Cassia alata (Linnaeus) Roxburgh for Skin: Natural Remedies for Atopic Dermatitis in Asia and Their Pharmacological Activities
Abstract
1. Introduction
2. Botanical Description and Classification
3. Ethnomedical Uses
4. Phytochemistry
5. Pharmacological Properties
5.1. Antimicrobial Activity
5.2. Wound Healing
5.3. Anti-Inflammatory
5.4. Antioxidant Activities
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Goh, Y.-Y.; Keshavarzi, F.; Chew, Y.L. Prevalence of atopic dermatitis and pattern of drug therapy in Malaysian children. Dermatitis 2018, 29, 151–161. [Google Scholar] [CrossRef]
- Buddenkotte, J.; Steinhoff, M. Pathophysiology and therapy of pruritus in allergic and atopic diseases. Allergy 2010, 65, 805–821. [Google Scholar] [CrossRef]
- Avena-Woods, C. Overview of atopic dermatitis. Am. J. Manag. Care 2017, 23, S115–S123. [Google Scholar]
- Chew, Y.-L.; Al-Nema, M.; Ong, V.W.-M. Management and treatment of atopic dermatitis with modern therapies, complementary and alternative medicines: A review. Orient. Pharm. Exp. Med. 2018, 18, 67–76. [Google Scholar] [CrossRef]
- Silverberg, J.I.; Vakharia, P.P.; Chopra, R.; Sacotte, R.; Patel, N.; Immaneni, S.; White, T.; Kantor, R.; Hsu, D.Y. Phenotypical differences of childhood-and adult-onset atopic dermatitis. J. Allergy Clin. Immunol. Pract. 2018, 6, 1306–1312. [Google Scholar] [CrossRef]
- Chew, Y.-L.; Khor, M.-A.; Xu, Z.; Lee, S.-K.; Keng, J.-W.; Sang, S.-H.; Akowuah, G.A.; Goh, K.W.; Liew, K.B.; Ming, L.C. Cassia alata, Coriandrum sativum, Curcuma longa and Azadirachta indica: Food ingredients as complementary and alternative therapies for atopic dermatitis—A comprehensive review. Molecules 2022, 27, 5475. [Google Scholar] [CrossRef]
- Chew, Y.-L. The beneficial properties of virgin coconut oil in management of atopic dermatitis. Pharmacogn. Rev. 2019, 13, 24. [Google Scholar] [CrossRef]
- Lee, J.; Kim, J.; Seok, J.; Kim, B. Correlation between socio-economic status and atopic dermatitis in Korean adults: The Korea national health and nutrition examination survey (2007–2014). J. Eur. Acad. Dermatol. Venereol. 2017, 31, 1509–1515. [Google Scholar] [CrossRef]
- Lee, K.-S.; Rha, Y.-H.; Oh, I.-H.; Choi, Y.-S.; Choi, S.-H. Socioeconomic and sociodemographic factors related to allergic diseases in Korean adolescents based on the Seventh Korea Youth Risk Behavior Web-based Survey: A cross-sectional study. BMC Pediatr. 2016, 16, 1–9. [Google Scholar] [CrossRef]
- Ho, C.-L.; Chang, L.-I.; Wu, W.-F. The prevalence and risk factors of atopic dermatitis in 6–8 year-old first graders in Taipei. Pediatr. Neonatol. 2019, 60, 166–171. [Google Scholar] [CrossRef] [PubMed]
- Lin, M.H.; Hsieh, C.J.; Caffrey, J.L.; Lin, Y.S.; Wang, I.J.; Ho, W.C.; Chen, P.C.; Wu, T.N.; Lin, R.S. Fetal growth, obesity, and atopic disorders in adolescence: A retrospective birth cohort study. Paediatr. Perinat. Epidemiol. 2015, 29, 472–479. [Google Scholar] [CrossRef] [PubMed]
- Hwang, C.-Y.; Chen, Y.-J.; Lin, M.-W.; Chen, T.-J.; Chu, S.-Y.; Chen, C.-C.; Lee, D.-D.; Chang, Y.-T.; Wang, W.-J.; Liu, H.-N. Prevalence of atopic dermatitis, allergic rhinitis and asthma in Taiwan: A national study 2000 to 2007. Acta Derm. Venereol. 2010, 90, 589–594. [Google Scholar]
- Xiao, Y.; Huang, X.; Jing, D.; Huang, Y.; Chen, L.; Zhang, X.; Zhao, S.; Zhang, M.; Luo, Z.; Su, J. The prevalence of atopic dermatitis and chronic spontaneous urticaria are associated with parental socioeconomic status in adolescents in China. Acta Derm. Venereol. 2019, 99, 321–326. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Li, P.; Tang, J.; Han, X.; Zou, X.; Xu, G.; Xu, Z.; Wei, F.; Liu, Q.; Wang, M. Prevalence of atopic dermatitis in Chinese children aged 1–7 ys. Sci. Rep. 2016, 6, 29751. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Li, L.-F.; Zhao, D.-Y.; Shen, Y.-W. Prevalence and clinical features of atopic dermatitis in China. BioMed Res. Int. 2016, 2016, 2568301. [Google Scholar] [CrossRef]
- Okada, Y.; Kumagai, H.; Morikawa, Y.; Akasawa, A. Epidemiology of pediatric allergic diseases in the Ogasawara Islands. Allergol. Int. 2016, 65, 37–43. [Google Scholar] [CrossRef][Green Version]
- Futamura, M.; Ohya, Y.; Akashi, M.; Adachi, Y.; Odajima, H.; Akiyama, K.; Akasawa, A. Age-related prevalence of allergic diseases in Tokyo schoolchildren. Allergol. Int. 2011, 60, 509–515. [Google Scholar] [CrossRef]
- Yura, A.; Kouda, K.; Iki, M.; Shimizu, T. Trends of allergic symptoms in school children: Large-scale long-term consecutive cross-sectional studies in Osaka Prefecture, Japan. Pediatr. Allergy Immunol. 2011, 22, 631–637. [Google Scholar] [CrossRef]
- Lee, K.S.; Oh, I.-H.; Choi, S.H.; Rha, Y.-H. Analysis of epidemiology and risk factors of atopic dermatitis in Korean children and adolescents from the 2010 Korean national health and nutrition examination survey. BioMed Res. Int. 2017, 2017, 5142754. [Google Scholar] [CrossRef]
- Parveen, S.; Shahzad, A. A review on in vitro culture of Cassia alata Linn. (Senna alata): Analysis of metabolites and biological activities. J. Funct. Environ. Bot. 2015, 5, 78. [Google Scholar] [CrossRef]
- Abille, J. A Review on the Medical Plant Cassia alata (L.) Roxb. (Fabaceae). Available online: https://www.researchgate.net/profile/Jaydhelle-Mae-Abille/publication/334680364_A_REVIEW_ON_THE_MEDICINAL_PLANT_CASSIA_ALATA_L_ROXB_FABACEAE/links/5d39c06da6fdcc370a5fcfae/A-REVIEW-ON-THE-MEDICINAL-PLANT-CASSIA-ALATA-L-ROXB-FABACEAE.pdf (accessed on 25 September 2022).
- Abdulwaliyu, I.; Arekemase, S.; Bala, S.; Ibraheem, A.; Dakare, A.; Sangodare, R.; Gero, M. Nutritional Properties of Senna alata linn leaf and flower. Int. J. Mod. Biol. Med. 2013, 4, 1–11. [Google Scholar]
- Fatmawati, S.; Purnomo, A.S.; Bakar, M.F.A. Chemical constituents, usage and pharmacological activity of Cassia alata. Heliyon 2020, 6, e04396. [Google Scholar] [CrossRef]
- Meenupriya, J.; Vinisha, A.S.; Priya, P. Cassia alata and Cassia auriculata—Review of their bioactive potential. World J. Pharm. Sci. 2014, 1760–1769. [Google Scholar]
- Onyegeme-Okerenta, B.; Nwosu, T.; Wegwu, M. Proximate and phytochemical composition of leaf extract of Senna alata (L.) Roxb. J. Pharmacogn. Phytochem. 2017, 6, 320–326. [Google Scholar]
- Oladeji, O.S.; Adelowo, F.E.; Oluyori, A.P.; Bankole, D.T. Ethnobotanical description and biological activities of Senna alata. Evid. Based Complement. Altern. Med. 2020, 2020, 2580259. [Google Scholar] [CrossRef]
- Adigun, R.A.; Faruq, U.Z.; Birnin Yauri, U.A.; Oyeniyi, Y.J. Analysis of amino and fatty acids composition of Senna alata seed. Am. Chem. Sci. J. 2015, 7, 1–6. [Google Scholar] [CrossRef]
- Missouri Botanical Garden. Senna alata. Available online: https://www.missouribotanicalgarden.org/PlantFinder/PlantFinderDetails.aspx?taxonid=280477&isprofile=0&cv=5 (accessed on 21 June 2022).
- Oladeji, S.O.; Adelowo, F.E.; Odelade, K.A. Mass spectroscopic and phytochemical screening of phenolic compounds in the leaf extract of Senna alata (L.) Roxb.(Fabales: Fabaceae). Braz. J. Biol. Sci. 2016, 3, 209–219. [Google Scholar] [CrossRef]
- Hennebelle, T.; Weniger, B.; Joseph, H.; Sahpaz, S.; Bailleul, F. Senna alata. Fitoterapia 2009, 80, 385–393. [Google Scholar] [CrossRef]
- Ranjanie, D.; Yuhanis, F.; Mohammed Ali, N.; Fouad Saleih, R.; Aman Shah, A. A review on Cassia alata: Pharmacological, traditional and medicinal aspects. Aust. Herb. Insight 2019, 2, E016–E021. [Google Scholar]
- National Park of Singapore. Senna alata (Linnaeus) Roxburgh. Available online: https://www.nparks.gov.sg/florafaunaweb/flora/2/4/2450 (accessed on 22 September 2022).
- West African Health Organization. West African Herbal Pharmacopoeia. Available online: https://www.wahooas.org/web-ooas/sites/default/files/publications/2185/west-african-herbal-pharmacopoeiaok.pdf (accessed on 24 September 2022).
- Schmelzer, G.H.; Gurib-Fakim, A.E. Medicinal Plants; Prota Foundation: Wageningen, The Netherlands, 2008; Volume 11. [Google Scholar]
- Gritsanapan, W.; Mangmeesri, P. Standardized Senna alata leaf extract. J. Health Res. 2009, 23, 59–64. [Google Scholar]
- Globinmed. Senna alata (L.) Roxb. Available online: https://www.globinmed.com/index.php?option=com_content&view=article&id=106145:senna-alata-l-roxb&catid=286&Itemid=357 (accessed on 23 June 2021).
- Phansawan, B.; Pongsabangpho, S. Determination of gallic acid and rutin in extracts Cassia alata and Andrographis paniculata. Sci. Asia 2014, 40, 414–419. [Google Scholar] [CrossRef]
- Rahman, M.; Ali, M.; Ali, M.; Moynul Hasan, A. Studies on the lipid and glyceride compositions of Cassia alata seed oil. Bangladesh J. Sci. Ind. Res. 2006, 41, 83–88. [Google Scholar] [CrossRef]
- Muhammad, S.L.; Wada, Y.; Mohammed, M.; Ibrahim, S.; Musa, K.Y.; Olonitola, O.S.; Ahmad, M.H.; Mustapha, S.; Abdul Rahman, Z.; Sha’aban, A. Bioassay-guided identification of bioactive compounds from Senna alata L. against methicillin-resistant Staphylococcus aureus. Appl. Microbiol. 2021, 1, 520–536. [Google Scholar] [CrossRef]
- Geoghegan, J.A.; Irvine, A.D.; Foster, T.J. Staphylococcus aureus and atopic dermatitis: A complex and evolving relationship. Trends Microbiol. 2018, 26, 484–497. [Google Scholar] [CrossRef] [PubMed]
- Blicharz, L.; Rudnicka, L.; Samochocki, Z. Staphylococcus aureus: An underestimated factor in the pathogenesis of atopic dermatitis? Postep. Dermatol. Alergol. 2019, 36, 11. [Google Scholar] [CrossRef]
- Simpson, E.L.; Villarreal, M.; Jepson, B.; Rafaels, N.; David, G.; Hanifin, J.; Taylor, P.; Boguniewicz, M.; Yoshida, T.; De Benedetto, A. Patients with atopic dermatitis colonized with Staphylococcus aureus have a distinct phenotype and endotype. J. Investig. Dermatol. 2018, 138, 2224–2233. [Google Scholar] [CrossRef]
- Kanedi, M. Healing effect of leaf extract of candlebush (Cassia alata L.) on cutaneous wound infected with Trichophyton rubrum. World J. Pharm. Life Sci. 2016, 2, 42–50. [Google Scholar]
- Riaz, A.; Rasul, A.; Hussain, G.; Zahoor, M.K.; Jabeen, F.; Subhani, Z.; Younis, T.; Ali, M.; Sarfraz, I.; Selamoglu, Z. Astragalin: A bioactive phytochemical with potential therapeutic activities. Adv. Pharmacol. Sci. 2018, 2018, 9794625. [Google Scholar] [CrossRef]
- Bertino, L.; Guarneri, F.; Cannavò, S.P.; Casciaro, M.; Pioggia, G.; Gangemi, S. Oxidative stress and atopic dermatitis. Antioxidants 2020, 9, 196. [Google Scholar] [CrossRef]
- Vargas, F.; Díaz, Y.; Carbonell, K. Antioxidant and scavenging activity of emodin, aloe-emodin, and rhein on free-radical and reactive oxygen species. Pharm. Biol. 2004, 42, 342–348. [Google Scholar] [CrossRef]
- Xu, Y.; Tang, G.; Zhang, C.; Wang, N.; Feng, Y. Gallic acid and diabetes mellitus: Its association with oxidative stress. Molecules 2021, 26, 7115. [Google Scholar] [CrossRef]
- Ogonowska, P.; Gilaberte, Y.; Barańska-Rybak, W.; Nakonieczna, J. Colonization with Staphylococcus aureus in atopic dermatitis patients: Attempts to reveal the unknown. Front. Microbiol. 2021, 11, 3468. [Google Scholar] [CrossRef] [PubMed]
- Lübbe, J. Secondary infections in patients with atopic dermatitis. Am. J. Clin. Dermatol. 2003, 4, 641–654. [Google Scholar] [CrossRef] [PubMed]
- Alam, M.; Karim, M.; Khan, S.N. Antibacterial activity of different organic extracts of Achyranthes aspera and Cassia alata. J. Sci. Res. 2009, 1, 393–398. [Google Scholar] [CrossRef]
- Somchit, M.; Reezal, I.; Nur, I.E.; Mutalib, A. In vitro antimicrobial activity of ethanol and water extracts of Cassia alata. J. Ethnopharmacol. 2003, 84, 1–4. [Google Scholar] [CrossRef]
- El-Mahmood, A.; Doughari, J. Phytochemical screening and antibacterial evaluation of the leaf and root extracts of Cassia alata Linn. Afr. J. Pharm. Pharmacol. 2008, 2, 124–129. [Google Scholar]
- Iraqui, P.; Chakraborty, T.; Das, M.K.; Yadav, R. Herbal antimicrobial gel with leaf extract of Cassia alata L. J. Drug Deliv. Ther. 2019, 9, 82–94. [Google Scholar] [CrossRef]
- Hazni, H.; Ahmad, N.; Hitotsuyanagi, Y.; Takeya, K.; Choo, C.-Y. Phytochemical constituents from Cassia alata with inhibition against methicillin-resistant Staphylococcus aureus (MRSA). Planta Med. 2008, 74, 1802–1805. [Google Scholar] [CrossRef]
- Paul, B.; Mitra, P.; Ghosh, T.; Salhan, R.; Singh, T.A.; Chakrabarti, A.; Gupta, S.; Basu, B.; Mitra, P.K. Isolation and structural determination of an anti bacterial constituent from the leaves of Cassia alata Linn. J. Pharmacogn. Phytochem. 2013, 2, 326–333. [Google Scholar]
- Kępa, M.; Miklasińska-Majdanik, M.; Wojtyczka, R.D.; Idzik, D.; Korzeniowski, K.; Smoleń-Dzirba, J.; Wąsik, T.J. Antimicrobial potential of caffeic acid against Staphylococcus aureus clinical strains. BioMed. Res. Int. 2018, 2018, 7413504. [Google Scholar] [CrossRef]
- Chew, Y.L.; Mahadi, A.M.; Wong, K.M.; Goh, J.K. Anti-methicillin-resistance Staphylococcus aureus (MRSA) compounds from Bauhinia kockiana Korth. And their mechanism of antibacterial activity. BMC Complement. Altern. Med. 2018, 18, 70. [Google Scholar] [CrossRef] [PubMed]
- Andrade, M.; Benfeito, S.; Soares, P.; Magalhães e Silva, D.; Loureiro, J.; Borges, A.; Borges, F.; Simoes, M. Fine-tuning of the hydrophobicity of caffeic acid: Studies on the antimicrobial activity against Staphylococcus aureus and Escherichia coli. RSC Adv. 2015, 5, 53915–53925. [Google Scholar] [CrossRef]
- Chew, Y.L.; Goh, J.K.; Arasi, C. Investigation on antibacterial activity of pyrogallol in methicillin resistant Staphylococcus aureus. Curr. Trends Biotechnol. Pharm. 2020, 14, 176–180. [Google Scholar] [CrossRef]
- Chew, Y.-L.; Arasi, C.; Goh, J.-K. Pyrogallol Induces Antimicrobial Effect and Cell Membrane Disruption on Methicillin-Resistant Staphylococcus aureus (MRSA). Curr. Bioact. Compd. 2022, 18, 38–46. [Google Scholar] [CrossRef]
- Shi, Y.-g.; Zhang, R.-r.; Zhu, C.-m.; Liang, X.-r.; Ettelaie, R.; Jiang, L.; Lin, S. On the mechanism behind enhanced antibacterial activity of alkyl gallate esters against foodborne pathogens and its application in Chinese icefish preservation. Food Microbiol. 2021, 99, 103817. [Google Scholar] [CrossRef]
- Hirai, I.; Okuno, M.; Katsuma, R.; Arita, N.; Tachibana, M.; Yamamoto, Y. Characterisation of anti-Staphylococcus aureus activity of quercetin. Int. J. Food Sci. Technol. 2010, 45, 1250–1254. [Google Scholar] [CrossRef]
- Betts, J.W.; Sharili, A.S.; Phee, L.M.; Wareham, D.W. In vitro activity of epigallocatechin gallate and quercetin alone and in combination versus clinical isolates of methicillin-resistant Staphylococcus aureus. J. Nat. Prod. 2015, 78, 2145–2148. [Google Scholar] [CrossRef]
- Nguyen, T.L.A.; Bhattacharya, D. Antimicrobial activity of quercetin: An approach to its mechanistic principle. Molecules 2022, 27, 2494. [Google Scholar] [CrossRef]
- Fras-Zemljič, L.; Kokol, V.; Čakara, D. Antimicrobial and antioxidant properties of chitosan-based viscose fibres enzymatically functionalized with flavonoids. Text. Res. J. 2011, 81, 1532–1540. [Google Scholar] [CrossRef]
- Ahmad, A.; Kaleem, M.; Ahmed, Z.; Shafiq, H. Therapeutic potential of flavonoids and their mechanism of action against microbial and viral infections—A review. Food Res. Int. 2015, 77, 221–235. [Google Scholar] [CrossRef]
- Yang, D.; Wang, T.; Long, M.; Li, P. Quercetin: Its Main Pharmacological Activity and Potential Application in Clinical Medicine. Oxidative Med. Cell. Longev. 2020, 2020, 8825387. [Google Scholar] [CrossRef] [PubMed]
- Yu, L.; Xiang, H.; Fan, J.; Wang, D.; Yang, F.; Guo, N.; Jin, Q.; Deng, X. Global transcriptional response of Staphylococcus aureus to rhein, a natural plant product. J. Biotechnol. 2008, 135, 304–308. [Google Scholar] [CrossRef]
- Mathew-Steiner, S.S.; Roy, S.; Sen, C.K. Collagen in Wound Healing. Bioengineering 2021, 8, 63. [Google Scholar] [CrossRef] [PubMed]
- Tokura, Y. Extrinsic and intrinsic types of atopic dermatitis. J. Dermatol. Sci. 2010, 58, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Palanichamy, S.; Bhaskar, E.A.; Bakthavathsalam, R.; Nagarajan, S. Wound healing activity of Cassia alata. Fitoterapia 1991, 62, 153–156. [Google Scholar]
- Midawa, S.; Ali, B.; Mshelia, B.; Johnson, J. Cutaneous wound healing activity of the ethanolic extracts of the leaf of Senna alata L. (Fabaceae). J. Biol. Sci. Conserv. 2010, 2, 63–68. [Google Scholar]
- Cardoso, C.R.; Favoreto, S., Jr.; Oliveira, L.L.; Vancim, J.O.; Barban, G.B.; Ferraz, D.B.; Silva, J.S. Oleic acid modulation of the immune response in wound healing: A new approach for skin repair. Immunobiology 2011, 216, 409–415. [Google Scholar] [CrossRef]
- Mena, S.J.; Manosalva, C.; Carretta, M.D.; Teuber, S.; Olmo, I.; Burgos, R.A.; Hidalgo, M.A. Differential free fatty acid receptor-1 (FFAR1/GPR40) signalling is associated with gene expression or gelatinase granule release in bovine neutrophils. Innate Immun. 2016, 22, 479–489. [Google Scholar] [CrossRef]
- Knight, B.E.; Kozlowski, N.; Havelin, J.; King, T.; Crocker, S.J.; Young, E.E.; Baumbauer, K.M. TIMP-1 attenuates the development of inflammatory pain through MMP-dependent and receptor-mediated cell signaling mechanisms. Front. Mol. Neurosci. 2019, 12, 220. [Google Scholar] [CrossRef]
- Villaseñor, I.M.; Canlas, A.P.; Pascua, M.P.I.; Sabando, M.N.; Soliven, L.A.P. Bioactivity studies on Cassia alata Linn. leaf extracts. Phytother. Res. 2002, 16, 93–96. [Google Scholar] [CrossRef] [PubMed]
- Lewis, A.; Levy, A. Anti-inflammatory activities of Cassia alata leaf extract in complete Freund’s adjuvant arthritis in rats. West Indian Med. J. 2011, 60, 615–621. [Google Scholar] [PubMed]
- Sivaranjani, N.; Rao, S.V.; Rajeev, G. Role of reactive oxygen species and antioxidants in atopic dermatitis. J. Clin. Diagn. Res. 2013, 7, 2683–2685. [Google Scholar] [CrossRef] [PubMed]
- Chatterjee, S.; Chatterjee, S.; Dey, K.; Dutta, S. Study of antioxidant activity and immune stimulating potency of the ethnomedicinal plant, Cassia alata (L.) Roxb. Med. Aromat. Plants 2013, 2, 1000131. [Google Scholar] [CrossRef]
- Chua, L.Y.W.; Chua, B.L.; Figiel, A.; Chong, C.H.; Wojdyło, A.; Szumny, A.; Lech, K. Characterisation of the convective hot-air drying and vacuum microwave drying of Cassia alata: Antioxidant activity, essential oil volatile composition and quality studies. Molecules 2019, 24, 1625. [Google Scholar] [CrossRef]
- Sagnia, B.; Fedeli, D.; Casetti, R.; Montesano, C.; Falcioni, G.; Colizzi, V. Antioxidant and anti-inflammatory activities of extracts from Cassia alata, Eleusine indica, Eremomastax speciosa, Carica papaya and Polyscias fulva medicinal plants collected in Cameroon. PLoS ONE 2014, 9, e103999. [Google Scholar] [CrossRef]
- Casetti, F.; Bartelke, S.; Biehler, K.; Augustin, M.; Schempp, C.; Frank, U. Antimicrobial activity against bacteria with dermatological relevance and skin tolerance of the essential oil from Coriandrum sativum L. fruits. Phytother. Res. 2012, 26, 420–424. [Google Scholar] [CrossRef]
- Nowak, A.; Cybulska, K.; Makuch, E.; Kucharski, Ł.; Różewicka-Czabańska, M.; Prowans, P.; Czapla, N.; Bargiel, P.; Petriczko, J.; Klimowicz, A. In vitro human skin penetration, antioxidant and antimicrobial activity of ethanol-water extract of fireweed (Epilobium angustifolium L.). Molecules 2021, 26, 329. [Google Scholar] [CrossRef]
- Sikora, B.C.; Wortzman, M.; Nelson, D.B.; Dover, J.S. A pilot study evaluating the efficacy and tolerability of a comprehensive, hydrating topical antioxidant developed specifically for men. J. Cosmet. Dermatol. 2021, 20, 2816. [Google Scholar] [CrossRef]

| Country | Prevalence of AD (%) (Age Group) | References | ||
|---|---|---|---|---|
| Children | Adolescent | General Population | ||
| Taiwan | 10.7 (6–7 year old) | 7.6 (13–14 year old) | 6.7 | [8,9,10,11,12] |
| China | 12.95 (1–7 year old) | 4.6 | 7.8 | [13,14,15] |
| Japan | 4.6 (7–12 year old) | n.a | [16,17,18] | |
| 10.9–19.6% (6–14 year old) | ||||
| South Korea | 15 (1–18 year old) 13.5 (7–18 year old) | n.a | [19] | |
| Malaysia | 13.4 (1–6 year old) | n.a | [1] | |
| Plant Parts | Traditional Uses | References |
|---|---|---|
| Whole plant | In Cuba, medical treatments include:
| [26,33] |
| Leaves | In Tanzania, Ghana, India, Indonesia, and Africa, the leaves are prepared as an infusion and decoction to treat constipation. The leaves are rubbed on the surface of the skin for the management of various skin diseases because of its various qualities:
In Nigeria, the fresh sap of leaves is rubbed into the skin for antifungal and ringworm treatment. The leaf decoction is also used for chronic lichen dermatosis management. In the Philippines, C. alata leaves are used on the skin for antibacterial, anti-inflammatory, analgesic and antifungal effects. The plant is also consumed to reduce blood glucose. In Togo and Gabon, the leaves are pounded and spread on the skin with palm oil for general skin disorder management. In India, the leaf decoction is used as:
In Brazil, the leaves are used to promote menstruation and improve blood circulation in female reproductive organs. In Egypt, a leaf decoction is used as a laxative to relieve constipation. In Sierra Leone, the leaves are prepared to relieve pain due to childbirth and abortion. In Thailand, leaf decoction (consisting of a minimum of 0.5% hydroxyanthracene derivatives) is used to relieve constipation. | [21,26,32,34,35] |
| Flowers | In Peru, an infusion prepared from flowers is used for diuretic and urinary tract infection treatment. In the Amazon, the Tikuna Indians prepare decoction of the flowers and consume them once daily to relieve constipation. | [21] |
| Seeds | In China, the seeds are made into a tea to improve eyesight and asthma. | [26] |
| Wood | Decoctions are consumed to reverse liver damage caused by hepatotoxins and to treat gastrointestinal issues (e.g., loss of appetite). The leaves are ground into powder and rubbed directly on the skin to counteract problems correlated with fungal infections. | [34,36] |
| (Not defined) | In Africa, plant parts serve the following medicinal purposes:
| [21] |
| Class | Phytochemical Compounds | Parts of Plant | Reference |
|---|---|---|---|
| Carotenoids | β-carotene | Leaves | [21,22] |
| Polyphenols (Phenolic acids) | Gallic acid | Leaves | [23,24,25,37] |
| Caffeic acid (3,4-Dihydroxycinnamic acid) | |||
| Chlorogenic acid | |||
| Flavonoids | Kaempferol | Leaves, seeds, twig, roots | [23,26] |
| Kaempferol-3-O-β-glucoside (astragalin) | |||
| trans-Dihydrokaempferol | |||
| Kaempferol-3-O-β-D-glucopyranosyl-(1→6)-β-D-glucopyranoside | |||
| Kaempferol-3-O-β-D glucopyranoside | |||
| Kaempferol 3-O-gentiobioside 50.0 ± 8.5 µM | |||
| 3,5,7,4′-Tetrahydroxy flavone | |||
| 2,5,7,4′-Tetrahydroxy isoflavones | |||
| 5,7,4′-Trihydroflavanone | |||
| 7,4′-Dihydroxy-5-methoxyflavone | |||
| Quercetin | |||
| Luteolin | |||
| Chrysoeriol-7-O-(2″-O-β-D mannopyranosyl)-β-D-allopyranoside | |||
| Rhamnetin-3-O-(2″-O-β-D-mannopyranosyl)-β-D-allopyranoside | |||
| ω-Hydroxyemodin | |||
| Ziganein | |||
| Apigenin | |||
| Naringenin | |||
| Propelargonidins | |||
| 2, 5, 7, 4′-Tetrahydroxy isoflavone | |||
| Alkaloids | Adenine | Leaves | [23,26] |
| Cannabinoid alkaloid (4-butylamine 10-methyl-6-hydroxy cannabinoid dronabinol) | |||
| Terpenoids | β-Caryophyllene | Leaves | [21] |
| Germacrene | |||
| α-Selinene | |||
| Bicyclogermacrene | |||
| Limonene | |||
| α-Phellandrene | |||
| α-Bulnesene | |||
| Anthraquinone derivatives | 1,3,5-Trihydroxy-7-methylanthracene-9,10-dione | Leaves, stem | [21,23,26] |
| 1,5,7-Trihydroxy-3-methyl-anthra-quinone | |||
| Aloe-emodin | |||
| Rhein | |||
| Emodin | |||
| Chrysophanol | |||
| 1,3,8-Trihydroxy-2-methyl anthraquinone | |||
| Hydroxymethyl anthraquinone | |||
| 1,5-Dihydroxy-8-methoxy-2-methylanthraquinone- | |||
| Alatinone | |||
| Alatonal | |||
| Sennoside A | |||
| Sennoside B | |||
| Sennoside C | |||
| Sennoside D | |||
| Chrysophanic acid | |||
| Physcione | |||
| Glycosides | Chrysoeriol-7-O-(2″-O-β-D-mannopyranosyl)-β-D-alopyranoside | Seed, stem, leaves | [23,26] |
| 3-O-Gentiobioside | |||
| Rhamnetin-3-O-(2″-O-β-D-mannopyranosyl)-β-D-allopyranoside | |||
| α-D-Galactopyranosyl | |||
| Fatty acids | 12-Methyltridecanoic acid | Seeds, leaves, flowers | [23,27,38,39] |
| 9-Hexadecenoic acid (Palmitoleic acid) | |||
| Hexadecanoic acid (methyl ester) (Palmitic acid) | |||
| n-Hexadecanoic acid (Palmitic acid) | |||
| cis-10-Heptadecenoic acid | |||
| Heptadecanoic acid | |||
| 9,12-Octadecadienoic acid (Linoleic acid) | |||
| Octadecanoic acid | |||
| Octadecanoic acid methyl ester | |||
| 9-Octadecenoic acid (Oleic acid) | |||
| 9,12-Epithio-9,11-octadecanoic acid 11-eicosenoic acid | |||
| Eicosanoic acid (Arachidic acid) | |||
| 15-Hydroxyl-9,12-octadecadienoic acid | |||
| 9,10-Dihydroxyoctadecanoic acid 6,9,12-octadecatrienoic acid (γ-linolenic acid) | |||
| Heneicosanoic acid | |||
| 9,10-Methylene-octadec-9-enoic acid (Sterculic acid) | |||
| Octadecanoic acid (Stearic acid) | |||
| 20-Methylheneicosanoic acid | |||
| Tricosanoic acid | |||
| Tetracosanoic acid | |||
| Pentacosanoic acid | |||
| Hexacosanoic acid | |||
| Behenic acid | |||
| 9-Dodecenoic acid | |||
| Nonadecanoic acid | |||
| 3,11-Tetradecadien-1-ol | |||
| Octadecanal | |||
| 9-Octadecenoicacid methyl ester | |||
| Phytosterols | β-Sitosterol | Leaves | [21] |
| Stigmasterol |
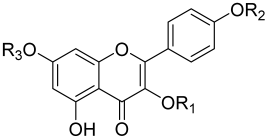 | |||||||
| Constituents | R1 | R2 | R3 | MIC Values (µg/mL) * | |||
| MIC10 | MIC30 | MIC50 | MIC80 | ||||
| Kaempferol | H | H | H | 6.0 ± 1.6 | 10.0 ± 0.7 | 13.0 ± 1.5 | 13.0 ± 1.5 |
| Kaempferol 3-O-β-glucopyranoside (Astragalin) | Glucoside | H | H | 40.0 ± 1.3 | 54.0 ± 1.2 | 83.0 ± 0.9 | 2000.0 ± 0.9 |
| Kaempferol 3-O-gentiobioside | Gentibiosyl | H | H | 110.0 ± 0.8 | 250.0 ± 1.1 | 560.0 ± 1.2 | 2000.0 ± 1.3 |
| Assays | Organism Tested | Dose/Concentration | Molecular Targets |
|---|---|---|---|
| LPS-induced mouse mastitis | Mouse mastitis | 10, 25 and 50 mg/kg | TNF-α ↓, IL-1β ↓, IL-6 ↓, p65 ┴, and IκBα ┴ |
| LPS-induced endotoxemia and lung injury in mice | Mice (lung) | 25, 50, and 75 mg/kg | TNF-α ┴, IL-1β ┴, and IL-6 ┴ |
| LPS-induced macrophages in mice | Mouse cells | 1–100 μg/mL | IL-6 ↓, MIP-1α ↓, MCP-1 ↓, NF-κB p65 ┴, IκBα ┴, and NO ┴ |
| LPS-induced RAW 264.7 cells | Mice (RAW 264.7 cells) | 1, 10, and 100 μM | NO ↓ and TNF-α ↓ |
| Inhibitory activity on the histamine release by KU812 cells | KU812 cells | 10 to 30 μmol/L | IL-4 ↓, IL-13 ↓, and (IFN- γ) no effect |
| LPS-induced Inflammation in RAW 264.7 cells | Mice (RAW 264.7 cells) | NO ┴, IL-6 ┴, and PGE2 ┴ | |
| P. gingivalis-induced human gingival epithelial (HGE) cells | Human gingival epithelial cells | COX-2 ┴, IL-6 ┴, IL-8 ┴, MMP-1 ┴, MMP-3 ┴, PGE-2 ┴, and IL-4 ┴ | |
| Anti-inflammatory effects on Leptospira interrogans-induced inflammatory response | Uterine and endometrial epithelial cells of mice | 100 μg/mL | p38 ┴, p-p38 MAPK ↓, ERK ┴, JNK ┴, and p-p65 ↓ |
| Protective effects against ovalbumin- (OVA-) induced allergic inflammation | Mouse model of allergic asthma | 0.5 mg/kg and 1 mg/kg | SOCS-3 ┴, SOCS-5 ┴, and IFN- γ ↑ |
| Alleviation in hepatic fibrosis function | Diabetic rats and nondiabetic | PAR2 ┴, IL-1β ↓, IL-6 ↓, TNF-α ↓, and TGF-β1 ┴ | |
| Prevention from atopic dermatitis | NC/Nga mice | 1.5 mg/kg | IgE ↓ |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yon, J.-A.-L.; Lee, S.-K.; Keng, J.-W.; Chow, S.-C.; Liew, K.-B.; Teo, S.-S.; Shaik Mossadeq, W.M.; Marriott, P.J.; Akowuah, G.A.; Ming, L.C.; et al. Cassia alata (Linnaeus) Roxburgh for Skin: Natural Remedies for Atopic Dermatitis in Asia and Their Pharmacological Activities. Cosmetics 2023, 10, 5. https://doi.org/10.3390/cosmetics10010005
Yon J-A-L, Lee S-K, Keng J-W, Chow S-C, Liew K-B, Teo S-S, Shaik Mossadeq WM, Marriott PJ, Akowuah GA, Ming LC, et al. Cassia alata (Linnaeus) Roxburgh for Skin: Natural Remedies for Atopic Dermatitis in Asia and Their Pharmacological Activities. Cosmetics. 2023; 10(1):5. https://doi.org/10.3390/cosmetics10010005
Chicago/Turabian StyleYon, Jessica-Ai-Lyn, Sue-Kei Lee, Jing-Wen Keng, Sek-Chuen Chow, Kai-Bin Liew, Swee-Sen Teo, Wan Mastura Shaik Mossadeq, Philip J. Marriott, Gabriel Akyirem Akowuah, Long Chiau Ming, and et al. 2023. "Cassia alata (Linnaeus) Roxburgh for Skin: Natural Remedies for Atopic Dermatitis in Asia and Their Pharmacological Activities" Cosmetics 10, no. 1: 5. https://doi.org/10.3390/cosmetics10010005
APA StyleYon, J.-A.-L., Lee, S.-K., Keng, J.-W., Chow, S.-C., Liew, K.-B., Teo, S.-S., Shaik Mossadeq, W. M., Marriott, P. J., Akowuah, G. A., Ming, L. C., Goh, B. H., & Chew, Y.-L. (2023). Cassia alata (Linnaeus) Roxburgh for Skin: Natural Remedies for Atopic Dermatitis in Asia and Their Pharmacological Activities. Cosmetics, 10(1), 5. https://doi.org/10.3390/cosmetics10010005









