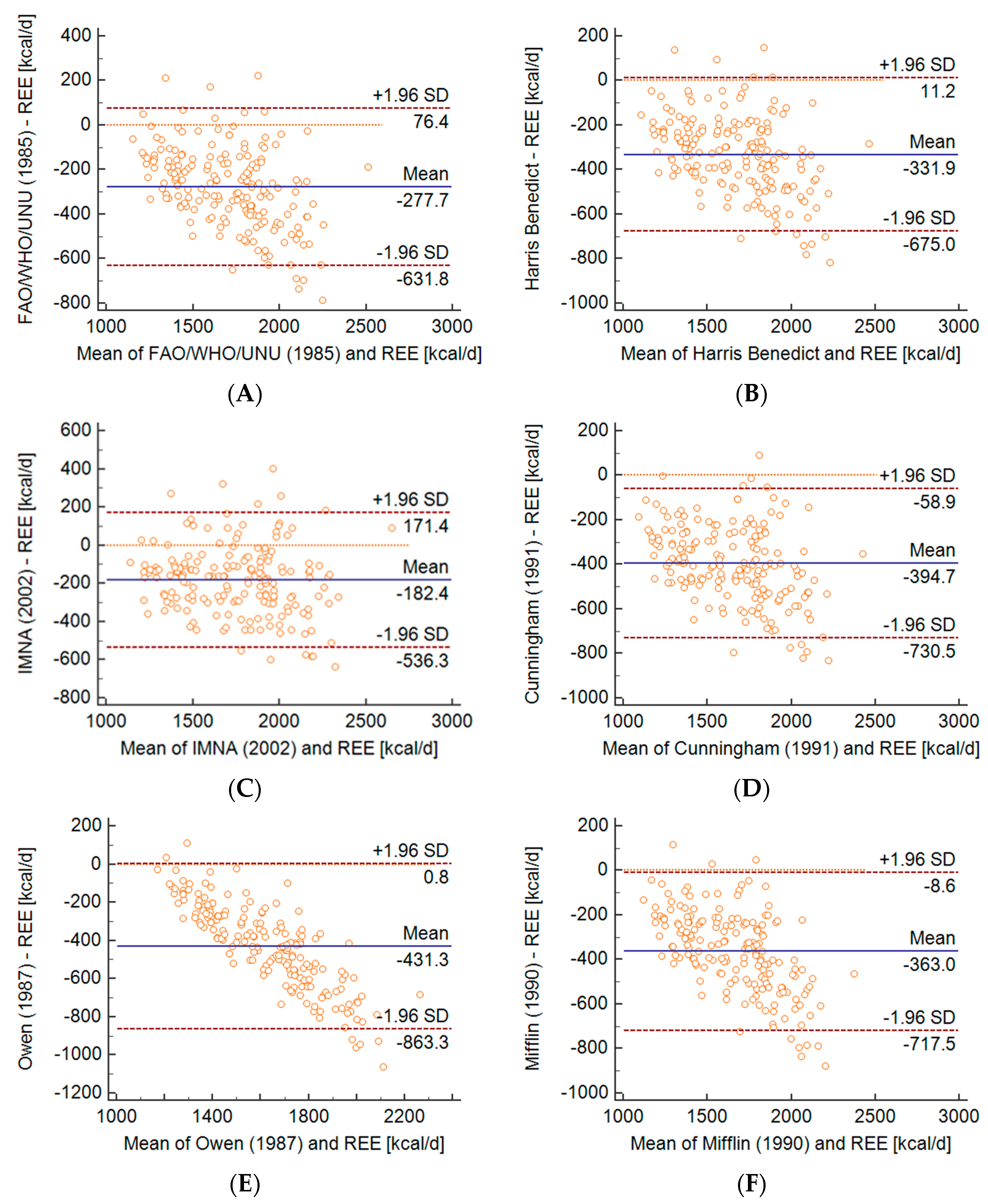
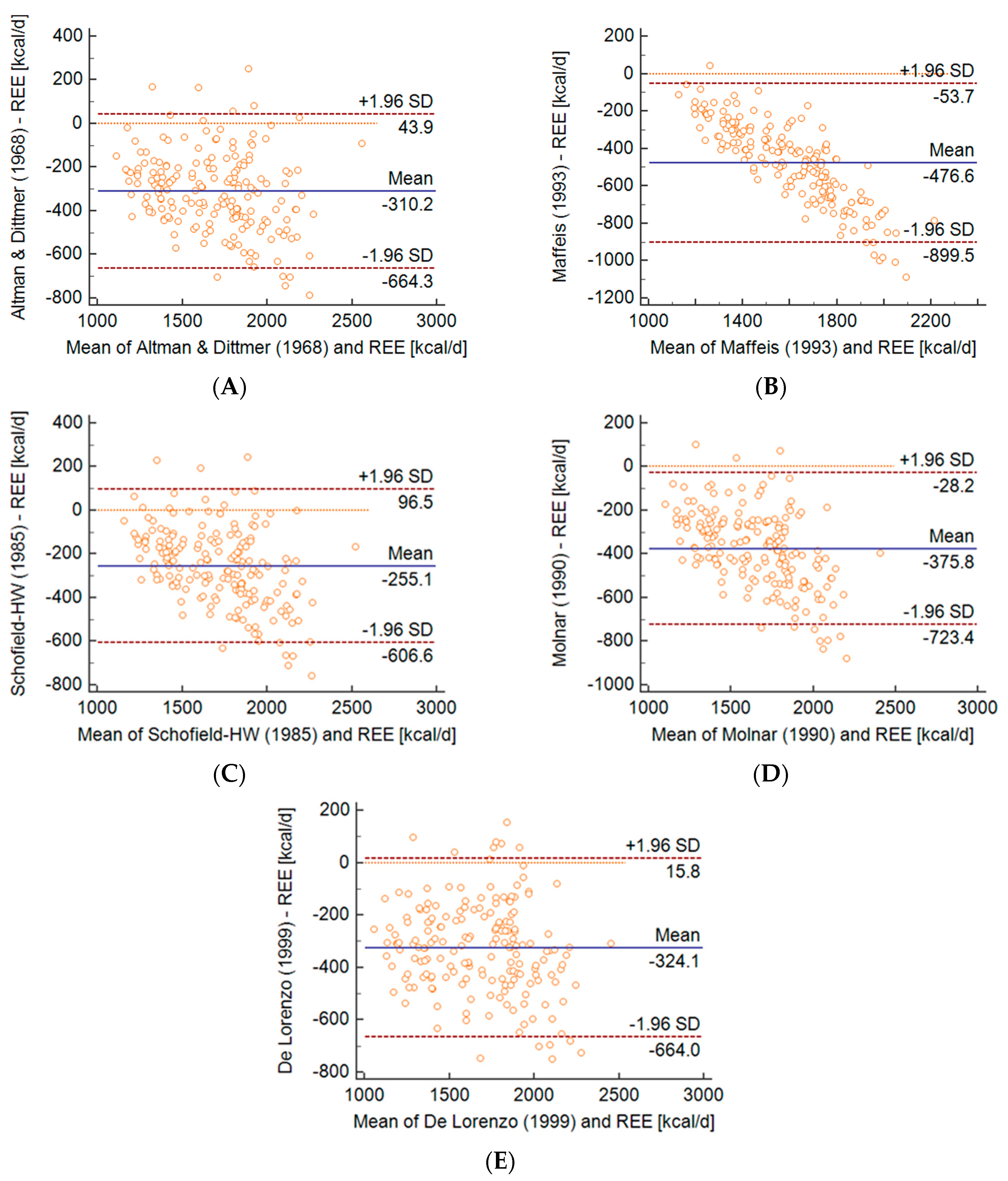
2.2. The Findings
3. Discussion
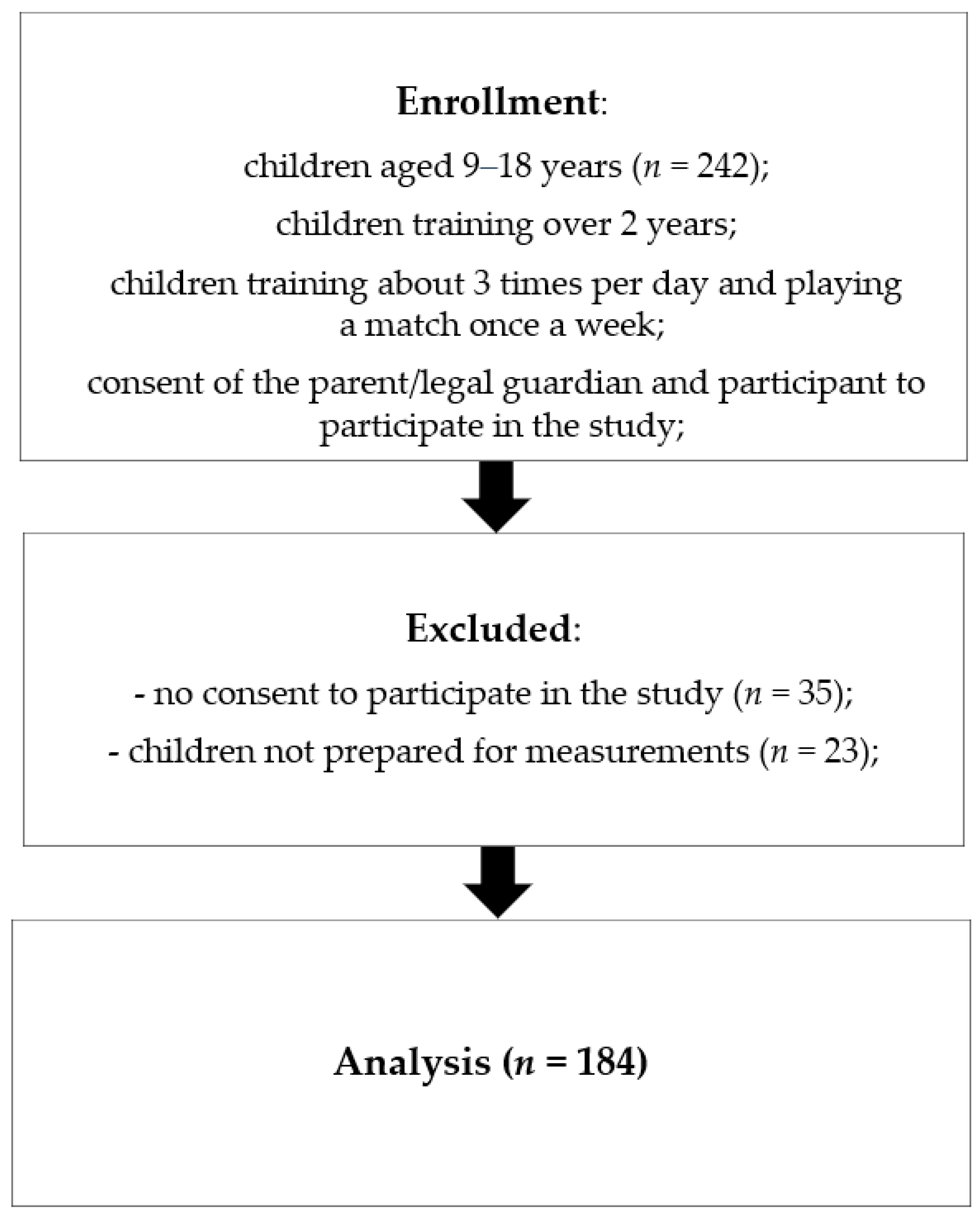
4. Materials and Methods
4.1. Subjects
4.2. General Procedures
4.2.1. Anthropometric Measurements, Body Composition and Body Mass Index
4.2.2. Resting Energy Expenditure Assessment by Indirect Calorimetry
4.2.3. Predictive REE Equation
4.3. Statistical Analysis
4.4. Ethics
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Physical Activity Guidelines Advisory Committee. Physical Activity Guidelines Advisory Committee Report; US Department of Health and Human Services: Washington, DC, USA, 2008; 683p.
- Ridley, K.; Ainsworth, B.E.; Olds, T.S. Development of a Compendium of Energy Expenditures for Youth: A second update of codes and MET values. Int. J. Behav. Nutr. Phys. Act. 2008, 5, 45. [Google Scholar] [CrossRef]
- Ainsworth, B.; Haskell, W.L.; Herrmann, S.D.; Meckes, N.; Bassett, D.R.; Tudor-Locke, C.; Greer, J.L.; Vezina, J.; Whitt-Glover, M.C.; Leon, A.S. Compendium of Physical Activities. Med. Sci. Sports Exerc. 2011, 43, 1575–1581. [Google Scholar] [CrossRef]
- Ainsworth, B.E.; Haskell, W.L.; Whitt, M.C.; Irwin, M.L.; Swartz, A.M.; Strath, S.J.; O’Brien, W.L.; Bassett, D.R., Jr.; Schmitz, K.H.; Emplaincourt, P.O.; et al. Compendium of Physical Activities: An update of activity codes and MET intensities. Med. Sci. Sports Exerc. 2000, 32 (Suppl. S9), S498–S516. [Google Scholar] [CrossRef]
- Schofield, W.N. Predicting basal metabolic rate, new standards and review of previous work. Hum. Nutr. Clin. Nutr. 1985, 39 (Suppl. S1), 5–41. [Google Scholar]
- Thomas, D.T.; Erdman, K.A.; Burke, L.M. Nutrition and Athletic Performance. Med. Sci. Sports Exerc. 2016, 48, 543–568. [Google Scholar] [CrossRef]
- Siervo, M.; Boschi, V.; Falconi, C. Which REE prediction equation should we use in normal-weight, overweight and obese women? Clin. Nutr. 2003, 22, 193–204. [Google Scholar] [CrossRef]
- Schmelzle, H.; Schröder, C.; Armbrust, S.; Unverzagt, S.; Fusch, C. Resting energy expenditure in obese children aged 4 to 15 years: Measured versus predicted data. Acta Paediatr. 2004, 93, 739–746. [Google Scholar] [CrossRef]
- Carpenter, A.; Pencharz, P.; Mouzaki, M. Accurate Estimation of Energy Requirements of Young Patients. J. Pediatr. Gastroenterol. Nutr. 2015, 60, 4–10. [Google Scholar] [CrossRef]
- Schlein, K.M.; Coulter, S.P. Best Practices for Determining Resting Energy Expenditure in Critically Ill Adults. Nutr. Clin. Pract. 2013, 29, 44–55. [Google Scholar] [CrossRef]
- Fukagawa, N.K.; Bandini, L.G.; Young, J.B. Effect of age on body composition and resting metabolic rate. Am. J. Physiol. Metab. 1990, 259, E233–E238. [Google Scholar] [CrossRef]
- Karhunen, L.; Franssila-Kallunki, A.; Rissanen, A.; Kervinen, K.; Kesaniemi, Y.; Uusitupa, M. Determinants of resting energy expenditure in obese non-diabetic caucasian women. Int. J. Obes. Relat Metab. Disord. 1997, 21, 197–202. [Google Scholar] [CrossRef]
- Nelson, K.M.; Weinsier, R.L.; Long, C.L.; Schutz, Y. Prediction of resting energy expenditure from fat-free mass and fat mass. Am. J. Clin. Nutr. 1992, 56, 848–856. [Google Scholar] [CrossRef]
- Segal, K.R.; Gutin, B.; Albu, J.; Pi-Sunyer, F.X. Thermal effects of food and exercise in lean and obese men of similar lean body mass. Am. J. Physiol. 1987, 252, E110–E117. [Google Scholar]
- Harris, J.A.; Benedict, F.G. A Biometric Study of Human Basal Metabolism. Proc. Natl. Acad. Sci. USA 1918, 4, 370–373. [Google Scholar] [CrossRef]
- Flack, K.D.; Siders, W.A.; Johnson, L.; Roemmich, J.N. Cross-Validation of Resting Metabolic Rate Prediction Equations. J. Acad. Nutr. Diet. 2016, 116, 1413–1422. [Google Scholar] [CrossRef]
- Hayes, M.; Chustek, M.; Wang, Z.; Gallagher, D.; Heshka, S.; Spungen, A.; Bauman, W.; Heymsfield, S.B. DXA: Potential for Creating a Metabolic Map of Organ-Tissue Resting Energy Expenditure Components. Obes. Res. 2002, 10, 969–977. [Google Scholar] [CrossRef]
- Haaf, T.T.; Weijs, P.J.M. Resting Energy Expenditure Prediction in Recreational Athletes of 18–35 Years: Confirmation of Cunningham Equation and an Improved Weight-Based Alternative. PLoS ONE 2014, 9, e108460. [Google Scholar] [CrossRef]
- Webb, P. Energy expenditure and fat-free mass in men and women. Am. J. Clin. Nutr. 1981, 34, 1816–1826. [Google Scholar] [CrossRef]
- Cunningham, J.J. A reanalysis of the factors influencing basal metabolic rate in normal adults. Am. J. Clin. Nutr. 1980, 33, 2372–2374. [Google Scholar] [CrossRef]
- MacKenzie-Shalders, K.; Byrne, N.M.; King, N.A.; Slater, G.J. Are increases in skeletal muscle mass accompanied by changes to resting metabolic rate in rugby athletes over a pre-season training period? Eur. J. Sport Sci. 2019, 19, 885–892. [Google Scholar] [CrossRef]
- Thompson, J.; Manore, M.M. Predicted and Measured Resting Metabolic Rate of Male and Female Endurance Athletes. J. Am. Diet. Assoc. 1996, 96, 30–34. [Google Scholar] [CrossRef]
- De Lorenzo, A.; Bertini, I.; Candeloro, N.; Piccinelli, R.; Innocente, I.; Brancati, A. A new predictive equation to calculate resting metabolic rate in athletes. J. Sports Med. Phys. Fit. 1999, 39, 213–219. [Google Scholar]
- Jagim, A.R.; Camic, C.L.; Kisiolek, J.; Luedke, J.; Erickson, J.; Jones, M.T.; Oliver, J.M. Accuracy of Resting Metabolic Rate Prediction Equations in Athletes. J. Strength Cond. Res. 2018, 32, 1875–1881. [Google Scholar] [CrossRef]
- Da Rocha, E.E.; Alves, V.G.; Silva, M.H.; Chiesa, C.A.; da Fonseca, R.B. Can measured resting energy expenditure be estimated by formulae in daily clinical nutrition practice? Curr. Opin. Clin. Nutr. Metab. Care 2005, 8, 319–328. [Google Scholar] [CrossRef]
- Mifflin, M.D.; Jeor, S.T.S.; Hill, L.A.; Scott, B.J.; Daugherty, S.A.; Koh, Y.O. A new predictive equation for resting energy expenditure in healthy individuals. Am. J. Clin. Nutr. 1990, 51, 241–247. [Google Scholar] [CrossRef]
- Owen, O.E.; Holup, J.L.; D’Alessio, D.A.; Craig, E.S.; Polansky, M.; Smalley, K.J.; Kavle, E.C.; Bushman, M.C.; Owen, L.R.; Mozzoli, M.A. A reappraisal of the caloric requirements of men. Am. J. Clin. Nutr. 1987, 46, 875–885. [Google Scholar] [CrossRef]
- Owen, O.E.; Kavle, E.; Owen, R.S.; Polansky, M.; Caprio, S.; Mozzoli, M.A.; Kendrick, Z.V.; Bushman, M.C.; Boden, G. A reappraisal of caloric requirements in healthy women. Am. J. Clin. Nutr. 1986, 44, 1–19. [Google Scholar] [CrossRef]
- De Lorenzo, A.; Bertini, I.; Puijia, A.; Testolin, G.; Testolin, C. Comparison between measured and predicted resting metabolic rate in moderately active adolescents. Acta Diabetol. 1999, 36, 141–145. [Google Scholar] [CrossRef]
- FAO/WHO/UNU. Energy and Protein Requirements: Report of a Joint FAO/WHO/UNU expert Consultation; FAO/WHO/UNU: Geneva, Switzerland, 1985; pp. 1–206. [Google Scholar]
- Ferrie, S.; Ward, M. Back to basics: Estimating energy requirements for adult hospital patients. Nutr. Diet. 2007, 64, 192–199. [Google Scholar] [CrossRef]
- Panel on Macronutrients; Panel on the Definition of Dietary Fiber; Subcommittee on Upper Reference Levels of Nutrients; Subcommittee on Interpretation and Uses of Dietary Reference Intakes; Standing Committee on the Scientific Evaluation of Dietary Reference Intakes; Food and Nutrition Board; Institute of Medicine of the National Academies (US). Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids. Chapter 5. Energy; The National Academies Press: Washington, DC, USA, 2002; pp. 107–264. [Google Scholar]
- Molnár, D.; Jeges, S.; Erhardt, E.; Schutz, Y. Measured and predicted resting metabolic rate in obese and nonobese adolescents. J. Pediatr. 1995, 127, 571–577. [Google Scholar] [CrossRef]
- Finan, K.; Larson, D.; Goran, M.I. Cross-Validation of Prediction Equations for Resting Energy Expenditure in Young, Healthy Children. J. Am. Diet. Assoc. 1997, 97, 140–145. [Google Scholar] [CrossRef]
- Maffeis, C.; Schutz, Y.; Micciolo, R.; Zoccante, L.; Pinelli, L. Resting metabolic rate in six- to ten-year-old obese and nonobese children. J. Pediatr. 1993, 122, 556–562. [Google Scholar] [CrossRef]
- Lawrence, J.; Lee, H.-M.; Kim, J.-H.; Kim, E.-K. Variability in results from predicted resting energy needs as compared to measured resting energy expenditure in Korean children. Nutr. Res. 2009, 29, 777–783. [Google Scholar] [CrossRef]
- Marra, M.; Montagnese, C.; Sammarco, R.; Amato, V.; Della Valle, E.; Franzese, A.; Contaldo, F.; Pasanisi, F. Accuracy of Predictive Equations for Estimating Resting Energy Expenditure in Obese Adolescents. J. Pediatr. 2015, 166, 1390–1396. [Google Scholar] [CrossRef]
- Henes, S.T.; Cummings, D.M.; Hickner, R.C.; Houmard, J.A.; Kolasa, K.M.; Lazorick, S.; Collier, D.N. Comparison of predictive equations and measured resting energy expenditure among obese youth attending a pediatric healthy weight clinic: One size does not fit all. Nutr. Clin. Pract. 2013, 28, 617–624. [Google Scholar] [CrossRef]
- Schusdziarra, V.; Wolfschläger, K.; Hausmann, M.; Wagenpfeil, S.; Erdmann, J. Accuracy of Resting Energy Expenditure Calculations in Unselected Overweight and Obese Patients. Ann. Nutr. Metab. 2014, 65, 299–309. [Google Scholar] [CrossRef]
- Uemura, A.; Mexitalia, M.; Susanto, J.C.; Yamauchi, T. Validating predictive factors for resting energy expenditure of adolescents in Indonesia. Int. J. Food Sci. Nutr. 2011, 63, 145–152. [Google Scholar] [CrossRef] [PubMed]
- Poehlman, E.T.; Melby, C.L.; Badylak, S.F. Resting metabolic rate and postprandial thermogenesis in highly trained and untrained males. Am. J. Clin. Nutr. 1988, 47, 793–798. [Google Scholar] [CrossRef] [PubMed]
- Horton, T.J.; A Geissler, C. Effect of habitual exercise on daily energy expenditure and metabolic rate during standardized activity. Am. J. Clin. Nutr. 1994, 59, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Schulz, L.O.; Nyomba, B.L.; Alger, S.; Anderson, T.E.; Ravussin, E. Effect of endurance training on sedentary energy expenditure measured in a respiratory chamber. Am. J. Physiol. Metab. 1991, 260, E257–E261. [Google Scholar] [CrossRef]
- Kim, J.-H.; Kim, M.-H.; Kim, G.-S.; Park, J.-S.; Kim, E.-K. Accuracy of predictive equations for resting metabolic rate in Korean athletic and non-athletic adolescents. Nutr. Res. Pract. 2015, 9, 370–378. [Google Scholar] [CrossRef] [PubMed]
- Müller, M.J.; Enderle, J.; Bosy-Westphal, A. Changes in Energy Expenditure with Weight Gain and Weight Loss in Humans. Curr. Obes. Rep. 2016, 5, 413–423. [Google Scholar] [CrossRef] [PubMed]
- Hunter, G.R.; Byrne, N.M.; Gower, B.A.; Sirikul, B.; Hills, A.P. Increased Resting Energy Expenditure after 40 Minutes of Aerobic But Not Resistance Exercise. Obesity 2006, 14, 2018–2025. [Google Scholar] [CrossRef] [PubMed]
- Poehlman, E.T.; Berke, E.M.; Joseph, J.R.; Gardner, A.W.; Katzman-Rooks, S.M.; Goran, M.I. Influence of aerobic capacity, body composition, and thyroid hormones on the age-related decline in resting metabolic rate. Metabolism 1992, 41, 915–921. [Google Scholar] [CrossRef]
- Rodríguez, G.; Moreno, L.; Sarría, A.; Fleta, J.; Bueno, M. Resting energy expenditure in children and adolescents: Agreement between calorimetry and prediction equations. Clin. Nutr. 2002, 21, 255–260. [Google Scholar] [CrossRef]
- Hofsteenge, G.H.; Chinapaw, M.J.; Delemarre-van de Waal, H.A.; Weijs, P.J. Validation of predictive equations for resting energy expenditure in obese adolescents. Am. J. Clin. Nutr. 2010, 91, 1244–1254. [Google Scholar] [CrossRef]
- Chima, L.; Mulrooney, H.; Warren, J.; Madden, A.M. A systematic review and quantitative analysis of resting energy expenditure prediction equations in healthy overweight and obese children and adolescents. J. Hum. Nutr. Diet. 2020, 33, 373–385. [Google Scholar] [CrossRef] [PubMed]
- Weinsier, R.L.; Schutz, Y.; Bracco, D. Reexamination of the relationship of resting metabolic rate to fat-free mass and to the metabolically active components of fat-free mass in humans. Am. J. Clin. Nutr. 1992, 55, 790–794. [Google Scholar] [CrossRef] [PubMed]
- Müller, M.J.; Geisler, C.; Hübers, M.; Pourhassan, M.; Braun, W.; Bosy-Westphal, A. Normalizing resting energy expenditure across the life course in humans: Challenges and hopes. Eur. J. Clin. Nutr. 2018, 72, 628–637. [Google Scholar] [CrossRef] [PubMed]
- Müller, M.J.; Wang, Z.; Heymsfield, S.B.; Schautz, B.; Bosy-Westphal, A. Advances in the understanding of specific metabolic rates of major organs and tissues in humans. Curr. Opin. Clin. Nutr. Metab. Care 2013, 16, 501–508. [Google Scholar] [CrossRef]
- García-Hermoso, A.; Hormazábal-Aguayo, I.; Fernández-Vergara, O.; Olivares, P.R.; Oriol-Granado, X. Physical activity, screen time and subjective well-being among children. Int. J. Clin. Health Psychol. 2020, 20, 126–134. [Google Scholar] [CrossRef] [PubMed]
- Meleleo, D.; Bartolomeo, N.; Cassano, L.; Nitti, A.; Susca, G.; Mastrototaro, G.; Armenise, U.; Zito, A.; DeVito, F.; Scicchitano, P.; et al. Evaluation of body composition with bioimpedence. A comparison between athletic and non-athletic children. Eur. J. Sport Sci. 2017, 17, 710–719. [Google Scholar] [CrossRef] [PubMed]
- Gutiérrez, R.; Aldea, L.; Cavia, M.M.; Alonso-Torre, S.R. Relation between the body composition and the sports practice in teenagers. Nutr. Hosp. 2015, 32, 336–345. [Google Scholar] [PubMed]
- Kalnina, L.; Sauka, M.; Timpka, T.; Dahlström, Ö.; Nylander, E.; Selga, G.; Ligere, R.; Karklina, H.; Priedite, I.S.; Larins, V. Body fat in children and adolescents participating in organized sports: Descriptive epidemiological study of 6048 Latvian athletes. Scand. J. Public Health 2015, 43, 615–622. [Google Scholar] [CrossRef] [PubMed]
- Matias, C.N.; Santos, D.A.; Fields, D.A.; Sardinha, L.; Silva, A.M. Is bioelectrical impedance spectroscopy accurate in estimating changes in fat-free mass in judo athletes? J. Sports Sci. 2012, 30, 1225–1233. [Google Scholar] [CrossRef]
- He, F.; Guan, P.; Liu, Q.; Crabtree, D.; Peng, L.; Wang, H. The relationship between obesity and body compositions with respect to the timing of puberty in Chongquing adolescents: A crosssectional study. BMC Public Health 2017, 17, 664. [Google Scholar] [CrossRef]
- Cheng, H.L.; Amatoury, M.; Steinbeck, K. Energy expenditure and intake during puberty in healthy nonobese adolescents: A systematic review. Am. J. Clin. Nutr. 2016, 104, 1061–1074. [Google Scholar] [CrossRef]
- Bullough, R.C.; A Gillette, C.; Harris, M.A.; Melby, C.L. Interaction of acute changes in exercise energy expenditure and energy intake on resting metabolic rate. Am. J. Clin. Nutr. 1995, 61, 473–481. [Google Scholar] [CrossRef]
- Speakman, J.R.; Selman, C. Physical activity and resting metabolic rate. Proc. Nutr. Soc. 2003, 62, 621–634. [Google Scholar] [CrossRef]
- Speakman, J.R.; Westerterp, K.R. Associations between energy demands, physical activity, and body composition in adult humans between 18 and 96 y of age. Am. J. Clin. Nutr. 2010, 92, 826–834. [Google Scholar] [CrossRef] [PubMed]
- Herring, J.L.; Molé, P.A.; Meredith, C.N.; Stern, J.S. Effect of suspending exercise training on resting metabolic rate in women. Med. Sci. Sports Exerc. 1992, 24, 59–65. [Google Scholar] [CrossRef] [PubMed]
- St-Onge, M.-P.; Roberts, A.L.; Chen, J.; Kelleman, M.; O’Keeffe, M.; Roychoudhury, A.; Jones, P.J.H. Short sleep duration increases energy intakes but does not change energy expenditure in normal-weight individuals. Am. J. Clin. Nutr. 2011, 94, 410–416. [Google Scholar] [CrossRef] [PubMed]
- De Jonge, L.; Zhao, X.; Mattingly, M.S.; Zuber, S.M.; Piaggi, P.; Csako, G.; Cizza, G.; NIDDK Sleep Extension Study Group. Poor sleep quality and sleep apnea are associated with higher resting energy expenditure in obese individuals with short sleep duration. J. Clin. Endocrinol. Metab. 2012, 97, 2881–2889. [Google Scholar] [CrossRef] [PubMed]
- Pietrobelli, A.; Rubiano, F.; St-Onge, M.-P.; Heymsfield, S.B. New bioimpedance analysis system: Improved phenotyping with whole-body analysis. Eur. J. Clin. Nutr. 2004, 58, 1479–1484. [Google Scholar] [CrossRef] [PubMed]
- Pietrobelli, A.; Rubiano, F.; Wangm, J.; Wangm, Z.; Heymsfieldm, S.M. Validation of contact electrode bioimpedance analysis in a pediatric population. Obes. Rev. 2005, 6, P451. [Google Scholar]
- Meredith-Jones, K.A.; Williams, S.M.; Taylor, R.W. Bioelectrical impedance as a measure of change in body composition in young children. Pediatr. Obes. 2014, 10, 252–259. [Google Scholar] [CrossRef] [PubMed]
- Kabiri, L.S.; Hernandez, D.C.; Mitchell, K. Reliability, Validity, and Diagnostic Value of a Pediatric Bioelectrical Impedance Analysis Scale. Child. Obes. 2015, 11, 650–655. [Google Scholar] [CrossRef]
- Barlow, S.E. Expert Committee Recommendations Regarding the Prevention, Assessment, and Treatment of Child and Adolescent Overweight and Obesity: Summary Report. Pediatrics 2007, 120, S164–S192. [Google Scholar] [CrossRef]
- Oshima, T.; Graf, S.; Heidegger, C.P.; Genton, L.; Pugin, J.; Pichard, C. Can calculation of energy expenditure based on CO2 measurements replace indirect calorimetry? Crit. Care 2017, 21, 13. [Google Scholar] [CrossRef]
- Gurven, M.D.; Trumble, B.C.; Stieglitz, J.; Yetish, G.; Cummings, D.; Blackwell, A.D.; Beheim, B.; Kaplan, H.S.; Pontzer, H. High resting metabolic rate among Amazonian forager-horticulturalists experiencing high pathogen burden. Am. J. Phys. Anthr. 2016, 161, 414–425. [Google Scholar] [CrossRef]
- Nieman, D.C.; Austin, M.D.; Benezra, L.; Pearce, S.; McInnis, T.; Unick, J.; Gross, S.J. Validation of Cosmed’s FitMate™ in Measuring Oxygen Consumption and Estimating Resting Metabolic Rate. Res. Sports Med. 2006, 14, 89–96. [Google Scholar] [CrossRef] [PubMed]
- Campbell, B.; Zito, G.; Colquhoun, R.; Martinez, N.; Louis, C.S.; Johnson, M.; Buchanan, L.; Lehn, M.; Smith, Y.; Cloer, B.; et al. Inter- and intra-day test-retest reliability of the Cosmed Fitmate ProTM indirect calorimeter for resting metabolic rate. J. Int. Soc. Sports Nutr. 2014, 11 (Suppl. S1), P46. [Google Scholar] [CrossRef]
- Compher, C.; Frankenfield, D.C.; Keim, N.L.; Roth-Yousey, L.; Evidence Analysis Working Group. Best Practice Methods to Apply to Measurement of Resting Metabolic Rate in Adults: A Systematic Review. J. Am. Diet. Assoc. 2006, 106, 881–903. [Google Scholar] [CrossRef] [PubMed]
- Bland, J.M.; Altman, D.G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986, 1, 307–310. [Google Scholar] [CrossRef]
| Variables | Mean | SD | Me | Min | Max |
|---|---|---|---|---|---|
| REE (kcal) | 1844.42 | 327.97 | 1883.00 | 1183.00 | 2639.00 |
| Age (years) | 13.20 | 2.16 | 13.00 | 10.00 | 16.00 |
| Height (cm) | 162.91 | 14.90 | 166.00 | 132.00 | 191.00 |
| Weight (kg) | 52.37 | 14.44 | 53.85 | 24.80 | 102.20 |
| BMI (kg/m2) | 19.27 | 2.57 | 19.05 | 13.60 | 28.00 |
| Fat (%) | 17.58 | 3.76 | 16.90 | 8.80 | 34.00 |
| Fat (kg) | 9.20 | 3.29 | 8.60 | 4.00 | 22.60 |
| FFM (kg) | 43.17 | 12.02 | 44.40 | 20.60 | 79.60 |
| TBW (kg) | 31.84 | 9.10 | 32.75 | 15.10 | 58.80 |
| PA (h/week) a | 10.69 | 0.59 | 10.50 | 10.00 | 12.00 |
| Equation | REE (kcal/d) | t-Test | Bias kcal/d | LLA kcal/d | ULA kcal/d | Bias (%) | r | p-Value (Correlation) | R2 | p-Value (Linear Regression) | CCC | Prediction | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | p-Value | Mean | SD | Mean | SD | Accurate% | Under% | Over % | ||||||||
| REE | 1844 | 328 | 100 | ||||||||||||||
| Harris Benedict | 1513 | 256 | <0.0001 | −332 | 175 | −675 | 11 | −17.5 | 8.0 | 0.84 | <0.0001 | 0.72 | <0.0001 | 0.50 | 14.7 | 84.8 | 0.5 |
| FAO/WHO/UNU (1985) | 1567 | 250 | <0.0001 | −278 | 181 | −632 | 76 | −14.4 | 8.4 | 0.84 | <0.0001 | 0.70 | <0.0001 | 0.56 | 25.0 | 73.4 | 1.6 |
| IMNA (2002) | 1662 | 303 | <0.0001 | −182 | 181 | −536 | 171 | −9.5 | 9.3 | 0.84 | <0.0001 | 0.70 | <0.0001 | 0.72 | 50.0 | 46.7 | 3.3 |
| Cunningham (1991) | 1450 | 264 | <0.0001 | −395 | 171 | −731 | −59 | −21.1 | 7.6 | 0.85 | <0.0001 | 0.73 | <0.0001 | 0.44 | 7.6 | 92.4 | 0.0 |
| Mifflin (1990) | 1481 | 224 | <0.0001 | −363 | 181 | −717 | −9 | −19.0 | 7.6 | 0.84 | <0.0001 | 0.72 | <0.0001 | 0.43 | 9.2 | 90.8 | 0.0 |
| Owen (1987) | 1413 | 147 | <0.0001 | −431 | 220 | −863 | 1 | −22.1 | 8.6 | 0.84 | <0.0001 | 0.70 | <0.0001 | 0.26 | 8.7 | 91.3 | 0.0 |
| Altman and Dittmer (1968) | 1534 | 283 | <0.0001 | −310 | 181 | −664 | 44 | −16.5 | 8.8 | 0.84 | <0.0001 | 0.70 | <0.0001 | 0.55 | 19.0 | 79.3 | 1.7 |
| Maffeis (1993) | 1368 | 150 | <0.0001 | −477 | 216 | −900 | −54 | −24.7 | 7.8 | 0.85 | <0.0001 | 0.72 | <0.0001 | 0.23 | 3.8 | 96.2 | 0.0 |
| Schofield-HW (1985) | 1589 | 253 | <0.0001 | −255 | 179 | −607 | 96 | −13.2 | 8.5 | 0.84 | <0.0001 | 0.71 | <0.0001 | 0.59 | 30.4 | 67.9 | 1.7 |
| Molnar (1990) | 1469 | 239 | <0.0001 | −324 | 173 | −723 | −28 | −19.8 | 7.6 | 0.85 | <0.0001 | 0.72 | <0.0001 | 0.43 | 10.3 | 89.7 | 0.0 |
| De Lorenzo (1999) | 1520 | 298 | <0.0001 | −376 | 177 | −664 | 16 | −17.5 | 8.7 | 0.84 | <0.0001 | 0.72 | <0.0001 | 0.55 | 17.4 | 82.6 | 0.0 |
| Criteria | Guidelines for Measurement | Study Group Recommendation |
|---|---|---|
| Fasting (thermic effect of food) | Minimum fast 5 h after meals or snacks (grade II) a, 4 h after small meal if longer fast is clinically inappropriate (grade II) | All recommendations concerning preparations for the study were outlined, including having rest for a minimum of 20 min, abstention from nicotine for a minimum 2 h, refraining from the consumption of meals 12 h before the test, refraining from drinking beverages with caffeine and alcohol content for the last 48 h before the test, as well as refraining from participation in physical activity for the previous 14 h. The method of conducting the study was explained in detail, and each study participant had the opportunity to visit the test rooms beforehand and familiarize themselves with the equipment so that it did not raise concerns or cause anxiety in the researched group. |
| Alcohol ingestion | Minimum abstention from alcohol for 2 h (grade III) | |
| Nicotine ingestion | Minimum abstention from nicotine for 2 h (grade II) | |
| Caffeine ingestion | Minimum abstention from caffeine for 4 h (grade II) | |
| Rest periods | Rest 10–20 min (grade III) | |
| Physical activity restriction | Minimum abstention from moderate aerobic or anaerobic exercise for 2 h before the test (grade II), for vigorous resistance exercise abstention of at least 14 h (grade III) | |
| Environmental conditions | Allow a room temperature of 20 °C–25 °C (68° F–77° F) (grade III) Ensure each individual is physically comfortable with measurement position during the test and repeated measures are in the same reclined position (grade V) | The rooms had a controlled temperature between 22 to 25 °C. In addition, each participant had the opportunity to acclimatize to the environment by lying flat for 30 min. |
| Gas collection devices | Use rigorous adherence to prevent air leaks (grade III). Further studies comparing modern gas collection devices are needed in healthy and clinical populations (grade V) | REE was measured using suitable silicone rubber pediatric masks (Cosmed, Rome, Italy) to ensure maximum sealing and prevent air leakage. This is essential for correct measurement. |
| Steady-state conditions and measurement interval | Discard initial 5 min. Then achieve a 5 min period with 10% CV b for VO2 c and VCO2 d (grade II) | We use a 10-min protocol in which the first 5 min of data are discarded, and the remaining 5 min of data have a coefficient of variation of no more than 10%. |
| No. of measures/24 h | Achieve steady state, and one measure is adequate; if not, two to three nonconsecutive measures improve accuracy (grade II) | 1 measure/24 h |
| Repeated measures (daily to monthly variation) | Repeated measures vary 3–5% over 24 h (grade II) and vary up to 10% over weeks to months (grade II) | - |
| Respiratory quotient (RQ) | RQ measures 0.70 or 1 suggest protocol violations or inaccurate gas measurement (grade II) | The Fitmate employs a turbine flowmeter for measuring ventilation and a galvanic fuel cell oxygen sensor for analyzing the fraction of oxygen in expired gases and uses standard metabolic formulas to calculate oxygen uptake. VCO2 is not measured directly but estimated assuming a fixed respiratory quotient (RQ) of 0.85. |
| Name [kcal/day] Equation for Males | Study Population * |
|---|---|
| Harris Benedict REE = 66.473 + [13.752 × weight] + [5.003 × height] − [655.093 × age] | 136 men, 103 women, 94 infants; normal body mass [15] |
| FAO/WHO/UNU REE = 16.6 × weight + (77 × height/100) + 572) | participants, including approx. 7500 children [30] |
| IMNA REE = 68 − [43.3 × age] + [712 × (height/100) + [19.2 × weight] | 1242 participants normal body mass; for people with moderate physical activity; a diverse group of respondents [32] |
| Cunningham REE = (22 × fat-free mass) + 500 | 120 men, 103 women; normal body mass [20] |
| Mifflin REE = [9.99 × weight] + [6.25 × height] − [4.92 × age] + 5 | 251 men, 247 women; a diverse group of respondents including obese individuals [26] |
| Owen REE = 879 + [10.2 × weight] | 60 men, 44 women; a diverse group of respondents including obese individuals [27,28] |
| Altman and Dittmer REE = [(0.0818 × weight) + 21.09] × 24 | >200–300 children aged 3–16 years old, average weight for height [34] |
| Maffeis REE = [1287 + (28.9 × weight) + (23.6 × height) − (69.1 × age)]/4.18 | 130 children (62 boys and 68 girls), including 97 normal body mass and 33 obese; 6–10 years [35] |
| Schofield-HW REE = [16.245 × weight] + [1.371 × height] + 515.3 | 3575 men, 1239 women; a diverse group of respondents; including about 1000 young male Italian soldiers and cadets [31] |
| Molnar REE = (12.16 × weight) + (6.04 × height) − (12.02 × age) + 6.43 | 193 children (116 non-obese and 77 obese); aged 10–16 years [33] |
| De Lorenzo REE = 857 + [9.0 × weight] + [11.7 × height] | 51 men, athletes, practicing sport 3 × a day [27,28] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Łuszczki, E.; Sokal, A.; Jarmakiewicz-Czaja, S.; Bartosiewicz, A.; Dereń, K.; Kuchciak, M.; Jagielski, P.; Mazur, A. Resting Energy Expenditure of Physically Active Boys in Southeastern Poland—The Accuracy and Validity of Predictive Equations. Metabolites 2020, 10, 493. https://doi.org/10.3390/metabo10120493
Łuszczki E, Sokal A, Jarmakiewicz-Czaja S, Bartosiewicz A, Dereń K, Kuchciak M, Jagielski P, Mazur A. Resting Energy Expenditure of Physically Active Boys in Southeastern Poland—The Accuracy and Validity of Predictive Equations. Metabolites. 2020; 10(12):493. https://doi.org/10.3390/metabo10120493
Chicago/Turabian StyleŁuszczki, Edyta, Aneta Sokal, Sara Jarmakiewicz-Czaja, Anna Bartosiewicz, Katarzyna Dereń, Maciej Kuchciak, Paweł Jagielski, and Artur Mazur. 2020. "Resting Energy Expenditure of Physically Active Boys in Southeastern Poland—The Accuracy and Validity of Predictive Equations" Metabolites 10, no. 12: 493. https://doi.org/10.3390/metabo10120493
APA StyleŁuszczki, E., Sokal, A., Jarmakiewicz-Czaja, S., Bartosiewicz, A., Dereń, K., Kuchciak, M., Jagielski, P., & Mazur, A. (2020). Resting Energy Expenditure of Physically Active Boys in Southeastern Poland—The Accuracy and Validity of Predictive Equations. Metabolites, 10(12), 493. https://doi.org/10.3390/metabo10120493