Abstract
Retinol is a compound used in many skin care formulations to act against skin conditions like acne, wrinkles, psoriasis, and ichthyosis. While retinol is used as an active ingredient, its efficacy is limited by an extreme sensitivity to light and temperature. Retinol can also generate toxicity at high concentrations. Microencapsulation is an alternative method to help overcome these issues. In this study, we develop a new encapsulation of retinol by solvent evaporation using a cationic polymer. We show that our particles have a narrow size distribution (350 nm), can encapsulate retinol with high efficiency, and protect it from oxidation for at least eight weeks. Finally, to demonstrate that the release of retinol from the particles can be controlled, we performed a kinetic study and showed that the particle releases the drug during 18 h.
1. Introduction
The past decades have seen a growing interest in applications of drug delivery systems, especially in the fields of pharmaceutics, cosmetics, and dermo-cosmetics, where drug administration, long-lasting effect, and toxicologic studies are crucial aspects. Many systems have been investigated allowing controlled release, targeting, and/or penetration enhancement of the active ingredient. Microparticles (MPs) figure among these delivery systems and are prepared mainly to obtain prolonged or controlled drug delivery, to improve bioavailability, stability, and targeting drug to specific sites. Microparticles can also offer advantages such, as limiting fluctuations within the therapeutic range, reducing side effects, decreasing administration frequency, and improving patient compliance [1,2,3,4,5,6,7,8].
Retinol is a derivative of vitamin A, often used as an active ingredient in many skin care formulations to reduce wrinkles, acne, UV-induced aging spots, or specific skin disorder (psoriasis, ichthyosis, etc.). However, retinol suffers from poor solubility in water and is highly sensitive to light and oxygen, leading to rapid degradation. Thereby, it is difficult to incorporate retinol into stable and effective formulations. It is also important to note that retinol has a narrow therapeutic window, leading it to be ineffective at low concentrations and toxic at high concentrations [5,9]. As a result, retinol is a good candidate for drug targeting using encapsulation processes.
Depending on the solubility of the drug, several processes can be achieved to prepare micro and nanoparticles. For example, previous work has been done on retinol encapsulation to prevent this degradation using sol–gel [10,11], solid lipid particles (SLNs) [12,13], or a complex formation [14] process. However, to the best of our knowledge, none of these processes has been carried out by evaporation of solvents.
The emulsification with solvent evaporation and/or extraction method is one of the most versatile. Indeed, solvent evaporation is one of the few processes that can encapsulate hydrophilic or lipophilic agents, by adjusting the emulsification process. For a lipophilic drug, like retinol, the drug and a polymer are dissolved in a volatile organic phase, which is dispersed in an aqueous phase to form an oil-in-water (O/W) emulsion. Then, the organic solvent diffuses into the external phase and evaporates, leading to polymer desolvation, droplet solidification, and drug encapsulation [3,15,16,17].
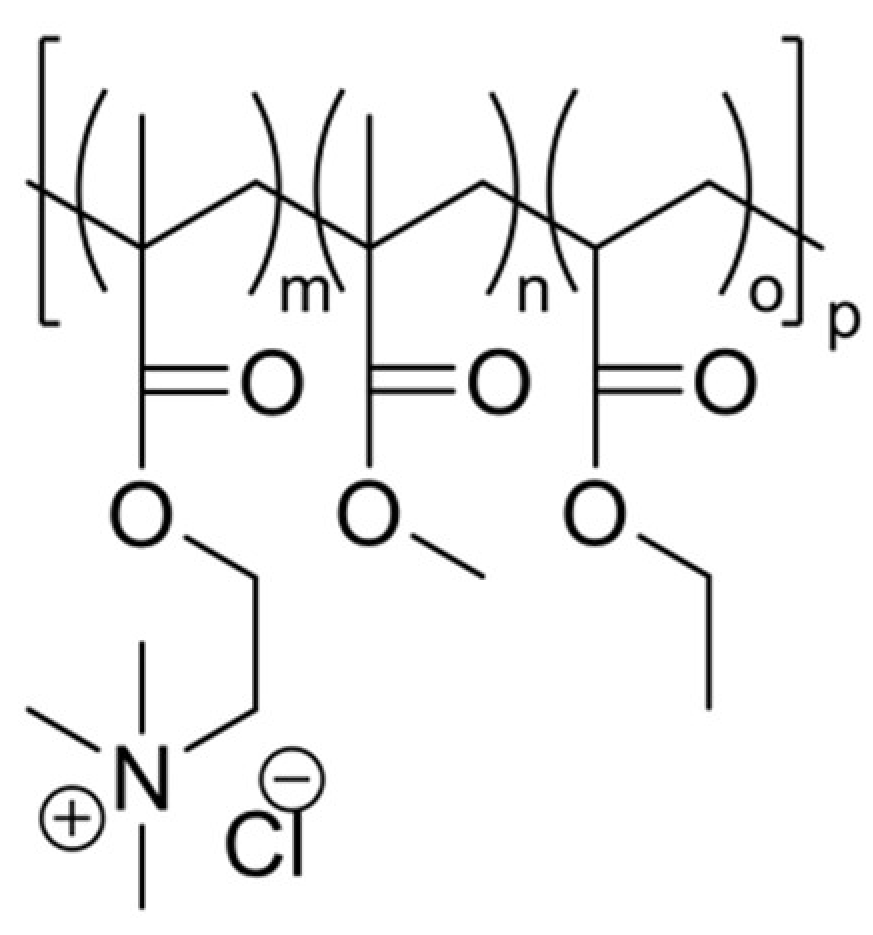
Previous studies have shown the interest in cationic particles for skin or hair formulation: the affinity of the particles with the treated anionic surface (the skin) conducts to a long-lasting effect. Eudragit RS 100 is a cationic copolymer of Poly(ethyl acrylate-co-methyl methacrylate-co-2-(trimethylammonio)ethyl methacrylate chloride) 1:2:0.1 (Figure 1). This copolymer is insoluble in aqueous media, but it is permeable and has a pH-independent release profile. The permeability of Eudragit is due to the presence of quaternary ammonium groups in its structure (between 4.4 and 6.8%) [17,18]. Eudragit RS 100 is commonly used for enteric coating of tablets and has been widely employed in the pharmaceutical field to improve controlled-release drug forms [19,20]. However, its positive charge presents a specific affinity with the skin and hair, which can allow longer residence time on the delivery site [21].
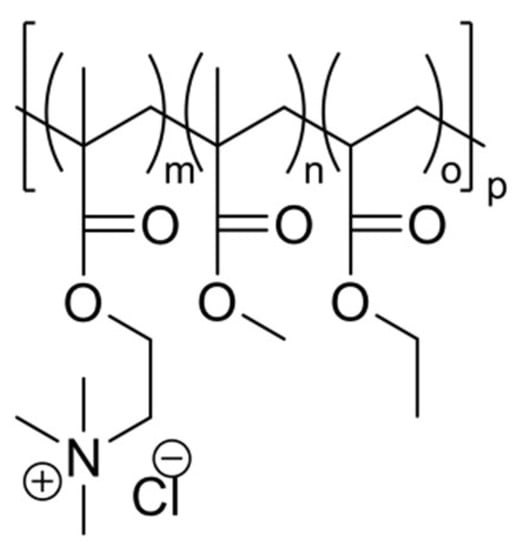
Figure 1.
Chemical structure of Eudragit RS 100.
The aim of this study was to encapsulate retinol in cationic copolymer (Eudragit RS 100) nanoparticles (MPs), as a novel delivery system for skin care applications.
2. Materials and Methods
2.1. Materials
Synthetic Retinol, >95%; CAS Number 68-26-8, was purchased from Sigma and Eudragit RS 100 was obtained from Evonik (Evonik Pharma, Germany), and both were used as received. Ethyl acetate was provided by Merck Chemical (Merck, France). Deionized water (Milli-Q) was purified by Millipore Q-T M system. All other chemicals were used as received. All solutions were made fresh before use.
2.2. Preparation of MPs
Nanoparticles were prepared by the emulsion solvent evaporation method. The drug–polymer solutions were prepared by dissolving 1.5 g of Eudragit RS 100 and retinol (between 0.1 and 1 g) into 20 mL of ethyl acetate using a magnetic stirrer. This mixture was poured into deionized water (50 mL) and stirred (Ultra Turax at 13,500 rpm, IKA, Wilmington, USA) for 15 min. The obtained emulsion was added to 150 mL of deionized water, stirred at 500 rpm for 180 min. Nanoparticles were isolated by centrifugation and lyophilized using a Sublimat 5 device (Labconco, Kansas City, USA).
2.3. Characterization of Nanoparticles
2.3.1. Size, Zeta, and Morphology
Nanoparticles’ size distribution and zeta were measured by Dynamic Light Scattering (DLS) (Zetasizer Nano ZS, Malvern Instruments, Montreal, Canada). Surface morphology was examined by scanning electron microscopy. The samples were coated with Au-Pd for 3 min using a Baltec MED020 (Baltec MED020, Leica, Concord, Ontario) system and examined using a JSM-6300F (JSM-630F, Jeol, Peabody, USA) microscope operating in secondary electron mode at 15 KeV accelerating voltage.
2.3.2. Encapsulation Yields
Encapsulation yields were measured by centrifuging loaded-nanoparticles at 10,000 rpm for 15 min, in order to isolate MPs from the supernatant. Retinol was extracted from particles using acetonitrile in a sonication bath (1 h at room temperature). Retinol was quantitatively analyzed by reverse-phase chromatography (Waters Symmetry C18 4.6 × 150 mm, 3.5 µm) on a Agilent 1100 HPLC system (HPLC 1100 series, Agilent, Santa Clara, USA) and was quantified by UV absorbance at 325 nm [22]. Samples were injected at 1 mL/min with an isocratic mobile phase (90:10 acetonitrile/water) for 15 min. Under these conditions, Retinol showed a limit of quantization of 1.10−3 g/L and a retention time of 8.2 min. The calibration curve was linear in the concentration range of 1.2–5.10−3 g/L, R² = 0.99.
The encapsulation yield was determined as the amount of recovered retinol into MPs divided by the initial amount of retinol employed (Equation (1)).
2.3.3. Drug Release from Nanoparticles
Drug release tests were performed by adding 2 mL of MPs into 20 mL of synthetic sweat solution. The synthetic sweat solution (Table 1) was prepared according to standard JIS L 0848 [23]. Each solution was stirred using a magnetic stirrer at 250 rpm. The temperature was controlled to 37 °C. Aliquots were withdrawn at predetermined time intervals and centrifuged at 10,000 rpm for 15 min to separate nanoparticles from supernatant. MPs and supernatant were analyzed by HPLC, using the method described above.

Table 1.
Synthetic sweat composition.
3. Results
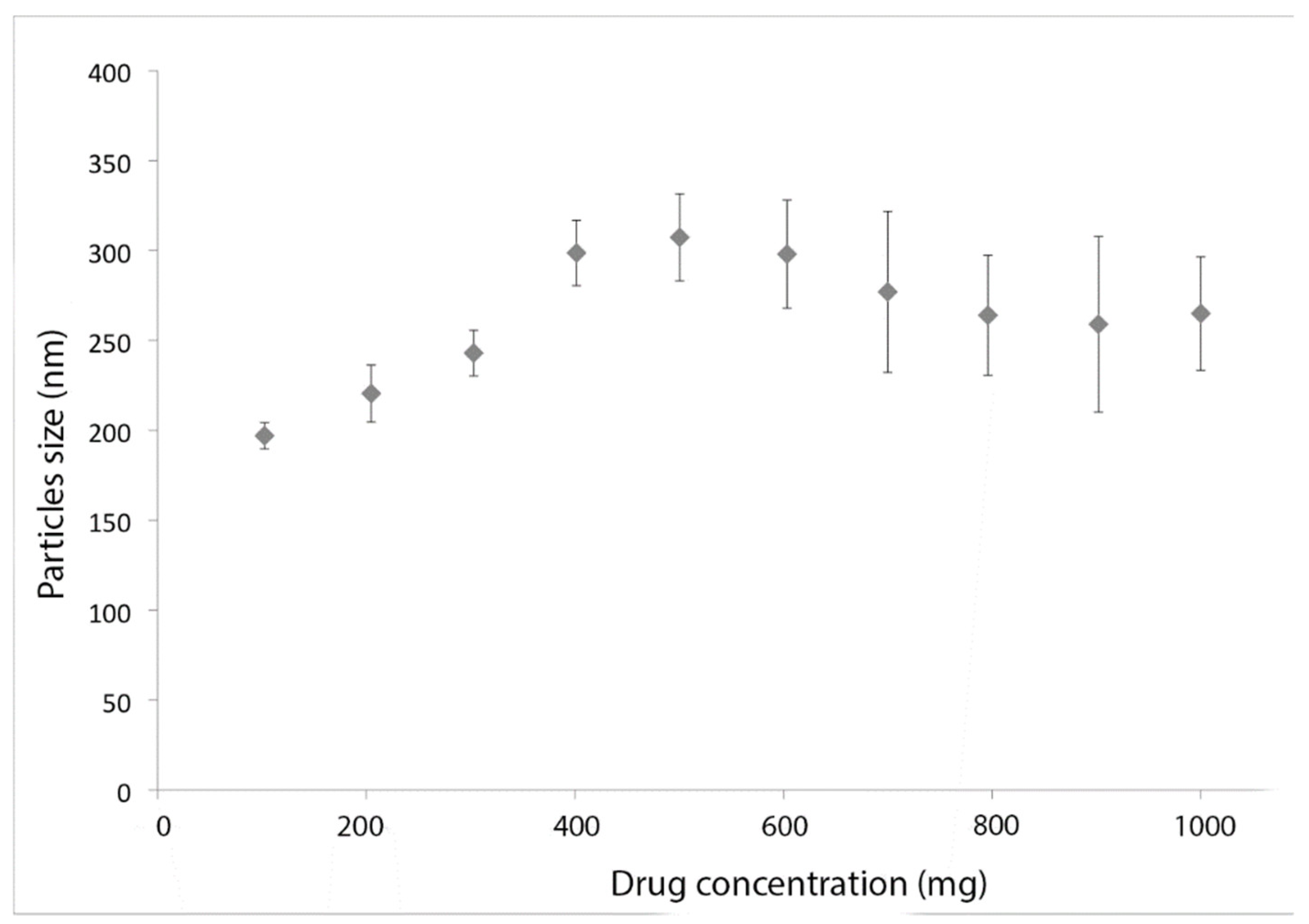
3.1. Influence of Retinol Concentration
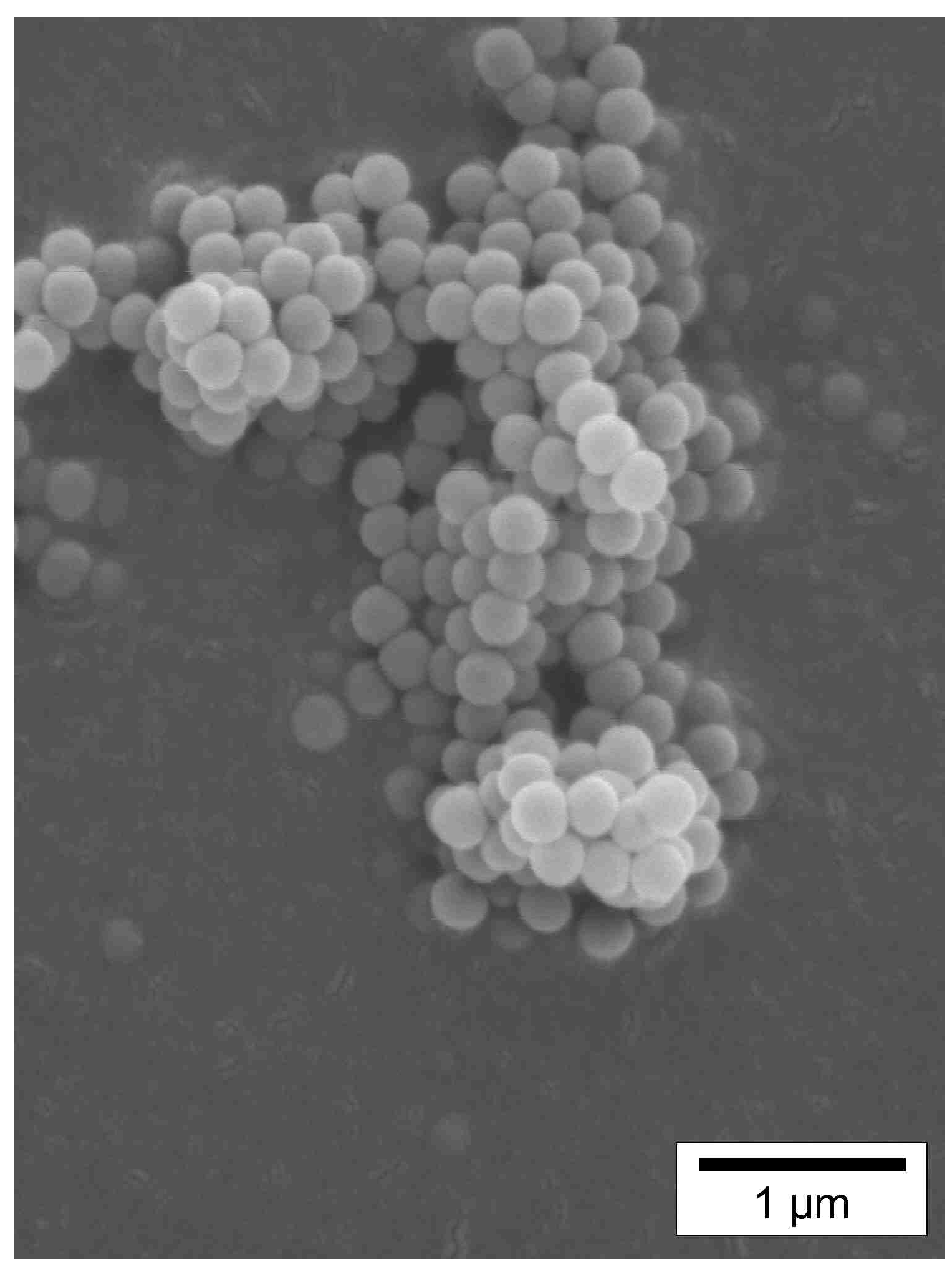
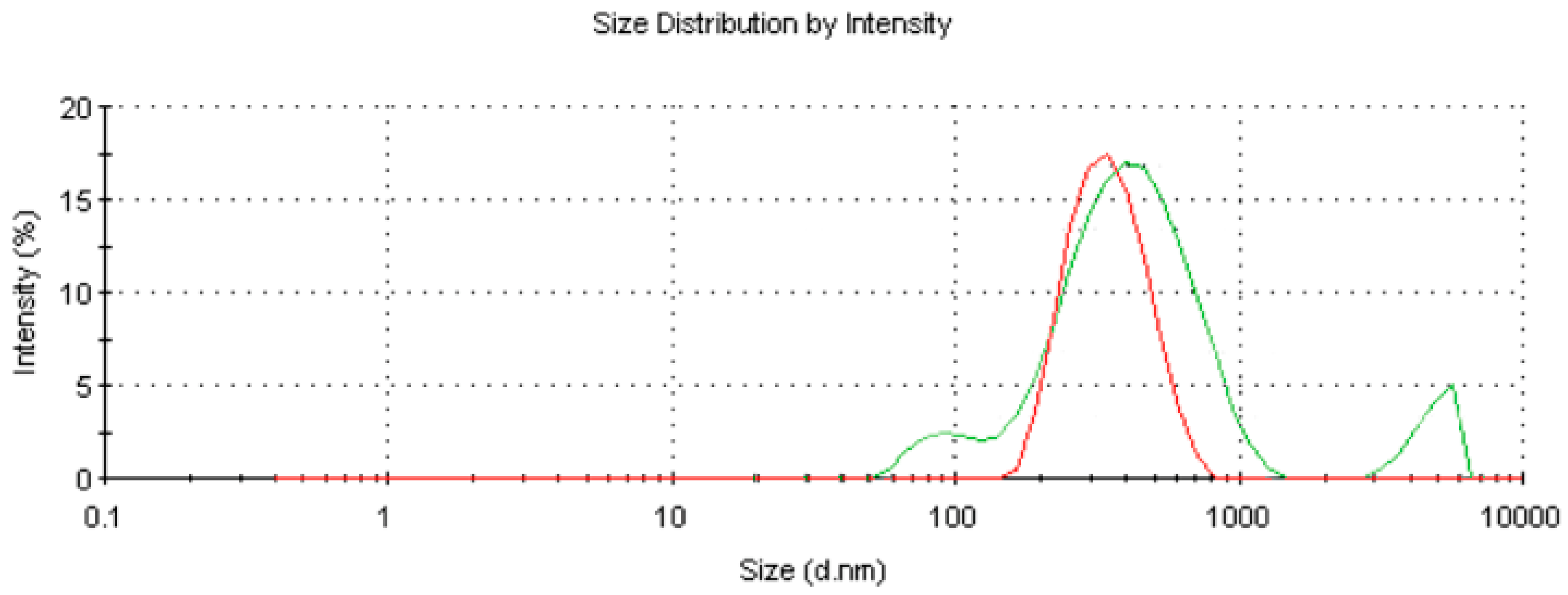
The influence of retinol concentration on particle size was first investigated. Several formulations were prepared and are described in Table 2. The results show (Figure 2) an increase in particle size (d average) with the amount of drug until 500 mg of retinol. For higher concentrations, the size decreased slightly and the standard deviation associated with the particle size increased. This phenomenon is due to an excessive load of active ingredient. According to Li et al. [23], a critical mass of active ingredient increases the risk of drug leakage due to a limited space inside the nanoparticles, leading to a reduction of particles size. The theoretical limit, in the emulsion diffusion process, is approximately 50% w/w [23]. The maximum drug amount loaded here seemed to be achieved for F-5/6 or about 40%–50% by weight of the amount of polymer. This result is confirmed by size distribution measurements, since F-5 exhibited a single population centered on 317 nm (Figure 3), while F-7 showed 3 populations centered on 93, 446, and 4771 nm (Figure 4). The zeta potential of the formulations is between 59,5 and 73,5 mV, which confirms the cationic charge of the particle. The size and zeta potential of each formulation is summarized in Table 3.

Table 2.
Compositions of the prepared nanoparticles.
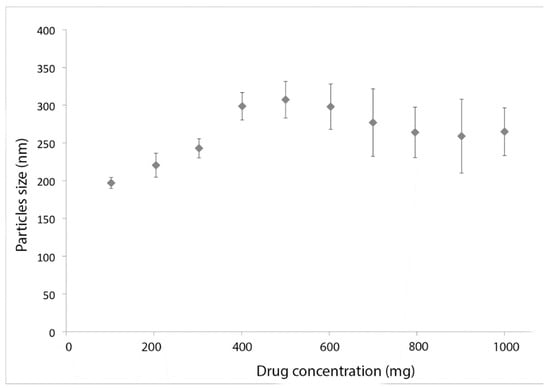
Figure 2.
Influence of retinol amount on particle size (d average).
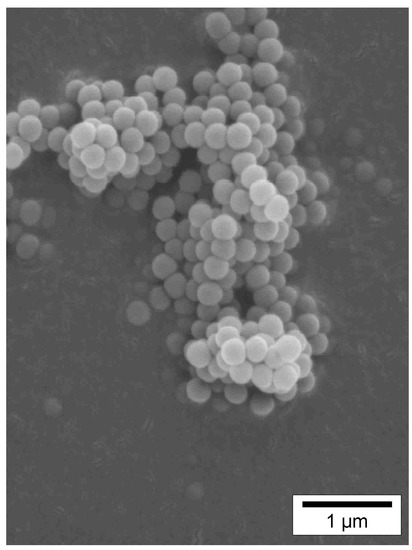
Figure 3.
Electronic microscopy of formulation F-5.
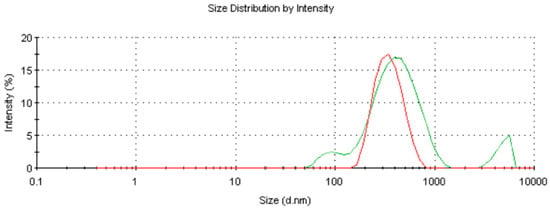
Figure 4.
F-5 (red) and F-7 (green) size distribution.

Table 3.
Size and zeta potential of each formulation.
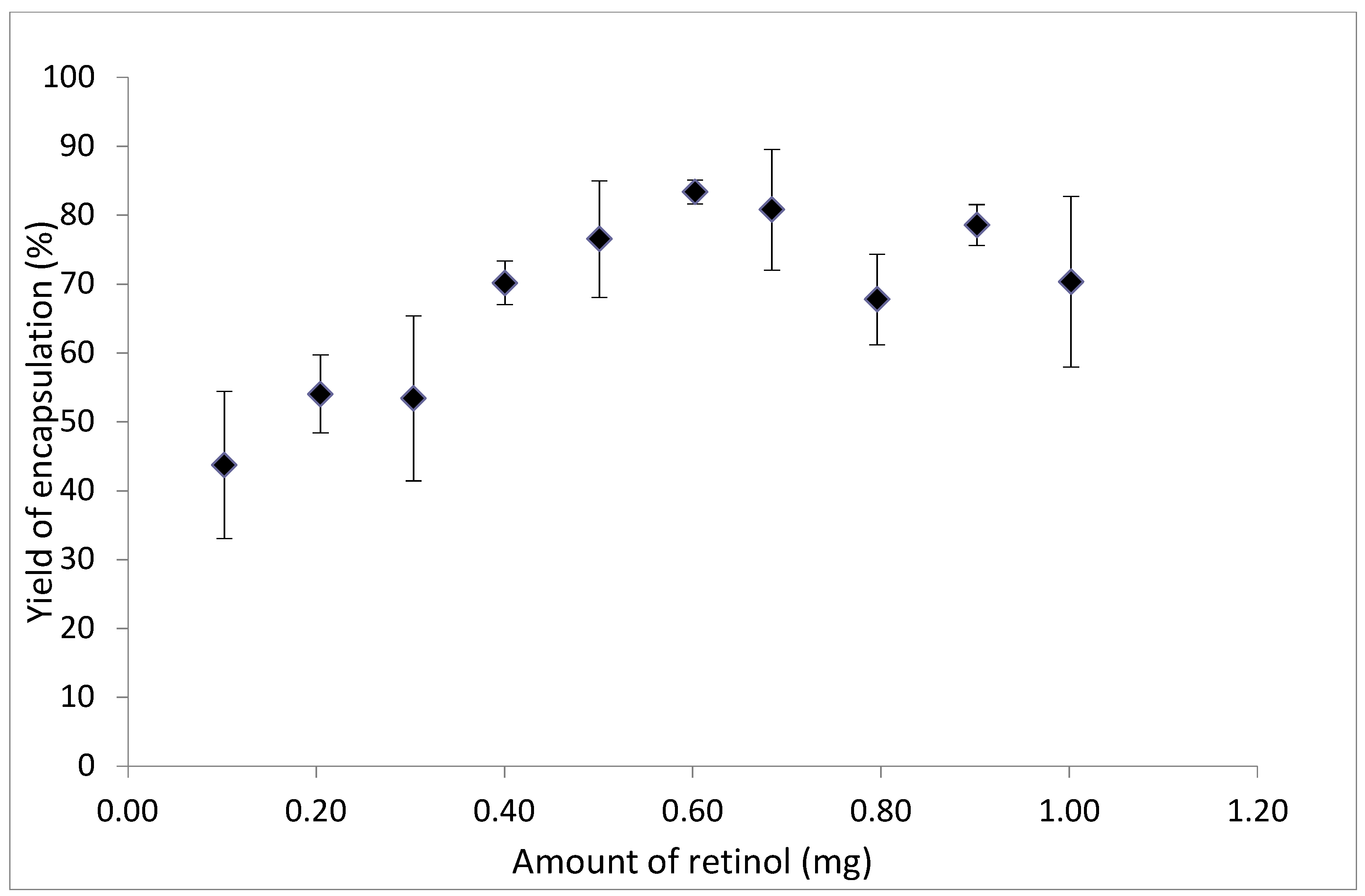
3.2. Encapsulation Efficiency
The evolution of encapsulation efficiency was calculated as a function of the initial mass of retinol, using the method described above. The encapsulation efficiency increased from 40% to 85% for a retinol mass ranging from 100 to 600 mg (Figure 5). For higher retinol concentrations, the yield decreased. The maximum encapsulation efficiency of retinol in nanoparticles is 86.3% and is reached for formulation F-6. Accounting for this efficiency, the mass of retinol in the particles is about 34.5% by weight of the polymer. This result is close to the theorical limit of 40% for encapsulation by solvent evaporation process [24]. Past this value, the encapsulation yield decreases until 60% for F-8.
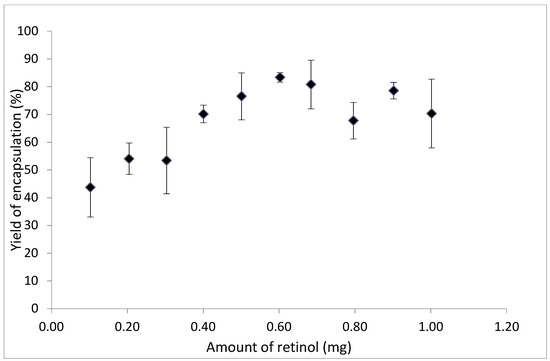
Figure 5.
Encapsulation efficiency as a function of retinol amount.
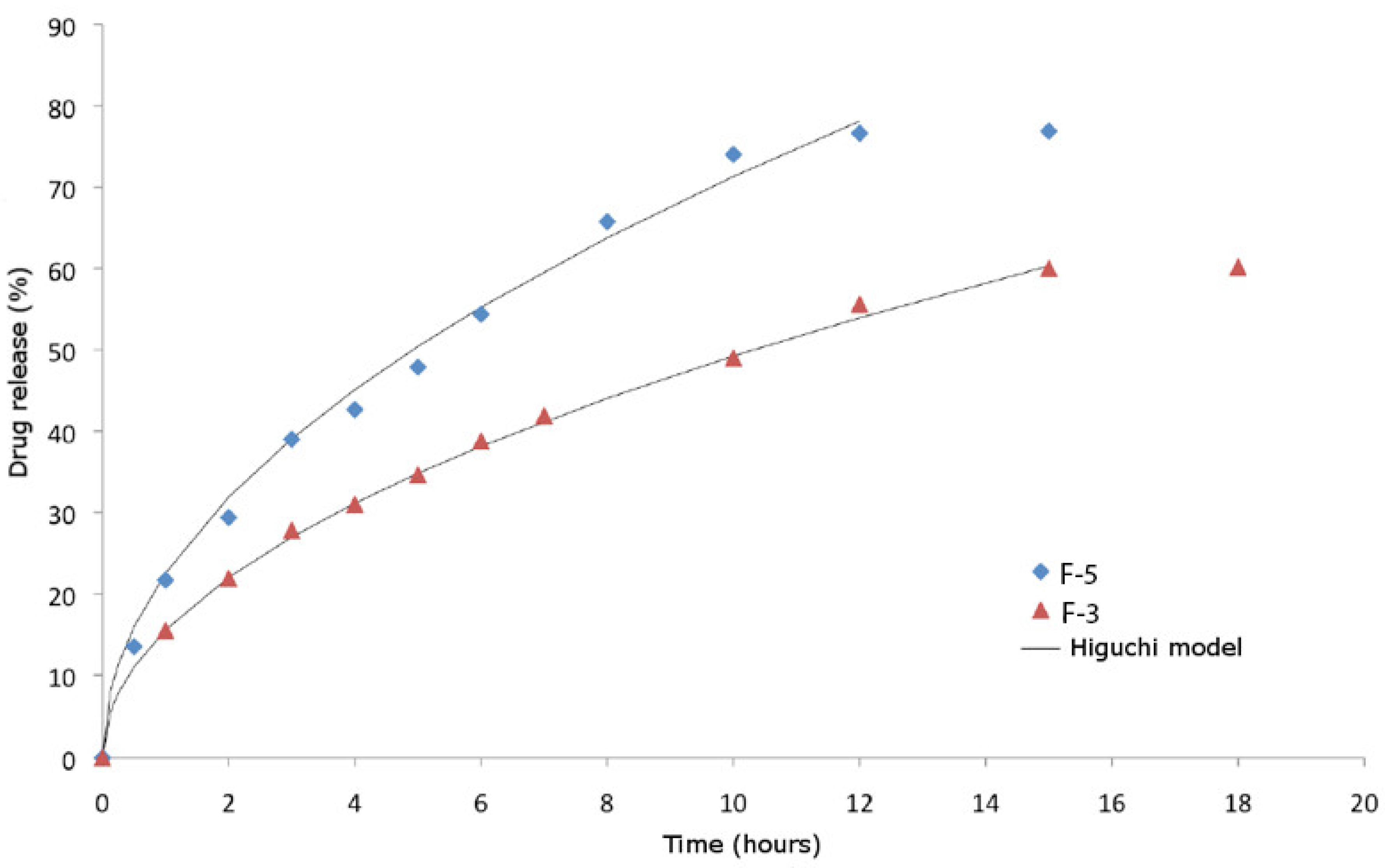
3.3. Drug Release
Several release models based on drug diffusion or drug delivery by polymer degradation were tested. The simplest model (order 0, Equation (2)) reflects a drug release regardless of its concentration [25]. The 1st order kinetics corresponds to release rates dependent on the active agent concentration (Equation (3)) [26]. Finally, the Higuchi model is based on Fickian diffusion [27] and characterizes a drug release from an insoluble polymeric matrix (Equation (4)).
where (g/s) is a constant dependent on the system
where is the initial concentration of drug and a first order constant
where is a constant dependent on the system
The release of retinol in the synthetic sweat model was evaluated for formulations F-3 and F-5 containing initially 300 and 500 mg of drug, respectively (Table 1). The release kinetics was slightly faster for formulation F-5. Indeed, the F-5 release profile reached a plateau after 10 h, whereas complete release was achieved at 15 h for F-3. The percentage of the drug released was close to 80% and 60% for F-5 and F-3, respectively. The 0 Order, first Order, and Higuchi kinetics models were evaluated for the prediction of the retinol release profile (Table 4). The best correlation was obtained with the Higuchi model based on diffusion phenomena (Table 4 and Figure 6). The diffusion through the polymeric membrane may depend on temperature [28], the nature of the external medium [29], or the pH [29]. However, these parameters being identical, the difference observed is linked to the retinol / polymer ratio: a larger ratio leads to faster release kinetics.

Table 4.
Regression coefficients and kinetic constants for various release models.
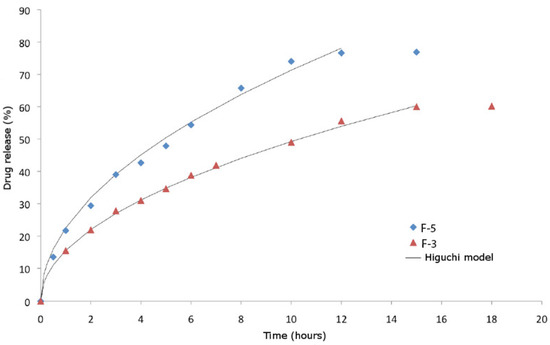
Figure 6.
Time-course monitoring of drug release for F-5 and F-3 formulations.
In addition, the encapsulation efficiency was followed weekly in order to verify that the particles do not release retinol in their storage environment (distilled water at room temperature). The results presented in Table 5 show a minor leakage of the active principle.

Table 5.
Stability of the formulation F-5.
4. Conclusions
Retinol is widely used in skin care products for its attractive properties. However, stability and toxicity issues limit its incorporation into formulations. In this study, we demonstrated that Eudragit RS 100 could encapsulate retinol to form nanoparticles, using the solvent-evaporation process with a good encapsulation efficiency. Our research shows that nanoparticles of Eudragit RS 100 can provide an attractive solution for a safer and effective retinol delivery. The obtained nanoparticles were able to protect and slowly release retinol over a prolonged period. Further studies are needed to demonstrate the ability of these particles to remain on skin thanks to the specific charge of Eudragit RS 100.
Author Contributions
Conceptualization, L.R.; methodology, L.R., Y.C.; investigation, L.R.; data curation, F.G.; writing—original draft preparation, F.G., Y.C.; writing—review and editing, L.R., Y.C. All authors have read and agree to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Gibbs, B.F.; Kermasha, S.; Alli, I.; Mulligan, C.N. Encapsulation in the food industry: A review. Int. J. Food Sci. Nutr. 1999, 50, 213–224. [Google Scholar] [PubMed]
- del Gaudio, P.; Colombo, P.; Colombo, G.; Russo, P.; Sonvico, F. Mechanisms of formation and disintegration of alginate beads obtained by prilling. Int. J. Pharm. 2005, 302, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Cilurzo, F.; Selmin, F.; Gennari, C.G.; Montanari, L.; Minghetti, P. Application of methyl methacrylate copolymers to the development of transdermal or loco-regional drug delivery systems. Expert Opin. Drug Deliv. 2014, 11, 1033–1045. [Google Scholar] [CrossRef] [PubMed]
- Martins, P.; Rosa, D.; Fernandes, A.; Baptista, P.V. Nanoparticle Drug Delivery Systems: Recent Patents and Applications in Nanomedicine. Recent Pat. Nanomed. 2014, 3, 105–118. [Google Scholar] [CrossRef]
- Casanova, F.; Santos, L. Encapsulation of cosmetic active ingredients for topical application—A review. J. Microencapsul. 2016, 33, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Wijaya, M.W. Microencapsulation Strategies for Long Term Protection of Ascorbic Acid. Ph.D. Thesis, RMIT University, Melbourne, Australia, 2011. [Google Scholar]
- Montenegro, L. Nanocarriers for skin delivery of cosmetic antioxidants. J. Pharm. Pharmacogn. Res. 2014, 2, 73–92. [Google Scholar]
- Prow, T.W.; Grice, J.E.; Lin, L.L.; Faye, R.; Butler, M.; Becker, W.; Wurm, E.M.T.; Yoong, C.; Robertson, T.A.; Soyer, H.P.; et al. Nanoparticles and microparticles for skin drug delivery. Adv. Drug Deliv. Rev. 2011, 63, 470–491. [Google Scholar] [CrossRef]
- Shields, C.W.; White, J.P.; Osta, E.G.; Patel, J.; Rajkumar, S.; Kirby, N.; Therrien, J.P.; Zauscher, S. Encapsulation and controlled release of retinol from silicone particles for topical delivery. J. Control. Release 2018, 278, 37–48. [Google Scholar] [CrossRef]
- Lee, M.H.; Oh, S.G.; Moon, S.K.; Bae, S.Y. Preparation of silica particles encapsulating retinol using o/w/o multiple emulsions. J. Colloid Interface Sci. 2001, 240, 83–89. [Google Scholar] [CrossRef]
- Ghouchi-Eskandar, N.; Simovic, S.; Prestidge, C.A. Solid-state nanoparticle coated emulsions for encapsulation and improving the chemical stability of all-trans-retinol. Int. J. Pharm. 2012, 423, 384–391. [Google Scholar] [CrossRef]
- Jee, J.P.; Lim, S.J.; Park, J.S.; Kim, C.K. Stabilization of all-trans retinol by loading lipophilic antioxidants in solid lipid nanoparticles. Eur. J. Pharm. Biopharm. 2006, 63, 134–139. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.-J.; Kim, C.-K. Formulation parameters determining the physicochemical characteristics of solid lipid nanoparticles loaded with all-trans retinoic acid. Int. J. Pharm. 2002, 243, 135–146. [Google Scholar] [CrossRef]
- Kim, D.G.; Jeong, Y.I.; Choi, C.; Roh, S.H.; Kang, S.K.; Jang, M.K.; Nah, J.W. Retinol-encapsulated low molecular water-soluble chitosan nanoparticles. Int. J. Pharm. 2006, 319, 130–138. [Google Scholar] [CrossRef] [PubMed]
- Thakral, S.; Thakral, N.K.; Majumdar, D.K. Eudragit®: A technology evaluation. Expert Opin. Drug Deliv. 2013, 10, 131–149. [Google Scholar] [CrossRef]
- Jana, U.; Mohanty, A.K.; Pal, S.L.; Manna, P.K.; Mohanta, G.P. Preparation and in vitro characterization of felodipine loaded eudragit® rs100 nanoparticles. Int. J. Pharm. Pharm. Sci. 2014, 6, 564–567. [Google Scholar]
- Joshi, M. Role of Eudragit in targeted drug delivery. Int. J. Curr. Pharm. Res. 2013, 5, 58–62. [Google Scholar]
- Cortesi, R.; Ravani, L.; Menegatti, E.; Esposito, E.; Ronconi, F. Eudragit® microparticles for the release of budesonide: A comparative study. Indian J. Pharm. Sci. 2012, 74, 415–421. [Google Scholar] [CrossRef]
- Contri, R.V.; Fiel, L.A.; Alnasif, N.; Pohlmann, A.R.; Guterres, S.S.; Schäfer-Korting, M. Skin penetration and dermal tolerability of acrylic nanocapsules: Influence of the surface charge and a chitosan gel used as vehicle. Int. J. Pharm. 2016, 507, 12–20. [Google Scholar] [CrossRef]
- Wu, X.; Landfester, K.; Musyanovych, A.; Guy, R.H. Disposition of charged nanoparticles after their topical application to the skin. Ski. Pharmacol. Physiol. 2010, 23, 117–123. [Google Scholar] [CrossRef]
- Kane, M.A.; Folias, A.E.; Napoli, J.L. HPLC/UV quantitation of retinal, retinol, and retinyl esters in serum and tissues. Anal. Biochem. 2008, 378, 71–79. [Google Scholar] [CrossRef]
- Aranyosi, P.; Csepregi, Z.; Rusznák, I.; Töke, L.; Víg, A. The light stability of azo dyes and azo dyeings. III. The effect of artificial perspiration on the light stability of reactive and non-reactive derivatives of two selected azo chromophores in aqueous solution. Dyes Pigment. 1998, 37, 33–45. [Google Scholar] [CrossRef]
- Li, M.; Rouaud, O.; Poncelet, D. Microencapsulation by solvent evaporation: State of the art for process engineering approaches. Int. J. Pharm. 2008, 363, 26–39. [Google Scholar] [CrossRef] [PubMed]
- Gibaldi, M.; Perrier, D. Pharmacokinetics, 2nd ed.; Wiley-Blackwell: Oxford, UK, 1983; Volume 72. [Google Scholar]
- Hadjiioannou, T.; Christian, G.; Koupparis, M.; Macheras, P. Quantitative Calculations in Pharmaceutical Practice and Research; VCH Publishers Inc.: Weinheim, Germany, 1993; pp. 345–348. [Google Scholar]
- Higuchi, T. Mechanism of sustained-action medication. Theoretical analysis of rate of release of solid drugs dispersed in solid matrices. J. Pharm. Sci. 1963, 52, 1145–1149. [Google Scholar] [CrossRef] [PubMed]
- Ujimori, J.F.; Onemochi, E.Y.; Ukuoka, E.F.; Erada, K.T. Application of Eudragit RS to Thermo-Sensitive Drug Delivery Systems. I. Thermo-Sensitive Drug Release from Acetaminophen Matrix Tablets Consisting of Eudragit RS/PEG 400 Blend Polymers. Chem. Pharm. Bull. 2002, 50, 408–412. [Google Scholar] [CrossRef] [PubMed]
- Eerikäinen, H.; Peltonen, L.; Raula, J.; Hirvonen, J.; Kauppinen, E.I. Nanoparticles containing ketoprofen and acrylic polymers prepared by an aerosol flow reactor method. AAPS PharmSciTech 2004, 5, e68. [Google Scholar] [CrossRef]
- Pignatello, R.; Ferro, M.; Puglisi, G. Preparation of solid dispersions of nonsteroidal anti-inflammatory drugs with acrylic polymers and studies on mechanisms of drug-polymer interactions. AAPS PharmSciTech 2002, 3, E10. [Google Scholar] [CrossRef]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).