Update on Prevalence of Pain in Patients with Cancer 2022: A Systematic Literature Review and Meta-Analysis
Simple Summary
Abstract
1. Introduction
2. Material and Methods
2.1. Search Strategy
2.2. Study Selection
2.3. Data Extraction
2.4. Methodological Quality
2.5. Data Analyses
3. Results
3.1. Study Selection
3.2. Study Characteristics
3.3. Prevalence of Pain
3.4. Pain Severity
3.5. Determinants of Pain Prevalence
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- IASP. Available online: https://www.iasp-pain.org/advocacy/global-year/cancer-pain/ (accessed on 15 June 2022).
- Cramer, J.D.; Johnson, J.T.; Nilsen, M.L. Pain in Head and Neck Cancer Survivors: Prevalence, Predictors, and Quality-of-Life Impact. Otolaryngol. Head Neck Surg. 2018, 159, 853–858. [Google Scholar] [CrossRef] [PubMed]
- Kroenke, K.; Theobald, D.; Wu, J.; Loza, J.K.; Carpenter, J.S.; Tu, W. The association of depression and pain with health-related quality of life, disability, and health care use in cancer patients. J. Pain Symptom Manag. 2010, 40, 327–341. [Google Scholar] [CrossRef] [PubMed]
- Ośmiałowska, E.; Misiąg, W.; Chabowski, M.; Jankowska-Polańska, B. Coping Strategies, Pain, and Quality of Life in Patients with Breast Cancer. J. Clin. Med. 2021, 10, 4469. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.C.; Lai, Y.L.; Ward, S.E. Effect of cancer pain on performance status, mood states, and level of hope among Taiwanese cancer patients. J. Pain Symptom Manag. 2003, 25, 29–37. [Google Scholar] [CrossRef]
- Strang, P. Cancer pain-a provoker of emotional, social and existential distress. Acta Oncol. 1998, 37, 641–644. [Google Scholar] [CrossRef]
- van den Beuken-van Everdingen, M.H.; Hochstenbach, L.M.; Joosten, E.A.; Tjan-Heijnen, V.C.; Janssen, D.J. Update on Prevalence of Pain in Patients with Cancer: Systematic Review and Meta-Analysis. J. Pain Symptom Manag. 2016, 51, 1070–1090.e9. [Google Scholar] [CrossRef]
- van den Beuken-van Everdingen, M.H.; de Rijke, J.M.; Kessels, A.G.; Schouten, H.C.; van Kleef, M.; Patijn, J. Prevalence of pain in patients with cancer: A systematic review of the past 40 years. Ann. Oncol. 2007, 18, 1437–1449. [Google Scholar] [CrossRef]
- Evenepoel, M.; Haenen, V.; De Baerdemaecker, T.; Meeus, M.; Devoogdt, N.; Dams, L.; Van Dijck, S.; Van der Gucht, E.; De Groef, A. Pain Prevalence During Cancer Treatment: A Systematic Review and Meta-Analysis. J. Pain Symptom Manag. 2022, 63, e317–e335. [Google Scholar] [CrossRef]
- Kwon, J.H. Overcoming barriers in cancer pain management. J. Clin. Oncol. 2014, 32, 1727–1733. [Google Scholar] [CrossRef]
- Mercadante, S.; Adile, C.; Tirelli, W.; Ferrera, P.; Penco, I.; Casuccio, A. Barriers and Adherence to Pain Management in Advanced Cancer Patients. Pain Pract. 2021, 21, 388–393. [Google Scholar] [CrossRef]
- Stoorvogel, H.; van Haastregt, J.; Theunissen, M.; Schoenmaekers, J.; Hoeben, A.; van den Beuken-van Everdingen, M.H. Unacceptable pain in oncology: The patients’ perspective on reasons for absence of pain interventions. Eur. J. Cancer Care 2022, 31, e13628. [Google Scholar] [CrossRef] [PubMed]
- Makhlouf, S.M.; Pini, S.; Ahmed, S.; Bennett, M.I. Managing Pain in People with Cancer-a Systematic Review of the Attitudes and Knowledge of Professionals, Patients, Caregivers and Public. J. Cancer Educ. 2020, 35, 214–240. [Google Scholar] [CrossRef] [PubMed]
- UN. Available online: https://www.un.org/en/development/desa/population/publications/pdf/ageing/WorldPopulationAgeing2019-Highlights.pdf (accessed on 20 July 2022).
- WHO. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 20 July 2022).
- Divo, M.J.; Martinez, C.H.; Mannino, D.M. Ageing and the epidemiology of multimorbidity. Eur. Respir. J. 2014, 44, 1055–1068. [Google Scholar] [CrossRef] [PubMed]
- Braunlin, M.; Belani, R.; Buchanan, J.; Wheeling, T.; Kim, C. Trends in the multiple myeloma treatment landscape and survival: A U.S. analysis using 2011–2019 oncology clinic electronic health record data. Leuk. Lymphoma 2021, 62, 377–386. [Google Scholar] [CrossRef] [PubMed]
- Douglas, S.R.; Lizarraga, I.M.; Boughey, J.C.; Weiss, A.; Hunt, K.K.; Dickson-Witmer, D.; Subhedar, P.D.; Park, K.U.; Zhao, B.; Blair, S.L. National Cancer Database trends in surgical resection of the breast primary for stage IV breast cancer. Surg. Oncol. 2022, 42, 101778. [Google Scholar] [CrossRef]
- Evers, J.; de Jaeger, K.; Hendriks, L.E.L.; van der Sangen, M.; Terhaard, C.; Siesling, S.; De Ruysscher, D.; Struikmans, H.; Aarts, M.J. Trends and variations in treatment of stage I-III non-small cell lung cancer from 2008 to 2018: A nationwide population-based study from the Netherlands. Lung Cancer 2021, 155, 103–113. [Google Scholar] [CrossRef]
- Lorenzen, S.; Lordick, F.; Loosen, S.H.; Tacke, F.; Trautwein, C.; Roderburg, C.; Ettrich, T.J.; Perkhofer, L.; Reinacher-Schick, A.; Stein, A. Current status of immunotherapy in gastrointestinal malignancies. Z. Gastroenterol. 2020, 58, 542–555. [Google Scholar] [CrossRef]
- Ju, C.; Wei, L.; Man, K.K.C.; Wang, Z.; Ma, T.T.; Chan, A.Y.L.; Brauer, R.; Chui, C.S.L.; Chan, E.W.; Jani, Y.H.; et al. Global, regional, and national trends in opioid analgesic consumption from 2015 to 2019: A longitudinal study. Lancet Public Health 2022, 7, e335–e346. [Google Scholar] [CrossRef]
- Bernard, S.A.; Chelminski, P.R.; Ives, T.J.; Ranapurwala, S.I. Management of Pain in the United States-A Brief History and Implications for the Opioid Epidemic. Health Serv. Insights 2018, 11, 1–6. [Google Scholar] [CrossRef]
- Brooks, J.V.; Poague, C.; Formagini, T.; Roberts, A.W.; Sinclair, C.T.; Keirns, C.C. Palliative Care’s Role Managing Cancer Pain During the Opioid Crisis: A Qualitative Study of Patients, Caregivers, and Clinicians. J. Pain Symptom Manag. 2020, 60, 1127–1135.e2. [Google Scholar] [CrossRef]
- Chen, Y.; Spillane, S.; Shiels, M.S.; Young, L.; Quach, D.; Berrington de González, A.; Freedman, N.D. Trends in Opioid Use among Cancer Patients in the United States: 2013–2018. JNCI Cancer Spectr. 2022, 6, pkab095. [Google Scholar] [CrossRef]
- Pain, Dutch Guideline of Cancer. Available online: https://www.pallialine.nl/pijn-bij-patienten-met-kanker (accessed on 4 July 2022).
- Fallon, M.; Giusti, R.; Aielli, F.; Hoskin, P.; Rolke, R.; Sharma, M.; Ripamonti, C.I. Management of cancer pain in adult patients: ESMO Clinical Practice Guidelines. Ann. Oncol. 2018, 29, iv166–iv191. [Google Scholar] [CrossRef] [PubMed]
- Swarm, R.A.; Paice, J.A.; Anghelescu, D.L.; Are, M.; Bruce, J.Y.; Buga, S.; Chwistek, M.; Cleeland, C.; Craig, D.; Gafford, E.; et al. Adult Cancer Pain, Version 3.2019, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. 2019, 17, 977–1007. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA Statement. Open Med. 2009, 3, e123–e130. [Google Scholar] [PubMed]
- Rietjens, J.A.; Bramer, W.M.; Geijteman, E.C.; van der Heide, A.; Oldenmenger, W.H. Development and validation of search filters to find articles on palliative care in bibliographic databases. Palliat. Med. 2019, 33, 470–474. [Google Scholar] [CrossRef] [PubMed]
- Serlin, R.C.; Mendoza, T.R.; Nakamura, Y.; Edwards, K.R.; Cleeland, C.S. When is cancer pain mild, moderate or severe? Grading pain severity by its interference with function. Pain 1995, 61, 277–284. [Google Scholar] [CrossRef]
- Leboeuf-Yde, C.; Lauritsen, J.M. The prevalence of low back pain in the literature. A structured review of 26 Nordic studies from 1954 to 1993. Spine (Phila. Pa. 1976) 1995, 20, 2112–2118. [Google Scholar] [CrossRef]
- Egger, M. Systematic Reviews, 2nd ed.; BMJ Publishing Group: London, UK, 2001. [Google Scholar]
- Alt-Epping, B.; Seidel, W.; Vogt, J.; Mehnert, A.; Thomas, M.; van Oorschot, B.; Wolff, H.; Schliephake, H.; Canis, M.; Dröge, L.H.; et al. Symptoms and Needs of Head and Neck Cancer Patients at Diagnosis of Incurability-Prevalences, Clinical Implications, and Feasibility of a Prospective Longitudinal Multicenter Cohort Study. Oncol. Res. Treat. 2016, 39, 186–192. [Google Scholar] [CrossRef]
- Andersen, K.G.; Aasvang, E.K.; Kroman, N.; Kehlet, H. Intercostobrachial nerve handling and pain after axillary lymph node dissection for breast cancer. Acta. Anaesthesiol. Scand. 2014, 58, 1240–1248. [Google Scholar] [CrossRef]
- Bibby, A.C.; Halford, P.; De Fonseka, D.; Morley, A.J.; Smith, S.; Maskell, N.A. The Prevalence and Clinical Relevance of Nonexpandable Lung in Malignant Pleural Mesothelioma. A Prospective, Single-Center Cohort Study of 229 Patients. Ann. Am. Thorac. Soc. 2019, 16, 1273–1279. [Google Scholar] [CrossRef]
- Efficace, F.; Gaidano, G.; Breccia, M.; Criscuolo, M.; Cottone, F.; Caocci, G.; Bowen, D.; Lübbert, M.; Angelucci, E.; Stauder, R.; et al. Prevalence, severity and correlates of fatigue in newly diagnosed patients with myelodysplastic syndromes. Br. J. Haematol. 2015, 168, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Esser, P.; Kuba, K.; Scherwath, A.; Schirmer, L.; Schulz-Kindermann, F.; Dinkel, A.; Balck, F.; Koch, U.; Kröger, N.; Götze, H.; et al. Posttraumatic stress disorder symptomatology in the course of allogeneic HSCT: A prospective study. J. Cancer Surviv. 2017, 11, 203–210. [Google Scholar] [CrossRef]
- Gjeilo, K.H.; Oksholm, T.; Follestad, T.; Wahba, A.; Rustøen, T. Trajectories of Pain in Patients Undergoing Lung Cancer Surgery: A Longitudinal Prospective Study. J. Pain Symptom Manag. 2020, 59, 818–828.e1. [Google Scholar] [CrossRef] [PubMed]
- Godby, R.C.; Dai, C.; Al-Obaidi, M.; Giri, S.; Young-Smith, C.; Kenzik, K.; McDonald, A.M.; Paluri, R.K.; Gbolahan, O.B.; Bhatia, S.; et al. Depression among older adults with gastrointestinal malignancies. J. Geriatr. Oncol. 2021, 12, 599–604. [Google Scholar] [CrossRef] [PubMed]
- Hong, J.; Wei, Z.; Wang, W. Preoperative psychological distress, coping and quality of life in Chinese patients with newly diagnosed gastric cancer. J. Clin. Nurs. 2015, 24, 2439–2447. [Google Scholar] [CrossRef]
- Kirchheiner, K.; Nout, R.A.; Czajka-Pepl, A.; Ponocny-Seliger, E.; Sturdza, A.E.; Dimopoulos, J.C.; Dörr, W.; Pötter, R. Health related quality of life and patient reported symptoms before and during definitive radio(chemo)therapy using image-guided adaptive brachytherapy for locally advanced cervical cancer and early recovery—A mono-institutional prospective study. Gynecol. Oncol. 2015, 136, 415–423. [Google Scholar] [CrossRef]
- Kuon, J.; Vogt, J.; Mehnert, A.; Alt-Epping, B.; van Oorschot, B.; Sistermanns, J.; Ahlborn, M.; Ritterbusch, U.; Stevens, S.; Kahl, C.; et al. Symptoms and Needs of Patients with Advanced Lung Cancer: Early Prevalence Assessment. Oncol. Res. Treat. 2019, 42, 650–659. [Google Scholar] [CrossRef]
- Lunde, S.; Petersen, K.K.; Kugathasan, P.; Arendt-Nielsen, L.; Søgaard-Andersen, E. Chronic Postoperative Pain after Robot-Assisted Laparoscopic Hysterectomy for Endometrial Cancer. J. Gynecol. Surg. 2019, 35, 140–146. [Google Scholar] [CrossRef]
- Ravn Munkvold, B.K.; Sagberg, L.M.; Jakola, A.S.; Solheim, O. Preoperative and Postoperative Headache in Patients with Intracranial Tumors. World Neurosurg. 2018, 115, e322–e330. [Google Scholar] [CrossRef]
- Roy, S.; Pathy, S.; Mohanti, B.K.; Raina, V.; Jaiswal, A.; Kumar, R.; Kalaivani, M. Accelerated hypofractionated radiotherapy with concomitant chemotherapy in locally advanced squamous cell carcinoma of lung: Evaluation of response, survival, toxicity and quality of life from a Phase II randomized study. Br. J. Radiol. 2016, 89, 20150966. [Google Scholar] [CrossRef]
- Russo, M.; Villani, V.; Taga, A.; Genovese, A.; Terrenato, I.; Manzoni, G.C.; Servadei, F.; Torelli, P.; Pace, A. Headache as a presenting symptom of glioma: A cross-sectional study. Cephalalgia 2018, 38, 730–735. [Google Scholar] [PubMed]
- Salwey, L.; L’Huillier, V.; Zaid, M.; Vené, Y.; Tavernier, L.; Mauvais, O. Neuropathic pain at diagnosis of head and neck squamous cell carcinoma. Eur. Ann. Otorhinolaryngol. Head Neck Dis. 2020, 137, 377–380. [Google Scholar] [CrossRef] [PubMed]
- Tang, M.H.; Castle, D.J.; Choong, P.F.M. Identifying the prevalence, trajectory, and determinants of psychological distress in extremity sarcoma. Sarcoma 2015, 2015, 745163. [Google Scholar] [CrossRef] [PubMed]
- Thomas, S.; Walsh, D.; Shrotriya, S.; Aktas, A.; Hullihen, B.; Estfan, B.; Budd, G.T.; Hjermstad, M.J.; O’Connor, B. Symptoms, Quality of Life, and Daily Activities in People with Newly Diagnosed Solid Tumors Presenting to a Medical Oncologist. Am. J. Hosp. Care 2017, 34, 611–621. [Google Scholar] [CrossRef]
- Wang, Y.J.; Chan, Y.N.; Jheng, Y.W.; Wu, C.J.; Lin, M.W.; Tseng, L.M.; Tsai, Y.F.; Liu, L.C. Chemotherapy-induced peripheral neuropathy in newly diagnosed breast cancer survivors treated with taxane: A prospective longitudinal study. Support. Care Cancer 2021, 29, 2959–2971. [Google Scholar] [CrossRef]
- Williams, G.R.; Al-Obaidi, M.; Dai, C.; Harmon, C.; Buford, T.W.; Gbolahan, O.; Pergolotti, M.; Bhatia, S.; Giri, S. Fatigue is independently associated with functional status limitations in older adults with gastrointestinal malignancies—Results from the CARE registry. Support. Care Cancer 2021, 29, 6793–6800. [Google Scholar] [CrossRef]
- Yao, H.H.I.; Crump, R.T.; Charbonneau, C.; Khan, A.; Barton, C.; Brotherhood, H.; Jiang, J.; Carlson, K.V.; Baverstock, R.J. Baseline patient reported outcomes data shows high prevalence of overactive bladder, sexual dysfunction, depression and anxiety in Canadian men with newly diagnosed localized prostate cancer. Transl. Androl. Urol. 2020, 9, 2046–2053. [Google Scholar] [CrossRef]
- Berliere, M.; Piette, N.; Bernard, M.; Lacroix, C.; Gerday, A.; Samartzi, V.; Coyette, M.; Roelants, F.; Docquier, M.A.; Touil, N.; et al. Hypnosis sedation reduces the duration of different side effects of cancer treatments in breast cancer patients receiving neoadjuvant chemotherapy. Cancers 2021, 13, 4147. [Google Scholar] [CrossRef]
- Bretschneider, C.E.; Doll, K.M.; Bensen, J.T.; Gehrig, P.A.; Wu, J.M.; Geller, E.J. Prevalence of pelvic floor disorders in women with suspected gynecological malignancy: A survey-based study. Int. Urogynecol. J. 2016, 27, 1409–1414. [Google Scholar] [CrossRef]
- Browall, M.; Brandberg, Y.; Nasic, S.; Rydberg, P.; Bergh, J.; Rydén, A.; Xie, H.; Eriksson, I.; Wengström, Y.; Rydén, A.; et al. A prospective exploration of symptom burden clusters in women with breast cancer during chemotherapy treatment. Support. Care Cancer 2017, 25, 1423–1429. [Google Scholar] [CrossRef]
- Calderon, C.; Carmona-Bayonas, A.; Hernández, R.; Ghanem, I.; Castelo, B.; Martinez de Castro, E.; Ferreira, E.; Ciria, L.; Muñiz, M.; Jimenez-Fonseca, P. Effects of pessimism, depression, fatigue, and pain on functional health-related quality of life in patients with resected non-advanced breast cancer. Breast 2019, 44, 108–112. [Google Scholar] [CrossRef] [PubMed]
- Choo, S.B.; Saifulbahri, A.; Zullkifli, S.N.; Fadzil, M.L.; Redzuan, A.M.; Abdullah, N.; Bustamam, R.S.A.; Ahmad, H.Z.; Shah, N.M. Adjuvant endocrine therapy side-effects among postmenopausal breast cancer patients in Malaysia. Climacteric 2019, 22, 175–181. [Google Scholar] [CrossRef]
- de Menezes Couceiro, T.C.; Valença, M.M.; Raposo, M.C.F.; de Orange, F.A.; Amorim, M.M.R. Prevalence of Post-Mastectomy Pain Syndrome and Associated Risk Factors: A Cross-Sectional Cohort Study. Pain Manag. Nurs. 2014, 15, 731–737. [Google Scholar] [CrossRef] [PubMed]
- Dylke, E.S.; Kilbreath, S. Current rehabilitation processes do not prevent long-term impairments after treatment for breast cancer in Australia. Aust. Fam. Physician 2015, 44, 405–409. [Google Scholar] [PubMed]
- El-Aqoul, A.; Obaid, A.; Yacoub, E.; Al-Najar, M.; Ramadan, M.; Darawad, M. Factors Associated with Inadequate Pain Control among Postoperative Patients with Cancer. Pain Manag. Nurs. 2018, 19, 130–138. [Google Scholar] [CrossRef]
- Fenlon, D.; Powers, C.; Simmonds, P.; Clough, J.; Addington-Hall, J. The JACS prospective cohort study of newly diagnosed women with breast cancer investigating joint and muscle pain, aches, and stiffness: Pain and quality of life after primary surgery and before adjuvant treatment. BMC Cancer 2014, 14, 467. [Google Scholar] [CrossRef]
- Fjell, M.; Langius-Eklöf, A.; Nilsson, M.; Wengström, Y.; Sundberg, K. Reduced symptom burden with the support of an interactive app during neoadjuvant chemotherapy for breast cancer—A randomized controlled trial. Breast 2020, 51, 85–93. [Google Scholar] [CrossRef]
- Hagiwara, Y.; Ohashi, Y.; Uesaka, K.; Boku, N.; Fukutomi, A.; Okamura, Y.; Konishi, M.; Matsumoto, I.; Kaneoka, Y.; Shimizu, Y.; et al. Health-related quality of life of adjuvant chemotherapy with S-1 versus gemcitabine for resected pancreatic cancer: Results from a randomised phase III trial (JASPAC 01). Eur. J. Cancer 2018, 93, 79–88. [Google Scholar] [CrossRef] [PubMed]
- Haryani, H.; Hsu, Y.Y.; Warsini, S.; Wang, S.T. Measuring the Symptom Experience of Patients with Cancer in Indonesia: Cross-Cultural Adaptation and Validation of the Memorial Symptom Assessment Scale—Indonesian Version. J. Pain Symptom Manag. 2018, 56, 920–927. [Google Scholar] [CrossRef]
- Ho, R.T.H.; Kwan, T.T.C.; Cheung, I.K.M.; Chan, C.K.P.; Lo, P.H.Y.; Yip, P.S.F.; Luk, M.Y.; Chan, C.L.W. Association of fatigue with perceived stress in Chinese women with early stage breast cancer awaiting adjuvant radiotherapy. Stress Health 2015, 31, 214–221. [Google Scholar] [CrossRef]
- Hong, J.S.; Tian, J. Prevalence of anxiety and depression and their risk factors in Chinese cancer patients. Support. Care Cancer 2014, 22, 453–459. [Google Scholar] [CrossRef] [PubMed]
- Jarden, M.; Møller, T.; Christensen, K.B.; Buchardt, A.S.; Kjeldsen, L.; Adamsen, L. Longitudinal symptom burden in adult patients with acute leukaemia participating in the PACE-AL randomised controlled exercise trial—An explorative analysis. Eur. J. Cancer Care 2021, 30, e13462. [Google Scholar] [CrossRef] [PubMed]
- Jensen, N.B.K.; Pötter, R.; Kirchheiner, K.; Fokdal, L.; Lindegaard, J.C.; Kirisits, C.; Mazeron, R.; Mahantshetty, U.; Jürgenliemk-Schulz, I.M.; Segedin, B.; et al. Bowel morbidity following radiochemotherapy and image-guided adaptive brachytherapy for cervical cancer: Physician- and patient reported outcome from the EMBRACE study. Radiother. Oncol. 2018, 127, 431–439. [Google Scholar] [CrossRef] [PubMed]
- Khan, Q.J.; Kimler, B.F.; Reddy, P.S.; Sharma, P.; Klemp, J.R.; Nydegger, J.L.; Yeh, H.W.; Fabian, C.J. Randomized trial of vitamin D3 to prevent worsening of musculoskeletal symptoms in women with breast cancer receiving adjuvant letrozole. The VITAL trial. Breast Cancer Res. Treat. 2017, 166, 491–500. [Google Scholar] [CrossRef]
- Kim, Y.S.; Do, H.; Lee, J.W.; Jeong, J.; Shin, Y.W.; Yi, K.; Kim, J.; Lee, S.B.; Sohn, G.; Yang, N.; et al. Patient reporting pain intensity immediately after surgery can be associated with underlying depression in women with breast cancer. Psychooncology 2016, 25, 308–315. [Google Scholar] [CrossRef]
- Kirkham, A.A.; Eves, N.D.; Shave, R.E.; Bland, K.A.; Bovard, J.; Gelmon, K.A.; Virani, S.A.; McKenzie, D.C.; Stöhr, E.J.; Waburton, D.E.R.; et al. The effect of an aerobic exercise bout 24 h prior to each doxorubicin treatment for breast cancer on markers of cardiotoxicity and treatment symptoms: A RCT. Breast Cancer Res. Treat. 2018, 167, 719–729. [Google Scholar] [CrossRef]
- Lewis, L.; Williams, A.M.; Athifa, M.; Brown, D.; Budgeon, C.A.; Bremner, A.P. Evidence-Based Self-care Guidelines for People Receiving Chemotherapy: Do They Reduce Symptom Burden and Psychological Distress? Cancer Nurs. 2015, 38, e1–e8. [Google Scholar] [CrossRef]
- Lewis, S.; Pandey, S.; Salins, N.; Deodhar, J.; Patil, V.; Gupta, T.; Laskar, S.G.; Budrukkar, A.; Murthy, V.; Joshi, A.; et al. Distress Screening in Head and Neck Cancer Patients Planned for Cancer-Directed Radiotherapy. Laryngoscope 2021, 131, 2023–2029. [Google Scholar] [CrossRef]
- McFarland, D.C.; Shaffer, K.M.; Tiersten, A.; Holland, J. Prevalence of physical problems detected by the distress thermometer and problem list in patients with breast cancer. Psychooncology 2018, 27, 1394–1403. [Google Scholar] [CrossRef]
- Moloney, N.; Sung, J.M.W.; Kilbreath, S.; Dylke, E. Prevalence and risk factors associated with pain 21 months following surgery for breast cancer. Support. Care Cancer 2016, 24, 4533–4539. [Google Scholar] [CrossRef]
- Nogueira de Oliveira Martins, T.; dos Santos, L.F.; do Nascimento Petter, G.; da Silva Ethur, J.N.; Medeiros Braz, M.; Foletto Pivetta, H.M. Immediate breast reconstruction versus non-reconstruction after mastectomy: A study on quality of life, pain and functionality. Fisioter. Pesqui. 2017, 24, 412–419. [Google Scholar]
- Okamoto, A.; Yamasaki, M.; Yokota, I.; Mori, M.; Matsuda, M.; Yamaguchi, Y.; Yamakita, S.; Ueno, H.; Sawa, T.; Taguchi, T.; et al. Classification of acute pain trajectory after breast cancer surgery identifies patients at risk for persistent pain: A prospective observational study. J. Pain Res. 2018, 11, 2197–2206. [Google Scholar] [CrossRef] [PubMed]
- Ribas, Y.; Bonet, M.; Torres, L.; Núñez, M.; Esther Jovell-Fernández, E.; Aranda, E.; Andreyev, H.J. Bowel dysfunction in survivors of gynaecologic malignancies. Support. Care Cancer 2020, 28, 5501–5510. [Google Scholar] [CrossRef] [PubMed]
- Røhrl, K.; Guren, M.G.; Miaskowski, C.; Cooper, B.A.; Diep, L.M.; Rustøen, T. No Differences in Symptom Burden Between Colorectal Cancer Patients Receiving Curative Versus Palliative Chemotherapy. J. Pain Symptom Manag. 2016, 52, 539–547. [Google Scholar] [CrossRef] [PubMed]
- Shaulov, A.; Rodin, G.; Popovic, G.; Caraiscos, V.B.; Le, L.W.; Rydall, A.; Schimmer, A.D.; Zimmermann, C. Pain in patients with newly diagnosed or relapsed acute leukemia. Support. Care Cancer 2019, 27, 2789–2797. [Google Scholar] [CrossRef] [PubMed]
- Tran, B.T.; Pham, N.H.; Nguyen, T.X.; Choi, K.S.; Sohn, D.K.; Kim, S.Y.; Suh, J.K.; Nguyen, T.D.; Phan, V.S.; Tran, D.T.; et al. Measurement of health-related quality of life among colorectal cancer patients using the vietnamese value set of the eq-5d-5l. Patient Prefer. Adherence 2020, 14, 2427–2437. [Google Scholar] [CrossRef]
- Xu, Y.; Hu, X.; Zhou, L.; Zhao, Y. Effect of sequencing of preoperative systemic therapy on patients with locally advanced breast cancer. Breast J. 2020, 26, 1987–1994. [Google Scholar] [CrossRef]
- Yi, M.; Hwang, E. Pain and Menopause Symptoms of Breast Cancer Patients with Adjuvant Hormonal Therapy in Korea: Secondary Analysis. Asia Pac. J. Oncol. Nurs. 2018, 5, 262–269. [Google Scholar] [CrossRef]
- Agarwal, S.; Garg, R.; Minhas, V.; Bhatnagar, S.; Mishra, S.; Kumar, V.; Bharati, S.J.; Gupta, N.; Khan, M.A. To assess the Prevalence and Predictors of Cancer-related Fatigue and its Impact on Quality of Life in Advanced Cancer Patients Receiving Palliative Care in a Tertiary Care Hospital: A Cross-sectional Descriptive Study. Indian J. Palliat. Care 2020, 26, 523–527. [Google Scholar]
- Al-Zahrani, O.; Eldali, A.; Al-Shahri, M.Z. Prevalence and severity of pain in cancer patients in an outpatient palliative care setting in Saudi Arabia. Qatar Med. J. 2014, 1, 38–45. [Google Scholar] [CrossRef][Green Version]
- Blank, A.T.; Lerman, D.M.; Shaw, S.; Dadrass, F.; Zhang, Y.; Liu, W.; Hung, M.; Jones, K.B.; Randall, R.L. PROMIS(®) scores in operative metastatic bone disease patients: A multicenter, prospective study. J. Surg. Oncol. 2018, 118, 532–535. [Google Scholar] [CrossRef] [PubMed]
- Bouché, O.; Le Cesne, A.; Rios, M.; Chaigneau, L.; Italiano, A.; Duffaud, F.; Lecomte, T.; Arsène, D.; Manfredi, S.; Aparicio, T.; et al. EPigist: An observational real-life study on patients with metastatic gastrointestinal stromal tumors receiving imatinib. PLoS ONE 2018, 13, e0204117. [Google Scholar] [CrossRef] [PubMed]
- Bullock, A.; Stuart, K.; Jacobus, S.; Abrams, T.; Wadlow, R.; Goldstein, M.; Miksad, R. Capecitabine and oxaliplatin as first and second line treatment for locally advanced and metastatic pancreatic ductal adenocarcinoma. J. Gastrointest. Oncol. 2017, 8, 945–952. [Google Scholar] [CrossRef] [PubMed]
- Green, A.K.; Corty, R.W.; Wood, W.A.; Meeneghan, M.; Reeder-Hayes, K.E.; Basch, E.; Milowsky, M.I.; Dusetzina, S.B. Comparative effectiveness of mitoxantrone plus prednisone versus prednisone alone in metastatic castrate-resistant prostate cancer after docetaxel failure. Oncologist 2015, 20, 516–522. [Google Scholar] [CrossRef][Green Version]
- Iwase, S.; Kawaguchi, T.; Tokoro, A.; Yamada, K.; Kanai, Y.; Matsuda, Y.; Kashiwaya, Y.; Okuma, K.; Inada, S.; Ariyoshi, K.; et al. Assessment of cancer-related fatigue, pain, and quality of life in cancer patients at palliative care team referral: A multicenter observational study (JORTC PAL-09). PLoS ONE 2015, 10, e0134022. [Google Scholar] [CrossRef]
- Jespersen, E.; Nielsen, L.K.; Larsen, R.F.; Möller, S.; Jarlbæk, L. Everyday living with pain-reported by patients with multiple myeloma. Scand. J. Pain 2021, 21, 127–134. [Google Scholar] [CrossRef]
- King, M.T.; Stockler, M.R.; O’Connell, R.L.; Buizen, L.; Joly, F.; Lanceley, A.; Hilpert, F.; Okamoto, A.; Aotani, E.; Bryce, J.; et al. Measuring what matters MOST: Validation of the Measure of Ovarian Symptoms and Treatment, a patient-reported outcome measure of symptom burden and impact of chemotherapy in recurrent ovarian cancer. Qual. Life Res. 2018, 27, 59–74. [Google Scholar] [CrossRef]
- Koldenhof, J.J.; Witteveen, P.O.; De Vos, R.; Walraven, M.; Tillier, C.N.; Verheul, H.M.W.; Teunissen, S.C.C.M. Symptoms from treatment with sunitinib or sorafenib: A multicenter explorative cohort study to explore the influence of patient-reported outcomes on therapy decisions. Support. Care Cancer 2014, 22, 2371–2380. [Google Scholar] [CrossRef]
- Lavdaniti, M.; Fradelos, E.C.; Troxoutsou, K.; Zioga, E.; Mitsi, D.; Alikari, V.; Zyga, S. Symptoms in Advanced Cancer Patients in a Greek Hospital: A Descriptive Study. Asian Pac. J. Cancer Prev. 2018, 19, 1047–1052. [Google Scholar]
- LeBlanc, T.W.; Nickolich, M.; Rushing, C.N.; Samsa, G.P.; Locke, S.C.; Abernethy, A.P. What bothers lung cancer patients the most? A prospective, longitudinal electronic patient-reported outcomes study in advanced non-small cell lung cancer. Support. Care Cancer 2015, 23, 3455–3463. [Google Scholar] [CrossRef]
- Lechner, B.; Chow, S.; Chow, R.; Zhang, L.; Tsao, M.; Danjoux, C.; Barnes, E.; DeAngelis, C.; Vuong, S.; Ganesh, V.; et al. The incidence of neuropathic pain in bone metastases patients referred for palliative radiotherapy. Radiother. Oncol. 2016, 118, 557–561. [Google Scholar] [CrossRef] [PubMed]
- Madsen, M.; Grønbæk, H.; Finnerup, N.B.; Dam, G. A descriptive cross-sectional study of pain in patients with neuroendocrine tumors. Scand. J. Gastroenterol. 2017, 52, 431–436. [Google Scholar] [CrossRef] [PubMed]
- McFarland, D.C.; Shaffer, K.M.; Polizzi, H.; Mascarenhas, J.; Kremyanskaya, M.; Holland, J.; Hoffman, R. Prevalence of Physical Problems Detected by the Distress Thermometer and Problem List in Patients with Myeloproliferative Disorders. J. Natl. Compr. Cancer Netw. 2017, 15, 1503–1508. [Google Scholar] [CrossRef] [PubMed]
- Mercadante, S.; Aielli, F.; Masedu, F.; Valenti, M.; Verna, L.; Porzio, G. Age differences in the last week of life in advanced cancer patients followed at home. Support. Care Cancer 2016, 24, 1889–1895. [Google Scholar] [CrossRef] [PubMed]
- Sampogna, F.; Paradisi, A.; Iemboli, M.L.; Ricci, F.; Sonego, G.; Abeni, D. Comparison of quality of life between melanoma and non-melanoma skin cancer patients. Eur. J. Dermatol. 2019, 29, 185–191. [Google Scholar]
- Selvy, M.; Kerckhove, N.; Pereira, B.; Barreau, F.; Nguyen, D.; Busserolles, J.; Giraudet, F.; Cabrespine, A.; Chaleteix, C.; Soubrier, M.; et al. Prevalence of Chemotherapy-Induced Peripheral Neuropathy in Multiple Myeloma Patients and its Impact on Quality of Life: A Single Center Cross-Sectional Study. Front. Pharmacol. 2021, 12, 637593. [Google Scholar] [CrossRef]
- Steel, J.L.; Geller, D.A.; Kim, K.H.; Butterfield, L.H.; Spring, M.; Grady, J.; Sun, W.; Marsh, W.; Antoni, M.; Dew, M.A.; et al. Web-based collaborative care intervention to manage cancer-related symptoms in the palliative care setting. Cancer 2016, 122, 1270–1282. [Google Scholar] [CrossRef]
- Walling, A.M.; Weeks, J.C.; Kahn, K.L.; Tisnado, D.; Keating, N.L.; Dy, S.M.; Arora, N.K.; Mack, J.W.; Pantoja, P.M.; Malin, J.L. Symptom prevalence in lung and colorectal cancer patients. J. Pain Symptom Manag. 2015, 49, 192–202. [Google Scholar] [CrossRef]
- Zhou, T.; Yang, K.; Thapa, S.; Liu, H.; Wang, B.; Yu, S. Differences in Symptom Burden among Cancer Patients with Different Stages of Cachexia. J. Pain Symptom Manag. 2017, 53, 919–926. [Google Scholar] [CrossRef]
- Abu-Saad Huijer, H.; Sagherian, K.; Tamim, H. Validation of the Arabic Version of the Memorial Symptom Assessment Scale among Lebanese Cancer Patients. J. Pain Symptom Manag. 2015, 50, 559–565. [Google Scholar] [CrossRef]
- Bernardes, C.M.; Beesley, V.; Martin, J.; Sabesan, S.; Baade, P.; Meiklejohn, J.A.; Garvey, G.; Valery, P.C. Unmet supportive care needs among people with cancer: A cross-cultural comparison between Indigenous and Non-Indigenous Australians. Eur. J. Cancer Care 2019, 28, e13080. [Google Scholar] [CrossRef] [PubMed]
- Chan, A.; Lim, E.; Ng, T.; Shih, V.; Quek, R.; Cheung, Y.T. Symptom burden and medication use in adult sarcoma patients. Support. Care Cancer 2015, 23, 1709–1717. [Google Scholar] [CrossRef] [PubMed]
- Chen, F.; Leng, Y.; Zhang, L.; Xu, J.; Zhang, D.; Qin, Y.; Li, J.; Zheng, Y. The Correlation of Symptom Clusters and Functional Performance in Adult Acute Leukemia Patients under Chemotherapy. Cancer Nurs. 2021, 44, E287–E295. [Google Scholar] [CrossRef] [PubMed]
- Cheng, H.L.; Molassiotis, A.; Leung, A.K.T.; Wong, K.H. Docetaxel-Induced Peripheral Neuropathy in Breast Cancer Patients Treated with Adjuvant or Neo-Adjuvant Chemotherapy. Breast Care 2021, 16, 269–275. [Google Scholar] [CrossRef]
- Damm, M.; Weniger, M.; Kölsch, A.K.; Lampert, C.; Ceyhan, G.O.; Beer, S.; Schorn, S.; Moir, J.; Michl, P.; Rosendahl, J. The quality of pain management in pancreatic cancer: A prospective multi-center study. Pancreatology 2020, 20, 1511–1518. [Google Scholar] [CrossRef]
- Fujii, A.; Yamada, Y.; Takayama, K.; Nakano, T.; Kishimoto, J.; Morita, T.; Nakanishi, Y. Longitudinal assessment of pain management with the pain management index in cancer outpatients receiving chemotherapy. Support. Care Cancer 2017, 25, 925–932. [Google Scholar] [CrossRef]
- Gosselin, T.K.; Beck, S.; Abbot, D.H.; Grambow, S.C.; Provenzale, D.; Berry, P.; Kahn, K.L.; Malin, J.L. The Symptom Experience in Rectal Cancer Survivors. J. Pain Symptom Manag. 2016, 52, 709–718. [Google Scholar] [CrossRef]
- Han, C.J.; Reding, K.; Cooper, B.A.; Paul, S.M.; Conley, Y.P.; Hammer, M.; Kober, K.M.; Levine, J.D.; Miaskowski, C. Stability of Symptom Clusters in Patients with Gastrointestinal Cancers Receiving Chemotherapy. J. Pain Symptom Manag. 2019, 58, 989–1001.e10. [Google Scholar] [CrossRef]
- Joseph, A.O.; Salako, O.; Alabi, A.; Habeebu, M.; Balogun, O.; Ayodele, O.; Awofeso, O.M.; Adenipekun, A. Cancer pain control in a Nigerian oncology clinic: Treating the disease and not the patient. Pan Afr. Med. J. 2021, 40, 104. [Google Scholar] [CrossRef]
- Kim, H.S.; Oh, E.G.; Lee, H.; Kim, S.H.; Kim, H.K. Predictors of symptoms experience in Korean patients with cancer undergoing chemotherapy. Eur. J. Oncol. Nurs. 2015, 19, 644–653. [Google Scholar] [CrossRef]
- Kuperus, J.M.; Busman, R.D.; Kuipers, S.K.; Broekhuizen, H.T.; Noyes, S.L.; Brede, C.M.; Tobert, C.M.; Lane, B.R. Comparison of Side Effects and Tolerability Between Intravesical Bacillus Calmette-Guerin, Reduced-Dose BCG and Gemcitabine for Non-Muscle Invasive Bladder Cancer. Urology 2021, 156, 191–198. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.; Takita, C.; Wright, J.L.; Reis, I.M.; Zhao, W.; Nelson, O.L.; Hu, J.J. Characterization of risk factors for adjuvant radiotherapy-associated pain in a tri-racial/ethnic breast cancer population. Pain 2016, 157, 1122–1131. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Shi, Q.; Liu, M.; Jia, L.; He, B.; Yang, Y.; Liu, J.; Lin, H.; Lin, H.K.; Li, P.; et al. Validation and Application of the MD Anderson Symptom Inventory for Traditional Chinese Medicine (MDASI-TCM). J. Natl. Cancer Inst. Monogr. 2017, 52, lgx010. [Google Scholar] [CrossRef]
- Llamas Ramos, I.; Llamas Ramos, R.; Martín Nogueras, A.M.; Alvarado Omenat, J.J.; Calvo Arenillas, J.I.; Fonseca Sánchez, E.; Cortés Rodríguez, M. Reliability and Validity of the Spanish Version of the Memorial Symptom Assessment Scale in Oncology Patients. J. Pain Symptom Manag. 2016, 52, 884–891. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, Y.; Yoshida, Y.; Kiba, S.; Yamashiro, S.; Nogami, H.; Ohashi, N.; Kajitani, R.; Munechika, T.; Nagano, H.; Komono, A.; et al. Acute chemotherapy-induced peripheral neuropathy due to oxaliplatin administration without cold stimulation. Support. Care Cancer 2020, 28, 5405–5410. [Google Scholar] [CrossRef] [PubMed]
- Molassiotis, A.; Cheng, H.L.; Lopez, V.; Au, J.S.K.; Chan, A.; Bandla, A.; Leung, K.T.; Li, Y.C.; Wong, K.H.; Suen, L.K.P.; et al. Are we mis-estimating chemotherapy-induced peripheral neuropathy? Analysis of assessment methodologies from a prospective, multinational, longitudinal cohort study of patients receiving neurotoxic chemotherapy. BMC Cancer 2019, 19, 132. [Google Scholar] [CrossRef]
- Moye, J.; June, A.; Martin, L.A.; Gosian, J.; Herman, L.I.; Naik, A.D. Pain is prevalent and persisting in cancer survivors: Differential factors across age groups. J. Geriatr. Oncol. 2014, 5, 190–196. [Google Scholar] [CrossRef]
- Pearce, A.; Haas, M.; Viney, R.; Pearson, S.A.; Haywood, P.; Brown, C.; Ward, R. Incidence and severity of self-reported chemotherapy side effects in routine care: A prospective cohort study. PLoS ONE 2017, 12, e0184360. [Google Scholar] [CrossRef]
- Pérez, C.; Sánchez-Martínez, N.; Ballesteros, A.; Blanco, T.; Collazo, A.; González, F.; Villoria, J. Prevalence of pain and relative diagnostic performance of screening tools for neuropathic pain in cancer patients: A cross-sectional study. Eur. J. Pain 2015, 19, 752–761. [Google Scholar] [CrossRef]
- Pettersson, G.; Berterö, C.; Unosson, M.; Börjeson, S. Symptom prevalence, frequency, severity, and distress during chemotherapy for patients with colorectal cancer. Support. Care Cancer 2014, 22, 1171–1179. [Google Scholar] [CrossRef]
- Raj, S.X.; Thronaes, M.; Brunelli, C.; Hjermstad, M.J.; Klepstad, P.; Kaasa, S. A cross-sectional study on prevalence of pain and breakthrough pain among an unselected group of outpatients in a tertiary cancer clinic. Support. Care Cancer 2014, 22, 1965–1971. [Google Scholar] [CrossRef] [PubMed]
- Ritchie, C.; Dunn, L.B.; Paul, S.M.; Cooper, B.A.; Skerman, H.; Merriman, J.D.; Aouizerat, B.; Alexander, K.; Yates, P.; Cataldo, J.; et al. Differences in the symptom experience of older oncology outpatients. J. Pain Symptom Manag. 2014, 47, 697–709. [Google Scholar] [CrossRef] [PubMed]
- Salvetti, M.G.; Machado, C.S.P.; Donato, S.C.T.; Silva, A.M.D. Prevalence of symptoms and quality of life of cancer patients. Rev. Bras. Enferm. 2020, 73, e20180287. [Google Scholar] [CrossRef] [PubMed]
- Schumacher, O.; Galvao, D.A.; Taaffe, D.R.; Spry, N.; Joseph, D.; Tang, C.; Chee, R.; Newton, R.U. Effect of Exercise Adjunct to Radiation and Androgen Deprivation Therapy on Patient-Reported Treatment Toxicity in Men with Prostate Cancer: A Secondary Analysis of 2 Randomized Controlled Trials. Pract. Radiat. Oncol. 2021, 11, 215–225. [Google Scholar] [CrossRef]
- Seven, M.; Sahin, E.; Yilmaz, S.; Akyuz, A. Palliative care needs of patients with gynaecologic cancer. J. Clin. Nurs. 2016, 25, 3152–3159. [Google Scholar] [CrossRef] [PubMed]
- Spoelstra, S.L.; Given, C.W.; Sikorskii, A.; Majumder, A.; Schueller, M.; Given, B.A. Treatment with oral anticancer agents: Symptom severity and attribution, and interference with comorbidity management. Oncol. Nurs. Forum 2015, 42, 80–88. [Google Scholar] [CrossRef]
- Stamm, S.L.; Spichiger, E.; Pabst, T.; Bachnick, S.; Jeitziner, M.M. Symptom prevalence and health-related quality of life in patients undergoing autologous stem cell transplantation—A longitudinal observational study. Eur. J. Oncol. Nurs. 2021, 53, 101997. [Google Scholar] [CrossRef]
- Steffen McLouth, L.E.; Lycan, T.W.; Levine, B.J.; Gabbard, J.; Ruiz, J.; Farris, M.; Grant, S.C.; Pajewski, N.M.; Weaver, K.E.; Petty, W.J. Patient-Reported Outcomes From Patients Receiving Immunotherapy or Chemoimmunotherapy for Metastatic Non–Small-Cell Lung Cancer in Clinical Practice. Clin. Lung Cancer 2020, 21, 255–263.e4. [Google Scholar] [CrossRef]
- Thiagarajan, M.; Chan, C.M.; Fuang, H.G.; Beng, T.S.; Atiliyana, M.A.; Yahaya, N.A. Symptom Prevalence and Related Distress in Cancer Patients Undergoing Chemotherapy. Asian Pac. J. Cancer Prev. 2016, 17, 171–176. [Google Scholar] [CrossRef]
- Turner, J.P.; Shakib, S.; Singhal, N.; Hogan-Doran, J.; Prowse, R.; Johns, S.; Thynne, T.; Bell, J.S. Statin use and pain in older people with cancer: A cross-sectional study. J. Am. Geriatr. Soc. 2014, 62, 1900–1905. [Google Scholar] [CrossRef]
- Unseld, M.; Zeilinger, E.L.; Fellinger, M.; Lubowitzki, S.; Krammer, K.; Nader, I.W.; Hafner, M.; Kitta, A.; Adamidis, F.; Masel, E.K.; et al. Prevalence of pain and its association with symptoms of post-traumatic stress disorder, depression, anxiety and distress in 846 cancer patients: A cross sectional study. Psychooncology 2021, 30, 504–510. [Google Scholar] [CrossRef]
- van der Baan, F.H.; Koldenhof, J.J.; de Nijs, E.J.; Echteld, M.A.; Zweers, D.; Hesselmann, G.M.; Vervoort, S.C.; Vos, J.B.; de Graaf, E.; Witteveen, P.O.; et al. Validation of the Dutch version of the Edmonton Symptom Assessment System. Cancer Med. 2020, 9, 6111–6121. [Google Scholar] [CrossRef]
- Wang, D.; Fu, J. Symptom clusters and quality of life in China patients with lung cancer undergoing chemotherapy. Afr. Health Sci. 2014, 14, 49–55. [Google Scholar] [CrossRef]
- Yahaya, N.A.; Subramanian, P.; Bustam, A.Z.; Taib, N.A. Symptom experiences and coping strategies among multi- ethnic solid tumor patients undergoing chemotherapy in Malaysia. Asian Pac. J. Cancer Prev. 2015, 16, 723–730. [Google Scholar] [CrossRef]
- Zhong, B.L.; Li, S.H.; Lv, S.Y.; Tian, S.L.; Liu, Z.D.; Li, X.B.; Zhuang, H.Q.; Tao, R.; Zhang, W.; Zhuo, C.J. Suicidal ideation among Chinese cancer inpatients of general hospitals: Prevalence and correlates. Oncotarget 2017, 8, 25141–25150. [Google Scholar] [CrossRef]
- Adams, E.; Boulton, M.G.; Horne, A.; Rose, P.W.; Durrant, L.; Collingwood, M.; Oskrochi, R.; Davidson, S.E.; Watson, E.K. The effects of pelvic radiotherapy on cancer survivors: Symptom profile, psychological morbidity and quality of life. Clin. Oncol. (R. Coll. Radiol.) 2014, 26, 10–17. [Google Scholar] [CrossRef]
- Ahmed, A.; Bhatnagar, S.; Rana, S.P.S.; Ahmad, S.M.; Joshi, S.; Mishra, S. Prevalence of phantom breast pain and sensation among postmastectomy patients suffering from breast cancer: A prospective study. Pain Pract. 2014, 14, E17–E28. [Google Scholar] [CrossRef]
- Al Maqbali, M. Sleep disturbance among Arabic breast cancer survivors. Support. Care Cancer 2021, 29, 5179–5186. [Google Scholar] [CrossRef]
- Andersen, K.G.; Duriaud, H.M.; Jensen, H.E.; Kroman, N.; Kehlet, H. Predictive factors for the development of persistent pain after breast cancer surgery. Pain 2015, 156, 2413–2422. [Google Scholar] [CrossRef]
- Asplund, D.; Prytz, M.; Bock, D.; Haglind, E.; Angenete, E. Persistent perineal morbidity is common following abdominoperineal excision for rectal cancer. Int. J. Color. Dis. 2015, 30, 1563–1570. [Google Scholar] [CrossRef]
- Baden, M.; Lu, L.; Drummond, F.J.; Gavin, A.; Sharp, L. Pain, fatigue and depression symptom cluster in survivors of prostate cancer. Support. Care Cancer 2020, 28, 4813–4824. [Google Scholar] [CrossRef] [PubMed]
- Bao, T.; Seidman, A.; Li, Q.; Seluzicki, C.; Blinder, V.; Meghani, S.H.; Farrar, J.T.; Mao, J.J. Living with chronic pain: Perceptions of breast cancer survivors. Breast Cancer Res. Treat. 2018, 169, 133–140. [Google Scholar] [CrossRef]
- Bennedsgaard, K.; Ventzel, L.; Themistocleous, A.C.; Bennett, D.L.; Jensen, A.B.; Jensen, A.R.; Andersen, N.T.; Jensen, T.S.; Tankisi, H.; Finnerup, N.B. Long-term symptoms of polyneuropathy in breast and colorectal cancer patients treated with and without adjuvant chemotherapy. Cancer Med. 2020, 9, 5114–5123. [Google Scholar] [CrossRef]
- Boehmer, U.; Potter, J.; Clark, M.A.; Ozonoff, A.; Winter, M.; Berklein, F.; Ward, K.C.; Hartshorn, K. Assessing the relationship between symptoms and health care utilization in colorectal cancer survivors of different sexual orientations. Support. Care Cancer 2021, 29, 5821–5830. [Google Scholar] [CrossRef] [PubMed]
- Bøhn, S.K.H.; Thorsen, L.; Kiserud, C.E.; Fosså, S.D.; Lie, H.C.; Loge, J.H.; Wisløff, T.; Haugnes, H.S.; Reinertsen, K.V. Chronic fatigue and associated factors among long-term survivors of cancers in young adulthood. Acta Oncol. 2019, 58, 753–762. [Google Scholar] [CrossRef]
- Bonhof, C.S.; Trompetter, H.R.; Vreugdenhil, G.; van de Poll-Franse, L.V.; Mols, F. Painful and non-painful chemotherapy-induced peripheral neuropathy and quality of life in colorectal cancer survivors: Results from the population-based PROFILES registry. Support. Care Cancer 2020, 28, 5933–5941. [Google Scholar] [CrossRef] [PubMed]
- Bovbjerg, D.H.; Keefe, F.J.; Soo, M.S.; Manculich, J.; Van Denburg, A.; Zuley, M.L.; Ahrendt, G.M.; Skinner, C.S.; Edmond, S.N.; Shelby, R.A. Persistent breast pain in post-surgery breast cancer survivors and women with no history of breast surgery or cancer: Associations with pain catastrophizing, perceived breast cancer risk, breast cancer worry, and emotional distress. Acta Oncol. 2019, 58, 763–768. [Google Scholar] [CrossRef]
- Bulley, C.; Coutts, F.; Blyth, C.; Jack, W.; Chetty, U.; Barber, M.; Tan, C.W. A morbidity Screening Tool for identifying fatigue, pain, upper limb dysfunction and lymphedema after breast cancer treatment: A validity study. Eur. J. Oncol. Nurs. 2014, 18, 218–227. [Google Scholar] [CrossRef]
- Cameron, K.E.; Kole, M.B.; Sammel, M.D.; Ginsberg, J.P.; Gosiengfiao, Y.; Mersereau, J.E.; Su, H.I.; Gracia, C.R. Acute Menopausal Symptoms in Young Cancer Survivors Immediately following Chemotherapy. Oncology 2018, 94, 200–206. [Google Scholar] [CrossRef]
- Capelan, M.; Battisti, N.M.L.; McLoughlin, A.; Maidens, V.; Snuggs, N.; Slyk, P.; Peckitt, C.; Ring, A.; Battisti, N.M.L. The prevalence of unmet needs in 625 women living beyond a diagnosis of early breast cancer. Br. J. Cancer 2017, 117, 1113–1120. [Google Scholar] [CrossRef]
- Chiang, D.L.C.; Rice, D.A.; Helsby, N.A.; Somogyi, A.A.; Kluger, M.T. The Prevalence, Impact, and Risk Factors for Persistent Pain After Breast Cancer Surgery in a New Zealand Population. Pain Med. 2019, 20, 1803–1814. [Google Scholar] [CrossRef] [PubMed]
- Cui, L.; Fan, P.; Qiu, C.; Hong, Y. Single institution analysis of incidence and risk factors for post-mastectomy pain syndrome. Sci. Rep. 2018, 8, 11494. [Google Scholar] [CrossRef]
- De Groef, A.; Van Kampen, M.; Vervloesem, N.; De Geyter, S.; Christiaens, M.R.; Neven, P.; Vos, L.; De Vrieze, T.; Geraerts, I.; Devoogdt, N. Myofascial techniques have no additional beneficial effects to a standard physical therapy programme for upper limb pain after breast cancer surgery: A randomized controlled trial. Clin. Rehabil. 2017, 31, 1625–1635. [Google Scholar] [CrossRef] [PubMed]
- Dieterich, M.; Allmendinger, S.; Gerber, B.; Reimer, T.; Hartmann, S.; Stachs, A.; Stubert, J. Prevalence, Clinical Significance and Risk Factors for Developing Scar Pain and Sensibility Disorders in Breast Cancer Patients after Breast-Conserving Therapy and Mastectomy. Breast Care 2021, 16, 507–515. [Google Scholar] [CrossRef] [PubMed]
- Drury, A.; Payne, S.; Brady, A.M. The cost of survival: An exploration of colorectal cancer survivors’ experiences of pain. Acta Oncol. 2017, 56, 205–211. [Google Scholar] [CrossRef]
- Dualé, C.; Ouchchane, L.; Schoeffler, P.; Dubray, C. Neuropathic aspects of persistent postsurgical pain: A French multicenter survey with a 6-month prospective follow-up. J. Pain 2014, 15, e1–e24. [Google Scholar] [CrossRef]
- Efficace, F.; Breccia, M.; Avvisati, G.; Cottone, F.; Intermesoli, T.; Borlenghi, E.; Carluccio, P.; Rodeghiero, F.; Fabbiano, F.; Luppi, M.; et al. Health-related quality of life, symptom burden, and comorbidity in long-term survivors of acute promyelocytic leukemia. Leukemia 2019, 33, 1598–1607. [Google Scholar] [CrossRef] [PubMed]
- Engvall, K.; Gréen, H.; Fredriksson, M.; Åvall-Lundqvist, E. Persistent neuropathy among early-stage breast cancer survivors in a population-based cohort. Br. J. Cancer 2021, 125, 445–457. [Google Scholar] [CrossRef] [PubMed]
- Ezendam, N.P.M.; Pijlman, B.; Bhugwandass, C.; Pruijt, J.F.M.; Mols, F.; Vos, M.C.; Pijnenborg, J.M.A.; Van De Poll-Franse, L.V. Chemotherapy-induced peripheral neuropathy and its impact on health-related quality of life among ovarian cancer survivors: Results from the population-based PROFILES registry. Gynecol. Oncol. 2014, 135, 510–517. [Google Scholar] [CrossRef]
- Farrukh, N.; Hageman, L.; Chen, Y.; Wu, J.; Ness, E.; Kung, M.; Francisco, L.; Parman, M.; Landier, W.; Arora, M.; et al. Pain in older survivors of hematologic malignancies after blood or marrow transplantation: A BMTSS report. Cancer 2020, 126, 2003–2012. [Google Scholar] [CrossRef]
- Feddern, M.L.; Jensen, T.S.; Laurberg, S. Chronic pain in the pelvic area or lower extremities after rectal cancer treatment and its impact on quality of life: A population-based cross-sectional study. Pain 2015, 156, 1765–1771. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, A.R.; Di Meglio, A.; Pistilli, B.; Gbenou, A.S.; El-Mouhebb, M.; Dauchy, S.; Charles, C.; Joly, F.; Everhard, S.; Lambertini, M.; et al. Differential impact of endocrine therapy and chemotherapy on quality of life of breast cancer survivors: A prospective patient-reported outcomes analysis. Ann. Oncol. 2019, 30, 1784–1795. [Google Scholar] [CrossRef]
- Gallaway, M.S.; Townsend, J.S.; Shelby, D.; Puckett, M.C. Pain among Cancer Survivors. Prev. Chronic Dis. 2020, 17, E54. [Google Scholar] [CrossRef]
- Gong, Y.; Tan, Q.; Qin, Q.; Wei, C. Prevalence of postmastectomy pain syndrome and associated risk factors: A large single-institution cohort study. Medicine 2020, 99, e19834. [Google Scholar] [CrossRef] [PubMed]
- Götze, H.; Taubenheim, S.; Dietz, A.; Lordick, F.; Mehnert, A. Comorbid conditions and health-related quality of life in long-term cancer survivors-associations with demographic and medical characteristics. J. Cancer Surviv. 2018, 12, 712–720. [Google Scholar] [CrossRef] [PubMed]
- Hammer, S.M.; Brown, J.C.; Segal, S.; Chu, C.S.; Schmitz, K.H. Cancer-related impairments influence physical activity in uterine cancer survivors. Med. Sci. Sports Exerc. 2014, 46, 2195–2201. [Google Scholar] [CrossRef]
- Hamood, R.; Hamood, H.; Merhasin, I.; Keinan-Boker, L.A. Feasibility study to assess the validity of administrative data sources and self-reported information of breast cancer survivors. Isr. J. Health Policy Res. 2016, 5, 50. [Google Scholar] [CrossRef]
- Hamood, R.; Hamood, H.; Merhasin, I.; Keinan-Boker, L. Chronic pain and other symptoms among breast cancer survivors: Prevalence, predictors, and effects on quality of life. Breast Cancer Res. Treat. 2018, 167, 157–169. [Google Scholar] [CrossRef]
- Haviland, J.S.; Mannino, M.; Griffin, C.; Porta, N.; Sydenham, M.; Bliss, J.M.; Yarnold, J.R. Late normal tissue effects in the arm and shoulder following lymphatic radiotherapy: Results from the UK START (Standardisation of Breast Radiotherapy) trials. Radiother. Oncol. 2017, 126, 155–162. [Google Scholar] [CrossRef]
- Henderson, J.R.; Tao, A.; Kirwan, C.C.; Barr, L. Immediate breast reconstruction does not increase postmastectomy pain. Ann. Surg. Oncol. 2014, 21, 113–117. [Google Scholar] [CrossRef]
- Henry, M.; Alias, A.; Cherba, M.; Woronko, C.; Rosberger, Z.; Hier, M.; Zeitouni, A.; Kost, K.; Mlynarek, A.; Richardson, K.; et al. Immediate post-treatment supportive care needs of patients newly diagnosed with head and neck cancer. Support. Care Cancer 2020, 28, 5557–5567. [Google Scholar] [CrossRef]
- Hope-Stone, L.; Brown, S.L.; Heimann, H.; Damato, B.; Salmon, P. Phantom Eye Syndrome: Patient Experiences after Enucleation for Uveal Melanoma. Ophthalmology 2015, 122, 1585–1590. [Google Scholar] [CrossRef]
- Huang, I.C.; Alberts, N.M.; Buckley, M.G.; Li, Z.; Ehrhardt, M.J.; Brinkman, T.M.; Allen, J.; Krull, K.R.; Klosky, J.L.; Greene, W.L.; et al. Change in pain status and subsequent opioid and marijuana use among long-term adult survivors of childhood cancer. JNCI Cancer Spectr. 2020, 4, pkaa070. [Google Scholar] [CrossRef]
- Janah, A.; Bouhnik, A.D.; Touzani, R.; Bendiane, M.K.; Peretti-Watel, P. Underprescription of Step III Opioids in French Cancer Survivors with Chronic Pain: A Call for Integrated Early Palliative Care in Oncology. J. Pain Symptom Manag. 2020, 59, 836–847. [Google Scholar] [CrossRef]
- Jansen, F.; Eerenstein, S.E.J.; Lissenberg-Witte, B.I.; van Uden-Kraan, C.F.; Leemans, C.R.; Leeuw, I.M.V.D. Unmet supportive care needs in patients treated with total laryngectomy and its associated factors. Head Neck 2018, 40, 2633–2641. [Google Scholar] [CrossRef]
- Jardim, L.C.; Flores, P.T.; do Carmo dos Santos Araújo, M.; Chiesa, J.; de Moraes, C.M.B.; Antoniazzi, R.P. Oral health–related quality of life in breast cancer survivors. Support. Care Cancer 2020, 28, 65–71. [Google Scholar] [CrossRef]
- Jariwala, P.; Kaur, N.A. descriptive study on prevalence of arm/shoulder problems and its impact on quality of life in breast cancer survivors. Indian J. Cancer 2021, 58, 201–206. [Google Scholar] [PubMed]
- Johannsdottir, I.M.R.; Hamre, H.; Fosså, S.D.; Loge, J.H.; Drolsum, L.; Lund, M.B.; Nordsletten, L.; Kiserud, C. Adverse Health Outcomes and Associations with Self-Reported General Health in Childhood Lymphoma Survivors. J. Adolesc. Young Adult Oncol. 2017, 6, 470–476. [Google Scholar] [CrossRef]
- Johannsen, M.; Christensen, S.; Zachariae, R.; Jensen, A.B. Socio-demographic, treatment-related, and health behavioral predictors of persistent pain 15 months and 7–9 years after surgery: A nationwide prospective study of women treated for primary breast cancer. Breast Cancer Res. Treat. 2015, 152, 645–658. [Google Scholar] [CrossRef] [PubMed]
- Juhl, A.A.; Christiansen, P.; Damsgaard, T.E. Persistent pain after breast cancer treatment: A questionnaire-based study on the prevalence, associated treatment variables, and pain type. J. Breast Cancer 2016, 19, 447–454. [Google Scholar] [CrossRef] [PubMed]
- Karlson, C.W.; Alberts, N.M.; Liu, W.; Brinkman, T.M.; Annett, R.D.; Mulrooney, D.A.; Schulte, F.; Leisenring, W.M.; Gibson, T.M.; Howell, R.M.; et al. Longitudinal pain and pain interference in long-term survivors of childhood cancer: A report from the Childhood Cancer Survivor Study. Cancer 2020, 126, 2915–2923. [Google Scholar] [CrossRef]
- Kaur, N.; Gupta, A.; Sharma, A.K.; Jain, A. Survivorship issues as determinants of quality of life after breast cancer treatment: Report from a limited resource setting. Breast 2018, 41, 120–126. [Google Scholar] [CrossRef]
- Kelada, L.; Wakefield, C.E.; Heathcote, L.C.; Jaaniste, T.; Signorelli, C.; Fardell, J.E.; Donoghoe, M.; McCarthy, M.C.; Gabriel, M.; Cohn, R.J. Perceived cancer-related pain and fatigue, information needs, and fear of cancer recurrence among adult survivors of childhood cancer. Patient Educ. Couns. 2019, 102, 2270–2278. [Google Scholar] [CrossRef] [PubMed]
- Kibar, S.; Dalyan Aras, M.; Ünsal Delialioğlu, S. The risk factors and prevalence of upper extremity impairments and an analysis of effects of lymphoedema and other impairments on the quality of life of breast cancer patients. Eur. J. Cancer Care 2017, 26, e12433. [Google Scholar] [CrossRef] [PubMed]
- Kjær, T.K.; Johansen, C.; Andersen, E.; Karlsen, R.; Nielsen, A.L.; Frederiksen, K.; Rørth, M.; Ibfelt, E.; Dalton, S.O. Influence of social factors on patient-reported late symptoms: Report from a controlled trial among long-term head and neck cancer survivors in Denmark. Head Neck 2016, 38, e1713–e1721. [Google Scholar] [CrossRef] [PubMed]
- Knowlton, S.E.; O’Donnell, E.K.; Horick, N.; Perez, G.K.; Park, E.; Rabin, J.; Quain, K.M.; Garton, J.; Peppercorn, J.M. Moving forward on all fronts: Impact, patterns, and barriers to exercise in cancer survivors and patients living with advanced disease. Support. Care Cancer 2020, 28, 4979–4988. [Google Scholar] [CrossRef]
- Koehler, L.A.; Hunter, D.W.; Blaes, A.H.; Haddad, T.C. Function, Shoulder Motion, Pain, and Lymphedema in Breast Cancer with and Without Axillary Web Syndrome: An 18-Month Follow-Up. Phys. Ther. 2018, 98, 518–527. [Google Scholar] [CrossRef] [PubMed]
- Kramer, N.; Shamley, D.; Ramjith, J. Prevalence of shoulder morbidity after treatment for breast Cancer in South Africa. Support. Care Cancer 2019, 27, 2591–2598. [Google Scholar] [CrossRef]
- Lou, D.I.; Dietrich, M.S.; Deng, J.; Murphy, B.A. Mechanisms of pain and their manifestations in head and neck cancer: Importance of classifying pain subtypes. Head Neck 2021, 43, 3720–3729. [Google Scholar] [CrossRef]
- Lunde, S.; Petersen, K.K.; Søgaard-Andersen, E.; Arendt-Nielsen, L. Preoperative quantitative sensory testing and robot-assisted laparoscopic hysterectomy for endometrial cancer: Can chronic postoperative pain be predicted? Scand. J. Pain 2020, 20, 693–705. [Google Scholar] [CrossRef]
- Mao, H.; Bao, T.; Shen, X.; Li, Q.; Seluzicki, C.; Im, E.O.; Mao, J.J. Prevalence and risk factors for fatigue among breast cancer survivors on aromatase inhibitors. Eur. J. Cancer 2018, 101, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Mertz, B.G.; Duriaud, H.M.; Kroman, N.; Andersen, K.G. Pain, sensory disturbances and psychological distress are common sequelae after treatment of ductal carcinoma in situ: A cross-sectional study. Acta Oncol. 2017, 56, 724–729. [Google Scholar] [CrossRef] [PubMed]
- Miaskowski, C.; Paul, S.M.; Cooper, B.; West, C.; Levine, J.D.; Elboim, C.; Hamolsky, D.; Abrams, G.; Luce, J.; Dhruva, A.; et al. Identification of patient subgroups and risk factors for persistent arm/shoulder pain following breast cancer surgery. Eur. J. Oncol. Nurs. 2014, 18, 242–253. [Google Scholar] [CrossRef]
- Min, J.; Yoo, S.; Kim, M.J.; Yang, E.; Hwang, S.; Kang, M.; Yu, M.S.; Yoon, C.; Heo, J.E.; Choi, Y.; et al. Exercise participation, barriers, and preferences in Korean prostate cancer survivors. Ethn. Health 2021, 26, 1130–1142. [Google Scholar] [CrossRef]
- Mulrooney, D.A.; Hyun, G.; Ness, K.K.; Bhakta, N.; Pui, C.H.; Ehrhardt, M.J.; Krull, K.R.; Crom, D.B.; Chemaitilly, W.; Srivastava, D.K.; et al. The changing burden of long-term health outcomes in survivors of childhood acute lymphoblastic leukaemia: A retrospective analysis of the St Jude Lifetime Cohort Study. Lancet Haematol. 2019, 6, e306–e316. [Google Scholar] [CrossRef]
- Paek, J.; Choi, Y.J. Association between hand grip strength and impaired health-related quality of life in Korean cancer survivors: A cross-sectional study. BMJ Open 2019, 9, e030938. [Google Scholar] [CrossRef] [PubMed]
- Park, J.W.; Kim, H.S.; Yun, J.Y.; Han, I. Neuropathic pain after sarcoma surgery: Prevalence and predisposing factors. Medicine 2018, 97, e10852. [Google Scholar] [CrossRef]
- Poço Gonçalves, J.; Veiga, D.; Araújo, A. Chronic pain, functionality and quality of life in cancer survivors. Br. J. Pain 2021, 15, 401–410. [Google Scholar] [CrossRef]
- Reilly, C.M.; Esiashvili, N.; Parashar, S.; Higgins, M. Subclinical Cardiovascular Disease in Lymphoma Survivors by Sex. J. Obstet. Gynecol. Neonatal Nurs. 2016, 45, 438–453. [Google Scholar] [CrossRef]
- Ren, J.L.; Rojo, R.D.; Perez, J.V.D.; Yeung, S.C.J.; Hanna, E.Y.; Reyes-Gibby, C.C. Variations in pain prevalence, severity, and analgesic use by duration of survivorship: A cross-sectional study of 505 post-treatment head and neck cancer survivors. BMC Cancer 2021, 21, 1304. [Google Scholar] [CrossRef]
- Rogers, J.L.; Vera, E.; Acquaye, A.; Briceno, N.; Jammula, V.; King, A.L.; Leeper, H.; Quezado, M.M.; Gonzalez Alarcon, J.; Boris, L.; et al. Living with a central nervous system (CNS) tumor: Findings on long-term survivorship from the NIH Natural History Study. Neurooncol. Pract. 2021, 8, 460–474. [Google Scholar] [CrossRef]
- Rosenberg, S.M.; Stanton, A.L.; Petrie, K.J.; Partridge, A.H. Symptoms and symptom attribution among women on endocrine therapy for breast cancer. Oncologist 2015, 20, 598–604. [Google Scholar] [CrossRef]
- Sanchez-Birkhead, A.C.; Carbajal-Salisbury, S.; Larreta, J.A.; Lovlien, L.; Hendricks, H.; Dingley, C.; Beck, S.L. A Community-Based Approach to Assessing the Physical, Emotional, and Health Status of Hispanic Breast Cancer Survivors. Hisp. Health Care Int. 2017, 15, 166–172. [Google Scholar] [CrossRef] [PubMed]
- Sanford, N.N.; Sher, D.J.; Butler, S.S.; Xu, X.; Ahn, C.; Aizer, A.A.; Mahal, B.A. Prevalence of chronic pain among cancer survivors in the United States, 2010–2017. Cancer 2019, 125, 4310–4318. [Google Scholar] [CrossRef]
- Schou Bredal, I.; Smeby, N.A.; Ottesen, S.; Warncke, T.; Schlichting, E. Chronic pain in breast cancer survivors: Comparison of psychosocial, surgical, and medical characteristics between survivors with and without pain. J. Pain Symptom Manag. 2014, 48, 852–862. [Google Scholar] [CrossRef]
- Selvy, M.; Pereira, B.; Kerckhove, N.; Gonneau, C.; Feydel, G.; Pétorin, C.; Vimal-Baguet, A.; Melnikov, S.; Kullab, S.; Hebbar, M.; et al. Long-term prevalence of sensory chemotherapy-induced peripheral neuropathy for 5 years after adjuvant folfox chemotherapy to treat colorectal cancer: A multicenter cross-sectional study. J. Clin. Med. 2020, 9, 2400. [Google Scholar] [CrossRef] [PubMed]
- Steyaert, A.; Forget, P.; Dubois, V.; Lavand’homme, P.; De Kock, M.; Lavand’homme, P. Does the perioperative analgesic/anesthetic regimen influence the prevalence of long-term chronic pain after mastectomy? J. Clin. Anesth. 2016, 33, 20–25. [Google Scholar] [CrossRef]
- Terkawi, A.S.; Tsang, S.; Alshehri, A.S.; Mulafikh, D.S.; Alghulikah, A.A.; AlDhahri, S.F. The burden of chronic pain after major head and neck tumor therapy. Saudi J. Anaesth. 2017, 11, s71–s79. [Google Scholar] [CrossRef]
- Tonning Olsson, I.; Alberts, N.M.; Li, C.; Ehrhardt, M.J.; Mulrooney, D.A.; Liu, W.; Pappo, A.S.; Bishop, M.W.; Anghelescu, D.L.; Srivastava, D.; et al. Pain and functional outcomes in adult survivors of childhood cancer: A report from the St. Jude Lifetime Cohort study. Cancer 2021, 127, 1679–1689. [Google Scholar] [CrossRef]
- Tung, S.; Davis, L.E.; Hallet, J.; Mavros, M.N.; Mahar, A.L.; Bubis, L.D.; Hammad, A.; Zhao, H.; Earle, C.C.; Barbera, L.; et al. Population-Level Symptom Assessment Following Pancreaticoduodenectomy for Adenocarcinoma. JAMA Surg. 2019, 154, e193348. [Google Scholar] [CrossRef]
- van de Luijtgaarden, A.C.M.; Kapusta, L.; Bellersen, L.; Bokkerink, J.P.M.; Kaal, S.E.J.; Versleijen-Jonkers, Y.M.H.; Schreuder, H.W.B.; van der Graaf, W.T.A. High prevalence of late adverse events in malignant bone tumour survivors diagnosed at adult age. Neth. J. Med. 2014, 72, 516–522. [Google Scholar] [PubMed]
- van Eck, I.; Den Hollander, D.; Desar, I.M.E.; Soomers, V.L.M.N.; van de Sande, M.A.J.; de Haan, J.J.; Verhoef, C.; Vriens, I.J.H.; Bonenkamp, J.J.; van der Graaf, W.T.A.; et al. Unraveling the heterogeneity of sarcoma survivors’ health-related quality of life regarding primary sarcoma location: Results from the Survsarc study. Cancers 2020, 12, 3083. [Google Scholar] [CrossRef] [PubMed]
- Variawa, M.L.; Scribante, J.; Perrie, H.; Chetty, S. The prevalence of chronic postmastectomy pain syndrome in female breast cancer survivors. S. Afr. J. Anaesth. Analg. 2016, 22, 108–113. [Google Scholar] [CrossRef]
- Vuksanovic, D.; Sanmugarajah, J.; Lunn, D.; Sawhney, R.; Eu, K.; Liang, R. Unmet needs in breast cancer survivors are common, and multidisciplinary care is underutilised: The Survivorship Needs Assessment Project. Breast Cancer 2021, 28, 289–297. [Google Scholar] [CrossRef]
- Wilson, C.L.; Brinkman, T.M.; Cook, C.; Huang, S.; Hyun, G.; Green, D.M.; Furman, W.L.; Bhakta, N.; Ehrhardt, M.J.; Krasin, M.J.; et al. Clinically ascertained health outcomes, quality of life, and social attainment among adult survivors of neuroblastoma: A report from the St. Jude Lifetime Cohort. Cancer 2020, 126, 1330–1338. [Google Scholar] [CrossRef]
- Aktas, A.; Walsh, D.; Hu, B. Cancer symptom clusters: An exploratory analysis of eight statistical techniques. J. Pain Symptom Manag. 2014, 48, 1254–1266. [Google Scholar] [CrossRef]
- Corli, O.; Pellegrini, G.; Bosetti, C.; Riva, L.; Crippa, M.; Amodio, E.; Scaccabarozzi, G. Impact of palliative care in evaluating and relieving symptoms in patients with advanced cancer. Results from the demetra study. Int. J. Environ. Res. Public Health 2020, 17, 8429. [Google Scholar] [CrossRef] [PubMed]
- de la Cruz, M.; Noguera, A.; San Miguel-Arregui, M.T.; Williams, J.; Chisholm, G.; Bruera, E. Delirium, agitation, and symptom distress within the final seven days of life among cancer patients receiving hospice care. Palliat. Support. Care 2015, 13, 211–216. [Google Scholar] [CrossRef]
- Drat-Gzubicka, J.; Pyszora, A.; Budzyński, J.; Currow, D.; Krajnik, M. Is neuropathic pain a good marker of peripheral neuropathy in hospice patients with advanced cancer? The single center pilot study. Diagnostics 2021, 11, 1377. [Google Scholar] [CrossRef]
- Gupta, M.; Sahi, M.S.; Bhargava, A.K.; Talwar, V. A Prospective Evaluation of Symptom Prevalence and Overall Symptom Burden among Cohort of Critically Ill Cancer Patients. Indian J. Palliat. Care 2016, 22, 118–124. [Google Scholar] [CrossRef]
- Guthrie, D.M.; Harman, L.E.; Barbera, L.; Burge, F.; Lawson, B.; McGrail, K.; Sutradhar, R.; Seow, H. Quality Indicator Rates for Seriously Ill Home Care Clients: Analysis of Resident Assessment Instrument for Home Care Data in Six Canadian Provinces. J. Palliat. Med. 2019, 22, 1346–1356. [Google Scholar] [CrossRef] [PubMed]
- Hui, D.; Abdelghani, E.; Chen, J.; Dibaj, S.; Zhukovsky, D.; Dev, R.; Tanco, K.; Haider, A.; Azhar, A.; Reddy, A.; et al. Chronic non-malignant pain in patients with cancer seen at a timely outpatient palliative care clinic. Cancers 2020, 12, 214. [Google Scholar] [CrossRef] [PubMed]
- Mejin, M.; Keowmani, T.; Abdul Rahman, S.; Liew, J.; Lai, J.; Chua, M.; Ilmiyah, C.W. Prevalence of pain and treatment outcomes among cancer patients in a Malaysian palliative care unit. Pharm. Pract. 2019, 17, 1–9. [Google Scholar] [CrossRef]
- Mercadante, S.; Masedu, F.; Balzani, I.; De Giovanni, D.; Montanari, L.; Pittureri, C.; Bertè, R.; Russo, D.; Ursini, L.; Marinangeli, F.; et al. Prevalence of delirium in advanced cancer patients in home care and hospice and outcomes after 1 week of palliative care. Support. Care Cancer 2018, 26, 913–919. [Google Scholar] [CrossRef] [PubMed]
- Morita, T.; Sato, K.; Miyashita, M.; Yamagishi, A.; Kizawa, Y.; Shima, Y.; Kinoshita, H.; Suzuki, S.; Shirahige, Y.; Yamaguchi, T.; et al. Does a regional comprehensive palliative care program improve pain in outpatient cancer patients? Support. Care Cancer 2014, 22, 2445–2455. [Google Scholar] [CrossRef] [PubMed]
- Rojas-Concha, L.; Hansen, M.B.; Petersen, M.A.; Groenvold, M. Which symptoms and problems do advanced cancer patients admitted to specialized palliative care report in addition to those included in the EORTC QLQ-C15-PAL? A register-based national study. Support. Care Cancer 2020, 28, 1725–1735. [Google Scholar] [CrossRef]
- Seow, H.; Guthrie, D.M.; Stevens, T.; Barbera, L.C.; Burge, F.; McGrail, K.; Chan, K.K.W.; Peacock, S.J.; Sutradhar, R. Trajectory of End-of-Life Pain and Other Physical Symptoms among Cancer Patients Receiving Home Care. Curr. Oncol. 2021, 28, 1641–1651. [Google Scholar] [CrossRef]
- Silvia, A.P.; Adriana, P.N.; Laura, G.G.; Edith, M.C.; Emma, V.A. Reality, Delays, and Challenges within Pain Prevalence and Treatment in Palliative Care Patients: A Survey of First-Time Patients at the National Cancer Institute in Mexico. J. Palliat. Care 2021, 36, 181–187. [Google Scholar] [CrossRef]
- Tofthagen, C.; Visovsky, C.; Dominic, S.; McMillan, S. Neuropathic symptoms, physical and emotional well-being, and quality of life at the end of life. Support. Care Cancer 2019, 27, 3357–3364. [Google Scholar] [CrossRef]
- Yamagishi, A.; Sato, K.; Miyashita, M.; Shima, Y.; Kizawa, Y.; Umeda, M.; Kinoshita, H.; Shirahige, Y.; Akiyama, M.; Yamaguchi, T.; et al. Changes in quality of care and quality of life of outpatients with advanced cancer after a regional palliative care intervention program. J. Pain Symptom Manag. 2014, 48, 602–610. [Google Scholar] [CrossRef]
- Yanaizumi, R.; Nagamine, Y.; Harada, S.; Kojima, K.; Tazawa, T.; Goto, T. Prevalence of neuropathic pain in terminally ill patients with cancer admitted to a general ward: A prospective observational study. J. Int. Med. Res. 2021, 49, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Aguilar, M.L.; Sandow, P.; Werning, J.W.; Brenneman, L.; Psoter, W.J. The Head and Neck Cancer Patient Concern Inventory(©): Patient Concerns’ Prevalence, Dental Concerns’ Impact, and Relationships of Concerns with Quality of Life Measures. J. Prosthodont. 2017, 26, 186–195. [Google Scholar] [CrossRef] [PubMed]
- Alemayehu, M.; Deyessa, N.; Medihin, G.; Fekadu, A. A descriptive analysis of depression and pain complaints among patients with cancer in a low income country. PLoS ONE 2018, 13, e0193713. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, T.S.; Vera-Bolanos, E.; Acquaye, A.A.; Gilbert, M.R.; Ladha, H.; Mendoza, T. The symptom burden of primary brain tumors: Evidence for a core set of tumor- and treatment-related symptoms. Neuro-Oncology 2016, 18, 252–260. [Google Scholar] [CrossRef]
- Bacorro, W.R.; Sy Ortin, T.T.; Suarez, C.G.; Mendoza, T.R.; Que, J.C. Validation of the MD Anderson Symptom Inventory-Head-and-Neck-Filipino (MDASI-HN-F): Clinical utility of symptom screening among patients with head-and-neck cancer. BMJ Support. Palliat. Care 2017, 7, 140–149. [Google Scholar] [CrossRef]
- Batalini, F.; Gomes, M.; Fábio, I.; Kuwae, F.; Macanhan, G.; Pereira, J.L.B. Cancer complaints: The profile of patients from the emergency department of a Brazilian oncology teaching hospital. F1000Research 2017, 6, 1919.3. [Google Scholar] [CrossRef]
- Bauml, J.; Chen, L.; Chen, J.; Boyer, J.; Kalos, M.; Li, S.Q.; DeMichele, A.; Mao, J.J. Arthralgia among women taking aromatase inhibitors: Is there a shared inflammatory mechanism with co-morbid fatigue and insomnia? Breast Cancer Res. 2015, 17, 89. [Google Scholar] [CrossRef]
- Beesley, V.L.; Wockner, L.F.; O’Rourke, P.; Janda, M.; Goldstein, D.; Gooden, H.; Merrett, N.D.; O’Connell, D.L.; Rowlands, I.J.; Wyld, D.K.; et al. Risk factors for current and future unmet supportive care needs of people with pancreatic cancer. A longitudinal study. Support. Care Cancer 2016, 24, 3589–3599. [Google Scholar] [CrossRef]
- Bhattacharya, I.S.; Haviland, J.S.; Kirby, A.M.; Kirwan, C.C.; Hopwood, P.; Yarnold, J.R.; Bliss, J.M.; Coles, C.E. Patient-Reported Outcomes Over 5 Years After Whole- or Partial-Breast Radiotherapy: Longitudinal Analysis of the IMPORT LOW (CRUK/06/003) Phase III Randomized Controlled Trial. J. Clin. Oncol. 2019, 37, 305–317. [Google Scholar] [CrossRef]
- Bonhof, C.S.; Mols, F.; Vos, M.C.; Pijnenborg, J.M.A.; Boll, D.; Vreugdenhil, G.; Ezendam, N.P.M.; van de Poll-Franse, L.V. Course of chemotherapy-induced peripheral neuropathy and its impact on health-related quality of life among ovarian cancer patients: A longitudinal study. Gynecol. Oncol. 2018, 149, 455–463. [Google Scholar] [CrossRef]
- Bouhassira, D.; Luporsi, E.; Krakowski, I. Prevalence and incidence of chronic pain with or without neuropathic characteristics in patients with cancer. Pain 2017, 158, 1118–1125. [Google Scholar] [CrossRef] [PubMed]
- Boyes, A.W.; Clinton-McHarg, T.; Waller, A.E.; Steele, A.; D’Este, C.A.; Sanson-Fisher, R.W. Prevalence and correlates of the unmet supportive care needs of individuals diagnosed with a haematological malignancy. Acta Oncol. 2015, 54, 507–514. [Google Scholar] [CrossRef] [PubMed]
- Braamse, A.M.J.; Van Meijel, B.; Visser, O.; Huijgens, P.C.; Beekman, A.T.F.; Dekker, J. Distress, problems and supportive care needs of patients treated with auto-or allo-SCT. Bone Marrow Transplant. 2014, 49, 292–298. [Google Scholar] [CrossRef]
- Braga-Neto, M.B.; Carneiro, J.G.; de Castro Barbosa, A.M.; Silva, I.S.; Maia, D.C.; Maciel, F.S.; de Alcântara, R.J.A.; Vasconscelos, P.R.L.; Braga, L.L.B.C.; de Alcântara, R.J.A. Clinical characteristics of distal gastric cancer in young adults from Northeastern Brazil. BMC Cancer 2018, 18, 131. [Google Scholar] [CrossRef] [PubMed]
- Bubis, L.D.; Davis, L.E.; Canaj, H.; Gupta, V.; Jeong, Y.; Barbera, L.; Li, Q.; Moody, L.; Karanicolas, P.J.; Sutradhar, R.; et al. Patient-Reported Symptom Severity Among 22,650 Cancer Outpatients in the Last Six Months of Life. J. Pain Symptom Manag. 2020, 59, 58–66.e4. [Google Scholar] [CrossRef]
- Buckley, S.A.; Jimenez-Sahagun, D.; Othus, M.; Walter, R.B.; Lee, S.J.; Jimenez-Sahagun, D. Quality of life from the perspective of the patient with acute myeloid leukemia. Cancer 2018, 124, 145–152. [Google Scholar] [CrossRef]
- Cho, S.F.; Rau, K.M.; Shao, Y.Y.; Yen, C.J.; Wu, M.F.; Chen, J.S.; Chang, C.S.; Yeh, S.P.; Chiou, T.J.; Hsieh, R.K.; et al. Patients with head and neck cancer may need more intensive pain management to maintain daily functioning: A multi-center study. Support. Care Cancer 2019, 27, 1663–1672. [Google Scholar] [CrossRef]
- Clover, K.A.; Rogers, K.M.; Britton, B.; Oldmeadow, C.; Attia, J.; Carter, G.L. Reduced prevalence of pain and distress during 4 years of screening with QUICATOUCH in Australian oncology patients. Eur. J. Cancer Care 2017, 26, e12636. [Google Scholar] [CrossRef]
- Daly, L.E.; Dolan, R.D.; Power, D.G.; Ní Bhuachalla, É.; Sim, W.; Cushen, S.J.; Fallon, M.; Simmons, C.; McMillan, D.C.; Laird, B.J.; et al. Determinants of quality of life in patients with incurable cancer. Cancer 2020, 126, 2872–2882. [Google Scholar] [CrossRef]
- Davies, A.; Buchanan, A.; Todd, J.; Gregory, A.; Batsari, K.M. Oral symptoms in patients with advanced cancer: An observational study using a novel oral symptom assessment scale. Support. Care Cancer 2021, 29, 4357–4364. [Google Scholar] [CrossRef]
- Davis, L.E.; Bubis, L.D.; Mahar, A.L.; Li, Q.; Sussman, J.; Moody, L.; Barbera, L.; Holloway, C.M.B.; Coburn, N.G. Patient-reported symptoms after breast cancer diagnosis and treatment: A retrospective cohort study. Eur. J. Cancer 2018, 101, 1–11. [Google Scholar] [CrossRef]
- De Groef, A.; Van Kampen, M.; Tieto, E.; Schönweger, P.; Christiaens, M.R.; Neven, P.; Geraerts, I.; Gebruers, N.; Devoogdt, N. Arm lymphoedema and upper limb impairments in sentinel node-negative breast cancer patients: A one year follow-up study. Breast 2016, 29, 102–108. [Google Scholar] [CrossRef] [PubMed]
- De Mello, M.R.S.P.; Moura, S.F.; Muzi, C.D.; Guimarães, R.M. Clinical evaluation and pattern of symptoms in colorectal cancer patients. Arq. Gastroenterol. 2020, 57, 131–136. [Google Scholar] [CrossRef] [PubMed]
- De Oliveira, G.S., Jr.; Chang, R.; Khan, S.A.; Hansen, N.M.; Khan, J.H.; McCarthy, R.J.; Apkarian, A.V. Factors associated with the development of chronic pain after surgery for breast cancer: A prospective cohort from a tertiary center in the United States. Breast J. 2014, 20, 9–14. [Google Scholar] [CrossRef] [PubMed]
- Deshields, T.L.; Potter, P.; Olsen, S.; Liu, J. The persistence of symptom burden: Symptom experience and quality of life of cancer patients across one year. Support. Care Cancer 2014, 22, 1089–1096. [Google Scholar] [CrossRef] [PubMed]
- Deshields, T.L.; Penalba, V.; Liu, J.; Avery, J. Comparing the symptom experience of cancer patients and non-cancer patients. Support. Care Cancer 2017, 25, 1103–1109. [Google Scholar] [CrossRef]
- Dhingra, L.K.; Lam, K.; Cheung, W.; Shao, T.; Li, Z.; Van de Maele, S.; Chang, V.T.; Chen, J.; Ye, H.; Wong, R.; et al. Variation in symptom distress in underserved Chinese American cancer patients. Cancer 2015, 121, 3352–3359. [Google Scholar] [CrossRef] [PubMed]
- Donovan, K.A.; Boyington, A.R.; Judson, P.L.; Wyman, J.F. Bladder and bowel symptoms in cervical and endometrial cancer survivors. Psychooncology 2014, 23, 672–678. [Google Scholar] [CrossRef]
- Doubova, S.V.; Pérez-Cuevas, R. Association of supportive care needs and quality of patient-centered cancer care with depression in women with breast and cervical cancer in Mexico. Psychooncology 2021, 30, 591–601. [Google Scholar] [CrossRef]
- Feiten, S.; Dünnebacke, J.; Heymanns, J.; Köppler, H.; Thomalla, J.; van Roye, C.; Wey, D.; Weide, R. Breast cancer morbidity: Questionnaire survey of patients on the long term effects of disease and adjuvant therapy. Dtsch. Ärztebl. Int. 2014, 111, 537–544. [Google Scholar]
- Fokdal, L.; Pötter, R.; Kirchheiner, K.; Lindegaard, J.C.; Jensen, N.B.K.; Kirisits, C.; Chargari, C.; Mahantshetty, U.; Jürgenliemk-Schulz, I.M.; Segedin, B.; et al. Physician assessed and patient reported urinary morbidity after radio-chemotherapy and image guided adaptive brachytherapy for locally advanced cervical cancer. Radiother. Oncol. 2018, 127, 423–430. [Google Scholar] [CrossRef] [PubMed]
- Giuliani, M.E.; Milne, R.A.; Puts, M.; Sampson, L.R.; Kwan, J.Y.Y.; Le, L.W.; Alibhai, S.M.H.; Howell, D.; Abdelmutti, N.; Liu, G.; et al. The prevalence and nature of supportive care needs in lung cancer patients. Curr. Oncol. 2016, 23, 258–265. [Google Scholar] [CrossRef] [PubMed]
- Götze, H.; Köhler, N.; Taubenheim, S.; Lordick, F.; Mehnert, A. Polypharmacy, limited activity, fatigue and insomnia are the most frequent symptoms and impairments in older hematological cancer survivors (70+): Findings from a register-based study on physical and mental health. J. Geriatr. Oncol. 2019, 10, 55–59. [Google Scholar] [CrossRef] [PubMed]
- Gough, N.; Koffman, J.; Ross, J.R.; Riley, J.; Judson, I. Symptom Burden in Advanced Soft-Tissue Sarcoma. J. Pain Symptom Manag. 2017, 53, 588–597. [Google Scholar] [CrossRef]
- Guedes, T.S.R.; Dantas de Oliveira, N.P.; Holanda, A.M.; Reis, M.A.; Silva, C.P.; Rocha e Silva, B.L.; Cancela, M.C.; de Souza, D.L.B. Body Image of Women Submitted to Breast Cancer Treatment. Asian Pac. J. Cancer Prev. 2018, 19, 1487–1493. [Google Scholar] [PubMed]
- Honkanen, N.; Mustonen, L.; Kalso, E.; Meretoja, T.; Harno, H. Breast reconstruction after breast cancer surgery—Persistent pain and quality of life 1–8 years after breast reconstruction. Scand. J. Pain 2021, 21, 522–529. [Google Scholar] [CrossRef] [PubMed]
- Horick, N.K.; Muzikansky, A.; Gutierrez, H.L.; Boyd, K.L.; Finkelstein, D.M. Physical symptoms in long-term survivors of rare cancer. J. Cancer Surviv. 2018, 12, 835–842. [Google Scholar] [CrossRef]
- Huang, W.; Yang, J.; Liu, Y.; Liu, C.; Zhang, X.; Fu, W.; Shi, L.; Liu, G. Assessing health-related quality of life of patients with colorectal cancer using EQ-5D-5L: A cross-sectional study in Heilongjiang of China. BMJ Open 2018, 8, e022711. [Google Scholar] [CrossRef]
- Hunnicutt, J.N.; Tjia, J.; Lapane, K.L. Hospice Use and Pain Management in Elderly Nursing Home Residents with Cancer. J. Pain Symptom Manag. 2017, 53, 561–570. [Google Scholar] [CrossRef]
- Jesdale, B.M.; Mack, D.S.; Forrester, S.N.; Lapane, K.L. Cancer Pain in Relation to Metropolitan Area Segregation and Nursing Home Racial and Ethnic Composition. J. Am. Med. Dir. Assoc. 2020, 21, 1302–1308.e7. [Google Scholar] [CrossRef]
- Jewett, P.I.; Teoh, D.; Petzel, S.; Lee, H.; Messelt, A.; Kendall, J.; Hatsukami, D.; Everson-Rose, S.A.; Blaes, A.H.; Vogel, R.I. Cancer-Related Distress: Revisiting the Utility of the National Comprehensive Cancer Network Distress Thermometer Problem List in Women with Gynecologic Cancers. JCO Oncol. Pract. 2020, 16, e649–e659. [Google Scholar] [CrossRef]
- Karawekpanyawong, N.; Kaewkitikul, K.; Maneeton, B.; Maneeton, N.; Siriaree, S. The prevalence of depressive disorder and its association in Thai cervical cancer patients. PLoS ONE 2021, 16, e0252779. [Google Scholar] [CrossRef]
- Khan, S.Z.; Nofil, S.; Arif, A.; Jan, M.M.I.R.; Riaz, B.; Sherwani, N.Z.F.K. Frequency and Risk Factors for Post Mastectomy Pain Syndrome [PMPS] in Female Breast Cancer patients. Pak. J. Med. Health Sci. 2021, 15, 2530–2533. [Google Scholar]
- Kim, S.H.; Jo, M.W.; Lee, J.W.; Lee, H.J.; Kim, J.K. Validity and reliability of EQ-5D-3L for breast cancer patients in Korea. Health Qual. Life Outcomes 2015, 13, 203. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.R.; Shin, Y.S.; Kim, J.H.; Choi, M.; Yoo, S.H. Differences in Type Composition of Symptom Clusters as Predictors of Quality of Life in Patients with Meningioma and Glioma. World Neurosurg. 2017, 98, 50–59. [Google Scholar] [CrossRef] [PubMed]
- Lefkowits, C.; Rabow, W.M.; Sherman, A.E.; Kiet, T.K.; Ruskin, R.; Chan, J.K.; Chen, L.M. Predictors of high symptom burden in gynecologic oncology outpatients: Who should be referred to outpatient palliative care? Gynecol. Oncol. 2014, 132, 698–702. [Google Scholar] [CrossRef]
- Liu, S.; Sun, Y.; Louie, W. Symptom Distress and Its Association with Traditional Chinese Medicine Use in Chinese American Women with Cancer. Oncol. Nurs. Forum 2015, 42, e24–e32. [Google Scholar] [CrossRef]
- Loh, K.P.; Zittel, J.; Kadambi, S.; Pandya, C.; Xu, H.; Flannery, M.; Magnuson, A.; Bautista, J.; McHugh, C.; Mustian, K.; et al. Elucidating the associations between sleep disturbance and depression, fatigue, and pain in older adults with cancer. J. Geriatr. Oncol. 2018, 9, 464–468. [Google Scholar] [CrossRef]
- Lu, F.; Song, L.; Xie, T.; Tian, J.; Fan, Y.; Liu, H. Current Status of Malignant Neuropathic Pain in Chinese Patients with Cancer: Report of a Hospital-based Investigation of Prevalence, Etiology, Assessment, and Treatment. Pain Pract. 2017, 17, 88–98. [Google Scholar] [CrossRef]
- Mavros, M.N.; Davis, L.E.; Hallet, J.; Tung, S.; Mahar, A.L.; Bubis, L.D.; Hammad, A.; Zhao, H.; Earle, C.C.; Barbera, L.; et al. Symptom Burden of Nonresected Pancreatic Adenocarcinoma: An Analysis of 10,753 Patient-Reported Outcome Assessments. Pancreas 2020, 49, 1083–1089. [Google Scholar] [CrossRef]
- Mejdahl, M.K.; Mertz, B.G.; Bidstrup, P.E.; Andersen, K.G. Preoperative distress predicts persistent pain after breast cancer treatment: A prospective cohort study. J. Natl. Compr. Cancer Netw. 2015, 13, 995–1003. [Google Scholar] [CrossRef]
- Nakanotani, T.; Akechi, T.; Takayama, T.; Karato, A.; Kikuuchi, Y.; Okamoto, N.; Katayama, K.; Yokoo, M.; Ogawa, A. Characteristics of elderly cancer patients’ concerns and their quality of life in Japan: A Web-based survey. Jpn J. Clin. Oncol. 2014, 44, 448–455. [Google Scholar] [CrossRef]
- Nappi, R.E.; Palacios, S.; Bruyniks, N.; Particco, M.; Panay, N. The European Vulvovaginal Epidemiological Survey (EVES). Impact of history of breast cancer on prevalence, symptoms, sexual function and quality of life related to vulvovaginal atrophy. Gynecol. Endocrinol. 2021, 37, 78–82. [Google Scholar] [CrossRef]
- Oosterling, A.; te Boveldt, N.; Verhagen, C.; van der Graaf, W.T.; Van Ham, M.; Van der Drift, M.; Vissers, K.; Engels, Y. Neuropathic Pain Components in Patients with Cancer: Prevalence, Treatment, and Interference with Daily Activities. Pain Pract. 2016, 16, 413–421. [Google Scholar] [CrossRef]
- Pandya, C.; Magnuson, A.; Flannery, M.; Zittel, J.; Duberstein, P.; Loh, K.P.; Ramsdale, E.; Gilmore, N.; Dale, W.; Mohile, S.G. Association Between Symptom Burden and Physical Function in Older Patients with Cancer. J. Am. Geriatr. Soc. 2019, 67, 998–1004. [Google Scholar] [CrossRef]
- Pinto, E.; Gonçalves, F.; Sacarlal, J.; Castro, L.; Rego, G. Pain management in cancer patients in the main hospitals in Mozambique. Ann. Palliat. Med. 2021, 10, 4069–4079. [Google Scholar] [CrossRef]
- Ramsenthaler, C.; Osborne, T.R.; Wei, G.; Siegert, R.J.; Edmonds, P.M.; Schey, S.A.; Higginson, I.J.; Gao, W. The impact of disease-related symptoms and palliative care concerns on health-related quality of life in multiple myeloma: A multi-centre study. BMC Cancer 2016, 16, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Rau, K.M.; Chen, J.S.; Wu, H.B.; Lin, S.F.; Lai, M.K.; Chow, J.M.; Huang, M.L.; Wang, C.J.; Tai, C.J.; Hwang, W.L.; et al. The impact of pain control on physical and psychiatric functions of cancer patients: A nation-wide survey in Taiwan. Jpn J. Clin. Oncol. 2015, 45, 1042–1049. [Google Scholar] [CrossRef] [PubMed]
- Reuter, Q.; Marshall, A.; Zaidi, H.; Sista, P.; Powell, E.S.; McCarthy, D.M.; Dresden, S.M. Emergency Department-Based Palliative Interventions: A Novel Approach to Palliative Care in the Emergency Department. J. Palliat. Med. 2019, 22, 649–655. [Google Scholar] [CrossRef] [PubMed]
- Rosario, C.O.; Puts, M.; Jang, R.; Bezjak, A.; Yokom, D.; Alibhai, S.M.H. Exploring the geriatric needs of oncology inpatients at an academic cancer centre. J. Geriatr. Oncol. 2019, 10, 824–828. [Google Scholar] [CrossRef]
- Saarelainen, L.K.; Turner, J.P.; Shakib, S.; Singhal, N.; Hogan-Doran, J.; Prowse, R.; Johns, S.; Lees, J.; Bell, J.S. Potentially inappropriate medication use in older people with cancer: Prevalence and correlates. J. Geriatr. Oncol. 2014, 5, 439–446. [Google Scholar] [CrossRef] [PubMed]
- Sager, Z.S.; Wachen, J.S.; Naik, A.D.; Moye, J. Post-Traumatic Stress Disorder Symptoms from Multiple Stressors Predict Chronic Pain in Cancer Survivors. J. Palliat. Med. 2020, 23, 1191–1197. [Google Scholar] [CrossRef] [PubMed]
- Sakurai, H.; Miyashita, M.; Imai, K.; Miyamoto, S.; Otani, H.; Oishi, A.; Kizawa, Y.; Matsushima, E. Validation of the Integrated Palliative care Outcome Scale (IPOS)—Japanese Version. Jpn. J. Clin. Oncol. 2019, 49, 257–262. [Google Scholar] [CrossRef] [PubMed]
- Sampogna, F.; Abeni, D.; Gieler, U.; Tomas-Aragones, L.; Lien, L.; Poot, F.; Jemec, G.B.E.; Szabo, C.; Linder, D.; Van Middendorp, H.; et al. Exploring the EQ-5D dimension of pain/discomfort in dermatology outpatients from a multicentre study in 13 European countries. Acta Derm. Venereol. 2020, 100, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Sánchez Sánchez, E.; González Baena, A.C.; González Cáliz, C.; Caballero Paredes, F.; Moyano Calvo, J.L.; Castiñeiras Fernández, J. Prevalence of Anxiety and Depression in Prostate Cancer Patients and Their Spouses: An Unaddressed Reality. Prostate Cancer 2020, 2020, 4393175. [Google Scholar] [CrossRef] [PubMed]
- Schreiber, K.L.; Zinboonyahgoon, N.; Flowers, K.M.; Hruschak, V.; Fields, K.G.; Patton, M.E.; Schwartz, E.; Azizoddin, D.; Soens, M.; King, T.; et al. Prediction of Persistent Pain Severity and Impact 12 Months After Breast Surgery Using Comprehensive Preoperative Assessment of Biopsychosocial Pain Modulators. Ann. Surg. Oncol. 2021, 28, 5015–5038. [Google Scholar] [CrossRef]
- Shen, W.C.; Chen, J.S.; Shao, Y.Y.; Lee, K.D.; Chiou, T.J.; Sung, Y.C.; Rau, K.M.; Yen, C.J.; Liao, Y.M.; Liu, T.C.; et al. Impact of Undertreatment of Cancer Pain with Analgesic Drugs on Patient Outcomes: A Nationwide Survey of Outpatient Cancer Patient Care in Taiwan. J. Pain Symptom Manag. 2017, 54, 55–65.e1. [Google Scholar] [CrossRef]
- Sloan, J.A.; Cheville, A.L.; Liu, H.; Novotny, P.J.; Wampfler, J.A.; Garces, Y.I.; Clark, M.M.; Yang, P. Impact of self-reported physical activity and health promotion behaviors on lung cancer survivorship. Health Qual. Life Outcomes 2016, 14, 66. [Google Scholar] [CrossRef]
- Smith, T.G.; Troeschel, A.N.; Castro, K.M.; Arora, N.K.; Stein, K.; Lipscomb, J.; Brawley, O.W.; McCabe, R.M.; Clauser, S.B.; Ward, E. Perceptions of Patients with Breast and Colon Cancer of the Management of Cancer-Related Pain, Fatigue, and Emotional Distress in Community Oncology. J. Clin. Oncol. 2019, 37, 1666–1676. [Google Scholar] [CrossRef]
- Tadele, N. Evaluation of quality of life of adult cancer patients attending Tikur Anbessa specialized referral hospital, Addis Ababa Ethiopia. Ethiop. J. Health Sci. 2015, 25, 53–62. [Google Scholar] [CrossRef]
- Tegegn, H.G.; Gebreyohannes, E.A. Cancer Pain Management and Pain Interference with Daily Functioning among Cancer Patients in Gondar University Hospital. Pain Res. Manag. 2017, 2017, 5698640. [Google Scholar] [CrossRef]
- Tjong, M.C.; Doherty, M.; Tan, H.; Chan, W.C.; Zhao, H.; Hallet, J.; Darling, G.; Kidane, B.; Wright, F.C.; Mahar, A.; et al. Province-Wide Analysis of Patient-Reported Outcomes for Stage IV Non-Small Cell Lung Cancer. Oncologist 2021, 26, e1800–e1811. [Google Scholar] [CrossRef] [PubMed]
- Tung, S.; Coburn, N.G.; Davis, L.E.; Mahar, A.L.; Myrehaug, S.; Zhao, H.; Earle, C.C.; Nathens, A.; Hallet, J. Population-based study of the prevalence and management of self-reported high pain scores in patients with non-resected pancreatic adenocarcinoma. Br. J. Surg. 2019, 106, 1666–1675. [Google Scholar] [CrossRef] [PubMed]
- Valery, P.C.; Bernardes, C.M.; Beesley, V.; Hawkes, A.L.; Baade, P.; Garvey, G. Unmet supportive care needs of Australian Aboriginal and Torres Strait Islanders with cancer: A prospective, longitudinal study. Support. Care Cancer 2017, 25, 869–877. [Google Scholar] [CrossRef] [PubMed]
- Van Arsdale, A.; Rosenbaum, D.; Kaur, G.; Pinto, P.; Kuo, D.Y.S.; Barrera, R.; Goldberg, G.L.; Nevadunsky, N.S. Prevalence and factors associated with cognitive deficit in women with gynecologic malignancies. Gynecol. Oncol. 2016, 141, 323–328. [Google Scholar] [CrossRef]
- van den Brekel, L.; van der Baan, F.H.; Zweers, D.; Koldenhof, J.J.; Vos, J.B.H.; de Graeff, A.; Witteveen, P.O.; Teunissen, S.C.C.M. Predicting Anxiety in Hospitalized Cancer Patients. J. Pain Symptom Manag. 2020, 60, 522–530.e1. [Google Scholar] [CrossRef]
- Vistad, I.; Cvancarova, M.; Lindviksmoen Astrup, G.; Rustøen, T.; Liavaag, A.H. Symptom Experience and Self-rated Physical Functioning in Patients with Ovarian Cancer Receiving Chemotherapy: A Longitudinal Study. Int. J. Gynecol. Cancer 2018, 28, 1167–1175. [Google Scholar] [CrossRef]
- von Gruenigen, V.E.; Huang, H.Q.; Cella, D.; Zevon, M.; LaChance, J.A.; Walker, J.L.; Salani, R.; Modesitt, S.C.; Morris, R.T.; Bradley, W.H.; et al. Quality of life, symptoms and care needs in patients with persistent or recurrent platinum-resistant ovarian cancer: An NRG Oncology/Gynecologic Oncology Group study. Gynecol. Oncol. 2018, 150, 119–126. [Google Scholar] [CrossRef]
- Williams, G.R.; Al-Obaidi, M.; Dai, C.; Mir, N.; Challa, S.A.; Daniel, M.; Patel, H.; Barlow, B.; Young-Smith, C.; Gbolahan, O.; et al. Association of malnutrition with geriatric assessment impairments and health-related quality of life among older adults with gastrointestinal malignancies. Cancer 2020, 126, 5147–5155. [Google Scholar] [CrossRef]
- Xu, N.; Li, Z.; Wei, F.; Liu, X.; Jiang, L.; Meng, N.; Jiang, P.; Yu, M.; Wu, F.; Dang, L.; et al. A Cross-sectional Study on the Symptom Burden of Patients with Spinal Tumor: Validation of the Chinese Version of the M.D. Anderson Symptom Inventory—Spine Tumor Module. J. Pain Symptom Manag. 2017, 53, 605–613. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Shrestha, S.; Kc, B.; Blebil, A.Q.; Teoh, S.L. Pharmacist Involvement in Cancer Pain Management: A Systematic Review and Meta-Analysis. J. Pain 2022, 23, 1123–1142. [Google Scholar] [CrossRef] [PubMed]
- Jho, H.J.; Kim, Y.; Kong, K.A.; Kim, D.H.; Choi, J.Y.; Nam, E.J.; Choi, J.Y.; Koh, S.; Hwang, K.O.; Baek, S.K.; et al. Knowledge, practices, and perceived barriers regarding cancer pain management among physicians and nurses in Korea: A nationwide multicenter survey. PLoS ONE 2014, 9, e105900. [Google Scholar] [CrossRef] [PubMed]
- Silbermann, M.; Calimag, M.M.; Eisenberg, E.; Futerman, B.; Fernandez-Ortega, P.; Oliver, A.; Yaeger Monje, J.P.; Guo, P.; Charalambous, H.; Nestoros, S.; et al. Evaluating Pain Management Practices for Cancer Patients among Health Professionals: A Global Survey. J. Palliat. Med. 2022, 25, 1243–1248. [Google Scholar] [CrossRef] [PubMed]
- Bouya, S.; Balouchi, A.; Maleknejad, A.; Koochakzai, M.; AlKhasawneh, E.; Abdollahimohammad, A. Cancer Pain Management among Oncology Nurses: Knowledge, Attitude, Related Factors, and Clinical Recommendations: A Systematic Review. J. Cancer Educ. 2019, 34, 839–846. [Google Scholar] [CrossRef] [PubMed]
- Deandrea, S.; Montanari, M.; Moja, L.; Apolone, G. Prevalence of undertreatment in cancer pain. A review of published literature. Ann. Oncol. 2008, 19, 1985–1991. [Google Scholar] [CrossRef]
- Greco, M.T.; Roberto, A.; Corli, O.; Deandrea, S.; Bandieri, E.; Cavuto, S.; Apolone, G. Quality of cancer pain management: An update of a systematic review of undertreatment of patients with cancer. J. Clin. Oncol. 2014, 32, 4149–4154. [Google Scholar] [CrossRef]
- Roberto, A.; Greco, M.T.; Uggeri, S.; Cavuto, S.; Deandrea, S.; Corli, O.; Apolone, G. Living systematic review to assess the analgesic undertreatment in cancer patients. Pain Pract. 2022, 22, 487–496. [Google Scholar] [CrossRef]
- Mielgo-Rubio, X.; Uribelarrea, E.A.; Cortés, L.Q.; Moyano, M.S. Immunotherapy in non-small cell lung cancer: Update and new insights. J. Clin. Transl. Res. 2021, 7, 1–21. [Google Scholar]
- Valkema, M.J.; Mostert, B.; Lagarde, S.M.; Wijnhoven, B.P.L.; van Lanschot, J.J.B. The effectivity of targeted therapy and immunotherapy in patients with advanced metastatic and non-metastatic cancer of the esophagus and esophago-gastric junction. Updates Surg. 2022. [Google Scholar] [CrossRef]
- Zhou, X.; Qiao, G.; Ren, J.; Wang, X.; Wang, S.; Zhu, S.; Yuan, Y.; Morse, M.A.; Hobeika, A.; Lyerly, H.K. Adoptive immunotherapy with autologous T-cell infusions reduces opioid requirements in advanced cancer patients. Pain 2020, 161, 127–134. [Google Scholar] [CrossRef]
- Abbas, N.T.; Sheikha, A.; Mjali, A. Clinical outcomes of patients with plasma cell neoplasm in sulaymaniyah province of Iraq. Syst. Rev. Pharm. 2020, 11, 1142–1144. [Google Scholar]
- Alkhayyat, M.; Saleh, M.A.; Coronado, W.; Abureesh, M.; Zmaili, M.; Qapaja, T.; Almomani, A.; Khoudari, G.; Mansoor, E.; Cooper, G. Epidemiology of neuroendocrine tumors of the appendix in the USA: A population-based national study (2014–2019). Ann. Gastroenterol. 2021, 34, 713–720. [Google Scholar] [CrossRef]
- Baburao, A.; Narayanswamy, H. Clinico-Pathological Profile and Haematological Abnormalities Associated with Lung Cancer in Bangalore, India. Asian Pac. J. Cancer Prev. 2015, 16, 8235–8238. [Google Scholar] [CrossRef] [PubMed]
- Bassey, G.O.; Osunde, O.D.; Anyanechi, C.E. Maxillofacial tumors and tumor-like lesions in a Nigerian teaching hospital: An eleven year retrospective analysis. Afr. Health Sci. 2014, 14, 56–63. [Google Scholar] [CrossRef] [PubMed]
- Comelli, I.; Lippi, G.; Campana, V.; Servadei, F.; Cervellin, G. Clinical presentation and epidemiology of brain tumors firstly diagnosed in adults in the Emergency Department: A 10-year, single center retrospective study. Ann. Transl. Med. 2017, 5, 269. [Google Scholar] [CrossRef] [PubMed]
- Dai, J.; Liao, N.; Shi, J.; Tao, J.Q. Study of prevalence and influencing factors of depression in tumor patients and the therapeutic effects of fluoxetine. Eur. Rev. Med. Pharmacol. Sci. 2017, 21, 4966–4974. [Google Scholar]
- de Carvalho, W.R.S.; de Souza, L.L.; Pontes, F.S.C.; Uchôa, D.C.C.; Corrêa, D.L.; de Cáceres, C.V.B.L.; Lopes, M.A.; Santos-Silva, A.R.; Vargas, P.A.; de Andrade, B.A.B.; et al. A multicenter study of oral sarcomas in Brazil. Oral Dis. 2020, 26, 43–52. [Google Scholar] [CrossRef] [PubMed]
- Du Plessis, D.E.; Van Deventer, H.; Fernandez, P.; Van Der Merwe, A. A prospective observational study of the epidemiology and pathological profile of RCC in a South African referral centre. Afr. J. Urol. 2020, 26, 15. [Google Scholar] [CrossRef]
- Glover, M.; Mansoor, E.; Panhwar, M.; Parasa, S.; Cooper, G.S. Epidemiology of Colorectal Cancer in Average Risk Adults 20–39 Years of Age: A Population-Based National Study. Dig. Dis. Sci. 2019, 64, 3602–3609. [Google Scholar] [CrossRef]
- Hanna, E.Y.; Mendoza, T.R.; Rosenthal, D.I.; Gunn, G.B.; Sehra, P.; Yucel, E.; Cleeland, C.S. The symptom burden of treatment-naive patients with head and neck cancer. Cancer 2015, 121, 766–773. [Google Scholar] [CrossRef] [PubMed]
- Hlapane, R.S.; Khumalo, T.L.; Makhathini, B.S.; Moodley, J. Impact of a delayed diagnosis of vulvar cancer and its association with HIV infection: A 4-year review at a tertiary hospital in KwaZulu-Natal, South Africa. S. Afr. J. HIV Med. 2021, 22, 1272. [Google Scholar] [CrossRef] [PubMed]
- Hu, X.L.; Xu, S.T.; Wang, X.C.; Hou, D.N.; Chen, C.C.; Song, Y.L.; Yang, D. Prevalence of and risk factors for presenting initial respiratory symptoms in patients undergoing surgery for lung cancer. J. Cancer 2018, 9, 3515–3521. [Google Scholar] [CrossRef] [PubMed]
- Iglesias, P.; Nocete, I.; Moure Rodríguez, M.D.; Venegas-Moreno, E.; Ares, J.; Biagetti, B.; Rodríguez Berrocal, V.; Guerrero-Pérez, F.; Vicente, A.; Villar-Taibo, R.; et al. Craniopharyngioma in the Elderly: A Multicenter and Nationwide Study in Spain. Neuroendocrinology 2021, 111, 925–936. [Google Scholar] [CrossRef]
- Khawaja, S.N.; Jamshed, A.; Hussain, R.T. Prevalence of pain in oral cancer: A retrospective study. Oral Dis. 2021, 27, 1806–1812. [Google Scholar] [CrossRef]
- Kkrishnappa, P.; Loh, E.J.; Mohamad, I.B.; Tata, M.D.; Akhilesh, M.; Palayan, K. Histomorphology and Immunohistochemistry of Gastrointestinal Stromal Tumors in a Malaysian Population. Asian Pac. J. Cancer Prev. 2016, 17, 2795–2799. [Google Scholar] [PubMed]
- Kono, Y.; Kanzaki, H.; Tsuzuki, T.; Takatani, M.; Nasu, J.; Kawai, D.; Takenaka, R.; Tanaka, T.; Iwamuro, M.; Kawano, S.; et al. A multicenter observational study on the clinicopathological features of gastric cancer in young patients. J. Gastroenterol. 2019, 54, 419–426. [Google Scholar] [CrossRef]
- Kuguyo, O.; Misi, F.D.; Chibonda, S.; Matimba, A.; Nhachi, C.; Tsikai, N. Pain management strategies among cervical cancer patients in Zimbabwe. Pain Manag. 2021, 11, 715–729. [Google Scholar] [CrossRef]
- Kurnatowski, P.; Moqbil, S.; Kaczmarczyk, D. Signs, symptoms and the prevalence of fungi detected from the oral cavity and pharynx of radiotherapy subjects with head and neck tumors, and their susceptibility to chemotherapeutics. Ann. Parasitol. 2014, 60, 207–213. [Google Scholar]
- Lal, P.; Saleh, M.A.; Khoudari, G.; Gad, M.M.; Mansoor, E.; Isenberg, G.; Cooper, G.S. Epidemiology of Large Bowel Carcinoid Tumors in the USA: A Population-Based National Study. Dig. Dis. Sci. 2020, 65, 269–275. [Google Scholar] [CrossRef]
- Marchegiani, G.; Andrianello, S.; Miatello, C.; Pollini, T.; Secchettin, E.; Tedesco, G.; D’Onofrio, M.; Malleo, G.; Bassi, C.; Salvia, R. The Actual Prevalence of Symptoms in Pancreatic Cystic Neoplasms: A Prospective Propensity Matched Cohort Analysis. Dig. Surg. 2019, 36, 522–529. [Google Scholar] [CrossRef]
- Mohme, M.; Mende, K.C.; Krätzig, T.; Plaetke, R.; Beseoglu, K.; Hagedorn, J.; Steiger, H.J.; Floeth, F.W.; Eicker, S.O. Impact of spinal cord compression from intradural and epidural spinal tumors on perioperative symptoms—Implications for surgical decision making. Neurosurg. Rev. 2017, 40, 377–387. [Google Scholar] [CrossRef] [PubMed]
- Paganini Piazzolla, L.; Medeiros De Almeida, R.; Nóbrega Dos Santos, A.C.; Gonçalves De Oliveira, P.; Freitas Da Silva, E.; Batista De Sousa, J. Does aging influence clinical presentation and pathological staging in colorectal cancer? Eur. Geriatr. Med. 2015, 6, 433–436. [Google Scholar] [CrossRef]
- Pakish, J.B.; Lu, K.H.; Sun, C.C.; Burzawa, J.K.; Greisinger, A.; Smith, F.A.; Fellman, B.; Urbauer, D.L.; Soliman, P.T. Endometrial Cancer Associated Symptoms: A Case-Control Study. J. Womens Health 2016, 25, 1187–1192. [Google Scholar] [CrossRef] [PubMed]
- Philip, E.J.; Bergerot, C.D.; Clark, K.; Bergerot, P.; Loscalzo, M. Obesity and psychosocial well-being among cancer patients and survivors. Psychooncology 2019, 28, 2141–2148. [Google Scholar] [CrossRef] [PubMed]
- Poursadegh, M.; Poursadegh, F.; Esmaeili, M.; Bakhshaee, M. Epidemiological survey of sinonasal malignancy in North-East Iran. Iran. J. Otorhinolaryngol. 2015, 27, 225–229. [Google Scholar]
- Rudd, P.; Gorman, D.; Meja, S.; Mtonga, P.; Jere, Y.; Chidothe, I.; Msusa, A.T.; Bates, M.J.; Brown, E.; Masamba, L. Cervical cancer in southern Malawi: A prospective analysis of presentation, management, and outcomes. Malawi Med. J. 2017, 29, 124–129. [Google Scholar] [CrossRef][Green Version]
- Shen, C.; Dasari, A.; Xu, Y.; Zhou, S.; Gu, D.; Chu, Y.; Halperin, D.M.; Shih, Y.T.; Yao, J.C. Pre-existing Symptoms and Healthcare Utilization Prior to Diagnosis of Neuroendocrine Tumors: A SEER-Medicare Database Study. Sci. Rep. 2018, 8, 16863. [Google Scholar] [CrossRef]
- Antony, A.; Joel, J.J.; Shetty, J.; Umar, N.F. Identification and analysis of adverse drug reactions associated with cancer chemotherapy in hospitalized patients. Int. J. Pharm. Pharm. Sci. 2016, 8, 448–451. [Google Scholar]
- Berger, A.; Kumar, G.; LeVan, T.; Meza, J. Symptom Clusters And Quality Of Life Over 1 Year In Breast Cancer Patients Receiving Adjuvant Chemotherapy. Asia Pac. J. Oncol. Nurs. 2020, 7, 134–140. [Google Scholar] [CrossRef]
- Bianchini, C.; Malagò, M.; Crema, L.; Aimoni, C.; Matarazzo, T.; Bortolazzi, S.; Ciorba, A.; Pelucchi, S.; Pastore, A. Post-operative pain management in head and neck cancer patients: Predictive factors and efficacy of therapy. Acta Otorhinolaryngol. Ital. 2016, 36, 91–96. [Google Scholar] [CrossRef]
- Dervis, E.; Ayer, M.; Belli, A.A.; Barut, S.G. Cutaneous adverse reactions of imatinib therapy in patients with chronic myeloid leukemia: A six-year follow up. Eur. J. Dermatol. 2016, 26, 133–137. [Google Scholar] [CrossRef] [PubMed]
- Fatiregun, O.; Sowunmi, A.C.; Habeebu, M.; Okediji, P.; Alabi, A.; Fatiregun, O.; Adeniji, A.; Awofeso, O.; Adegboyega, B. Prevalence and Correlates of Unmet Supportive Needs of Nigerian Patients with Cancer. J. Glob. Oncol. 2019, 5, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Frowen, J.; Hughes, R.; Skeat, J. The prevalence of patient-reported dysphagia and oral complications in cancer patients. Support. Care Cancer 2020, 28, 1141–1150. [Google Scholar] [CrossRef] [PubMed]
- Germano, F.; Melone, P.; Testi, D.; Arcuri, L.; Marmiroli, L.; Petrone, A.; Arcuri, C. Oral complications of head and neck radiotherapy: Prevalence and management. Minerva Stomatol. 2015, 64, 189–202. [Google Scholar]
- Kartin, P.T.; Tasci, S.; Soyuer, S.; Elmali, F. Effect of an oral mucositis protocol on quality of life of patients with head and neck cancer treated with radiation therapy. Clin. J. Oncol. Nurs. 2014, 18, e118–e125. [Google Scholar] [CrossRef]
- Rahnama, M.; Madej-Czerwonka, B.; Jastrzębska-Jamrogiewicz, I.; Jamrogiewicz, R. Analysis of the influence of parenteral cancer chemotherapy on the health condition of oral mucosa. Contemp. Oncol. 2015, 19, 77–82. [Google Scholar] [CrossRef]
- Sahora, K.; Crippa, S.; Zamboni, G.; Ferrone, C.; Warshaw, A.L.; Lillemoe, K.; Mino-Kenudson, M.; Falconi, M.; Fernandez-del Castillo, C. Intraductal papillary mucinous neoplasms of the pancreas with concurrent pancreatic and periampullary neoplasms. Eur. J. Surg. Oncol. 2016, 42, 197–204. [Google Scholar] [CrossRef]
- Takayama, Y.; Kaneoka, Y.; Maeda, A.; Takahashi, T.; Kiriyama, M.; Seita, K. Assessment of perioperative symptoms of patients with gastric cancer using the edmonton symptom assessment system revised japanese version (Esas-r-j). J. Med. Investig. 2021, 68, 90–95. [Google Scholar] [CrossRef]
- Wagland, R.; Richardson, A.; Ewings, S.; Armes, J.; Lennan, E.; Hankins, M.; Griffiths, P. Prevalence of cancer chemotherapy-related problems, their relation to health-related quality of life and associated supportive care: A cross-sectional survey. Support. Care Cancer 2016, 24, 4901–4911. [Google Scholar] [CrossRef]
- Wang, Y.; Lu, Q.; Zhang, L.; Zhuang, B.; Zhang, T.; Jin, S.; Sun, Y.; Xiao, S.; Zheng, B.; Fang, Y.; et al. Nutrition Impact Symptom Clusters in Patients with Head and Neck Cancer Receiving Concurrent Chemoradiotherapy. J. Pain Symptom Manag. 2021, 62, 277–285. [Google Scholar] [CrossRef]
- Yanque, O. Uterine leiomyosarcoma: A 10-year review in a referral hospital in Peru, 2005–2014. S. Afr. J. Obstet. Gynaecol. 2018, 24, 87–89. [Google Scholar] [CrossRef]
- Ahmadi, Z.; Wysham, N.G.; Lundström, S.; Janson, C.; Currow, D.C.; Ekström, M. End-of-life care in oxygen-dependent ILD compared with lung cancer: A national population-based study. Thorax 2016, 71, 510–516. [Google Scholar] [CrossRef]
- Alsirafy, S.A.; Abd El-Aal, H.H.; Farag, D.E.; Radwan, R.H.; El-Sherief, W.A.; Fawzy, R. High Symptom Burden among Patients with Newly Diagnosed Incurable Cancer in a Developing Country. J. Pain. Symptom Manag. 2016, 51, e1–e5. [Google Scholar] [CrossRef]
- Bischoff, K.E.; O’Riordan, D.L.; Fazzalaro, K.; Kinderman, A.; Pantilat, S.Z. Identifying Opportunities to Improve Pain among Patients with Serious Illness. J. Pain Symptom Manag. 2018, 55, 881–889. [Google Scholar] [CrossRef] [PubMed]
- Cuyun Carter, G.; Kaltenboeck, A.; Ivanova, J.; Liepa, A.M.; San Roman, A.; Koh, M.; Rajan, N.; Cheng, R.; Birnbaum, H.; Chen, J.S. Treatment patterns in patients with advanced gastric cancer in Taiwan. Asia Pac. J. Clin. Oncol. 2017, 13, 185–194. [Google Scholar] [CrossRef]
- Eriksson, H.; Milberg, A.; Hjelm, K.; Friedrichsen, M. End of Life Care for Patients Dying of Stroke: A Comparative Registry Study of Stroke and Cancer. PLoS ONE 2016, 11, e0147694. [Google Scholar] [CrossRef]
- Family, L.; Xu, H.; Cannavale, K.; Mehta, B.; Pourmoussa, A.; Xu, L.; Chao, C. Symptom burdens related to chemotherapy-induced anemia in stage IV cancer. J. Community Support. Oncol. 2018, 16, e260–e271. [Google Scholar] [CrossRef]
- Hasegawa, T.; Goto, N.; Matsumoto, N.; Sasaki, Y.; Ishiguro, T.; Kuzuya, N.; Sugiyama, Y. Prevalence of unmet needs and correlated factors in advanced-stage cancer patients receiving rehabilitation. Support. Care Cancer 2016, 24, 4761–4767. [Google Scholar] [CrossRef]
- Langlais, B.T.; Geyer, H.; Scherber, R.; Mesa, R.A.; Dueck, A.C. Quality of life and symptom burden among myeloproliferative neoplasm patients: Do symptoms impact quality of life? Leuk. Lymphoma 2019, 60, 402–408. [Google Scholar] [CrossRef]
- Nnonyelum, O.N.; Anazoeze, M.J.; Eunice, N.O.; Emmanuel, O.O.; Stella, A.T.; Marcus, A.I.; Taiwo, B.M.; Olufela, K.O.; Chinawaeze, A.J.; Orkuma, J.A.; et al. Multiple myeloma in Nigeria: A multi-centre epidemiological and biomedical study. Pan Afr. Med. J. 2015, 22, 292. [Google Scholar] [CrossRef]
- Pimentel, L.E.; Yennurajalingam, S.; Chisholm, G.; Edwards, T.; Guerra-Sanchez, M.; De La Cruz, M.; Tanco, K.; Vidal, M.; Bruera, E. The frequency and factors associated with the use of a dedicated Supportive Care Center Telephone Triaging Program in patients with advanced cancer at a comprehensive cancer center. J. Pain Symptom Manag. 2015, 49, 939–944. [Google Scholar] [CrossRef] [PubMed]
- Richter, J.; Sanchez, L.; Biran, N.; Wang, C.K.; Tanenbaum, K.; DeVincenzo, V.; Grunman, B.; Vesole, D.H.; Siegel, D.S.; Pecora, A.; et al. Prevalence and Survival Impact of Self-Reported Symptom and Psychological Distress among Patients with Multiple Myeloma. Clin. Lymphoma Myeloma Leuk. 2021, 21, e284–e289. [Google Scholar] [CrossRef] [PubMed]
- Sandgren, A.; Strang, P. Palliative care needs in hospitalized cancer patients: A 5-year follow-up study. Support. Care Cancer 2018, 26, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Scharf, M.; Petry, V.; Daniel, H.; Rinke, A.; Gress, T.M. Bone Metastases in Patients with Neuroendocrine Neoplasm: Frequency and Clinical, Therapeutic, and Prognostic Relevance. Neuroendocrinology 2018, 106, 30–37. [Google Scholar] [CrossRef]
- Spence, W.; Ghosh, S.; Palen, M.; Liska, A.; Ha, V.; Wong, R.; Huang, F. Symptom burden among Northern Alberta radiotherapy patients with advanced cancer: Mapping needs and gaps. Support. Care Cancer 2020, 28, 4963–4969. [Google Scholar] [CrossRef]
- Unseld, M.; Fischöder, S.; Jachs, M.; Drimmel, M.; Siebenhüner, A.; Bianconi, D.; Kieler, M.; Puhr, H.; Minichsdorfer, C.; Winder, T.; et al. Different toxicity profiles predict third line treatment efficacy in metastatic colorectal cancer patients. J. Clin. Med. 2020, 9, 1772. [Google Scholar] [CrossRef]
- Wangnamthip, S.; Euasobhon, P.; Siriussawakul, A.; Jirachaipitak, S.; Laurujisawat, J.; Vimolwattanasarn, K. Effective Pain Management for Inpatients at Siriraj Hospital: A Retrospective Study. J. Med. Assoc. Thai. 2016, 99, 565–571. [Google Scholar]
- Yanamandra, U.; Saini, N.; Chauhan, P.; Sharma, T.; Khadwal, A.; Prakash, G.; Varma, N.; Lad, D.; Varma, S.; Malhotra, P. AYA-Myeloma: Real-World, Single-Center Experience Over Last 5 Years. J. Adolesc. Young Adult Oncol. 2018, 7, 120–124. [Google Scholar] [CrossRef]
- Yi, Y.S.; Ban, W.H.; Sohng, K.Y. Effect of COPD on symptoms, quality of life and prognosis in patients with advanced non-small cell lung cancer. BMC Cancer 2018, 18, 1053. [Google Scholar] [CrossRef]
- Abid, H.; Kober, K.M.; Smoot, B.; Paul, S.M.; Hammer, M.; Levine, J.D.; Lee, K.; Wright, F.; Cooper, B.A.; Conley, Y.P.; et al. Common and Distinct Characteristics Associated with Trajectories of Morning and Evening Energy in Oncology Patients Receiving Chemotherapy. J. Pain Symptom Manag. 2017, 53, 887–900.e2. [Google Scholar] [CrossRef]
- Agyemang-Yeboah, F.; Yorke, J.; Obirikorang, C.; Batu, E.N.; Acheampong, E.; Frempong, E.A.; Anto, E.O.; Amankwaa, B. Patterns and presentations of colorectal cancer at Komfo-Anokye teaching hospital Kumasi, Ghana. Pan Afr. Med. J. 2017, 28, 121. [Google Scholar] [PubMed]
- Allgar, V.L.; Chen, H.; Richfield, E.; Currow, D.; Macleod, U.; Johnson, M.J. Psychometric Properties of the Needs Assessment Tool-Progressive Disease Cancer in U.K. Primary Care. J. Pain Symptom Manag. 2018, 56, 602–612. [Google Scholar] [CrossRef]
- Alsughayer, L.Y.; Altamimi, L.A.; Alsaleh, F.S.; Alsaghan, L.; Alfurayh, I.; Abdel-Aziz, N.M.; Alsaleh, K.A.; Alosaimi, F.D. Prevalence and determinants of distress among oncology patients at a tertiary care medical city in Riyadh, Saudi Arabia. Saudi Med. J. 2021, 42, 761–768. [Google Scholar] [CrossRef]
- Bell, S.G.; Dalton, L.; McNeish, B.L.; Fang, F.; Henry, N.L.; Kidwell, K.M.; McLean, K. Aromatase inhibitor use, side effects and discontinuation rates in gynecologic oncology patients. Gynecol. Oncol. 2020, 159, 509–514. [Google Scholar] [CrossRef]
- Crossnohere, N.L.; Richardson, D.R.; Reinhart, C.; O’Donoghue, B.; Love, S.M.; Smith, B.D.; Bridges, J.F.P. Side effects from acute myeloid leukemia treatment: Results from a national survey. Curr. Med. Res. Opin. 2019, 35, 1965–1970. [Google Scholar] [CrossRef] [PubMed]
- Hirpara, D.H.; Gupta, V.; Davis, L.E.; Zhao, H.; Hallet, J.; Mahar, A.L.; Sutradhar, R.; Doherty, M.; Louie, A.V.; Kidane, B.; et al. Severe symptoms persist for Up to one year after diagnosis of stage I-III lung cancer: An analysis of province-wide patient reported outcomes. Lung Cancer 2020, 142, 80–89. [Google Scholar] [CrossRef]
- Jazieh, A.M.; AlSumai, T.S.; Ali, Y.Z.; Sheblaq, N.R.; Alkaiyat, M. The pattern of bone involvement, management, and outcomes in patients with nonsmall cell lung cancer: A retrospective study. Ann. Thorac. Med. 2018, 13, 150–155. [Google Scholar]
- Kawazoe, H.; Mori, N.; Ido, S.; Uozumi, R.; Tsuneoka, K.; Takeuchi, A.; Matsuo, M.; Yamauchi, M.; Nakai, M.; Sumikawa, S.; et al. Liquid Formulation of Gemcitabine Increases Venous Pain in Patients with Cancer: A Retrospective Study. Clin. Ther. 2020, 42, 712–719. [Google Scholar] [CrossRef]
- Kebebew, T.; Mavhandu-Mudzusi, A.H.; Mosalo, A. A cross-sectional assessment of symptom burden among patients with advanced cervical cancer. BMC Palliat. Care 2021, 20, 190. [Google Scholar] [CrossRef] [PubMed]
- Kokkonen, K.; Tasmuth, T.; Lehto, J.T.; Kautiainen, H.; Elme, A.; Jaaskelainen, A.S.; Saarto, T. Cancer patients’ symptom burden and health-related quality of life (HRQoL) at Tertiary Cancer Center from 2006 to 2013: A cross-sectional study. Anticancer Res. 2019, 39, 271–277. [Google Scholar] [CrossRef]
- Kolb, N.A.; Smith, A.G.; Singleton, J.R.; Beck, S.L.; Howard, D.; Dittus, K.; Karafiath, S.; Mooney, K. Chemotherapy-related neuropathic symptom management: A randomized trial of an automated symptom-monitoring system paired with nurse practitioner follow-up. Support. Care Cancer 2018, 26, 1607–1615. [Google Scholar] [CrossRef] [PubMed]
- Ladaninejad, S.; Ilali, E.; Mousavinasab, N.; Taraghi, Z. The Relationship between Depressive Symptoms and Demographic-Medical Characteristics among Elder People with Cancer. Asia Pac. J. Oncol. Nurs. 2019, 6, 424–430. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.S.; Koh, C.E.; Liu, H.; Solomon, M.J.; Johnstone, C.S.H. The Price We Pay for Radical Curative Pelvic Exenterations: Prevalence and Management of Pain. Dis. Colon Rectum 2018, 61, 314–319. [Google Scholar] [CrossRef]
- Molassiotis, A.; Cheng, H.L.; Leung, K.T.; Li, Y.C.; Wong, K.H.; Au, J.S.K.; Sundar, R.; Chan, A.; Ng, T.R.D.; Suen, L.K.P.; et al. Risk factors for chemotherapy-induced peripheral neuropathy in patients receiving taxane- and platinum-based chemotherapy. Brain Behav. 2019, 9, e01312. [Google Scholar] [CrossRef]
- Motah, M.; Gams Massi, D.; Fouda Bekolo, F.; Akweseh Nju, N.; Ndoumbe, A.; Moumi, M.; Sango, A.; Shu, P.; Eyenga, V. Epidemiological profile of brain tumors in Cameroon: A retrospective study. Egypt. J. Neurol. Psychiatr. Neurosurg. 2021, 57, 126. [Google Scholar] [CrossRef]
- Neves Duarte Lisboa, I.; Dantas De Sá Tinôco, J.; Dias Fernandes, M.I.D.C.; Da Silva, R.R.; Student, N.; Barbosa Da Silva, J.; Freire Delgado, M.; Oliveira Lopes, M.V.; Brandão De Carvalho Lira, A.L. Constipation in Chemotherapy Patients: A Diagnostic Accuracy Study. Asian Pac. J. Cancer Prev. 2021, 22, 3017–3021. [Google Scholar] [CrossRef] [PubMed]
- Parás-Bravo, P.; Paz-Zulueta, M.; Alonso-Blanco, M.C.; Salvadores-Fuentes, P.; Alconero-Camarero, A.R.; Santibañez, M. Association among presence of cancer pain, inadequate pain control, and psychotropic drug use. PLoS ONE 2017, 12, e0178742. [Google Scholar] [CrossRef] [PubMed]
- Porta-Sales, J.; Nabal-Vicuna, M.; Vallano, A.; Espinosa, J.; Planas-Domingo, J.; Verger-Fransoy, E.; Julià-Torras, J.; Serna, J.; Pascual-López, A.; Rodríguez, D.; et al. Have We Improved Pain Control in Cancer Patients? A Multicenter Study of Ambulatory and Hospitalized Cancer Patients. J. Palliat. Med. 2015, 18, 923–932. [Google Scholar] [CrossRef]
- Pozzar, R.A.; Hammer, M.J.; Paul, S.M.; Cooper, B.A.; Kober, K.M.; Conley, Y.P.; Levine, J.D.; Miaskowski, C. Distinct sleep disturbance profiles among patients with gynecologic cancer receiving chemotherapy. Gynecol. Oncol. 2021, 163, 419–426. [Google Scholar] [CrossRef]
- Santos, I.; Mendes, L.; Mansinho, H.; Santos, C.A. Nutritional status and functional status of the pancreatic cancer patients and the impact of adjacent symptoms. Clin. Nutr. 2021, 40, 5486–5493. [Google Scholar] [CrossRef]
- Williams, L.A.; Bohac, C.; Hunter, S.; Cella, D. Patient and health care provider perceptions of cancer-related fatigue and pain. Support. Care Cancer 2016, 24, 4357–4363. [Google Scholar] [CrossRef] [PubMed]
- Beyaz, S.G.; Ergönenç, J.Ş.; Ergönenç, T.; Sönmez, Ö.U.; Erkorkmaz, Ü.; Altintoprak, F. Postmastectomy pain: A cross-sectional study of prevalence, pain characteristics, and effects on quality of life. Chin. Med. J. 2016, 129, 66–71. [Google Scholar] [CrossRef]
- Cardoso, L.R.; Rizzo, C.C.; de Oliveira, C.Z.; dos Santos, C.R.; Carvalho, A.L. Myofascial pain syndrome after head and neck cancer treatment: Prevalence, risk factors, and influence on quality of life. Head Neck 2015, 37, 1733–1737. [Google Scholar] [CrossRef] [PubMed]
- Cox-Martin, E.; Anderson-Mellies, A.; Borges, V.; Bradley, C. Chronic pain, health-related quality of life, and employment in working-age cancer survivors. J. Cancer Surviv. 2020, 14, 179–187. [Google Scholar] [CrossRef] [PubMed]
- Fuchs, H.; Hölscher, A.H.; Leers, J.; Bludau, M.; Brinkmann, S.; Schröder, W.; Alakus, H.; Mönig, S.; Gutschow, C.A. Long-term quality of life after surgery for adenocarcinoma of the esophagogastric junction: Extended gastrectomy or transthoracic esophagectomy? Gastric Cancer 2016, 19, 312–317. [Google Scholar] [CrossRef]
- Huang, I.C.; Hudson, M.M.; Robison, L.L.; Krull, K.R. Differential Impact of Symptom Prevalence and Chronic Conditions on Quality of Life in Cancer Survivors and Non-Cancer Individuals: A Population Study. Cancer Epidemiol. Biomark. Prev. 2017, 26, 1124–1132. [Google Scholar] [CrossRef] [PubMed]
- Jefford, M.; Ward, A.C.; Lisy, K.; Lacey, K.; Emery, J.D.; Glaser, A.W.; Cross, H.; Krishnasamy, M.; McLachlan, S.A.; Bishop, J. Patient-reported outcomes in cancer survivors: A population-wide cross-sectional study. Support. Care Cancer 2017, 25, 3171–3179. [Google Scholar] [CrossRef]
- Jiang, C.; Wang, H.; Wang, Q.; Luo, Y.; Sidlow, R.; Han, X. Prevalence of Chronic Pain and High-Impact Chronic Pain in Cancer Survivors in the United States. JAMA Oncol. 2019, 5, 1224–1226. [Google Scholar] [CrossRef]
- Kimberg, C.I.; Klosky, J.L.; Zhang, N.; Brinkman, T.M.; Ness, K.K.; Srivastava, D.K.; Robison, L.L.; Hudson, M.M.; Krull, K.R. Predictors of health care utilization in adult survivors of childhood cancer exposed to central nervous system-directed therapy. Cancer 2015, 121, 774–782. [Google Scholar] [CrossRef]
- Lang, A.E.; Murphy, M.; Dickerson, C.R.; Stavness, I.; Soo, Y.K. Shoulder Dysfunction in Breast Cancer Survivors: Can Treatment Type or Musculoskeletal Factors Identify Those at Higher Risk? Rehabil. Oncol. 2021, 39, 143–151. [Google Scholar] [CrossRef]
- Maass, S.; Boerman, L.M.; Brandenbarg, D.; Verhaak, P.F.M.; Maduro, J.H.; de Bock, G.H.; Berendsen, A.J. Symptoms in long-term breast cancer survivors: A cross-sectional study in primary care. Breast 2020, 54, 133–138. [Google Scholar] [CrossRef] [PubMed]
- Maguire, R.; Drummond, F.J.; Hanly, P.; Gavin, A.; Sharp, L. Problems sleeping with prostate cancer: Exploring possible risk factors for sleep disturbance in a population-based sample of survivors. Support. Care Cancer 2019, 27, 3365–3373. [Google Scholar] [CrossRef] [PubMed]
- Mahmood, N.G.; Mahmood, R.A.; Ibrahim, R.H. The postmastectomy pain syndrome among women in city of mosul-iraq. Teikyo Med. J. 2021, 44, 1625–1630. [Google Scholar]
- McDonough, A.L.; Lei, Y.; Kwak, A.H.; Haggett, D.E.; Jimenez, R.B.; Johnston, K.T.; Moy, B.; Spring, L.M.; Peppercorn, J. Implementation of a Brief Screening Tool to Identify Needs of Breast Cancer Survivors. Clin. Breast Cancer 2021, 21, e88–e95. [Google Scholar] [CrossRef]
- Mehdizadeh, O.B.; Dhar, S.I.; Evangelista, L.; Nativ-Zeltzer, N.; Bewley, A.F.; Belafsky, P.C. Prevalence of profound laryngeal sensory neuropathy in head and neck cancer survivors with feeding tube-dependent oropharyngeal dysphagia. Head Neck 2020, 42, 898–904. [Google Scholar] [CrossRef]
- Moreno, P.I.; Ramirez, A.G.; San Miguel-Majors, S.L.; Castillo, L.; Fox, R.S.; Gallion, K.J.; Munoz, E.; Estabrook, R.; Perez, A.; Lad, T.; et al. Unmet supportive care needs in Hispanic/Latino cancer survivors: Prevalence and associations with patient-provider communication, satisfaction with cancer care, and symptom burden. Support. Care Cancer 2019, 27, 1383–1394. [Google Scholar] [CrossRef]
- Mustafa Ali, M.; Moeller, M.; Rybicki, L.; Moore, H.C.F. Prevalence and correlates of patient-reported symptoms and comorbidities in breast cancer survivors at a tertiary center. J. Cancer Surviv. 2017, 11, 743–750. [Google Scholar] [CrossRef]
- Oancea, S.C.; Brinkman, T.M.; Ness, K.K.; Krull, K.R.; Smith, W.A.; Srivastava, D.K.; Robison, L.L.; Hudson, M.M.; Gurney, J.G. Emotional distress among adult survivors of childhood cancer. J. Cancer Surviv. 2014, 8, 293–303. [Google Scholar] [CrossRef]
- Olsson, I.T.; Lubas, M.M.; Li, C.; Mandrell, B.N.; Banerjee, P.; Howell, C.R.; Ness, K.K.; Srivastava, D.; Robison, L.L.; Hudson, M.M.; et al. Insomnia and neurocognitive functioning in adult survivors of childhood cancer. JNCI Cancer Spectr. 2020, 4, pkaa008. [Google Scholar] [CrossRef]
- Pezdirec, M.; Strojan, P.; Boltezar, I.H. Swallowing disorders after treatment for head and neck cancer. Radiol. Oncol. 2019, 53, 225–230. [Google Scholar] [CrossRef]
- Romero, A.; Torà-Rocamora, I.; Baré, M.; Barata, T.; Domingo, L.; Ferrer, J.; Torà, N.; Comas, M.; Merenciano, C.; Macià, F.; et al. Prevalence of persistent pain after breast cancer treatment by detection mode among participants in population-based screening programs. BMC Cancer 2016, 16, 735. [Google Scholar] [CrossRef]
- Salani, R.; Preston, M.M.; Hade, E.M.; Johns, J.; Fowler, J.M.; Paskett, E.P.; Katz, M.L. Swelling among women who need education about leg lymphedema: A descriptive study of lymphedema in women undergoing surgery for endometrial cancer. Int. J. Gynecol. Cancer 2014, 24, 1507–1512. [Google Scholar] [CrossRef]
- Soares, E.W.S.; Nagai, H.M.; Bredt, L.C.; da Cunha Jr, A.D.; Andrade, R.J.; Soares, G.V.S. Morbidity after conventional dissection of axillary lymph nodes in breast cancer patients. World J. Surg. Oncol. 2014, 12, 67. [Google Scholar] [CrossRef] [PubMed]
- Wulff-Burchfield, E.; Dietrich, M.S.; Ridner, S.; Murphy, B.A. Late systemic symptoms in head and neck cancer survivors. Support. Care Cancer 2019, 27, 2893–2902. [Google Scholar] [CrossRef]
- Yen, H.J.; Eissa, H.M.; Bhatt, N.S.; Huang, S.; Ehrhardt, M.J.; Bhakta, N.; Ness, K.K.; Krull, K.R.; Srivastava, D.K.; Robison, L.L.; et al. Patient-reported outcomes in survivors of childhood hematologic malignancies with hematopoietic stem cell transplant. Blood 2020, 135, 1847–1858. [Google Scholar] [CrossRef] [PubMed]
- Bandeali, S.; des Ordons, A.R.; Sinnarajah, A. Comparing the physical, psychological, social, and spiritual needs of patients with non-cancer and cancer diagnoses in a tertiary palliative care setting. Palliat. Support. Care 2020, 18, 513–518. [Google Scholar] [CrossRef] [PubMed]
- Covarrubias-Gómez, A.; Hernández-Martínez, E.E.; Ruiz-Ramírez, S.; López Collada-Estrada, M. Assessment of pain and other symptoms in Mexican patients with advanced illness. J. Pain Palliat. Care Pharmacother. 2014, 28, 394–398. [Google Scholar] [CrossRef]
- Díez-Manglano, J.; Isasi de Isasmendi Pérez, S.; García Fenoll, R.; Sánchez, L.Á.; Formiga, F.; Giner Galvañ, V.; Dueñas, C.; Roca, B.; Estrada Díaz, C.; Casariego Vales, E. Palliative Sedation in Patients Hospitalized in Internal Medicine Departments. J. Pain Symptom Manag. 2020, 59, 302–309. [Google Scholar] [CrossRef]
- Effendy, C.; Vissers, K.; Osse, B.H.P.; Tejawinata, S.; Vernooij-Dassen, M.; Engels, Y. Comparison of Problems and Unmet Needs of Patients with Advanced Cancer in a European Country and an Asian Country. Pain Pract. 2015, 15, 433–440. [Google Scholar] [CrossRef]
- Goto, H.; Yoshikawa, S.; Otsuka, M.; Omodaka, T.; Yoshimi, K.; Yoshida, Y.; Yamamoto, O.; Kiyohara, Y. Symptom prevalence in patients with advanced skin cancer. J. Dermatol. 2017, 44, 123–126. [Google Scholar] [CrossRef]
- Jaime-Pérez, J.C.; Turrubiates-Hernández, G.A.; Nava-Obregón, T.; Coronado-Hernández, B.; Gutiérrez-Aguirre, H.; Cantú-Rodríguez, O.G.; Herrera-Garza, J.L.; Gómez-Almaguer, D. Palliative Care for Patients with Hematologic Malignancies in a Low-Middle Income Country: Prevalence of Symptoms and the Need for Improving Quality of Attention at the End of Life. Am. J. Hosp. Palliat. Care 2020, 37, 600–605. [Google Scholar] [CrossRef]
- Jakobsen, T.B.T.; Pittureri, C.; Seganti, P.; Borissova, E.; Balzani, I.; Fabbri, S.; Amati, P.; Donigaglia, S.; Gallina, S.; Fabbri, E. Incidence and prevalence of pressure ulcers in cancer patients admitted to hospice: A multicentre prospective cohort study. Int. Wound J. 2020, 17, 641–649. [Google Scholar] [CrossRef]
- Janberidze, E.; Pereira, S.M.; Hjermstad, M.J.; Knudsen, A.K.; Kaasa, S.; van der Heide, A.; Onwuteaka-Philipsen, B. Depressive symptoms in the last days of life of patients with cancer: A nationwide retrospective mortality study. BMJ Support. Palliat. Care 2016, 6, 201–209. [Google Scholar] [CrossRef]
- Mercadante, S.; Aielli, F.; Masedu, F.; Valenti, M.; Ficorella, C.; Porzio, G. Pain characteristics and analgesic treatment in an aged adult population: A 4-week retrospective analysis of advanced cancer patients followed at home. Drugs Aging 2015, 32, 315–320. [Google Scholar] [CrossRef] [PubMed]
- Parra Palacio, S.; Giraldo Hoyos, C.E.; Arias Rodríguez, C.; Mejía Arrieta, D.; Vargas Gómez, J.J.; Krikorian, A. Palliative sedation in advanced cancer patients hospitalized in a specialized palliative care unit. Support. Care Cancer 2018, 26, 3173–3180. [Google Scholar] [CrossRef] [PubMed]
- Prado, B.L.; Gomes, D.B.D.; Usón Júnior, P.L.S.; Taranto, P.; França, M.S.; Eiger, D.; Mariano, R.C.; Hui, D.; Del Giglio, A. Continuous palliative sedation for patients with advanced cancer at a tertiary care cancer center. BMC Palliat. Care 2018, 17, 13. [Google Scholar] [CrossRef] [PubMed]
- Romem, A.; Tom, S.E.; Beauchene, M.; Babington, L.; Scharf, S.M.; Romem, A. Pain management at the end of life: A comparative study of cancer, dementia, and chronic obstructive pulmonary disease patients. Palliat. Med. 2015, 29, 464–469. [Google Scholar] [CrossRef]
- Seiler, A.; Schubert, M.; Hertler, C.; Schettle, M.; Blum, D.; Guckenberger, M.; Weller, M.; Ernst, J.; von Känel, R.; Boettger, S. Predisposing and precipitating risk factors for delirium in palliative care patients. Palliat. Support. Care 2020, 18, 437–446. [Google Scholar] [CrossRef] [PubMed]
- Soares, L.G.L.; Japiassu, A.M.; Gomes, L.C.; Pereira, R.; Peçanha, C.; Goldgaber, T. Prevalence and intensity of dyspnea, pain, and agitation among people dying with late stage dementia compared with people dying with advanced cancer: A single-center preliminary study in Brazil. Ann. Palliat. Med. 2018, 7, 437–443. [Google Scholar] [CrossRef]
- Aboumrad, M.; Shiner, B.; Riblet, N.; Mills, P.D.; Watts, B.V. Factors contributing to cancer-related suicide: A study of root-cause analysis reports. Psychooncology 2018, 27, 2237–2244. [Google Scholar] [CrossRef]
- Aghdassi, A.; Christoph, A.; Dombrowski, F.; Döring, P.; Barth, C.; Christoph, J.; Lerch, M.M.; Simon, P. Gastrointestinal Stromal Tumors: Clinical Symptoms, Location, Metastasis Formation, and Associated Malignancies in a Single Center Retrospective Study. Dig. Dis. 2018, 36, 337–345. [Google Scholar] [CrossRef] [PubMed]
- Aldossary, M.Y.; Alayed, A.A.; Amr, S.S.; Alqahtani, S.; Alnahawi, M.; Alqahtani, M.S. Gallbladder cancer in Eastern Province of Saudi Arabia: A retrospective cohort study. Ann. Med. Surg. 2018, 35, 117–123. [Google Scholar] [CrossRef]
- Aljumah, A.A.; Kuriry, H.; Alzunaitan, M.; Al Ghobain, M.; Al Muaikeel, M.; Al Olayan, A.; Azzumeea, F.; Almutairi, B.; Alalwan, A.; Alghamdi, H. Clinical Presentation, Risk Factors, and Treatment Modalities of Hepatocellular Carcinoma: A Single Tertiary Care Center Experience. Gastroenterol. Res. Pract. 2016, 2016, 1989045. [Google Scholar] [CrossRef] [PubMed]
- Alsalamah, A.K.; Maktabi, A.M.Y.; Alkatan, H.M. Adult orbital lesions in Saudi Arabia: A multi-centered demographic study with clinicopathological correlation. J. Epidemiol. Glob. Health 2020, 10, 359–366. [Google Scholar] [CrossRef] [PubMed]
- Alzghoul, B.N.; Zayed, Y.; Obeidat, A.; Alzghoul, B.; Naser, A.; Shilbayeh, A.R.; Innabi, A.; Al-Hakim, T.; Buchanan, M.; Mehrad, B.; et al. Clinical Characteristics of Sarcoidosis Patients with Self-Reported Lymphoma: A US Nationwide Registry Study. Lung 2021, 199, 611–618. [Google Scholar] [CrossRef]
- Anvari, M.S.; Naderan, M.; Eslami Shahr Babaki, A.; Shoar, S.; Boroumand, M.A.; Abbasi, K. Clinicopathologic review of non-myxoma cardiac tumors: A 10-year single-center experience. Cardiology 2014, 129, 199–202. [Google Scholar] [CrossRef] [PubMed]
- Bentley, R.; O’Cathail, M.; Aznar-Garcia, L.; Crosby, V.; Wilcock, A.; Christian, J. Defining patterns of care in the management of patients with brain metastases in a large oncology centre: A single-centre retrospective audit of 236 cases. Eur. J. Cancer Care 2019, 28, e13059. [Google Scholar] [CrossRef]
- Bubis, L.D.; Delibasic, V.; Davis, L.E.; Jeong, Y.; Chan, K.; Kosyachkova, E.; Mahar, A.; Karanicolas, P.; Coburn, N.G. Patient-reported symptoms in metastatic gastric cancer patients in the last 6 months of life. Support. Care Cancer 2021, 29, 515–524. [Google Scholar] [CrossRef]
- Bunduc, Ș.; Iacob, R.; Costache, R.; Stoica, B.; Radu, C.; Gheorghe, C. Very Early Onset Pancreatic Adenocarcinoma-Clinical Presentation, Risk Factors and Therapeutic Options. Chirurgia 2018, 113, 405–411. [Google Scholar] [CrossRef]
- De Melo, N.B.; de Sousa, V.M.; Bernardino, Í.M.; de Melo, D.P.; Castro Gomes, D.Q.; Bento, P.M. Oral health related quality of life and determinant factors in patients with head and neck cancer. Med. Oral Patol. Oral Cir. Bucal 2019, 24, e281–e289. [Google Scholar] [CrossRef]
- de Sire, A.; Losco, L.; Cisari, C.; Gennari, A.; Boldorini, R.; Fusco, N.; Cigna, E.; Invernizzi, M. Axillary web syndrome in women after breast cancer surgery referred to an Oncological Rehabilitation Unit: Which are the main risk factors? A retrospective case-control study. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 8028–8035. [Google Scholar] [PubMed]
- Diallo, I.; Ndiaye, B.; Touré, M.; Sow, A.; Mbengue, A.; Diawara, P.S.; Gning, S.B.; Mbaye, P.S.; Fall, F.; Mbengue, M. Hepatocellular carcinoma in senegal: Epidemiological, clinical and etiological aspects about 229 cases at hôpital principal de dakar. PAMJ One Health 2021, 38, 99. [Google Scholar] [CrossRef]
- Dubé, C.E.; Mack, D.S.; Hunnicutt, J.N.; Lapane, K.L. Cognitive Impairment and Pain among Nursing Home Residents with Cancer. J. Pain Symptom Manag. 2018, 55, 1509–1518. [Google Scholar] [CrossRef] [PubMed]
- Guérin, A.; Sasane, M.; Zhang, J.; Culver, K.W.; Dea, K.; Nitulescu, R.; Wu, E.Q. Brain metastases in patients with ALK+ non-small cell lung cancer: Clinical symptoms, treatment patterns and economic burden. J. Med. Econ. 2015, 18, 312–322. [Google Scholar] [CrossRef] [PubMed]
- Hallet, J.; Davis, L.E.; Mahar, A.L.; Law, C.H.L.; Isenberg-Grzeda, E.; Bubis, L.D.; Singh, S.; Myrehaug, S.; Zhao, H.; Beyfuss, K.; et al. Patterns of Symptoms Burden in Neuroendocrine Tumors: A Population-Based Analysis of Prospective Patient-Reported Outcomes. Oncologist 2019, 24, 1384–1394. [Google Scholar] [CrossRef] [PubMed]
- Hamieh, N.M.; Akel, R.; Anouti, B.; Traboulsi, C.; Makki, I.; Hamieh, L.; Tfayli, A. Cancer-Related Pain: Prevalence, Severity and Management in a Tertiary Care Center in the Middle East. Asian Pac. J. Cancer Prev. 2018, 19, 769–775. [Google Scholar]
- Haynes-Lewis, H.; Clayton, M.F.; Viswanathan, S.; Moadel-Robblee, A.; Clark, L.; Caserta, M. Distress and Supportive Care Needs of Ethnically Diverse Older Adults with Advanced or Recurrent Cancer. Oncol. Nurs. Forum 2018, 45, 496–507. [Google Scholar] [CrossRef]
- Iadeluca, L.; Mardekian, J.; Chander, P.; Hopps, M.; Makinson, G.T. The burden of selected cancers in the US: Health behaviors and health care resource utilization. Cancer Manag. Res. 2017, 9, 721–730. [Google Scholar] [CrossRef]
- Jeon, M.S.; Dhillon, H.M.; Koh, E.S.; Nowak, A.K.; Hovey, E.; Descallar, J.; Miller, L.; Marshall, N.S.; Agar, M.R. Exploring sleep disturbance among adults with primary or secondary malignant brain tumors and their caregivers. Neurooncol. Pract. 2021, 8, 48–59. [Google Scholar] [CrossRef]
- Kamieniarz, L.; Armeni, E.; O’Mahony, L.F.; Leigh, C.; Miah, L.; Narayan, A.; Bhatt, A.; Cox, N.; Mandair, D.; Navalkissoor, S.; et al. Orbital metastases from neuroendocrine neoplasms: Clinical implications and outcomes. Endocrine 2020, 67, 485–493. [Google Scholar] [CrossRef]
- Miyashita, M.; Wada, M.; Morita, T.; Ishida, M.; Onishi, H.; Sasaki, Y.; Narabayashi, M.; Wada, T.; Matsubara, M.; Takigawa, C.; et al. Independent Validation of the Japanese Version of the EORTC QLQ-C15-PAL for Patients with Advanced Cancer. J. Pain Symptom Manag. 2015, 49, 953–959. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, J.M.; Marmissolle, F.; Bestani, C.; Pesce, V.; Belli, S.; Dominichini, E.; Mendez, G.; Price, P.; Giacomi, N.; Pairola, A.; et al. Observational study of patients with gastroenteropancreatic and bronchial neuroendocrine tumors in argentina: Results from the large database of a multidisciplinary group clinical multicenter study. Mol. Clin. Oncol. 2014, 2, 673–684. [Google Scholar] [CrossRef]
- Parrozzani, R.; Lombardi, G.; Midena, E.; Londei, D.; Padovan, M.; Marchione, G.; Caccese, M.; Midena, G.; Zagonel, V.; Frizziero, L. Ocular Side Effects of EGFR-Inhibitor ABT-414 in Recurrent Glioblastoma: A Long-Term Safety Study. Front. Oncol. 2020, 10, 593461. [Google Scholar] [CrossRef] [PubMed]
- Phanphaisarn, A.; Patumanond, J.; Settakorn, J.; Chaiyawat, P.; Klangjorhor, J.; Pruksakorn, D. Prevalence and Survival Patterns of Patients with Bone Metastasis from Common Cancers in Thailand. Asian Pac. J. Cancer Prev. 2016, 17, 4335–4340. [Google Scholar] [PubMed]
- Pimentel, C.B.; Briesacher, B.A.; Gurwitz, J.H.; Rosen, A.B.; Pimentel, M.T.; Lapane, K.L. Pain management in nursing home residents with cancer. J. Am. Geriatr. Soc. 2015, 63, 633–641. [Google Scholar] [CrossRef]
- Presley, C.J.; Canavan, M.; Wang, S.Y.; Feder, S.L.; Kapo, J.; Saphire, M.L.; Sheinfeld, E.; Kent, E.E.; Davidoff, A.J. Severe functional limitation due to pain & emotional distress and subsequent receipt of prescription medications among older adults with cancer. J. Geriatr. Oncol. 2020, 11, 960–968. [Google Scholar] [PubMed]
- Roila, F.; Fumi, G.; Ruggeri, B.; Antonuzzo, A.; Ripamonti, C.; Fatigoni, S.; Cavanna, L.; Gori, S.; Fabi, A.; Marzano, N.; et al. Prevalence, characteristics, and treatment of fatigue in oncological cancer patients in Italy: A cross-sectional study of the Italian Network for Supportive Care in Cancer (NICSO). Support. Care Cancer 2019, 27, 1041–1047. [Google Scholar] [CrossRef]
- Sadik, M.; Ozlem, K.; Huseyin, M.; AliAyberk, B.; Ahmet, S.; Ozgur, O. Attributes of cancer patients admitted to the emergency department in one year. World J. Emerg. Med. 2014, 5, 85–90. [Google Scholar] [CrossRef]
- Saito, M.; Kage, H.; Ando, T.; Sawada, R.; Amano, Y.; Goto, Y.; Shinoda, Y.; Nagase, T. Prevalence of bone pain decreases as lymph node stage increases in nonsmall cell lung cancer patients. Curr. Probl. Cancer 2019, 43, 86–91. [Google Scholar] [CrossRef]
- Santos, H.B.P.; dos Santos, T.K.G.; Paz, A.R.; Cavalcanti, Y.W.; Nonaka, C.F.W.; Godoy, G.P.; Alves, P.M. Clinical findings and risk factors to oral squamous cell carcinoma in young patients: A 12-year retrospective analysis. Med. Oral Patol. Oral Cir. Bucal 2016, 21, e151–e156. [Google Scholar] [CrossRef]
- Somboon, K.; Siramolpiwat, S.; Vilaichone, R.K. Epidemiology and survival of hepatocellular carcinoma in the central region of Thailand. Asian Pac. J. Cancer Prev. 2014, 15, 3567–3570. [Google Scholar] [CrossRef] [PubMed]
- Song, P.H.; Beyhaghi, H.; Sommer, J.; Bennett, A.V. Symptom burden and life challenges reported by adult chordoma patients and their caregivers. Qual. Life Res. 2017, 26, 2237–2244. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Taghizadeh, A.; Pourali, L.; Vaziri, Z.; Saedi, H.R.; Behdani, F.; Amel, R. Psychological distress in cancer patients. Middle East J. Cancer 2018, 9, 143–149. [Google Scholar]
- Teo, I.; Cheung, Y.B.; Lim, T.Y.K.; Namuduri, R.P.; Long, V.; Tewani, K. The relationship between symptom prevalence, body image, and quality of life in Asian gynecologic cancer patients. Psychooncology 2018, 27, 69–74. [Google Scholar] [CrossRef]
- van Londen, G.J.; Beckjord, E.B.; Dew, M.A.; Cooper, K.L.; Davidson, N.E.; Bovbjerg, D.H.; Donovan, H.S.; Thurston, R.C.; Morse, J.Q.; Nutt, S.; et al. Associations between adjuvant endocrine therapy and onset of physical and emotional concerns among breast cancer survivors. Support. Care Cancer 2014, 22, 937–945. [Google Scholar] [CrossRef] [PubMed]
- Wei-Yun, W.; Shung-Tai, H.; Shang-Liang, W.; Chi-Ming, C.; Chun-Sung, S.; Kwua-Yun, W.; Chun-Yu, L.; Wang, W.Y.; Ho, S.T.; Wu, S.L.; et al. Trends in Clinically Significant Pain Prevalence among Hospitalized Cancer Patients at an Academic Hospital in Taiwan: A Retrospective Cohort Study. Medicine 2016, 95, e2099. [Google Scholar]
- Yassin, M.A.; Taher, A.; Mathews, V.; Hou, H.A.; Shamsi, T.; Tuğlular, T.F.; Xiao, Z.; Kim, S.J.; Depei, W.; Li, J.; et al. MERGE: A Multinational, Multicenter Observational Registry for Myeloproliferative Neoplasms in Asia, including Middle East, Turkey, and Algeria. Cancer Med. 2020, 9, 4512–4526. [Google Scholar] [CrossRef]
- Yates, P.; Miaskowski, C.; Cataldo, J.K.; Paul, S.M.; Cooper, B.A.; Alexander, K.; Aouizerat, B.; Dunn, L.; Ritchie, C.; McCarthy, A.; et al. Differences in Composition of Symptom Clusters Between Older and Younger Oncology Patients. J. Pain Symptom Manag. 2015, 49, 1025–1034. [Google Scholar] [CrossRef]
- Yenugadhati, N.; Albalawi, A.N.; Qureshey, A.T.; Qureshey, E.T.; Al-Jahdali, H.; Jazieh, A.R.; Ahmed, A.E. Associated factors for oral health problems in a sample of saudi cancer patients. Cancer Manag. Res. 2018, 10, 1285–1293. [Google Scholar] [CrossRef]
- Yung, C.S.Y.; Leung, D.K.C.; Cheung, J.P.Y. The prevalence and impact of cervical spine pathologies in patients with nasopharyngeal carcinoma. Oral Oncol. 2019, 90, 48–53. [Google Scholar] [CrossRef]
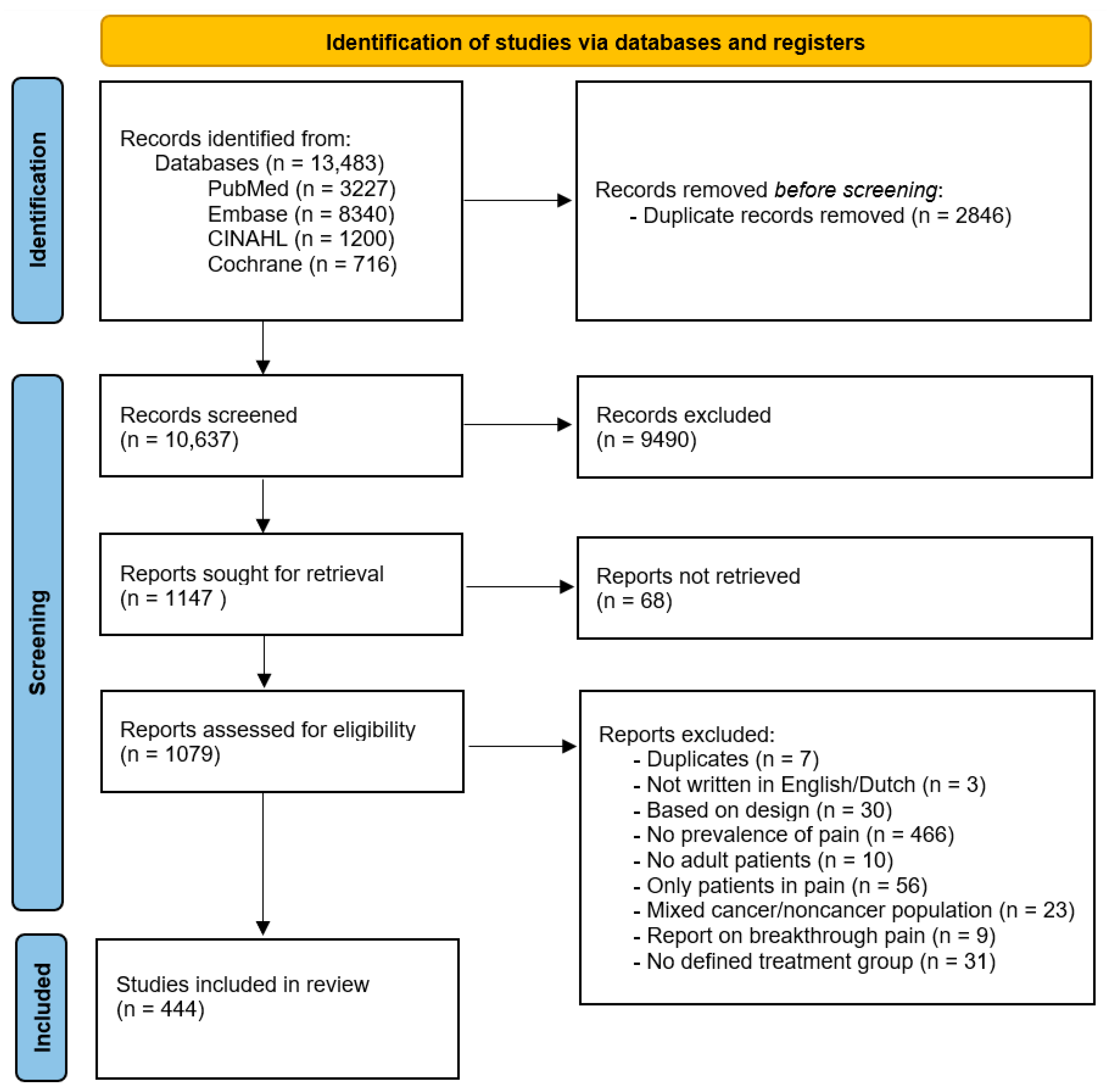
| A. Representatives of population | 1. At least one of the following should apply for the study: an entire target population, randomly selected sample, or sample stated to represent the target population (two points) |
| 2. At least one of the following: reasons for nonresponse described, non-responders described, comparison of responders and non-responders, or comparison of sample and target population (two points) | |
| 3. Response rate ≥90% (two points) Response rate 70–90% (one point) Response rate ˂70% (zero points) | |
| B. Quality of data | 4. Were the primary data from a prevalence study (two points) or were they taken from a survey not specifically designed for the purpose (one point)? |
| 5. The same mode of data collection should be used for all subjects (two points), if not (zero points). | |
| 6. The data have been collected directly from the patient by means of a validated questionnaire/interview (three points), no validated questionnaire/interview (two points), data have been collected from proxies or retrospectively from medical record (zero points) | |
| C. General description of method and results | 7. Description of the target population and setting where patients were found (two points) |
| 8. Description of stage of disease (one point) | |
| 9. Description of type of cancer, gender, and age: all (two points), 2 of 3 (one point), 1 of 3 (zero points) | |
| 10. Final sample size (one point) | |
| D. Definition of pain prevalence | 11. Prevalence recall periods should be stated (one point) |
| % Pain | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study | Quality | Continent a | Setting b | Cancer c | Mean Age | Sample | None | Mild | Moderate | ModSev d | Severe | Overall |
| Alt-Epping, 2016 [33] | 16 | 2 | 2 | 60.6 | 22 | 22.7 | 18.2 | 45.5 | 59.1 | 13.6 | 77.3 | |
| Andersen, 2014 [34] | 16 | 2 | 2 | 5 | 133 | 60 | 7 | 37 | ||||
| Bibby, 2019 [35] | 15 | 2 | 2 | 11 | 64 | 229 | 43.7 | |||||
| Efficace, 2015 [36] | 16 | 1,2,3 | 2 | 10 | 70.02 | 280 | 45 | 43.2 | 11.8 | 55 | ||
| Esser, 2017 [37] | 15 | 2 | 2 | 10 | 50.4 | 239 | 15 | |||||
| Gjeilo, 2020 [38] | 18 | 2 | 1,2 | 4 | 65.8 | 264 | 60 | 40 | ||||
| Godby–a, 2021 [39] Godby–b, 2021 [39] | 18 18 | 1 1 | 2 2 | 6 6 | 70 70 | 46 309 | 75.6 40.7 | |||||
| Hong, 2015 [40] | 15 | 3 | 1 | 6 | 62.18 | 165 | 62.4 | |||||
| Kirchheiner, 2015 [41] | 17 | 2 | 2 | 9 | 50 | 6.0 | ||||||
| Kuon, 2019 [42] | 17 | 2 | 2 | 4 | 63.6 | 208 | 34.6 | |||||
| Lunde, 2019 [43] | 18 | 2 | 2 | 9 | 67.2 | 207 | 16.9 | |||||
| Ravn Munkvold, 2018 [44] | 18 | 2 | 1 | 2 | 507 | 48 | 30 | 12 | 22 | 10 | 52 | |
| Roy, 2016 [45] | 16 | 3 | 2 | 4 | 56.4 | 36 | 47.2 | |||||
| Russo, 2018 [46] | 17 | 2 | 2 | 2 | 52.7 | 527 | 12.5 | |||||
| Salwey, 2020 [47] | 19 | 2 | 2 | 60 | 26.7 | 20 | 53.3 | 73.3 | ||||
| Tang, 2015 [48] | 18 | 6 | 1 | 11 | 55.1 | 91 | 46.8 | 21.1 | 63.2 | |||
| Thomas, 2017 [49] | 15 | 1 | 2 | 1 | 66 | 105 | 63 | |||||
| Wang, 2021 [50] | 16 | 3 | 2 | 5 | 50.99 | 88 | 4.5 | |||||
| Williams, 2021 [51] | 15 | 1 | 2 | 6 | 70.1 | 364 | 45.1 | |||||
| Yao, 2020 [52] | 15 | 1 | 2 | 7 | 83 | 69.2 | 23.1 | 5.8 | 7.7 | 1.9 | 30.8 | |
| % Pain | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study | Quality | Continent a | Setting b | Cancer c | Mean Age | Sample | None | Mild | Moderate | ModSev d | Severe | Overall |
| Andersen, 2014 [34] | 16 | 2 | 2 | 5 | 133 | 20 | 26 | 78 | ||||
| Berliere–a, 2021 [53] Berliere–b, 2021 [53] | 16 16 | 2 2 | 1,2 1,2 | 5 5 | 53 | 32 31 | 46.0 29.0 | |||||
| Bretschneider, 2016 [54] | 16 | 1 | 2 | 9 | 58.1 | 152 | 53.4 | 29.7 | 8.8 | 16.9 | 8.1 | 46.6 |
| Browall, 2017 [55] | 17 | 2 | 2 | 5 | 59 | 124 | 67 | |||||
| Calderon, 2019 [56] | 15 | 2 | 2 | 5 | 53.2 | 240 | 4.2 | |||||
| Choo, 2019 [57] | 17 | 3 | 2 | 5 | 60.35 | 192 | 59.9 | |||||
| de Menezes Couceiro, 2014 [58] | 16 | 4 | 2 | 5 | 54 | 250 | 44.4 | |||||
| Dylke, 2015 [59] | 15 | 6 | 2 | 5 | 55 | 157 | 83 | |||||
| El-Aqoul, 2018 [60] | 17 | 3 | 1 | 1 | 47.6 | 800 | 43.6 e | 56.4 | ||||
| Fenlon, 2014 [61] | 16 | 2 | 2 | 5 | 57 | 455 | 53 | |||||
| Fjell, 2020 [62] | 16 | 2 | 2 | 5 | 49 | 150 | 42.5 | |||||
| Hagiwara–a, 2018 [63] Hagiwara–b, 2018 [63] | 19 19 | 3 3 | 2 2 | 6 6 | 178 176 | 42.0 41.0 | ||||||
| Haryani, 2018 [64] | 16 | 3 | 2 | 1 | 50.51 | 207 | 38.2 | 17.9 | 22.7 | 4.8 | 60.87 | |
| Ho, 2015 [65] | 15 | 3 | 2 | 5 | 49 | 133 | 24 | |||||
| Hong, 2014 [66] | 16 | 3 | 1 | 1 | 51.24 | 1217 | 88 | 12 | ||||
| Jarden, 2021 [67] | 16 | 2 | 1 | 10 | 53.1 | 70 | 55.2 | |||||
| Jensen, 2018 [68] | 17 | 2 | 2 | 9 | 49 | 1176 | 60.6 | 26.8 | 9.1 | 12.6 | 3.5 | 39.4 |
| Khan–a, 2017 [69] Khan–b, 2017 [69] | 15 15 | 1 1 | 2 2 | 5 5 | 62 60.5 | 80 80 | 36 50 | 30 20 | 30 26 | 30 27 | 0 1 | 60 47 |
| Kim, 2016 [70] | 16 | 3 | 1 | 5 | 50.3 | 1499 | 8.8 e | 91.2 | ||||
| Kirchheiner, 2015 [41] | 17 | 2 | 2 | 9 | 50 | 42.0 | ||||||
| Kirkham, 2018 [71] | 15 | 1 | 1 | 5 | 50 | 24 | 54 | |||||
| Lewis, 2015 [72] | 16 | 6 | 2 | 1 | 61 | 276 | 55.0 | |||||
| Lewis, 2021 [73] | 18 | 3 | 2 | 2 | 600 | 45.2 | ||||||
| McFarland, 2018 [74] | 15 | 1 | 2 | 5 | 55.4 | 125 | 19.5 | |||||
| Moloney, 2016 [75] | 16 | 6 | 1 | 5 | 54.2 | 121 | 24 | 46.2 | ||||
| Nogueira de Oliveira Martins–a, 2017 [76] Nogueira de Oliveira Martins–b, 2017 [76] | 17 17 | 4 4 | 2 2 | 5 5 | 49.6 49.6 | 11 11 | 90.9 72.2 | |||||
| Okamoto, 2018 [77] | 17 | 3 | 2 | 5 | 59 | 123 | 48.8 | 42.3 | 8.9 | 14 | 5.1 | 51.2 |
| Ribas, 2020 [78] | 15 | 2 | 2 | 9 | 65 | 109 | 20.1 | |||||
| Røhrl, 2016 [79] | 17 | 2 | 2 | 6 | 60.7 | 68 | 44.1 | |||||
| Shaulov, 2019 [80] | 16 | 1 | 1,2 | 10 | 49.1 | 318 | 51.3 | 8.3 | 22.9 | 40.4 | 17.5 | 49.2 |
| Tran, 2020 [81] | 16 | 3 | 1 | 6 | 57.7 | 197 | 87 | |||||
| Wang, 2021 [50] | 16 | 3 | 2 | 5 | 80 | 12.5 | ||||||
| Xu–a, 2020 [82] Xu–b, 2020 [82] Xu–c, 2020 [82] | 15 15 15 | 3 3 3 | 2 2 2 | 5 5 5 | 51 51 51 | 235 210 227 | 66.1 70.5 72.2 | 20.9 19.5 19.4 | 11.5 9.5 8.4 | 12.35 10 8.4 | 0.85 0.5 0 | 33.25 29.5 27.8 |
| Yi, 2018 [83] | 16 | 3 | 2 | 5 | 53.56 | 110 | 13.6 | 61.8 | 20 | 24.5 | 4.5 | 86.4 |
| % Pain | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study | Quality | Continent a | Setting b | Cancer c | Mean Age | Sample | None | Mild | Moderate | ModSev d | Severe | Overall |
| Agarwal, 2020 [84] | 15 | 3 | 3 | 1 | 46.8 | 110 | 4.5 | 24.5 | 38.2 | 70.9 | 32.7 | 95.5 |
| Al-Zahrani, 2014 [85] | 18 | 3 | 3 | 1 | 56 | 124 | 14.5 | 43.5 | 85.5 | |||
| Blank, 2018 [86] | 15 | 1 | 2 | 1 | 13 | 0 | 7.7 | 46.2 | 92.4 | 46.2 | 100 * | |
| Bouché, 2018 [87] | 17 | 2 | 2 | 6 | 151 | 22.5 | ||||||
| Bullock, 2017 [88] | 16 | 1 | 2 | 6 | 40 | 80 | ||||||
| Green, 2015 [89] | 17 | 1 | 2 | 7 | 396 | 6 | 8 | 2 | ||||
| Iwase, 2015 [90] | 16 | 3 | 2 | 1 | 63.5 | 183 | 10.5 | 25.4 | 27.6 | 64.1 | 36.5 | 89.5 |
| Jespersen, 2021 [91] | 16 | 2 | 2 | 10 | 92 | 13.0 | 23.9 | 56.5 | 63.0 | 6.5 | 86.9 | |
| King, 2018 [92] | 15 | 1,2,3,6 | 2 | 9 | 62.5 | 903 | 20.5 | 38.5 | 23.1 | 41 | 17.9 | 79.5 |
| Koldenhof–a, 2014 [93] Koldenhof–b, 2014 [93] | 16 16 | 2 2 | 2 2 | 6 6 | 62 66 | 26 16 | 23 17 | |||||
| Lavdaniti, 2018 [94] | 17 | 2 | 1 | 1 | 63.8 | 123 | 41.5 | 0 | 17.1 | 58.5 | 41.4 | 58.5 |
| LeBlanc, 2015 [95] | 16 | 1 | 2 | 4 | 63 | 97 | 22.7 | 32 | 9.3 | |||
| Lechner, 2016 [96] | 16 | 1 | 1,2 | 1 | 62 | 25.8 | ||||||
| Madsen, 2017 [97] | 17 | 2 | 2 | 11 | 63 | 112 | 45 | |||||
| McFarland, 2017 [98] | 15 | 1 | 2 | 10 | 57.7 | 117 | 21.5 | |||||
| Mercadante–a, 2016 [99] Mercadante–b, 2016 [99] Mercadante–c, 2016 [99] Mercadante–d, 2016 [99] | 15 15 15 15 | 2 2 2 2 | 4 4 4 4 | 1 1 1 1 | 54.5 69.6 79.7 88.8 | 103 89 116 104 | 35.0 38.2 42.2 44.2 | 45.6 34.8 31.9 31.7 | 15.5 20.2 22.4 20.2 | 19.4 26.9 25.8 24.0 | 3.9 6.7 3.4 3.8 | 65.0 61.7 57.7 55.7 |
| Røhrl, 2016 [79] | 17 | 2 | 2 | 6 | 65.5 | 52 | 59.6 | |||||
| Sampogna–a, 2019 [100] Sampogna–b, 2019 [100] | 17 17 | 2 2 | 2 2 | 11 11 | 63.9 63.9 | 368 65 | 24 5 | |||||
| Selvy, 2021 [101] | 17 | 2 | 2 | 10 | 66.7 | 67 | 59.7 | |||||
| Steel, 2016 [102] | 15 | 1 | 1 | 61 | 261 | 31.7 | ||||||
| Walling, 2015 [103] | 15 | 1 | 4,6 | 5422 | 15 | 48.2 | ||||||
| Zhou–a, 2017 [104] | 17 | 1 | 2 | 1 | 51.4 | 119 | 19.3 | |||||
| Zhou–b, 2017 [104] | 17 | 1 | 2 | 1 | 49.6 | 42 | 19.0 | |||||
| Zhou–c, 2017 [104] | 17 | 1 | 2 | 1 | 50.2 | 93 | 43.0 | |||||
| Zhou–d, 2017 [104] | 17 | 1 | 2 | 1 | 48.7 | 52 | 50.0 | |||||
| % Pain | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study | Quality | Continent a | Setting b | Cancer c | Mean Age | Sample | None | Mild | Moderate | ModSev d | Severe | Overall |
| Abu-Saad Huijer, 2015 [105] | 16 | 3 | 2 | 1 | 54.32 | 190 | 45.3 | |||||
| Bernardes, 2019 [106] | 15 | 6 | 1,2 | 1 | 125 | 81 | 10 | 10 | 20 | |||
| Chan, 2015 [107] | 16 | 3 | 11 | 57.3 | 79 | 25.3 | ||||||
| Chen, 2021 [108] | 15 | 3 | 2 | 10 | 41.7 | 132 | 57.6 | |||||
| Cheng, 2021 [109] | 15 | 3 | 2 | 5 | 127 | 21.3 | ||||||
| Damm, 2020 [110] | 16 | 2 | 1,2 | 6 | 139 | 43.9 | 17.9 | 18.6 | 0.7 | 63 | ||
| Fujii, 2017 [111] | 19 | 3 | 2 | 1 | 60.8 | 524 | 46.2 | 39.9 | 7.6 | 13.9 | 6.3 | 53.8 |
| Gosselin, 2016 [112] | 15 | 1 | 2 | 6 | 275 | 48 | 24 | 28 | 28 | 0 | 52 | |
| Han, 2019 [113] | 15 | 1 | 2 | 1 | 57.9 | 399 | 59.4 | |||||
| Joseph, 2021 [114] | 15 | 5 | 2 | 1 | 347 | 14.1 | 21.9 | 48.7 | 64 | 15.3 | 85.9 | |
| Kim, 2015 [115] | 15 | 3 | 2 | 1 | 60.02 | 167 | 25.7 | 92.8 | ||||
| Kuperus, 2021 [116] | 15 | 1 | 2 | 8 | 113 | 74 | 14.7 | 8.8 | 11.3 | 2.5 | 26 | |
| Lee–a, 2016 [117] Lee–b, 2016 [117] | 20 20 | 1 1 | 2 2 | 5 5 | 56.0 56.0 | 358 335 | 16 f 31 f | |||||
| Li, 2017 [118] | 15 | 3 | 1 | 55.36 | 317 | 60.25 | 29.02 | 5.36 | 10.41 | 5.05 | 39.43 | |
| Llamas Ramos, 2016 [119] | 15 | 2 | 2 | 1 | 59.98 | 246 | 13.4 | 24.4 | 37 | 12.6 | 50.4 | |
| Matsumoto, 2020 [120] | 19 | 3 | 2 | 6 | 45 | 55.6 | ||||||
| Molassiotis, 2019 [121] | 16 | 2,3 | 1,2 | 1 | 55.15 | 343 | 14.2 | |||||
| Moye, 2014 [122] | 16 | 1 | 2,3,6 | 64.66 | 170 | 21.6 | 32.4 | 10.8 | ||||
| Pearce–a, 2017 [123] Pearce–b, 2017 [123] Pearce–c, 2017 [123] | 15 15 15 | 6 6 6 | 2 2 2 | 5 6 4 | 243 142 56 | 74 77 77 | ||||||
| Pérez, 2015 [124] | 17 | 2 | 2 | 1 | 60.7 | 358 | 45.8 | 26.3 | 54.2 | |||
| Pettersson, 2014 [125] | 16 | 2 | 2 | 6 | 65 | 104 | 41 | |||||
| Raj, 2014 [126] | 19 | 2 | 2 | 1 | 60 | 305 | 48.2 | |||||
| Ritchie–a, 2014 [127] Ritchie–b, 2014 [127] Ritchie–c, 2014 [127] Ritchie–d, 2014 [127] | 16 16 16 16 | 6 6 6 6 | 2 2 2 2 | 1 1 1 1 | 62.1 67.3 72.4 78.8 | 78 94 76 82 | 66.7 50.0 59.2 53.7 | |||||
| Salvetti, 2020 [128] | 15 | 4 | 1 | 55 | 107 | 42.1 | ||||||
| Schumacher–a, 2021 [129] Schumacher–b, 2021 [129] | 15 15 | 6 6 | 2 2 | 7 7 | 67.9 67.8 | 72 43 | 18.1 23.3 | |||||
| Seven, 2016 [130] | 15 | 2 | 1 | 9 | 59 | 134 | 57.3 | 15.7 | 20.2 | 26.9 | 6.7 | 42.6 |
| Spoelstra, 2015 [131] | 16 | 1 | 2 | 1 | 65.1 | 30 | 63.3 | |||||
| Stamm, 2021 [132] | 15 | 2 | 2 | 10 | 61 | 47 | 69 | |||||
| Steffen McLouth, 2020 [133] | 16 | 1 | 4 | 62.5 | 60 | 41.7 | ||||||
| Thiagarajan, 2016 [134] | 16 | 3 | 1,2 | 1 | 52.7 | 303 | 15.6 | 13.8 | 19.4 | 23.8 | 4.4 | 37.6 |
| Turner, 2014 [135] | 15 | 6 | 2 | 1 | 76.7 | 385 | 26 | |||||
| Unseld, 2021 [136] | 15 | 2 | 2 | 1 | 57.4 | 846 | 36.5 | 43.5 | 13.6 | 20 | 6.4 | 63.5 |
| van der Baan, 2020 [137] | 15 | 2 | 1,2 | 1 | 58.2 | 1919 | 24 | |||||
| Wang, 2014 [138] | 16 | 3 | 4 | 58.25 | 183 | 71 | ||||||
| Yahaya, 2015 [139] | 16 | 3 | 1 | 53.4 | 268 | 51.1 | ||||||
| Zhong, 2017 [140] | 17 | 3 | 1 | 1 | 59.7 | 517 | 70.2 e | 29.8 | ||||
| % Pain | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study | Quality | Continent a | Setting b | Cancer c | Mean Age | Sample | None | Mild | Moderate | ModSev d | Severe | Overall |
| Adams, 2014 [141] | 17 | 2 | 2 | 1 | 70.6 | 418 | 15.5 | |||||
| Ahmed, 2014 [142] | 17 | 3 | 2 | 5 | 49.33 | 73 | 5.4 | |||||
| Al Maqbali, 2021 [143] | 15 | 3 | 2 | 5 | 133 | 45.1 | ||||||
| Andersen, 2015 [144] | 19 | 2 | 2 | 5 | 475 | 86 | 14 | |||||
| Asplund, 2015 [145] | 18 | 2 | 2 | 6 | 545 | 79 | 7 | 21 | ||||
| Baden, 2020 [146] | 18 | 2 | 2 | 7 | 3348 | 24 | ||||||
| Bao, 2018 [147] | 18 | 1 | 2 | 5 | 1280 | 33.3 | ||||||
| Bennedsgaard–a, 2020 [148] Bennedsgaard–b, 2020 [148] | 17 17 | 2 2 | 2 2 | 5 6 | 56.6 68.0 | 80 52 | 47.5 45.1 | |||||
| Boehmer–a, 2021 [149] Boehmer–b, 2021 [149] | 17 17 | 1 1 | 2 2 | 6 6 | 116 302 | 6.1 6.6 | ||||||
| Bøhn, 2019 [150] | 16 | 2 | 2 | 1 | 49.1 | 1088 | 10 | |||||
| Bonhof, 2020 [151] | 17 | 2 | 2 | 6 | 477 | 9 | ||||||
| Bovbjerg, 2019 [152] | 15 | 1 | 2 | 5 | 59.4 | 417 | 50.6 | |||||
| Bulley, 2014 [153] | 15 | 2 | 2 | 5 | 62.3 | 595 | 28.8 | |||||
| Cameron, 2018 [154] | 16 | 1 | 2 | 1 | 26.9 | 124 | 54.5 | |||||
| Capelan, 2017 [155] | 15 | 2 | 2 | 5 | 214 | 29 | ||||||
| Chiang, 2019 [156] | 18 | 6 | 2 | 5 | 60.2 | 201 | 23 | 4 | 55 | |||
| Cramer, 2018 [2] | 18 | 1 | 2 | 2 | 175 | 54.9 | 22 | 11.6 | 23.1 | 11.5 | 45.1 | |
| Cui, 2018 [157] | 15 | 3 | 2 | 5 | 52.4 | 420 | 36.2 | |||||
| de Groef, 2017 [158] | 16 | 2 | 2 | 5 | 54.1 | 147 | 50 | |||||
| Dieterich–a, 2021 [159] Dieterich–b, 2021 [159] | 15 15 | 2 2 | 2 2 | 5 5 | 60.9 64.4 | 120 55 | 60.8 62.3 | 27.5 20.8 | 8.4 15 | 11.7 16.9 | 3.3 1.9 | 39.2 37.7 |
| Drury, 2017 [160] | 17 | 2 | 2 | 6 | 66.4 | 252 | 64 | 26 | 8 | 10 | 2 | 36 |
| Dualé, 2014 [161] | 18 | 2 | 2 | 5 | 442 | 37.1 | ||||||
| Efficace, 2019 [162] | 15 | 2 | 2 | 10 | 52.5 | 244 | 51 | 27 | 22 | 49 | ||
| Engvall, 2021 [163] | 16 | 2 | 2 | 5 | 60.7 | 646 | 46.3 | |||||
| Esser, 2017 [37] | 15 | 2 | 2 | 10 | 47.7 | 102 | 8 | |||||
| Ezendam, 2014 [164] | 17 | 2 | 2 | 9 | 65 | 180 | 31.7 | |||||
| Farrukh, 2020 [165] | 17 | 1 | 2 | 10 | 736 | 39.4 | ||||||
| Feddern, 2015 [166] | 19 | 2 | 2 | 6 | 1369 | 13 | 13 | 18 | 5 | 31 | ||
| Ferreira, 2019 [167] | 18 | 2 | 2 | 5 | 4262 | 51 | ||||||
| Gallaway, 2020 [168] | 17 | 1 | 2 | 1 | 12,019 | 9.5 | ||||||
| Gjeilo, 2020 [38] | 18 | 2 | 2 | 4 | 194 | 55 | ||||||
| Gong, 2020 [169] | 16 | 3 | 2 | 5 | 49.3 | 1983 | 28.2 | |||||
| Götze–a, 2018 [170] Götze–b, 2018 [170] | 16 16 | 2 2 | 2 2 | 1 1 | 66.3 67.3 | 660 342 | 51.2 50.8 | |||||
| Hammer, 2014 [171] | 15 | 1 | 2 | 9 | 63.5 | 213 | 22.5 | |||||
| Hamood–a, 2016 [172] Hamood–b, 2016 [172] | 15 15 | 3 3 | 2 2 | 5 5 | 57 50 | 54 29 | 25.9 10.3 | 9.3 10.3 | 48.2 34.5 | 48.2 55.2 | 0 20.7 | 57.4 65.5 |
| Hamood, 2018 [173] | 17 | 3 | 2 | 5 | 410 | 64 | 74.4 | |||||
| Haviland, 2017 [174] | 17 | 2 | 2 | 5 | 55.1 | 864 | 32.3 | |||||
| Henderson–a, 2014 [175] Henderson–b, 2014 [175] | 16 16 | 2 2 | 2 2 | 5 5 | 63 49 | 138 134 | 73.2 61.9 | 17.4 26.1 | 9.4 10.4 | 9.4 11.9 | 0 1.5 | 26.8 38 |
| Henry, 2020 [176] | 16 | 1 | 2 | 63.3 | 145 | 16.6 | 15.9 | 21.4 | 5.5 | 37.9 | ||
| Hope-Stone, 2015 [177] | 15 | 2 | 2 | 11 | 66.7 | 179 | 77 | 23 | ||||
| Huang, 2020 [178] | 15 | 1 | 2 | 1 | 33.6 | 1208 | 18.7 | |||||
| Janah, 2020 [179] | 16 | 2 | 2 | 1 | 4093 | 36.5 | 63.5 | |||||
| Jansen, 2018 [180] | 15 | 2 | 2 | 2 | 70 | 283 | 8.8 | |||||
| Jardim, 2020 [181] | 16 | 4 | 2 | 5 | 55 | 151 | 18.5 | |||||
| Jariwala, 2021 [182] | 19 | 3 | 2 | 5 | 50 | 212 | 12 | |||||
| Johannsdottir, 2017 [183] | 15 | 2 | 2 | 11 | 124 | 56.1 | 33.3 | 10.6 | 10.6 | 0 | 43.9 | |
| Johannsen, 2015 [184] | 17 | 2 | 2 | 5 | 1905 | 72.7 | ||||||
| Juhl, 2016 [185] | 19 | 2 | 2 | 5 | 63.6 | 261 | 13 | 19.2 | 25.3 | 6.1 | 38.3 | |
| Karlson, 2020 [186] | 15 | 1 | 2 | 1 | 10,012 | 71.4 e | 20.5 | 28.6 | 8.1 | |||
| Kaur, 2018 [187] | 15 | 3 | 2 | 5 | 49.76 | 230 | 63.5 | |||||
| Kelada, 2019 [188] | 16 | 6 | 2 | 10,11 | 26.27 | 404 | 28.7 | |||||
| Kibar, 2017 [189] | 16 | 2 | 2 | 5 | 52.5 | 201 | 68.2 | 31.8 | ||||
| Kjaer, 2016 [190] | 15 | 2 | 2 | 2 | 64 | 369 | 16.0 | |||||
| Knowlton, 2020 [191] | 15 | 1 | 2 | 1 | 294 | 24.2 | ||||||
| Koehler, 2018 [192] | 19 | 1 | 2 | 5 | 56 | 36 | 44.0 | |||||
| Kramer, 2019 [193] | 15 | 5 | 2 | 5 | 60.05 | 349 | 26 | 46 | 14 | 28 | 14 | 74 |
| Lou, 2021 [194] | 16 | 1 | 2 | 2 | 59.3 | 77 | 40 f | |||||
| Lunde, 2019 [43] | 18 | 2 | 2 | 9 | 67.2 | 207 | 14.9 | |||||
| Lunde, 2020 [195] | 19 | 2 | 2 | 9 | 66.1 | 140 | 13.6 | |||||
| Madsen, 2017 [97] | 17 | 2 | 2 | 11 | 63 | 95 | 37 | |||||
| Mao, 2018 [196] | 15 | 1 | 2 | 5 | 1103 | 26.2 | ||||||
| Mertz, 2017 [197] | 19 | 2 | 2 | 5 | 473 | 67 | 21 | 12 | 33 | |||
| Miaskowski, 2014 [198] | 18 | 1 | 2 | 5 | 54.98 | 394 | 41.6 | 58.4 | ||||
| Min, 2021 [199] | 15 | 3 | 2 | 7 | 64 | 111 | 12.6 | |||||
| Mulrooney, 2019 [200] | 19 | 1 | 2 | 10 | 980 | 70 | 23 | 5 | 7 | 2 | 30 | |
| Paek, 2019 [201] | 18 | 3 | 2 | 1 | 62.2 | 1037 | 71.9 | 28.1 | 28.1 | |||
| Park, 2018 [202] | 17 | 3 | 2 | 11 | 36.43 | 144 | 75 | 25 | ||||
| Poço Conçalves, 2021 [203] | 17 | 2 | 2 | 1 | 65.33 | 85 | 77.6 | 0 | 20 | 22.4 | 2.4 | 22.4 |
| Ravn Munkvold, 2018 [44] | 18 | 2 | 2 | 2 | 357 | 70 | 19 | 7 | 11 | 4 | 30 | |
| Reilly, 2016 [204] | 17 | 1 | 2 | 10 | 47.6 | 31 | 68 | |||||
| Ren, 2021 [205] | 17 | 1 | 2 | 2 | 61.5 | 505 | 55 | 17.7 | 19.5 | 26.9 | 7.4 | 45 |
| Rogers, 2021 [206] | 15 | 1 | 2 | 11 | 47 | 248 | 49 | |||||
| Rosenberg, 2015 [207] | 15 | 1 | 2 | 5 | 55.8 | 2086 | 48 | |||||
| Sanchez-Birkhead, 2017 [208] | 15 | 1 | 2 | 5 | 52.6 | 35 | 38.3 | 79 | ||||
| Sanford, 2019 [209] | 15 | 1 | 2 | 1 | 7565 | 67.5 | 32.5 | |||||
| Schou Bredal, 2014 [210] | 16 | 2 | 2 | 5 | 56 | 834 | 21 | 17 | 20 | 3 | 41 | |
| Selvy, 2020 [211] | 16 | 2 | 2 | 6 | 66.3 | 406 | 11.5 | |||||
| Steyaert, 2016 [212] | 15 | 2 | 2 | 5 | 56.5 | 128 | 43.8 | |||||
| Tang, 2015 [48] | 18 | 6 | 1 | 11 | 55.1 | 76 | 53.9 | 19.7 | 46.1 | |||
| Terkawi, 2017 [213] | 16 | 3 | 2 | 2 | 49.6 | 102 | 30 | |||||
| Tonning Olsson, 2021 [214] | 16 | 1 | 2 | 1 | 32.2 | 2836 | 61.1 | 38.9 | 38.9 | |||
| Tung, 2019 [215] | 18 | 1 | 2 | 6 | 615 | 44.87 | ||||||
| van de Luijtgaarden, 2014 [216] | 17 | 2 | 2 | 11 | 45.7 | 24 | 93 | |||||
| van Eck, 2020 [217] | 15 | 2 | 2 | 11 | 60 | 752 | 14 | |||||
| Variawa, 2016 [218] | 18 | 5 | 2 | 5 | 58.54 | 92 | 38.04 | |||||
| Vuksanovic, 2021 [219] | 16 | 6 | 2 | 5 | 130 | 34.4 | ||||||
| Wang, 2021 [50] | 16 | 3 | 2 | 5 | 75 | 4.5 | ||||||
| Wilson, 2020 [220] | 17 | 1 | 1 | 11 | 136 | 16.3 | ||||||
| % Pain | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study | Quality | Continent a | Setting b | Cancer c | Mean Age | Sample | None | Mild | Moderate | ModSev d | Severe | Overall |
| Aktas, 2014 [221] | 17 | 1 | 4 | 1 | 1000 | 84 | ||||||
| Corli, 2020 [222] | 19 | 2 | 1,2,4 | 1 | 74.2 | 865 | 60.5 | |||||
| de la Cruz, 2015 [223] | 15 | 1 | 4 | 1 | 78 | 51 | ||||||
| Drat-Gzubicka, 2021 [224] | 18 | 2 | 3 | 76 | 29 | |||||||
| Gupta, 2016 [225] | 16 | 3 | 1 | 1 | 52.49 | 110 | 32.73 | 11.82 | 22.73 | 55.46 | 32.73 | 67.27 |
| Guthrie, 2019 [226] | 15 | 1 | 2 | 1 | 21,119 | 48.3 | ||||||
| Hui, 2020 [227] | 18 | 1 | 4 | 1 | 60 | 200 | 67 | |||||
| Mejin, 2019 [228] | 15 | 3 | 3 | 1 | 57,1 | 151 | 18.5 | 14.6 | 19.2 | 66.9 | 47.7 | 81.5 |
| Mercadante, 2018 [229] | 15 | 2 | 3 | 1 | 72.1 | 263 | 6.9 | |||||
| Morita–a, 2014 [230] Morita–b, 2014 [230] | 16 16 | 3 3 | 4 5 | 1 1 | 67 68 | 859 857 | 42 43 | 41 40 | 8.9 8.4 | 17.2 16 | 8.3 7.6 | 58 59 |
| Rojas-Concha, 2020 [231] | 17 | 2 | 3 | 1 | 5449 | 95.8 | 0.4 | 1.8 | 3.9 | 2.1 | 4.2 | |
| Seow–a, 2021 [232] Seow–b, 2021 [232] | 15 15 | 1 1 | 2 1 | 11,407 15,888 | 64.9 61.4 | |||||||
| Silvia, 2021 [233] | 17 | 4 | 3 | 1 | 490 | 49.6 | 26.5 | 12.9 | 23.9 | 11 | 50.4 | |
| Tofthagen, 2019 [234] | 16 | 1 | 4 | 1 | 72.7 | 717 | 68.9 | |||||
| van der Baan, 2020 [137] | 15 | 2 | 1,2 | 1 | 63.4 | 224 | 45 | |||||
| Yamagishi, 2014 [235] | 16 | 3 | 1 | 1 | 67 | 859 | 84 | 16 | ||||
| Yanaizumi, 2021 [236] | 17 | 3 | 2 | 1 | 108 | 6.5 | 12.9 | 80.6 | 93.5 | |||
| % Pain | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study | Quality | Continent a | Setting b | Cancer c | Mean Age | Sample | None | Mild | Moderate | ModSev d | Severe | Overall |
| Aguilar, 2017 [237] | 16 | 1 | 2 | 2 | 61.7 | 23 | 20.3 | |||||
| Alemayehu, 2018 [238] | 18 | 5 | 1,2 | 1 | 43.5 | 390 | 31 e | 69 | ||||
| Armstrong, 2016 [239] | 15 | 1 | 2 | 11 | 621 | 15.6 | ||||||
| Bacorro, 2017 [240] | 15 | 3 | 1,2 | 2 | 51.8 | 100 | 53 | 26 | 9 | 21 | 12 | 47 |
| Batalini, 2017 [241] | 16 | 4 | 2 | 1 | 59 | 277 | 40 | |||||
| Bauml, 2015 [242] | 16 | 1 | 2 | 5 | 60.5 | 203 | 78.7 e | 21.3 | ||||
| Beesley, 2016 [243] | 15 | 6 | 2 | 6 | 67 | 116 | 32 | |||||
| Bhattacharya, 2019 [244] | 16 | 2 | 2 | 5 | 957 | 10.5 | ||||||
| Bonhof, 2018 [245] | 16 | 2 | 2 | 9 | 64.8 | 98 | 37.5 | |||||
| Bouhassira, 2017 [246] | 18 | 2 | 2 | 1 | 61.4 | 509 | 28.2 | |||||
| Boyes, 2015 [247] | 17 | 6 | 2 | 10 | 311 | 12 | ||||||
| Braamse–a, 2014 [248] Braamse–b, 2014 [248] | 16 16 | 2 2 | 2 2 | 10 10 | 55.4 57.8 | 123 125 | 34.8 32.2 | |||||
| Braga-Neto, 2018 [249] | 16 | 4 | 2 | 6 | 207 | 83 | ||||||
| Bubis, 2020 [250] | 15 | 1 | 2,4 | 1 | 22,650 | 33 | ||||||
| Buckley, 2018 [251] | 16 | 1 | 1,2 | 10 | 82 | 60 | ||||||
| Cho–a, 2019 [252] Cho–b, 2019 [252] | 16 16 | 3 3 | 2 1 | 53.7 58.02 | 708 2581 | 60.6 44 | ||||||
| Clover, 2017 [253] | 15 | 6 | 2 | 1 | 62 | 9133 | 17 | |||||
| Daly, 2020 [254] | 15 | 2 | 5 | 1 | 1027 | 25.3 | ||||||
| Davies, 2021 [255] | 17 | 2 | 3 | 1 | 250 | 6.0 | 11.6 | 24.5 | 12.9 | 30.5 | ||
| Davis, 2018 [256] | 15 | 1 | 2 | 5 | 59.7 | 23,840 | 35.5 | 13.2 | ||||
| de Groef, 2016 [257] | 18 | 2 | 2 | 5 | 60.5 | 100 | 50 | |||||
| de Mello, 2020 [258] | 16 | 4 | 1 | 6 | 348 | 55.61 | ||||||
| de Oliveira, 2014 [259] | 18 | 1 | 2 | 5 | 300 | 36.7 | ||||||
| Deshields, 2014 [260] | 16 | 1 | 2 | 1 | 60.6 | 513 | 44 | |||||
| Deshields, 2017 [261] | 16 | 1 | 2 | 1 | 60.63 | 558 | 45 | |||||
| Dhingra, 2015 [262] | 17 | 1 | 2 | 1 | 62.3 | 1436 | 44.9 | |||||
| Donovan, 2014 [263] | 18 | 1 | 2 | 9 | 56 | 104 | 31.7 | |||||
| Doubova–a, 2021 [264] Doubova–b, 2021 [264] | 19 19 | 4 4 | 2 2 | 5 9 | 247 165 | 75.3 e 67.3 e | 24.7 32.7 | |||||
| Feiten, 2014 [265] | 16 | 2 | 2 | 5 | 730 | 34 | ||||||
| Fokdal, 2018 [266] | 18 | 1,2,3 | 2 | 9 | 914 | 13.4 | ||||||
| Giuliani, 2016 [267] | 15 | 1 | 2 | 4 | 89 | 21 | ||||||
| Götze, 2019 [268] | 16 | 2 | 2 | 10 | 75.6 | 200 | 34 | |||||
| Gough, 2017 [269] | 16 | 2 | 11 | 59 | 113 | 24 | 77 | |||||
| Guedes, 2018 [270] | 16 | 4 | 2 | 5 | 55.97 | 103 | 44.7 | 55.3 | ||||
| Honkanen, 2021 [271] | 16 | 2 | 2 | 5 | 56.9 | 121 | 35.5 | 14 | 49.5 | |||
| Horick, 2018 [272] | 18 | 1 | 2 | 1 | 309 | 45 | ||||||
| Huang, 2018 [273] | 17 | 3 | 1 | 6 | 59 | 300 | 39.7 | 25 | 25.3 | 35.5 | 10 | 60.3 |
| Hunnicutt–a, 2017 [274] Hunnicutt–b, 2017 [274] | 15 15 | 1 1 | 4 1 | 1 1 | 27,790 31,271 | 40.0 50.0 | 38.2 31.6 | 21.7 18.4 | 59.9 50.0 | |||
| Jesdale–a, 2020 [275] Jesdale–b, 2020 [275] Jesdale–c, 2020 [275] | 15 15 15 | 1 1 1 | 2 2 2 | 329,150 42,317 12,290 | 77.8 74.6 75.4 | |||||||
| Jewett, 2020 [276] | 17 | 1 | 2 | 9 | 59.9 | 355 | 25.1 | |||||
| Karawekpanyawong–a, 2021 [277] Karawekpanyawong–b, 2021 [277] | 16 16 | 3 3 | 2 2 | 9 9 | 52.7 55.8 | 27 173 | 23.51 46.3 | |||||
| Khan, 2021 [278] | 15 | 3 | 2 | 5 | 97 | 75.3 | 24.7 | |||||
| Kim, 2015 [279] | 15 | 3 | 2 | 5 | 52.1 | 827 | 56.5 | 1.1 | 43.5 | |||
| Kim–a, 2017 [280] Kim–b, 2017 [280] | 15 15 | 3 3 | 2 2 | 2 2 | 53.2 43.6 | 77 81 | 37.7 27.0 | |||||
| Lefkowits, 2014 [281] | 15 | 1 | 2 | 9 | 305 | 32 | 60.1 | |||||
| Liu, 2015 [282] | 16 | 1 | 5 | 5 | 51.7 | 97 | 53.6 | |||||
| Loh, 2018 [283] | 15 | 1 | 2 | 1 | 389 | 49.6 | ||||||
| Lu, 2017 [284] | 15 | 3 | 2 | 1 | 52.9 | 919 | 49.4 | |||||
| Mavros, 2020 [285] | 16 | 1 | 5 | 6 | 2168 | 39 | ||||||
| Mejdahl, 2015 [286] | 15 | 2 | 2 | 5 | 286 | 28 | ||||||
| Nakanotani, 2014 [287] | 15 | 3 | 2 | 1 | 57.6 | 807 | 17.6 | |||||
| Nappi, 2021 [288] | 15 | 2 | 2 | 5 | 58.4 | 175 | 65.9 | |||||
| Oosterling, 2016 [289] | 17 | 2 | 2 | 1 | 892 | 77 e | 23 | |||||
| Pandya, 2019 [290] | 16 | 1 | 1 | 1 | 81 | 359 | 56 | |||||
| Pinto, 2021 [291] | 15 | 5 | 1,3 | 1 | 46.1 | 294 | 33.3 | 62.6 | 29.3 | 83.7 | ||
| Ramsenthaler, 2016 [292] | 15 | 2 | 1,2 | 10 | 68.4 | 557 | 24 | 34 | 47.8 | 13.8 | 71.5 | |
| Rau, 2015 [293] | 19 | 3 | 2 | 1 | 57.47 | 2075 | 50.7 | |||||
| Reuter, 2019 [294] | 16 | 1 | 2 | 1 | 61.62 | 817 | 35.4 | |||||
| Rosario, 2019 [295] | 17 | 1 | 1 | 1 | 75 | 33 | 60 | |||||
| Saarelainen, 2014 [296] | 15 | 6 | 2 | 1 | 76.7 | 385 | 26 | |||||
| Sager, 2020 [297] | 18 | 1 | 2 | 1 | 65.31 | 123 | 26.8 | |||||
| Sakurai, 2019 [298] | 17 | 3 | 2,3 | 1 | 64.4 | 142 | 66.2 | |||||
| Sampogna, 2020 [299] | 16 | 2 | 2 | 11 | 44.3 | |||||||
| Sánchez Sánchez, 2020 [300] | 15 | 2 | 2 | 7 | 70.71 | 184 | 60.9 | 39.1 | 39.1 | |||
| Schreiber, 2021 [301] | 15 | 1 | 2 | 5 | 55.5 | 201 | 32 | |||||
| Shen, 2017 [302] | 16 | 3 | 2 | 1 | 57 | 2652 | 37.4 | 29.8 | 23.2 | 32.8 | 9.6 | 62.6 |
| Sloan–a, 2016 [303] Sloan–b, 2016 [303] | 16 16 | 1 1 | 2 2 | 4 4 | 66 66 | 296 1013 | 49.0 33.5 | |||||
| Smith, 2019 [304] | 15 | 1 | 2 | 5,6 | 59.7 | 2257 | 61.2 | |||||
| Tadele, 2015 [305] | 18 | 5 | 2 | 1 | 388 | 77.6 | ||||||
| Tegegn, 2017 [306] | 15 | 5 | 1 | 1 | 83 | 8.4 | 25.3 | 57.8 | 66.2 | 8.4 | 91.6 | |
| Tjong, 2021 [307] | 17 | 1 | 2 | 4 | 13,289 | 62 | ||||||
| Tung, 2019 [308] | 18 | 1 | 2 | 6 | 2623 | 61.8 | ||||||
| Valery, 2017 [309] | 15 | 6 | 1 | 82 | 10 | |||||||
| van Arsdale, 2016 [310] | 16 | 1 | 2 | 9 | 59 | 165 | 18.8 | |||||
| van den Brekel, 2020 [311] | 15 | 2 | 1 | 1 | 60 | 2144 | 28 | |||||
| Vistad, 2018 [312] | 16 | 2 | 9 | 61.9 | 82 | 56 | ||||||
| von Gruenigen, 2018 [313] | 17 | 1 | 2 | 9 | 63.6 | 65 | 69 | |||||
| Williams, 2020 [314] | 17 | 1 | 1 | 6 | 70.1 | 336 | 20.9 | |||||
| Xu, 2017 [315] | 15 | 3 | 2 | 11 | 43.5 | 142 | 30 | |||||
| N Studies | N cancer Patients | Overall Pain | |
|---|---|---|---|
| Group 1 | 18 | 3294 | 40.3% (95% CI 30.2–50.4) |
| Group 2 | 31 | 7995 | 47.8% (95% CI 39.4–56.1) |
| Group 3 | 19 | 8719 | 54.3% (95% CI 42.0–66.6) |
| Group 4 | 32 | 9118 | 50.3% (95% CI 42.5–58.0) |
| Group 5 | 77 | 59,766 | 35.8% (95% CI 31.5–40.1) |
| Group 6 | 15 | 33,162 | 55.2% (95% CI 39.2–71.3) |
| Group 7 | 66 | 508,827 | 45.0% (95% CI 39.8–50.1) |
| Group 8 | 81 | 25,832 | 50.3% (95% CI 44.6–56.1) |
| Group 9 | 34 | 41,881 | 54.6% (95% CI 43.8–65.5) |
| Moderate–Severe Pain | |||
| Group 1 | 9 | 1895 | 33.1% (95% CI 22.0–44.2) |
| Group 2 | 12 | 5483 | 27.8% (95% CI 6.7–48.8) |
| Group 3 | 11 | 8057 | 39.1% (95% CI 30.0–48.1) |
| Group 4 | 16 | 4966 | 25.2% (95% CI 19.0–31.4) |
| Group 5 | 30 | 24,490 | 22.8% (95% CI 19.0–26.7) |
| Group 6 | 7 | 35,319 | 43.3% (95% CI 19.7–66.9) |
| Group 7 | 22 | 107,128 | 34.2% (95% CI 27.6–40.8) |
| Group 8 | 39 | 18,506 | 31.0% (95% CI 22.7–39.3) |
| Group 9 | 18 | 43,376 | 40.7% (95% CI 28.5–52.9) |
| Determinant | β (95% CI) | p-Value |
|---|---|---|
| Age (years) | ||
| 18–49 | 0.45 (0.37 to 0.54) | ref. |
| 50–59 | 0.01 (–0.09 to 0.11) | 0.787 |
| 60–69 | –0.03 (–0.13 to 0.07) | 0.570 |
| 70+ | 0.01 (–0.12 to 0.15) | 0.843 |
| Type of cancer | ||
| Prostate | 0.25 (0.08 to 0.41) | ref. |
| Head and neck | 0.16 (–0.04 to 0.35) | 0.116 |
| Lung | 0.22 (0.01 to 0.43) | 0.039 |
| Breast | 0.19 (0.01 to 0.36) | 0.036 |
| Gastro-intestinal | 0.18 (–0.01 to 0.36) | 0.061 |
| Gynaecological | 0.11 (–0.08 to 0.30) | 0.253 |
| Haematological | 0.21 (0.02 to 0.40) | 0.034 |
| Ethnicity | ||
| Caucasian | 0.38 (0.18 to 0.59) | ref. |
| Black | 0.36 (–0.15 to 0.87) | 0.144 |
| Asian | 0.17 (–0.12 to 0.45) | 0.219 |
| Hispanic | 0.39 (–0.01 to 0.78) | 0.054 |
| Performance status | ||
| ECOG 2 | 0.68 (0.43 to 0.94) | ref. |
| ECOG 0 | –0.28 (–0.74 to 0.17) | 0.198 |
| ECOG 1 | –0.05 (–0.35 to 0.25) | 0.733 |
| Data collection method | ||
| Questionnaire patient | 0.43 (0.40 to 0.45) | ref. |
| Interview patient | 0.07 (–0.02 to 0.16) | 0.106 |
| Medical record | 0.19 (0.05 to 0.32) | 0.007 |
| Recall period | ||
| Point | 0.50 (0.45 to 0.55) | ref. |
| Week(s) | –0.08 (–0.14 to –0.02) | 0.013 |
| Month(s) | –0.18 (–0.28 to –0.07) | 0.001 |
| Setting | ||
| Outpatient | 0.42 (0.39 to 0.45) | ref. |
| Inpatient | 0.08 (–0.02 to 0.18) | 0.115 |
| Palliative care setting | 0.16 (0.01 to 0.32) | 0.040 |
| Continent of origin | ||
| Europe | 0.39 (0.36 to 0.43) | ref. |
| North America | 0.06 (–0.00 to 0.12) | 0.068 |
| South America | 0.15 (0.01 to 0.29) | 0.033 |
| Asia | 0.08 (0.01 to 0.14) | 0.016 |
| Africa | 0.43 (0.25 to 0.62) | 0.000 |
| Australia/New Zealand | 0.06 (–0.03 to 0.16) | 0.193 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Snijders, R.A.H.; Brom, L.; Theunissen, M.; van den Beuken-van Everdingen, M.H.J. Update on Prevalence of Pain in Patients with Cancer 2022: A Systematic Literature Review and Meta-Analysis. Cancers 2023, 15, 591. https://doi.org/10.3390/cancers15030591
Snijders RAH, Brom L, Theunissen M, van den Beuken-van Everdingen MHJ. Update on Prevalence of Pain in Patients with Cancer 2022: A Systematic Literature Review and Meta-Analysis. Cancers. 2023; 15(3):591. https://doi.org/10.3390/cancers15030591
Chicago/Turabian StyleSnijders, Rolf A. H., Linda Brom, Maurice Theunissen, and Marieke H. J. van den Beuken-van Everdingen. 2023. "Update on Prevalence of Pain in Patients with Cancer 2022: A Systematic Literature Review and Meta-Analysis" Cancers 15, no. 3: 591. https://doi.org/10.3390/cancers15030591
APA StyleSnijders, R. A. H., Brom, L., Theunissen, M., & van den Beuken-van Everdingen, M. H. J. (2023). Update on Prevalence of Pain in Patients with Cancer 2022: A Systematic Literature Review and Meta-Analysis. Cancers, 15(3), 591. https://doi.org/10.3390/cancers15030591





