The Infinity-Lock System for Chronic Grade III AC Joint Dislocation: A Novel Technique, Rehabilitation Protocol and Short Term Results
Abstract
1. Introduction
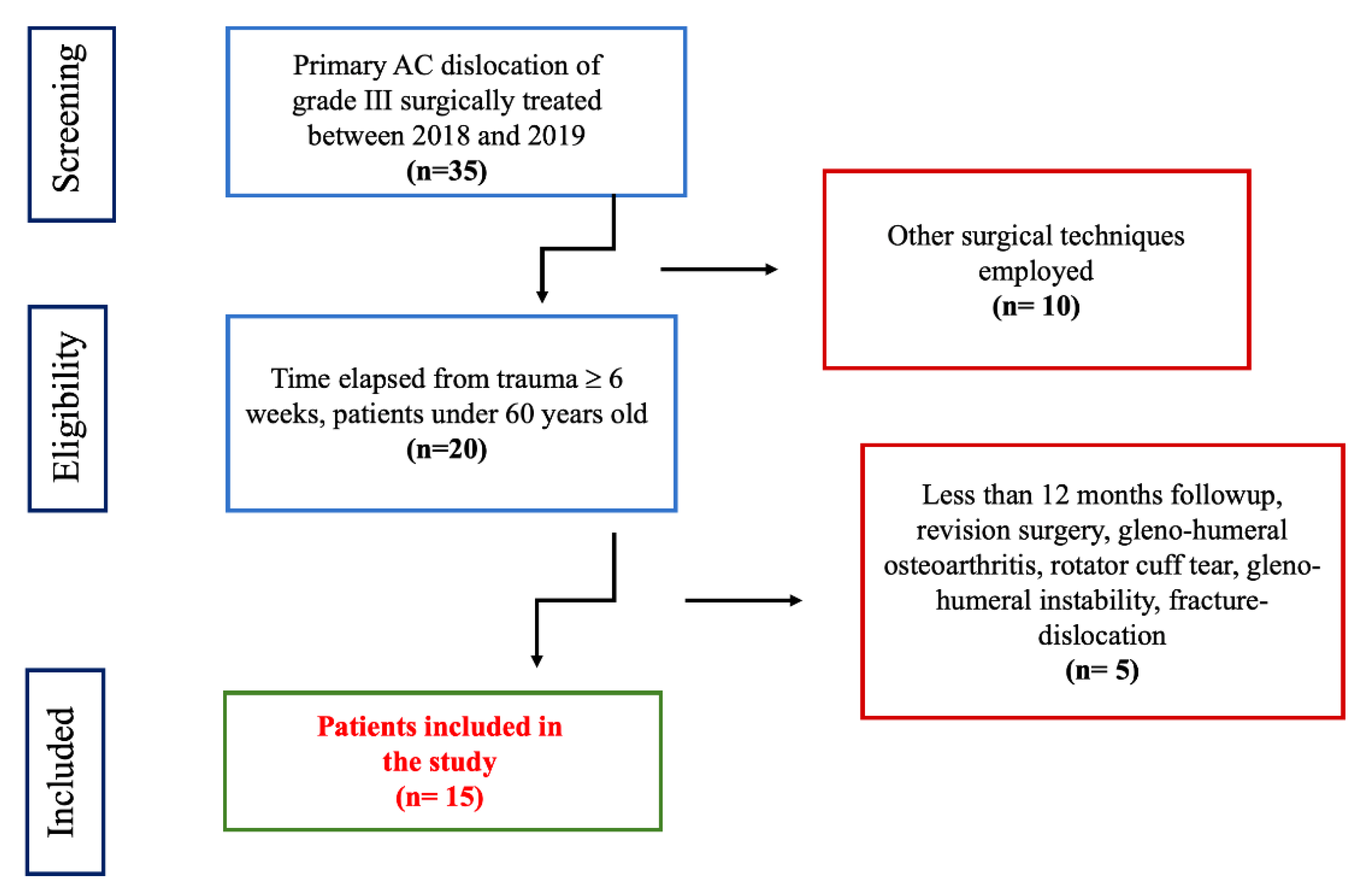
2. Material and Methods
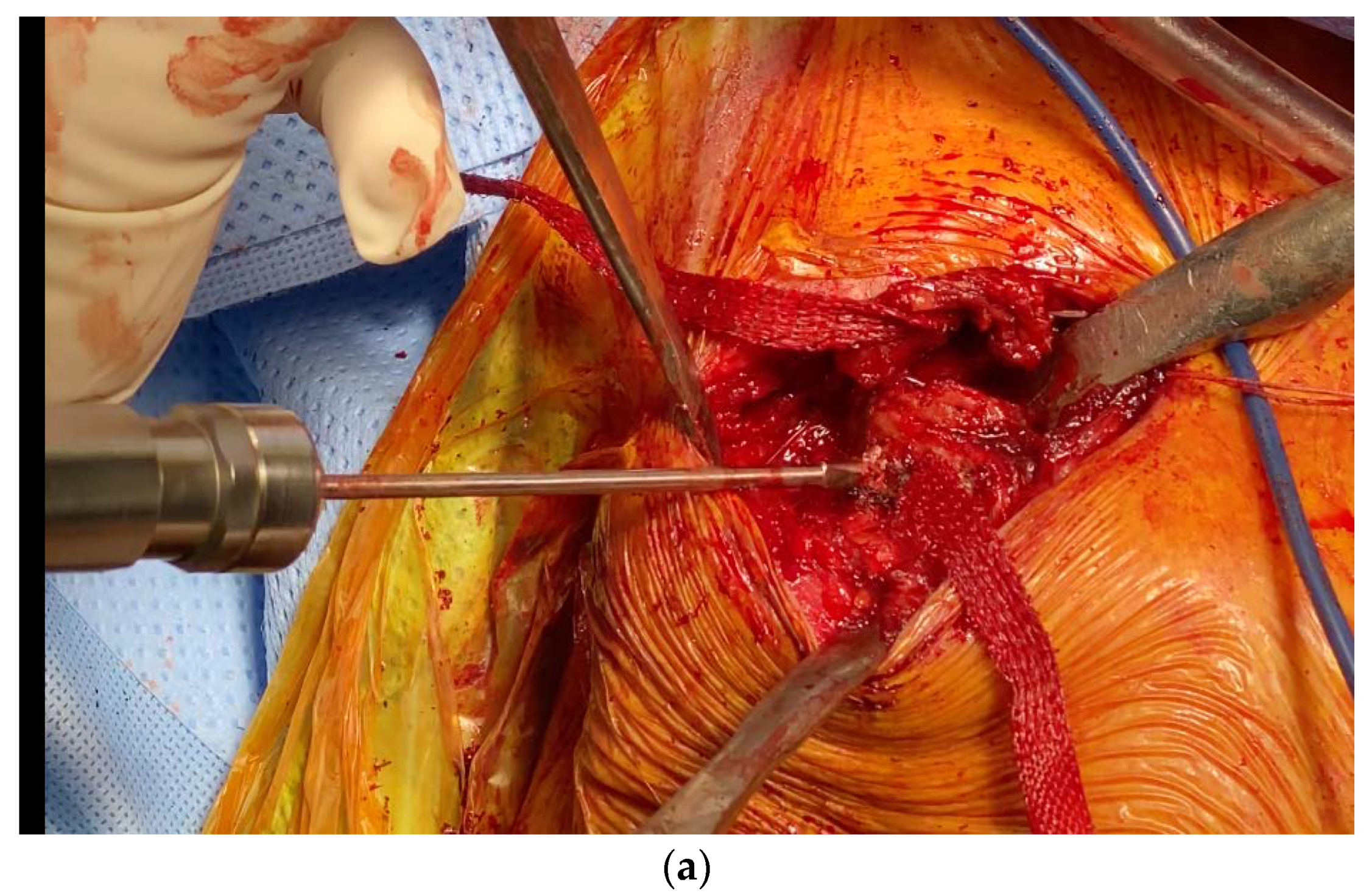
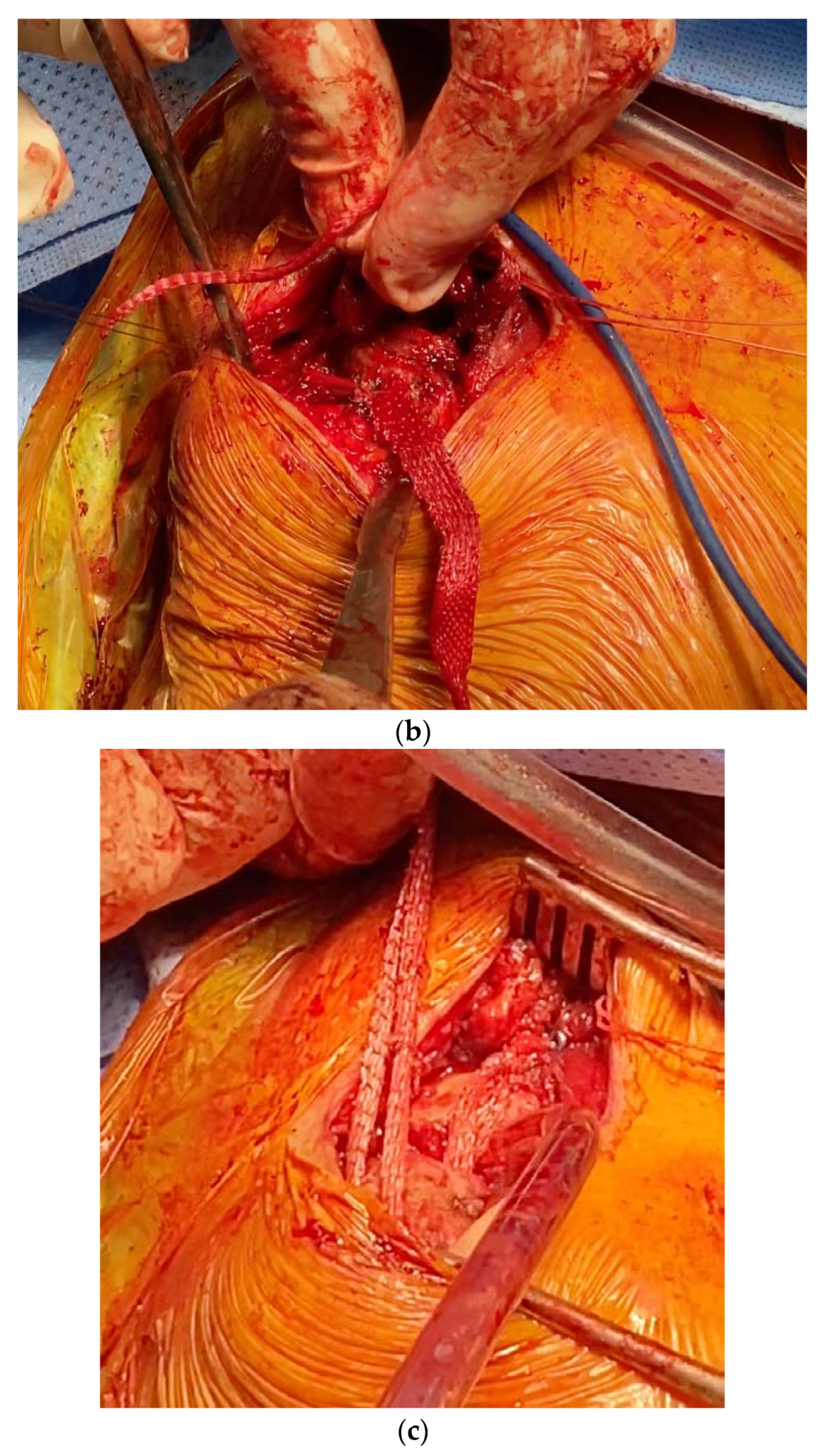
2.1. Surgical Technique
2.2. Rehabilitation
2.3. Statistical Analysis
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Hindle, P.; Davidson, E.K.; Biant, L.C.; Court-Brown, C.M. Appendicular joint dislocations. Injury 2013, 44, 1022–1027. [Google Scholar] [CrossRef]
- Simovitch, R.; Sanders, B.; Ozbaydar, M.; Lavery, K.; Warner, J.J.P. Acromioclavicular Joint Injuries: Diagnosis and Management. J. Am. Acad. Orthop. Surg. 2009, 17, 207–219. [Google Scholar] [CrossRef] [PubMed]
- Pallis, M.; Cameron, K.L.; Svoboda, S.J.; Owens, B.D. Epidemiology of Acromioclavicular Joint Injury in Young Athletes. Am. J. Sports Med. 2012, 40, 2072–2077. [Google Scholar] [CrossRef] [PubMed]
- Domos, P.; Ascione, F.; Wallace, A.L. Arthroscopic Bankart repair with remplissage for non–engaging Hill–Sachs lesion in professional collision athletes. Shoulder Elb. 2019, 11, 17–25. [Google Scholar] [CrossRef] [PubMed]
- Moatshe, G.; Kruckeberg, B.M.; Chahla, J.; Godin, J.A.; Cinque, M.E.; Provencher, M.T.; LaPrade, R.F. Acromioclavicular and Coracoclavicular Ligament Reconstruction for Acromioclavicular Joint Instability: A Systematic Review of Clinical and Radiographic Outcomes. Arthrosc. J. Arthrosc. Relat. Surg. 2018, 34, 1979–1995.e8. [Google Scholar] [CrossRef]
- Younis, F.; Ajwani, S.; Bibi, A.; Riley, E.; Hughes, P.J. Operative Versus Non–operative Treatment of Grade III Acromioclavicular Joint Dislocations and the Use of SurgiLig: A Retrospective Review. Ortop. Traumatol. Rehabil. 2017, 19, 523–530. [Google Scholar] [CrossRef]
- Spencer, E.E. Treatment of Grade III Acromioclavicular Joint Injuries: A Systematic Review. Clin. Orthop. 2007, 455, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Bain, G.; Sood, A.; Wallwork, N. Clinical results of coracoacromial ligament transfer in acromioclavicular dislocations: A review of published literature. Int. J. Shoulder Surg. 2008, 2, 13. [Google Scholar] [CrossRef][Green Version]
- Tamaoki, M.J.S.; Belloti, J.C.; Lenza, M.; Matsumoto, M.H.; Gomes dos Santos, J.B.; Faloppa, F. Surgical versus conservative interventions for treating acromioclavicular dislocation of the shoulder in adults. Cochrane Database Syst. Rev. 2010. [Google Scholar] [CrossRef]
- Lu, N.; Zhu, L.; Ye, T.; Chen, A.; Jiang, X.; Zhang, Z.; Zhu, Q.; Guo, Q.; Yang, D. Evaluation of the coracoclavicular reconstruction using LARS artificial ligament in acute acromioclavicular joint dislocation. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 2223–2227. [Google Scholar] [CrossRef]
- Breslow, M.J.; Jazrawi, L.M.; Bernstein, A.D.; Kummer, F.J.; Rokito, A.S. Treatment of acromioclavicular joint separation: Suture or suture anchors? J. Shoulder Elb. Surg. 2002, 11, 225–229. [Google Scholar] [CrossRef] [PubMed]
- Stucken, C.; Cohen, S.B. Management of Acromioclavicular Joint Injuries. Orthop. Clin. N. Am. 2015, 46, 57–66. [Google Scholar] [CrossRef] [PubMed]
- Thiel, E.; Mutnal, A.; Gilot, G.J. Surgical Outcome Following Arthroscopic Fixation of Acromioclavicular Joint Disruption With the TightRope Device. Orthopedics 2011. [Google Scholar] [CrossRef] [PubMed]
- Jeon, I.-H.; Dewnany, G.; Hartley, R.; Neumann, L.; Wallace, W.A. Chronic acromioclavicular separation: The medium term results of coracoclavicular ligament reconstruction using braided polyester prosthetic ligament. Injury 2007, 38, 1247–1253. [Google Scholar] [CrossRef]
- Malahias, M.-A.; Sarlikiotis, T.; Brilakis, E.; Gerogiannis, D.; Avramidis, G.; Antonogiannakis, E. The clinical outcome of the ‘Surgilig’ technique for the reconstruction of acromioclavicular dislocations: A systematic review. J. Orthop. 2020, 18, 126–131. [Google Scholar] [CrossRef]
- Fauci, F.; Merolla, G.; Paladini, P.; Campi, F.; Porcellini, G. Surgical treatment of chronic acromioclavicular dislocation with biologic graft vs synthetic ligament: A prospective randomized comparative study. J. Orthop. Traumatol. 2013, 14, 283–290. [Google Scholar] [CrossRef]
- Fraschini, G.; Ciampi, P.; Scotti, C.; Ballis, R.; Peretti, G.M. Surgical treatment of chronic acromioclavicular dislocation: Comparison between two surgical procedures for anatomic reconstruction. Injury 2010, 41, 1103–1106. [Google Scholar] [CrossRef]
- Motamedi, A.R.; Blevins, F.T.; Willis, M.C.; McNally, T.P.; Shahinpoor, M. Biomechanics of the Coracoclavicular Ligament Complex and Augmentations Used in Its Repair and Reconstruction. Am. J. Sports Med. 2000, 28, 380–384. [Google Scholar] [CrossRef]
- Kocaoglu, B.; Ulku, T.K.; Gereli, A.; Karahan, M.; Türkmen, M. Palmaris longus tendon graft versus modified Weaver–Dunn procedure via dynamic button system for acromioclavicular joint reconstruction in chronic cases. J. Shoulder Elbow Surg. 2017, 26, 1546–1552. [Google Scholar] [CrossRef]
- Borbas, P.; Churchill, J.; Ek, E.T. Surgical management of chronic high-grade acromioclavicular joint dislocations: A systematic review. J. Shoulder Elb. Surg. 2019, 28, 2031–2038. [Google Scholar] [CrossRef]
- Larsen, E.; Bjerg-Nielsen, A.; Christensen, P. Conservative or surgical treatment of acromioclavicular dislocation. A prospective, controlled, randomized study. J. Bone Joint Surg. Am. 1986, 68, 552–555. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Zhang, J. Acromioclavicular joint reconstruction by coracoid process transfer augmented with hook plate. Injury 2014, 45, 949–954. [Google Scholar] [CrossRef] [PubMed]
- Bosworth, B.M. Acromioclavicular Dislocation. Ann. Surg. 1948, 127, 98–111. [Google Scholar] [CrossRef] [PubMed]
- Defoort, S.; Verborgt, O. Functional and radiological outcome after arthroscopic and open acromioclavicular stabilization using a double–button fixation system. Acta Orthop. Belg. 2010, 76, 585–591. [Google Scholar] [PubMed]
- Hosseini, H.; Friedmann, S.; Tröger, M.; Lobenhoffer, P.; Agneskirchner, J.D. Arthroscopic reconstruction of chronic AC joint dislocations by transposition of the coracoacromial ligament augmented by the Tight Rope device: A technical note. Knee Surg. Sports Traumatol. Arthrosc. 2009, 17, 92–97. [Google Scholar] [CrossRef]
- Bhattacharya, R.; Goodchild, L.; Rangan, A. Acromioclavicular joint reconstruction using the Nottingham Surgilig: A preliminary report. Acta Orthop. Belg. 2008, 74, 167–172. [Google Scholar]
- Tauber, M.; Gordon, K.; Koller, H.; Fox, M.; Resch, H. Semitendinosus Tendon Graft versus a Modified Weaver–Dunn Procedure for Acromioclavicular Joint Reconstruction in Chronic Cases: Prospective Comparative Study. Am. J. Sports Med. 2009, 37, 181–190. [Google Scholar] [CrossRef]
- Bugelli, G.; Dell’Osso, G.; Ascione, F.; Gori, E.; Bottai, V.; Giannotti, S. LARSTM in ACL reconstruction: Evaluation of 60 cases with 5–year minimum follow–up. Musculoskelet. Surg. 2017. [Google Scholar] [CrossRef]
- Barwood, S.A.; French, J.A.; Watson, L.A.; Balster, S.M.; Hoy, G.A.; Pizzari, T. The Specific AC Score (SACS): A new and validated method of assessment of isolated acromioclavicular joint pathology. J. Shoulder Elb. Surg. 2018, 27, 2214–2223. [Google Scholar] [CrossRef]
- Constant, C.R.; Murley, A.H. A clinical method of functional assessment of the shoulder. Clin. Orthop. 1987, 160–164. [Google Scholar] [CrossRef]
- Romano, A.M.; Oliva, F.; Nastrucci, G.; Casillo, P.; Di Giunta, A.; Susanna, M.; Ascione, F. Reverse shoulder arthroplasty patient personalized rehabilitation protocol. Preliminary results according to prognostic groups. Muscle Ligaments Tendons J. 2019, 7, 263. [Google Scholar] [CrossRef]
- Smith, T.O.; Chester, R.; Pearse, E.O.; Hing, C.B. Operative versus non–operative management following Rockwood grade III acromioclavicular separation: A meta-analysis of the current evidence base. J. Orthop. Traumatol. 2011, 12, 19–27. [Google Scholar] [CrossRef]
- Flint, J.H.; Wade, A.M.; Giuliani, J.; Rue, J.-P. Defining the Terms Acute and Chronic in Orthopaedic Sports Injuries: A Systematic Review. Am. J. Sports Med. 2014, 42, 235–241. [Google Scholar] [CrossRef] [PubMed]
- Rolf, O.; Hann von Weyhern, A.; Ewers, A.; Boehm, T.D.; Gohlke, F. Acromioclavicular dislocation Rockwood III–V: Results of early versus delayed surgical treatment. Arch. Orthop. Trauma Surg. 2008, 128, 1153–1157. [Google Scholar] [CrossRef] [PubMed]
- Weaver, J.K.; Dunn, H.K. Treatment of acromioclavicular injuries, especially complete acromioclavicular separation. J. Bone Joint Surg. Am. 1972, 54, 1187–1194. [Google Scholar] [CrossRef]
- Kay, J.; Memon, M.; Alolabi, B. Return to Sport and Clinical Outcomes After Surgical Management of Acromioclavicular Joint Dislocation: A Systematic Review. Arthrosc. J. Arthrosc. Relat. Surg. 2018, 34, 2910–2924.e1. [Google Scholar] [CrossRef]
- Beitzel, K.; Cote, M.P.; Apostolakos, J.; Solovyova, O.; Judson, C.H.; Ziegler, C.G.; Edgar, C.M.; Imhoff, A.B.; Arciero, R.A.; Mazzocca, A.D. Current Concepts in the Treatment of Acromioclavicular Joint Dislocations. Arthrosc. J. Arthrosc. Relat. Surg. 2013, 29, 387–397. [Google Scholar] [CrossRef]
- Cook, J.B.; Tokish, J.M. Surgical Management of Acromioclavicular Dislocations. Clin. Sports Med. 2014, 33, 721–737. [Google Scholar] [CrossRef]
- Shin, S.-J.; Kim, N.-K. Complications After Arthroscopic Coracoclavicular Reconstruction Using a Single Adjustable–Loop-Length Suspensory Fixation Device in Acute Acromioclavicular Joint Dislocation. Arthrosc. J. Arthrosc. Relat. Surg. 2015, 31, 816–824. [Google Scholar] [CrossRef]
- Modi, C.S.; Beazley, J.; Zywiel, M.G.; Lawrence, T.M.; Veillette, C.J.H. Controversies relating to the management of acromioclavicular joint dislocations. Bone Jt. J. 2013, 95–B, 1595–1602. [Google Scholar] [CrossRef]
- Kumar, S.; Penematsa, S.R.; Selvan, T. Surgical reconstruction for chronic painful acromioclavicular joint dislocations. Arch. Orthop. Trauma Surg. 2007, 127, 481–484. [Google Scholar] [CrossRef] [PubMed]
- Arirachakaran, A.; Boonard, M.; Piyapittayanun, P.; Kanchanatawan, W.; Chaijenkij, K.; Prommahachai, A.; Kongtharvonskul, J. Post-operative outcomes and complications of suspensory loop fixation device versus hook plate in acute unstable acromioclavicular joint dislocation: A systematic review and meta–analysis. J. Orthop. Traumatol. 2017, 18, 293–304. [Google Scholar] [CrossRef] [PubMed]
- Lee, T.Q.; Black, A.D.; Tibone, J.E.; McMahon, P.J. Release of the coracoacromial ligament can lead to glenohumeral laxity: A biomechanical study. J. Shoulder Elb. Surg. 2001, 10, 68–72. [Google Scholar] [CrossRef]
- Lin, H.-Y.; Wong, P.-K.; Ho, W.-P.; Chuang, T.-Y.; Liao, Y.-S.; Wong, C.-C. Clavicular hook plate may induce subacromial shoulder impingement and rotator cuff lesion—Dynamic sonographic evaluation. J. Orthop. Surg. 2014, 9, 6. [Google Scholar] [CrossRef]
- Martetschläger, F.; Horan, M.P.; Warth, R.J.; Millett, P.J. Complications After Anatomic Fixation and Reconstruction of the Coracoclavicular Ligaments. Am. J. Sports Med. 2013, 41, 2896–2903. [Google Scholar] [CrossRef]
- Nelson, A.; Esposito, J.; Ono, Y.; Lo, I.; Boorman, R.; Thornton, G. Complications following arthroscopic fixation of acromioclavicular separations: A systematic review of the literature. Open Access J. Sports Med. 2015, 97. [Google Scholar] [CrossRef][Green Version]
- Spiegl, U.J.; Smith, S.D.; Euler, S.A.; Dornan, G.J.; Millett, P.J.; Wijdicks, C.A. Biomechanical Consequences of Coracoclavicular Reconstruction Techniques on Clavicle Strength. Am. J. Sports Med. 2014, 42, 1724–1730. [Google Scholar] [CrossRef]
- Sinagra, Z.P.; Kop, A.; Pabbruwe, M.; Parry, J.; Clark, G. Foreign Body Reaction Associated With Artificial LARS Ligaments: A Retrieval Study. Orthop. J. Sports Med. 2018, 6. [Google Scholar] [CrossRef]
- Wright, J.; Osarumwense, D.; Ismail, F.; Umebuani, Y.; Orakwe, S. Stabilisation for the Disrupted Acromioclavicular Joint Using a Braided Polyester Prosthetic Ligament. J. Orthop. Surg. 2015, 23, 223–228. [Google Scholar] [CrossRef]



| Technique | Advantages | Disadvantages |
|---|---|---|
| Weaver-Dunn/ Dewar | Widely used in literature | Sacrifice of CA ligament/conjoint tendon, lower strength of construct, may require augmentation |
| Bosworth | Low cost, readily available | Bicortical and bi-bone fixation, risk of fracture/screw loosening or breakage, may require removal |
| Hook Plate/ K wires | Strong construct | Plate impingement, skin and infections problems, second operation required |
| Tendon grafts | Good outcomes, biological construct, no sacrifice of CA ligament | Donor site related problems, infections, additional costs for allograft, additional surgical time |
| Synthetic ligaments | Biomechanically proven, non-harvesting technique, no sacrifice of CA ligament, enable soft tissue ingrowth, good tensile strength, low complications rate | Possible soft tissue irritation/reaction, fixation screw may require removal, bone fracture risk |
| Suture loops/ suspensory systems | Biomechanically proven, non-harvesting technique, loop around coracoid, strong fixation, no sacrifice of CA ligament | Bone fractures, loss of reduction, bony erosion, implant migration |
| Infinity Lock System | non-harvesting technique, single 4mm clavicle tunnel, loop around coracoid, no sacrifice of CA ligament, good tensile strength, titanium button on clavicle maintains reduction, low complications rate | Possible soft tissue irritation/reaction |
| PRE | POST | p | |
|---|---|---|---|
| FF | 70 ± 28 | 162 ± 8 | <0.05 |
| ER1 | 15 ± 5 | 35 ± 10 | <0.05 |
| ER2 | 46 ± 9 | 84 ± 5 | <0.05 |
| IR1 (out of 10), points | 5 ± 3 | 9 ± 1 | NS |
| IR2 | 38 ± 9 | 88 ± 1 | <0.05 |
| SACS | 52 ± 15.7 | 10 ± 8.2 | <0.00001 |
| CS | 38 ± 15 | 95 ± 3 | <0.00001 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Romano, A.M.; Casillo, P.; De Simone, M.; Nastrucci, G.; Risorto, D.; Susanna, M.; Di Giunta, A.; Ascione, F. The Infinity-Lock System for Chronic Grade III AC Joint Dislocation: A Novel Technique, Rehabilitation Protocol and Short Term Results. J. Clin. Med. 2020, 9, 2519. https://doi.org/10.3390/jcm9082519
Romano AM, Casillo P, De Simone M, Nastrucci G, Risorto D, Susanna M, Di Giunta A, Ascione F. The Infinity-Lock System for Chronic Grade III AC Joint Dislocation: A Novel Technique, Rehabilitation Protocol and Short Term Results. Journal of Clinical Medicine. 2020; 9(8):2519. https://doi.org/10.3390/jcm9082519
Chicago/Turabian StyleRomano, Alfonso Maria, Pasquale Casillo, Monica De Simone, Guglielmo Nastrucci, Donatella Risorto, Massimiliano Susanna, Angelo Di Giunta, and Francesco Ascione. 2020. "The Infinity-Lock System for Chronic Grade III AC Joint Dislocation: A Novel Technique, Rehabilitation Protocol and Short Term Results" Journal of Clinical Medicine 9, no. 8: 2519. https://doi.org/10.3390/jcm9082519
APA StyleRomano, A. M., Casillo, P., De Simone, M., Nastrucci, G., Risorto, D., Susanna, M., Di Giunta, A., & Ascione, F. (2020). The Infinity-Lock System for Chronic Grade III AC Joint Dislocation: A Novel Technique, Rehabilitation Protocol and Short Term Results. Journal of Clinical Medicine, 9(8), 2519. https://doi.org/10.3390/jcm9082519





