A Cluster of Candida auris Blood Stream Infections in a Tertiary Care Hospital in Oman from 2016 to 2019
Abstract
1. Introduction
2. Results
2.1. Clinical Characteristics and Manifestations
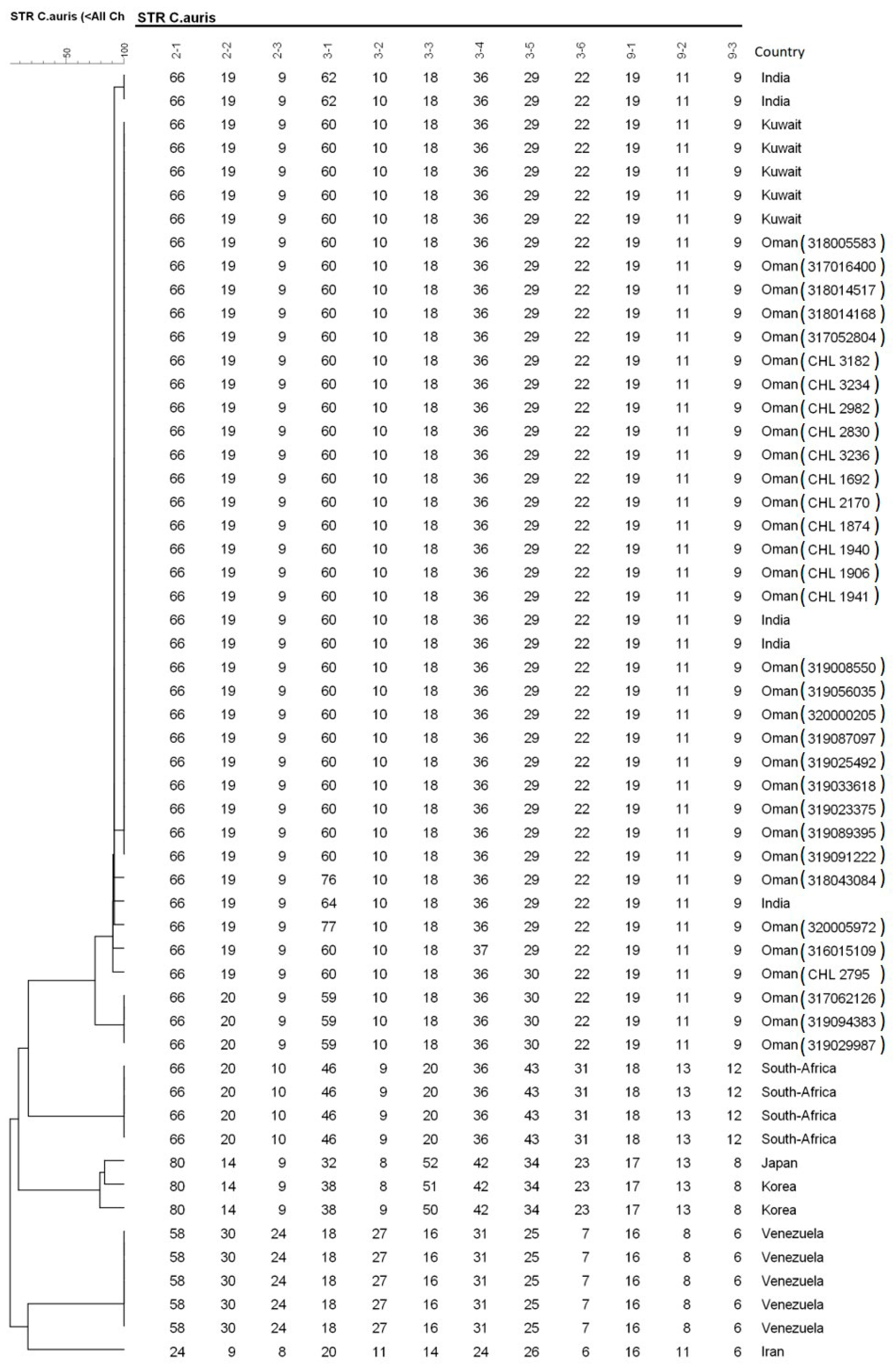
2.2. Microbiology
2.3. Treatment and Outcome
3. Discussion
4. Materials and Methods
4.1. Samples
4.2. Laboratory Investigations
4.3. Molecular Identification Using ITS-Sequencing and STR-Genotyping
4.4. Antifungal Susceptibility Testing
4.5. Ethical Statement
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Pfaller, M.; Diekema, D.J.; Turnidge, J.D.; Castanheira, M.; Jones, R.N. Twenty Years of the SENTRY Antifungal Surveillance Program: Results for Candida Species from 1997–2016. Open Forum Infect. Dis. 2019, 6, 79–94. [Google Scholar] [CrossRef] [PubMed]
- Montagna, M.T.; Caggiano, G.; Lovero, G.; De Giglio, O.; Coretti, C.; Cuna, T.; Iatta, R.; Giglio, M.; Dalfino, L.; Bruno, F.; et al. Epidemiology of invasive fungal infections in the intensive care unit: Results of a multicenter Italian survey (AURORA Project). Infection 2013, 41, 645–653. [Google Scholar] [CrossRef] [PubMed]
- Bassetti, M.; Merelli, M.; Righi, E.; Diaz-Martin, A.; Rosello, E.M.; Luzzati, R.; Parra, A.; Trecarichi, E.M.; Sanguinetti, M.; Posteraro, B.; et al. Epidemiology, Species Distribution, Antifungal Susceptibility, and Outcome of Candidemia across Five Sites in Italy and Spain. J. Clin. Microbiol. 2013, 51, 4167–4172. [Google Scholar] [CrossRef] [PubMed]
- Klingspor, L.; Tortorano, A.M.; Pemán, J.; Willinger, B.; Hamal, P.; Sendid, B.; Velegraki, A.; Kibbler, C.; Meis, J.F.; Sabino, R.F.P.; et al. Invasive Candida infections in surgical patients in intensive care units: A prospective, multicentre survey initiated by the European Confederation of Medical Mycology (ECMM) (2006–2008). Clin. Microbiol. Infect. 2015, 21, 87. [Google Scholar] [CrossRef] [PubMed]
- Lamoth, F.; Lockhart, S.R.; Berkow, E.L.; Calandra, T. Changes in the epidemiological landscape of invasive candidiasis. J. Antimicrob. Chemother. 2018, 73, 4–13. [Google Scholar] [CrossRef]
- Kean, R.; Brown, J.L.; Gülmez, D.; Ware, A.; Ramage, G. Candida auris: A Decade of Understanding of an Enigmatic Pathogenic Yeast. J. Fungi 2020, 6, 30. [Google Scholar] [CrossRef]
- Chowdhary, A.; Sharma, C.; Meis, J.F. Candida auris: A rapidly emerging cause of hospital-acquired multidrug-resistant fungal infections globally. PLoS Pathog. 2017, 13, 1006290. [Google Scholar] [CrossRef]
- Calandra, T.; A Roberts, J.; Antonelli, M.; Bassetti, M.; Vincent, J.-L. Diagnosis and management of invasive candidiasis in the ICU: An updated approach to an old enemy. Crit. Care 2016, 20, 125. [Google Scholar] [CrossRef]
- Pristov, K.E.; Ghannoum, M. Resistance of Candida to azoles and echinocandins worldwide. Clin. Microbiol. Infect. 2019, 25, 792–798. [Google Scholar] [CrossRef]
- Jackson, B.R.; Chow, N.; Forsberg, K.; Litvintseva, A.P.; Lockhart, S.R.; Welsh, R.; Vallabhaneni, S.; Chiller, T. On the Origins of a Species: What Might Explain the Rise of Candida auris? J. Fungi 2019, 5, 58. [Google Scholar] [CrossRef]
- Borman, A.M.; Johnson, E.M. Candida auris in the UK: Introduction, dissemination, and control. PLoS Pathog. 2020, 16, e1008563. [Google Scholar] [CrossRef]
- Al Maani, A.; Paul, H.; Al-Rashdi, A.; Al Wahaibi, A.; Al-Jardani, A.; Abri, A.; Albalushi, M.A.H.; Al-Abri, S.; Al Reesi, M.; Al Maqbali, A.; et al. Ongoing Challenges with Healthcare-Associated Candida auris Outbreaks in Oman. J. Fungi 2019, 5, 101. [Google Scholar] [CrossRef]
- Benedict, K.; Roy, M.; Kabbani, S.; Anderson, E.J.; Farley, M.M.; Harb, S.; Harrison, L.H.; Bonner, L.; Wadu, V.L.; Marceaux, K.; et al. Neonatal and Pediatric Candidemia: Results from Population-Based Active Laboratory Surveillance in Four US Locations, 2009–2015. J. Pediatr. Infect. Dis. Soc. 2018, 7, 78–85. [Google Scholar] [CrossRef]
- Chowdhary, A.; Kumar, V.A.; Sharma, C.; Prakash, A.; Agarwal, K.; Babu, R.; Dinesh, K.R.; Karim, S.; Singh, S.K.; Hagen, F.; et al. Multidrug-resistant endemic clonal strain of Candida auris in India. Eur. J. Clin. Microbiol. Infect. Dis. 2013, 33, 919–926. [Google Scholar] [CrossRef]
- Mohsin, J.; Hagen, F.; Al-Balushi, Z.A.M.; De Hoog, S.; Chowdhary, A.; Meis, J.F.; Al-Hatmi, A.M.S. The first cases of Candida auris candidaemia in Oman. Mycoses 2017, 60, 569–575. [Google Scholar] [CrossRef]
- Al-Siyabi, T.; Al Busaidi, I.; Balkhair, A.; Al-Muharrmi, Z.; Al-Salti, M.; Al’Adawi, B. First report of Candida auris in Oman: Clinical and microbiological description of five candidemia cases. J. Infect. 2017, 75, 373–376. [Google Scholar] [CrossRef]
- Eyre, D.W.; Sheppard, A.E.; Madder, H.; Moir, I.; Moroney, R.; Quan, T.P.; Griffiths, D.; George, S.; Butcher, L.; Morgan, M.; et al. A Candida auris Outbreak and Its Control in an Intensive Care Setting. N. Engl. J. Med. 2018, 379, 1322–1331. [Google Scholar] [CrossRef]
- Lockhart, S.R.; Berkow, E.L.; Chow, N.; Welsh, R.M. Candida auris for the clinical microbiology laboratory: Not your grandfather’s Candida species. Clin. Microbiol. Newsl. 2017, 39, 99–103. [Google Scholar] [CrossRef]
- Astvad, K.; Johansen, H.K.; Røder, B.L.; Rosenvinge, F.S.; Knudsen, J.D.; Lemming, L.; Schønheyder, H.C.; Hare, R.K.; Kristensen, L.; Nielsen, L.; et al. Update from a twelve-year nationwide fungaemia surveillance: Increasing intrinsic and acquired resistance causes concern. J. Clin. Microbiol. 2018, 56, 107–119. [Google Scholar]
- Shastri, P.; Shankarnarayan, S.A.; Oberoi, J.; Rudramurthy, S.M.; Wattal, C.; Chakrabarti, A. Candida auris candidaemia in an intensive care unit—Prospective observational study to evaluate epidemiology, risk factors, and outcome. J. Crit. Care 2020, 57, 42–48. [Google Scholar] [CrossRef]
- Rudramurthy, S.M.; Chakrabarti, A.; Paul, R.A.; Sood, P.; Kaur, H.; Capoor, M.R.; Kindo, A.J.; Marak, R.S.K.; Arora, A.; Sardana, R.; et al. Candida auris candidaemia in Indian ICUs: Analysis of risk factors. J. Antimicrob. Chemother. 2017, 72, 1794–1801. [Google Scholar] [CrossRef] [PubMed]
- Piedrahita, C.T.; Cadnum, J.L.; Jencson, A.L.; Shaikh, A.A.; Ghannoum, M.A.; Donskey, C.J. Environmental Surfaces in Healthcare Facilities are a Potential Source for Transmission ofCandida aurisand OtherCandidaSpecies. Infect. Control. Hosp. Epidem. 2017, 38, 1107–1109. [Google Scholar] [CrossRef]
- Schelenz, S.; Hagen, F.; Rhodes, J.; Abdolrasouli, A.; Chowdhary, A.; Hall, A.; Ryan, L.; Shackleton, J.; Trimlett, R.; Meis, J.F.; et al. First hospital outbreak of the globally emerging Candida auris in a European hospital. Antimicrob. Resist. Infect. Control. 2016, 5, 35. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Gaitán, A.; Moret, A.M.; Tasias-Pitarch, M.; Aleixandre-Lopez, A.I.; Martínez-Morel, H.; Calabuig, E.; Salavert-Lletí, M.; Ramírez, P.; Hontangas, J.L.L.; Hagen, F.; et al. An outbreak due to Candida auris with prolonged colonisation and candidaemia in a tertiary care European hospital. Mycoses 2018, 61, 498–505. [Google Scholar] [CrossRef] [PubMed]
- Welsh, R.M.; Bentz, M.L.; Shams, A.; Houston, H.; Lyons, A.; Rose, L.J.; Litvintseva, A.P. Survival, Persistence, and Isolation of the Emerging Multidrug-Resistant Pathogenic Yeast Candida auris on a Plastic Health Care Surface. J. Clin. Microbiol. 2017, 55, 2996–3005. [Google Scholar] [CrossRef]
- Forsberg, K.; Woodworth, K.; Walters, M.; Berkow, E.L.; Jackson, B.; Chiller, T.; Vallabhaneni, S. Candida auris: The recent emergence of a multidrug-resistant fungal pathogen. Med Mycol. 2018, 57, 1–12. [Google Scholar] [CrossRef]
- Tsay, S.; Welsh, R.M.; Adams, E.H.; Chow, N.A.; Gade, L.; Berkow, E.L.; Poirot, E.; Lutterloh, E.; Quinn, M.; Chaturvedi, S.; et al. Notes from the field: Ongoing transmission of Candida auris in health care facilities—United States, June 2016–May 2017. MMWR Morb. Mortal. Wkly. Rep. 2017, 66, 514. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. 2017. Candida Auris, Case Count Updated: 15 May 2020. Available online: https://www.cdc.gov/fungal/diseases/candidiasis/candida-auris.html (accessed on 4 July 2020).
- Sekyere, J.O. Candida auris: A systematic review and meta-analysis of current updates on an emerging multidrug-resistant pathogen. Microbiology 2019, 8, e00901. [Google Scholar] [CrossRef]
- Jeffery-Smith, A.; Taori, S.K.; Schelenz, S.; Jeffery, K.; Johnson, E.M.; Borman, A.M.; Manuel, R.; Brown, C.S. Candida auris: A Review of the Literature. Clin. Microbiol. Rev. 2017, 31, e00029-17. [Google Scholar] [CrossRef]
- Adam, R.D.; Revathi, G.; Okinda, N.; Fontaine, M.; Shah, J.; Kagotho, E.; Castanheira, M.; Pfaller, M.A.; Maina, D. Analysis of Candida auris fungemia at a single facility in Kenya. Int. J. Infect. Dis. 2019, 85, 182–187. [Google Scholar] [CrossRef]
- Lockhart, S.R.; Etienne, K.A.; Vallabhaneni, S.; Farooqi, J.; Chowdhary, A.; Govender, N.P.; Colombo, A.L.; Calvo, B.; Cuomo, C.A.; Desjardins, C.A.; et al. Simultaneous Emergence of Multidrug-Resistant Candida auris on 3 Continents Confirmed by Whole-Genome Sequencing and Epidemiological Analyses. Clin. Infect. Dis. 2016, 64, 134–140. [Google Scholar] [CrossRef] [PubMed]
- Alfouzan, W.; Dhar, R.; Albarrag, A.; Al-Abdely, H. The emerging pathogen Candida auris: A focus on the Middle-Eastern countries. J. Infect. Public Heal. 2019, 12, 451–459. [Google Scholar] [CrossRef]
- Ahmad, S.; Khan, Z.; Al-Sweih, N.; Alfouzan, W.; Joseph, L. Candida auris in various hospitals across Kuwait and their susceptibility and molecular basis of resistance to antifungal drugs. Mycoses 2019, 63, 104–112. [Google Scholar] [CrossRef] [PubMed]
- Almaghrabi, R.S.; AlBalawi, R.; Mutabagani, M.; Atienza, E.; Aljumaah, S.; Gade, L.; Forsberg, K.; Litvintseva, A.; Althawadi, S. Molecular characterisation and clinical outcomes of Candida auris infection: Single-centre experience in Saudi Arabia. Mycoses 2020, 63, 452–460. [Google Scholar] [CrossRef]
- De Hoog, G.S.; Guarro, J.; Gené, J.; Ahmed, S.; Al-Hatmi, A.M.S.; Figueras, M.J.; Vitale, R.G. Atlas of Clinical Fungi, 4th ed.; Westerdijk Institute, Universitat Rovira i Virgili: Utrecht, The Netherlands, 2019. [Google Scholar]
- Lone, S.A.; Ahmad, A. Candida auris—The growing menace to global health. Mycoses 2019, 62, 620–637. [Google Scholar] [CrossRef]
- Chow, N.A.; de Groot, T.; Badali, H.; Abastabar, M.; Chiller, T.M.; Meis, J.F. Potential fifth clade of Candida auris, Iran, 2018. Emerg. Infect. Dis. 2019, 25, 1780–1781. [Google Scholar]
- De Groot, T.; Puts, Y.; Berrio, I.; Chowdhary, A.; Meis, J.F. Development of Candida auris Short Tandem Repeat Typing and Its Application to a Global Collection of Isolates. mBio 2020, 11, e02971-19. [Google Scholar] [CrossRef]
- Kenters, N.; Kiernan, M.; Chowdhary, A.; Denning, D.W.; Pemán, J.; Saris, K.; Schelenz, S.; Tartari, E.; Widmer, A.; Meis, J.F.; et al. Control of Candida auris in healthcare institutions: Outcome of an International Society for Antimicrobial Chemotherapy expert meeting. Int. J. Antimicrob. Agents 2019, 54, 400–406. [Google Scholar] [CrossRef]
- Caceres, D.H.; Forsberg, K.; Welsh, R.M.; Sexton, D.J.; Lockhart, S.R.; Jackson, B.R.; Chiller, T. Candida auris: A Review of Recommendations for Detection and Control in Healthcare Settings. J. Fungi 2019, 5, 111. [Google Scholar] [CrossRef]
- Arendrup, M.C.; Prakash, A.; Meletiadis, J.; Sharma, C.; Chowdhary, A. Comparison of EUCAST and CLSI Reference Microdilution MICs of Eight Antifungal Compounds for Candida auris and Associated Tentative Epidemiological Cutoff Values. Antimicrob. Agents Chemother. 2017, 61, e00485-17. [Google Scholar] [CrossRef]

| Sample No | MALDI-TOF/Sequencing | Age/Year | Sex | Duration of Treatment (Days) | Time of Candidemia Post Admission (Weeks) | MIC Values (mg/L) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AMB | FLC | ITC | VOR | POS | ISA | ANI | MICA | ||||||
| 317062126 | C. auris | 54 | M | 16 | 3 | 1 | >64 | 0.125 | 0.5 | 0.063 | 0.063 | 0.125 | 0.125 |
| 318005583 | C. auris | 50 | M | 28 | 2 | 1 | >64 | 0.125 | 0.5 | 0.063 | 0.031 | 0.5 | 0.25 |
| 317078724 | C. auris | 78 | F | 24 | 12 | 2 | 32 | 0.25 | 1 | 0.016 | 0.5 | 0.25 | 0.25 |
| 317052804 | C. auris | 69 | M | 14 | 1 | 0.5 | 64 | 0.063 | 0.25 | 0.016 | 0.125 | 0.25 | 0.125 |
| 318014168 | C. auris | 63 | F | 14 | 8 | 1 | 32 | 0.063 | 0.5 | 0.063 | 0.5 | 0.125 | 0.25 |
| 318014517 | C. auris | 30 | M | 4 | NA | 1 | 64 | 0.031 | 1 | 0.031 | 0.063 | 0.5 | 0.25 |
| 318028905 | C. auris | 76 | F | 10 | 16 | 1 | >64 | 0.125 | 1 | 0.063 | 0.031 | 0.25 | 0.25 |
| 318043084 | C. auris | 2 | M | 16 | 1 | 1 | >64 | 0.125 | 0.5 | 0.063 | 0.5 | 0.125 | 0.125 |
| 318066628 | C. auris | 0.5 | M | 15 | 4 | 2 | 64 | 0.5 | 0.5 | 0.031 | 0.063 | 0.5 | 0.25 |
| 318071689 | C. auris | 83 | M | NA | NA | 0.5 | 32 | 0.25 | 1 | 0.125 | 0.031 | 0.5 | 0.125 |
| 318095154 | C. auris | 70 | F | 17 | 3 | 1 | 64 | 0.125 | 1 | 0.063 | 0.063 | 0.125 | 0.25 |
| 319008550 | C. auris | 54 | M | 30 | 9 | 2 | >64 | 0.25 | 0.5 | 0.063 | 0.125 | 0.25 | 0.125 |
| 319056035 | C. auris | 62 | M | 2 | 2 | 2 | >64 | 0.063 | 0.5 | 0.063 | 0.25 | 0.125 | 0.125 |
| 320000205 | C. auris | 51 | M | 14 | 3 | 1 | 32 | 0.031 | 0.5 | 0.016 | 0.25 | 0.5 | 0.25 |
| 319087097 | C. auris | 62 | M | 2 | 5 | 1 | 64 | 0.125 | 1 | 0.031 | 0.063 | 0.5 | 0.25 |
| 319025492 | C. auris | 50 | M | 48 | 15 | 0.5 | >64 | 0.125 | 0.5 | 0.016 | 0.016 | 0.5 | 0.125 |
| 319033618 | C. auris | 47 | F | 16 | 2 | 1 | 32 | 0.125 | 0.25 | 0.016 | 0.016 | 0.5 | 0.25 |
| 319023375 | C. auris | 62 | M | 14 | 15 | 2 | >64 | 0.25 | 0.5 | 0.063 | 0.125 | 0.25 | 0.25 |
| 319089395 | C. auris | 49 | F | 11 | 5 | 1 | 32 | 0.063 | 0.5 | 0.016 | 0.125 | 0.5 | 0.25 |
| 319091222 | C. auris | 54 | M | 14 | 6 | 1 | 64 | 0.063 | 1 | 0.25 | 0.031 | 0.25 | 0.125 |
| 320005972 | C. auris | 31 | M | 14 | 1 | 1 | >64 | 0.5 | 1 | 0.125 | 0.5 | 0.25 | 0.125 |
| 319094383 | C. auris | 47 | M | 14 | 2 | 1 | 64 | 0.125 | 1 | 0.031 | 0.031 | 0.25 | 0.125 |
| 319029987 | C. auris | 64 | F | 17 | 2 | 1 | 64 | 0.125 | 1 | 0.25 | 0.031 | 0.25 | 0.125 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mohsin, J.; Weerakoon, S.; Ahmed, S.; Puts, Y.; Al Balushi, Z.; Meis, J.F.; Al-Hatmi, A.M.S. A Cluster of Candida auris Blood Stream Infections in a Tertiary Care Hospital in Oman from 2016 to 2019. Antibiotics 2020, 9, 638. https://doi.org/10.3390/antibiotics9100638
Mohsin J, Weerakoon S, Ahmed S, Puts Y, Al Balushi Z, Meis JF, Al-Hatmi AMS. A Cluster of Candida auris Blood Stream Infections in a Tertiary Care Hospital in Oman from 2016 to 2019. Antibiotics. 2020; 9(10):638. https://doi.org/10.3390/antibiotics9100638
Chicago/Turabian StyleMohsin, Jalila, Sanjeewani Weerakoon, Sarah Ahmed, Ynze Puts, Zainab Al Balushi, Jacques F. Meis, and Abdullah M.S. Al-Hatmi. 2020. "A Cluster of Candida auris Blood Stream Infections in a Tertiary Care Hospital in Oman from 2016 to 2019" Antibiotics 9, no. 10: 638. https://doi.org/10.3390/antibiotics9100638
APA StyleMohsin, J., Weerakoon, S., Ahmed, S., Puts, Y., Al Balushi, Z., Meis, J. F., & Al-Hatmi, A. M. S. (2020). A Cluster of Candida auris Blood Stream Infections in a Tertiary Care Hospital in Oman from 2016 to 2019. Antibiotics, 9(10), 638. https://doi.org/10.3390/antibiotics9100638






