Clinical and Radiologic Outcomes of Combined Use of Biocomposite and PEEK Suture Anchors during Arthroscopic Rotator Cuff Repair: A Prospective Observational Study
Abstract
1. Introduction
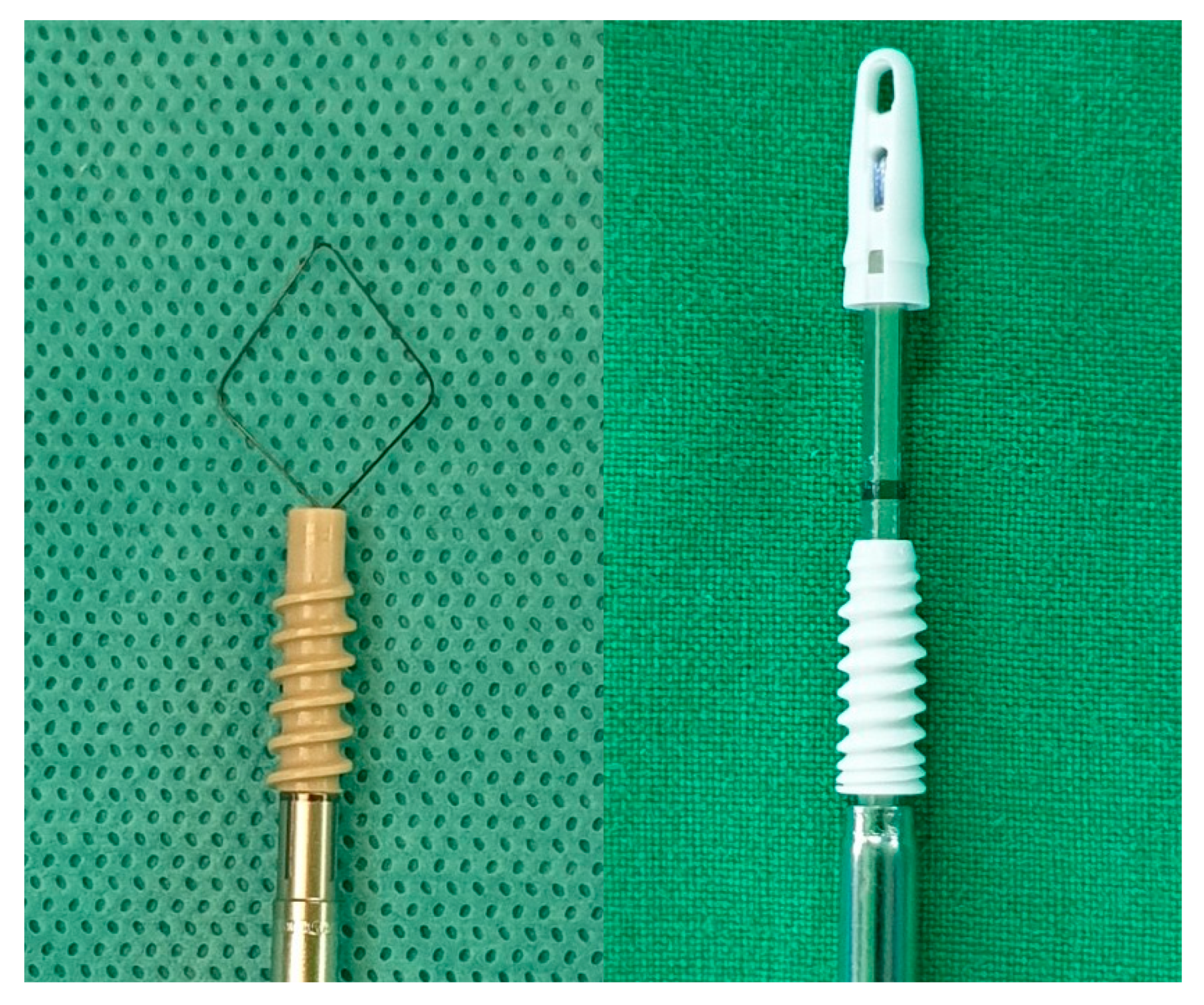
2. Materials and Methods
2.1. Patient Selection
2.2. Sample Size Calculation
2.3. Surgical Procedure and Rehabilitation
2.4. Clinical Outcome
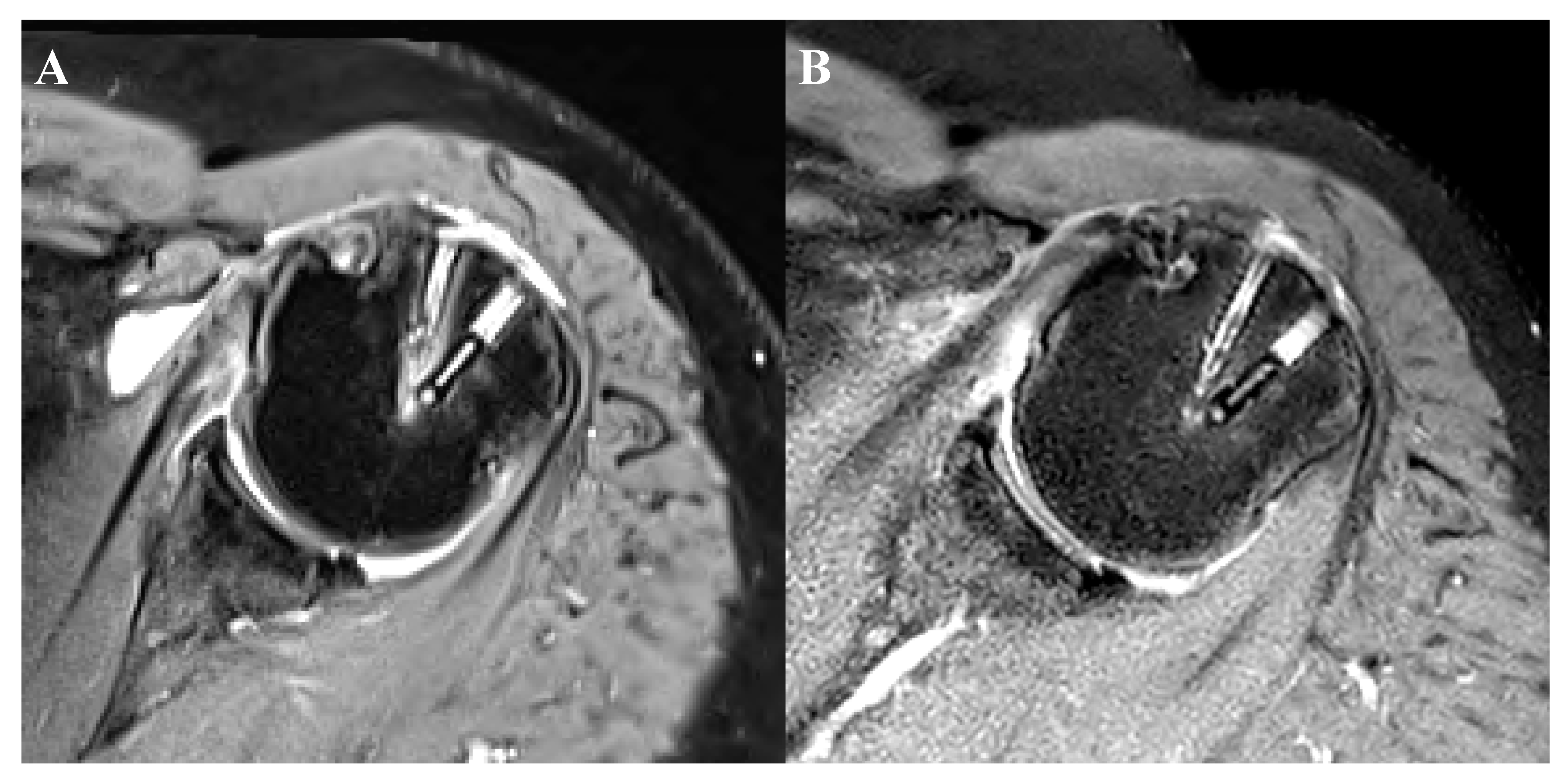
2.5. Postoperative Imaging Evaluation
2.6. Statistical Analysis
3. Results
3.1. Comparison between Biocomposite and PEEK Anchors
3.1.1. Patients’ Demographics
3.1.2. Functional Assessment
3.1.3. Radiographic Assessment
3.1.4. Perianchor Cyst Formation
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Grutter, P.W.; McFarland, E.G.; Zikria, B.A.; Dai, Z.; Petersen, S.A. Techniques for suture anchor removal in shoulder surgery. Am. J. Sports Med. 2010, 38, 1706–1710. [Google Scholar] [CrossRef] [PubMed]
- Jeong, J.H.; Shin, S.J. Arthroscopic removal of proud metallic suture anchors after Bankart repair. Arch Orthop. Trauma Surg. 2009, 129, 1109–1115. [Google Scholar] [CrossRef] [PubMed]
- Silver, M.D.; Daigneault, J.P. Symptomatic interarticular migration of glenoid suture anchors. Arthroscopy 2000, 16, 102–105. [Google Scholar] [CrossRef]
- Zlatkin, M.B. MRI of the postoperative shoulder. Skeletal Radiol. 2002, 31, 63–80. [Google Scholar] [CrossRef] [PubMed]
- Benson, E.C.; MacDermid, J.C.; Drosdowech, D.S.; Athwal, G.S. The incidence of early metallic suture anchor pullout after arthroscopic rotator cuff repair. Arthroscopy 2010, 26, 310–315. [Google Scholar] [CrossRef]
- Bostman, O.; Hirvensalo, E.; Makinen, J.; Rokkanen, P. Foreign-body reactions to fracture fixation implants of biodegradable synthetic polymers. J. Bone Joint Surg. Br. 1990, 72, 592–596. [Google Scholar] [CrossRef]
- Busfield, B.T.; Anderson, L.J. Sterile pretibial abscess after anterior cruciate reconstruction from bioabsorbable interference screws: A report of 2 cases. Arthroscopy 2007, 23, 911. [Google Scholar] [CrossRef]
- Mastrokalos, D.S.; Paessler, H.H. Allergic reaction to biodegradable interference poly-L-lactic acid screws after anterior cruciate ligament reconstruction with bone-patellar tendon-bone graft. Arthroscopy 2008, 24, 732–733. [Google Scholar] [CrossRef]
- Weiler, A.; Helling, H.J.; Kirch, U.; Zirbes, T.K.; Rehm, K.E. Foreign-body reaction and the course of osteolysis after polyglycolide implants for fracture fixation: Experimental study in sheep. J. Bone Joint Surg. Br. 1996, 78, 369–376. [Google Scholar] [CrossRef]
- Galatz, L.M.; Ball, C.M.; Teefey, S.A.; Middleton, W.D.; Yamaguchi, K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J. Bone Joint Surg. Am. 2004, 86, 219–224. [Google Scholar] [CrossRef]
- Burkhart, S.S.; Danaceau, S.M.; Pearce, C.E., Jr. Arthroscopic rotator cuff repair: Analysis of results by tear size and by repair technique-margin convergence versus direct tendon-to-bone repair. Arthroscopy 2001, 17, 905–912. [Google Scholar] [CrossRef]
- Barber, F.A.; Spenciner, D.B.; Bhattacharyya, S.; Miller, L.E. Biocomposite Implants Composed of Poly(Lactide-co-Glycolide)/beta-Tricalcium Phosphate: Systematic Review of Imaging, Complication, and Performance Outcomes. Arthroscopy 2017, 33, 683–689. [Google Scholar] [CrossRef]
- Yang, I.; Kim, S.; Kang, H.; Lee, H.; Kwon, J.; Kim, S. A Study on Evaluation of Bioabsorbable Anchor (PLGA + β-TCP) Through Mechanical Test under Moisture Difference1. J. Med. Devices 2016, 10. [Google Scholar] [CrossRef]
- Kim, S.H.; Oh, J.H.; Lee, O.S.; Lee, H.R.; Hargens, A.R. Postoperative imaging of bioabsorbable anchors in rotator cuff repair. Am. J. Sports Med. 2014, 42, 552–557. [Google Scholar] [CrossRef] [PubMed]
- Park, M.C.; Elattrache, N.S.; Ahmad, C.S.; Tibone, J.E. “Transosseous-equivalent” rotator cuff repair technique. Arthroscopy 2006, 22, 1360. [Google Scholar] [CrossRef] [PubMed]
- Park, J.G.; Cho, N.S.; Song, J.H.; Baek, J.H.; Jeong, H.Y.; Rhee, Y.G. Rotator Cuff Repair in Patients over 75 Years of Age: Clinical Outcome and Repair Integrity. Clin. Orthop. Surg. 2016, 8, 420–427. [Google Scholar] [CrossRef] [PubMed]
- Haneveld, H.; Hug, K.; Diederichs, G.; Scheibel, M.; Gerhardt, C. Arthroscopic double-row repair of the rotator cuff: A comparison of bio-absorbable and non-resorbable anchors regarding osseous reaction. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 1647–1654. [Google Scholar] [CrossRef]
- Sugaya, H.; Maeda, K.; Matsuki, K.; Moriishi, J. Repair integrity and functional outcome after arthroscopic double-row rotator cuff repair. A prospective outcome study. J. Bone Joint Surg. Am. 2007, 89, 953–960. [Google Scholar] [CrossRef]
- DeOrio, J.K.; Cofield, R.H. Results of a second attempt at surgical repair of a failed initial rotator-cuff repair. J. Bone Joint Surg. Am. 1984, 66, 563–567. [Google Scholar] [CrossRef]
- Cho, N.S.; Yi, J.W.; Lee, B.G.; Rhee, Y.G. Retear patterns after arthroscopic rotator cuff repair: Single-row versus suture bridge technique. Am. J. Sports Med. 2010, 38, 664–671. [Google Scholar] [CrossRef] [PubMed]
- Goutallier, D.; Postel, J.M.; Bernageau, J.; Lavau, L.; Voisin, M.C. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin. Orthop. Relat. Res. 1994, 304, 78–83. [Google Scholar]
- Fuchs, B.; Weishaupt, D.; Zanetti, M.; Hodler, J.; Gerber, C. Fatty degeneration of the muscles of the rotator cuff: Assessment by computed tomography versus magnetic resonance imaging. J. Shoulder Elbow Surg. 1999, 8, 599–605. [Google Scholar] [CrossRef]
- Cho, N.S.; Rhee, Y.G. The Factors Affecting the Clinical Outcome and Integrity of Arthroscopically Repaired Rotator Cuff Tears of the Shoulder. Clin. Orthop. Surg. 2009, 1, 96–104. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.H.; Kim, D.Y.; Kwon, J.E.; Park, J.S.; Oh, J.H. Perianchor Cyst Formation Around Biocomposite Biodegradable Suture Anchors After Rotator Cuff Repair. Am. J. Sports Med. 2015, 43, 2907–2912. [Google Scholar] [CrossRef]
- Chung, S.W.; Oh, K.S.; Kang, S.J.; Yoon, J.P.; Kim, J.Y. Clinical Outcomes of Arthroscopic Rotator Cuff Repair Using Poly Lactic-co-glycolic Acid Plus β-tricalcium Phosphate Biocomposite Suture Anchors. Clin. Shoulder Elbow 2018, 21, 22–29. [Google Scholar] [CrossRef]
- Ro, K.; Pancholi, S.; Son, H.S.; Rhee, Y.G. Perianchor Cyst Formation After Arthroscopic Rotator Cuff Repair Using All-Suture-Type, Bioabsorbable-Type, and PEEK-Type Anchors. Arthroscopy 2019, 35, 2284–2292. [Google Scholar] [CrossRef] [PubMed]
- Chung, S.W.; Lee, Y.-S.; Kim, J.-Y.; Lee, J.-H.; Ki, S.-Y.; Oh, K.-S.; Yoon, J.P.; Kim, J.Y. Changes in Perianchor Cyst Formation Over Time After Rotator Cuff Repair: Influential Factors and Outcomes. Am. J. Sports Med. 2019, 47, 165–172. [Google Scholar] [CrossRef]
- Kim, J.-H.; Kim, Y.-S.; Park, I.; Lee, H.-J.; Han, S.-Y.; Jung, S.; Shin, S.-J. A Comparison of Open-Construct PEEK Suture Anchor and Non-Vented Biocomposite Suture Anchor in Arthroscopic Rotator Cuff Repair: A Prospective Randomized Clinical Trial. Arthroscopy 2020, 36, 389–396. [Google Scholar] [CrossRef]
- Vonhoegen, J.; John, D.; Hagermann, C. Osteoconductive resorption characteristics of a novel biocomposite suture anchor material in rotator cuff repair. J. Orthop. Surg. Res. 2019, 14, 12. [Google Scholar] [CrossRef]
| 29 Patients in Total | |
|---|---|
| Gender (male–female (%)) | 11 (37.9):18 (62.1) |
| Age (mean (range, SD)) | 57.8 (27–74, 9.0) |
| Involvement of dominant extremity (%) | 20 (69%) |
| History of trauma (%) | 10 (34.5%) |
| Occupation (%) | |
| Manual labourer | 3 (10.3) |
| Indoor office worker | 10 (34.5) |
| Unemployed | 10 (34.5) |
| Others | 6 (20.7) |
| Regular physical activity (%) | 6 (20.7) |
| Smoking | 4 (13.8) |
| Diabetes mellitus | 7 (24.1) |
| Osteoporosis (n (%), mean bone mineral density) | 5 (17.2%), −3.16 |
| Thyroid disease | 5 (17.2) |
| Previous history of steroid injection | 12 (41.4) |
| Preoperative | Postoperative at 3 Months | Postoperative at 6 Months | p-Value | |
|---|---|---|---|---|
| Mean (Range, SD) | ||||
| pVAS | 5.6 (1–10, 2.1) | 3.2 (0–6, 1.5) | 2.6 (1–5, 0.9) | 0.001 * |
| SST | 4.7 (0–10, 2.7) | 6.4 (3–9, 1.7) | 7.5 (4–9, 1.6) | 0.005 * |
| UCLA | 17.1 (3–34, 6.6) | 21.6 (10–30, 5.7) | 24 (15–30, 5.1) | 0.001 * |
| ASES | 53.6 (11.9–90, 20.7) | 72.5 (49.1–89.1, 11.7) | 79.1 (59.1–90, 7.3) | <0.001 * |
| CSS | 45.6 (14–82,18.5) | 54.8 (25–79, 14.3) | 60.7(35–79, 12.1) | 0.004 * |
| Range of motion | ||||
| Forward extension | 154.31 (0–180, 41.1) | 165.4 (100–180, 27) | 173.3 (90–180, 21.4) | 0.137 |
| External rotation | 63.3 (10–90, 23.5) | 75.4 (40–90, 14.8) | 85 (60–90, 9.2) | 0.001 * |
| Internal rotation | 7 (T11, 1–15, 5.9) | 2.32 (L3–4, 1–15, 2.9) | 6.4 (T11–12, 1–15, 6.4) | 0.752 |
| Total 29 Patients | |
|---|---|
| Tear pattern (n, (%)) | |
| Full thickness | 24 (82.8) |
| Partial thickness-bursal | 3 (10.3) |
| Partial thickness-articular | 2 (6.9) |
| Muscle Involvement | |
| Supraspinatus only | 16 (55.2) |
| Supraspinatus and infraspinatus | 4 (13.8) |
| Surpraspinatus + subscapularis | 5 (17.2) |
| Supraspinatus and infraspinatus + subscapularis | 4 (13.8) |
| Tear size of supraspinatus (mean, (range, SD)) | 18.7 (5–50, 11.8) |
| Degree of fatty infiltration (grade, (%)) | |
| Grade 0 | 1 (3.4) |
| Grade 1 | 8 (27.6) |
| Grade 2 | 10 (34.5) |
| Grade 3 | 4 (13.8) |
| Grade 4 | 6 (20.7) |
| Biceps lesion (n, (%)) | 9 (31) |
| Capsulitis | 3 (10.3) |
| Anchor Placement (Biocomposite/PEEK), n (%) | ||||||
|---|---|---|---|---|---|---|
| Anterior | 21 (72.4)/8 (27.6) | |||||
| Posterior | 8 (27.6)/21 (72.4) | |||||
| Cyst formation, n (%) | 3 months | p-value | 6 months | p-value | ||
| Biocomposite | PEEK | Biocomposite | PEEK | |||
| Grade 0 | 8 (27.6) | 12 (41.4) | 0.085 | 7 (24.1) | 8 (27.6) | 0.581 |
| Grade 1 | 7 (24.1) | 11 (37.9) | 11 (37.9) | 11 (37.9) | ||
| Grade 2 | 6 (20.7) | 1 (3.4) | 5 (17.2) | 6 (20.7) | ||
| Grade 3 | 5 (17.2) | 4 (13.8) | 3 (10.3) | 4 (13.8) | ||
| Grade 4 | 3 (10.3) | 1 (3.4) | 3 (10.3) | - | ||
| Low grade (grade 0 or 1) | 15 (51.7) | 23 (79.3) | 0.028 * | 18 (62.1) | 19 (65.5) | 0.787 |
| High grade (grade 2, 3, or 4) | 14 (48.3) | 6 (20.7) | 11 (37.9) | 10 (34.5) | ||
| Anchor absorption | none | none | none | none | ||
| Retear, n (%) | 4 (13.8) | 4 (13.8) | ||||
| Retear pattern (type I/II) | 0/4 | 0/4 | ||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.-H.; Lee, Y.-B. Clinical and Radiologic Outcomes of Combined Use of Biocomposite and PEEK Suture Anchors during Arthroscopic Rotator Cuff Repair: A Prospective Observational Study. J. Clin. Med. 2020, 9, 2545. https://doi.org/10.3390/jcm9082545
Lee J-H, Lee Y-B. Clinical and Radiologic Outcomes of Combined Use of Biocomposite and PEEK Suture Anchors during Arthroscopic Rotator Cuff Repair: A Prospective Observational Study. Journal of Clinical Medicine. 2020; 9(8):2545. https://doi.org/10.3390/jcm9082545
Chicago/Turabian StyleLee, Jae-Hoo, and Yong-Beom Lee. 2020. "Clinical and Radiologic Outcomes of Combined Use of Biocomposite and PEEK Suture Anchors during Arthroscopic Rotator Cuff Repair: A Prospective Observational Study" Journal of Clinical Medicine 9, no. 8: 2545. https://doi.org/10.3390/jcm9082545
APA StyleLee, J.-H., & Lee, Y.-B. (2020). Clinical and Radiologic Outcomes of Combined Use of Biocomposite and PEEK Suture Anchors during Arthroscopic Rotator Cuff Repair: A Prospective Observational Study. Journal of Clinical Medicine, 9(8), 2545. https://doi.org/10.3390/jcm9082545






