1. Introduction
Oily skin is characterized by excessive sebaceous gland activity, leading to increased sebum secretion, persistent shine (particularly in the T-zone), and a tendency to develop comedones and inflammatory lesions [
1,
2]. Its pathogenesis is multifactorial, influenced by hormonal, genetic, age-related, and environmental factors [
1,
3]. Despite high sebum output, oily skin is often dehydrated, reflecting disruption of the hydrolipid barrier [
4]. Studies further show that these features can negatively affect patients’ self-esteem and quality of life [
5].
A precise analysis of oily skin parameters is crucial for understanding its functioning and for optimizing both skincare and therapeutic interventions [
6]. Advanced measurement technologies have shown that individuals with oily skin exhibit significantly elevated sebum secretion and increased transepidermal water loss (TEWL), which may indicate epidermal barrier dysfunction [
7]. Moreover, skin imaging techniques using devices such as Visioface
® have revealed an increased number and diameter of pores, correlating with uneven skin surface texture [
1].
Notably, excessive sebum production does not necessarily correlate with optimal skin barrier function; on the contrary, it may promote an environment conducive to microbial colonization, including Cutibacterium acnes, thereby contributing to the development or exacerbation of acne and other disorders of the pilosebaceous unit [
8,
9].
Microneedle mesotherapy (microneedling) is a minimally invasive dermatological technique that induces controlled microinjuries to stimulate wound-healing cascades. The release of growth factors (TGF-β, PDGF, VEGF, FGF) enhances fibroblast proliferation and synthesis of collagen, elastin, and glycosaminoglycans, resulting in improved skin firmness, elasticity, and texture [
10,
11,
12,
13,
14]. Additionally, microchannels created during the procedure transiently increase skin permeability, facilitating transdermal delivery of active substances [
15,
16]. Clinical evidence shows that microneedling is safe, well tolerated, and associated mainly with mild, short-lived side effects such as erythema or discomfort, with minimal downtime [
17,
18]. These findings confirm that microneedling is a minimally invasive procedure suitable for various skin types, including oily skin [
19,
20].
Conventional topical agents with seboregulating activity are limited by barrier function of the stratum corneum, which hinders their penetration into the deeper layers where sebaceous glands are located [
21]. In contrast, classical needle mesotherapy allows for the direct delivery of active substances into the dermis, but it is an invasive procedure associated with a higher risk of adverse effects and lower patient acceptance [
22]. The combination of microneedling with a sebum-regulating ampoule differs from both approaches: it exploits the microchannels created during treatment as pathways for the transport of active compounds, thereby enhancing their bioavailability within the sebaceous glands while maintaining minimal invasiveness. Moreover, microneedling itself stimulates skin regeneration and improves tissue structure, and its synergistic use with a seboregulating formulation can be expected to yield more pronounced and longer-lasting effects than either method alone. To our knowledge, this is the first study to evaluate the efficacy of such a combined therapeutic approach in individuals with oily skin.
In this study, a mesotherapy ampoule was used containing a combination of active substances specifically designed to regulate sebaceous gland activity and improve the overall condition of oily skin. Its formulation includes biomimetic peptides, non-crosslinked hyaluronic acid, vitamins (B6, B5, B12, E, retinol), zinc and copper compounds, exfoliating acids (e.g., glycolic acid), and soothing agents such as allantoin. This composition provides a multifaceted mode of action: normalization of sebum secretion, reduction in bacterial colonization, regulation of follicular keratinization, and simultaneous enhancement of skin hydration and barrier function. The rationale for selecting this formulation lies in its ability to target the key mechanisms underlying sebaceous gland hyperactivity and its clinical manifestations. When combined with microneedling, which facilitates transdermal delivery of bioactive compounds into deeper skin layers, a synergistic effect is expected, offering greater therapeutic efficacy compared with conventional topical treatments.
Myristoyl Hexapeptide-23 exhibits potent antibacterial activity, effectively targeting
Cutibacterium acnes. Retinol, a derivative of vitamin A, is well-documented in the management of oily and acne-prone skin. Topical application reduces inflammatory lesions and comedones while improving overall skin texture, thereby alleviating symptoms linked to excessive sebum secretion [
23,
24]. Glycolic acid, an alpha-hydroxy acid (AHA), accelerates stratum corneum desquamation and prevents blockage of sebaceous ducts. Literature highlights that AHAs enhance the condition of oily skin, decreasing shine and pore visibility [
25,
26]. Zinc demonstrates antibacterial and sebum-regulating activity. It helps reduce inflammation, lesion count, and skin shine, partly through inhibition of androgen-driven sebocyte activity and modulation of the cutaneous microbiome [
27,
28]. Copper pyrrolidone carboxylate, combining copper ions with pyroglutamic acid, shows anti-inflammatory and antibacterial properties and supports the regulation of sebaceous gland function. Hyaluronic acid (HA) improves hydration and elasticity, and thanks to its lightweight nature, it is well tolerated by oily skin without clogging pores [
29]. Tocopherol (vitamin E) acts as a potent antioxidant, protecting against oxidative stress and supporting regeneration, with evidence of benefits in inflammatory skin conditions such as acne [
30]. Pyridoxine (vitamin B6) has been shown to upregulate filaggrin expression, thereby strengthening the epidermal barrier and enhancing hydration [
31]. Panthenol exhibits both hydrating and anti-inflammatory properties, supporting the restoration of the skin barrier and alleviation of irritation [
32]. Cyanocobalamin (vitamin B12) demonstrates anti-inflammatory and regenerative properties, with studies confirming symptom reduction in inflammatory dermatoses [
33]. Allantoin adds soothing and healing activity, diminishing irritation and promoting recovery [
34]. Together, these ingredients act synergistically to hydrate the skin, regulate sebum production, alleviate inflammation, and support regeneration, thereby improving the overall condition of oily skin.
Despite available methods for sebum regulation and topical treatments, there is a lack of studies evaluating the effectiveness of combining microneedling with a seboregulating ampoule in individuals with oily skin. Therefore, the aim of this study was to assess the effects of a series of microneedle mesotherapy sessions using a seboregulating ampoule on selected parameters of oily skin. Nineteen volunteers underwent six treatments performed at three-week intervals. Skin parameters were assessed at baseline, after three sessions, and upon completion of the full series. Measurements were carried out using the MPA system (Courage & Khazaka) with dedicated probes: Sebumeter (sebum content), Corneometer (skin hydration), pH-meter (skin surface pH), Glossymeter (skin gloss), and Tewameter (transepidermal water loss, TEWL).
2. Materials and Methods
2.1. Selection of Study Population
The study included 19 women aged between 18 and 42 years. Detailed data on the participants’ age and duration of oily skin are presented in
Table 1.
Inclusion criteria: age ≥ 18 years, presence of oily skin, and provision of written informed consent to participate in the study.
Exclusion criteria: active fungal, bacterial, or viral skin infections; fever; recent sunburn or artificial tanning; inflammatory stage of acne; wounds; pregnancy and breastfeeding; tendency to form keloids; allergy to nickel (used in needles); coagulation disorders; neoplastic, metabolic or autoimmune diseases; and hypersensitivity to ingredients of the applied preparations.
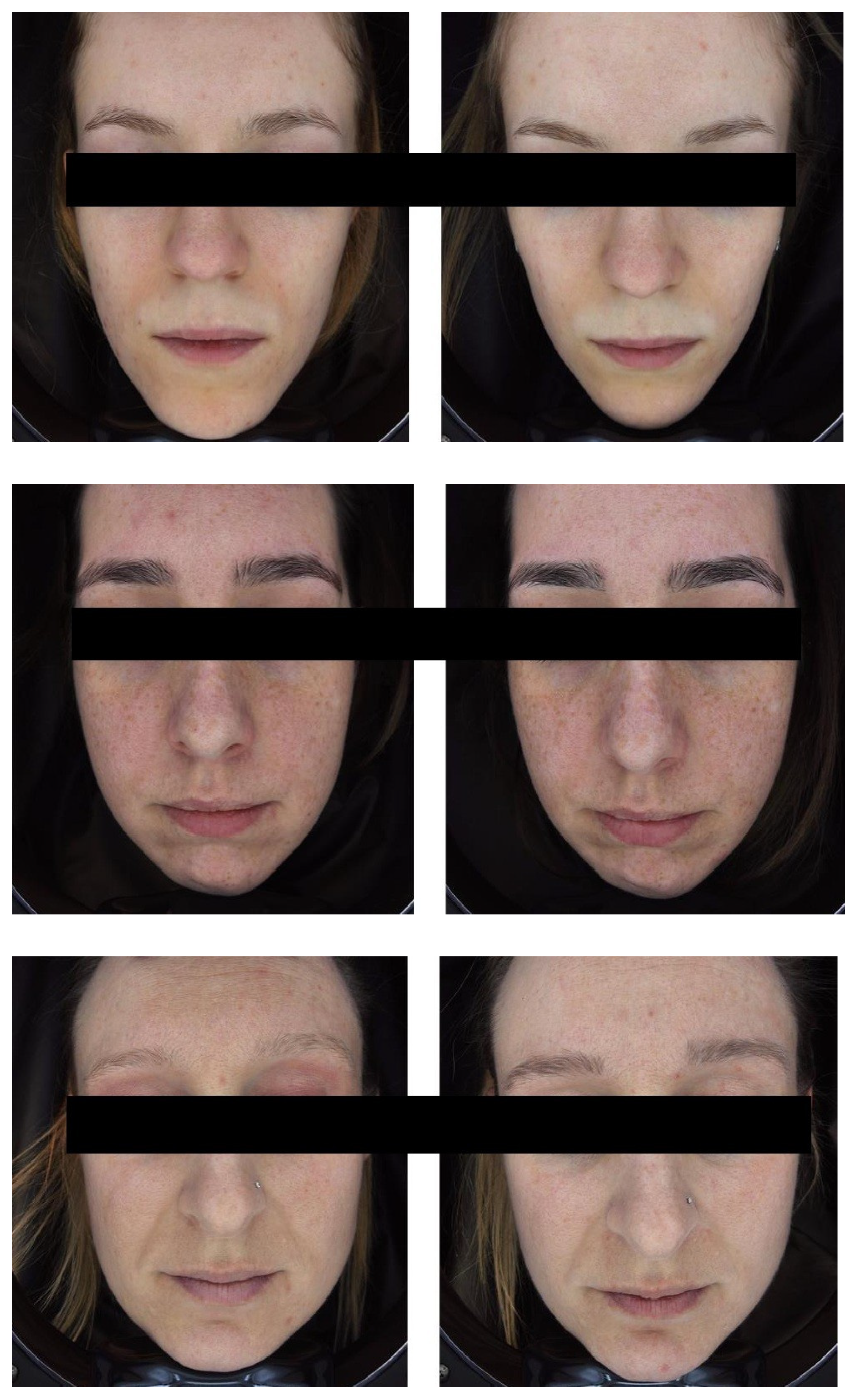
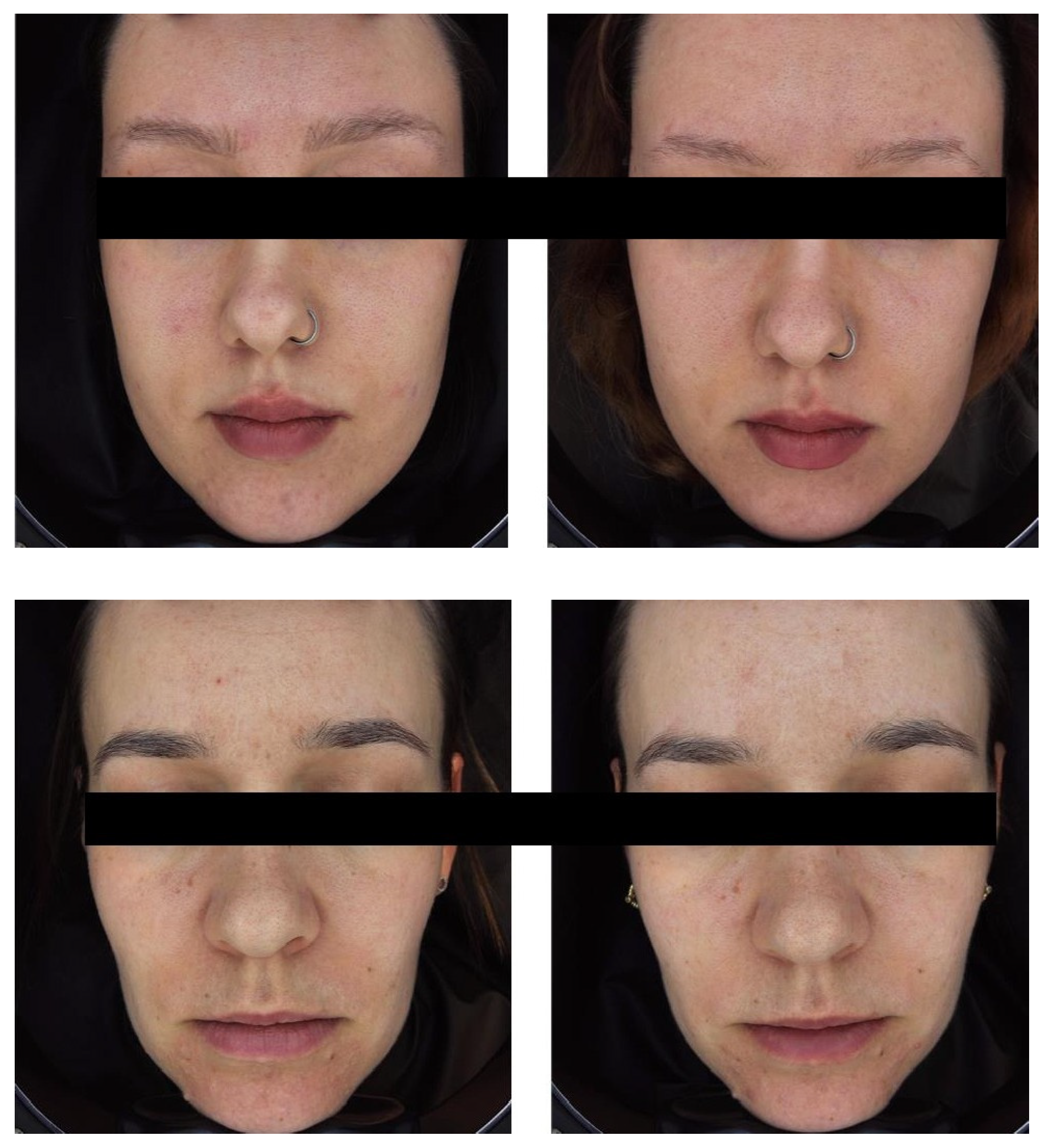
The study was approved by the Ethics Committee of the Medical University of Lublin (approval no. KE-0254/111/04/2023). Informed consent for participation was obtained from all subjects involved in the study. Informed consent for publication was obtained from all identifiable human participants.
2.2. Treatment Protocol
All participants underwent six sessions of microneedle mesotherapy, each performed with a 2.5 mL ampoule containing seboregulating active ingredients.
Microneedle mesotherapy treatments were performed using a dermapen device (m.pen [pro], Mesoestetic) at three-week intervals. The needle depth was adjusted depending on the treatment area: 0.25 mm for the forehead, nose, chin, and infraorbital region, and 0.5 mm for the cheeks. Microneedling was performed using the stamping technique. The device operated at a speed of 9500 punctures per minute, utilizing cartridges containing 24 needles.
During each session, a seboregulatory ampoule (Acneout, Dives Med) was applied. The full INCI composition of the preparation was as follows: Citrate Buffered Saline, Sodium Hyaluronate, Zinc Sulfate, Tocopherol, Myristoyl Hexapeptide-23, Copper Pyrrolidine Carboxylate, Pyridoxine, Retinyl Palmitate, Panthenol, Glycolic Acid, Cyanocobalamin, and Allantoin. The ampoule contained the following active ingredients:
Biomimetic peptide: Myristoyl Hexapeptide-23;
Non-crosslinked hyaluronic acid: 5 mg/mL;
Retinol;
Vitamins: Tocopherol (vitamin E), Pyridoxine (vitamin B6), Panthenol (pro-vitamin B5), Cyanocobalamin (vitamin B12);
Strengthening agents: Zinc, Copper Pyrrolidine Carboxylate, Glycolic Acid, Allantoin.
The preparation was selected based on the analysis of its relevance to the primary objective of the study, which was to evaluate the effects of microneedling mesotherapy on oily skin parameters, with particular focus on sebum regulation. The active ingredients used in the formulation have documented efficacy in the scientific literature in addressing common features of seborrheic skin, including hyperkeratosis, excessive activity of sebaceous glands, and impaired epidermal barrier function.
An additional criterion for selecting the preparation was its safety profile in microneedling procedures, and its suitability for ensuring a uniform therapeutic regimen across the entire study group. The use of a single, standardized formula enabled methodological consistency and facilitated a reliable assessment of its effect in the population of women with oily skin.
The safety of the applied preparation was confirmed prior to the study. The product is registered on the market as a cosmetic and is intended for use in microneedling mesotherapy procedures. Participants with allergies to the product’s ingredients were excluded from the study. Throughout the study, volunteers were monitored for potential adverse effects, such as erythema, itching, or burning. No serious adverse events or lasting skin changes were observed, confirming the high tolerability of microneedling mesotherapy combined with the sebum-regulating ampoule.
2.3. Measuring Apparatus
Skin parameters were assessed using a multifunctional measurement device, the MPA® (Multi Probe Adapter; Courage+Khazaka Electronic GmbH, Cologne, Germany). This system enables precise and non-invasive evaluation of various physiological skin properties through the use of specialized measurement probes.
The following probes were used in the study:
Corneometer® CM 825—a probe used to measure the hydration level of the stratum corneum. Values are expressed in arbitrary units (AU). It operates by assessing the dielectric capacitance of the skin, which is directly proportional to its water content.
Sebumeter® SM 815—a probe designed to measure the amount of sebum on the skin surface. Values are expressed in µg/cm2. It uses a specialized matrix tape that collects sebum and a photometric system that analyses the tape’s transparency—the more sebum absorbed, the greater the transparency.
Tewameter® TM 300—is a probe used to measure transepidermal water loss (TEWL), which reflects functional integrity of the epidermal barrier. Values are expressed in g/m2/h. It operates by analyzing the gradient of water vapor evaporation above the skin surface, measured using two sensors that detect temperature and humidity. Higher TEWL values indicate impaired epidermal barrier function.
pH-Meter® PH 905—an electrode used to measure the surface pH of the skin. Values are expressed on the standard pH scale (0–14). The parameter reflects the acid-base balance of the epidermis and may indicate disturbances in its protective function as well as potential effects of treatment on the skin microbiome.
Glossymeter® GL 200—a device used to measure skin gloss by analyzing the intensity of light reflected from the skin surface. The device quantifies the parameter Gloss DSC (Differential Specular Component), which reflects the amount of light specularly reflected from the skin surface and provides an objective measure of skin gloss in gloss units (GU).
Changes in skin gloss may be associated with sebum content, hydration level, and the smoothness or roughness of the skin surface.
Measurements were taken at three time points:
Before the initiation of therapy (baseline measurement);
After the third treatment, three weeks post-administration;
After completion of the full series of six treatments, also three weeks following the final session.
All measurements were performed under controlled conditions using the MPA Courage+Khazaka device, in strict accordance with the manufacturer’s instructions. Prior to the assessments, participants underwent a minimum 15 min acclimatization period in a room with constant temperature and humidity to stabilize skin conditions.
The analysis focused on two facial areas:
The T-zone (forehead and chin), typically characterized by increased sebaceous gland activity;
The cheek area, representing a region with a more balanced skin type.
Data collected from both areas allowed for the assessment of regional differences in the skin response to the applied therapy, as well as the overall effect of the microneedle mesotherapy treatment series on the physiological parameters of oily skin. All parameter measurements were carried out consistently at the same predefined points on the facial skin.
2.4. Statistical Analysis
Statistical analysis was performed using IBM SPSS Statistics 26 software. Initially, the distribution of variables was evaluated using the Shapiro–Wilk test, supplemented by an assessment of skewness and kurtosis, which was especially important given the small sample size (N = 19).
The study analyzed five physiological parameters, each measured at three time points: before the start of the therapy, after the third treatment, and after the sixth treatment, separately for the T-zone and the cheeks. Non-parametric statistical methods were applied in all subsequent analyses, regardless of whether normality assumptions were met in individual cases. To assess the differences between the three measurements, the Friedman rank ANOVA test was applied, with the corresponding values reported in column F. The table also includes post hoc data. Results are presented as minimum and maximum values, means (M), medians (Me), and standard deviations (SD). Statistical significance was set at p < 0.001 (***).
In addition, percentage changes were calculated for each parameter as:
These percentage changes were analyzed separately for the T-zone and the cheeks. One-sample Student’s t-tests were applied to determine whether the mean percentage change differed significantly from zero. Results for percentage changes are reported as mean ± standard deviation (SD) and median (interquartile range, IQR). Effect sizes were expressed as Cohen’s d. A p-value < 0.05 was considered statistically significant.
4. Discussion
The results of the present study indicate that microneedle mesotherapy using a sebum-regulating formulation can effectively improve the physiological parameters of oily skin, particularly by increasing hydration and reducing oiliness. The use of a standardized therapeutic protocol and formulation enabled a reliable assessment of the treatment’s efficacy in a cohort of women with seborrheic skin.
A significant increase in hydration levels, observed in both the T-zone and the cheeks, confirms the effectiveness of microneedling in stimulating skin regeneration and enhancing barrier function. Microneedling promotes keratinocyte proliferation and the induction of growth factors, a mechanism that has been extensively documented in the literature [
35]. Additionally, the hyaluronic acid used in this study, even in its non-crosslinked form, has demonstrated the ability to bind water molecules, thereby supporting the maintenance of proper hydration in the stratum corneum [
36].
The reduction in sebum levels, particularly pronounced after the completion of the entire treatment series, confirms the efficacy of active ingredients in the formulation, such as retinol, zinc, and the biomimetic peptide. Retinoids, including retinol, play a key role in a normalizing keratinisation and inhibiting sebaceous gland activity, partly by regulating the expression of genes involved in the proliferation and differentiation of keratinocytes and sebocytes [
37]. Zinc, on the other hand, exhibits anti-inflammatory, antioxidant, and sebostatic properties, making it an effective component in the treatment of oily and acne-prone skin.
The results indicate a faster reduction in skin greasiness in the cheek area compared to the T-zone, which may be attributed to anatomical differences. The cheeks are characterized by a lower density of sebaceous glands and milder seborrhoea, whereas the T-zone of the face contains the highest concentration of these glands and exhibits the greatest activity. Consequently, the more intensive sebum production in the T-zone may require a greater number of treatments to achieve comparable therapeutic effects.
Skin pH analysis revealed transient changes during the treatment series. In both the T-zone and cheeks, a significant decrease in pH was observed after three treatments, returning to baseline levels after six treatments (
Table 8). Individual percentage changes relative to 0% (
Table 10) showed no significant differences at the end of the treatment series. These findings suggest that microneedle mesotherapy with the sebum-regulating ampoule induces minor, physiologically meaningful adjustments in skin pH without disrupting barrier function. The temporary decrease in pH may result from active ingredients, such as glycolic acid, while the return to baseline indicates effective homeostatic mechanisms within the skin, supporting the safety of the therapy. Maintaining pH within the physiological range (4.5–5.5) is crucial for enzymatic activity, skin microflora balance, and protection against pathogens.
The analysis of transepidermal water loss (TEWL) revealed a specific pattern depending on the statistical approach used. In the repeated-measures ANOVA (
Table 11), no significant changes over time were observed in either the T-zone or the cheeks, indicating that the mean TEWL values did not change substantially across the measurement points. However, the analysis of individual percentage changes relative to 0% (
Table 13) showed a significant increase in TEWL in the T-zone, while no significant changes were found in the cheeks.
These apparent discrepancies result from the different statistical perspectives: ANOVA evaluates changes over time within the group, accounting for within-subject variance, whereas the one-sample
t-test compares the average percentage change against 0% across all participants. The high heterogeneity in individual responses, evident in
Table 12, may lead to non-significant results in ANOVA, even when the mean percentage change relative to 0% is statistically significant in the T-zone.
The observed increase in TEWL in the T-zone may reflect regional, adaptive differences in epidermal barrier function, associated with higher sebaceous gland activity and thinner stratum corneum in this area. In the cheeks, which have lower sebaceous activity and a more stable barrier, TEWL remained unchanged. These findings suggest that microneedle mesotherapy, conducted according to the described protocol, does not compromise long-term epidermal barrier function, while localized increases in the T-zone may represent adaptive skin responses following the treatment series.
The absence of significant changes in skin gloss suggests that the observed reduction in sebum production and improvement in epidermal hydration did not markedly affect the skin’s optical properties as measured by the MPA Glossymeter (Courage+Khazaka). This device represents an advanced method for gloss analysis, based on measuring the directional reflection of light from the skin surface, thereby enabling quantitative assessment of changes related to smoothness, oiliness, and epidermal texture.
It is worth noting, however, that skin gloss is a complex phenomenon influenced not only by sebum but also by the skin’s structural characteristics. It is possible that the applied therapy contributed to smoothing the skin surface and reducing pore size, which may have compensated for the decreased sebum levels, resulting in a statistically insignificant change in gloss parameters. This type of compensatory effect could explain the apparent stability of skin gloss despite the beneficial changes in skin condition. Therefore, it appears essential to expand future research to include additional techniques for assessing skin topography, enabling a more comprehensive understanding of the mechanisms underlying changes in skin gloss in response to the applied therapy.
The results of this study indicate a beneficial effect of a series of microneedle mesotherapy treatments on the parameters of oily skin. The use of a standardized formulation within the study group eliminated variability arising from differences in composition or application technique, thereby enhancing the reliability of the obtained results. The procedure itself was also performed uniformly—all participants underwent the same microneedling technique, with needle depth adjusted according to the treatment area. Nevertheless, it is important to acknowledge significant limitations of the study, including the small sample size (N = 19) and the absence of a control group. Future studies should aim to increase the sample size, include a control group, and evaluate the long-term therapeutic effects.
5. Conclusions
The conducted study indicates that a series of microneedle mesotherapy treatments using a formulation containing retinol, zinc, a biomimetic peptide, hyaluronic acid, a vitamin complex (vitamins E, B6, B12, pro-vitamin B5), copper pyroglutamate, and allantoin contributes to beneficial changes in the physiology of facial skin. Significant improvements in skin hydration and a reduction in skin oiliness were observed, particularly after completing the full series of six treatments. These effects were more pronounced in the cheek area than in the T-zone, probably due to anatomical and functional differences in sebaceous gland distribution and activity across facial regions.
The use of a standardized treatment technique and a uniform formulation constitutes a key strength of the study. However, limitations include the small sample size (N = 19) and the absence of a control group. Future studies, should aim to increase the number of participants, incorporate a placebo control group, and extend the post-treatment follow-up period. This would allow for a more comprehensive assessment of the durability of therapeutic effects and their impact on the microstructure and function of the skin.