Abstract
This original article presents the findings of a comprehensive case series, shedding light on the efficacy of diverse treatment modalities for managing precancerous and cancerous skin lesions and their remarkable rejuvenation effects on the skin. A particular focus is placed on the promising outcomes achieved through the application of a combination treatment involving 5-Fluorouracil (5-FU) and salicylic acid, which demonstrates enduring and noteworthy results. Furthermore, alternative therapeutic approaches, including 5-FU monotherapy, Methyl aminolevulinate–photodynamic therapy (MAL-PDT), and the combination of Imiquimod therapy with MAL-PDT, exhibit substantial potential for patients seeking non-surgical solutions. These treatments manifest as valuable tools in improving skin texture and mitigating the effects of photodamage. Nevertheless, the intricate interplay between the chosen treatment, the extent of photodamage, and individual patient characteristics, with a particular emphasis on age, necessitates long-term follow-up to gauge treatment outcomes and the likelihood of lesion recurrence. Notably, these treatments are associated with a significant degree of inflammation, igniting curiosity regarding enhanced skin cellular turnover and the potential for a more youthful skin appearance. Our findings accentuate the promise of topical fluorouracil (5-FU) and photodynamic therapy (PDT) in combating photoaging among patients with actinic keratoses. However, a need for further in-depth research is evident to unravel the nuanced relationships between these treatments, the severity of photodamage, and the influence of patient-specific factors. Such comprehensive investigations are instrumental in optimizing patient care and outcomes, offering a holistic approach to managing photodamage within the context of actinic keratoses. This work, when combined with existing literature, provides valuable insights and serves as a catalyst for future research to fully unlock the potential of these treatments, ultimately enhancing the quality of patient care.
1. Introduction
Actinic keratosis and non-melanoma skin cancers pose significant challenges in the field of dermatology, often necessitating aggressive therapeutic interventions that profoundly impact both the patient’s aesthetic appearance and, consequently, their overall quality of life.
The primary objective of these treatments is centered on effectively eradicating precancerous and cancerous skin lesions, embodying the core principles of medical intervention in this domain. However, recent discoveries have unveiled an additional dimension to these therapeutic modalities that transcends traditional disease management. A growing body of evidence suggests that in addition to their primary function, these treatments can inadvertently confer substantial cosmetic benefits to patients. These advantages include, but are not limited to, improvements in skin texture, the mitigation of photodamage, and the potential for a more youthful and rejuvenated skin appearance.
The focal point of this study lies in the exploration of the convergence between medical treatment and aesthetic outcomes. Through the analysis of a case series, we aim to delve deeply into the rejuvenating effects of these treatments, considering various treatment modalities and patient-specific variables, with a particular focus on age. Our research seeks to unveil the full extent of these rejuvenating effects, ensuring a comprehensive understanding of their potential. By taking into account both medical and cosmetic aspects, this research paves the way for a more holistic and patient-centered approach, revolutionizing our approach to actinic keratosis and non-melanoma skin cancer treatments in the future.
1.1. Photoaging
Photoaging is the primary cause of age-associated cosmetic skin issues in individuals with fair skin. In populations of European and North American adults with phototypes I, II, and III, photoaging is highly prevalent, affecting up to 80–90% of individuals [1]. Several risk factors contribute to this condition, including older age, male gender, light skin phototypes, extensive sun exposure, and residing in sun-exposed areas [2].
Chronic ultraviolet (UV) exposure, mainly from UVA, is recognized as the chief culprit behind photoaging. UVA penetrates deeply into the dermis and is more abundant in terrestrial sunlight, making it a significant contributor to photodamage. UVB, on the other hand, primarily affects the epidermis, causing sunburn and inflammation and playing a role in skin cancer [3,4,5].
Visible light, constituting a substantial portion of solar irradiation, has also emerged as a factor in photoaging. It can induce the production of reactive oxygen species (ROS), proinflammatory cytokines, and matrix metalloproteinases (MMPs), affecting the dermal matrix [3,6]. Notably, melanin, which offers protection against UV radiation, may enhance the harmful effects of visible light, especially in individuals with darker skin.
In populations with darker skin, wrinkle formation typically occurs later and is less pronounced compared to individuals with lighter skin. However, hyperpigmentation tends to be an earlier and more prominent sign of photoaging [7].
Beyond sunlight, environmental factors like air pollution and tobacco smoke can accelerate skin aging. Air pollution, which includes indoor and outdoor pollutants, has been linked to skin aging, supported by epidemiological studies. Smoking is known to contribute to the development of “smoker’s face”, characterized by wrinkles and an uneven complexion, likely due to impaired collagen synthesis and degradation [2,8].
In conclusion, photoaging is a complex process influenced by various factors, including UV radiation, ROS, visible light, and environmental pollutants. The impact varies according to skin type and color, necessitating comprehensive strategies for the prevention and treatment of age-associated cosmetic skin issues.
Photodamaged skin undergoes microscopic changes, including epidermal atrophy, flattened dermoepidermal junction, reduced collagen, and the deposition of thickened, disintegrated elastic fibers and breakdown products (solar elastosis). Atypical melanocytes and epidermal cells may increase [9].
The clinical features of sun-induced skin changes vary due to factors like age, sex, geographic location, and skin type. In individuals with phototypes I to IV (lighter skin), photoaging leads to fine and coarse wrinkles, solar elastosis, lentigines, mottled pigmentation, actinic keratoses, telangiectasias, loss of translucency and elasticity, xerotic texture, and sallow color. Populations with skin types I or II exhibit atrophic and dysplastic changes, including actinic keratoses. In contrast, skin types III or IV display increased thickness, deep wrinkles, and a leathery appearance. Hyperpigmented macules and mottled pigmentation are common in photodamaged skin [10].
In individuals with phototypes V to VI (darker skin), the effects of photodamage occur later and are less severe. Premature aging is seen in the midface with prominent nasolabial folds but fewer wrinkles. Dyschromia and features like mottled pigmentation, rough skin, dermatosis papulosa nigra, seborrheic keratoses, and solar lentigines may be present. Ultraviolet (UV) exposure has a more limited role in skin aging for darker skin tones [11].
Diagnosis is primarily clinical, with typical features including wrinkles, lentigines, pigmentation changes, loss of translucency, and sallow color. Photographic scales can aid patient evaluation.
Photoaging treatment involves various modalities, including sun protection, topical medications, and cosmetic procedures. Educating patients on year-round sun protection is the first step, emphasizing sunscreen, protective clothing, shade, and avoiding peak sun hours [12]. Topical retinoids, like tretinoin, are the primary medical therapy for mild to severe photoaging, stimulating collagen production and reducing skin atypia [13].
1.2. Age-Related Skin Changes
The natural aging process of the skin, distinct from sun-induced “photoaging”, involves significant structural and functional changes. Skin aging leads to atrophy, decreased elasticity, and compromised metabolic and reparative responses. These age-related transformations are separate from those attributed to prolonged sun exposure.
During the aging process, the epidermis undergoes thinning, and the dermoepidermal junction flattens, rendering the skin more susceptible to shear stress [14].
The loss of undulations at the dermoepidermal junction reduces the area available for nutrient transfer, including protective lipids in the stratum corneum. This leads to xerosis and compromises the skin’s barrier function [15]. Furthermore, epidermal turnover slows due to reduced keratinocyte division and prolonged migration from the basal layer to the skin surface [16].
Age-related alterations include decreases in melanocytes, immunologically active Langerhans cells, a 50 percent overall reduction in nail growth, and diminished sweat and sebaceous gland activity [17].
Other age-related changes unrelated to sun damage encompass thinning of the dermis, linked to reduced vascularity and the biosynthetic capacity of resident fibroblasts, contributing to delayed wound healing [16]. Dermal collagen levels may decrease by up to 75 percent with age, and the remaining collagen becomes fragmented. The elastic fiber network degenerates as elastin biosynthesis significantly declines after the fourth decade. Changes in glycosaminoglycan macromolecules in the dermis lead to loss of hydration and reduced skin resilience [18].
Diminished subdermal fat contributes to skin wrinkling, sagging, and increased susceptibility to trauma [19].
Remarkably, topical administration of tretinoin appears to reverse several age-related changes in sun-protected skin, causing improvements in epidermal thickness, rete ridges, capillaries, matrix proteins, collagen, and elastin levels [19].
1.3. Cutaneous Precancerosis and Non-Melanoma Skin Cancer
Actinic keratosis (AK), also known as solar keratosis, is one of the most frequently diagnosed dermatological conditions in the United States and Europe. Estimates of the proportion of adults with AKs in these locations range from 11 to 26 percent.
These lesions often manifest on areas of the body exposed to sunlight, such as the face, neck, backs of the hands, forearms, and lower legs [20].
The risk of AK development appears to correlate with cumulative ultraviolet (UV) exposure, primarily affecting older individuals (>60 years) with Fitzpatrick skin types I or II [21].
It is widely accepted that AK serves as the precursor to cutaneous squamous cell carcinoma (SCC) via UVB-induced mutations in critical genes, including p53. UVB rays specifically interact with the basal layer of the interfollicular epidermis, causing DNA damage and fostering SCC formation [22]. UVA rays contribute to damage through the generation of indiscriminate free radicals [23]. Importantly, compromised immune function, such as in solid organ transplant recipients (SOTRs), has been shown to promote the transformation of AK into SCC [24]. Interestingly, chronic sun exposure has also been demonstrated to induce epidermal immunosuppression, aside from its direct damage to oncogenes [25].
AK lesions exhibit a spectrum of phenotypes, typically presenting as erythematous scaly papules on sun-exposed areas. Treatment selection predominantly relies on visible features of AK, the extent of the affected area, treatment efficacy, patient tolerance, and individual preferences [26,27,28].
Pharmacological approaches primarily aim at clearing or preventing AK lesions, based on the concept of “field cancerization.” This concept suggests that areas of the skin extensively damaged by UV radiation are prone to producing both a higher number of AK lesions and lesions with a greater potential to progress to SCC [27,28].
Actinic keratoses also serve as precursors to basal cell carcinoma (BCC) and share pivotal risk factors in the development of BCC, which prominently encompass protracted and repeated exposure to ultraviolet (UV) radiation from both natural sunlight and tanning bed utilization. Basal cell carcinoma, the most prevalent form of skin cancer, predominantly affects individuals with fair skin who have a history of excessive sun exposure. Furthermore, hereditary predisposition and familial factors can further heighten this susceptibility. While BCC infrequently undergoes metastasis, it can engender significant complications, including local tissue infiltration, leading to structural impairment and disfigurement [29].
Currently, specific topical pharmacotherapies are available for the treatment of actinic keratosis and superficial basal cell carcinoma [30].
Topical 5-Flurouracil (5-FU), a thymidylate synthase inhibitor, is employed in pathologies requiring apoptosis of rapidly dividing cells and is known to increase p53 expression. For decades, 5-FU has been used in the treatment of actinic keratoses (AKs) in the form of a 5% cream applied twice daily for 2–4 weeks. Given its irritative nature, researchers have explored less caustic dosing regimens, such as 0.5% 5-FU applied daily for 4–6 weeks or 4% 5-FU to be applied daily or twice daily for up to 4 weeks. A combination of 5-FU and salicylic acid (SA), a keratolytic agent, has also proven to be an effective spot treatment for hypertrophic AKs [27,28,30,31].
Imiquimod topical cream is a well-established treatment for AKs, stimulating cell-mediated attacks against AK lesions through the production of IFN-α, TNF-α, IL-6, and IL-8, as well as the recruitment of activated CD4+ and CD8+ T cells and mast cells. Imiquimod is available as a 5% cream to be applied three times weekly for 12–16 weeks, or a 3.75% cream. It has also emerged as a valuable therapeutic modality for managing superficial basal cell carcinoma when used five times weekly for 6 weeks, resulting in both lesion resolution and favorable cosmetic outcomes [27,28,30,32].
Diclofenac, a non-steroidal anti-inflammatory drug capable of inhibiting both cyclooxygenase-1 (COX-1) and cyclooxygenase-2 (COX-2), thereby preventing the formation of inflammatory mediators such as prostaglandins and thromboxanes and reducing angiogenesis and cell proliferation, is a well-tolerated but only mildly effective treatment option [27,28,30,33].
Tirbanibulin 1% ointment is a novel drug option in the treatment of AKs. It serves as a microtubule and Src kinase inhibitor, eliciting the drug’s antiproliferative effects and acting as a p53 inducer, thereby potentiating apoptosis in target cells when used once daily for 3–5 days [27,28,30,34].
In addition to topical pharmacotherapies, traditional photodynamic light therapy (PDT) in conjunction with 5-aminolevulinic acid (ALA) or the more recent photosensitizer methyl 5-aminolevulinate (MAL) has shown satisfactory results. ALA and MAL are two prodrugs that are eventually metabolized into protoporphyrin IX (PPIX) by neoplastic cells. Subsequent irradiation at specific wavelengths promotes PPIX-induced, mitochondrially mediated destruction of abnormal tissue. Pain, erythema, and post-treatment inflammation are the most common and significant side effects associated with PDT, with ALA being more commonly linked to pain compared to treatments using MAL as a photosensitizer. Apart from traditional PDT, daylight photodynamic therapy (dPDT) has emerged, involving exposure to natural light following the application of a photosensitizer, resulting in less pain than traditional PDT [27,28,30,35].
Adverse events for these treatments include local skin reactions such as erythema, pain, inflammation, erosion, scabbing, and pigmentation, which typically resolve on their own following treatment cessation or after some weeks and serve as positive indicators of treatment efficacy [27,28].
2. Materials and Methods
This prospective case-series study was conducted from November 2020 to March 2023 at the Department of Dermatology and Venereology, University of Turin, Turin, Italy.
To be eligible for enrollment, patients were required to provide written informed consent, exhibit one or more actinic keratosis lesions or be diagnosed with one basocellular carcinoma through dermoscopy, and be suitable for topical treatments with 0.5% 5-fluorouracil (5-FU) combined with 10% salicylic acid (5-FU/SA), 5% 5-FU, imiquimod 5%, or photodynamic therapy with Methyl aminolevulinate (MAL-PDT).
The treatment regimens adhered to the prescribing information approved by the national medicines agency (AIFA).
Patients’ lesions were assessed by the same physician at baseline (Week 0) and again at five months following the completion of treatment (Week 20), in accordance with the selected procedure.
Simultaneously, local skin rejuvenation was evaluated by investigators, considering parameters such as xerosis or dehydration, wrinkles, elastosis, laxity, poichilodermia, accentuation of skin markings, skin turgor, and vascular telangiectasias. Rejuvenation was categorized as mild, moderate, or significant.
3. Results
3.1. Case n.1
A 77-year-old woman was initially seen in November 2020. She presented with multiple slightly itchy erythematous macules with poorly defined borders and minimal hyperkeratosis on her right cheek. The perilesional skin displayed clinical signs of ultraviolet radiation damage, such as xerosis, accentuation of skin markings, uneven pigmentation, and vascular telangiectasia.
During the dermoscopic examination of the affected skin, we observed multiple lesions showing a pink-reddish vascular pseudonetwork surrounding hair follicles with minimal white scaling, configuring a ‘strawberry’ pattern with a “rosette sign”. Overall, the presentation strongly suggested field cancerization with multiple actinic keratoses.
We prescribed 0.5% 5-FU with 10% salicylic acid (5-FU/SA) topical treatment once daily for 12 weeks. However, after one month, the patient experienced a significant inflammatory reaction characterized by erythema, edema, erosions, and crusting at the site of the topical treatment application. The patient reported an intense burning sensation, leading us to prescribe topical anti-inflammatory treatment with Gentamicin/Betamethasone 0.1%/0.05% cream applied twice daily until the symptoms remitted.
Two months later, we clinically and dermoscopically documented the remission of precancerous lesions and inflammatory signs. During skin examination, we also observed concurrent improvements in skin texture, with a reduction in poichilodermia, smoothing of skin markings, and enhanced skin turgor, all of which appeared indicative of significant skin rejuvenation.
Upon regular follow-up three years later, we observed consistent clinical presentation with no signs of recurrence or emergence of new lesions in the treated area and sustained improvement in skin quality (Figure 1).
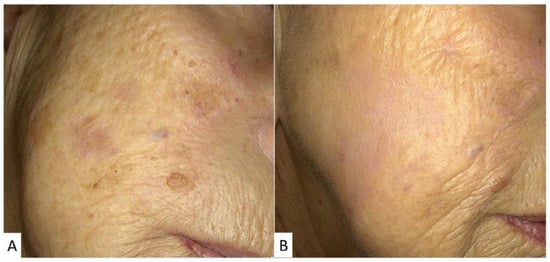
Figure 1.
A 77-year-old female patient with actinic keratosis and extensive keratinization on the right cheek (A). Following treatment with a solution containing 0.5% 5-fluorouracil and 10% salicylic acid, applied once daily for 12 weeks. During the treatment, significant erythema was observed at the site of application, which resolved completely after 20 days after therapy cessation (B). It is noteworthy that the therapeutic and aesthetic outcome was excellent, with the disappearance of actinic keratoses and improved skin tone.
3.2. Case n.2
An 82-year-old female presented to our dermatology clinic in April 2022 with a single infra-orbital erythematous plaque displaying minimally elevated borders and brownish scaling. Dermoscopic examination revealed a strawberry pattern with atypical vessels.
These clinical findings raised suspicion of bowenoid actinic keratosis. Notably, the patient’s facial skin exhibited pronounced signs of photo/chrono-aging, including wrinkles, elastosis, laxity, and dehydration.
For the management of the precancerous lesion, we initiated a regimen of daily 5% 5-FU topical treatment for a duration of 28 days.
Approximately two weeks into the treatment, the patient reported the onset of a marked inflammatory reaction at the treated area, which persisted for four weeks even after discontinuation of the cream.
In August 2022, the patient returned for a follow-up visit, and we observed complete remission of the cutaneous lesion that had undergone treatment with a favorable aesthetic outcome. Furthermore, the quality of the skin at the treatment site displayed marginal improvement compared to the surrounding skin, with reduced accentuation of skin markings. Only slight post-inflammatory hyperpigmentation remained. These findings were indicative of mild skin rejuvenation (Figure 2).
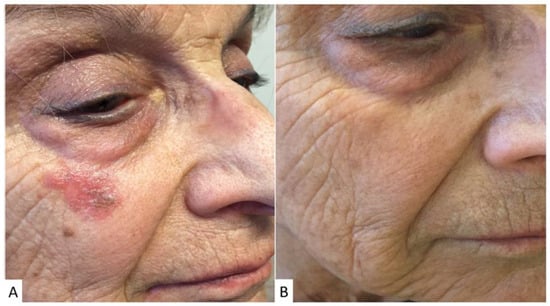
Figure 2.
An 82-year-old female patient with Bowenoid actinic keratosis infra-orbital on the right (A). After treatment with an ointment containing 5% 5-fluorouracil, applied once daily for 4 weeks, there was a progressive reduction in the lesion with complete clinical resolution (B) and excellent aesthetic results. It is worth noting the partial reduction in wrinkles at the site of ointment application and the excellent preservation of facial mimetic structures.
3.3. Case n.3
A 58-year-old healthy female presented in March 2023 with a fair skin type and a history of recreational sun exposure. On clinical examination, we observed diffuse superficial actinic keratosis on the patient’s forehead. Additionally, we noted associated signs of significant photodamage, including solar lentigo, alterations in skin texture, and multiple telangiectasias, along with expression lines.
Given the extent of the presentation, despite the lesions being superficial and the patient’s relative youth and cooperation, we elected to proceed with a session of photodynamic therapy with Methyl aminolevulinate (MAL-PDT).
During the treatment and for the subsequent 10 days, the patient experienced significant local inflammation, accompanied by a burning sensation, for which Gentamicin/Betamethasone 0.1%/0.05% cream was prescribed twice daily until remission.
Five months after the single MAL-PDT session, the patient returned for dermatologic evaluation, demonstrating marked improvement in the actinic keratosis presentation, with minimal residual superficial lesions. Notably, there was near-complete remission of the cancerization field, accompanied by a noticeable improvement in the dermatoheliosis picture. This improvement included reduced dyschromia, lightening of previously observed solar lentigines, improved skin texture regularity, and partial smoothing of expression lines, consistent with moderate skin rejuvenation.
Considering the substantial progress achieved, we scheduled a follow-up MAL-PDT session, which the patient is currently awaiting (Figure 3).
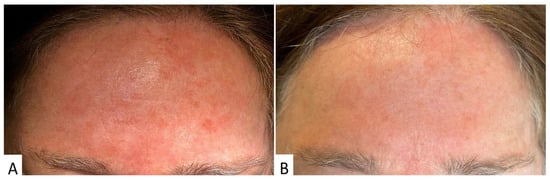
Figure 3.
A 58-year-old female patient with a field of cancerization and numerous superficial actinic keratoses on the forehead (A). After photodynamic therapy with methyl aminolevulinic acid (single session), resolution of superficial lesions and a reduction in cutaneous imperfections (including hyperpigmented macules) were observed. This result was durable even at 5 months post-photodynamic therapy (B).
3.4. Case n.4
In January 2023, a 67-year-old female patient visited our dermatology clinic, presenting with a single erythematous translucent patch of the nasogenian groove measuring approximately 7 mm in diameter, accompanied by a central ulceration.
Dermoscopy revealed diagnostic features consistent with basal cell carcinoma, including arborizing telangiectasia, erosions, and white structures.
The patient exhibited diffuse telangiectasia on her skin, along with altered texture, indicative of sun damage and physiological skin aging.
Given the challenging location of the cutaneous neoplasm, which was situated in a cosmetically sensitive area of the patient’s face, we opted for a medical approach. A six-week course of topical therapy using Imiquimod 5% cream once daily was prescribed and was followed by a single session of MAL-PDT 14 days after the completion of the topical therapy.
The patient reported a significant inflammatory reaction during the Imiquimod therapy and following MAL-PDT with erythema, edema, and crust formation.
After 20 weeks following the procedure, the patient returned for a follow-up visit.
Upon clinical examination, we observed complete clinical and dermoscopic remission of the treated basal cell carcinoma, with full restoration of the skin and an excellent aesthetic outcome. The treated skin displayed fewer telangiectasias and appeared plumper compared to the surrounding areas. These clinical findings were indicative of a mild rejuvenation of the skin subjected to treatment. A follow-up visit at 24 months confirmed the complete clearance of basal cell carcinoma and the sustained improvement in skin tone.
The outcomes of these clinical cases demonstrate the effectiveness of tailored treatment approaches for patients presenting with diverse skin conditions and age-related concerns. In Case 1, a 77-year-old woman with actinic keratoses on her cheek received a combination of 0.5% 5-FU and 10% salicylic acid (5-FU/SA) topical therapy. Although she initially experienced an inflammatory reaction, after two months, there was a notable improvement in both the precancerous lesions and skin texture. Long-term follow-up revealed no recurrence, underscoring the treatment’s lasting benefits. Case 2 involved an 82-year-old woman with bowenoid actinic keratosis treated with 5% 5-FU, leading to significant inflammation. However, this inflammatory phase eventually resolved, resulting in complete remission of the lesion and mild skin rejuvenation. In Case 3, a 58-year-old woman with superficial actinic keratosis on her forehead underwent photodynamic therapy with Methyl aminolevulinate (MAL-PDT), which initially induced inflammation and a burning sensation. Despite these challenges, the patient achieved significant improvement in her actinic keratosis, along with noticeable skin rejuvenation. The success of this treatment approach prompted a follow-up MAL-PDT session. In the fourth case, a 67-year-old woman with basal cell carcinoma in a cosmetically sensitive area was managed with a combination of Imiquimod 5% cream and MAL-PDT. The treatment resulted in complete clinical remission of the carcinoma, with the treated skin displaying fewer telangiectasias and improved plumpness compared to the surrounding areas, indicative of mild skin rejuvenation. These cases collectively emphasize the efficacy of personalized treatments for addressing both precancerous skin lesions and the enhancement of skin aesthetics. Patients experienced not only the resolution of their primary concerns but also improvements in skin texture, contributing to overall satisfaction and well-being (Figure 4).
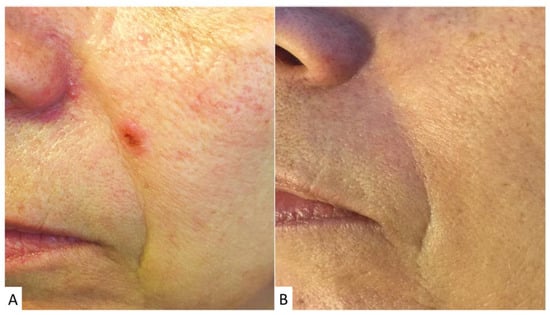
Figure 4.
A 67-year-old female patient with basal cell carcinoma in the left nasogenian groove (A). Following treatment with 5% Imiquimod cream, applied once daily for 6 weeks, and subsequent photodynamic therapy with methyl aminolevulinic acid (single session), complete resolution of the lesion was observed with no recurrence at 24 months (B). A favorable cosmetic effect was also noted, with the underlying wrinkle appearing less pronounced following the therapeutic intervention.
4. Discussion
These four case reports detail the management and outcomes of patients with various types of precancerous and cancerous skin lesions, as well as the associated photodamage and signs of aging.
The management of actinic keratoses (AKs) and the concurrent presence of photoaging represents a critical challenge in dermatology.
Our findings suggest that the combination of 5-FU and salicylic acid effectively treats actinic keratoses while yielding the most significant benefits in terms of skin rejuvenation. Long-term follow-up for our patient who underwent this treatment underscores the durability of these outcomes. Additionally, 5-FU alone demonstrated moderate effectiveness in improving skin texture while managing precancerous lesions.
Our results align with several previous studies that indicate a potential for improvement through topical fluorouracil (5-FU) treatment [36]. The mechanism of action underlying 5-FU treatment is intriguing, as it involves the induction of epidermal injury, subsequent wound healing, and the facilitation of dermal matrix remodeling, ultimately leading to an enhanced skin appearance. This favorable effect of 5-FU on the clinical signs of photoaging has been consistently noted in various observational studies [36,37].
For instance, a study focusing on 21 patients aged 56 to 85 years with multiple facial actinic keratoses and moderate to severe photoaging is particularly noteworthy [36]. These individuals received a two-week treatment of 5-FU 5%. In addition to the expected clearance of actinic keratoses, the study identified a significant improvement in parameters of photoaging, including wrinkling, tactile roughness, lentigines, hyperpigmentation, and sallowness. Of significance, these improvements commenced four to six weeks after the treatment’s completion and continued to be observable through week 24, suggesting the potential for sustained benefits.
However, it is important to note that the relationship between 5-FU treatment and photodamage is not without complexity. A secondary analysis of data from a randomized trial involving 932 veterans who received standard topical fluorouracil treatment for the chemoprevention of basal and squamous cell carcinoma of the skin did not reveal a significant difference in photodamage, as measured by four photonumeric scales, between baseline and the 6-, 12-, and 18-month post-treatment assessments [38]. This discrepancy emphasizes the need for comprehensive research to unravel the nuanced interplay between 5-FU treatment, photodamage, and the potential influencing factors.
In parallel, photodynamic therapy (PDT) emerges as an intriguing modality in our case series for addressing photoaging alongside AKs. Our observations revealed that MAL-PDT treatment for actinic keratosis can moderately contribute to the rejuvenation of photodamaged skin. Furthermore, we found that the combination of Imiquimod therapy and MAL-PDT, although applied exclusively to the small area affected by the epithelioma, produced mild results in terms of rejuvenation.
These results appears complementary to the findings from various studies in the existing literature [39,40,41,42]. These studies consistently report significant improvements in fine wrinkles, mottled hyperpigmentation, roughness, and sallowness following PDT, which is a common treatment for actinic keratosis and field cancerization. The mechanisms underlying PDT’s role in ameliorating photodamage are postulated to encompass the upregulation of collagen production and increased epidermal proliferation [43].
PDT can be employed as a standalone treatment or in combination with other modalities to address photoaging concerns in patients suffering from actinic keratosis and NMSC [44,45]. Nevertheless, it is crucial to recognize that one of the primary side effects associated with PDT is the sensation of pain during illumination. To mitigate this, daylight PDT has emerged as a valuable alternative, as it is linked with minimal or no pain, potentially enhancing patient acceptance and compliance [46].
Of significance, our findings highlight a common thread among these treatments, with each inducing a high degree of inflammation in our patients. This observed inflammation may hold implications for an increased turnover of skin cells, potentially contributing to the observed improvements in skin appearance and quality [47].
While promising, these results underscore the importance of acknowledging individual patient factors, especially age, in understanding treatment response and the extent of skin rejuvenation.
5. Conclusions
In conclusion, our case series highlights the effectiveness of diverse treatment approaches for managing not only both precancerous and cancerous skin lesions, but also for achieving remarkable rejuvenation effects on the skin, with a particular emphasis on the promising results achieved through the combination of 5-FU and salicylic acid. Notably, our observations underscore the enduring durability of this treatment approach, emphasizing its potential clinical value.
Furthermore, the moderate improvements in skin texture and photodamaged skin rejuvenation observed with alternative medical treatments for precancerous skin lesions and NMSC, such as 5-FU alone, MAL-PDT, and the combination of Imiquimod therapy and MAL-PDT, offer encouraging prospects for patients seeking non-surgical solutions.
However, it is crucial to acknowledge the intricate interplay between these treatments, the extent of photodamage, and individual patient factors, notably age, which may influence treatment outcomes and the degree of skin rejuvenation. Therefore, long-term follow-up remains imperative to monitor the persistence of results and the potential for lesion recurrence. The association of these treatments with a notable degree of inflammation further fuels curiosity regarding enhanced skin cellular turnover and the prospect of a more youthful skin appearance.
In particular, our combined findings underscore the promise of both topical fluorouracil and PDT in addressing photoaging among patients with actinic keratoses. Nonetheless, the complex relationship between these treatments, photodamage, and patient-specific factors necessitates further comprehensive research and clinical investigation. These investigations are essential to better define the efficacy and limitations of these treatment modalities in managing photodamage within the context of actinic keratoses, thereby offering a more holistic understanding of their clinical potential. Our case series, together with the existing literature, provides valuable insights into the capacity of these treatments, but their full scope and nuances warrant further exploration to optimize patient care and outcomes.
Author Contributions
Conceptualization, N.S. and F.R.; methodology, N.S.; software F.R.; validation, S.R., P.Q. and P.B.; formal analysis, L.M.; investigation N.S.; resources P.B.; data curation, S.B. (Silvia Borriello) and S.B. (Sara Boskovic); writing—original draft preparation, F.R.; writing—review and editing, N.S.; visualization, F.R.; supervision, P.B.; project administration, P.Q.; funding acquisition, S.R. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Informed Consent Statement
The patients in this manuscript signed written informed consent to media publication.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationship that could be construed as a potential conflict of interest.
References
- Maddin, S.; Lauharanta, J.; Agache, P.; Burrows, L.; Zultak, M.; Bulger, L. Isotretinoin improves the appearance of photodamaged skin: Results of a 36-week, multicenter, double-blind, placebo-controlled trial. J. Am. Acad. Dermatol. 2000, 42 Pt 1, 56–63. [Google Scholar] [CrossRef]
- Green, A.C.; Hughes, M.C.; McBride, P.; Fourtanier, A. Factors associated with premature skin aging (photoaging) before the age of 55: A population-based study. Dermatology 2011, 222, 74–80. [Google Scholar] [CrossRef]
- Yaar, M.; Gilchrest, B.A. Photoageing: Mechanism, prevention and therapy. Br. J. Dermatol. 2007, 157, 874–887. [Google Scholar] [CrossRef]
- Benjamin, C.L.; Ullrich, S.E.; Kripke, M.L.; Ananthaswamy, H.N. p53 tumor suppressor gene: A critical molecular target for UV induction and prevention of skin cancer. Photochem. Photobiol. 2008, 84, 55–62. [Google Scholar] [CrossRef]
- Schwarz, T. 25 years of UV-induced immunosuppression mediated by T cells-from disregarded T suppressor cells to highly respected regulatory T cells. Photochem. Photobiol. 2008, 84, 10–18. [Google Scholar] [CrossRef]
- Fisher, G.J.; Kang, S.; Varani, J.; Bata-Csorgo, Z.; Wan, Y.; Datta, S.; Voorhees, J.J. Mechanisms of photoaging and chronological skin aging. Arch. Dermatol. 2002, 138, 1462–1470. [Google Scholar] [CrossRef]
- Chung, J.H.; Lee, S.H.; Youn, C.S.; Park, B.J.; Kim, K.H.; Park, K.C.; Cho, K.H.; Eun, H.C. Cutaneous photodamage in Koreans: Influence of sex, sun exposure, smoking, and skin color. Arch. Dermatol. 2001, 137, 1043–1051. [Google Scholar]
- Li, M.; Vierkötter, A.; Schikowski, T.; Hüls, A.; Ding, A.; Matsui, M.S.; Deng, B.; Ma, C.; Ren, A.; Zhang, J.; et al. Epidemiological evidence that indoor air pollution from cooking with solid fuels accelerates skin aging in Chinese women. J. Dermatol. Sci. 2015, 79, 148–154. [Google Scholar] [CrossRef]
- Lee, H.; Hong, Y.; Kim, M. Structural and Functional Changes and Possible Molecular Mechanisms in Aged Skin. Int. J. Mol. Sci. 2021, 22, 12489. [Google Scholar] [CrossRef]
- Vierkötter, A.; Hüls, A.; Yamamoto, A.; Stolz, S.; Krämer, U.; Matsui, M.S.; Morita, A.; Wang, S.; Li, Z.; Jin, L.; et al. Extrinsic skin ageing in German, Chinese and Japanese women manifests differently in all three groups depending on ethnic background, age and anatomical site. J. Dermatol. Sci. 2016, 83, 219–225. [Google Scholar] [CrossRef]
- Chien, A.L.; Qi, J.; Grandhi, R.; Kim, N.; César, S.S.A.; Harris-Tryon, T.; Jang, M.S.; Olowoyeye, O.; Kuhn, D.; Leung, S.; et al. Effect of Age, Gender, and Sun Exposure on Ethnic Skin Photoaging: Evidence Gathered Using a New Photonumeric Scale. J. Natl. Med. Assoc. 2018, 110, 176–181. [Google Scholar] [CrossRef]
- Rigel, D.S.; Taylor, S.C.; Lim, H.W.; Alexis, A.F.; Armstrong, A.W.; Fuxench, Z.C.C.; Draelos, Z.D.; Hamzavi, I.H. Photoprotection for skin of all color: Consensus and clinical guidance from an expert panel. J. Am. Acad. Dermatol. 2022, 86, S1–S8. [Google Scholar] [CrossRef]
- Cho, S.; Lowe, L.; Hamilton, T.A.; Fisher, G.J.; Voorhees, J.J.; Kang, S. Long-term treatment of photoaged human skin with topical retinoic acid improves epidermal cell atypia and thickens the collagen band in papillary dermis. J. Am. Acad. Dermatol. 2005, 53, 769–774. [Google Scholar] [CrossRef]
- Moragas, A.; Castells, C.; Sans, M. Mathematical morphologic analysis of aging-related epidermal changes. Anal. Quant. Cytol. Histol. 1993, 15, 75–82. [Google Scholar]
- Montagna, W.; Carlisle, K. Structural changes in ageing skin. Br. J. Dermatol. 1990, 122 (Suppl. 35), 61–70. [Google Scholar] [CrossRef]
- Ashcroft, G.S.; Mills, S.J.; Ashworth, J.J. Ageing and wound healing. Biogerontology 2002, 3, 337–345. [Google Scholar] [CrossRef]
- Yaar, M.; Gilchrest, B.A. Skin aging: Postulated mechanisms and consequent changes in structure and function. Clin. Geriatr. Med. 2001, 17, 617–630. [Google Scholar] [CrossRef]
- Uitto, J. The role of elastin and collagen in cutaneous aging: Intrinsic aging versus photoexposure. J. Drugs Dermatol. 2008, 7 (Suppl. 2), s12–s16. [Google Scholar]
- McCullough, J.L.; Kelly, K.M. Prevention and treatment of skin aging. Ann. N. Y. Acad. Sci. 2006, 1067, 323–331. [Google Scholar] [CrossRef]
- Salasche, S.J. Epidemiology of actinic keratoses and squamous cell carcinoma. J. Am. Acad. Dermatol. 2000, 42 Pt 2, 4–7. [Google Scholar] [CrossRef]
- Engel, A.; Johnson, M.L.; Haynes, S.G. Health effects of sunlight exposure in the United States. Results from the first National Health and Nutrition Examination Survey, 1971–1974. Arch. Dermatol. 1988, 124, 72–79. [Google Scholar] [CrossRef]
- Thomson, J.; Bewicke-Copley, F.; Anene, C.A.; Gulati, A.; Nagano, A.; Purdie, K.; Inman, G.J.; Proby, C.M.; Leigh, I.M.; Harwood, C.A.; et al. The Genomic Landscape of Actinic Keratosis. J. Investig. Dermatol. 2021, 141, 1664–1674.e7. [Google Scholar] [CrossRef]
- Madani, S.; Marwaha, S.; Dusendang, J.R.; Alexeeff, S.; Pham, N.; Chen, E.H.; Han, S.; Herrinton, L.J. Ten-Year Follow-up of Persons with Sun-Damaged Skin Associated with Subsequent Development of Cutaneous Squamous Cell Carcinoma. JAMA Dermatol. 2021, 157, 559–565. [Google Scholar] [CrossRef]
- Boyle, J.; Briggs, J.; Mackie, R.M.; Junor, B.; Aitchison, T. Cancer, warts, and sunshine in renal transplant patients. A case-control study. Lancet 1984, 1, 702–705. [Google Scholar] [CrossRef]
- Frost, C.; Green, A.C.; Williams, G.M. The prevalence and determinants of solar keratoses at a subtropical latitude (Queensland, Australia). Br. J. Dermatol. 1998, 139, 1033–1039. [Google Scholar] [CrossRef]
- Dirschka, T.; Gupta, G.; Micali, G.; Stockfleth, E.; Basset-Séguin, N.; Del Marmol, V.; Dummer, R.; Jemec, G.B.E.; Malvehy, J.; Peris, K.; et al. Real-world approach to actinic keratosis management: Practical treatment algorithm for office-based dermatology. J. Dermatol. Treat. 2017, 28, 431–442. [Google Scholar] [CrossRef]
- Worley, B.; Harikumar, V.; Reynolds, K.; Dirr, M.A.; Christensen, R.E.; Anvery, N.; Yi, M.D.; Poon, E.; Alam, M. Treatment of actinic keratosis: A systematic review. Arch. Dermatol. Res. 2023, 315, 1099–1108. [Google Scholar] [CrossRef]
- Arcuri, D.; Ramchatesingh, B.; Lagacé, F.; Iannattone, L.; Netchiporouk, E.; Lefrançois, P.; Litvinov, I.V. Pharmacological Agents Used in the Prevention and Treatment of Actinic Keratosis: A Review. Int. J. Mol. Sci. 2023, 24, 4989. [Google Scholar] [CrossRef]
- McDaniel, B.; Badri, T.; Steele, R.B. Basal Cell Carcinoma. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Werner, R.N.; Stockfleth, E.; Connolly, S.M.; Correia, O.; Erdmann, R.; Foley, P.; Gupta, A.; Jacobs, A.; Kerl, H.; Lim, H.; et al. Evidence-and consensus-based (S3) Guidelines for the Treatment of Actinic Keratosis-International League of Dermatological Societies in cooperation with the European Dermatology Forum-Short version. J. Eur. Acad. Dermatol. Venereol. 2015, 29, 2069–2079. [Google Scholar] [CrossRef]
- Walker, J.L.; Siegel, J.A.; Sachar, M.; Pomerantz, H.; Chen, S.C.; Swetter, S.M.; Dellavalle, R.P.; Stricklin, G.P.; Qureshi, A.A.; DiGiovanna, J.J.; et al. 5-Fluorouracil for Actinic Keratosis Treatment and Chemoprevention: A Randomized Controlled Trial. J. Investig. Dermatol. 2017, 137, 1367–1370. [Google Scholar] [CrossRef]
- Sharma, M.; Sharma, G.; Singh, B.; Katare, O.P. Actinic keratosis and imiquimod: A review of novel carriers and patents. Expert Opin. Drug Deliv. 2019, 16, 101–112. [Google Scholar] [CrossRef]
- Javor, S.; Cozzani, E.; Parodi, A. Topical treatment of actinic keratosis with 3.0% diclofenac in 2.5% hyaluronan gel: Review of the literature about the cumulative evidence of its efficacy and safety. G. Ital. Dermatol. Venereol. 2016, 151, 275–280. [Google Scholar]
- Schlesinger, T.; Stockfleth, E.; Grada, A.; Berman, B. Tirbanibulin for Actinic Keratosis: Insights into the Mechanism of Action. Clin. Cosmet. Investig. Dermatol. 2022, 15, 2495–2506. [Google Scholar] [CrossRef]
- Szeimies, R.-M.; Dirschka, T.; Fargnoli, M.C.; Gilaberte, Y.; Hædersdal, M.; Chavda, R.; Calzavara-Pinton, P. A Review of MAL-PDT for the Treatment Strategy of Actinic Keratosis: Broader Clinical Perspectives Beyond the Data and Guideline Recommendations. Dermatol. Ther. 2023, 13, 1409–1421. [Google Scholar] [CrossRef]
- Sachs, D.L.; Kang, S.; Hammerberg, C.; Helfrich, Y.; Karimipour, D.; Orringer, J.; Johnson, T.; Hamilton, T.A.; Fisher, G.; Voorhees, J.J. Topical fluorouracil for actinic keratoses and photoaging: A clinical and molecular analysis. Arch. Dermatol. 2009, 145, 659–666. [Google Scholar] [CrossRef]
- Guimaraes, C.O.Z.; Miot, H.A.; Bagatin, E. Five percent 5-fluorouracil in a cream or for superficial peels in the treatment of advanced photoaging of the forearms: A randomized comparative study. Dermatol. Surg. 2014, 40, 610–617. [Google Scholar]
- Korgavkar, K.; Lee, K.C.; Weinstock, M.A. Veterans Affairs Keratinocyte Carcinoma Chemoprevention (VAKCC) Trial Group. Effect of Topical Fluorouracil Cream on Photodamage: Secondary Analysis of a Randomized Clinical Trial. JAMA Dermatol. 2017, 153, 1142–1146. [Google Scholar] [CrossRef]
- Kohl, E.; Torezan, L.A.; Landthaler, M.; Szeimies, R.M. Aesthetic effects of topical photodynamic therapy. J. Eur. Acad. Dermatol. Venereol. 2010, 24, 1261–1269. [Google Scholar] [CrossRef]
- Sanclemente, G.; Medina, L.; Villa, J.-F.; Barrera, L.-M.; Garcia, H.-I. A prospective split-face double-blind randomized placebo-controlled trial to assess the efficacy of methyl aminolevulinate + red-light in patients with facial photodamage. J. Eur. Acad. Dermatol. Venereol. 2011, 25, 49–58. [Google Scholar] [CrossRef]
- Le Pillouer-Prost, A.; Cartier, H. Photodynamic Photorejuvenation: A Review. Dermatol. Surg. 2016, 42, 21–30. [Google Scholar] [CrossRef]
- Morton, C.A.; Szeimies, R.M.; Sidoroff, A.; Braathen, L.R. European guidelines for topical photodynamic therapy part 2: Emerging indications--field cancerization, photorejuvenation and inflammatory/infective dermatoses. J. Eur. Acad. Dermatol. Venereol. 2013, 27, 672–679. [Google Scholar] [CrossRef] [PubMed]
- Fonda-Pascual, P.; Moreno-Arrones, O.M.; Alegre-Sanchez, A.; Saceda-Corralo, D.; Buendia-Castaño, D.; Pindado-Ortega, C.; Fernandez-Gonzalez, P.; Velazquez-Kennedy, K.; Calvo-Sánchez, M.I.; Harto-Castaño, A.; et al. In situ production of ROS in the skin by photodynamic therapy as a powerful tool in clinical dermatology. Methods 2016, 109, 190–202. [Google Scholar] [CrossRef] [PubMed]
- Szeimies, R.; Lischner, S.; Philipp-Dormston, W.; Walker, T.; Hiepe-Wegener, D.; Feise, K.; Podda, M.; Prager, W.; Kohl, E.; Karrer, S. Photodynamic therapy for skin rejuvenation: Treatment options-results of a consensus conference of an expert group for aesthetic photodynamic therapy. J. Dtsch. Dermatol. Ges. 2013, 11, 632–636. [Google Scholar] [CrossRef] [PubMed]
- Bruscino, N.; Rossi, R.; Dindelli, M.; Ghersetich, I.; Lotti, T. Therapeutic Hotline: Facial skin rejuvenation in a patient treated with photodynamic therapy for actinic keratosis. Dermatol. Ther. 2010, 23, 86–89. [Google Scholar] [CrossRef]
- Lane, K.L.; Hovenic, W.; Ball, K.; Zachary, C.B. Daylight photodynamic therapy: The Southern California experience. Lasers Surg. Med. 2015, 47, 168. [Google Scholar] [CrossRef]
- Spataro, E.A.; Dierks, K.; Carniol, P.J. Microneedling-Associated Procedures to Enhance Facial Rejuvenation. Facial Plast. Surg. Clin. N. Am. 2022, 30, 389–397. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).