Pigmentation and Scaring Management after Hypodermoclysis, a Case Report
Abstract
:1. Introduction
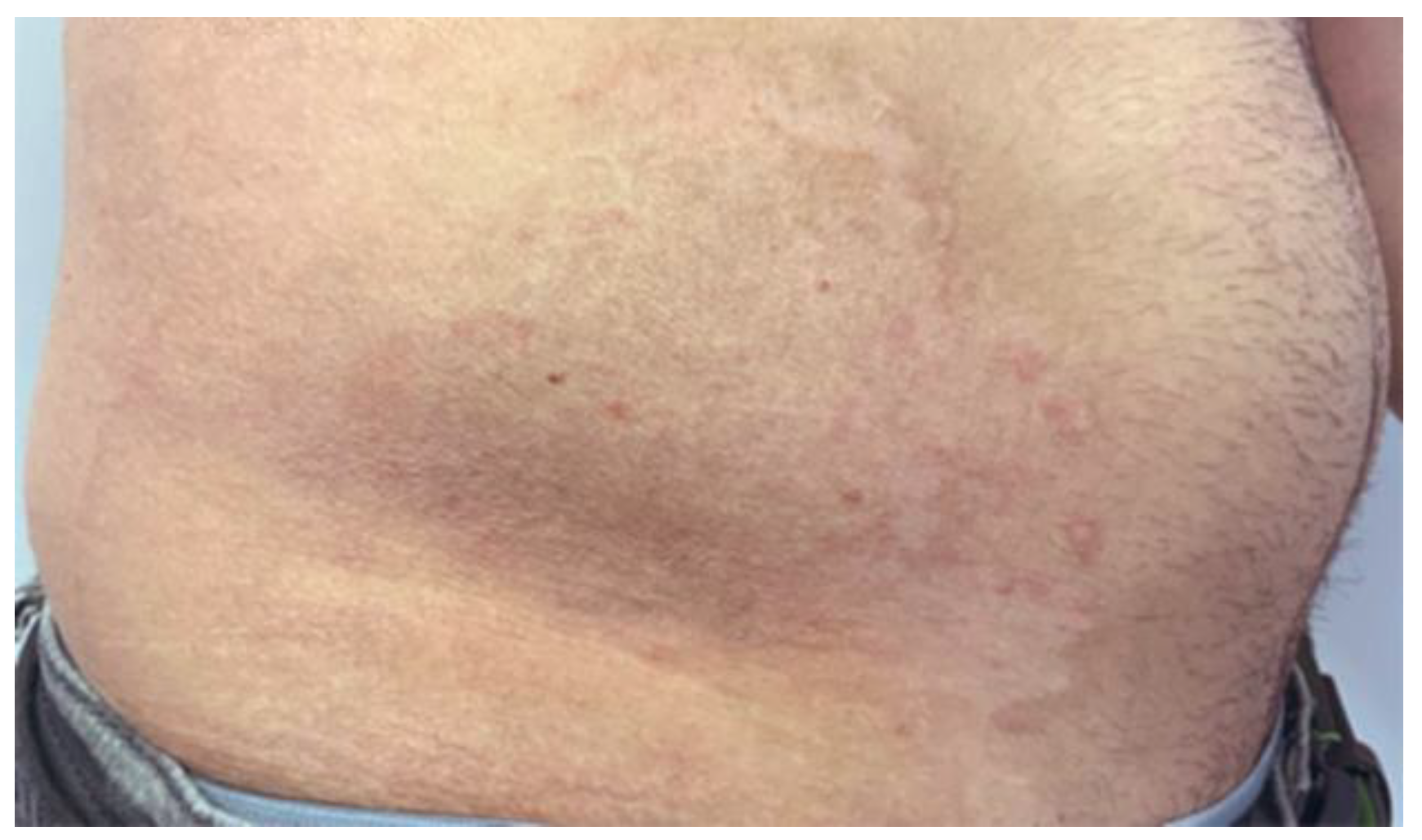
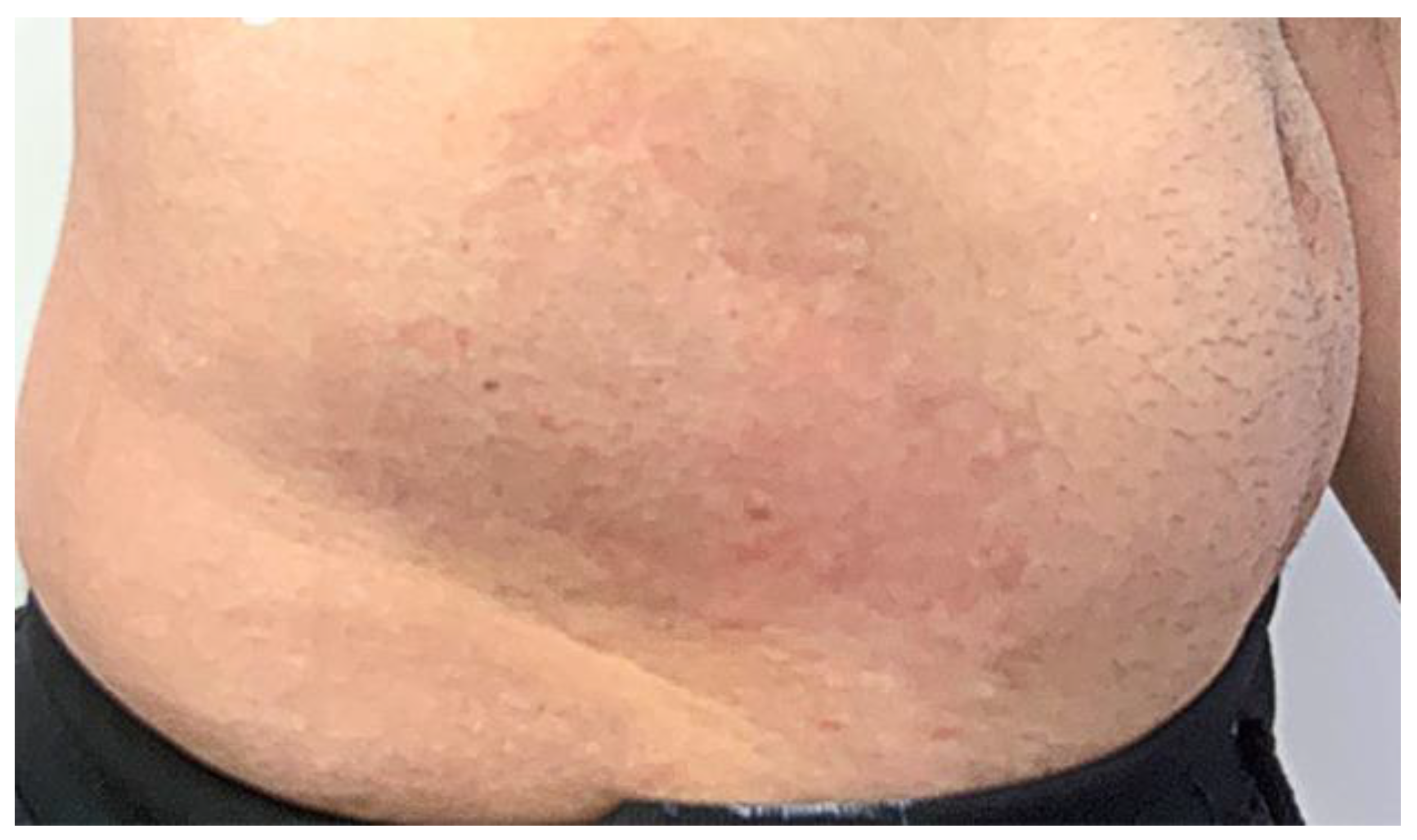
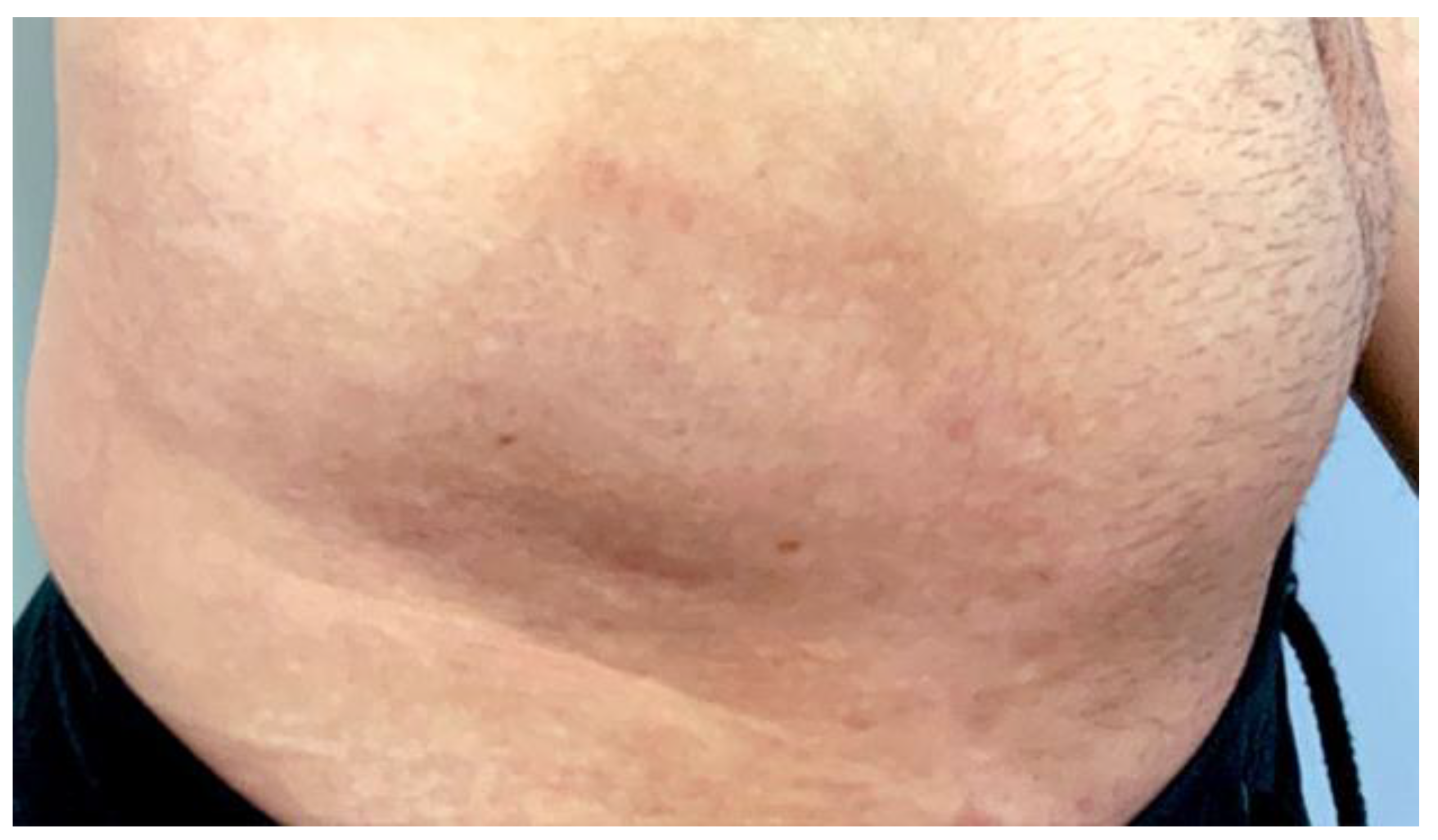
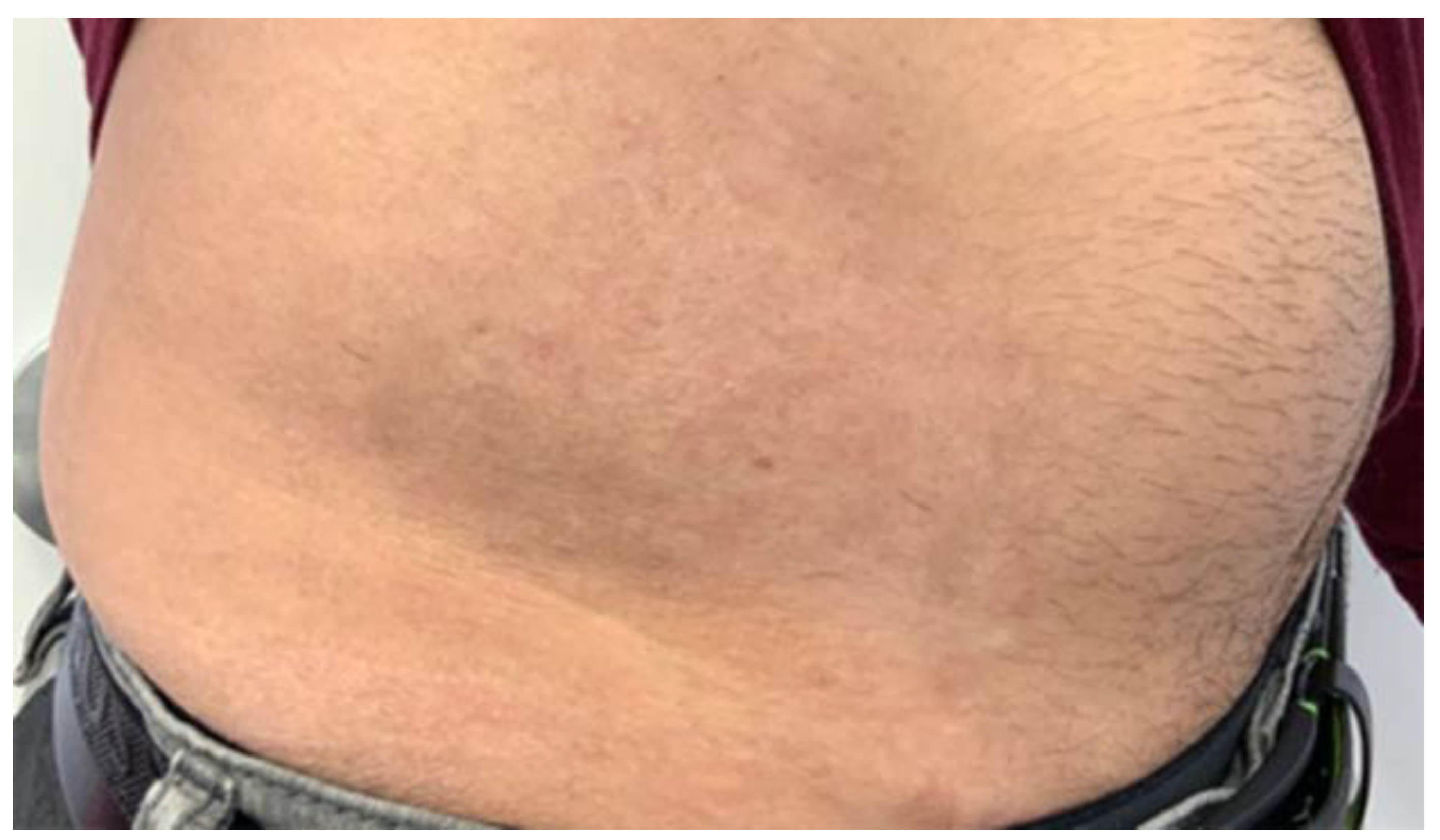
2. Case Report
2.1. Lesion Assessment
2.2. Preparation Phase
2.3. Treatment Phase
3. Stage One
4. Stage Two
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Marks, L.R.; Nolan, N.S.; Liang, S.Y.; Durkin, M.J.; Weimer, M.B. Infectious Complications of Injection Drug Use. Med. Clin. 2022, 106, 187–200. [Google Scholar] [CrossRef]
- Robertson, R.; Broers, B.; Harris, M. Injecting drug use, the skin and vasculature. Addiction 2021, 116, 1914–1924. [Google Scholar] [CrossRef] [PubMed]
- Richardson, T.; Kerr, D. Skin-related complications of insulin therapy. Am. J. Clin. Dermatol. 2003, 4, 661–667. [Google Scholar] [CrossRef]
- Binder, E.; Lange, O.; Edlinger, M.; Meraner, D.; Abt, D.; Moser, C.; Steichen, E.; Hofer, S.E. Frequency of dermatological side effects of continuous subcutaneous insulin infusion in children and adolescents with type 1 diabetes. Exp. Clin. Endocrinol. Diabetes 2015, 123, 260–264. [Google Scholar] [CrossRef]
- Berg, A.K.; Olsen, B.S.; Thyssen, J.P.; Zachariae, C.; Simonsen, A.B.; Pilgaard, K.; Svensson, J. High frequencies of dermatological complications in children using insulin pumps or sensors. Pediatric Diabetes 2018, 19, 733–740. [Google Scholar] [CrossRef]
- Conwell, L.S.; Pope, E.; Artiles, A.M.; Mohanta, A.; Daneman, A.; Daneman, D. Dermatological complications of continuous subcutaneous insulin infusion in children and adolescents. J. Pediatrics 2008, 152, 622–628. [Google Scholar] [CrossRef]
- Al Hallak, K.; Tomi, S.; Omran, D. Q-switch nanosecond laser as innovative and instant management for bruises discoloration, a case report. J. Cosmet. Laser Ther. 2021, 23, 19–23. [Google Scholar] [CrossRef]
- Ogawa, R. The Most Current Algorithms for the Treatment and Prevention of Hypertrophic Scars and Keloids: A 2020 Update of the Algorithms Published 10 Years Ago. Plast. Reconstr. Surg. 2022, 149, 79e–94e. [Google Scholar] [CrossRef] [PubMed]
- Sarkar, R.; Choubey, V.; Devadasan, S. Hyperpigmentary Skin Disorders. Atlas Dermatol. Dermatopathol. Venereol. Inflamm. Dermatoses 2022, 11, 223. [Google Scholar]
- Nestor, M.S.; Fischer, D.; Arnold, D.; Matin, T.; Jones, J.L. Lasers and Aesthetic Devices: Skin Resurfacing, Tattoo Removal, and Body Contouring. In Tips and Tricks in Plastic Surgery; Springer: Cham, Switzerland, 2022; pp. 541–552. [Google Scholar]
- Gaffey, M.M.; Johnson, A.B. Laser Treatment of Pigmented Lesions; StatPearls: Treasure Island, FL, USA, 2020. [Google Scholar]
- Alhallak, K.; Omran, D.; Tomi, S.; Abdulhafid, A. Skin, Light and their Interactions, an In-Depth Review for Modern Light-Based Skin Therapies. J. Clin. Derm. Ther. 2021, 7, 2. [Google Scholar] [CrossRef]
- Jagdeo, J.; Austin, E.; Mamalis, A.; Wong, C.; Ho, D.; Siegel, D.M. Light-emitting diodes in dermatology: A systematic review of randomized controlled trials. Lasers Surg. Med. 2018, 50, 613–628. [Google Scholar] [CrossRef]
- Busche, M.N.; Thraen, A.-C.J.; Gohritz, A.; Rennekampff, H.-O.; Vogt, P.M. Burn scar evaluation using the cutometer® MPA 580 in comparison to “patient and observer scar assessment scale” and “vancouver scar scale”. J. Burn. Care Res. 2018, 39, 516–526. [Google Scholar] [CrossRef]
- Moran, B.; Humphrey, S.; Seal, A.; Berkowitz, J.; Zloty, D. Photographic assessment of postsurgical facial scars epidermally sutured with rapidly absorbable polyglactin 910 or nylon: A randomized clinical trial. J. Am. Acad. Dermatol. 2020, 83, 1395–1399. [Google Scholar] [CrossRef]
- Oosterhoff, T.C.; Beekman, V.K.; van der List, J.P.; Niessen, F.B. Laser treatment of specific scar characteristics in hypertrophic scars and keloid: A systematic review. J. Plast. Reconstr. Aesthetic Surg. 2021, 74, 48–64. [Google Scholar] [CrossRef] [PubMed]
- Wu, D.C.; Goldman, M.P.; Wat, H.; Chan, H.H. A systematic review of picosecond laser in dermatology: Evidence and recommendations. Lasers Surg. Med. 2021, 53, 9–49. [Google Scholar] [CrossRef]
- Conforti, C.; Vezzoni, R.; Giuffrida, R.; Fai, A.; Fadda, S.; Marangi, G.F.; Persichetti, P.; Piccolo, D.; Segreto, F.; Zalaudek, I.; et al. An overview on the role of CO2 laser in general dermatology. Dermatol. Ther. 2021, 34, e14692. [Google Scholar] [CrossRef]
- Passeron, T.; Genedy, R.; Salah, L.; Fusade, T.; Kositratna, G.; Laubach, H.J.; Marini, L.; Badawi, A. Laser treatment of hyperpigmented lesions: Position statement of the European Society of Laser in Dermatology. J. Eur. Acad. Dermatol. Venereol. 2019, 33, 987–1005. [Google Scholar] [CrossRef]
- Fratila, A.; Gauglitz, G.; Strohbücker, A.; Radu, D. Selective photothermolysis of spider veins and reticular varices with the long-pulsed Nd: YAG laser. Phlebologie 2020, 49, 16–22. [Google Scholar]
- Ungaksornpairote, C.; Manuskiatti, W.; Junsuwan, N.; Wanitphakdeedecha, R. A prospective, split-face, randomized study comparing picosecond to Q-switched Nd: YAG laser for treatment of epidermal and dermal pigmented lesions in Asians. Dermatol. Surg. 2020, 46, 1671–1675. [Google Scholar] [CrossRef] [PubMed]
- Beyzaee, A.M.; Patil, A.; Goldust, M.; Moslemi, M.; Kazeminejad, A.; Rokni, G.R. Comparative Efficacy of Fractional CO2 Laser and Q-Switched Nd: YAG Laser in Combination Therapy with Tranexamic Acid in Refractory Melasma: Results of a Prospective Clinical Trial. Cosmetics 2021, 8, 37. [Google Scholar] [CrossRef]
- Robredo, I.G.C. Q-switched 1064 nm Nd: YAG laser in treating axillary hyperpigmentation in Filipino women with skin types IV–V. J. Drugs Dermatol. 2020, 19, 66–69. [Google Scholar] [CrossRef] [PubMed]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alhallak, K.; Abdulhafid, A.; Tomi, S.; Omran, D. Pigmentation and Scaring Management after Hypodermoclysis, a Case Report. Cosmetics 2022, 9, 10. https://doi.org/10.3390/cosmetics9010010
Alhallak K, Abdulhafid A, Tomi S, Omran D. Pigmentation and Scaring Management after Hypodermoclysis, a Case Report. Cosmetics. 2022; 9(1):10. https://doi.org/10.3390/cosmetics9010010
Chicago/Turabian StyleAlhallak, Kamal, Adel Abdulhafid, Salem Tomi, and Dima Omran. 2022. "Pigmentation and Scaring Management after Hypodermoclysis, a Case Report" Cosmetics 9, no. 1: 10. https://doi.org/10.3390/cosmetics9010010
APA StyleAlhallak, K., Abdulhafid, A., Tomi, S., & Omran, D. (2022). Pigmentation and Scaring Management after Hypodermoclysis, a Case Report. Cosmetics, 9(1), 10. https://doi.org/10.3390/cosmetics9010010




