Review of Contemporary Self-Assembled Systems for the Controlled Delivery of Therapeutics in Medicine
Abstract
1. Introduction
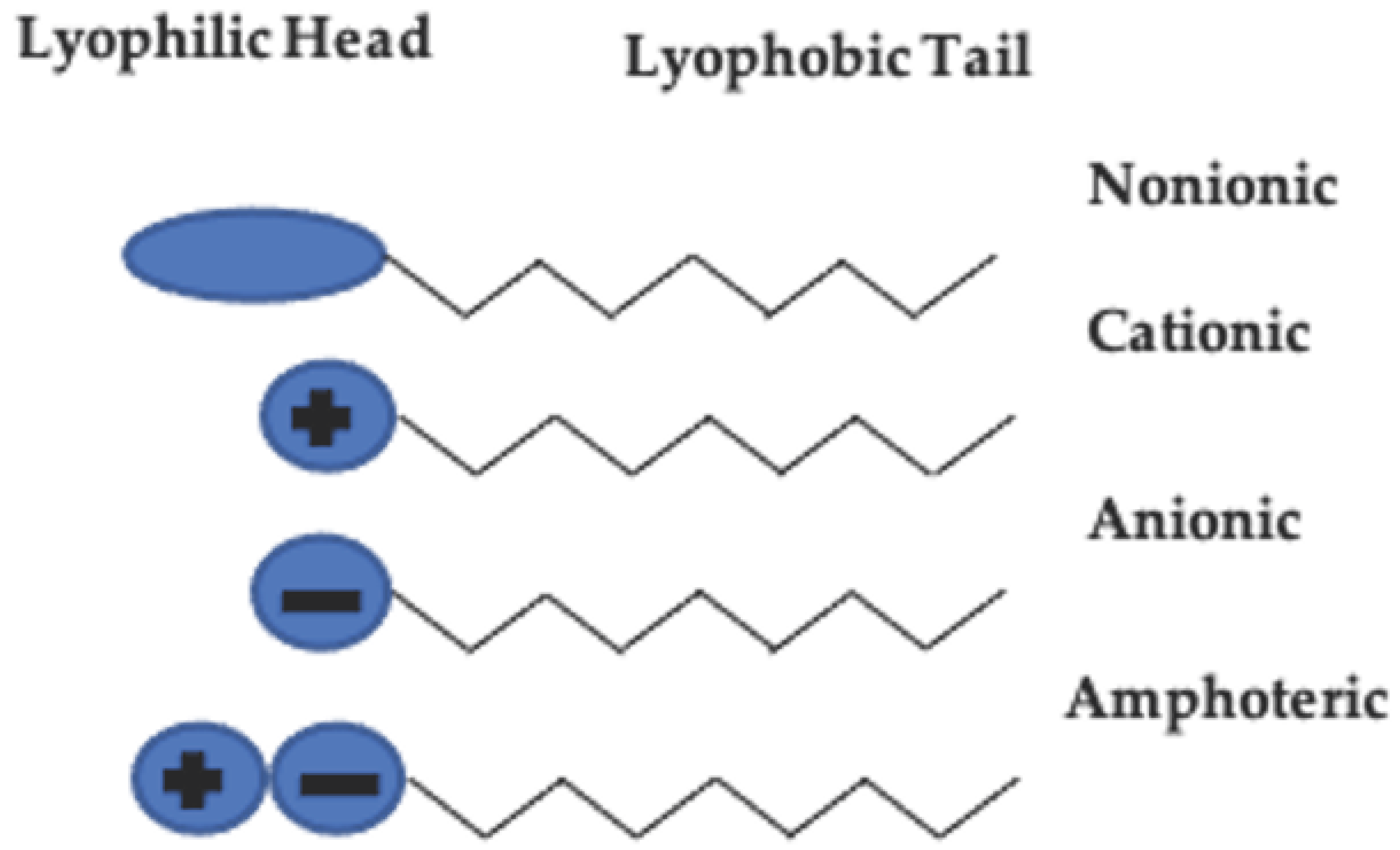
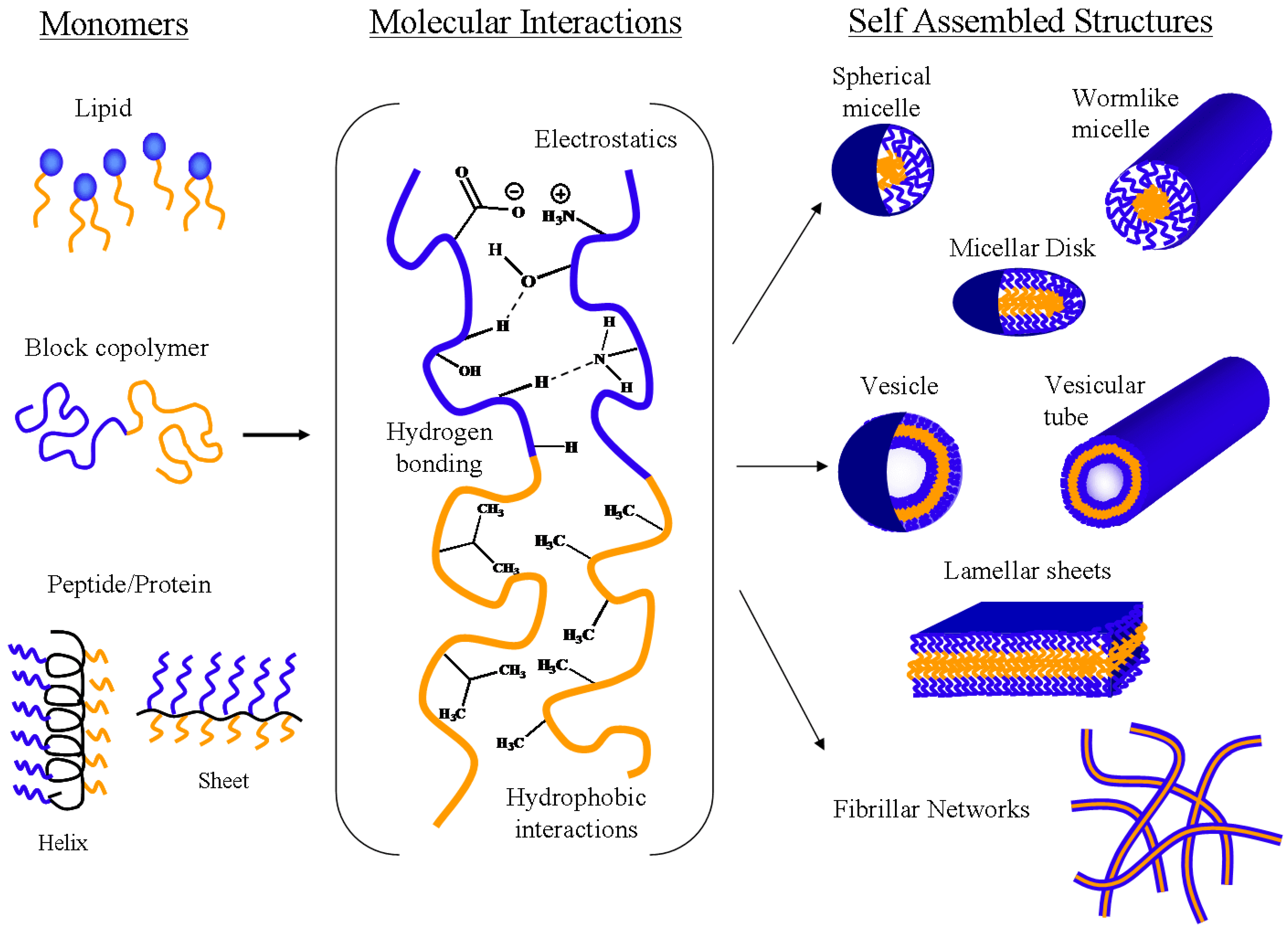
2. Amphiphilic Molecules—The Building Blocks of Self-Assembled Systems
2.1. Surfactants and Phospholipids
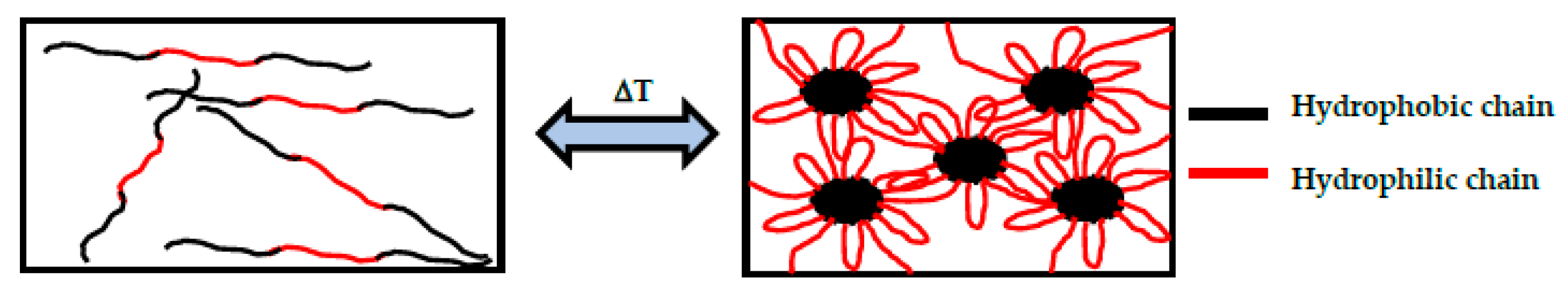
2.2. Amphiphilic Block Copolymers
3. General Thermodynamics Self-Assembly of Block Copolymers in Aqueous Solutions
4. Self-Assembled Structures and Their Applications in Drug Delivery
4.1. Micelles
4.2. Hydrogels
4.3. Vesicles
5. Clinical Potential of Self-Assembled Structures in Drug Delivery
6. Summary, Future Perspectives, and Tools
Author Contributions
Funding
Conflicts of Interest
References
- Danhier, F.; Feron, O.; Préat, V. To exploit the tumor microenvironment: Passive and active tumor targeting of nanocarriers for anti-cancer drug delivery. J. Control. Release 2010, 148, 135–146. [Google Scholar] [CrossRef] [PubMed]
- Branco, M.C.; Schneider, J.P. Self-assembling materials for therapeutic delivery. Acta Biomater. 2009, 5, 817–831. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.C.; Kwon, I.K.; Park, K. Hydrogels for delivery of bioactive agents: A historical perspective. Adv. Drug. Deliv. Rev. 2013, 65, 17–20. [Google Scholar] [CrossRef] [PubMed]
- Buwalda, S.J.; Boere, K.W.M.; Dijkstra, P.J.; Feijen, J.; Vermonden, T.; Hennink, W.E. Hydrogels in a historical perspective: From simple networks to smart materials. J. Control. Release 2014, 190, 254–273. [Google Scholar] [CrossRef] [PubMed]
- Siepmann, J.; Siegel, R.A.; Rathbone, M.J. (Eds.) Fundamentals and Applications of Controls Release Drug Delivery, 1st ed.; Springer US: New York, NY, USA, 2012; ISBN 978-1-4614-0880-2. [Google Scholar]
- Mateescu, M.A.; Ispas-Szabo, P.; Assaad, E. (Eds.) 5—Self-assembling in natural, synthetic, and hybrid materials with applications in controlled drug delivery. In Controlled Drug Delivery; Woodhead Publishing: Cambridge, UK, 2015; pp. 163–223. [Google Scholar]
- Lehn, J.M. Supramolecular chemistry. Science 1993, 260, 1762. [Google Scholar] [CrossRef]
- Lehn, J.-M. Supramolecular chemistry—Scope and perspectives molecules, supermolecules, and molecular devices (Nobel lecture). Angew. Chem. Int. Ed. Engl. 1988, 27, 89–112. [Google Scholar] [CrossRef]
- Lehn, J.-M. Perspectives in supramolecular chemistry—From molecular recognition towards molecular information processing and self-organization. Angew. Chem. Int. Ed. Engl. 1990, 29, 1304–1319. [Google Scholar] [CrossRef]
- Lehn, J.-M. From supermolecules to supramolecular assemblies. In Supramolecular Chemistry: Concepts and Perspectives; Lehn, J.-M., Ed.; Wiley-VCH: Hoboken, NJ, USA, 2006. [Google Scholar]
- Alexandridis, P.; Lindman, B. Amphiphilic Block Copolymers: Self-Assembly and Applications, 1st ed.; Elsevier Science B.V.: Amsterdam, The Netherlands, 2000; ISBN 9780444824417. [Google Scholar]
- Elstad, N.L.; Fowers, K.D. OncoGel (ReGel/paclitaxel)—Clinical applications for a novel paclitaxel delivery system. Adv. Drug Deliv. Rev. 2009, 61, 785–794. [Google Scholar] [CrossRef]
- Jeong, B.; Han Bae, Y.; Wan Kim, S. Biodegradable thermosensitive micelles of PEG-PLGA-PEG triblock copolymers. Colloids Surf. B Biointerfaces 1999, 16, 185–193. [Google Scholar] [CrossRef]
- McClements, D.J. Nanoparticle- and Microparticle-Based Delivery Systems: Encapsulation, Protection and Release of Active Compounds; CRC Press: Boca Raton, FL, USA, 2017; ISBN 9781138034037. [Google Scholar]
- Langer, R.; Peppas, N.A. Advances in biomaterials, drug delivery, and bionanotechnology. AIChE J. 2003, 49, 2990–3006. [Google Scholar] [CrossRef]
- Lombardo, D.; Kiselev, M.A.; Caccamo, M.T. Smart Nanoparticles for Drug Delivery Application: Development of Versatile Nanocarrier Platforms in Biotechnology and Nanomedicine. J. Nanomater. 2019, 2019, 3702518. [Google Scholar] [CrossRef]
- Yorulmaz Avsar, S.; Kyropoulou, M.; Di Leone, S.; Schoenenberger, C.-A.; Meier, W.P.; Palivan, C.G. Biomolecules Turn Self-Assembling Amphiphilic Block Co-polymer Platforms Into Biomimetic Interfaces. Front. Chem. 2019, 6. [Google Scholar] [CrossRef] [PubMed]
- Yetisgin, A.A.; Cetinel, S.; Zuvin, M.; Kosar, A.; Kutlu, O. Therapeutic Nanoparticles and Their Targeted Delivery Applications. Molecules 2020, 25, 2193. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Ding, X.; Guo, X. Assembly behaviors of calixarene-based amphiphile and supra-amphiphile and the applications in drug delivery and protein recognition. Adv. Colloid Interface Sci. 2019, 269, 187–202. [Google Scholar] [CrossRef] [PubMed]
- Zagami, R.; Romeo, A.; Mazzaglia, A. Bio-soft cyclodextrin nanomaterials. Riv. Nuovo Cim. 2019, 42, 407–441. [Google Scholar] [CrossRef]
- Zerkoune, L.; Angelova, A.; Lesieur, S. Nano-assemblies of modified cyclodextrins and their complexes with guest molecules: Incorporation in nanostructured membranes and amphiphile nanoarchitectonics design. Nanomaterials 2014, 4, 741–765. [Google Scholar] [CrossRef]
- Fried, J.R. Polymer Science & Technology, 3rd ed.; Prentice Hall: Upper Saddle River, NJ, USA, 2014; ISBN 978-0-13-703955-5. [Google Scholar]
- Santos, S.D.; Medronho, B.; Santos, T.D.; Antunes, F.E. Amphiphilic molecules in drug delivery systems. In Drug Delivery systems: Advanced Technologies Potentially Applicable in Personalised Treatment; Coelho, J., Ed.; Springer: Dordrecht, The Netherlands, 2013; pp. 35–85. [Google Scholar]
- Goodwin, J.W. Macromolecules and surfactants. In Colloids and Interfaces with Surfactants and Polymers—An Introduction; John Wiley & Sons, Ltd.: London, UK, 2004. [Google Scholar]
- Kronberg, B.; Holmberg, K.; Lindman, B. Surface Chemistry of Surfactants and Polymers; John Wiley & Sons, Ltd.: Weinheim, Germany, 2014; ISBN 978-1-119-96124-6. [Google Scholar]
- Chemistry and Technology of Surfactants; Farn, R.J., Ed.; Blackwell Publishing, Ltd.: Hoboken, NJ, USA, 2006; ISBN 978-1451-2696-0. [Google Scholar]
- Sagar, G.H.; Arunagirinathan, M.A.; Bellare, J.R. Self-assembled surfactant nano-structures important in drug delivery: A review. Indian J. Exp. Biol. 2007, 45, 133–159. [Google Scholar]
- Malmsten, M. Surfactants and Polymers in Drug Delivery; CRC Press: Boca Raton, FL, USA, 2002; ISBN 9780824708047. [Google Scholar]
- Lombardo, D.; Kiselev, M.A.; Magazu, S.; Calandra, P. Amphiphiles self-assembly: Basic concepts and future perspectives of supramolecular approaches. Adv. Condens. Matter Phys. 2015, 2015. [Google Scholar] [CrossRef]
- Carmignani, C.; Rossi, S.; Saettone, M.F.; Burgalassi, S. Ophthalmic Vehicles Containing Polymer-Solubilized Tropicamide: “In Vitro/In Vivo” Evaluation. Drug Dev. Ind. Pharm. 2002, 28, 101–105. [Google Scholar] [CrossRef]
- Jiao, J. Polyoxyethylated nonionic surfactants and their applications in topical ocular drug delivery. Adv. Drug Deliv. Rev. 2008, 60, 1663–1673. [Google Scholar] [CrossRef]
- Zimmer, A.K.; Maincent, P.; Thouvenot, P.; Kreuter, J. Hydrocortisone delivery to healthy and inflamed eyes using a micellar polysorbate 80 solution or albumin nanoparticles. Int. J. Pharm. 1994, 110, 211–222. [Google Scholar] [CrossRef]
- Alyami, H.; Abdelaziz, K.; Dahmash, E.Z.; Iyire, A. Nonionic surfactant vesicles (niosomes) for ocular drug delivery: Development, evaluation and toxicological profiling. J. Drug Deliv. Sci. Technol. 2020, 60, 102069. [Google Scholar] [CrossRef]
- Ali, I.; Saifullah, S.; Ahmed, F.; Ullah, S.; Imkan, I.; Hussain, K.; Imran, M.; Shah, M.R. Synthesis of long-tail nonionic surfactants and their investigation for vesicle formation, drug entrapment, and biocompatibility. J. Liposome Res. 2020, 30, 255–262. [Google Scholar] [CrossRef] [PubMed]
- Alami-Milani, M.; Zakeri-Milani, P.; Valizadeh, H.; Salehi, R.; Jelvehgari, M. Preparation and evaluation of PCL-PEG-PCL micelles as potential nanocarriers for ocular delivery of dexamethasone. Iran. J. Basic Med. Sci. 2018, 21, 153–164. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Chen, J.; Li, B.; Yang, X.; Zeng, R.; Liu, Y.; Li, T.; Ho, R.J.Y.; Shao, J. PLGA-PEG-PLGA triblock copolymeric micelles as oral drug delivery system: In Vitro drug release and in vivo pharmacokinetics assessment. J. Colloid Interface Sci. 2017, 490, 542–552. [Google Scholar] [CrossRef]
- Dibaei, M.; Rouini, M.-R.; Sheikholeslami, B.; Gholami, M.; Dinarvand, R. The effect of surface treatment on the brain delivery of curcumin nanosuspension: In Vitro and in vivo studies. Int. J. Nanomed. 2019, 14, 5477–5490. [Google Scholar] [CrossRef]
- Chen, L.; Xie, Z.; Hu, J.; Chen, X.; Jing, X. Enantiomeric PLA–PEG block copolymers and their stereocomplex micelles used as rifampin delivery. J. Nanopart. Res. 2007, 9, 777–785. [Google Scholar] [CrossRef]
- Tagami, T.; Ernsting, M.J.; Li, S.-D. Optimization of a novel and improved thermosensitive liposome formulated with DPPC and a Brij surfactant using a robust in vitro system. J. Control. Release 2011, 154, 290–297. [Google Scholar] [CrossRef]
- Raval, A.; Pillai, S.A.; Bahadur, A.; Bahadur, P. Systematic characterization of Pluronic® micelles and their application for solubilization and in vitro release of some hydrophobic anticancer drugs. J. Mol. Liq. 2017, 230, 473–481. [Google Scholar] [CrossRef]
- Bengani, L.C.; Chauhan, A. Extended delivery of an anionic drug by contact lens loaded with a cationic surfactant. Biomaterials 2013, 34, 2814–2821. [Google Scholar] [CrossRef]
- Lu, G.; Jun, H.W. Diffusion studies of methotrexate in Carbopol and Poloxamer gels. Int. J. Pharm. 1998, 160, 1–9. [Google Scholar] [CrossRef]
- Makwana, S.B.; Patel, V.A.; Parmar, S.J. Development and characterization of in-situ gel for ophthalmic formulation containing ciprofloxacin hydrochloride. Results Pharm. Sci. 2016, 6, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Duangjit, S.; Opanasopit, P.; Rojanarata, T.; Ngawhirunpat, T. Evaluation of Meloxicam-Loaded Cationic Transfersomes as Transdermal Drug Delivery Carriers. AAPS Pharm. Sci. Tech. 2013, 14, 133–140. [Google Scholar] [CrossRef] [PubMed]
- Huynh, D.P.; Nguyen, M.K.; Pi, B.S.; Kim, M.S.; Chae, S.Y.; Lee, K.C.; Kim, B.S.; Kim, S.W.; Lee, D.S. Functionalized injectable hydrogels for controlled insulin delivery. Biomaterials 2008, 29, 2527–2534. [Google Scholar] [CrossRef]
- Li, J.; Li, X.; Ni, X.; Wang, X.; Li, H.; Leong, K.W. Self-assembled supramolecular hydrogels formed by biodegradable PEO–PHB–PEO triblock copolymers and α-cyclodextrin for controlled drug delivery. Biomaterials 2006, 27, 4132–4140. [Google Scholar] [CrossRef]
- Alhmoud, H.A. The effect of surfactant above and below the critical micelle concentration (CMC) and the mathematical models used to determine the kinetics of drug release from the matrix system. Afr. J. Pharm. Pharmcol. 2016, 18, 88–94. [Google Scholar]
- Danafar, H.; Rostamizadeh, K.; Davaran, S.; Hamidi, M. PLA-PEG-PLA copolymer-based polymersomes as nanocarriers for delivery of hydrophilic and hydrophobic drugs: Preparation and evaluation with atorvastatin and lisinopril. Drug Dev. Ind. Pharm. 2014, 40, 1411–1420. [Google Scholar] [CrossRef]
- Li, M.; Lv, S.; Tang, Z.; Song, W.; Yu, H.; Sun, H.; Liu, H.; Chen, X. Polypeptide/doxorubicin hydrochloride polymersomes prepared through organic solvent-free technique as a smart drug delivery platform. Macromol. Biosci. 2013, 13, 1150–1162. [Google Scholar] [CrossRef]
- Som, I.; Bhatia, K.; Yasir, M. Status of surfactants as penetration enhancers in transdermal drug delivery. J. Pharm. Bioallied. Sci. 2012, 4, 2–9. [Google Scholar] [CrossRef]
- Iatrou, H.; Dimas, K.; Gkikas, M.; Tsimblouli, C.; Sofianopoulou, S. Polymersomes from polypeptide containing triblock co- and terpolymers for drug delivery against pancreatic cancer: Asymmetry of the external hydrophilic blocks. Macromol. Biosci. 2014, 14, 1222–1238. [Google Scholar] [CrossRef]
- Fang, J.-Y.; Hwang, T.-L.; Huang, Y.-L.; Fang, C.-L. Enhancement of the transdermal delivery of catechins by liposomes incorporating anionic surfactants and ethanol. Int. J. Pharm. 2006, 310, 131–138. [Google Scholar] [CrossRef] [PubMed]
- Kelly, J.M.; Gross, A.L.; Martin, D.R.; Byrne, M.E. Polyethylene glycol-b-poly(lactic acid) polymersomes as vehicles for enzyme replacement therapy. Nanomedicine 2017, 12, 2591–2606. [Google Scholar] [CrossRef] [PubMed]
- Cesaretti, A.; Carlotti, B.; Gentili, P.L.; Clementi, C.; Germani, R.; Elisei, F. Doxycycline and oxytetracycline loading of a zwitterionic amphoteric surfactant-gel and their controlled release. Phys. Chem. Chem. Phys. 2014, 16, 23096–23107. [Google Scholar] [CrossRef] [PubMed]
- Tang, F.; Li, L.; Chen, D. Mesoporous Silica Nanoparticles: Synthesis, Biocompatibility and Drug Delivery. Adv. Mater. 2012, 24, 1504–1534. [Google Scholar] [CrossRef]
- Zhang, X.; Wang, S.; Liu, M.; Hui, J.; Yang, B.; Tao, L.; Wei, Y. Surfactant-dispersed nanodiamond: Biocompatibility evaluation and drug delivery applications. Toxicol. Res. 2013, 2, 335–342. [Google Scholar] [CrossRef]
- Men, Y.; Peng, S.; Yang, P.; Jiang, Q.; Zhang, Y.; Shen, B.; Dong, P.; Pang, Z.; Yang, W. Biodegradable Zwitterionic Nanogels with Long Circulation for Antitumor Drug Delivery. ACS Appl. Mater. Interfaces 2018, 10, 23509–23521. [Google Scholar] [CrossRef]
- Pitto-Barry, A.; Barry, N.P.E. Pluronic® block-copolymers in medicine: From chemical and biological versatility to rationalisation and clinical advances. Polym. Chem. 2014, 5, 3291–3297. [Google Scholar] [CrossRef]
- Brazel, C.S.; Peppas, N.A. Pulsatile local delivery of thrombolytic and antithrombotic agents using poly(N-isopropylacrylamide-co-methacrylic acid) hydrogels. J. Control. Release 1996, 39, 57–64. [Google Scholar] [CrossRef]
- Kumar, N.; Ravikumar, M.N.V.; Domb, A.J. Biodegradable block copolymers. Adv. Drug Deliv./Rev. 2001, 53, 23–44. [Google Scholar] [CrossRef]
- Gohy, J.-F. Block copolymer micelles. In Block Copolymers II; Abetz, V., Ed.; Springer: Berlin/Heidelberg, Germany, 2005; pp. 65–136. [Google Scholar]
- Khorshid, N.K.; Zhu, K.; Knudsen, K.D.; Bekhradnia, S.; Sande, S.A.; Nystrom, B. Novel structural changes during temperature-induced self-assembling and gelation of PLGA-PEG-PLGA triblock copolymer in aquoues solutions. Macromol. Biosci. 2016, 16, 1838–1852. [Google Scholar] [CrossRef]
- Cascone, M.G.; Sim, B.; Sandra, D. Blends of synthetic and natural polymers as drug delivery systems for growth hormone. Biomaterials 1995, 16, 569–574. [Google Scholar] [CrossRef]
- Veronese, F.M.; Pasut, G. PEGylation, successful approach to drug delivery. Drug Dicov. Today 2005, 10, 1451–1458. [Google Scholar] [CrossRef]
- Sahlin, J.; Peppas, N.A. Enhanced hydrogel adhesion by polymer interdiffusion: Use of linear poly(ehtylene glycol) as an adhesion promoter. J. Biomater. Sci. Polym. Ed. 1997, 8, 421–436. [Google Scholar] [CrossRef] [PubMed]
- Bell, C.L.; Peppas, N.A. Modulation of drug permeation through interpolymer complexed hydrogels for drug delivery applications. J. Control. Release 1996, 39, 201–207. [Google Scholar] [CrossRef]
- Putnam, D.; Kopecek, J. Polymer conjugates with anticancer activity. In Biopolymers II; Peppas, N.A., Langer, R.S., Eds.; Springer: Berlin/Heidelberg, Germany, 1995; Volume 122. [Google Scholar]
- Burnham, N.L. Polymers for delivering peptides and proteins. Am. J. Health-Syst. Pharm. 1994, 51, 210–218. [Google Scholar] [CrossRef]
- Abuchowski, A.; Es, T.V.; Palczuk, N.C.; Davis, F.F. Alteration of Immunological Properties of Bovine Serum Albumin by Covalent Attachment of Polyethylene Glycol. J. Biol. Chem. 1977, 252, 3578–3581. [Google Scholar] [CrossRef]
- Abuchowski, A.; McCoy, J.R.; Palczuk, N.C.; Es, T.V.; Davis, F.F. Effect of Covalent Attachment of Polyethylene Glycol on Immunogenicity and Circulating Life of Bovie Liver Catalase. J. Biol. Chem. 1977, 252, 3582–3586. [Google Scholar] [CrossRef]
- Saffer, E.M.; Tew, G.N.; Bhatia, S.R. Poly(lactic acid)-poly(ethyelen oxide) block copolymers: New directions in self-assembly and biomedical applications. Curr. Med. Chem. 2011, 18, 5676–5686. [Google Scholar] [CrossRef]
- Sanabria-DeLong, N.; Agrawal, S.K.; Bhatia, S.R.; Tew, G.N. Controlling hydrogel properties by crystallization of hydrophobic domains. Macromolecules 2006, 39, 1308–1310. [Google Scholar] [CrossRef]
- Ramchandani, M.; Robinson, D. In Vitro and in vivo release of ciprofloxacin from PLGA 50:50 implants. J. Control. Release 1998, 54, 167–175. [Google Scholar] [CrossRef]
- Hatefi, A.; Amsden, B. Biodegradable injectable in situ forming drug delivery systems. J. Control. Release 2002, 80, 9–28. [Google Scholar] [CrossRef]
- Garric, X.; Garreau, H.; Vert, M.; Molès, J.-P. Behaviors of keratinocytes and fibroblasts on films of PLA50–PEO–PLA50 triblock copolymers with various PLA segment lengths. J. Mater. Sci. Mater. Med. 2008, 19, 1645–1651. [Google Scholar] [CrossRef] [PubMed]
- Hanefeld, P.; Westedt, U.; Wombacher, R.; Kissel, T.; Schaper, A.; Wendorff, J.H.; Greiner, A. Coating of poly(p-xylylene) by PLA-PEO-PLA triblock copolymers with excellent polymer−polymer adhesion for stent applications. Biomacromolecules 2006, 7, 2086–2090. [Google Scholar] [CrossRef] [PubMed]
- Selek, H.; Sahin, S.; Ercans, M.T.; Sargon, M.; Hincal, A.A.; Kas, H.S. Formulation and in vitro/in vivo evaluation of terbutaline sulphate incorporated in PLGA (25/75) and L-PLA microspheres. J. Microencapsul. 2003, 20, 261–271. [Google Scholar] [PubMed]
- Lambert, W.J.; Peck, K.D. Development of an in situ forming biodegradable poly-lactide-coglycolide system for the controlled release of proteins. J. Control. Release 1995, 33, 189–195. [Google Scholar] [CrossRef]
- Dang, J.M.; Leong, K.W. Natural polymers for gene delivery and tissue engineering. Adv. Drug Deliv. Rev. 2006, 58, 487–499. [Google Scholar] [CrossRef]
- Rees, D.A.; Welsh, E.J. Secondary and tertiary structure of polysaccharides in solutions and gels. Angew. Chem. Int. Ed. Engl. 1977, 16, 214–224. [Google Scholar] [CrossRef]
- Morris, E.R.; Rees, D.A.; Thom, D.; Welsh, E.J. Conformation and intermolecular interactions of carbohydrate chains. J. Supramol. Struct. 1977, 6, 259–274. [Google Scholar] [CrossRef]
- Leong, K.W.; Mao, H.Q.; Truong-Le, V.L.; Roy, K.; Walsh, S.M.; August, J.T. DNA-polycation nanospheres as non-viral gene delivery vehicles. J. Control. Release 1998, 53, 183–193. [Google Scholar] [CrossRef]
- Cortivo, R.; Brun, P.; Rastrelli, A.; Abatangelo, G. In Vitro studies on biocompatiblity of hyaluronic acid esters. Biomaterials 1991, 12. [Google Scholar] [CrossRef]
- Benedetti, L.M.; Topp, E.M.; Stella, V.J. Microspheres of hyaluronic acid esters—Fabrication methods and in vitro hydrocortisone release. J. Control. Release 1990, 13, 33–41. [Google Scholar] [CrossRef]
- Hunt, J.A.; Joshi, H.N.; Stella, V.J.; Topp, E.M. Diffusion and drug release in polymer films prepared from ester derivatives of hyaluronic acid. J. Control. Release 1990, 12, 159–169. [Google Scholar] [CrossRef]
- Mumper, R.J.; Huffman, A.S.; Puolakkainen, P.A.; Bouchard, L.S.; Gombotz, W.R. Calcium-alginate beads for the oral delivery of transforming growth factor-β1 (TGF-β1): Stabilization of TGF-β1 by the addition of polyacrylic acid within acid-treated beads. J. Control. Release 1994, 30, 241–251. [Google Scholar] [CrossRef]
- Kim, H.; Park, H.; Lee, J.W.; Lee, K.Y. Magnetic field-responsive release of transforming growth factor beta 1 from heparin-modified alginate ferrogels. Carbohydr. Polym. 2016, 151, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Kaul, G.; Amiji, M. Long-circulating poly(ehtylene glycol)-modified Gelating nanoparticles for intreacellular delivery. Pharm. Res. 2002, 19, 1061–1067. [Google Scholar] [CrossRef]
- Goosen, M.F.A.; O’Shea, G.M.; Gharapetian, H.M.; Chou, S.; Sun, A.M. Optimization of microencapsulation parameters: Semipermeable microcapsules as a bioartificial pancreas. Biotechnol. Bioeng. 1985, 27, 146–150. [Google Scholar] [CrossRef] [PubMed]
- Lopes, M.; Shrestha, N.; Correia, A.; Shahbazi, M.-A.; Sarmento, B.; Hirvonen, J.; Veiga, F.; Seiça, R.; Ribeiro, A.; Santos, H.A. Dual chitosan/albumin-coated alginate/dextran sulfate nanoparticles for enhanced oral delivery of insulin. J. Control. Release 2016, 232, 29–41. [Google Scholar] [CrossRef]
- Parmar, A.; Chavda, S.; Bahadur, P. Pluronic–cationic surfactant mixed micelles: Solubilization and release of the drug hydrochlorothiazide. Colloids Surf. A Physicochem. Eng. Asp. 2014, 441, 389–397. [Google Scholar] [CrossRef]
- Abetz, V.; Simon, P.F.W. Phase behaviour and morphologies of block copolymers. In Block Copolymers I; Abetz, V., Ed.; Springer: Berlin/Heidelberg, Germany, 2005; pp. 125–212. [Google Scholar]
- Won, Y.-Y.; Brannan, A.K.; Davis, H.T.; Bates, F.S. Cryogenic Transmission Electron Microscopy (Cryo-TEM) of Micelles and Vesicles Formed in Water by Poly(ethylene oxide)-Based Block Copolymers. J. Phys. Chem. B 2002, 106, 3354–3364. [Google Scholar] [CrossRef]
- Michaels, A.S. Polyelectrolyte complexes. Eng. Chem. 1965, 57, 32–40. [Google Scholar] [CrossRef]
- Shovsky, A.; Varga, I.; Makuška, R.; Claesson, P.M. Formation and Stability of Water-Soluble, Molecular Polyelectrolyte Complexes: Effects of Charge Density, Mixing Ratio, and Polyelectrolyte Concentration. Langmuir 2009, 25, 6113–6121. [Google Scholar] [CrossRef] [PubMed]
- Volodkin, D.; von Klitzing, R. Competing mechanisms in polyelectrolyte multilayer formation and swelling: Polycation–polyanion pairing vs. polyelectrolyte–ion pairing. Curr. Opin. Colloid Interface Sci. 2014, 19, 25–31. [Google Scholar] [CrossRef]
- Das, B.P.; Tsianou, M. From polyelectrolyte complexes to polyelectrolyte multilayers: Electrostatic assembly, nanostructure, dynamics, and functional properties. Adv. Colloid Interface Sci. 2017, 244, 71–89. [Google Scholar] [CrossRef]
- Lankalapalli, S.; Kolapalli, V.R.M. Polyelectrolyte Complexes: A Review of their Applicability in Drug Delivery Technology. Indian J. Pharm. Sci. 2009, 71, 481–487. [Google Scholar] [CrossRef]
- Velk, N.; Uhlig, K.; Vikulina, A.; Duschl, C.; Volodkin, D. Mobility of lysozyme in poly(l-lysine)/hyaluronic acid multilayer films. Colloids Surf. B Biointerfaces 2016, 147, 343–350. [Google Scholar] [CrossRef] [PubMed]
- Shiraishi, S.; Imai, T.; Otagiri, M. Controlled release of indomethacin by chitosan-polyelectrolyte complex: Optimization and in vivo/in vitro evaluation. J. Control. Release 1993, 25, 217–225. [Google Scholar] [CrossRef]
- Fan, J.; Liu, Y.; Wang, S.; Liu, Y.; Li, S.; Long, R.; Zhang, R.; Kankala, R.K. Synthesis and characterization of innovative poly(lactide-co-glycolide)-(poly-l-ornithine/fucoidan) core–shell nanocarriers by layer-by-layer self-assembly. RSC Adv. 2017, 7, 32786–32794. [Google Scholar] [CrossRef]
- de Villiers, M.M.; Otto, D.P.; Strydom, S.J.; Lvov, Y.M. Introduction to nanocoatings produced by layer-by-layer (LbL) self-assembly. Adv. Drug Deliv. Rev. 2011, 63, 701–715. [Google Scholar] [CrossRef]
- Tan, J.P.K.; Wang, Q.; Tam, K.C. Control of burst release from nanogels via layer by layer assembly. J. Control. Release 2008, 128, 248–254. [Google Scholar] [CrossRef] [PubMed]
- Shi, Y.; Li, L. Current advances in sustained-release systems for parenteral drug delivery. Expert Opin. Drug Deliv. 2005, 2, 1039–1058. [Google Scholar] [CrossRef]
- Mitchell, M.J.; Billingsley, M.M.; Haley, R.M.; Wechsler, M.E.; Peppas, N.A.; Langer, R. Engineering precision nanoparticles for drug delivery. Nat. Rev. Drug Discov. 2020. [Google Scholar] [CrossRef] [PubMed]
- Chan, Y.-P.; Meyrueix, R.; Kravtzoff, R.; Soula, O.; Soula, G. Basulin, a long-acting formulation of human insulin based on medusa nanoparticles. NanoBiotechnology 2005, 1, 317–318. [Google Scholar] [CrossRef]
- Mikhail, A.S.; Allen, C. Poly(ethylene glycol)-b-poly(ε-caprolactone) micelles containing chemically conjugated and physically entrapped docetaxel: Synthesis, characterization, and the influence of the drug on micelle morphology. Biomacromolecules 2010, 11, 1273–1280. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Zhang, L.; Liu, Y.; Tan, S.; Qu, R.; Wu, Z.; Wu, Y.; Zhou, Y.; Huang, J. Preparation of PGA-PAE-micelles for enhanced antitumor efficacy of cisplatin. ACS Appl Mater. Interfaces 2018, 10, 25006–25016. [Google Scholar] [CrossRef] [PubMed]
- Yang, D.H.; Kim, H.J.; Park, K.; Kim, J.K.; Chun, H.J. Preparation of poly-l-lysine-based nanoparticles with pH-sensitive release of curcumin for targeted imaging and therapy of liver cancer in vitro and in vivo. Drug Deliv. 2018, 25, 950–960. [Google Scholar] [CrossRef] [PubMed]
- Govender, T.; Stolnik, S.; Xiong, C.; Zhang, S.; Illum, L.; Davis, S.S. Drug–polyionic block copolymer interactions for micelle formation: Physicochemical characterisation. J. Control. Release 2001, 75, 249–258. [Google Scholar] [CrossRef]
- Wu, H.; Zhu, L.; Torchilin, V.P. pH-sensitive poly(histidine)-PEG/DSPE-PEG co-polymer micelles for cytosolic drug delivery. Biomaterials 2013, 34, 1213–1222. [Google Scholar] [CrossRef]
- Yuan, J.; Luo, Y.; Gao, Q. Self-assembled polyion complex micelles for sustained release of hydrophilic drug. J. Microencapsul. 2011, 28, 93–98. [Google Scholar] [CrossRef]
- Zhu, C.; Jung, S.; Luo, S.; Meng, F.; Zhu, X.; Park, T.G.; Zhong, Z. Co-delivery of siRNA and paclitaxel into cancer cells by biodegradable cationic micelles based on PDMAEMA–PCL–PDMAEMA triblock copolymers. Biomaterials 2010, 31, 2408–2416. [Google Scholar] [CrossRef]
- Zheng, C.; Zheng, M.; Gong, P.; Deng, J.; Yi, H.; Zhang, P.; Zhang, Y.; Liu, P.; Ma, Y.; Cai, L. Polypeptide cationic micelles mediated co-delivery of docetaxel and siRNA for synergistic tumor therapy. Biomaterials 2013, 34, 3431–3438. [Google Scholar] [CrossRef]
- Wohlfart, S.; Khalansky, A.S.; Bernreuther, C.; Michaelis, M.; Cinatl, J.; Glatzel, M.; Kreuter, J. Treatment of glioblastoma with poly(isohexyl cyanoacrylate) nanoparticles. Int. J. Pharm. 2011, 415, 244–251. [Google Scholar] [CrossRef] [PubMed]
- Khodaverdi, E.; Gharechahi, M.; Alibolandi, M.; Tekie, F.S.M.; Khashyarmanesh, B.Z.; Hadizadeh, F. Self-assembled supramolecular hydrogel based on PCL-PEG-PCL triblock copolymer and γ-cyclodextrin inclusion complex for sustained delivery of dexamethasone. Int. J. Pharm. Investig. 2016, 6, 78–85. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Singh, J. In Vitro release of levonorgestrel from phase sensitive and thermosensitive smart polymer delivery systems. Pharm. Dev. Technol. 2005, 10, 319–325. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Ning, W.; Wang, J.; Choi, A.; Lee, P.-Y.; Tyagi, P.; Huang, L. Controlled Gene Delivery System Based on Thermosensitive Biodegradable Hydrogel. Pharm. Res. 2003, 20, 884–888. [Google Scholar] [CrossRef]
- Matthes, K.; Mino-Kenudson, M.; Sahani, D.V.; Holalkere, N.; Fowers, K.D.; Rathi, R.; Brugge, W.R. EUS-guided injection of paclitaxel (OncoGel) provides therapeutic drug concentrations in the porcine pancreas (with video). Gastrointest. Endosc. 2007, 65, 448–453. [Google Scholar] [CrossRef]
- Sarwar, M.S.; Huang, Q.; Ghaffar, A.; Abid, M.A.; Zafar, M.S.; Khurshid, Z.; Latif, M. A Smart Drug Delivery System Based on Biodegradable Chitosan/Poly(allylamine hydrochloride) Blend Films. Pharmaceuties 2020, 12, 131. [Google Scholar] [CrossRef]
- Zhang, L.; Zhang, Z.; Mason, R.P.; Sarkaria, J.N.; Zhao, D. Convertible MRI contrast: Sensing the delivery and release of anti-glioma nano-drugs. Sci. Rep. 2015, 5, 9874. [Google Scholar] [CrossRef]
- Barbieri, S.; Sonvico, F.; Como, C.; Colombo, G.; Zani, F.; Buttini, F.; Bettini, R.; Rossi, A.; Colombo, P. Lecithin/chitosan controlled release nanopreparations of tamoxifen citrate: Loading, enzyme-trigger release and cell uptake. J. Control. Release 2013, 167, 276–283. [Google Scholar] [CrossRef]
- Yokoyama, M.; Kwon, G.S.; Okano, T.; Sakurai, Y.; Seto, T.; Kataoka, K. Preparation of micelle-forming polymer-drug conjugates. Bioconjug Chem. 1992, 3, 295–301. [Google Scholar] [CrossRef]
- Sutton, D.; Nasongkla, N.; Blanco, E.; Gao, J. Functionalized micellar systems for cancer targeted drug delivery. Pharm. Res. 2007, 24, 1029–1046. [Google Scholar] [CrossRef]
- Torchilin, V.P. Micellar nanocarriers: Pharmaceutical perspectives. Pharm. Res. 2006, 24, 1. [Google Scholar] [CrossRef] [PubMed]
- Murthy, R.S.R. Polymeric micelles in targeted drug delivery. In Targeted Drug Delivery: Concepts and Design; Devarajan, P.V., Jain, S., Eds.; Springer International Publishing: Cham, Switzerland, 2015; pp. 501–541. [Google Scholar]
- Masood, F. Polymeric nanoparticles for targeted drug delivery system for cancer therapy. Mater. Sci. Eng. C 2016, 60, 569–578. [Google Scholar] [CrossRef] [PubMed]
- Nguyen-Kim, V.; Prévost, S.; Seidel, K.; Maier, W.; Marguerre, A.-K.; Oetter, G.; Tadros, T.; Gradzielski, M. Solubilization of active ingredients of different polarity in Pluronic® micellar solutions—Correlations between solubilizate polarity and solubilization site. J. Colloid Interface Sci. 2016, 477, 94–102. [Google Scholar] [CrossRef]
- Gaucher, G.; Dufresne, M.-H.; Sant, V.P.; Kang, N.; Maysinger, D.; Leroux, J.-C. Block copolymer micelles: Preparation, characterization and application in drug delivery. J. Control. Release 2005, 109, 169–188. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Luo, J.; Tan, S.; Otieno, B.O.; Zhang, Z. The applications of Vitamin E TPGS in drug delivery. Eur. J. Pharm. Sci. 2013, 49, 175–186. [Google Scholar] [CrossRef]
- Zhang, Z.; Grijpma, D.W.; Feijen, J. Thermo-sensitive transition of monomethoxy poly(ethylene glycol)-block-poly(trimethylene carbonate) films to micellar-like nanoparticles. J. Control. Release 2006, 112, 57–63. [Google Scholar] [CrossRef]
- Elsabahy, M.; Wooley, K.L. Design of polymeric nanoparticles for biomedical delivery applications. Chem Soc. Rev. 2012, 41, 2545–2561. [Google Scholar] [CrossRef]
- Wang, N.; Chen, X.-C.; Ding, R.-L.; Yang, X.-L.; Li, J.; Yu, X.-Q.; Li, K.; Wei, X. Synthesis of high drug loading, reactive oxygen species and esterase dual-responsive polymeric micelles for drug delivery. RSC Adv. 2019, 9, 2371–2378. [Google Scholar] [CrossRef]
- Triolo, D.; Craparo, E.F.; Porsio, B.; Fiorica, C.; Giammona, G.; Cavallaro, G. Polymeric drug delivery micelle-like nanocarriers for pulmonary administration of beclomethasone dipropionate. Colloids Surf. B Biointerfaces 2017, 151, 206–214. [Google Scholar] [CrossRef]
- Rösler, A.; Vandermeulen, G.W.M.; Klok, H.-A. Advanced drug delivery devices via self-assembly of amphiphilic block copolymers. Adv. Drug Deliv. Rev. 2001, 53, 95–108. [Google Scholar] [CrossRef]
- Lv, S.; Kim, H.; Song, Z.; Feng, L.; Yang, Y.; Baumgartner, R.; Tseng, K.-Y.; Dillon, S.J.; Leal, C.; Yin, L.; et al. Unimolecular Polypeptide Micelles via Ultrafast Polymerization of N-Carboxyanhydrides. J. Am. Chem. Soc. 2020, 142, 8570–8574. [Google Scholar] [CrossRef] [PubMed]
- Razavi, B.; Abdollahi, A.; Roghani-Mamaqani, H.; Salami-Kalajahi, M. Light- and temperature-responsive micellar carriers prepared by spiropyran-initiated atom transfer polymerization: Investigation of photochromism kinetics, responsivities, and controlled release of doxorubicin. Polymer 2020, 187, 122046. [Google Scholar] [CrossRef]
- Lavasanifar, A.; Samuel, J.; Kwon, G.S. The effect of alkyl core structure on micellar properties of poly(ethylene oxide)-block-poly(l-aspartamide) derivatives. Colloids Surf. B Biointerfaces 2001, 22, 115–126. [Google Scholar] [CrossRef]
- Yang, L.; Alexandridis, P. Physicochemical aspects of drug delivery and release from polymer-based colloids. Curr. Opin. Colloid Interface Sci. 2000, 5, 132–143. [Google Scholar] [CrossRef]
- Allen, C.; Maysinger, D.; Eisenberg, A. Nano-engineering block copolymer aggregates for drug delivery. Colloids Surf. B Biointerfaces 1999, 16, 3–27. [Google Scholar] [CrossRef]
- Bodratti, A.M.; Alexandridis, P. Formulation of poloxamers for drug delivery. J. Funct. Biomater 2018, 9, 11. [Google Scholar] [CrossRef]
- Yoo, H.S.; Park, T.G. Folate receptor targeted biodegradable polymeric doxorubicin micelles. J. Control. Release 2004, 96, 273–283. [Google Scholar] [CrossRef]
- Farokhzad, O.C.; Jon, S.; Khademhosseini, A.; Tran, T.-N.T.; LaVan, D.A.; Langer, R. Nanoparticle-Aptamer Bioconjugates. Cancer Res. 2004, 64, 7668. [Google Scholar] [CrossRef]
- Jeong, Y.-I.; Nah, J.-W.; Lee, H.-C.; Kim, S.-H.; Cho, C.-S. Adriamycin release from flower-type polymeric micelle based on star-block copolymer composed of poly(γ-benzyl l-glutamate) as the hydrophobic part and poly(ethylene oxide) as the hydrophilic part. Int. J. Pharm. 1999, 188, 49–58. [Google Scholar] [CrossRef]
- Wang, P.; Kankala, R.K.; Fan, J.; Long, R.; Liu, Y.; Wang, S. Poly-L-ornithine/fucoidan-coated calcium carbonate microparticles by layer-by-layer self-assembly technique for cancer theranostics. J. Mater. Sci. Mater. Med. 2018, 29, 68. [Google Scholar] [CrossRef]
- Wang, P.; Kankala, R.K.; Chen, B.; Long, R.; Cai, D.; Liu, Y.; Wang, S. Poly-allylamine hydrochloride and fucoidan-based self-assembled polyelectrolyte complex nanoparticles for cancer therapeutics. J. Biomed. Mater. Res. Part A 2019, 107, 339–347. [Google Scholar] [CrossRef] [PubMed]
- Matsumura, Y. Preclinical and clinical studies of anticancer drug-incorporated polymeric micelles. J. Drug Target. 2007, 15, 507–517. [Google Scholar] [CrossRef] [PubMed]
- Mu, L.; Chrastina, A.; Levchenko, T.; Torchilin, V.P. Micelles from poly(ethylene glycol)-phosphatidyl ethanolamine conjugates (Peg-Pe) as pharmaceutical nanocarriers for poorly soluble drug camptothecin. J. Biomed. Nanotechnol. 2005, 1, 190–195. [Google Scholar] [CrossRef]
- Wang, J.; Mongayt, D.A.; Lukyanov, A.N.; Levchenko, T.S.; Torchilin, V.P. Preparation and in vitro synergistic anticancer effect of Vitamin K3 and 1,8-diazabicyclo[5,4,0]undec-7-ene in poly(ethylene glycol)-diacyllipid micelles. Int. J. Pharm. 2004, 272, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Noori Koopaei, M.; Khoshayand, M.R.; Mostafavi, S.H.; Amini, M.; Khorramizadeh, M.R.; Jeddi Tehrani, M.; Atyabi, F.; Dinarvand, R. Docetaxel Loaded PEG-PLGA Nanoparticles: Optimized Drug Loading, In-vitro Cytotoxicity and In-vivo Antitumor Effect. Iran. J. Pharm. Res. 2014, 13, 819–833. [Google Scholar] [PubMed]
- Zhen, S.; Yi, X.; Zhao, Z.; Lou, X.; Xia, F.; Tang, B.Z. Drug delivery micelles with efficient near-infrared photosensitizer for combined image-guided photodynamic therapy and chemotherapy of drug-resistant cancer. Biomaterials 2019, 218, 119330. [Google Scholar] [CrossRef]
- Costamagna, F.; Hillaireau, H.; Vergnaud, J.; Clarisse, D.; Jamgotchian, L.; Loreau, O.; Denis, S.; Gravel, E.; Doris, E.; Fattal, E. Nanotoxicology at the particle/micelle frontier: Influence of core-polymerization on the intracellular distribution, cytotoxicity and genotoxicity of polydiacetylene micelles. Nanoscale 2020, 12, 2452–2463. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Yu, L.; Han, L.; Sha, X.; Fang, X. Difunctional Pluronic copolymer micelles for paclitaxel delivery: Synergistic effect of folate-mediated targeting and Pluronic-mediated overcoming multidrug resistance in tumor cell lines. Int. J. Pharm. 2007, 337, 63–73. [Google Scholar] [CrossRef]
- Su, C.-Y.; Liu, J.-J.; Ho, Y.-S.; Huang, Y.-Y.; Chang, V.H.-S.; Liu, D.-Z.; Chen, L.-C.; Ho, H.-O.; Sheu, M.-T. Development and characterization of docetaxel-loaded lecithin-stabilized micellar drug delivery system (LsbMDDs) for improving the therapeutic efficacy and reducing systemic toxicity. Eur. J. Pharm. Biopharm. 2018, 123, 9–19. [Google Scholar] [CrossRef]
- Byrne, M.E.; Park, K.; Peppas, N.A. Molecular imprinting within hydrogels. Adv. Drug Deliv. Rev. 2002, 54, 149–161. [Google Scholar] [CrossRef]
- Xu, C.; Kopeček, J. Self-assembling hydrogels. Polym. Bull. 2007, 58, 53–63. [Google Scholar] [CrossRef]
- Peppas, N.A.; Bures, P.; Leobandung, W.; Ichikawa, H. Hydrogels in pharmaceutical formulations. Eur. J. Pharm. Biopharm. 2000, 50, 27–46. [Google Scholar] [CrossRef]
- Peppas, N.A.; Hilt, J.Z.; Khademhosseini, A.; Langer, R. Hydrogels in biology and medicine: From molecular principles to bionanotechnology. Adv. Mater. 2006, 18, 1345–1360. [Google Scholar] [CrossRef]
- Lowman, A.M.; Peppas, N.A. Hydrogels. In Encyclopedia of Controlled Drug Delivery; Mathiowitz, E., Ed.; Wiley: New York, NY, USA, 1999; pp. 397–418. [Google Scholar]
- Peppas, N.A. Hydrogels in Medicine and Pharmacy; CRC Press: Boca Raton, FL, USA, 1987. [Google Scholar]
- Kopeček, J. Hydrogels from soft contact lenses and implants to self-assembled nanomaterials. J. Polym Sci. A Polym. Chem. 2009, 47, 5929–5946. [Google Scholar] [CrossRef] [PubMed]
- Wichterle, O.; LÍM, D. Hydrophilic gels for biological use. Nature 1960, 185, 117. [Google Scholar] [CrossRef]
- Caló, E.; Khutoryanskiy, V.V. Biomedical applications of hydrogels: A review of patents and commercial products. Eur. Polym. J. 2015, 65, 252–267. [Google Scholar] [CrossRef]
- Park, K. Controlled Drug Delivery: Challenges and Strategies; ACS: Washington, DC, USA, 1997. [Google Scholar]
- Singh, N.K.; Lee, D.S. In Situ gelling pH- and temperature-sensitive biodegradable block copolymer hydrogels for drug delivery. J. Control. Release 2014, 193, 214–227. [Google Scholar] [CrossRef] [PubMed]
- Peppas, N.A. Hydrogels and drug delivery. Curr. Opin. Colloid. Interface Sci. 1997, 2, 531–537. [Google Scholar] [CrossRef]
- Thrimawithana, T.R.; Rupenthal, I.D.; Young, S.A.; Alany, R.G. Environment-sensitive polymers for ophthalmic drug delivery. J. Drug Deliv. Sci. Technol. 2012, 22, 117–124. [Google Scholar] [CrossRef]
- Hoare, T.R.; Kohane, D.S. Hydrogels in drug delivery: Progress and challenges. Polymer 2008, 49, 1993–2007. [Google Scholar] [CrossRef]
- Vert, M.; Schwach, G.; Engel, R.; Coudane, J. Something new in the field of PLA/GA bioresorbable polymers? J. Control. Release 1998, 53, 85–92. [Google Scholar] [CrossRef]
- Samchenko, Y.; Ulberg, Z.; Korotych, O. Multipurpose smart hydrogel systems. Adv. Colloid Interface Sci. 2011, 168, 247–262. [Google Scholar] [CrossRef] [PubMed]
- Alexandridis, P.; Hatton, T.A. Poly(ethyelen oxide)-poly(propylene oxide)-poly(ethylene oxide) block copolymer surfactants in aqueous solutions and at interfaces: Thermodynamics, strucutre, dynamics, and modeling. Colloids Surf. A Physicochem. Eng. Asp. 1995, 96, 1–46. [Google Scholar] [CrossRef]
- Robinson, J.R.; Mlynek, G.M. Bioadhesive and phase-change polymers for ocular drug delivery. Adv. Drug Deliv. Rev. 1995, 16, 45–50. [Google Scholar] [CrossRef]
- Zeng, N.; Dumortier, G.; Maury, M.; Mignet, N.; Boudy, V. Influence of additives on a thermosensitive hydrogel for buccal delivery of salbutamol: Relation between micellization, gelation, mechanic and release properties. Int. J. Pharm. 2014, 467, 70–83. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, P.; Rupenthal, I.D. Injectable implants for the sustained release of protein and peptide drugs. Drug Discov. Today 2013, 18, 337–349. [Google Scholar] [CrossRef] [PubMed]
- Kamaly, N.; Yameen, B.; Wu, J.; Farokhzad, O.C. Degradable controlled-release polymers and polymeric nanoparticles: Mechanisms of controlling drug release. Chem. Rev. 2016, 116, 2602–2663. [Google Scholar] [CrossRef]
- Samlowski, W.E.; McGregor, J.R.; Jurek, M.; Baudys, M.; Zentner, G.M.; Fowers, K.D. ReGel polymer-based delivery of interleukin-2 as a cancer treatment. J. Immunother. 2006, 29, 524–535. [Google Scholar] [CrossRef]
- Zhu, W.; Masaki, T.; Bae, Y.H.; Rathi, R.; Cheung, A.K.; Kern, S.E. Development of a sustained-release system for perivascular delivery of dipyridamole. J. Biomed. Mater. Res. Part B Appl. Biomater. 2006, 77, 135–143. [Google Scholar] [CrossRef]
- Choi, S.; Baudys, M.; Kim, S.W. Control of blood glucose by novel GLP-1 delivery using biodegradable triblock copolymer of PLGA-PEG-PLGA in type 2 diabetic rats. Pharm. Res. 2004, 21, 827–831. [Google Scholar] [CrossRef]
- Lee, A.L.Z.; Ng, V.W.L.; Gao, S.; Hedrick, J.L.; Yang, Y.Y. Injectable hydrogels from triblock copolymers of vitamin E-functionalized polycarbonate and poly(ethylene glycol) for subcutaneous delivery of antibodies for cancer therapy. Adv. Funct Mater. 2014, 24, 1538–1550. [Google Scholar] [CrossRef]
- Cheng, D.; Xu, J.; Sun, C.; Li, Y.; Fan, J.; Zhu, J.; Liu, D.; Zhao, J.; Xu, D. RADA 16-I hydrogel-released CXCL 12 stably promotes stem cell migration. J. Tissue Sci. Eng. 2019, 9. [Google Scholar] [CrossRef]
- Spencer, D.S.; Shodeinde, A.B.; Beckman, D.W.; Luu, B.C.; Hodges, H.R.; Peppas, N.A. Biodegradable cationic nanogels with tunable size, swelling and pKa for drug delivery. Int. J. Pharm. 2020, 588, 119691. [Google Scholar] [CrossRef]
- Laddha, U.D.; Mahajan, H.S. An insight to ocular in situ gelling systems. Int. J. Adv. Pharm. 2017, 6, 31–40. [Google Scholar] [CrossRef]
- Wu, Y.; Liu, Y.; Li, X.; Kebebe, D.; Zhang, B.; Ren, J.; Lu, J.; Li, J.; Du, S.; Liu, Z. Research progress of in-situ gelling ophthalmic drug delivery system. Asian J. Pharm. Sci. 2019, 14, 1–15. [Google Scholar] [CrossRef]
- Destruel, P.-L.; Zeng, N.; Maury, M.; Mignet, N.; Boudy, V. In Vitro and in vivo evaluation of in situ gelling systems for sustained topical ophthalmic delivery: State of the art and beyond. Drug Discov. Today 2017, 22, 638–651. [Google Scholar] [CrossRef]
- Liu, W.; Borrell, M.A.; Venerus, D.C.; Mieler, W.F.; Kang-Mieler, J.J. Characterization of Biodegradable Microsphere-Hydrogel Ocular Drug Delivery System for Controlled and Extended Release of RanibizumabLiu et al. Transl. Vis. Sci. Technol. 2019, 8, 12. [Google Scholar] [CrossRef]
- Shedden, A.; Laurence, J.; Tipping, R. Efficacy and tolerability of timolol maleate ophthalmic gel-forming solution versus timolol ophthalmic solution in adults with open-angle glaucoma or ocular hypertension: A six-month, double-masked, multicenter study. Clin. Ther. 2001, 23, 440–450. [Google Scholar] [CrossRef]
- Mundorf, T.K.; Ogawa, T.; Naka, H.; Novack, G.D.; Stephens Crockett, R. A 12-month, multicenter, randomized, double-masked, parallel-group comparison of timolol-LA once daily and timolol maleate ophthalmic solution twice daily in the treatment of adults with glaucoma or ocular hypertension. Clin. Ther. 2004, 26, 541–551. [Google Scholar] [CrossRef]
- Morsi, N.; Ghorab, D.; Refai, H.; Teba, H. Ketoroloac tromethamine loaded nanodispersion incorporated into thermosensitive in situ gel for prolonged ocular delivery. Int. J. Pharm. 2016, 506, 57–67. [Google Scholar] [CrossRef] [PubMed]
- Yu, Y.; Feng, R.; Li, J.; Wang, Y.; Song, Y.; Tan, G.; Liu, D.; Liu, W.; Yang, X.; Pan, H.; et al. A hybrid genipin-crosslinked dual-sensitive hydrogel/nanostructured lipid carrier ocular drug delivery platform. Asian J. Pharm. Sci. 2019, 14, 423–434. [Google Scholar] [CrossRef]
- Yu, A.; Shi, H.; Liu, H.; Bao, Z.; Dai, M.; Lin, D.; Lin, D.; Xu, X.; Li, X.; Wang, Y. Mucoadhesive dexamethasone-glycol chitosan nanoparticles for ophthalmic drug delivery. Int. J. Pharm. 2020, 575, 118943. [Google Scholar] [CrossRef] [PubMed]
- Bao, Z.; Yu, A.; Shi, H.; Hu, Y.; Jin, B.; Lin, D.; Dai, M.; Lei, L.; Li, X.; Wang, Y. Glycol chitosan/oxidized hyaluronic acid hydrogel film for topical ocular delivery of dexamethasone and levofloxacin. Int. J. Biol. Macromol. 2021, 167, 659–666. [Google Scholar] [CrossRef]
- Kankala, R.K.; Wang, S.-B.; Chen, A.-Z.; Zhang, Y.S. Chapter 2—Self-Assembled Nanogels: From Particles to Scaffolds and Membranes. In Handbook of Nanomaterials for Cancer Theranostics; Conde, J., Ed.; Elsevier: Amsterdam, The Netherlands, 2018; pp. 33–62. [Google Scholar]
- Tan, Y.-L.; Liu, C.-G. Self-aggregated nanoparticles from linoleic acid modified carboxymethyl chitosan: Synthesis, characterization and application in vitro. Colloids Surf. B Biointerfaces 2009, 69, 178–182. [Google Scholar] [CrossRef] [PubMed]
- González-Urías, A.; Manzanares-Guevara, L.A.; Licea-Claveríe, Á.; Ochoa-Terán, A.; Licea-Navarro, A.F.; Bernaldez-Sarabia, J.; Zapata-González, I. Stimuli responsive nanogels with intrinsic fluorescence: Promising nanovehicles for controlled drug delivery and cell internalization detection in diverse cancer cell lines. Eur. Polym. J. 2021, 144, 110200. [Google Scholar] [CrossRef]
- Peng, S.; Ouyang, B.; Xin, Y.; Zhao, W.; Shen, S.; Zhan, M.; Lu, L. Hypoxia-degradable and long-circulating zwitterionic phosphorylcholine-based nanogel for enhanced tumor drug delivery. Acta Pharm. Sin. B 2020. [Google Scholar] [CrossRef]
- Choi, H.; Hwang, B.W.; Park, K.M.; Kim, K.S.; Hahn, S.K. Degradable Nanomotors Using Platinum Deposited Complex of Calcium Carbonate and Hyaluronate Nanogels for Targeted Drug Delivery. Part. Part. Syst Charact. 2020, 37, 1900418. [Google Scholar] [CrossRef]
- Tyliszczak, B.; Drabczyk, A.; Kudłacik-Kramarczyk, S.; Bialik-Wąs, K.; Sobczak-Kupiec, A. In Vitro cytotoxicity of hydrogels based on chitosan and modified with gold nanoparticles. J. Polym. Res. 2017, 24, 153. [Google Scholar] [CrossRef]
- Wang, W.; Deng, L.; Huang, P.; Xu, S.; Li, X.; Lv, N.; Wang, L.; Hu, R.; Zhang, J.; Dong, A. Toxicity and in vivo biological effect of the nanoparticular self-supported hydrogel of a thermosensitive copolymer for non-invasive drug delivery. J. Biomed. Mater. Res. Part A 2014, 102, 17–29. [Google Scholar] [CrossRef]
- Fetsch, C.; Gaitzsch, J.; Messager, L.; Battaglia, G.; Luxenhofer, R. Self-Assembly of amphiphilic block copolypeptoids – Micelles, worms and polymersomes. Sci. Rep. 2016, 6, 33491. [Google Scholar] [CrossRef]
- Lee, J.S.; Feijen, J. Polymersomes for drug delivery: Design, formation and characterization. J. Control. Release 2012, 161, 473–483. [Google Scholar] [CrossRef] [PubMed]
- Hearnden, V.; Sankar, V.; Hull, K.; Juras, D.V.; Greenberg, M.; Kerr, A.R.; Lockhart, P.B.; Patton, L.L.; Porter, S.; Thornhill, M.H. New developments and opportunities in oral mucosal drug delivery for local and systemic disease. Adv. Drug Deliv. Rev. 2012, 64, 16–28. [Google Scholar] [CrossRef] [PubMed]
- Bangham, A.D. Physical structure and behavior of lipids and lipid enzymes. Adv. Lipid Res. 1963, 1, 65–104. [Google Scholar] [PubMed]
- Bangham, A.D. Liposomes: The Babraham connection. Chem. Phys. Lipids 1993, 64, 275–285. [Google Scholar] [CrossRef]
- Ventola, C.L. Progress in nanomedicine: Approved and investigational nanodrugs. P T Peer-Rev. J. Formul. Manag. 2017, 42, 742–755. [Google Scholar]
- Akbarzadeh, A.; Rezaei-Sadabady, R.; Davaran, S.; Joo, S.W.; Zarghami, N.; Hanifehpour, Y.; Samiei, M.; Kouhi, M.; Nejati-Koshki, K. Liposome: Classification, preparation, and applications. Nanoscale Res. Lett. 2013, 8, 102. [Google Scholar] [CrossRef]
- Ceh, B.; Lasic, D.D. A rigorous theory of remote loading of drugs into liposomes. Langmuir 1995, 11, 3356–3368. [Google Scholar] [CrossRef]
- Demel, R.A.; De Kruyff, B. The function of sterols in membranes. Biochim. Biophys. Acta (BBA)-Rev. Biomembr. 1976, 457, 109–132. [Google Scholar] [CrossRef]
- Papahadjopoulos, D.; Jacobson, K.; Nir, S.; Isac, I. Phase transitions in phospholipid vesicles Fluorescence polarization and permeability measurements concerning the effect of temperature and cholesterol. Biochim. Biophys. Acta (BBA)-Biomembr. 1973, 311, 330–348. [Google Scholar] [CrossRef]
- Virden, J.W.; Berg, J.C. Sodium chloride-induced aggregation of dipalmitoylphoshpatidylglycerol small unilamellar vesicles with varying amounts of incorporated cholesterol. Langmuir 1992, 8, 1532–1537. [Google Scholar] [CrossRef]
- Briuglia, M.L.; Rotella, C.; McFarlane, A.; Lamprou, D.A. Influence of cholesterol on liposome stability and on in vitro drug release. Drug Deliv. Transl. Res. 2015, 5, 231–242. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.-C.; Lee, K.-E.; Kim, J.-J.; Lim, S.-H. The Effect of Cholesterol in the Liposome Bilayer on the Stabilization of Incorporated Retinol. J. Liposome Res. 2005, 15, 157–166. [Google Scholar] [CrossRef] [PubMed]
- Anajafi, T.; Mallik, S. Polymersome-based drug-delivery strategies for cancer therapeutics. Ther. Deliv. 2015, 6, 521–534. [Google Scholar] [CrossRef] [PubMed]
- Kelly, J.M.; Pearce, E.E.; Martin, D.R.; Byrne, M.E. Lyoprotectants modify and stabilize self-assembly of polymersomes. Polymer 2016, 87, 316–322. [Google Scholar] [CrossRef]
- Photos, P.J.; Bacakova, L.; Discher, B.; Bates, F.S.; Discher, D.E. Polymer vesicles in vivo: Correlations with PEG molecular weight. J. Control. Release 2003, 90, 323–334. [Google Scholar] [CrossRef]
- Ahmed, F.; Pakunlu, R.I.; Srinivas, G.; Brannan, A.; Bates, F.; Klein, M.L.; Minko, T.; Discher, D.E. Shrinkage of a rapidly growing tumor by drug-loaded polymersomes: pH-triggered release through copolymer degradation. Mol. Pharm. 2006, 3, 340–350. [Google Scholar] [CrossRef]
- Choucair, A.; Lim Soo, P.; Eisenberg, A. Active loading and tunable release of doxorubicin from block copolymer vesicles. Langmuir 2005, 21, 9308–9313. [Google Scholar] [CrossRef]
- Qin, S.; Geng, Y.; Discher, D.E.; Yang, S. Temperature-controlled assembly and release from polymer vesicles of poly(ethylene oxide)-block- poly(N-isopropylacrylamide). Adv. Mater. 2006, 18, 2905–2909. [Google Scholar] [CrossRef]
- Meng, F.; Zhong, Z.; Feijen, J. Stimuli-responsive polymersomes for programmed drug delivery. Biomacromolecules 2009, 10, 197–209. [Google Scholar] [CrossRef]
- Daubian, D.; Gaitzsch, J.; Meier, W. Synthesis and complex self-assembly of amphiphilic block copolymers with a branched hydrophobic poly(2-oxazoline) into multicompartment micelles, pseudo-vesicles and yolk/shell nanoparticles. Polym. Chem. 2020, 11, 1237–1248. [Google Scholar] [CrossRef]
- Krishnamoorthy, B.; Karanam, V.; Chellan, V.R.; Siram, K.; Natarajan, T.s.; Gregory, M. Polymersomes as an effective drug delivery system for glioma—A review. J. Drug Target. 2014, 22, 469–477. [Google Scholar] [CrossRef] [PubMed]
- Larsen, J.M.; Pearce, E.E.; Martin, D.R.; Byrne, M.E. Polymersomes: Towards Treatment of Neurodegenerative Disorders through Enzyme Replacement Therapy. In Proceedings of the Society for Biomaterials 2014 Annual Meeting & Exposition, Denver, CO, USA, 16–19 April 2014. [Google Scholar]
- Sanson, C.; Diou, O.; Thévenot, J.; Ibarboure, E.; Soum, A.; Brûlet, A.; Miraux, S.; Thiaudière, E.; Tan, S.; Brisson, A.; et al. Doxorubicin loaded magnetic polymersomes: Theranostic nanocarriers for MR imaging and magneto-chemotherapy. ACS Nano 2011, 5, 1122–1140. [Google Scholar] [CrossRef] [PubMed]
- Walvekar, P.; Gannimani, R.; Salih, M.; Makhathini, S.; Mocktar, C.; Govender, T. Self-assembled oleylamine grafted hyaluronic acid polymersomes for delivery of vancomycin against methicillin resistant Staphylococcus aureus (MRSA). Colloids Surf. B Biointerfaces 2019, 182, 110388. [Google Scholar] [CrossRef] [PubMed]
- Mohammed, M.; Japir, A.A.-W.; Lu, N.; Wang, Y.; Felix Mukerabigwi, J.; Zhou, Q.; Ge, Z. Membrane-cross-linked polymersomes with tumor pH-tunable selective permeability as intelligent nanoreactors and drug delivery vehicles. Eur. Polym. J. 2020, 138, 109982. [Google Scholar] [CrossRef]
- Zavvar, T.; Babaei, M.; Abnous, K.; Taghdisi, S.M.; Nekooei, S.; Ramezani, M.; Alibolandi, M. Synthesis of multimodal polymersomes for targeted drug delivery and MR/fluorescence imaging in metastatic breast cancer model. Int. J. Pharm. 2020, 578, 119091. [Google Scholar] [CrossRef]
- Wei, P.; Sun, M.; Yang, B.; Xiao, J.; Du, J. Ultrasound-responsive polymersomes capable of endosomal escape for efficient cancer therapy. J. Control. Release 2020, 322, 81–94. [Google Scholar] [CrossRef]
- Zhou, Y.; Chen, R.; Yang, H.; Bao, C.; Fan, J.; Wang, C.; Lin, Q.; Zhu, L. Light-responsive polymersomes with a charge-switch for targeted drug delivery. J. Mater. Chem. B 2020, 8, 727–735. [Google Scholar] [CrossRef]
- Ghorbanizamani, F.; Moulahoum, H.; Sanli, S.; Bayir, E.; Zihnioglu, F.; Timur, S. pH-bioresponsive poly(ε-caprolactone)-based polymersome for effective drug delivery in cancer and protein glycoxidation prevention. Arch. Biochem. Biophys. 2020, 695, 108643. [Google Scholar] [CrossRef]
- Verma, R.K.; Garg, S. Current Status of Drug Delivery Technologies and Future Directions. Pharm. Technol. On-Line 2001, 25, 1–14. [Google Scholar]
- Controlled Release Drug Delivery Market Analysis Report by Eechnology (Implants, t#ransdermal, Microencapsulation, Targeted Delivery), by Release Mechanisms, by Applications, and Segment Forecasts, 2018–2025; Grand View Research, Inc.: San Francisco, CA, USA, 2018; p. 124.
- Caster, J.M.; Patel, A.N.; Zhang, T.; Wang, A. Investigational nanomedicines in 2016: A review of nanotherapeutics currently undergoing clinical trials. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2017, 9, e1416. [Google Scholar] [CrossRef] [PubMed]
- Hamaguchi, T.; Kato, K.; Yasui, H.; Morizane, C.; Ikeda, M.; Ueno, H.; Muro, K.; Yamada, Y.; Okusaka, T.; Shirao, K.; et al. A phase I and pharmacokinetic study of NK105, a paclitaxel-incorporating micellar nanoparticle formulation. Br. J. Cancer 2007, 97, 170–176. [Google Scholar] [CrossRef] [PubMed]
- Matsumura, Y.; Hamaguchi, T.; Ura, T.; Muro, K.; Yamada, Y.; Shimada, Y.; Shirao, K.; Okusaka, T.; Ueno, H.; Ikeda, M.; et al. Phase I clinical trial and pharmacokinetic evaluation of NK911, a micelle-encapsulated doxorubicin. Br. J. Cancer 2004, 91, 1775–1781. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.S.; Chung, H.C.; Im, S.A.; Park, Y.H.; Kim, C.S.; Kim, S.-B.; Rha, S.Y.; Lee, M.Y.; Ro, J. Multicenter phase II trial of Genexol-PM, a Cremophor-free, polymeric micelle formulation of paclitaxel, in patients with metastatic breast cancer. Breast Cancer Res. Treat. 2008, 108, 241–250. [Google Scholar] [CrossRef]
- Bobo, D.; Robinson, K.J.; Islam, J.; Thurecht, K.J.; Corrie, S.R. Nanoparticle-Based Medicines: A Review of FDA-Approved Materials and Clinical Trials to Date. Pharm. Res. 2016, 33, 2373–2387. [Google Scholar] [CrossRef]
- Barenholz, Y. Doxil®—The first FDA-approved nano-drug: Lessons learned. J. Control. Release 2012, 160, 117–134. [Google Scholar] [CrossRef]
- Clemons, K.V.; Stevens, D.A. Comparative efficacies of four amphotericin B formulations--Fungizone, amphotec (Amphocil), AmBisome, and Abelcet--against systemic murine aspergillosis. Antimicrob. Agents Chemother. 2004, 48, 1047–1050. [Google Scholar] [CrossRef]
- Nicolini, A.; Giardino, R.; Carpi, A.; Ferrari, P.; Anselmi, L.; Colosimo, S.; Conte, M.; Fini, M.; Giavaresi, G.; Berti, P.; et al. Metastatic breast cancer: An updating. Biomed. Pharm. 2006, 60, 548–556. [Google Scholar] [CrossRef]
- Silverman, J.A.; Deitcher, S.R. Marqibo® (vincristine sulfate liposome injection) improves the pharmacokinetics and pharmacodynamics of vincristine. Cancer Chemother. Pharm. 2013, 71, 555–564. [Google Scholar] [CrossRef]
- Lindner, L.H.; Hossann, M.; Vogeser, M.; Teichert, N.; Wachholz, K.; Eibl, H.; Hiddemann, W.; Issels, R.D. Dual role of hexadecylphosphocholine (miltefosine) in thermosensitive liposomes: Active ingredient and mediator of drug release. J. Control. Release 2008, 125, 112–120. [Google Scholar] [CrossRef]
- Cortes, J.E.; Goldberg, S.L.; Feldman, E.J.; Rizzeri, D.A.; Hogge, D.E.; Larson, M.; Pigneux, A.; Recher, C.; Schiller, G.; Warzocha, K.; et al. Phase II, multicenter, randomized trial of CPX-351 (cytarabine:daunorubicin) liposome injection versus intensive salvage therapy in adults with first relapse AML. Cancer 2015, 121, 234–242. [Google Scholar] [CrossRef] [PubMed]
- Clancy, J.P.; Dupont, L.; Konstan, M.W.; Billings, J.; Fustik, S.; Goss, C.H.; Lymp, J.; Minic, P.; Quittner, A.L.; Rubenstein, R.C.; et al. Phase II studies of nebulised Arikace in CF patients with Pseudomonas aeruginosa infection. Thorax 2013, 68, 818–825. [Google Scholar] [CrossRef]
- Mazzotta, E.; Tavano, L.; Muzzalupo, R. Thermo-sensitive vesicles in controlled drug delivery for chemotherapy. Pharmer 2018, 10, 150. [Google Scholar] [CrossRef] [PubMed]
- Lidar, Z.; Mardor, Y.; Jonas, T.; Pfeffer, R.; Faibel, M.; Nass, D.; Hadani, M.; Ram, Z. Convection-enhanced delivery of paclitaxel for the treatment of recurrent malignant glioma: A phase I/II clinical study. J. Neurosurg. 2004, 100, 472–479. [Google Scholar] [CrossRef] [PubMed]
- Salvatori, R.; Woodmansee, W.W.; Molitch, M.; Gordon, M.B.; Lomax, K.G. Lanreotide extended-release aqueous-gel formulation, injected by patient, partner or healthcare provider in patients with acromegaly in the United States: 1-year data from the SODA registry. Pituitary 2014, 17, 13–21. [Google Scholar] [CrossRef]
- Mandal, A.; Clegg, J.R.; Anselmo, A.C.; Mitragotri, S. Hydrogels in the clinic. Bioeng. Transl. Med. 2020, 5, e10158. [Google Scholar] [CrossRef]
- Bhatia, D.; Mehtab, S.; Krishnan, R.; Indi, S.S.; Basu, A.; Krishnan, Y. Icosahedral DNA nanocapsules by modular assembly. Angew. Chem. Int. Ed. Engl. 2009, 48, 4134–4137. [Google Scholar] [CrossRef]
- Nimjee, S.M.; White, R.R.; Becker, R.C.; Sullenger, B.A. Aptamers as Therapeutics. Annu. Rev. Pharmacol. Toxicol. 2017, 57, 61–79. [Google Scholar] [CrossRef]
- Wilner, O.I.; Willner, I. Functionalized DNA nanostructures. Chem. Rev. 2012, 112, 2528–2556. [Google Scholar] [CrossRef]
- Sundaram, P.; Kurniawan, H.; Byrne, M.E.; Wower, J. Therapeutic RNA aptamers in clinical trials. Eur. J. Pharm. Sci. 2013, 48, 259–271. [Google Scholar] [CrossRef]
- Sundaram, P.; Wower, J.; Byrne, M.E. A nanoscale drug delivery carrier using nucleic acid aptamers for extended release of therapeutic. Nanomed. Nanotechnol. Biol. Med. 2012, 8, 1143–1151. [Google Scholar] [CrossRef] [PubMed]
- Battig, M.R.; Soontornworajit, B.; Wang, Y. Programmable release of multiple protein drugs from aptamer-functionalized hydrogels via nucleic acid hybridization. J. Am. Chem. Soc. 2012, 134, 12410–12413. [Google Scholar] [CrossRef] [PubMed]
- Soontornworajit, B.; Zhou, J.; Snipes, M.P.; Battig, M.R.; Wang, Y. Affinity hydrogels for controlled protein release using nucleic acid aptamers and complementary oligonucleotides. Biomaterials 2011, 32, 6839–6849. [Google Scholar] [CrossRef] [PubMed]


| Surfactant Formulation | Therapeutic(s) Delivered | Medical Application | Ref. |
|---|---|---|---|
| Non-Ionic | |||
| SDC-PC (40 nm) | Ciprofloxacin | ** | [34,35] |
| Sorbitan monostearate (Span 60) (77–84 nm) | Policarpine HCl | Ocular | [33,36] |
| Tween 80 (46 to 114 nm) | Curcumin | Brain | [37,38] |
| Brij 78 (90 to 120 nm) | Doxorubicin | Oncology | [39,40] |
| Cationic | |||
| CKC (240 μm) | Dexamethasone 21-disodium phosphate | Ocular | [41,42] |
| Sodium alginate-HPMC | Cripofloxacin Hydrochloride | Ocular | [43] |
| DTAB (60–90 nm) | Meloxicam | Dermal Delivery | [44,45] |
| CPC (60–90 nm) | Meloxicam | Dermal Delivery | [44,46] |
| Anionic | |||
| SLS (130–220 nm) | Propranolol HCl | ** | [47,48] |
| ST (20 nm) | Propranolol HCl | ** | [47,49] |
| SDS (110–250 nm) | ** | Transdermal drug delivery | [50,51] |
| DA (400 nm) | (+)-catechin | Transdermal drug delivery | [52,53] |
| Amphoteric | |||
| pDoAo | Oxytetracycline | ** | [48,54] |
| LSB | ** | Transdermal drug delivery | [49,55] |
| Lecithin (611 nm) | Doxorubicin Hydrochloride | ** | [56] |
| PSBMA (230–290 nm) | Doxorubicin | Oncology | [57] |
| Formulation | Therapeutic(s) Delivered | Medical Application | Benefits | Ref. |
|---|---|---|---|---|
| Micelles | ||||
| PCL-b-PEG-b-PCL (10 nm) | Dexamethasone Docetaxel | Ocular Delivery Oncology | Extended Release | [35] [107] |
| PLGA-b-PEG-b-PLGA (77–84 nm) | US597@micelles | Oncology | Sustained oral formulation | [36] |
| PLA-b-PEG (<200 nm) | Rifampin | Bacterial infections | Micelle morphology and release profile controlled by the stereocomplex structure of PLA | [38] |
| Pluronics® (<60 nm) | Genistein, paclitaxel and quercetin Hydrochorothiazide | Oncology Diuretic | Extended Release | [40] [91] |
| PGA-b-PAE (100–200 nm) | Cisplatin | Oncology | Improved drug loading with small sized micelles | [108] |
| PLL-b-DOCA-b-mPEG (<200 nm) | Curcumin | Oncology | Prolonged blood circulation time and provided successful biodistribution images | [109] |
| PEG-b-Pasp (22 to 60 nm) | Diminazene aceturate | ** | Non-covalent interactions to form polyionic micelles | [110] |
| PLH-b-PEG (112 nm) | Paclitaxel | Oncology | Fast pH controlled drug release and cell internalization | [111] |
| PEI-g-PVP (142 nm) | Folic acid | ** | Drug loaded through electrostatic interaction. Drug release rate moderated by pH | [112] |
| PDMAEMA-PCL (<150 nm) | siRNA and paclitaxel | Oncology | Co-delivery of drugs with different physicochemical properties | [113] |
| PEG-b-PLL-b-PLLeu (100–125 nm) | Docetaxel and siRNA-Bcl-2 | Oncology | Cationic micelles for passive targeting of cancer cells | [114] |
| PIHCA-Tween80 (<320 nm) | Doxorubicin | Oncology | Spherical nanoparticles with high loading percentages | [115] |
| Hydrogels | ||||
| Pluronics® | Lidocaine | Topical Formulations | Release rate was controlled through the viscosity of the hydrogel | [42] |
| Sodium alginate-HPMC | Cripofloxacin Hydrochloride | Ocular | pH responsive release system | [43] |
| PCL-b-PEG-b-PCL | Dexamethasone Insulin | ** Glucose control | Extended Release | [116] [45] |
| PEO-b-PHB-b-PEO | FITC-Dextran | ** | Extended Release | [46] |
| PLGA-b-PEG-b-PLGA | Levonorgestrel DNA | Birth Control Gene therapy | Extended Release | [117] [118] |
| OncoGelTM | Paclitaxel | Solid tumors | Extended Release | [119] |
| PAH/Chitosan | Ciprofloxacin hydrochlorine monohydrate | ** | Release of hydrophilic and/or unstable agents | [120] |
| Vesicles (Polymersomes/Liposomes) | ||||
| PLA-b-PEG-b-PLA (200–300 nm) | Atorvastatin and lisinopril | Oncology | High encapsulation efficiency of hydrophobic and hydrophilic drugs | [48] |
| mPEG-b-(PPLG-g-MSA) * (20 nm) | Doxorubicin Hydrochloride | ** | Micelles formed through electrostatic interactions | [49] |
| PLL-b-PBLG-b-PEO (<300 nm) | Doxorubicin and Paclitaxel | Pancreatic cancer | Temperature- and pH responsive release | [51] |
| PEG-b-PLA (<200 nm) | Active beta-galactosidase | Enzyme Replacement Therapy | pH responsive release system | [53] |
| PS (100 nm) | Arsenic Trioxide | Glioblastoma Multiform (GBM) | pH responsive system | [121] |
| Lecithin/Chitosan (240 nm–1 μm) | Tamoxifen citrate | Oncology | Oral administration. Relese rate controlled by enzymatic degradation | [122] |
| Formulation | Therapeutic(s) | Medical Application | Clinical Phase | Ref. |
|---|---|---|---|---|
| Micelles | ||||
| PEG-pAsp | Paclitaxel | Advanced stomach cancer | II | [232] |
| PEG-b-pAsp | Doxorubicin | Pancreatic and colorectal cancer | II | [233] |
| Genexol™-PM (20–50 nm) | mPEG-PLGA-Paclitaxel | Breast cancer | IV | [234] |
| Adynovate | PEGylated factor VII | Hemophilia A | FDA Approved, 2015 | [16] [235] |
| EstrasorbTM | Estradiol | Menapause hormone Therapy | FDA Approved 2003 | [178] |
| Cimzia® | PEGylated antibody fragment | Chron’s disease, rheumatoid arthritis, psoriasis | FDA Approved 2008–2013 | [178] |
| Mircrea® | Erythropoiesis-stimulating agent | Anemica with chronic renal failure | FDA Approved 2007 | [178] |
| Plegridy® | PEGylated IFNbeta-1a | Multiple Sclerosis | FDA Approved 2014 | [178] |
| Polymersomes/Liposomes | ||||
| Doxil® (200–500 nm) | Doxorubicin | Ovarian cancer AIDS-related Kaposis’s sarcoma; breast cancer | FDA approved, 1995 | [236] [237] |
| Amphotech® | Amphotericin | Fungal infection | FDA approved, 1996 | [237] |
| Myocet | Doxorubicin | Metastatic Breast Cancer | [238] | |
| Marquibo® | Vincristine | Philadelphia chromosome-negative (Ph-) Acute lymphoblastic leukemia | FDA approved, 2012 | [239] |
| ThermoDox (50 to 200 nm) | Doxorubicin | Breast cancer, primary liver cancer | II and III | [240] |
| VyxeosTM | Daunorubicin and Cytarabine | Acute myeloid leukemia (AML), AML with myelodysplasia-related changes | FDA approved, 2017 | [204,241] |
| Arikayce | Amikacin | Chronic lung infections | I, II and III | [242] |
| Lipoquin | Ciprofloxacin | Cystic fibrosis (CF) and Non-CF bronchiectasis | II | [231] |
| HER2-targeted MM302 | Doxorubicin | HER2-positive breast cancer | I | [231] |
| ThermoDox® | Doxorubicin | Cancer | III | [243] |
| Onivyde | Irinotecan | Pancreatic Cancer | FDA Approved 2015 | [16] |
| Hydrogels | ||||
| OncoGelTM | Paclitaxel | Solid tumors | I and II | [244] |
| Pluronics® | Doxorubicin | Advanced esophageal adenocarcinoma | III | [58] |
| Somatuline® | Lanreotide | Acromegaly | ** | [245] |
| SpaceOAR® | PEGylated | Prostate cancer radiotherapy tissue protection | FDA Approved 2010, 2015 | [246] |
| Vantas® | Histrelin acetate and gonadotropin releasing hormone | Prostate cancer | FDA Approved 2004, 2005 | [246] |
| Radiesse® | Hydroxylapatite | Production of collagen | FDA Approved 2015 | [246] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Osorno, L.L.; Brandley, A.N.; Maldonado, D.E.; Yiantsos, A.; Mosley, R.J.; Byrne, M.E. Review of Contemporary Self-Assembled Systems for the Controlled Delivery of Therapeutics in Medicine. Nanomaterials 2021, 11, 278. https://doi.org/10.3390/nano11020278
Osorno LL, Brandley AN, Maldonado DE, Yiantsos A, Mosley RJ, Byrne ME. Review of Contemporary Self-Assembled Systems for the Controlled Delivery of Therapeutics in Medicine. Nanomaterials. 2021; 11(2):278. https://doi.org/10.3390/nano11020278
Chicago/Turabian StyleOsorno, Laura L., Alyssa N. Brandley, Daniel E. Maldonado, Alex Yiantsos, Robert J. Mosley, and Mark E. Byrne. 2021. "Review of Contemporary Self-Assembled Systems for the Controlled Delivery of Therapeutics in Medicine" Nanomaterials 11, no. 2: 278. https://doi.org/10.3390/nano11020278
APA StyleOsorno, L. L., Brandley, A. N., Maldonado, D. E., Yiantsos, A., Mosley, R. J., & Byrne, M. E. (2021). Review of Contemporary Self-Assembled Systems for the Controlled Delivery of Therapeutics in Medicine. Nanomaterials, 11(2), 278. https://doi.org/10.3390/nano11020278







