Biomimetic Properties of Force-Spun PHBV Membranes Functionalised with Collagen as Substrates for Biomedical Application
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Methods
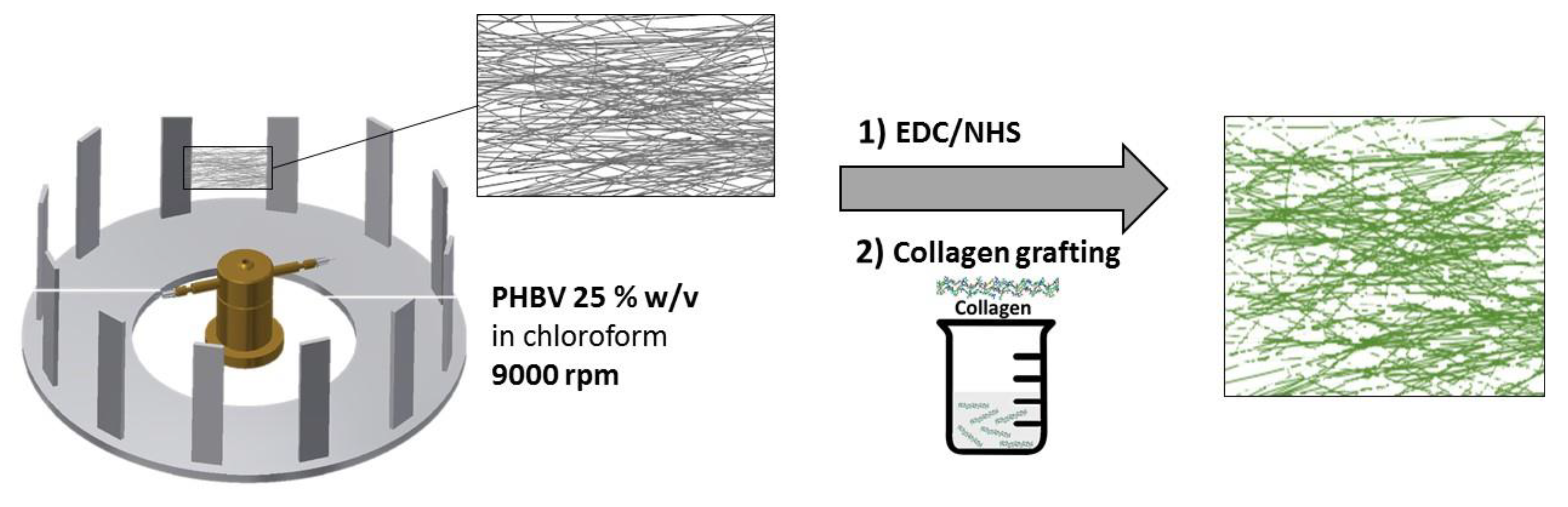
2.2.1. Preparation of PHBV Fibre Membranes and Films
2.2.2. Collagen Immobilisation
2.2.3. Fibre Morphology
2.2.4. ATR-FTIR (Attenuated Total Reflection, Fourier-Transform Infrared Spectroscopy)
2.2.5. XPS
2.2.6. Collagen Quantification—Sirius Red Assay
2.2.7. Contact Angle
2.2.8. Thermal Analysis
2.2.9. Hydrolytic Degradation
2.2.10. Cell Culture
2.2.11. Cytotoxicity (Live/Dead)
2.2.12. Metabolic Activity
2.2.13. Staining Cellular Cytoskeleton (Confocal)
2.3. Statistical Analysis
3. Results
3.1. Scaffold Characterisation
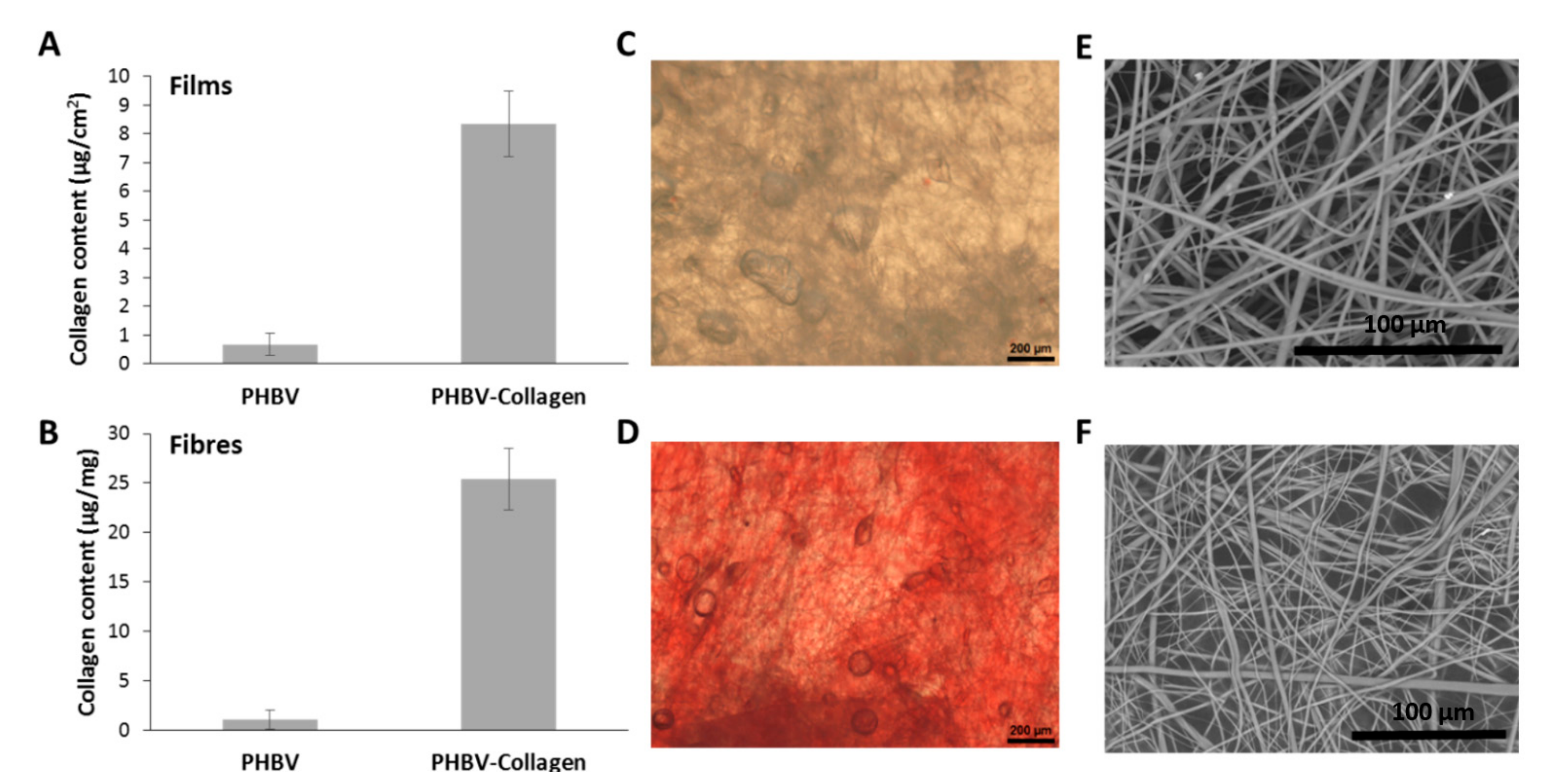
3.1.1. Fibre Collagen Content and Morphology
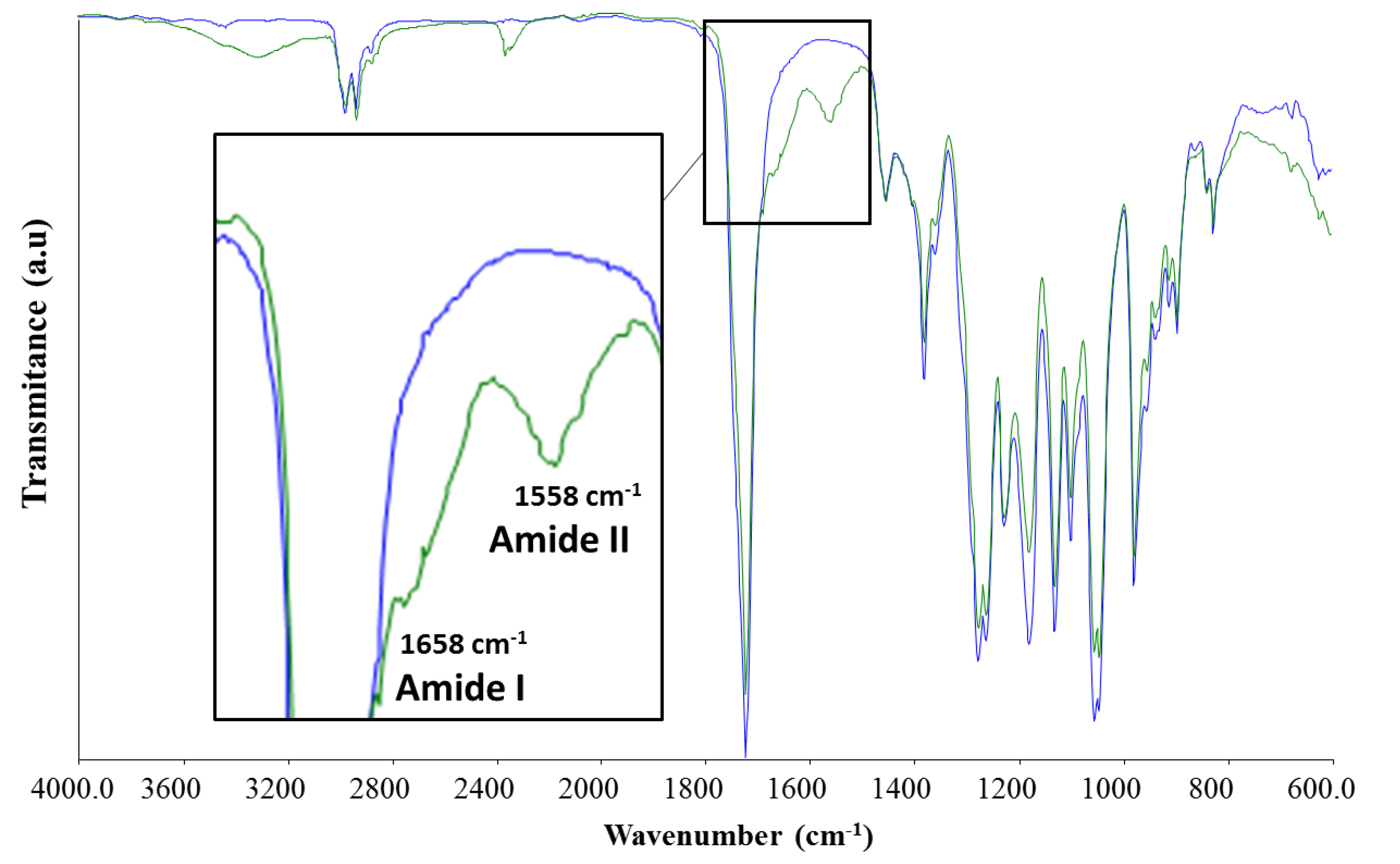
3.1.2. ATR-FTIR
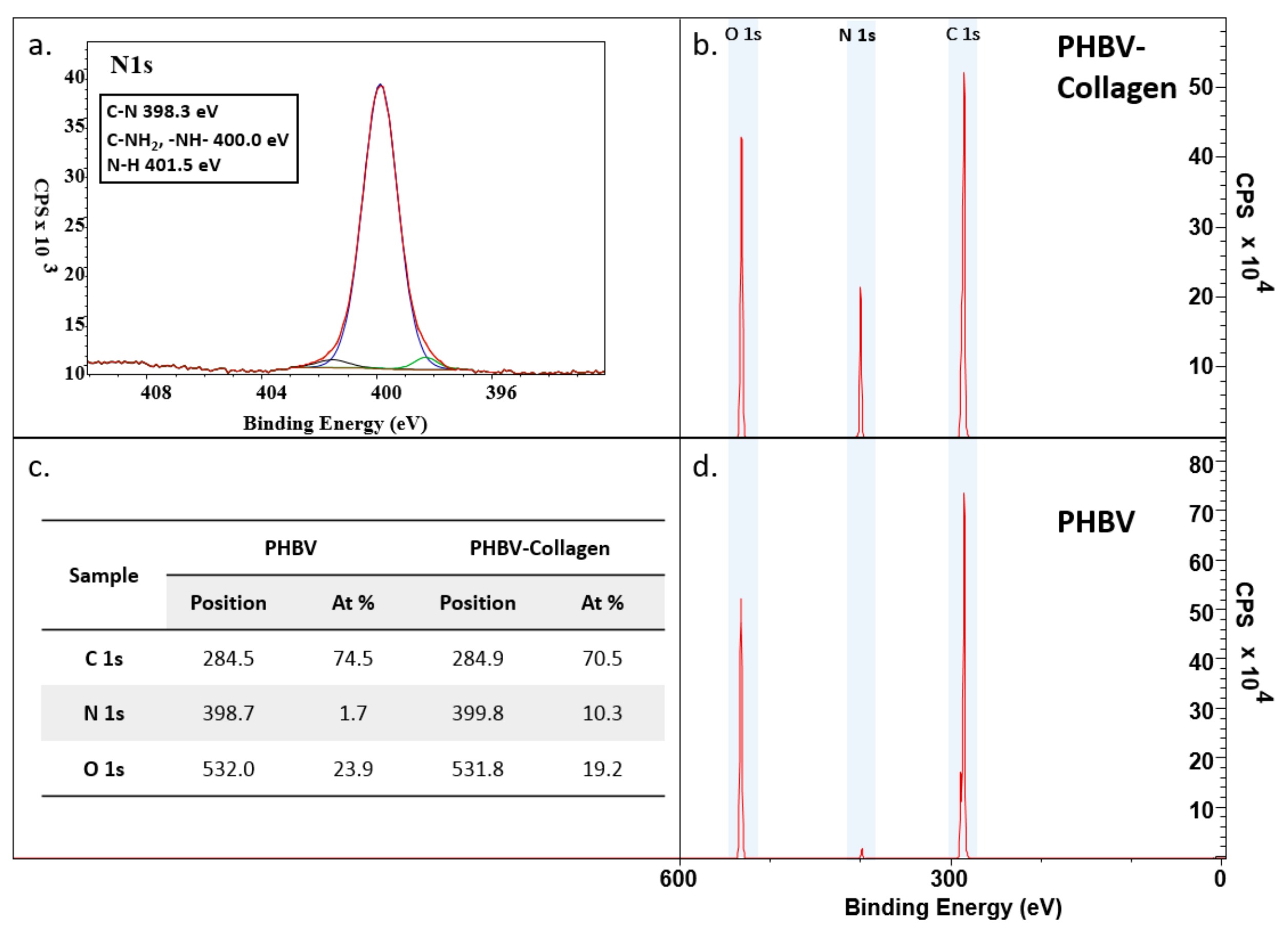
3.1.3. XPS
3.1.4. Differential Scanning Calorimetry
3.1.5. Contact Angle
3.1.6. In Vitro Degradation Study
3.2. Cytocompatibility Studies
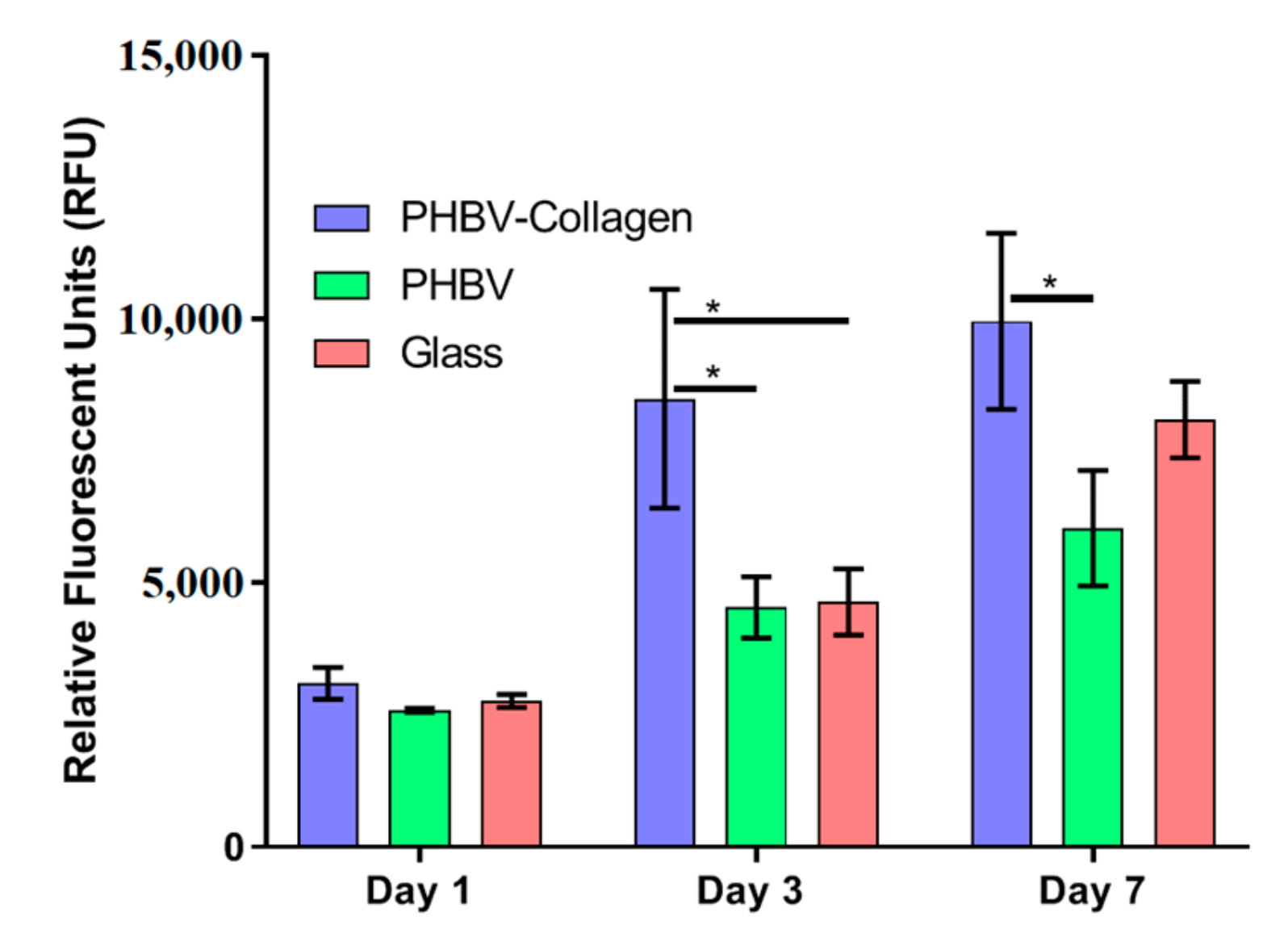
3.2.1. Metabolic Activity
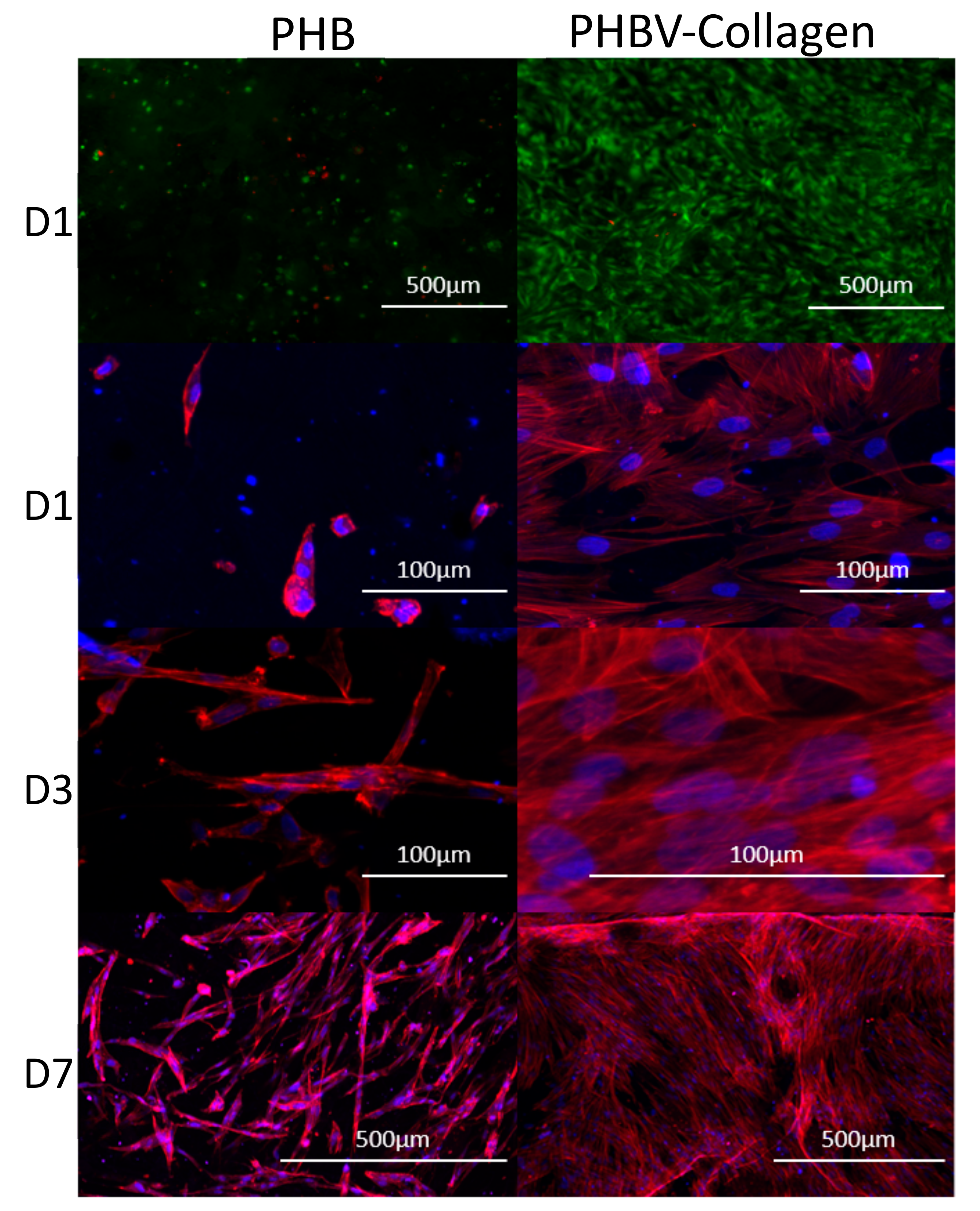
3.2.2. Cytocompatibility and Cell Morphology
4. Discussion
5. Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Williams, S.F.; Martin, D.P.; Horowitz, D.M.; Peoples, O.P. PHA applications: Addressing the price performance issue I. Tissue engineering. Int. J. Biol. Macromol. 1999, 25, 111–121. [Google Scholar] [CrossRef]
- Han, I.; Shim, K.J.; Kim, J.Y.; Im, S.U.; Sung, Y.K.; Kim, M.; Kang, I.-K.; Kim, J.C. Effect of poly(3-hydroxybutyrate-co-3-hydroxyvalerate) nanofiber matrices cocultured with hair follicular epithelial and dermal cells for biological wound dressing. Artif. Organs 2007, 31, 801–808. [Google Scholar] [CrossRef]
- Chen, G.; Wu, Q. The application of polyhydroxyalkanoates as tissue engineering materials. Biomaterials 2005, 26, 6565–6578. [Google Scholar] [CrossRef]
- Ghebi, A.; Khoshnevisan, K.; Ketabchi, N.; Derakhshan, M.A.; Babadi, A.A. Application of electrospun nanofibrous PHBV scaffold in neural graft and regeneration: A mini-review. Nanomed. Res. J. 2016, 1, 107–111. [Google Scholar]
- Keshel, S.H.; Biazar, E.; Rezaei, T.M.; Rahmati, R.M.; Ronaghi, A.; Ebrahimi, M.; Rad, H.; Sahebalzamani, A.; Rakhshan, A.; Afsordeh, K. The healing effect of unrestricted somatic stem cells loaded in collagen-modified nanofibrous PHBV scaffold on full-thickness skin defects. Artif. Cells Nanomed. Biotechnol. 2004, 42, 210–216. [Google Scholar] [CrossRef]
- Vasita, R.; Katti, D.S. Nanofibers and their applications in tissue engineering. Int. J. Nanomed. 2006, 1, 15–30. [Google Scholar] [CrossRef]
- Murphy, C.M.; Haugh, M.G.; O’Brien, F.J. The effect of mean pore size on cell attachment, proliferation and migration in collagen-glycosaminoglycan scaffolds for bone tissue engineering. Biomaterials 2010, 31, 461–466. [Google Scholar] [CrossRef]
- Sarkar, K.; Gomez, C.; Zambrano, S.; Ramirez, M.; de Hoyos, E.; Vasquez, H.; Lozano, K. Electrospinning to forcespinningTM. Mater. Today 2010, 13, 12–14. [Google Scholar] [CrossRef]
- Upson, S.J.; O’Haire, T.; Russell, S.J.; Dalgarno, K.; Ferreira, A.M. Centrifugally spun PHBV micro and nanofibres. Mater. Sci. Eng. C 2017, 76, 190–195. [Google Scholar] [CrossRef]
- Veleirinho, B.; Coelho, D.S.; Dias, P.F.; Maraschin, M.; Ribeiro-do-Valle, R.M.; Lopes-da-Silva, J.A. Nanofibrous poly(3-hydroxybutyrate-co-3-hydroxyvalerate)/chitosan scaffolds for skin regeneration. Int. J. Biol. Macromol. 2012, 51, 343–350. [Google Scholar] [CrossRef]
- Veleirinho, B.; Ribeiro-do-Valle, R.M.; Lopes-da-Silva, J.A. Processing conditions and characterization of novel electrospun poly(3-hydroxybutyrate-co-hydroxyvalerate)/chitosan blend fibers. Mater. Lett. 2011, 65, 2216–2219. [Google Scholar] [CrossRef]
- Peschel, G.; Dahse, H.-M.; Konrad, A.; Wieland, G.D.; Mueller, P.-J.; Martin, D.P.; Roth, M. Growth of keratinocytes on porous films of poly(3-hydroxybutyrate) and poly(4-hydroxybutyrate) blended with hyaluronic acid and chitosan. J. Biomed. Mater. Res. Part A 2008, 85, 1072–1081. [Google Scholar] [CrossRef]
- Wang, X.; Yan, H.; Zhou, Y.; Lou, X.; Zhang, Y. Fabrication of fibrous PLLA/PHBV scaffolds with shape memory capability. J. Control. Release 2017, 259, e144–e145. [Google Scholar] [CrossRef]
- Thadavirul, N.; Pavasant, P.; Supaphol, P. Fabrication and evaluation of polycaprolactone-poly(hydroxybutyrate) or poly(3-hydroxybutyrate-co-3-hydroxyvalerate) dual-leached porous scaffolds for bone tissue engineering applications. Macromol. Mater. Eng. 2017, 302, 1600289. [Google Scholar] [CrossRef]
- Li, W.; Nooeaid, P.; Roether, J.A.; Schubert, D.W.; Boccaccini, A.R. Preparation and characterization of vancomycin releasing PHBV coated 45S5 Bioglass®-based glass–ceramic scaffolds for bone tissue engineering. J. Eur. Ceram. Soc. 2014, 34, 505–514. [Google Scholar] [CrossRef]
- Li, W.; Ding, Y.; Rai, R.; Roether, J.A.; Schubert, D.W.; Boccaccini, A.R. Preparation and characterization of PHBV microsphere/45S5 bioactive glass composite scaffolds with vancomycin releasing function. Mater. Sci. Eng. C 2014, 41, 320–328. [Google Scholar] [CrossRef]
- Sajesh, K.M.; Kiran, K.; Nair, S.V.; Jayakumar, R. Sequential layer-by layer electrospinning of nano SrCO3/PRP loaded PHBV fibrous scaffold for bone tissue engineering. Compos. Part B Eng. 2016, 99, 445–452. [Google Scholar] [CrossRef]
- Prabhakaran, M.P.; Vatankhah, E.; Ramakrishna, S. Electrospun aligned PHBV/collagen nanofibers as substrates for nerve tissue engineering. Biotechnol. Bioeng. 2013, 110, 2775–2784. [Google Scholar] [CrossRef]
- Gelse, K.; Pöschl, E.; Aigner, T. Collagens—Structure, function, and biosynthesis. Adv. Drug Deliv. Rev. 2003, 55, 1531–1546. [Google Scholar] [CrossRef]
- Kiran, S.; Nune, K.C.; Misra, R.D.K. The significance of grafting collagen on polycaprolactone composite scaffolds: Processing-structure-functional property relationship. J. Biomed. Mater. Res. Part A 2015, 103, 2919–2931. [Google Scholar] [CrossRef]
- Sousa, I.; Mendes, A.; Bártolo, P.J. PCL scaffolds with collagen bioactivator for applications in tissue engineering. Procedia Eng. 2013, 59, 279–284. [Google Scholar] [CrossRef]
- Cui, M.; Liu, L.; Guo, N.; Su, R.; Ma, F. Preparation, cell compatibility and degradability of collagen-modified poly(lactic acid). Molecules 2015, 20, 595–607. [Google Scholar] [CrossRef]
- Castillo-Briceño, P.; Bihan, D.; Nilges, M.; Hamaia, S.; Meseguer, J.; García-Ayala, A.; Farndale, R.W.; Mulero, V. A role for specific collagen motifs during wound healing and inflammatory response of fibroblasts in the teleost fish gilthead seabream. Mol. Immunol. 2011, 48, 826–834. [Google Scholar] [CrossRef]
- Ferreira, A.M.; Gentile, P.; Chiono, V.; Ciardelli, G.A. Collagen for bone tissue regeneration. Acta Biomater. 2012, 8, 3191–3200. [Google Scholar] [CrossRef]
- Wang, Y.; Ke, Y.; Ren, L.; Wu, G.; Chen, X.; Zhao, Q. Surface engineering of PHBV by covalent collagen immobilization to improve cell compatibility. J. Biomed. Mater. Part A 2009, 88, 616–627. [Google Scholar] [CrossRef]
- Ai, J.; Keshel, S.H.; Ghorbani, F.; Ejazi, F.; Biazar, E.; Asefnejad, A.; Pourshamsian, K.; Montazeri, M. Fabrication of coated-collagen electrospun PHBV nanofiber film by plasma method and its cellular study. J. Nanomater. 2011, 2011, 123724. [Google Scholar] [CrossRef]
- Zeugolis, D.I.; Khew, S.T.; Yew, E.S.Y.; Ekaputra, A.K.; Tong, Y.W.; Yung, L.-Y.L.; Hutmacher, D.W.; Sheppard, C.; Raghunath, M. Electro-spinning of pure collagen nano-fibres—Just an expensive way to make gelatin? Biomaterials 2008, 29, 2293–2305. [Google Scholar] [CrossRef]
- Hexafluoroisopropanol MSDS, Sigma Aldrich. Available online: http://www.sigma-aldrich.com (accessed on 3 May 2019).
- Lü, L.-X.; Wang, Y.-Y.; Mao, X.; Xiao, Z.-D.; Huang, N.-P. The effects of PHBV electrospun fibers with different diameters and orientations on growth behavior of bone-marrow-derived mesenchymal stem cells. Biomed. Mater. 2012, 7, 015002. [Google Scholar] [CrossRef]
- Gentile, P.; McColgan-Bannon, K.; Gianone, N.C.; Sefat, F.; Dalgarno, K.; Ferreira, A.M. Biosynthetic PCL-graft-collagen bulk material for tissue engineering applications. Materials 2017, 10, 693. [Google Scholar] [CrossRef]
- De Campos Vidal, B.; Mello, M.L.S. Collagen type I amide I band infrared spectroscopy. Micron 2011, 42, 283–289. [Google Scholar] [CrossRef]
- Zhang, X.-Y.; Zheng, Y.; Liu, C.-H.; Wang, P.-H.; Zhu, Y.-Y. Facile and large scale in situ synthesis of the thermal responsive fluorescent SiNPs/PNIPAM hydrogels. RSC Adv. 2016, 6, 55666–55670. [Google Scholar] [CrossRef]
- Dementjev, A.; de Graaf, A.; van de Sanden, M.C.M.; Maslakov, K.I.; Naumkin, A.V.; Serov, A.A. X-ray photoelectron spectroscopy reference data for identification of the C3N4 phase in carbon–nitrogen films. Diam. Relat. Mater. 2000, 9, 1904–1907. [Google Scholar] [CrossRef]
- Diller, K.; Klappenberger, F.; Allegretti, F.; Papageorgiou, A.C.; Fischer, S.; Duncan, D.A.; Maurer, R.J.; Lloyd, J.A.; Oh, S.C.; Reuter, K. Temperature-dependent templated growth of porphine thin films on the (111) facets of copper and silver. J. Chem. Phys. 2014, 141, 144703. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dapson, R.W.; Fagan, C.; Kiernan, J.A.; Wickersham, T.W. Certification procedures for sirius red F3B (CI 35780, Direct red 80). Biotech. Histochem. 2011, 86, 133–139. [Google Scholar] [CrossRef] [PubMed]
- Ramakrishna, S.; Fujihara, K.; Teo, W.-E.; Yong, T.; Ma, Z.; Ramaseshan, R. Electrospun nanofibers: Solving global issues. Mater. Today 2006, 9, 40–50. [Google Scholar] [CrossRef]
- Keshel, S.H.; Azhdadi, S.N.K.; Asefnezhad, A.; Sadraeian, M.; Montazeri, M.; Biazar, E. The relationship between cellular adhesion and surface roughness for polyurethane modified by microwave plasma radiation. Int. J. Nanomed. 2011, 6, 641–647. [Google Scholar] [Green Version]
- Khalili, A.A.; Ahmad, M.R. A review of cell adhesion studies for biomedical and biological applications. Int. J. Mol. Sci. 2015, 16, 18149–18184. [Google Scholar] [CrossRef]
- Dowling, D.P.; Miller, I.S.; Ardhaoui, M.; Gallagher, W.M. Effect of surface wettability and topography on the adhesion of osteosarcoma cells on plasma-modified polystyrene. J. Biomater. Appl. 2011, 26, 327–347. [Google Scholar] [CrossRef]
- Yuan, S.; Xiong, G.; Wang, X.; Zhang, S.; Choong, C. Surface modification of polycaprolactone substrates using collagen-conjugated poly(methacrylic acid) brushes for the regulation of cell proliferation and endothelialisation. J. Mater. Chem. 2012, 22, 13039–13049. [Google Scholar] [CrossRef]
- Shang, L.; Fei, Q.; Zhang, Y.H.; Wang, X.Z.; Fan, D.-D.; Chang, H.N. Thermal properties and biodegradability studies of poly(3-hydroxybutyrate-co-3-hydroxyvalerate). J. Polym. 2011, 20, 23–28. [Google Scholar] [CrossRef]
- Leikina, E.; Mertts, M.V.; Kuznetsova, N.; Leikin, S. Type I collagen is thermally unstable at body temperature. Proc. Natl. Sci. Acad. USA 2002, 99, 1314–1318. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ke, Y.; Wang, Y.; Ren, L.; Wu, G.; Xue, W. Surface modification of PHBV films with different functional groups: Thermal properties and in vitro degradation. J. Appl. Polym. Sci. 2010, 118, 390–398. [Google Scholar] [CrossRef]
- Amass, W.; Amass, A.; Tighe, B. A review of biodegradable polymers: uses, current developments in the synthesis and characterization of biodegradable polyesters, blends of biodegradable polymers and recent advances in biodegradation studies. Polym. Int. 1998, 47, 89–144. [Google Scholar] [CrossRef]
- Heino, J. The collagen family members as cell adhesion proteins. BioEssays 2007, 29, 1001–1010. [Google Scholar] [CrossRef] [PubMed]
- Sousa, I.; Mendes, A.; Pereira, R.F.; Bártolo, P.J. Collagen surface modified poly(ε-caprolactone) scaffolds with improved hydrophilicity and cell adhesion properties. Mater. Lett. 2014, 134, 263–267. [Google Scholar] [CrossRef]
- Insomphun, C.; Chuah, J.-A.; Kobayashi, S.; Fujiki, T.; Numata, K. Influence of hydroxyl groups on the cell viability of polyhydroxyalkanoate (PHA) scaffolds for tissue engineering. ACS Biomater. Sci. Eng. 2017, 3, 3064–3075. [Google Scholar] [CrossRef]
- Matschegewski, C.; Staehlke, S.; Loeffler, R.; Lange, R.; Chai, F.; Kern, D.P.; Beck, U.; Nebe, B.J. Cell architecture–cell function dependencies on titanium arrays with regular geometry. Biomaterials 2010, 31, 5729–5740. [Google Scholar] [CrossRef]
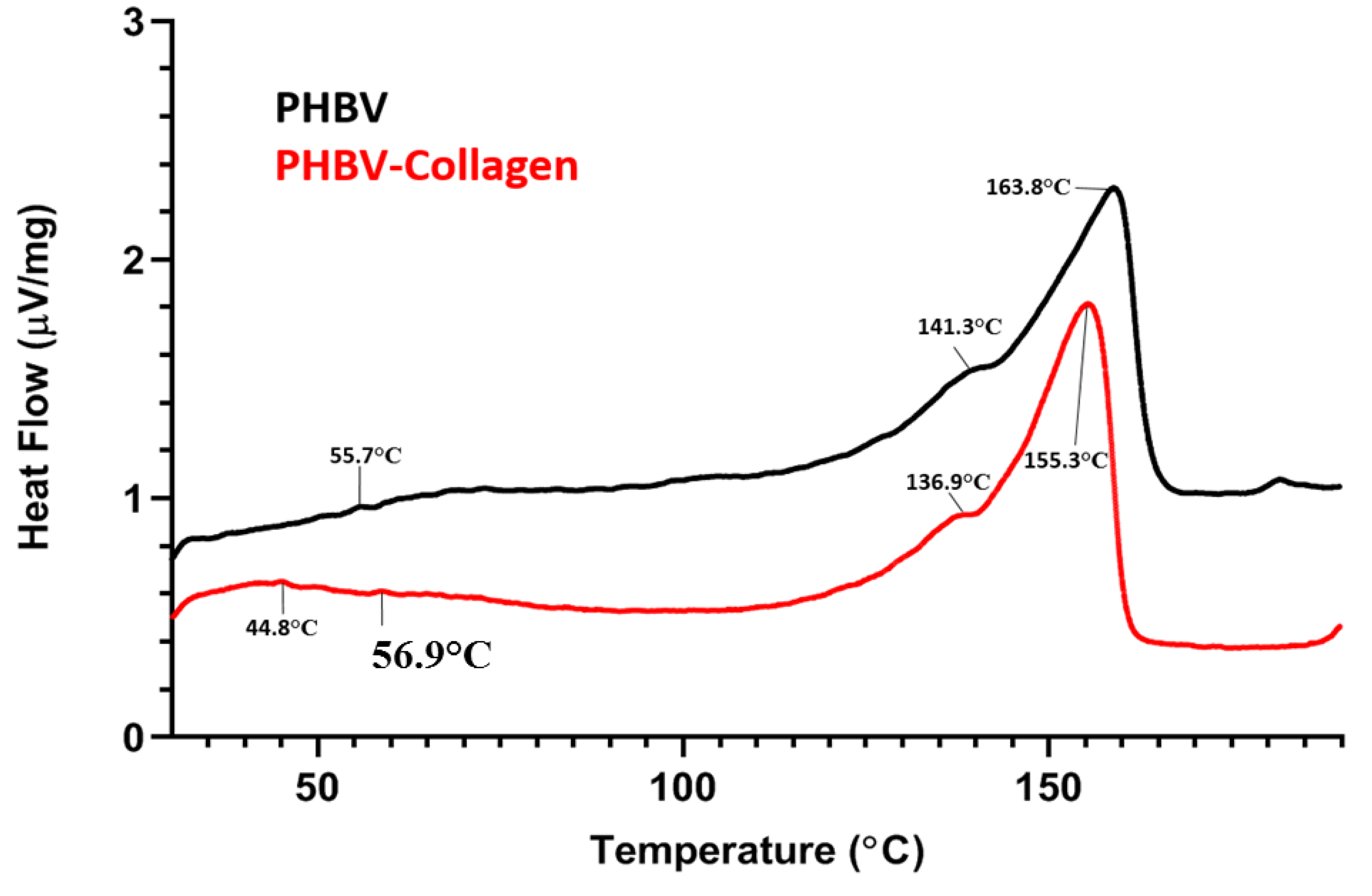

| Sample | Collagen Td (°C) | PHBV Tc (°C) | PHV Tm (°C) | PHB Tm (°C) | Collagen ΔHd (µV s/mg) | PHBV ΔHc (µV s/mg) | PHBV ΔHm (µV s/mg) |
|---|---|---|---|---|---|---|---|
| PHBV | – | 55.7 | 141.3 | 163.8 | – | 0.182 | 150.4 |
| PHBV-Collagen | 44.8 | 56.9 | 136.9 | 155.3 | 0.189 | 0.120 | 150.7 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
McColgan-Bannon, K.I.S.; Upson, S.; Gentile, P.; Tausif, M.; Russell, S.; Dalgarno, K.; Ferreira, A.M. Biomimetic Properties of Force-Spun PHBV Membranes Functionalised with Collagen as Substrates for Biomedical Application. Coatings 2019, 9, 350. https://doi.org/10.3390/coatings9060350
McColgan-Bannon KIS, Upson S, Gentile P, Tausif M, Russell S, Dalgarno K, Ferreira AM. Biomimetic Properties of Force-Spun PHBV Membranes Functionalised with Collagen as Substrates for Biomedical Application. Coatings. 2019; 9(6):350. https://doi.org/10.3390/coatings9060350
Chicago/Turabian StyleMcColgan-Bannon, Kegan I. S., Sarah Upson, Piergiorgio Gentile, Muhammad Tausif, Stephen Russell, Kenneth Dalgarno, and Ana Marina Ferreira. 2019. "Biomimetic Properties of Force-Spun PHBV Membranes Functionalised with Collagen as Substrates for Biomedical Application" Coatings 9, no. 6: 350. https://doi.org/10.3390/coatings9060350
APA StyleMcColgan-Bannon, K. I. S., Upson, S., Gentile, P., Tausif, M., Russell, S., Dalgarno, K., & Ferreira, A. M. (2019). Biomimetic Properties of Force-Spun PHBV Membranes Functionalised with Collagen as Substrates for Biomedical Application. Coatings, 9(6), 350. https://doi.org/10.3390/coatings9060350






