Virtual Reality, Augmented Reality, Gamification, and Telerehabilitation: Psychological Impact on Orthopedic Patients’ Rehabilitation
Abstract
1. Introduction
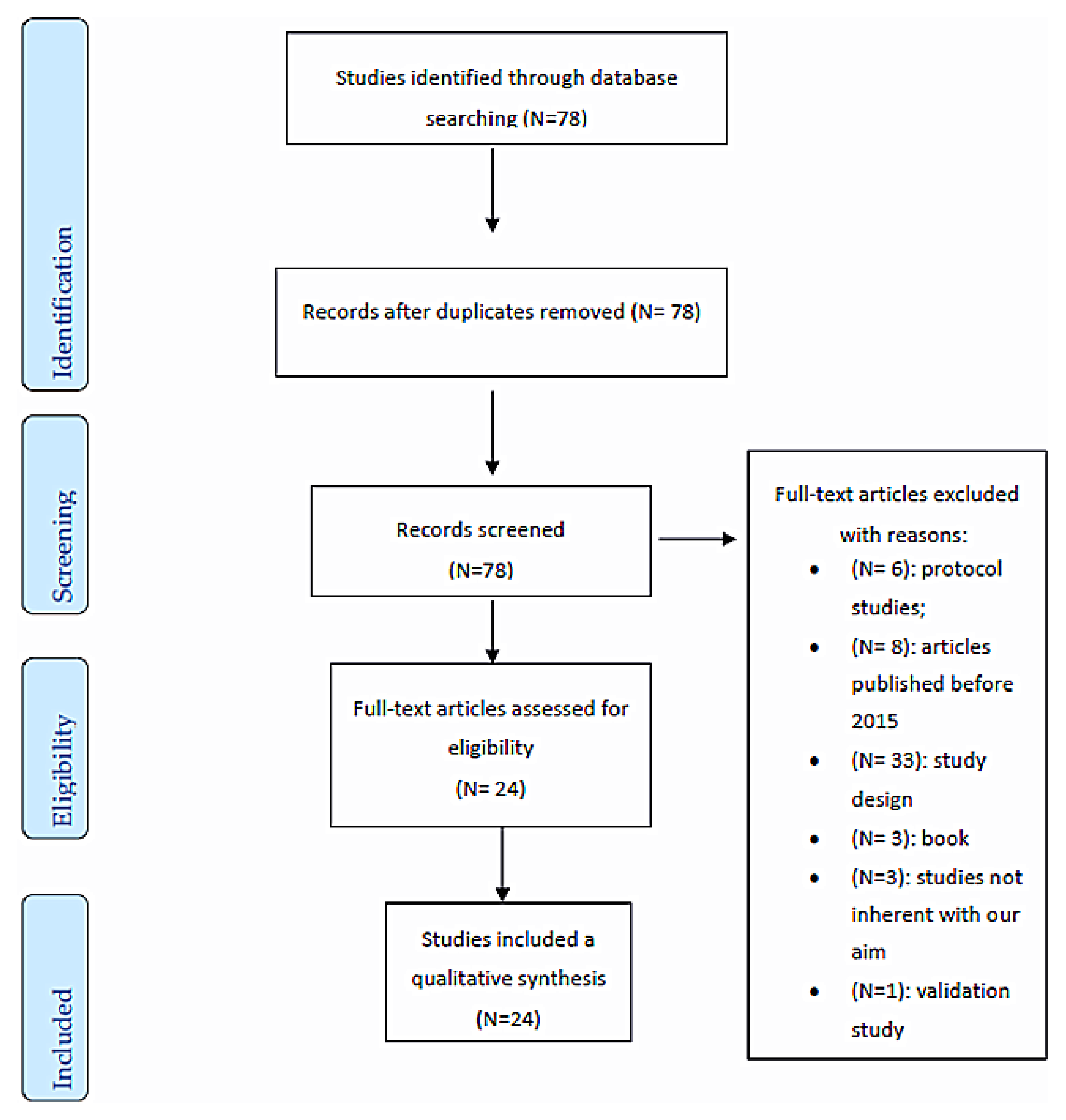
2. Materials and Methods
2.1. Eligibility Criteria and Search Strategy
2.2. Study Selection and Data Collection
2.3. Quality Assessment
2.4. Data Synthesis and Analysis
3. Results
3.1. Studies and Patients Characteristics
3.1.1. Qualitative Results
3.1.2. Quantitative Outcomes
3.2. Quality Assessment
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Khor, W.S.; Baker, B.G.; Amin, K.; Chan, A.; Patel, K.; Wong, J. Augmented and virtual reality in surgery—The digital surgical environment: Applications, limitations and legal pitfalls. Ann. Transl. Med. 2016, 4, 454. [Google Scholar] [CrossRef] [PubMed]
- Eriksson, L.; Lindström, B.; Ekenberg, L. Patients’ experiences of telerehabilitation at home after shoulder joint replacement. J. Telemed. Telecare 2011, 17, 25–30. [Google Scholar] [CrossRef] [PubMed]
- Negrillo-Cárdenas, J.; Jiménez-Pérez, J.-R.; Feito, F.R. The role of virtual and augmented reality in orthopedic trauma surgery: From diagnosis to rehabilitation. Comput. Methods Programs Biomed. 2020, 191, 105–407. [Google Scholar] [CrossRef] [PubMed]
- Chan, Z.Y.S.; MacPhail, A.J.C.; Au, I.P.H.; Zhang, J.H.; Lam, B.M.F.; Ferber, R.; Cheung, R.T.H. Walking with head-mounted virtual and augmented reality devices: Effects on position control and gait biomechanics. PLoS ONE 2019, 14, e0225972. [Google Scholar] [CrossRef]
- Allam, A.A.; Kostova, Z.; Nakamoto, K.; Schulz, P.J.; Merolli, M.; Lindsay, S.; Rini, C. The Effect of social support features and gamification on a web-based intervention for rheumatoid arthritis patients: Randomized controlled Trial. J. Med. Internet Res. 2015, 17, e14. [Google Scholar] [CrossRef]
- Kuether, J.; Moore, A.; Kahan, J.; Martucci, J.; Messina, T.; Perreault, R.; Sembler, R.; Tarutis, J.; Zazulak, B.; Rubin, L.E.; et al. Telerehabilitation for total hip and knee arthroplasty patients: A pilot series with high patient satisfaction. HSS J. 2019, 15, 221–225. [Google Scholar] [CrossRef]
- Doiron-Cadrin, P.; Kairy, D.; Vendittoli, P.-A.; Lowry, V.; Poitras, S.; Desmeules, F. Effects of a tele-prehabilitation program or an in-person prehabilitation program in surgical candidates awaiting total hip or knee arthroplasty: Protocol of a pilot single blind randomized controlled trial. Contemp. Clin. Trials Commun. 2016, 4, 192–198. [Google Scholar] [CrossRef]
- Then, J.W.; Shivdas, S.; Yahaya, T.S.T.A.; Ab Razak, N.I.; Choo, P.T. Gamification in rehabilitation of metacarpal fracture using cost-effective end-user device: A randomized controlled trial. J. Hand Ther. 2020. [Google Scholar] [CrossRef]
- Bernal, J.M.P.; Martín-Valero, R.; Barón-López, F.; García-Gómez, O. Effectiveness of telerehabilitation programme following surgery in shoulder impingement syndrome (SIS): Study protocol for a randomized controlled non-inferiority trial. Trials 2017, 18, 82. [Google Scholar] [CrossRef]
- Facchinetti, G.; D’Angelo, D.; Piredda, M.; Petitti, T.; Matarese, M.; Oliveti, A.; De Marinis, M.G. Continuity of care interventions for preventing hospital readmission of older people with chronic diseases: A meta-analysis. Int. J. Nurs. Stud. 2019, 101, 103–396. [Google Scholar] [CrossRef]
- Slim, K.; Nini, E.; Forestier, D.; Kwiatkowski, F.; Panis, Y.; Chipponi, J. Methodological index for non-randomized studies (minors): Development and validation of a new instrument. ANZ J. Surg. 2003, 73, 712–716. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Altman, U.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savović, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed]
- Liberati, A.; Altman, U.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef] [PubMed]
- Valenzuela-Pascual, F.; Molina, F.; Corbi, F.; Blanco, J.B.; Gil, R.; Soler-Gonzalez, J. The influence of a biopsychosocial educational internet-based intervention on pain, dysfunction, quality of life, and pain cognition in chronic low back pain patients in primary care: A mixed methods approach. BMC Med. Inform. Decis. Mak. 2015, 15, 97. [Google Scholar] [CrossRef]
- Van Der Kooij, K.; Van Dijsseldonk, R.B.; Van Veen, M.; Steenbrink, F.; De Weerd, C.; Overvliet, K.E. Gamification as a sustainable source of enjoyment during balance and gait exercises. Front. Psychol. 2019, 10, 294. [Google Scholar] [CrossRef]
- Kloster, M.; Babic, A. Mobile VR-application for neck exercises. Stud. Health Technol. Inform. 2019, 262, 206–209. [Google Scholar]
- Chughtai, M.; Kelly, J.J.; Newman, J.M.; Sultan, A.A.; Khlopas, A.; Sodhi, N.; Bhave, A.; Kolczun, M.C.; Mont, M.A. The role of virtual rehabilitation in total and unicompartmental knee arthroplasty. J. Knee Surg. 2018, 32, 105–110. [Google Scholar] [CrossRef]
- Gianola, S.; Stucovitz, E.; Castellini, G.; Mascali, M.; Vanni, F.; Tramacere, I.; Banfi, G.; Tornese, D. Effects of early virtual reality-based rehabilitation in patients with total knee arthroplasty. Medicine 2020, 99, e19136. [Google Scholar] [CrossRef]
- Matheve, T.; Bogaerts, K.; Timmermans, A. Virtual reality distraction induces hypoalgesia in patients with chronic low back pain: A randomized controlled trial. J. Neuroeng. Rehabil. 2020, 17, 12–55. [Google Scholar] [CrossRef]
- Pekyavas, N.O.; Ergun, N. Comparison of virtual reality exergaming and home exercise programs in patients with subacromial impingement syndrome and scapular dyskinesis: Short term effect. Acta Orthop. Traumatol. Turc. 2017, 51, 238–242. [Google Scholar] [CrossRef]
- Azma, K.; Rezasoltani, Z.; Rezaeimoghaddam, F.; Dadarkhah, A.; Mohsenolhosseini, S. Efficacy of tele-rehabilitation compared with office-based physical therapy in patients with knee osteoarthritis: A randomized clinical trial. J. Telemed. Telecare 2017, 24, 560–565. [Google Scholar] [CrossRef] [PubMed]
- Macías-Hernández, S.I.; Vásquez-Sotelo, D.S.; Ferruzca-Navarro, M.V.; Sánchez, S.H.B.; Gutiérrez-Martínez, J.; Núñez-Gaona, M.A.; Meneses, H.A.; Velez-Gutiérrez, O.B.; Tapia-Ferrusco, I.; Soria-Bastida, M.D.L.Á.; et al. Proposal and evaluation of a telerehabilitation platform designed for patients with partial rotator cuff tears: A Preliminary Study. Ann. Rehabil. Med. 2016, 40, 710–717. [Google Scholar] [CrossRef] [PubMed]
- Bini, S.; Mahajan, J. Clinical outcomes of remote asynchronous telerehabilitation are equivalent to traditional therapy following total knee arthroplasty: A randomized control study. J. Telemed. Telecare 2016, 23, 239–247. [Google Scholar] [CrossRef] [PubMed]
- Correia, F.D.; Nogueira, A.; Magalhães, I.; Guimarães, J.; Moreira, M.; Barradas, I.; Teixeira, L.; Tulha, J.; Seabra, R.; Lains, J.; et al. Home-based rehabilitation with a novel digital biofeedback system versus conventional in-person rehabilitation after Total knee replacement: A feasibility study. Sci. Rep. 2018, 8, 11299. [Google Scholar] [CrossRef]
- Eichler, S.; Salzwedel, A.; Rabe, S.; Mueller, S.; Mayer, F.; Wochatz, M.; Hadzic, M.; John, M.; Wegscheider, K.; Völler, H.; et al. The effectiveness of telerehabilitation as a supplement to rehabilitation in patients after total knee or hip replacement: Randomized controlled trial. JMIR Rehabil. Assist. Technol. 2019, 6, e14236. [Google Scholar] [CrossRef]
- Çubukçu, B.; Yuzgec, U.; Zileli, R.; Zileli, A. Reliability and validity analyzes of Kinect V2 based measurement system for shoulder motions. Med. Eng. Phys. 2019, 76, 20–31. [Google Scholar] [CrossRef]
- Doiron-Cadrin, P.; Kairy, D.; Vendittoli, P.-A.; Lowry, V.; Poitras, S.; Desmeules, F. Feasibility and preliminary effects of a tele-prehabilitation program and an in-person prehablitation program compared to usual care for total hip or knee arthroplasty candidates: A pilot randomized controlled trial. Disabil. Rehabil. 2019, 42, 989–998. [Google Scholar] [CrossRef]
- Tousignant, M.; Giguère, A.-M.; Morin, M.; Pelletier, J.; Sheehy, A.; Cabana, F. In-home telerehabilitation for proximal humerus fractures: A pilot study. Int. J. Telerehabil. 2015, 6, 31–37. [Google Scholar] [CrossRef]
- Nelson, M.J.; Crossley, K.M.; Bourke, M.G.; Russell, T.G. Telerehabilitation feasibility in total joint replacement. Int. J. Telerehabil. 2017, 9, 31–38. [Google Scholar] [CrossRef]
- Chughtai, M.; Shah, N.V.; Sultan, A.A.; Solow, M.; Tiberi, J.V.; Mehran, N.; North, T.; Moskal, J.T.; Newman, J.M.; Samuel, L.T.; et al. The role of prehabilitation with a telerehabilitation system prior to total knee arthroplasty. Ann. Transl. Med. 2019, 7, 68. [Google Scholar] [CrossRef]
- Richardson, B.R.; Truter, P.; Blumke, R.; Russell, T.G. Physiotherapy assessment and diagnosis of musculoskeletal disorders of the knee via telerehabilitation. J. Telemed. Telecare 2016, 23, 88–95. [Google Scholar] [CrossRef] [PubMed]
- Naeemabadi, M.; Søndergaard, J.H.; Klastrup, A.; Schlünsen, A.P.; Lauritsen, R.E.K.; Hansen, J.; Madsen, N.K.; Simonsen, O.; Andersen, O.K.; Kim, K.K.; et al. Development of an individualized asynchronous sensor-based telerehabilitation program for patients undergoing total knee replacement: Participatory design. Health Inform. J. 2020, 1460458220909779. [Google Scholar] [CrossRef] [PubMed]
- Tsvyakh, A.I.; Hospodarskyy, A.J. Telerehabilitation of Patients with Injuries of the Lower Extremities. Telemed. e-Health 2017, 23, 1011–1015. [Google Scholar] [CrossRef] [PubMed]
- Fusco, F.; Turchetti, G. Telerehabilitation after total knee replacement in Italy: Cost-effectiveness and cost-utility analysis of a mixed telerehabilitation-standard rehabilitation programme compared with usual care. BMJ Open 2016, 6, e009964. [Google Scholar] [CrossRef] [PubMed]
- Agostini, M.; Moja, L.; Banzi, R.; Pistotti, V.; Tonin, P.; Venneri, A.; Turolla, A. Telerehabilitation and recovery of motor function: A systematic review and meta-analysis. J. Telemed. Telecare 2015, 21, 202–213. [Google Scholar] [CrossRef]
- Bernal, J.M.P.; Martín-Valero, R.; Barón-López, F.J.; Estebanez-Pérez, M.J.; Kairy, D.; Peterson, S. Evidence of benefit of telerehabitation after orthopedic surgery: A systematic review. J. Med. Internet Res. 2017, 19, e142. [Google Scholar] [CrossRef]
- Blackwell, M.; Morgan, F.; Digioia, A.M. Augmented reality and its future in orthopaedics. Clin. Orthop. Relat. Res. 1998, 354, 111–122. [Google Scholar] [CrossRef]
- Cabana, F.; Pagé, C.; Svotelis, A.; Langlois-Michaud, S.; Tousignant, M. Is an in-home telerehabilitation program for people with proximal humerus fracture as effective as a conventional face-to face rehabilitation program? A study protocol for a noninferiority randomized clinical trial. BMC Sports Sci. Med. Rehabil. 2016, 8, 27. [Google Scholar] [CrossRef]
| Author and Country | Number of Patients | Study Design | Remote Virtual Rehabilitation Technology | Follow-Up |
|---|---|---|---|---|
| Valenzuela 2020, UK [14] | NA | Mixed (qualitative and RCT) | Gamification | 2 weeks |
| van der Kooij 2019, Netherlands [15] | 28 for first experiment | Pseudo-randomized trial | Gamification | 3 weeks |
| 22 for second experiment | ||||
| Then 2020, Malaysia [8] | 21 | RCT | Gamification | 2 weeks |
| Allam 2015, Switzerland [5] | 155 | RCT | Gamification | 6 months |
| Babic 2019, Norway [16] | 6 | Qualitative study | VR | 0 |
| Chan 2019, Hong Kong [4] | 13 | Feasibility study | VR/AR | 0 |
| Chughtai 2019, Ohio [17] | 157 | Non-randomized trial | VR | 1 month |
| Gianola 2020, Italy [18] | 85 but during the study lost 11 patients | RCT | VR | 10 days after surgery |
| Matheve 2020, Belgium [19] | 84 | RCT | VR | 21 months |
| Pekyavas 2017, Turkey [20] | 30 | RCT | VR | 2 months and half |
| Azma, 2017, Iran [21] | 54 | RCT | TR | 6 months |
| Hernandez, 2016, Mexico City [22] | 20 but during the study lost 9 patients | Auto-controlled study | TR | 6 months |
| Kuether 2019, USA [6] | 654 | Pilot study | TR | 12 weeks |
| Bini 2017, USA [23] | 51 | RCT | TR | 2 months |
| Correia 2018, Portugal [24] | 236, final analysis 69 (37 + 32). Completed the study 30 + 29 | Feasibility study | TR | 8 weeks |
| Eichler 2019, Germany [25] | 111 but during the study lost 24 patients | RCT | TR | 3 months |
| Çubukçu 2019, Turkey [26] | 40 | Non-randomized control trial | TR | 3 days |
| Doiron-Cadrin 2020, Canada [27] | 34 | RCT | TR | 12 weeks |
| Tousignant 2015, Canada [28] | 17 | Pilot study | TR | 8 weeks |
| Nelson 2017, Australia [29] | 75 | Qualitative study | TR | 2 months |
| Chughtai 2019, USA [30] | 476 | Cohort study | TR | 17 months |
| Richardson 2017, Australia [31] | 18 | Repeated-measures design | TR | 2 months |
| Naeemabadi 2020, Denmark [32] | NA | Qualitative study | TR | 2 weeks |
| Tsvyakh 2017, Ukraine [33] | 74 | RCT | TR | 3 months |
| Age | Social Context |
|---|---|
| 25–30 (35–9%) | University degree (35–9%) |
| 40–60 (312–79%) | Unemployed (31–8%) University degree (171–43%) Worked (108–27%) Retired (2–0.5%) |
| 60–80 (51–12%) | Retired (41–10%) Worked (8–2%) Semi-retired (2–0.5%) |
| Remote Virtual Rehabilitation Technology | Orthopedic Surgery | Orthopedic Disease | Total |
|---|---|---|---|
| Gamification | Immobilization for 4 to 6 weeks | Fracture of metacarpal | 21–1% |
| Gamification | NS | Rheumatoid arthritis | 155–7% |
| VR | TKA | Osteoarthritis | 85–4% |
| VR | NS | Chronic nonspecific low back pain | 84–4% |
| VR | NS | subacromial impingement syndrome and scapular dyskinesis | 30–1% |
| VR/AR | NS | Found in the hip, knee and ankle joint | 16–1% |
| TR | TKA or UKA or THA | Osteoarthritis | 1591–73% |
| TR | shoulder joint replacement | Primary osteoarthrosis or rheumatoid arthritis | 10–0.5% |
| TR | NS | Rotator cuff tears | 11–0.5% |
| TR | TJR | Severe hip and knee osteoarthritis | 75–3% |
| TR | hip fracture surgery | Acute hip fracture | 70–3% |
| TR | immobilization for 4 to 6 weeks | Proximal humerus fracture | 147–7% |
| TR | TKR | NS | 29–1% |
| Author and Country | Outcome Measure | Outcome Measure Result |
|---|---|---|
| Bini 2017, USA [23] | PRO (questionnaire) | Patient satisfaction overall with both the traditional patient care pathway and the digital interface was high, and there was no major difference. |
| Nelson 2017, Australia [29] | Questionnaire Franzen and Oppenheim | Only 35% reported feeling confident using technology. The results change considerably with advancing age: Telerehabilitation is feasible from the perspective of access to, feelings toward, and preferences for technology. |
| Doiron-Cadrin 2020, Canada [27] | Questionnaire | All participants (100%) felt they met their rehabilitation goals, felt positive about their telerehabilitation experience, and were satisfied with their physiotherapy treatments. |
| Babic 2019, Norway [16] | Interview A scale from one (low) to 5 (high) to collect the feedback. | The responses were that sometimes, negative feedback concerned nausea occurring during VR, but the overall experience was positive. |
| Naeemabadi 2020, Denmark [32] | Interviews Questionnaires (Likert scale) | Iteration 4: The user-friendliness of the TR was high to very high. The patients reported a lower level of satisfaction in the area of communication and training with the wearable sensors. Iteration 5: The level of motivation among patients increased. A higher level of self-confidence was reported. The participants believed that physiotherapist’s feedback on the patients’ performance and questions induced a sense of security. The majority of the users claim that the system can considerably reduce the need for travel. |
| Author and Country | Outcome Measure | Outcome Measure Result |
|---|---|---|
| van der Kooij 2019, Netherlands [15] | EXPERIMENT 1 | EXPERIMENT 1 |
| QMI | (1) IMI: game group scored higher than the control group: IG = −2.37, CG = 0.03 | |
| IMI | (2) QMI: did not differ significantly between the game and control group IG = 1.82, CG = 0.068 | |
| EXPERIMENT 2 | EXPERIMENT 2 | |
| CoM velocity; | (1) CoM velocity: effect of group F (1,37) = 0.48, p = 0.49, interaction of group and block F (2,74) = 1.16, p = 0.32, and effect of block, F (2,74) = 1.99, p = 0.14. | |
| CoM distance | (2) CoM distance: effect of block F (1.34,49.57) = 15.46 p < 0.001, effect of group F (1,37) = 2.32 p = 0.14, and interaction of group and block F (1.34,49.57) = 0.21 p = 0.72 | |
| QMI | (3) QMI: z = −1.06, p = 0.29 | |
| Then 2020, Malaysia [8] | grip strength; | -grip strength: IG = 36.15, CG = 30.74; |
| composite finger ROM; | -composite finger ROM: IG = 2.78, CG = 4.50 | |
| PRWE; | -PRWE: IG = 3.44, CG = 8.45 | |
| compliance (min/day) | -compliance: IG = 26.89, CG = 16.57 | |
| Allam 2015, Switzerland [5] | Exercise Behaviors Scale; | Exercise Behaviors Scale: (B = 3.39, p = 0.02) |
| Health Care Utilization Scale; | Health care system: (B = 2.79, p = 0.02) | |
| Prescription Opioid Misuse Index; | Prescription Opioid Misuse Index: (B = 12.06, p = 0.03); | |
| Chan 2019, Hong Kong [4] | CoP Ellipse area; | CoP Ellipse area: for AR 433.78 ± 229.27 (p), for VR 934.14 ± 745.09 (p); |
| Stride length; | Stride length: for AR 0.98 ± 0.07 (p), for VR 0.98 ± 0.06 (p) | |
| Cadence | Cadence: for AR 102.41 ± 7.90 (p), for VR 102.73 ± 6.59 (p) | |
| Chughtai 2018, Ohio [17] | KSS; SUS; | KSS pain and function scores improved, and the improvements were measured at 368% for TKA and 350% for UKA (pain) and 27% for UKA and 33% for TKA (function). Moreover, WOMAC scores improved by 57% and 66% for UKA and TKA patients, while the improvement in AM-PAC scores was at 22% and 24%. |
| WOMAC; | ||
| AM-PAC | ||
| Gianola 2020, Italy [18] | All the results are reported in change from before to after study | |
| VAS; | VAS: IG = −23.03, CG = −28.97 | |
| WOMAC; | WOMAC: IG = −790.28, CG = −765.77 | |
| EQ-5D; | EQ-5D: IG = 0.13, CG = 0.15 | |
| GPE; | GPE: IG = 4.58, CG = 4.71 | |
| FIM questionnaire | FIM: IG = 17.03; CG = 21.19 | |
| Matheve 2020, Belgium [19] | NPRS; | To evaluate pain-related fear there was a main effect for group (all p-values < 0.0001) and for TSK (all p-values < 0.02), but there was no interaction effect (all p-values > 0.54). To evaluate pain catastrophizing, a main effect for group (all p-values < 0.0001) and PCS (all p-values < 0.02) was present, but there was no interaction effect (all p-values > 0.5) |
| RMDQ; | ||
| PCS; | ||
| TSK | ||
| Pekyavas 2017, Turkey [20] | SPADI; | SPADI: IG = 8.13, CG = 11.41; |
| NEER; | NEER: IG = 0.00, CG = 0.08; | |
| HAWKINS; | HAWKINS: IG = 0.00, CG = 0.00; | |
| SRT; | SRT: IG = 2.22, CG = 0.08; | |
| SAT; | SAT: IG = 0.00, CG = 0.83; | |
| LSST | LSST: IG = 0.42, CG = 1.58 | |
| Azma 2017, Iran [21] | VAS; | VAS (62.5 ± 9.1); |
| WOMAC; | WOMAC (72.5 ± 23.2) | |
| KOOS | KOOS (79.4 ± 28.3); | |
| Macías-Hernández 2016, Mexico City [22] | VAS; | VAS pain (after 6 months 16 (0–30)); |
| CM | CM (after 6 months 85 (70–100)) | |
| Kuether 2019, USA [6] | KOORS; | KOOS 4.6. |
| HOOS | HOOS 4.4; | |
| Bini 2017, USA [23] | VAS; | VAS (−3.724); |
| VR-12; | VR-12 PCS (15.310); VR-12 MCS (3.611). | |
| KOOS-PS | KOOS (−17.415); | |
| Çubukçu 2019, Turkey [26] | Degree (Clinical goniometer and digital goniometer) | Clinical goniometer vs. Kinect V2: 0.33° (abduction), −2.83° (flexion), −0.50° (external rotation), −6.67° (internal rotation) and −0.10° (extension). Digital goniometer vs. Kinect V2: 1.10° (abduction), −1.63° (flexion), −0.38° (external rotation), −5.35° (internal rotation) and 0.03° (extension). |
| Eichler 2019, Germany [25] | WOMAC; | WOMAC (IG −14.9, CG −10.9); |
| SF-36; | SF-36 PCS (IG 10.7, CG 11.1); SF-36 MCS (IG −2.5, CG 0.1) | |
| Doiron-Cadrin 2020, Canada [27] | SPW; ST; WOMAC; SF-36; LEFS; TUG; GRC | LEFS (pre-TR 2.9 ± 13.9, in-person pre-rehab −2.6 ± 6.7, control −1.3 ± 11.1); WOMAC pain (pre-TR −0.3 ± 4.8, in-person pre-rehab −0.8 ± 2.8, control 0.5 ± 2.8); SF-36 PCS (pre-TR −0.5 ± 7.0, in-person pre-rehab 0.2 ± 7.0, control −0.4 ± 5.2); SF-36 MCS (pre-TR 1.0 ± 10.0, in-person pre-rehab 0.5 ± 8.0, control −1.0 ± 8.5); TUG (pre-TR −0.8 ± 1.7, in-person pre-rehab −0.2 ± 1.7, control 0.3 ± 1.5); SPW (pre-TR −5.0 ± 5.3, in-person pre-rehab −4.2 ± 5.4, control 0.9 ± 12.3); ST (pre-TR −2.1 ± 2.7, in-person pre-rehab −2.0 ± 5.7, control −2.6 ± 8.0); |
| Richardson 2017, Australia [31] | VAS; | VAS (« a high overall reporting of satisfaction ») Validity: 2 different/18 4 similar/18 Intra-rater reliability: 89% Inter-rater reliability: 67% |
| Tousignant 2015, Canada [28] | SF-MPQ; | SF-MPQ (10.6 ± 12.4); |
| VAS; | VAS (26.3 ± 21.8); | |
| F-DASH; | F-DASH (42.1 ± 11.4). | |
| questionnaire | Questionnaire (global score 82 ± 7%) | |
| Tsvyakh 2017, Ukraine [33] | LEFS | IG 44,62; CG 36.43 |
| Chughtai 2019, USA [30] | LOS | LOS 2.0 rehab; 2.7 GC |
| Correia 2018, Portugal [24] | TUG; KOOS | TUG (IG: −9.5, CG: −4.6) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Berton, A.; Longo, U.G.; Candela, V.; Fioravanti, S.; Giannone, L.; Arcangeli, V.; Alciati, V.; Berton, C.; Facchinetti, G.; Marchetti, A.; et al. Virtual Reality, Augmented Reality, Gamification, and Telerehabilitation: Psychological Impact on Orthopedic Patients’ Rehabilitation. J. Clin. Med. 2020, 9, 2567. https://doi.org/10.3390/jcm9082567
Berton A, Longo UG, Candela V, Fioravanti S, Giannone L, Arcangeli V, Alciati V, Berton C, Facchinetti G, Marchetti A, et al. Virtual Reality, Augmented Reality, Gamification, and Telerehabilitation: Psychological Impact on Orthopedic Patients’ Rehabilitation. Journal of Clinical Medicine. 2020; 9(8):2567. https://doi.org/10.3390/jcm9082567
Chicago/Turabian StyleBerton, Alessandra, Umile Giuseppe Longo, Vincenzo Candela, Sara Fioravanti, Lucia Giannone, Valeria Arcangeli, Viviana Alciati, Claudia Berton, Gabriella Facchinetti, Anna Marchetti, and et al. 2020. "Virtual Reality, Augmented Reality, Gamification, and Telerehabilitation: Psychological Impact on Orthopedic Patients’ Rehabilitation" Journal of Clinical Medicine 9, no. 8: 2567. https://doi.org/10.3390/jcm9082567
APA StyleBerton, A., Longo, U. G., Candela, V., Fioravanti, S., Giannone, L., Arcangeli, V., Alciati, V., Berton, C., Facchinetti, G., Marchetti, A., Schena, E., De Marinis, M. G., & Denaro, V. (2020). Virtual Reality, Augmented Reality, Gamification, and Telerehabilitation: Psychological Impact on Orthopedic Patients’ Rehabilitation. Journal of Clinical Medicine, 9(8), 2567. https://doi.org/10.3390/jcm9082567







