Analysis of Insertion Torque of Orthodontic Mini-Implants Depending on the System and the Morphological Substrate
Abstract
1. Introduction
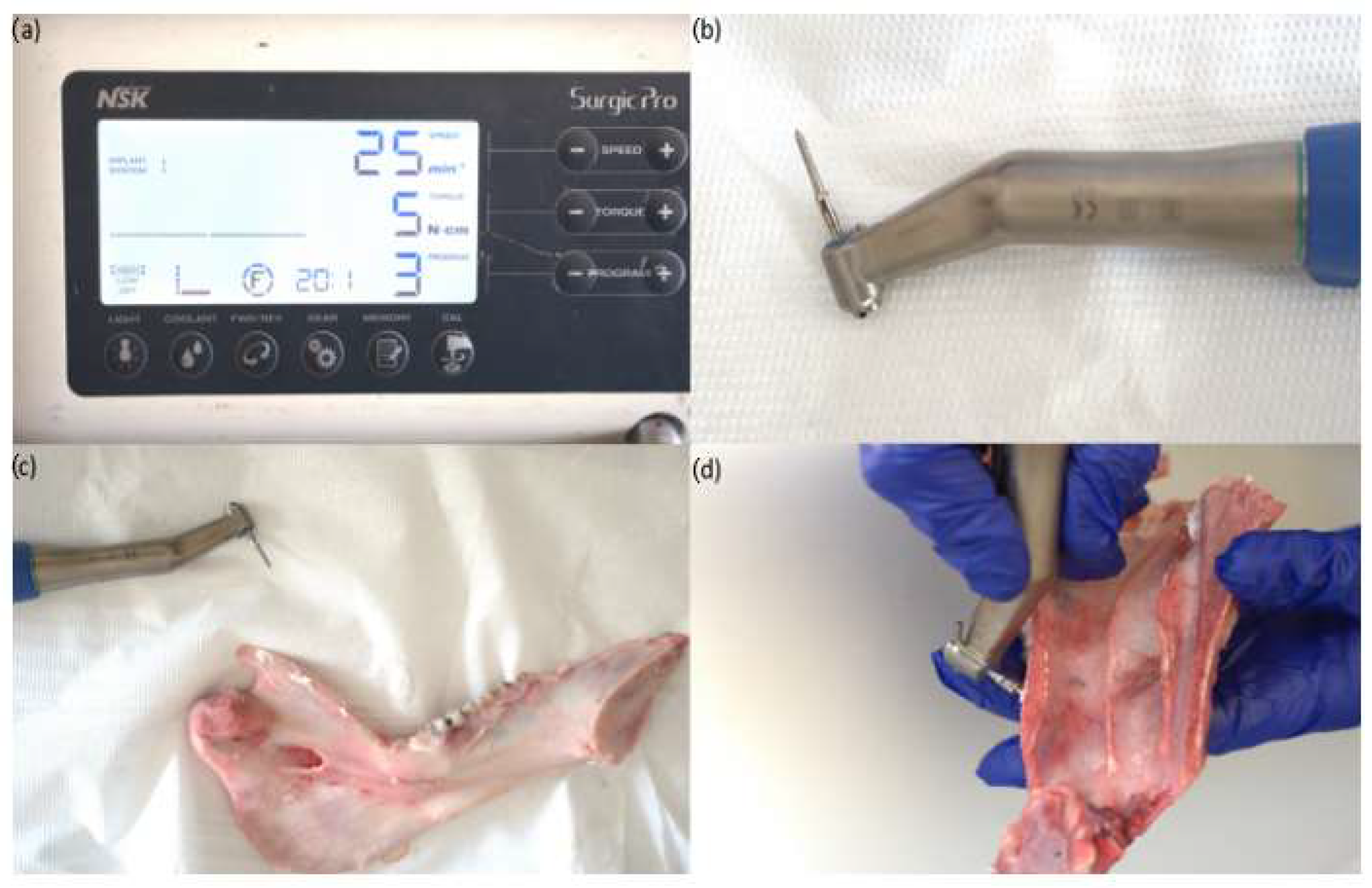
2. Materials and Methods
- Dual Top Anchor System (Jeil Medical Corporation, Seoul, Republic of Korea);
- OrthAnchor System (Osstem, Eschborn, Germany);
- Leone System (Leone orthodontic products, Sesto Fiorentino, Firenze, Italy).

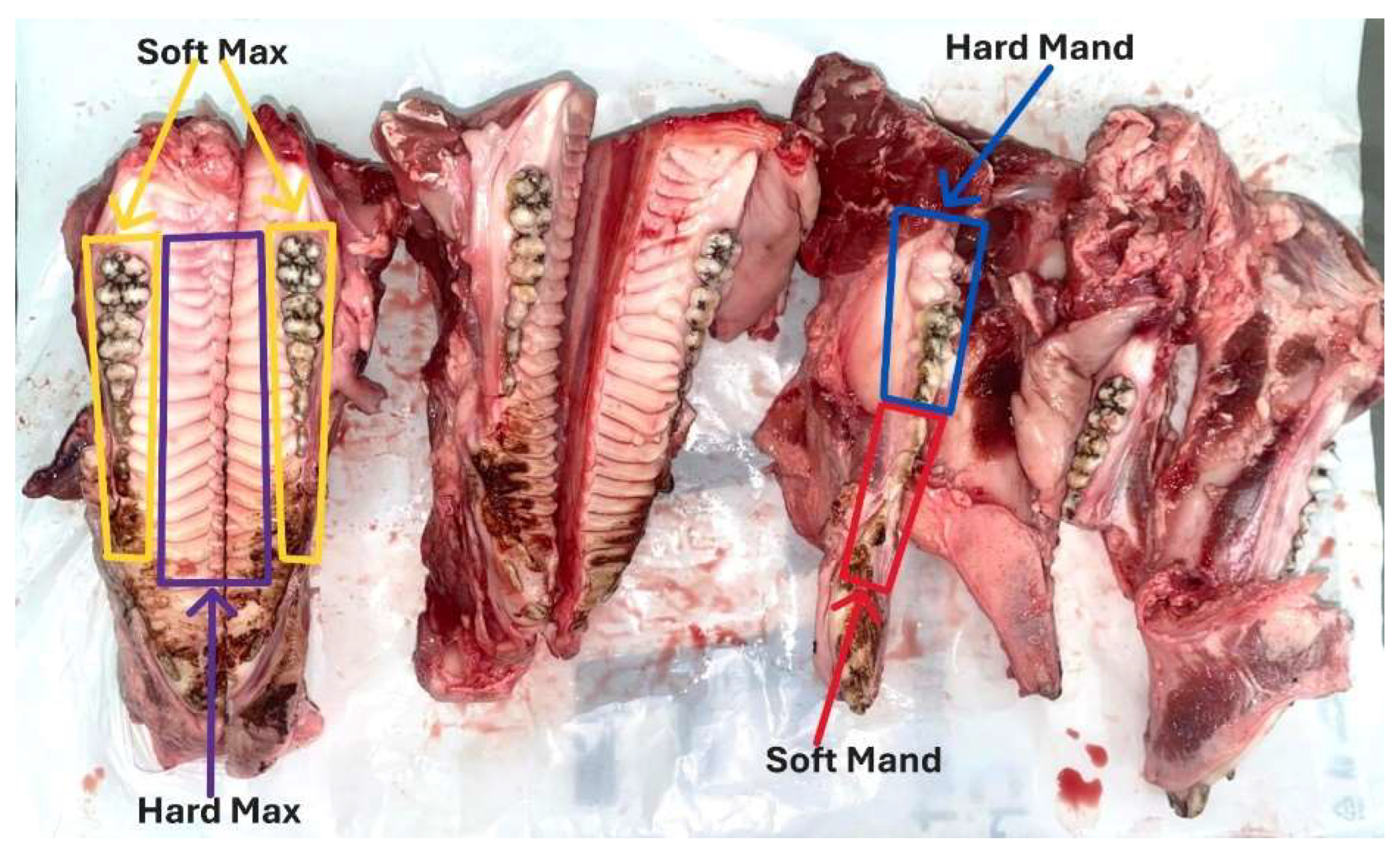
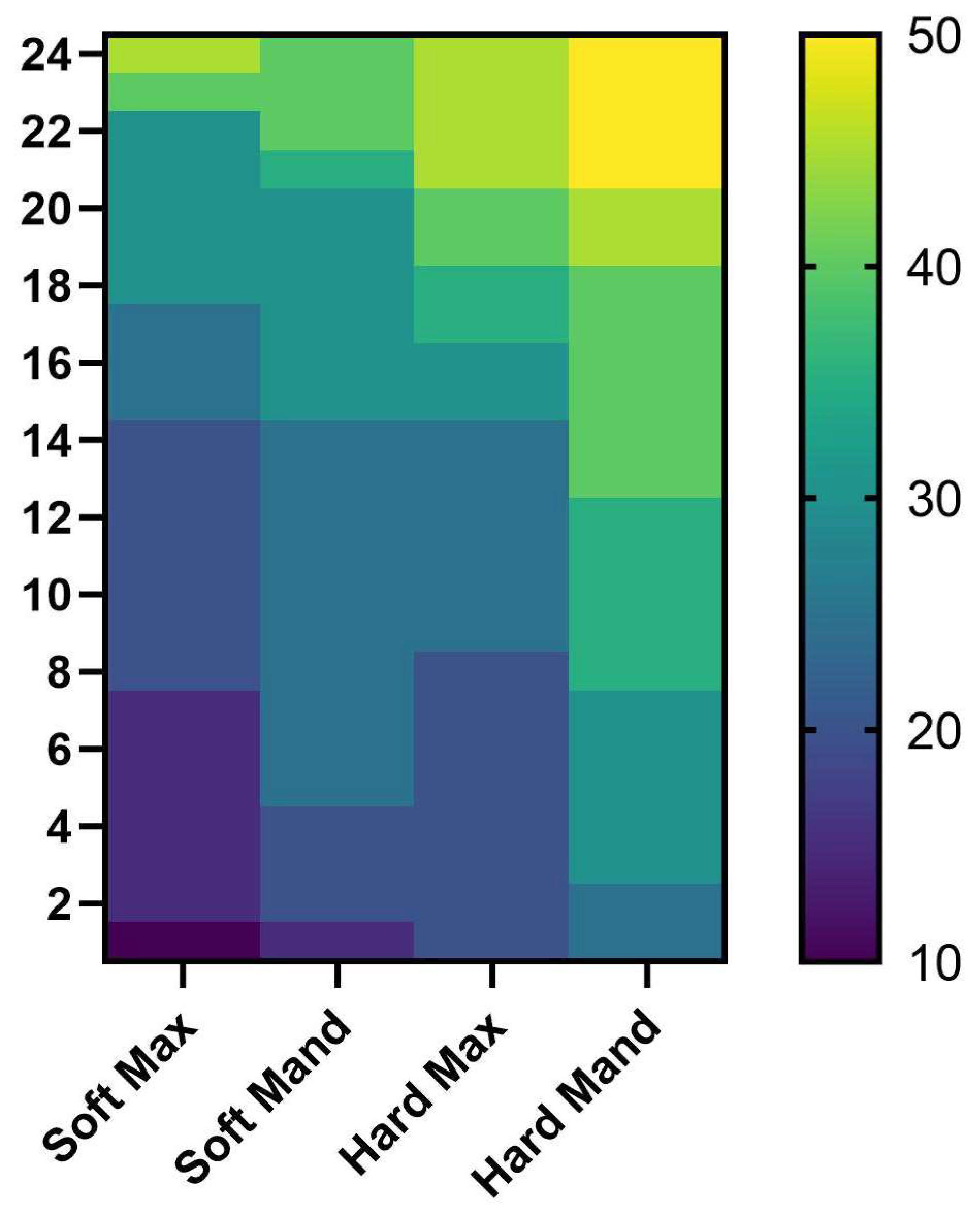
- Soft Mand—represents the mandibular interdental area of the premolars and premolar edentulous area;
- Hard Mand—represents the mandibular interdental area of the molars and the retromolar area;
- Soft Max—represents the maxillary interdental area of the molars, premolars and premolar edentulous area;
- Hard Max—represents the maxillary area at the level of the palatine vault.
Statistical Analysis
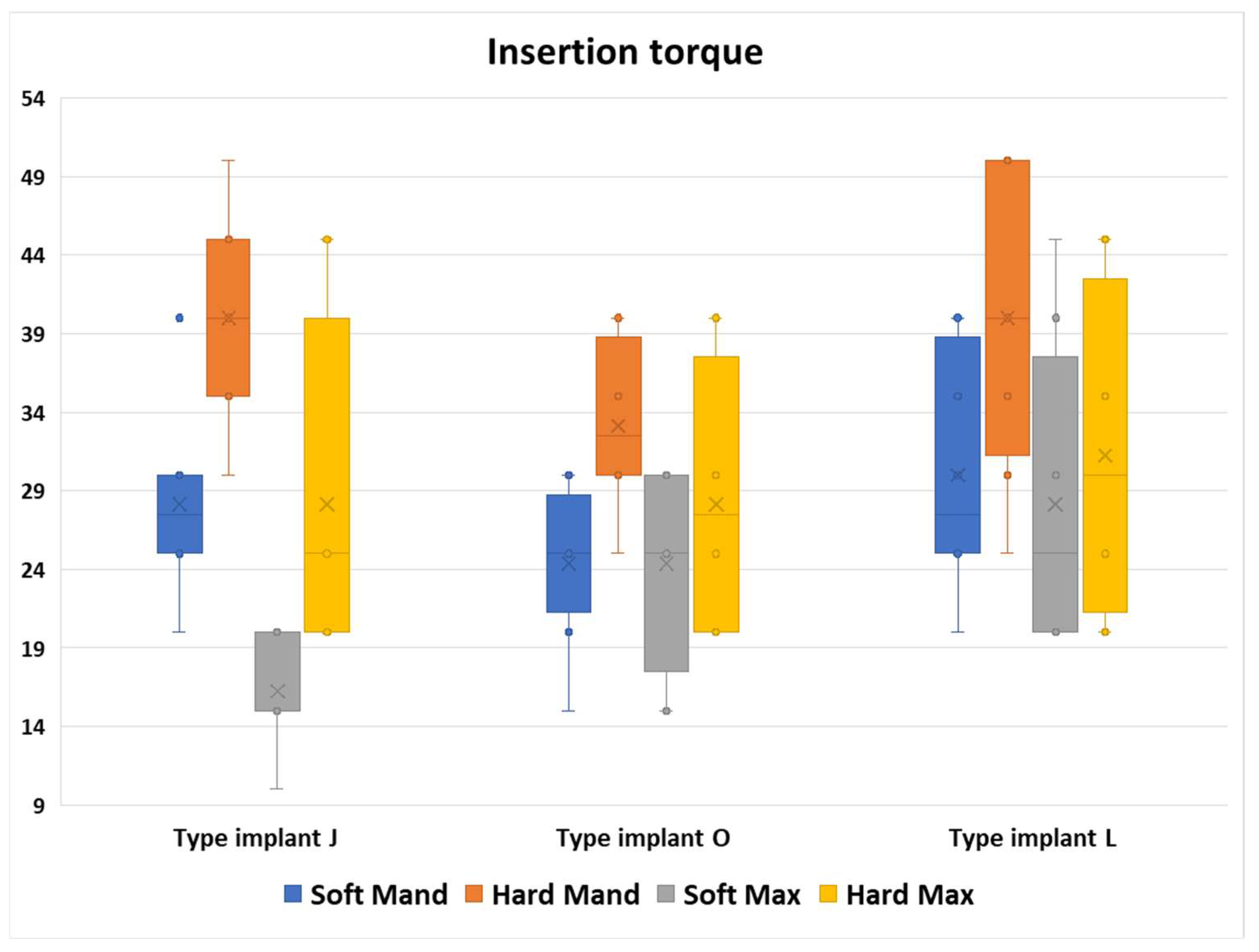
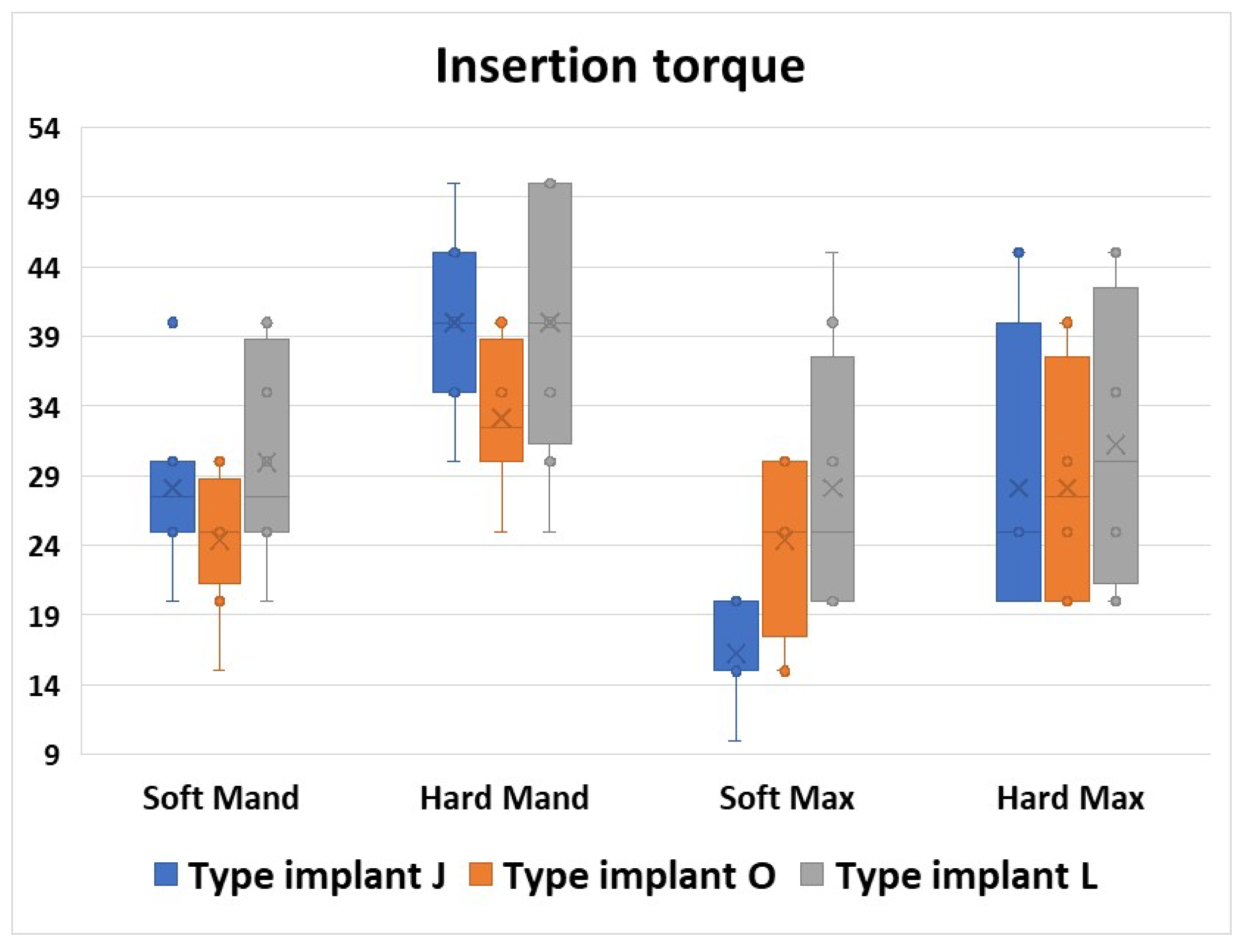
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Jahanbin, A.; Ziya, F.; Bardideh, E.; Hafez, S.; Abtahi, M. In vitro physical properties and clinical stability of reused orthodontic miniscrews: A systematic review and meta-analysis. J. World Fed. Orthod. 2024, 14, 97–110. [Google Scholar] [CrossRef]
- Meursinge Reynders, R.A.; Ronchi, L.; Ladu, L.; van Etten-Jamaludin, F.; Bipat, S. Insertion torque and success of orthodontic mini-implants: A systematic review. Am. J. Orthod. Dentofac. Orthop. 2012, 142, 596–614.e5. [Google Scholar] [CrossRef]
- Abdalla, K.L.; Ali Mahmood, T.M. The effect of different orthodontic mini-implant brands and geometry on primary stability (an in vitro study). Heliyon 2023, 9, e19858. [Google Scholar] [CrossRef]
- Migliorati, M.; Benedicenti, S.; Drago, S. Mini screw design and bone characterstics: Study of primary stability. Am. J. Orthod. Dentofac. Orthop. 2012, 142, 228–234. [Google Scholar] [CrossRef]
- Xavier, J.; Sarika, K.; Ajith, V.V.; Sapna Varma, N.K. Evaluation of Strain and Insertion Torque of Mini-implants at 90° and 45° Angulations on a Bone Model using Three-Dimensional Finite Element Analysis. Contemp. Clin. Dent. 2023, 14, 25–31. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Puls, G.L.; Marañón-Vásquez, G.A.; Ramos, C.A.V.; Reis, C.L.B.; Reis, A.C.D.; Stuani, M.B.S.; Romano, F.L.; Matsumoto, M.A.N. Insertion torque, flexural strength and surface alterations of stainless steel and titanium alloy orthodontic mini-implants: An in vitro study. Dent. Press. J. Orthod. 2024, 29, e2423282. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Antoniac, I.; Manescu Paltanea, V.; Antoniac, A.; Paltanea, G. Magnesium-based alloys with adapted interfaces for bone implants and tissue engineering. Regen. Biomater. 2023, 10, rbad095. [Google Scholar] [CrossRef]
- Vlasa, A.; Biris, C.; Lazar, L.; Bud, A.; Bud, E.; Molnar-Varlam, C.; Maris, M.; Pacurar, M. Scanning electron microscope analysis of titanium alloy orthodontic implants. Mater. Plast. 2017, 54, 345–347. [Google Scholar] [CrossRef]
- Sabley, K.H.; Shenoy, U.; Banerjee, S.; Akhare, P.; Hazarey, A.; Karia, H. Comparative evaluation of biomechanical performance of titanium and stainless steel mini implants at different angulations in maxilla: A finite element analysis. J. Indian Orthod. Soc. 2019, 53, 197–205. [Google Scholar] [CrossRef]
- Baser, B.; Ozel, M.B. Comparison of primary stability of used and unused self-tapping and self-drilling orthodontic mini-implants. Adv. Clin. Exp. Med. 2024, 33, 483–489. [Google Scholar] [CrossRef] [PubMed]
- Cha, J.-Y.; Kil, J.-K.; Yoon, T.-M.; Hwang, C.-J. Miniscrew stability evaluated with computerized tomography scanning, American. J. Orthod. Dentofac. Orthop. 2010, 137, 73–79. [Google Scholar] [CrossRef]
- Heo, Y.Y.; Cho, K.C.; Baek, S.H. Angled-predrilling depth and mini-implant shape effects on the mechanical properties of self-drilling orthodontic mini-implants during the angled insertion procedure. Angle Orthod. 2012, 82, 881–888. [Google Scholar] [CrossRef]
- Suzuki, E.Y.; Suzuki, B. Placement and removal torque values of orthodontic miniscrew implants. Am. J. Orthod. Dentofac. Orthop. 2011, 139, 669–678. [Google Scholar] [CrossRef]
- Martinez, H.; Davarpanah, M.; Missika, P.; Celletti, R.; Lazzara, R. Optimal implant stabilization in low density bone. Clin. Oral Implant. Res. 2001, 12, 423–432. [Google Scholar] [CrossRef]
- O’Sullivan, D.; Sennerby, L.; Meredith, N. Influence of implant taper on the primary and secondary stability of osseointegrated titanium implants. Clin. Oral Implant. Res. 2004, 15, 474–480. [Google Scholar] [CrossRef]
- Siegele, D.; Soltesz, U. Numerical investigations of the influence of implant shape on stress distribution in the jaw bone. Int. J. Oral Maxillofac. Implant. 1989, 4, 333–340. [Google Scholar]
- Wang, S.; Liu, Y.; Fang, D.; Shi, S. The miniature pig: A useful large animal model for dental and orofacial research. Oral Dis. 2007, 13, 530–537. [Google Scholar] [CrossRef] [PubMed]
- Jin, Y.; Yuan, X.; Zhang, H.; Jiang, Q.; Fan, Q.; Li, J.; Lai, W.; Long, H. A rat model for microimplant-assisted rapid palatal expansion. Biochem. Biophys. Res. Commun. 2024, 741, 150964. [Google Scholar] [CrossRef] [PubMed]
- Valeri, C.; Aloisio, A.; Quinzi, V.; di Stefano, G.; Marzo, G. Characterizing orthodontic mini-screws in the hard palate of pigs: An experimental and finite-element study. Heliyon 2024, 10, e24952. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Migliorati, M.; Drago, S.; Barberis, F.; Schiavetti, I.; Dalessandri, D.; Benedicenti, S.; Biavati, A.S. Torque Loss After Miniscrew Placement: An In-Vitro Study Followed by a Clinical Trial. Open Dent. J. 2016, 10, 251–260. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wilmes, B.; Su, Y.Y.; Drescher, D. Insertion angle impact on primary stability of orthodontic mini-implants. Angle Orthod. 2008, 78, 1065–1070. [Google Scholar] [CrossRef]
- Pithon, M.M.; Nojima, M.G.; Nojima, L.I. Primary stability of orthodontic mini-implants inserted into maxilla and mandible of swine. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2012, 113, 748–754. [Google Scholar] [CrossRef]
- Mohammed, H.; Wafaie, K.; Rizk, M.Z.; Almuzian, M.; Sosly, R.; Bearn, D.R. Role of anatomical sites and correlated risk factors on the survival of orthodontic miniscrew implants: A systematic review and meta-analysis. Prog. Orthod. 2018, 19, 36. [Google Scholar] [CrossRef]
- Moldoveanu, A.; Nicolescu, M.I.; Bucur, M.V.; Moldoveanu, G.G.; Funieru, C.; Neagoe, I.V.; Manda, G.; Ioana, T.R.; Ciocan, L.T. In vitro study of the orthodontic mini-implants influence on the growth of human osteoblasts. Rom. J. Morphol. Embryol. 2021, 62, 785–792. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ioana, T.R.; Boeru, F.G.; Antoniac, I.; Mitruț, I.; Staicu, I.E.; Rauten, A.M.; Uriciuc, W.A.; Manolea, H.O. Surface Analysis of Orthodontic Mini-Implants after Their Clinical Use. J. Funct. Biomater. 2024, 15, 244. [Google Scholar] [CrossRef]
- Stasiak, M.; Adamska, P. Should Cone-Beam Computed Tomography Be Performed Prior to Orthodontic Miniscrew Placement in the Infrazygomatic Crest Area?-A Systematic Review. Biomedicines 2023, 11, 2389. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sharan, J.; Bajoria, A.; Jena, A.K.; Sinha, P.; Shivakumar, A.; Kamal, V.K.; Marya, A. Assessment of Bone Thickness at the Infra Zygomatic Crest Region for Various Orthodontic Miniscrew Implant (OMSI) Insertion Angles: A Cone-Beam Computed Tomographic Study. Turk. J. Orthod. 2024, 37, 104–111. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Watanabe, K.; Mitchell, B.; Sakamaki, T.; Hirai, Y.; Kim, D.G.; Deguchi, T.; Suzuki, M.; Ueda, K.; Tanaka, E. Mechanical stability of orthodontic miniscrew depends on a thread shape. J. Dent. Sci. 2022, 17, 1244–1252. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Walter, A.; de la Iglesia, F.; Winsauer, H.; Ploder, O.; Wendl, B.; Puigdollers Perez, A. Evaluation of expansion forces of five pure bone-borne maxillary expander designs anchored with orthodontic mini-implants: An in vitro study. J. Orthod. 2023, 50, 335–343. [Google Scholar] [CrossRef] [PubMed]
- Labunet, A.; Iosif, C.; Kui, A.; Vigu, A.; Sava, S. Miniscrew-Assisted Rapid Palatal Expansion: A Scoping Review of Influencing Factors, Side Effects, and Soft Tissue Alterations. Biomedicines 2024, 12, 2438. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Meira, T.M.; Tanaka, O.M.; Ronsani, M.M.; Maruo, I.T.; Guariza-Filho, O.; Camargo, E.S.; Maruo, H. Insertion torque, pull-out strength and cortical bone thickness in contact with orthodontic mini-implants at different insertion angles. Eur. J. Orthod. 2013, 35, 766–771. [Google Scholar] [CrossRef]
- Lee, N.-K.; Baek, S.-H. Effects of the diameter and shape of orthodontic mini-implants on microdamage to the cortical bone. Am. J. Orthod. Dentofac. Orthop. 2010, 138, 8.e1–8.e8. [Google Scholar] [CrossRef]
- Meursinge Reynders, R.; Ladu, L.; Ronchi, L.; Di Girolamo, N.; de Lange, J.; Roberts, N.; Plüddemann, A. Insertion torque recordings for the diagnosis of contact between orthodontic mini-implants and dental roots: A systematic review. Syst. Rev. 2016, 5, 50. [Google Scholar] [CrossRef]
- Singh, J.; Singh, S.K.; Gupta, A.R.; Nayak, S.C.; Vatsa, R.; Priyadarshni, P. Comparative evaluation of primary stability of two different types of orthodontic mini-implants. J. Pharm. Bioallied Sci. 2021, 13 (Suppl. 1), S128–S131. [Google Scholar] [CrossRef]
- Motoyoshi, M.; Hirabayashi, M.; Uemura, M.; Shimizu, N. Recommended placement torque when tightening an orthodontic mini-implant. Clin. Oral Implant. Res. 2006, 17, 109–114. [Google Scholar] [CrossRef]
- Heidemann, W.; Gerlach, K.L.; Grobel, K.; Kollner, H. Influence of different pilot hole sizes on torque measurements and pullout analysis of osteosynthesis screws. J. Craniomaxillofac. Surg. 1998, 26, 50–55. [Google Scholar] [CrossRef]
- Vilani, G.N.; Ruellas, A.C.; Elias, C.N.; Mattos, C.T. Stability of smooth and rough mini-implants: Clinical and biomechanical evaluation-an in vivostudy. Dent. Press. J. Orthod. 2015, 20, 35–42. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Barros, S.E.; Vanz, V.; Chiqueto, K.; Janson, G.; Ferreira, E. Mechanical strength of stainless steel and titanium alloy mini-implants with different diameters an experimental laboratory study. Prog. Orthod. 2021, 22, 9. [Google Scholar] [CrossRef]
- Scribante, A.; Montasser, M.A.; Radwan, E.S.; Bernardinelli, L.; Alcozer, R.; Gandini, P. Reliability of orthodontic miniscrews bending and maximum load of different Ti-6Al-4V titanium and stainless steel temporary anchorage devices (TADs). Materials 2018, 11, 1138. [Google Scholar] [CrossRef]
- Vieira, C.A.; Pires, F.; Hattori, W.T.; de Araújo, C.A.; Garcia-Junior, M.A.; Zanetta-Barbosa, D. Structural resistance of orthodontic mini-screws inserted for extra-alveolar anchorage. Acta Odontol. Latinoam. 2021, 34, 27–34. [Google Scholar] [CrossRef]
- Barros, S.E.; Janson, G.; Chiqueto, K.; Garib, D.G.; Janson, M. Effect of mini-implant diameter on fracture risk and self-drilling efficacy. Am. J. Orthod. Dentofac. Orthop. 2011, 140, e181–e192. [Google Scholar] [CrossRef]
- Wilmes, B.; Panayotidis, A.; Drescher, D. Fracture resistance of orthodontic mini-implants: A biomechanical in vitro study. Eur. J. Orthod. 2011, 33, 396–401. [Google Scholar] [CrossRef]
- Copello, F.M.; Brunetto, D.P.; Elias, C.N.; Pithon, M.M.; Coqueiro, R.S.; Castro, A.C.R.; Sant’anna, E.F. Miniscrew-assisted rapid palatal expansion (MARPE): How to achieve greater stability. In vitro study. Dent. Press. J. Orthod. 2021, 26, e211967. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Morarend, C.; Qian, F.; Marshall, S.D.; Southard, K.A.; Grosland, N.M.; Morgan, T.A.; McManus, M.; Southard, T.E. Effect of screw diameter on orthodontic skeletal anchorage. Am. J. Orthod. Dentofac. Orthop. 2009, 136, 224–229. [Google Scholar] [CrossRef] [PubMed]
- Huja, S.S.; Litsky, A.S.; Beck, F.M.; Johnson, K.A.; Larsen, P.E. Pull-out strength of monocortical screws placed in the maxillae and mandibles of dogs. Am. J. Orthod. Dentofac. Orthop. 2005, 127, 307–313. [Google Scholar] [CrossRef]
- Duaibis, R.; Kusnoto, B.; Natarajan, R.; Zhao, L.; Evans, C. Factors affecting stresses in cortical bone around miniscrew implants: A three-dimensional finite element study. Angle Orthod. 2012, 82, 875–880. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Adell, R.; Lekholm, U.; Rockler, B.; Branemark, P.A. 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int. J. Oral Surg. 1981, 6, 387–416. [Google Scholar] [CrossRef]
- Albrektsson, T.; Zarb, G.; Worthington, D.; Erikson, R. The long-term efficacy of current dental implants. A review and proposed criteria for success. Int. J. Oral Maxillofac. Implant. 1986, 1, 11–25. [Google Scholar]
- Miyawaki, S.; Koyama, I.; Inoue, M.; Mishima, K.; Sugahara, T.; Takano-Yamamoto, T. Factors associated with the stability of tita niumscrewsplaced in the posterior region for orthodontic anchor age. Am. J. Orthod. Dentofac. Orthop. 2003, 124, 373–378. [Google Scholar] [CrossRef]
- Özkan, S.; Büyük, S.K.; Gök, F.; Benkli, Y.A. Evaluation of reused orthodontic mini-implants on stability: An in-vivo study. Am. J. Orthod. Dentofac. Orthop. 2022, 162, 689–694. [Google Scholar] [CrossRef]
- McManus, M.M.; Qian, F.; Grosland, N.M.; Marshall, S.D.; Southard, T.E. Effect of miniscrew placement torque on resistance to miniscrew movement under load. Am. J. Orthod. Dentofac. Orthop. 2011, 140, e93–e98. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, R.; Wadhwani, C.P.K.; Rosen, P.S.; Chung, K.H. Validating implant torque limiting devices with a custom tool: A dental technique. J. Prosthet. Dent. 2021, 125, 407–410. [Google Scholar] [CrossRef] [PubMed]
- Skvirsky, Y.; Giladi, H.Z.; Rizzante, F.A.P.; Teich, S.T.; Gutmacher, Z. Measurements of trueness and precision of various dental torque wrenches: An in vitro study. J. Prosthet. Dent. 2025; In Press. [Google Scholar] [CrossRef] [PubMed]
- Wadhwani, C.P.K.; O’Brien, R.; Rosen, P.S.; Chung, K.H. Testing and calibrating the mechanical-type toggle torque wrenches used in implant dentistry: A dental technique. J. Prosthet. Dent. 2020, 123, 403–407. [Google Scholar] [CrossRef]





| Feature | Jeil S20-JD-010 | Osstem OSSH1810 | Leone 003-2009-10 |
|---|---|---|---|
| Diameter | 2.0 mm | 1.8 mm | 2.0 mm |
| Length | 10 mm | 10 mm | 9 mm |
| Thread Design | Fine-pitch threads with self-tapping flutes; cylindrical-tapered transition | Corkscrew-style dual-thread (wider lower + finer upper) | Cylindrical self-tapping coil; thread ~1.75 mm |
| Implant Tip Geometry | Sharp, conical self-drilling tip with cutting edge and flutes | Sharp, self-drilling apical tip; likely conical | Sharp fluted drill-tip, 2 mm long; self-drilling |
| Material | Ti-6Al-4V (Grade 5 Titanium) | Ti-6Al-4V (Grade 5 Titanium) | Ti-6Al-4V (Grade 5 Titanium) |
| Insertion Technique | Self-drilling or predrilling (optional, for dense bone) | Self-drilling (predrilling may be needed in dense bone | Self-drilling (predrilling optional in dense bone) |
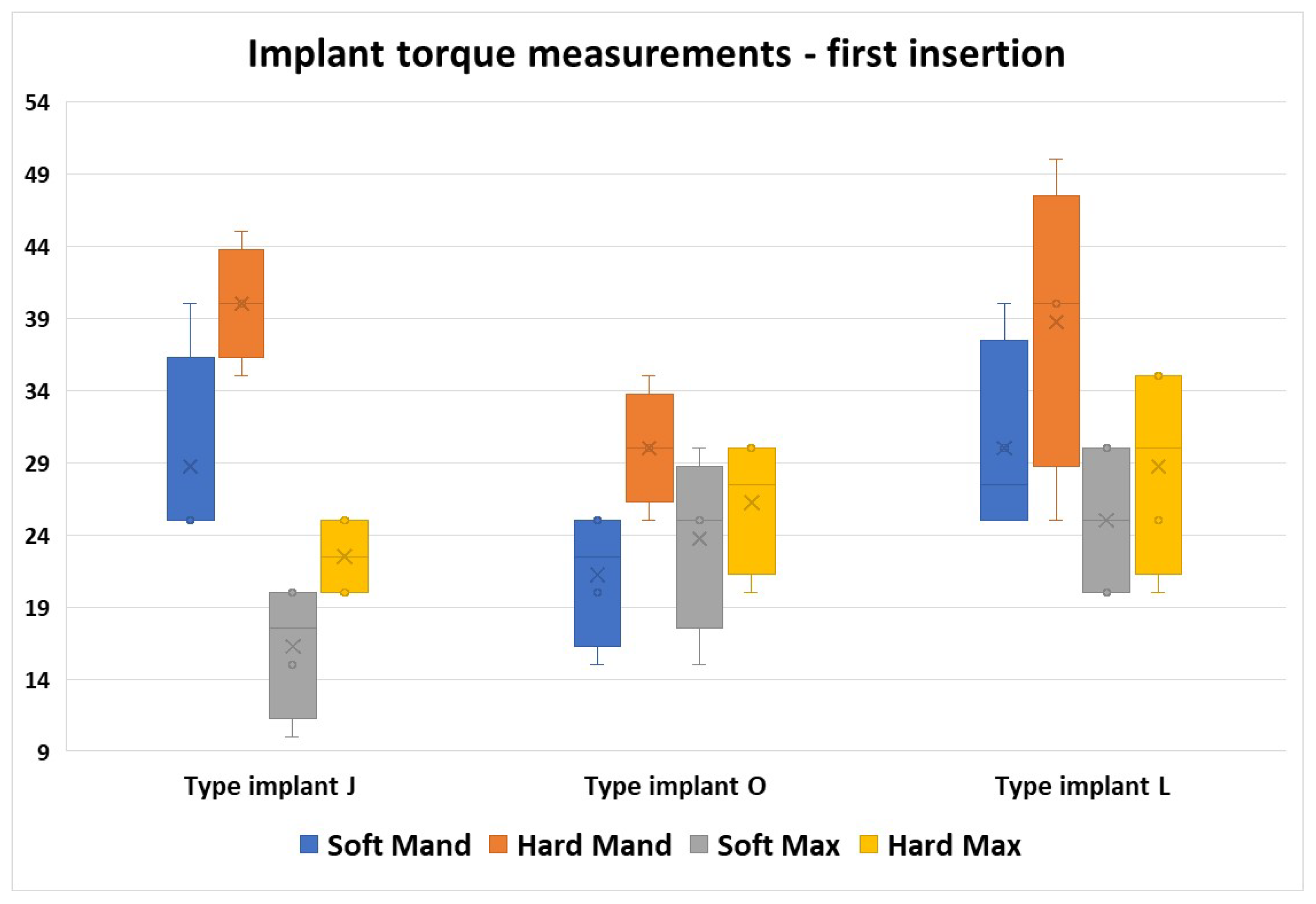
| Zone | Parameter | Torque Values (N/cm2) | ||
|---|---|---|---|---|
| Implant Type J | Implant Type O | Implant Type L | ||
| Soft Mand | Minimum | 20 | 15 | 20 |
| Maximum | 40 | 30 | 40 | |
| Median | 27.50 | 25.00 | 27.50 | |
| Variance | 35.268 | 24.554 | 57.143 | |
| Confidence interval—lower bound | 23.16 | 20.23 | 23.68 | |
| Confidence interval—upper bound | 33.09 | 28.52 | 36.32 | |
| Hard Mand | Minimum | 30 | 25 | 25 |
| Maximum | 50 | 40 | 50 | |
| Median | 40.00 | 32.50 | 40.00 | |
| Variance | 42.857 | 28.125 | 92.857 | |
| Confidence interval—lower bound | 34.53 | 28.69 | 31.94 | |
| Confidence interval—upper bound | 45.47 | 37.56 | 48.06 | |
| Soft Max | Minimum | 10 | 15 | 20 |
| Maximum | 20 | 30 | 45 | |
| Median | 15.00 | 25.00 | 25.00 | |
| Variance | 12.500 | 38.839 | 99.554 | |
| Confidence interval—lower bound | 13.29 | 19.16 | 19.78 | |
| Confidence interval—upper bound | 19.21 | 29.59 | 36.47 | |
| Hard Max | Minimum | 20 | 20 | 20 |
| Maximum | 45 | 40 | 45 | |
| Median | 25.00 | 27.50 | 30.00 | |
| Variance | 113.839 | 70.982 | 105.357 | |
| Confidence interval—lower bound | 19.21 | 21.08 | 22.67 | |
| Confidence interval—upper bound | 37.04 | 35.17 | 39.83 | |
| Area | Implant Type (Median Values) | p * | ||
|---|---|---|---|---|
| Type J | Type O | Type L | ||
| Soft Mand | 27.5 | 25 | 27.5 | 0.318 |
| Hard Mand | 40 | 32.5 | 40 | 0.127 |
| Soft Max | 15 | 25 | 25 | 0.009 # |
| Hard Max | 25 | 27.5 | 30 | 0.749 |
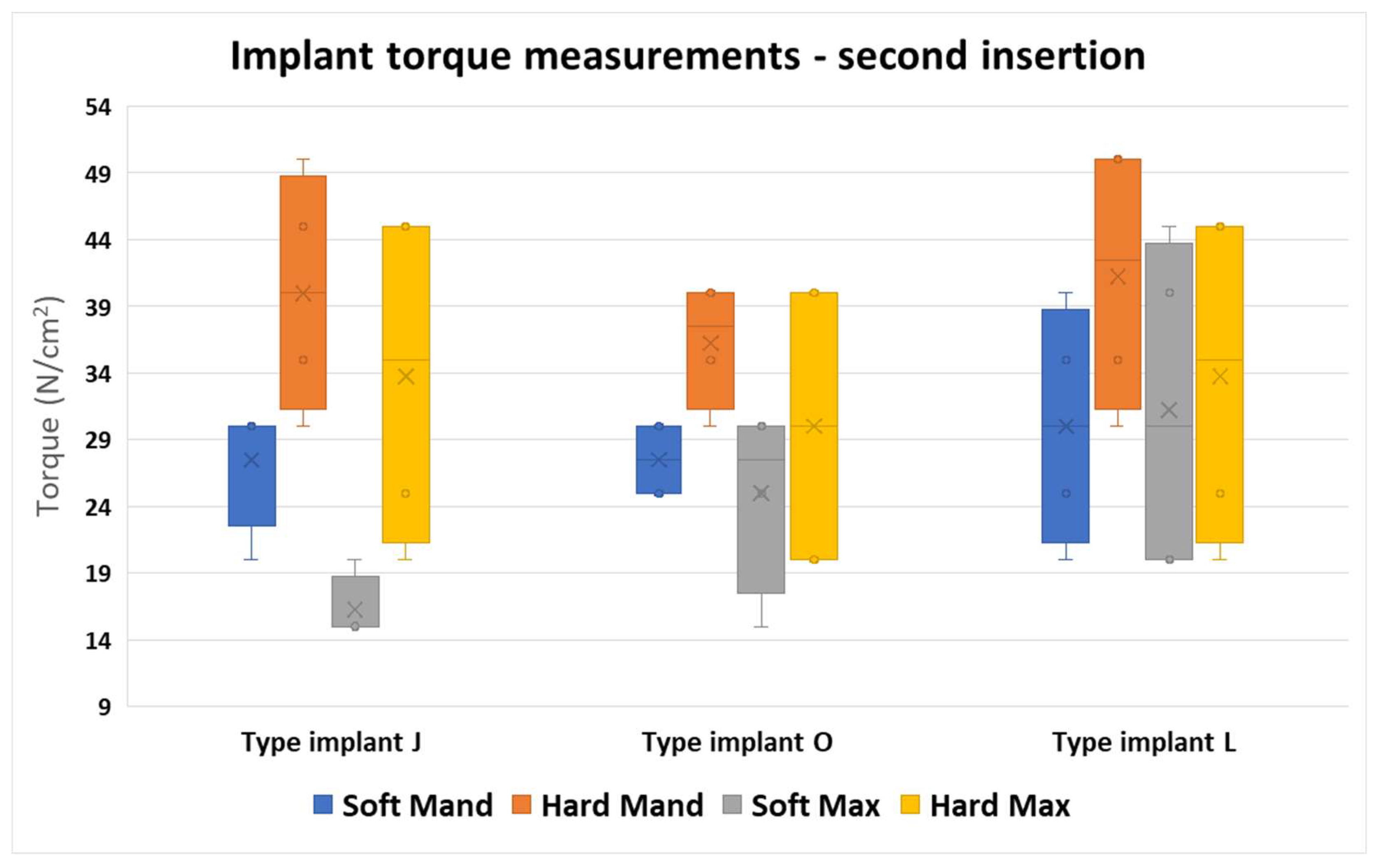
| Area | Implant Type J | p * | |
|---|---|---|---|
| J1 Insertion | J2 Insertion | ||
| Soft Mand | 25 | 30 | 1.000 |
| Hard Mand | 40 | 40 | 1.000 |
| Soft Max | 17.5 | 15 | 0.886 |
| Hard Max | 22.5 | 35 | 0.343 |
| Area | Implant Type O | p * | |
|---|---|---|---|
| O1 Insertion | O2 Insertion | ||
| Soft Mand | 22.5 | 27.5 | 0.114 |
| Hard Mand | 30 | 37.5 | 0.114 |
| Soft Max | 25 | 27.5 | 0.686 |
| Hard Max | 27.5 | 30 | 1.000 |
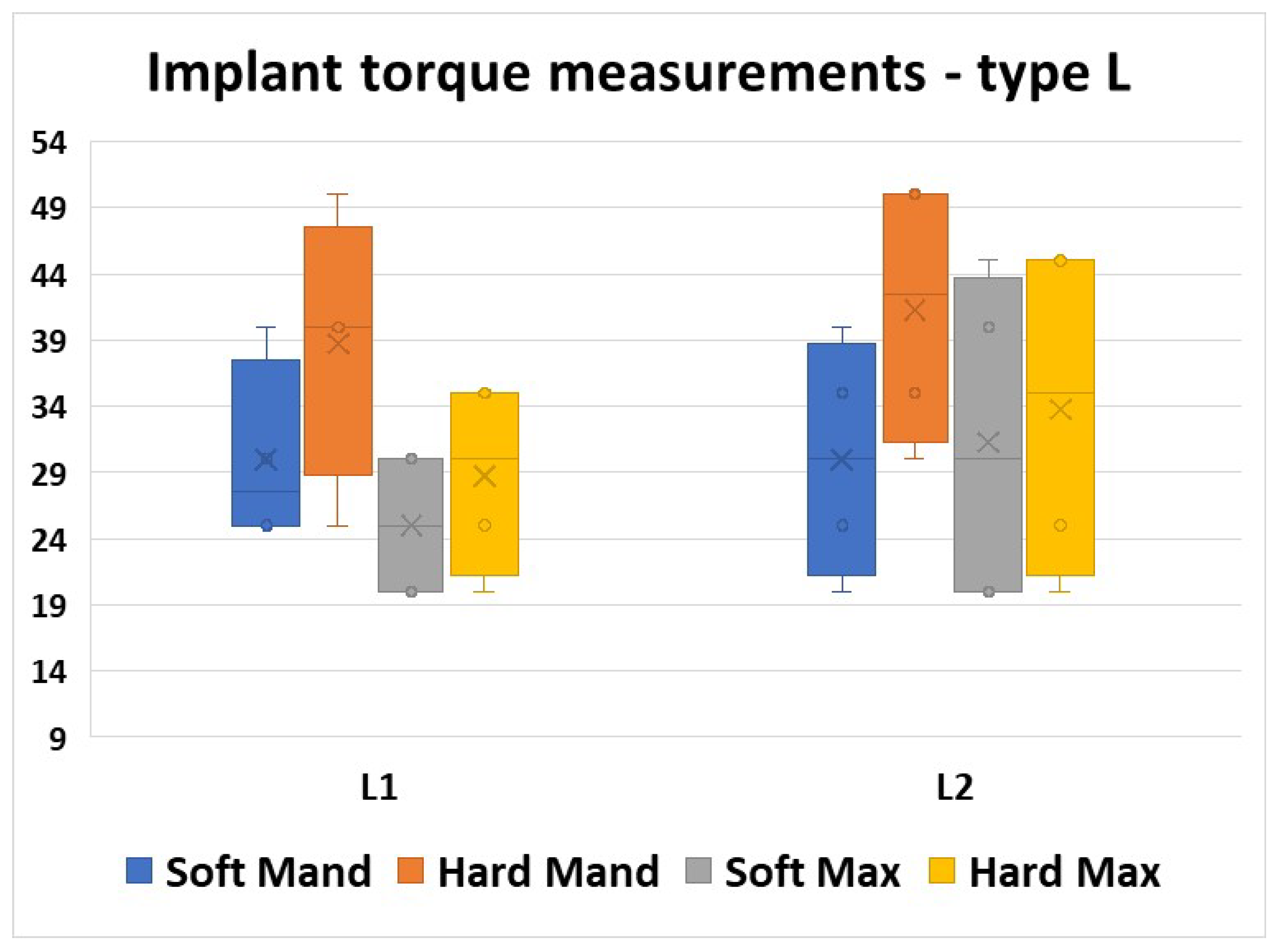
| Area | Implant Type L | p * | |
|---|---|---|---|
| L1 Insertion | L2 Insertion | ||
| Soft Mand | 27.5 | 30 | 0.886 |
| Hard Mand | 40 | 42.5 | 1.000 |
| Soft Max | 25 | 30 | 0.686 |
| Hard Max | 30 | 35 | 0.686 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ioana, T.R.; Boeru, F.G.; Mitruț, I.; Rauten, A.-M.; Elsaafin, M.; Ionescu, M.; Staicu, I.E.; Manolea, H.O. Analysis of Insertion Torque of Orthodontic Mini-Implants Depending on the System and the Morphological Substrate. J. Funct. Biomater. 2025, 16, 291. https://doi.org/10.3390/jfb16080291
Ioana TR, Boeru FG, Mitruț I, Rauten A-M, Elsaafin M, Ionescu M, Staicu IE, Manolea HO. Analysis of Insertion Torque of Orthodontic Mini-Implants Depending on the System and the Morphological Substrate. Journal of Functional Biomaterials. 2025; 16(8):291. https://doi.org/10.3390/jfb16080291
Chicago/Turabian StyleIoana, Tamara Rahela, Filip George Boeru, Ioana Mitruț, Anne-Marie Rauten, Mahmoud Elsaafin, Mihaela Ionescu, Ionela Elisabeta Staicu, and Horia Octavian Manolea. 2025. "Analysis of Insertion Torque of Orthodontic Mini-Implants Depending on the System and the Morphological Substrate" Journal of Functional Biomaterials 16, no. 8: 291. https://doi.org/10.3390/jfb16080291
APA StyleIoana, T. R., Boeru, F. G., Mitruț, I., Rauten, A.-M., Elsaafin, M., Ionescu, M., Staicu, I. E., & Manolea, H. O. (2025). Analysis of Insertion Torque of Orthodontic Mini-Implants Depending on the System and the Morphological Substrate. Journal of Functional Biomaterials, 16(8), 291. https://doi.org/10.3390/jfb16080291







