1. Introduction
Light-curing resin-based composites are among the most popular dental filling materials today. They meet high aesthetic demands and enable a seamless reconstruction of tooth structure in terms of color and, even more importantly and more difficult to mimic, translucency. Further advantages underline their choice in dentistry, as they can be used for minimally invasive dentistry, preserving healthy tooth structures and allowing them to be re-polished or repaired, if necessary, without having to replace the entire restoration. These characteristics are added to high survival rates of composite restorations, approaching 90% in a decade of clinical service [
1,
2].
The development toward the current high standard and level of maturity was only possible through understanding the relationship between material composition, microstructure, and clinical behavior—a process that is ongoing [
1]. Many innovations from other industries have been implemented in dental materials in recent decades, from the introduction of nanotechnology [
3] for fillers to new polymerization mechanisms of the organic polymer matrix [
4] to intrinsic coloration, which is intended to allow unlimited color adaptation of the material to its environment [
5] or bioactivity to prevent the development of secondary caries [
6].
The balance between aesthetics and mechanical stability is particularly important for materials used in areas of high mechanical stress, such as posterior restorations [
7]. Although there are some guidelines that specify the requirements for a composite for such restorations, for example, a flexural strength of at least 80 MPa [
8], there are no clearly defined values for the material properties that can guarantee the long-term clinical longevity of the restoration. For dental materials scientists, it is therefore clear that there is a significant need to establish and define a threshold for appropriate mechanical behavior to help clinicians select an appropriate restorative strategy. While it must be acknowledged that considerable effort has been made to identify these characteristics and define their thresholds, the correlation between laboratory-measured parameters and clinical behavior has been considered moderate to low in most studies to date [
9]. The current accepted opinion, supported by studies, is that there is not a single or even a few parameters that can define the clinical behavior but rather a whole series of parameters. Among these, flexural strength and modulus of elasticity [
9,
10] as well as fracture toughness [
7,
10] are considered the most important properties for material selection, given that the main reasons for the clinical failure of light-cured composite restorations in the posterior region in recent decades has been bulk fractures, which are responsible for about 70% of filling replacement [
2]. In addition, marginal breakdown and clinical fracture are rather related to fracture toughness [
10], while clinical wear was mainly connected to the flexural strength [
9,
10]. Although there is little confirmatory evidence, it is believed that clinical fractures and wear are related to fatigue resistance [
10].
The trend toward increased fractures in posterior composite restorations has even intensified in recent decades [
1,
2]. This is related to increasingly smaller filler sizes and amounts, which impair the mechanical properties of the material, but also to changes in the clinical indication for composite fillings. The clinical success of posterior composite restorations has made practitioners increasingly confident in gradually expanding the indication to include larger, more complex, and multi-surface cavities that are more prone to tooth and restoration fractures [
1,
2]. Additional factors such as type and location of the restoration, patient age, caries prevalence, bruxism, socioeconomic factors and also the quality and technique of the dentist are being explicitly evaluated and quantified in order to better focus all these effects on their cause and not to distort the effect of the material on the clinical behavior of the material [
11].
The comparison of composites tested under different loading conditions in the laboratory aims to simulate the load to which a filling in the oral cavity is subjected [
9]. In this context, parameters such as flexural strength, which includes both tensile and compressive stresses during testing, are very frequently determined and are well standardized [
8]. Although the flexural strength is measured on a precisely defined sample geometry and under precisely defined conditions to enable reproducible values, the result is valid only for the predefined shape, volume, and geometry of the sample as well as for the test conditions. This calls into question the direct transfer of the results to a dental restoration, whose size and shape vary greatly. More valuable would therefore be parameters that represent intrinsic material properties, i.e., properties that are inherent in a material and do not depend on the factors listed above. An example, therefore, is fracture toughness, which quantifies the ability of the material to resist crack propagation under applied stress. Originating from other industries, various methods to measure fracture toughness have also been introduced for dental materials [
12]. The most common are the single-edge notch, compact tensile, double torsion, and short-rod tests [
13]. Most of these methods require large sample sizes and are therefore expensive for dental materials. Furthermore, they rely on the application of a sharp pre-crack to initiate fracture, which is complex to implement, technique-sensitive, and prone to error [
13].
Based on the above listed reasons, the choice in this study was made on determining fracture toughness by the notch-free triangular prism test (NTP), in which the complex and error-prone pre-crack implementation is no longer necessary. The NTP-test was previously validated for different materials and proved consistent in its outcome with other established tests [
14]. Given that flexural strength measurement is the most commonly used method to assess the mechanical properties of composite materials, the idea arose to further exploit these data and complement them with a fractography study. The latter allows the investigation of characteristic fracture features, which can then be quantitatively interpreted to determine fracture toughness as described in Orr theory [
15]. In this way, a test that is essentially size-dependent, such as the flexural strength test, should allow the determination of an intrinsic material parameter such as fracture toughness. The aim of the study is therefore to apply principles of fractography and fracture mechanics to the results of a three-point bending test to determine an intrinsic material parameter, the mirror constant, and to verify its correlation with fracture toughness.
Based on the rationale outlined above, two research questions are identified:
The null hypothesis tested was that after examining a variety of modern dental composites, the fracture toughness determined by quantitative fractography is similar to the outcome of the NTP test.
4. Discussion
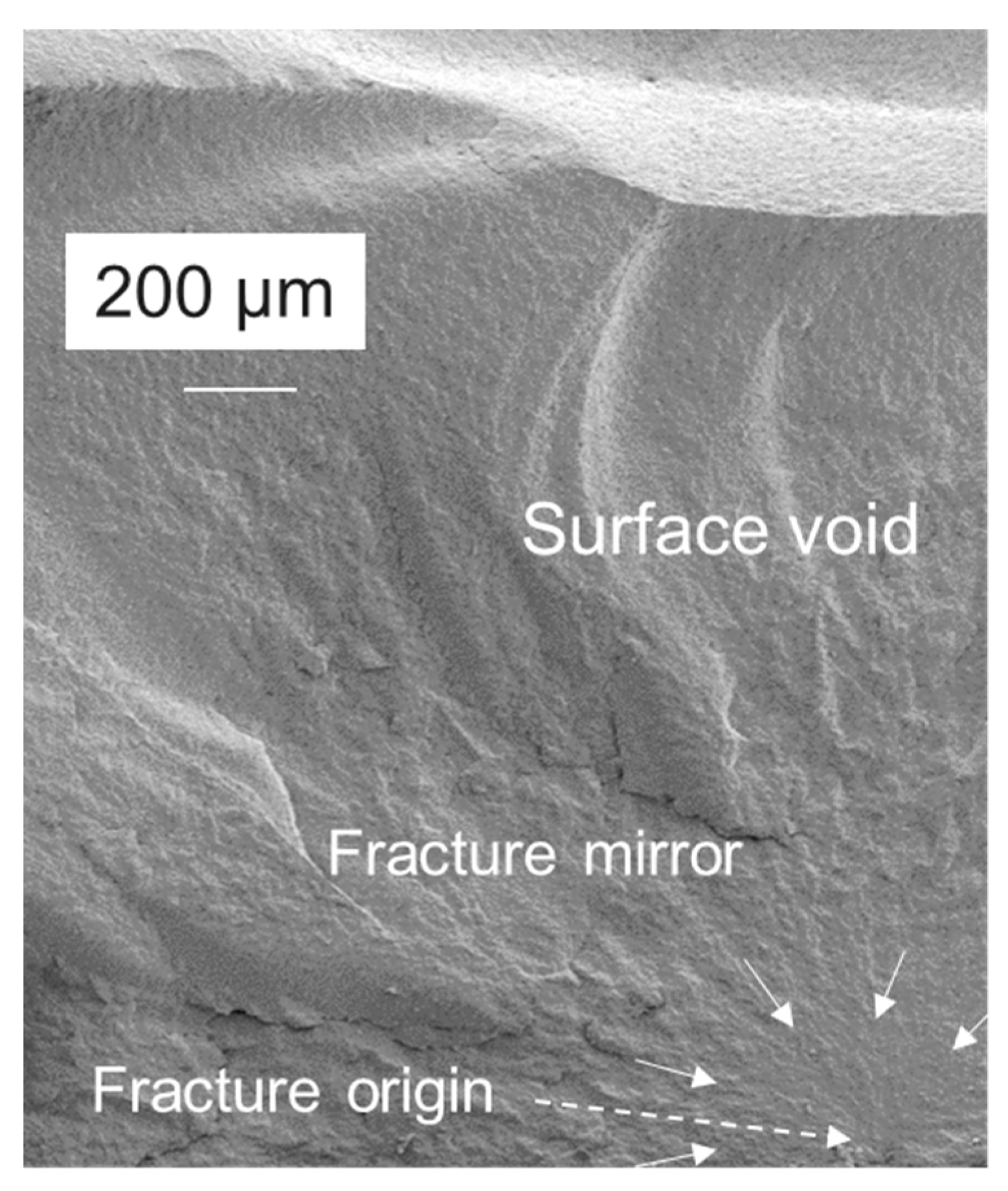
Intrinsic material properties are of great importance when it comes to translating laboratory measurements into the clinical behavior of a material placed in cavities of different sizes and geometries. Because dental composites are highly filled polymers, they exhibit pronounced brittle behavior. This was clearly evident in the present study in their fracture surfaces that allow the delineation of the fracture mirror, the smooth radial region surrounding the critical flaw that initiated fracture [
17]; the subsequent mist region formed by secondary cracks that fail to propagate due to decreasing energy [
18] as the crack velocity increases [
19]; and finally the transition into the region of larger radial ridges, the hackle lines with macroscopic crack branching [
20]. While these characteristic patterns depend on a variety of parameters, including the size and shape of the critical flaw [
19] or additional flaws encountered during crack propagation [
21], the critical flaw in the analyzed materials is always located on the tensile side of the specimen loaded in the 3-point bending test, and the fracture propagates toward the neutral axis, leaving a somewhat elongated mirror with an often flared, incomplete shape [
17] (
Figure 6). In this context, the fracture mirror draws attention to the origin of the fracture, indicating that internal voids and defects, rather than surface defects, were the cause of failure. Volume defects amounted to 80.4%, with many of the surface defects being originally internal voids that were opened during sample grinding. Grinding was deliberately chosen because it not only allows the removal of bulges, protrusions, and other defects that occurred during sample preparation but also corresponds to the clinically procedure for completing a composite restoration.
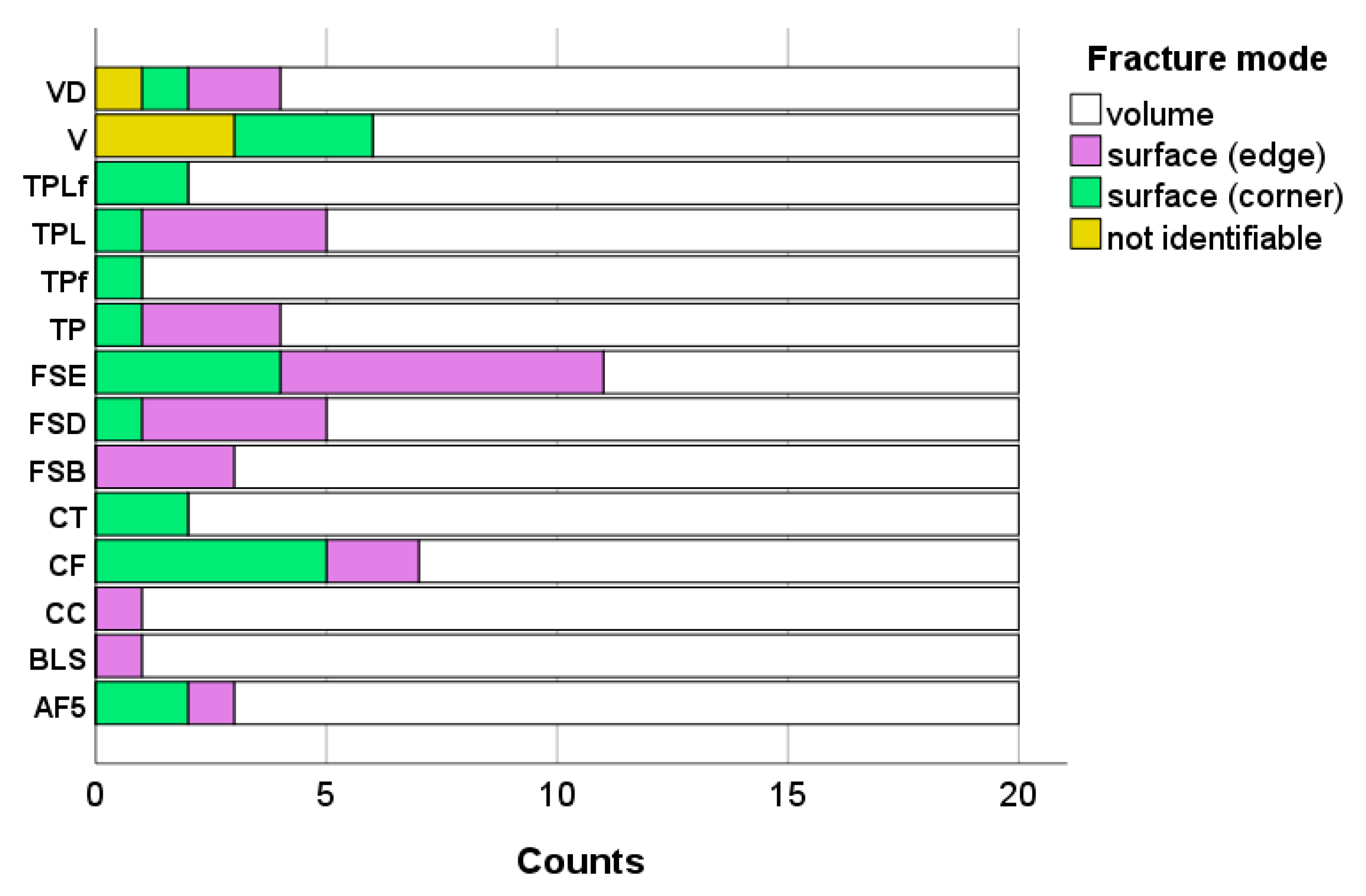
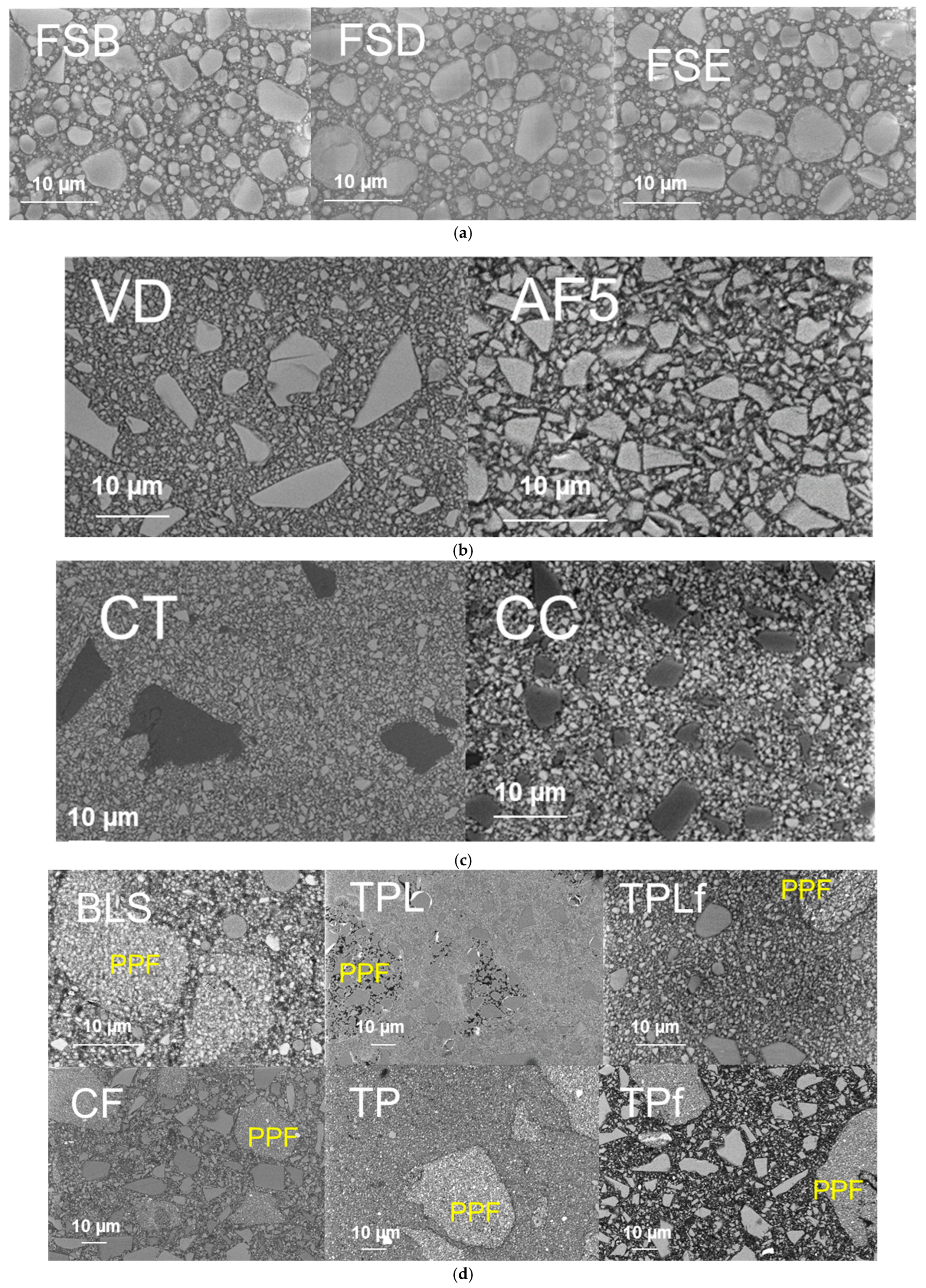
The incorporation of fillers into the monomer system to create a composite carries the risk of the formation of microdefects such as agglomerates or voids, which can trigger fractures. Voids may already be present in the unpolymerized composite paste but may also have arisen during compaction of the composite paste for sample preparation. On the other hand, surface treatment is sensitive to the material’s microstructure, so the occurrence of surface defects may in fact be related to filler size and inherent material roughness. Another aspect to consider is the quality of silanization, since fillers that are weakly embedded in the polymer matrix, as well as pre-polymer fillers, which are known to have a weaker bond to the organic matrix than compact fillers, can easily be pulled out during grinding, leaving a defect large enough to initiate fracture. The 14 composites analyzed illustrate the great diversity of dental composite microstructure. However, their fracture mode distribution, summarized in
Figure 5, does not allow a clear assignment of surface defects to the aforementioned aspects. Larger filler sizes or materials with pre-polymerized fillers do not appear to exhibit increased surface defects, which again demonstrates that various effects operate simultaneously in such complex materials.
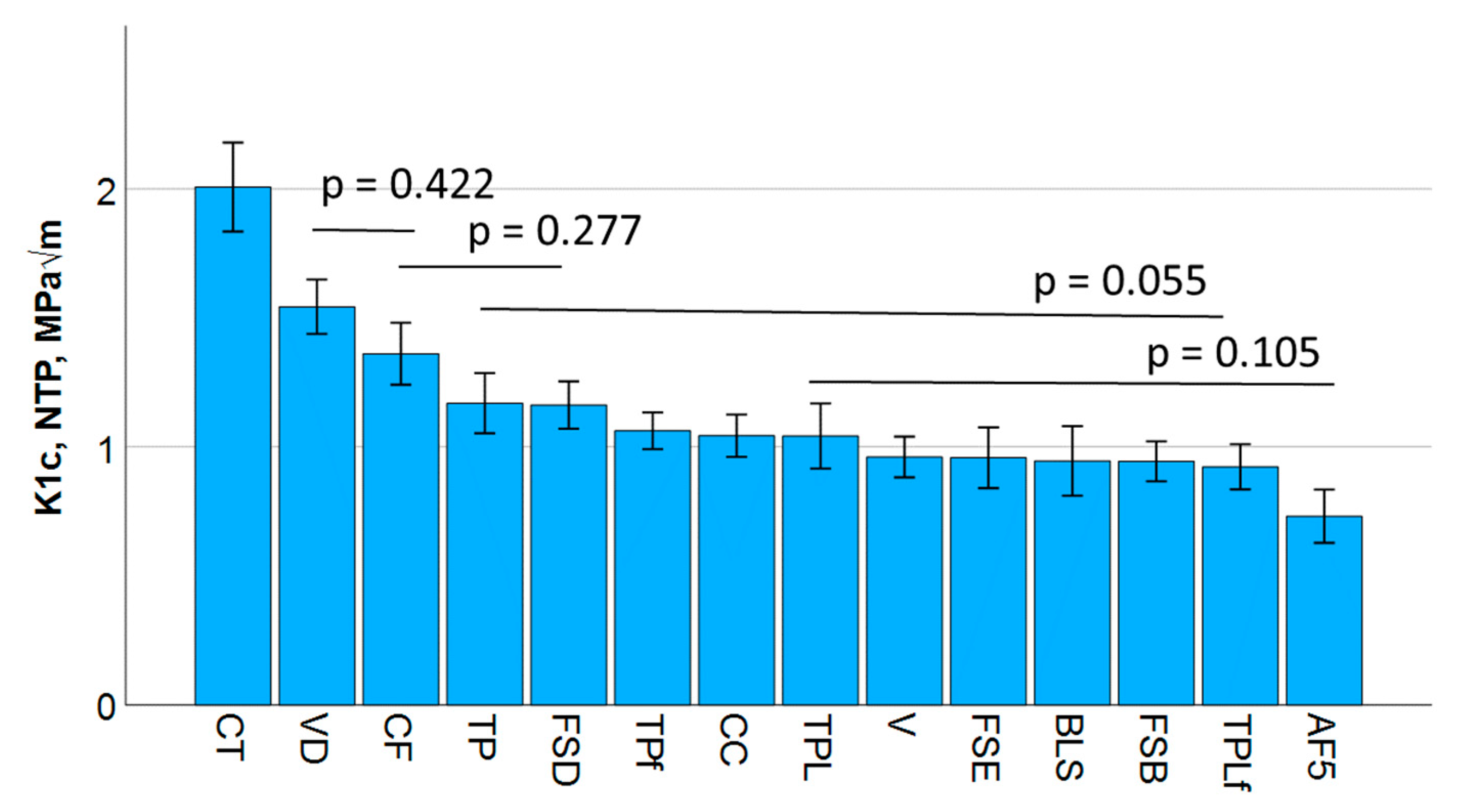
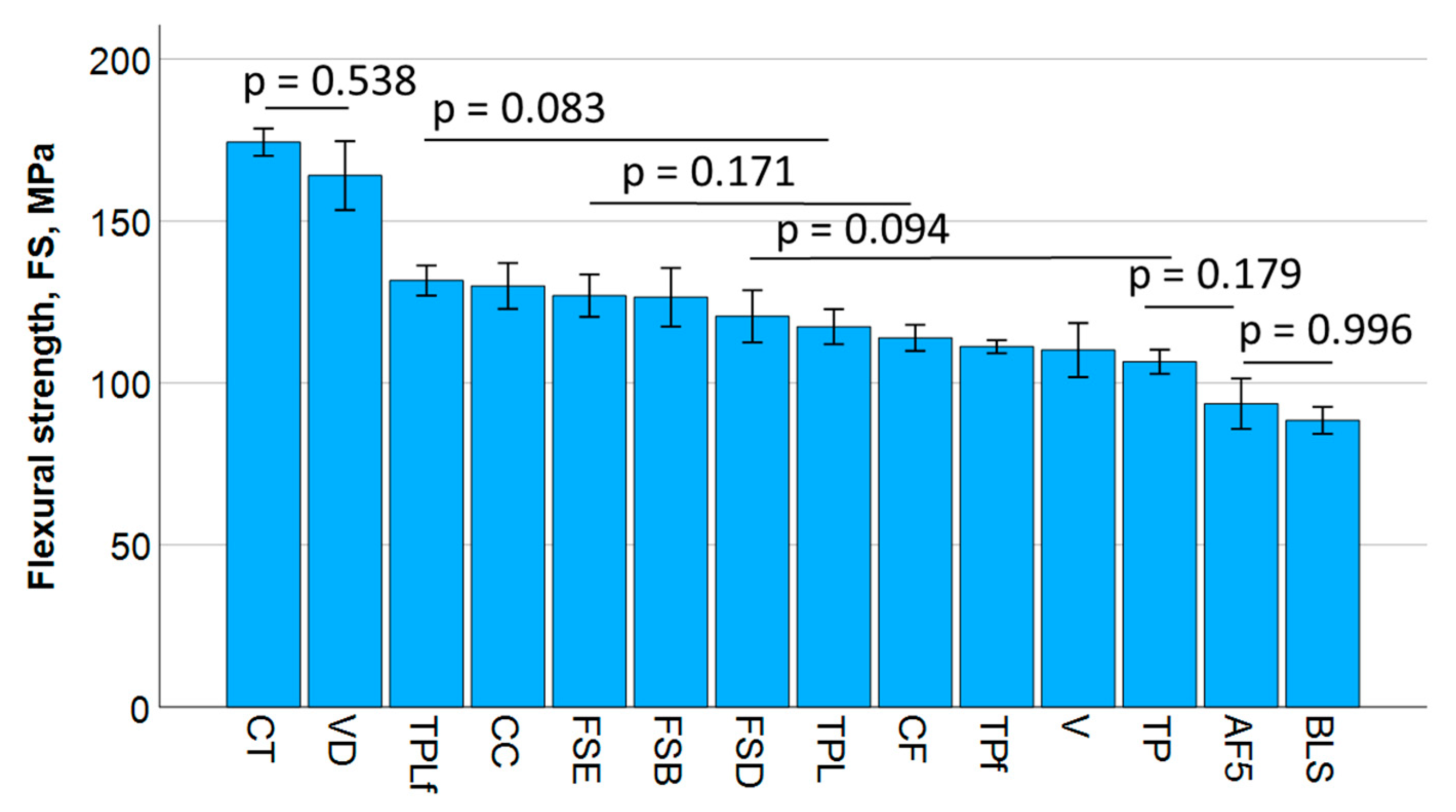
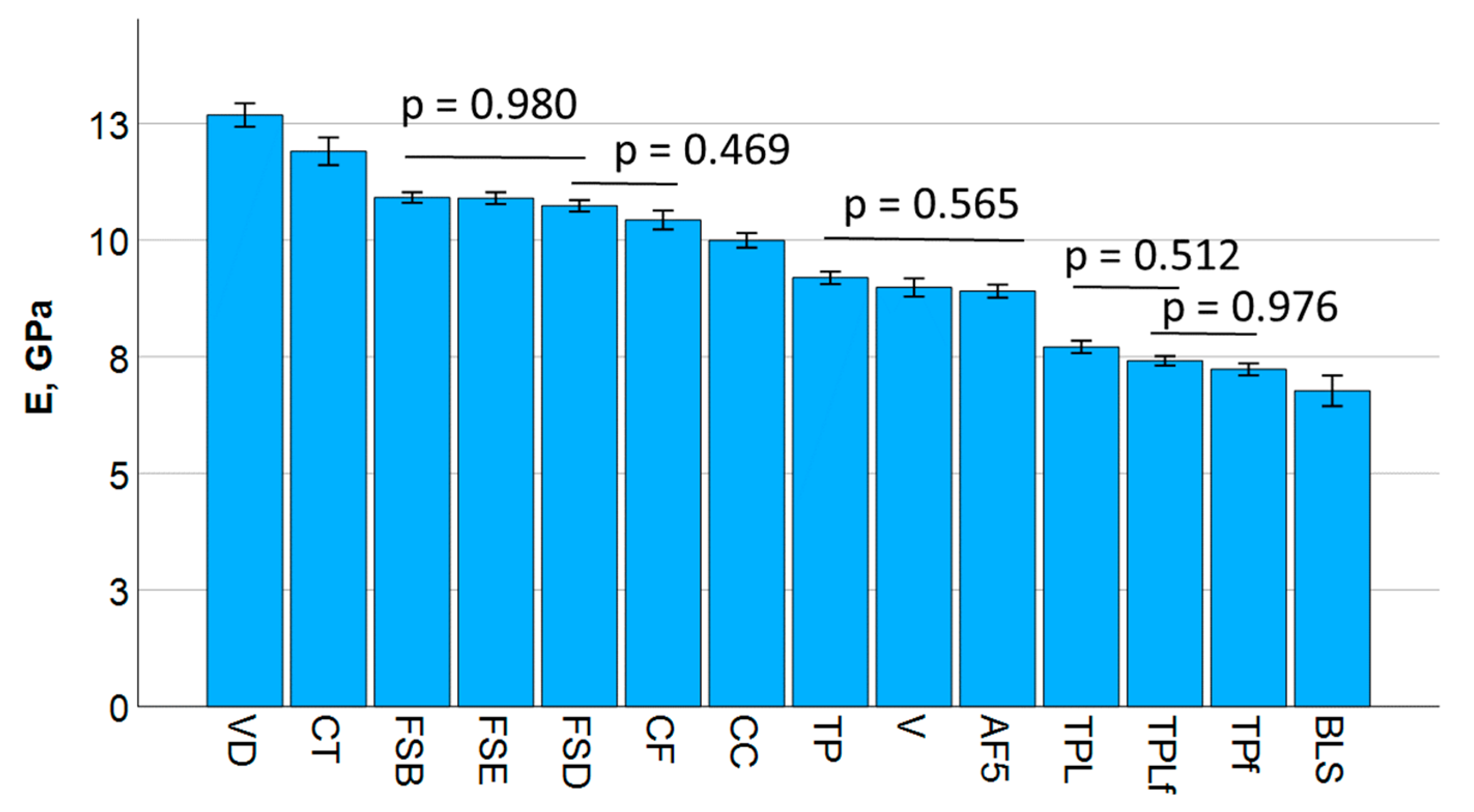
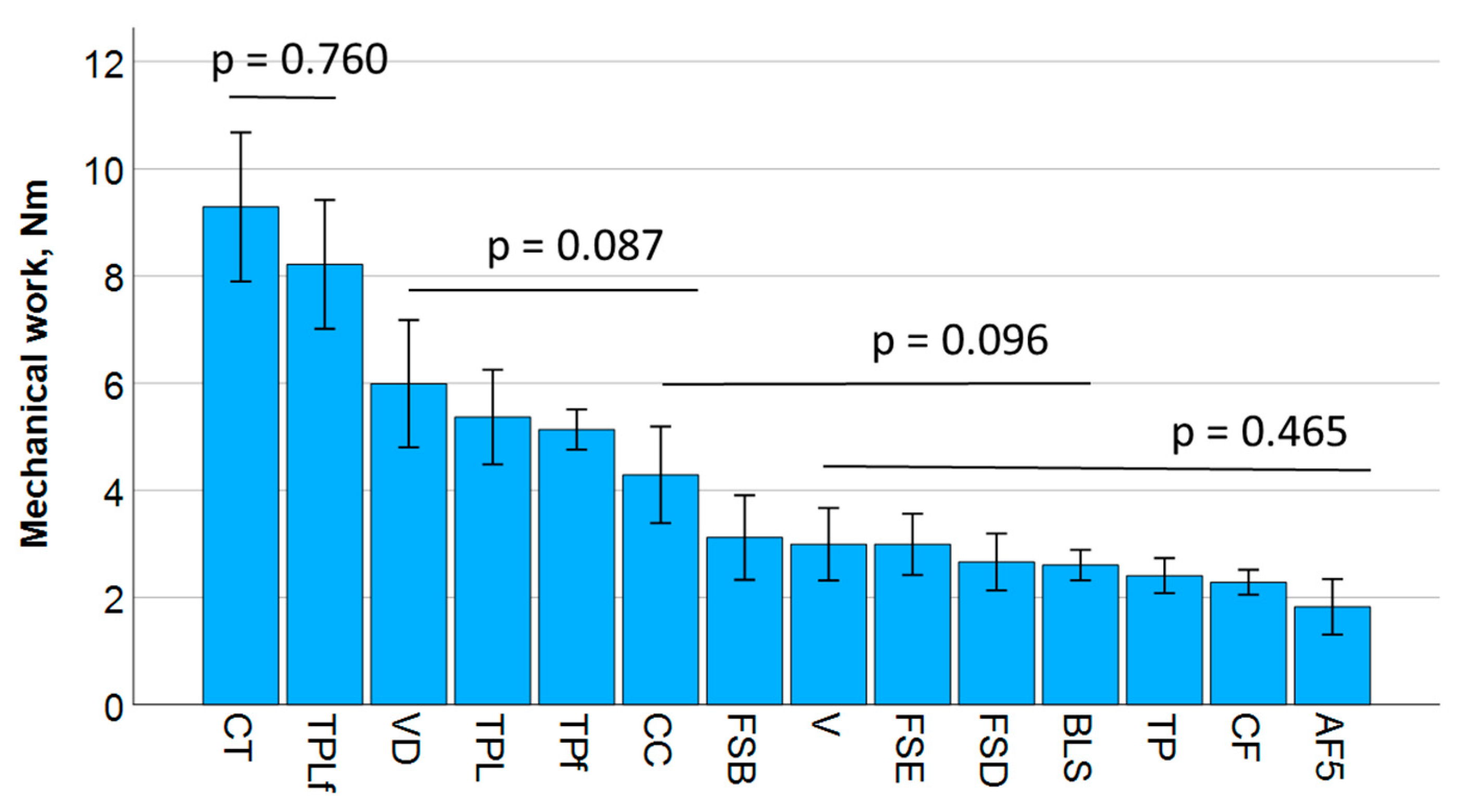
The flexural strength data for all materials significantly exceeded the ISO standard requirement of 80 MPa. This fact can distort the right decision for a material, as particularly for flowable, low-filled materials, the high polymer content leads to greater beam deflection during testing, resulting in a longer failure time and increased flexural strength. In contrast, the elastic modulus is directly related to the proportion of inorganic fillers, placing the tested low-filled flowable materials significantly at the bottom of the rankings. In addition, for materials with pre-polymer fillers, the total filler quantity indicated does not correspond to the quantity of inorganic filler, since this also includes the polymer phase of the filler, which has a lesser impact on the elastic modulus. Therefore, when selecting a suitable material, flexural strength data must always be accompanied by elastic modulus data. There is currently no threshold value for the modulus of elasticity when selecting materials for posterior restorations. However, in order to withstand elastic deformation, a high modulus should be chosen. Other factors such as size, shape, distribution, and the nature of the filler’s bond to the organic matrix may act antagonistically on the mechanical parameters. Filler size is particularly important for the primary dependence of mechanical properties such as wear [
22,
23]. In contrast, the filler shape influences flexural strength and elastic modulus, with irregular fillers exercising a positive effect compared to spherical fillers at a given volume fraction [
24]. The incorporation of fillers into a polymer matrix also hinders the formation, growth, and propagation of cracks or requires more energy for this resulting in higher fracture toughness values. The material VD tested in the present study was the composite with the highest filler content in both weight and volume percent, which was indeed clearly reflected in the highest elastic modulus. Due to the direct relationship between elastic modulus and fracture toughness, the highest fracture toughness would be expected for VD, but CT exceeded it. This behavior needs to be related to two other aspects: the smaller filler size in the CT, which allows for a consistently higher filler–matrix interface, thus favoring crack deviation and energy dissipation, and the incorporation of pre-polymerized fillers, even if only in a small proportion of 1%. These pre-polymerized fillers offer additional opportunities to increase fracture toughness, as the bond of the pre-polymerized filler to the matrix is weaker compared to compact fillers, which can lead to blunting of the crack tip and thus a delay in crack growth. The detachment of such regions can also delay crack growth and dissipate energy due to the reduced driving force at the crack tip.
The fracture mirror not only allows the identification of the fracture origin but also provides information about the magnitude and distribution of the stresses that caused the fracture [
12]. One century ago, it was empirically observed that the smaller the fracture mirror, the greater the stress at the point of origin. Conversely, larger mirrors indicate lower fracture stress and a large defect that initiated fracture. Orr expressed later this relationship mathematically by relating the applied stress to the inverse of the square root of the mirror radius, with the slope of this relationship representing a constant defined as the mirror constant [
15]. The relationship has been verified for glasses, polycrystalline ceramics of various compositions and microstructures, as well as single crystals [
19]. The principle of fracture mechanics has already been successfully applied to dental materials [
12]. This was primarily performed in the field of ceramics [
12] but has increasingly been applied to brittle CAD/CAM composites and light-curing composites [
15,
25].
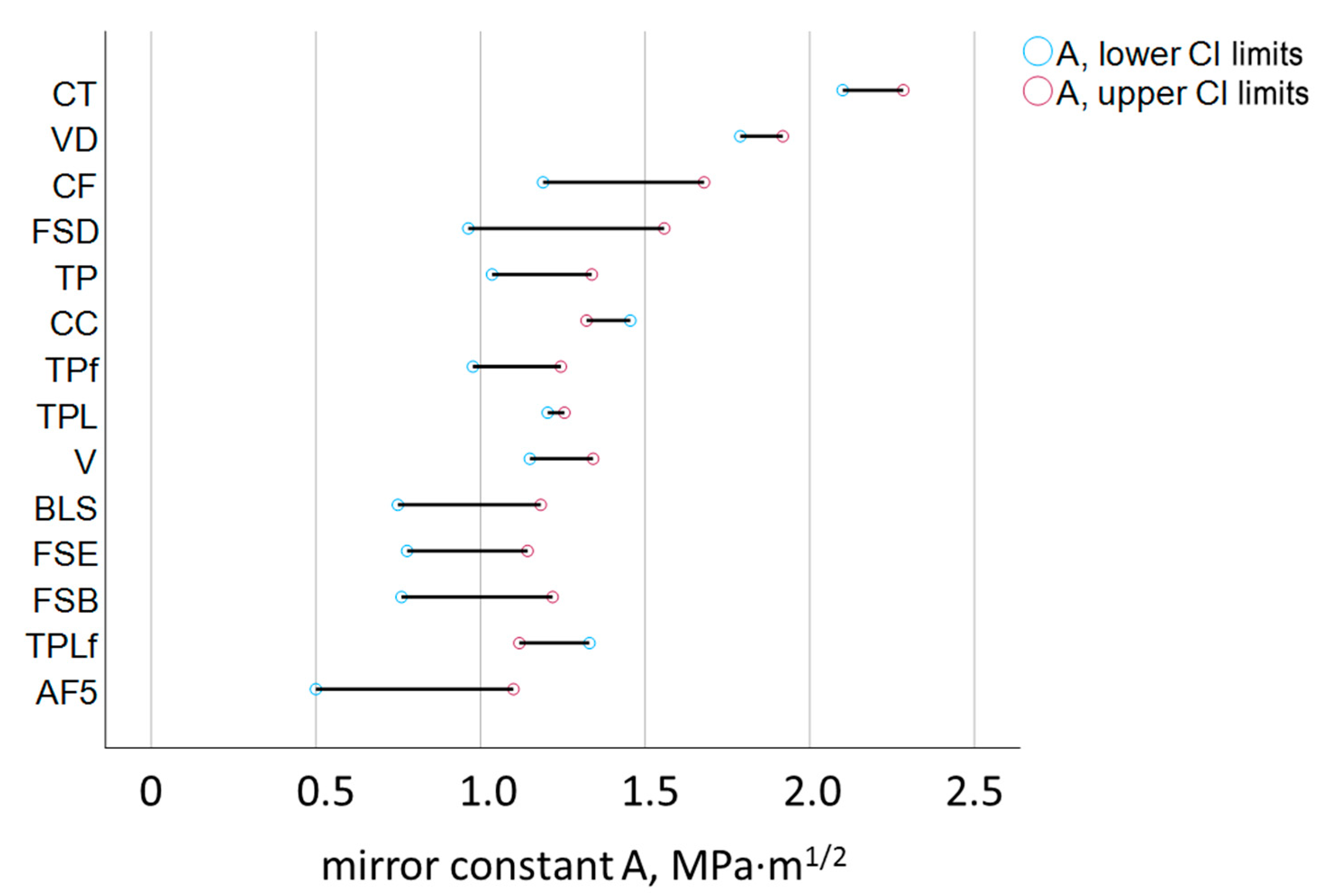
The fracture toughness, a material property that quantifies the resistance of a material to crack propagation under applied stress, and the mirror constant, derived from the size of the fracture mirror, are in good agreement in the present study and show a high correlation. This validates and encourages the use of quantitative fractography in brittle dental composites. However, it is noticeable that the data obtained by quantitative fractography have a significantly higher confidence interval (
Figure 7), which is due to the higher risk of error in the optical evaluation of the mirror boundaries. These were delineated as the first signs of noticeable roughness after the relatively smooth mirror surface. Although standardized illumination techniques and a trained operator were involved, the detection of the transition to the mist zone of the fractured surfaces is prone to individual perception and interpretation. Improvements can be achieved by involving multiple operators in the assessment [
12], by averaging the results and thus reducing operator-related errors. However, the ranking of the materials was comparable and the determined fracture toughness and mirror constant values were statistically similar for 9 of the 14 materials tested. Quantitative fractography revealed a slight overestimation of the mirror constant compared to K
Ic for only 5 materials—V, VD, CC, TPL, and TPLf. This means that the mirror radius was overestimated for these materials. A first plausible influencing factor would be the intrinsic roughness of the materials. Higher roughness can lead to a less smooth and shiny mirror and impair the accuracy of the delineation of the fracture mirror from the mist region. After a detailed analysis of the microstructure, this assumption is rejected because the above five materials actually have different compositions and exhibit strong differences in intrinsic roughness due to the different size and type of filler. V and VD are composites with compact glass filler, either the smallest or largest filler size of the tested materials. CC also contains a small amount of pre-polymerized filler, while TPL and TPLf are composites with a mixture of compact and pre-polymerized filler. The amount of filler cannot be used as an explanation in this context either, since the scatter of the filler amount between the five materials is also very high (
Table 1), which does not allow any differentiation with regard to the materials for which the radius was not overestimated. The lowest common denominator among the five materials appears to be the composition of the organic matrix, which is based on urethane methacrylate in all five materials. In contrast, the remaining tested materials are predominantly based on bis-GMA. Differences in optical properties, such as the lower refractive index of the organic matrix rich in urethane methacrylate compared to those based on bis-GMA, could therefore be taken into account, making the transition between the two regions more difficult to detect.
The determined material parameter, the mirror constant, and its relationship to fracture toughness can be applied in clinical fractography. In the case of a fractured composite restoration, the measurement of the fracture mirror size and knowledge of the material used for the restoration can be correlated with the mirror constant to provide an indicator of the stress the filling was subjected to during fracture. This information helps estimate the stress on the filling in the patient’s mouth and assess the resilience of a filling. This enables better and more efficient future treatment planning, as fractures are the most common reason for replacing a composite filling.