What Determines Spontaneous Physical Activity in Patients with Parkinson’s Disease?
Abstract
1. Introduction
2. Material and Methods
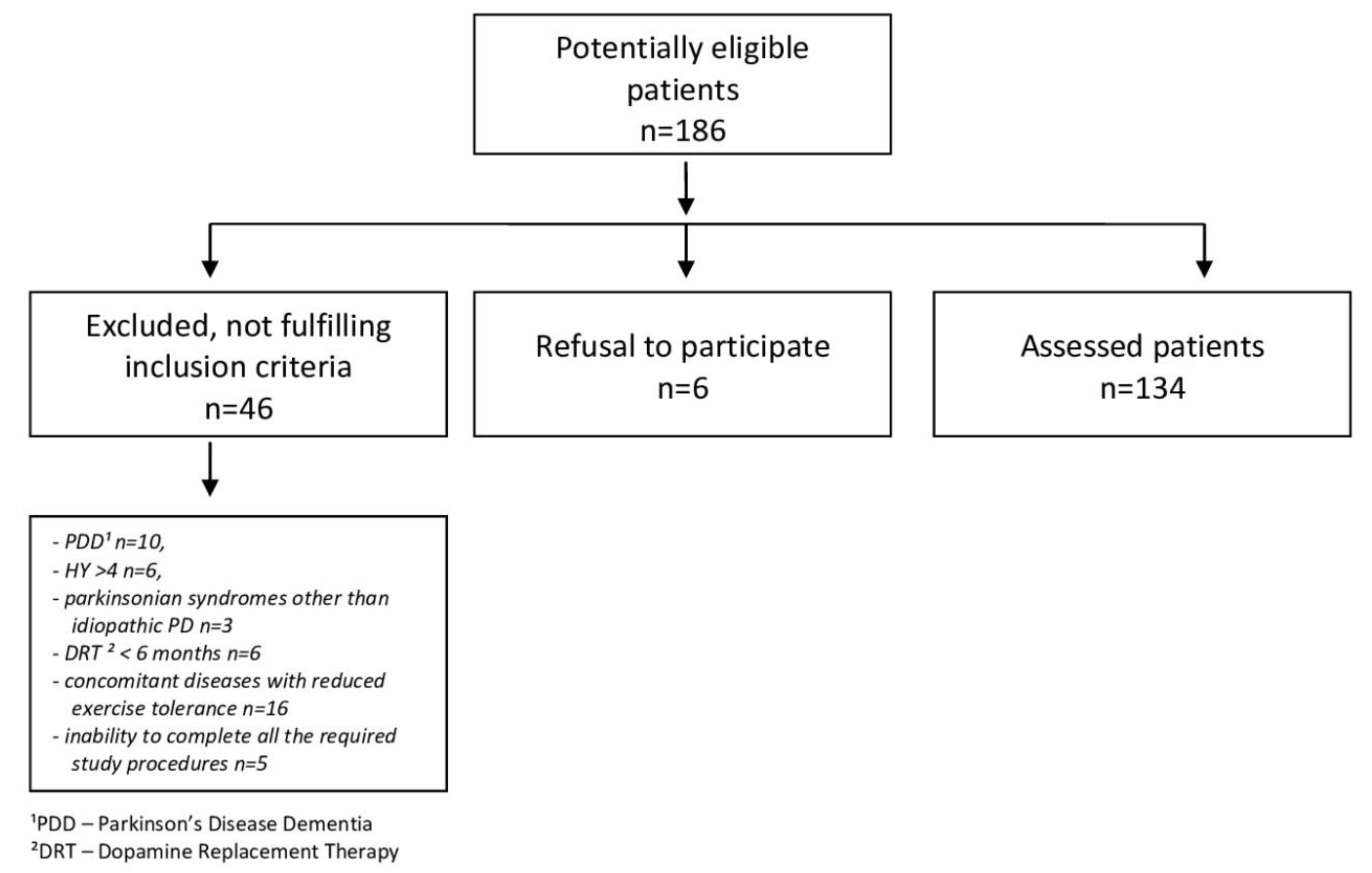
2.1. Subjects
2.2. Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Conflicts of Interest
References
- Elbaz, A.; Carcaillon, L.; Kab, S.; Moisan, S. Epidemiology of Parkinson’s disease. Rev. Neurol. 2016, 172, 14–26. [Google Scholar] [CrossRef] [PubMed]
- He, R.; Yan, X.; Guo, J.; Xu, Q.; Tang, B.; Sun, Q. Recent Advances in Biomarkers for Parkinson’s Disease. Front. Aging Neurosci. 2018, 10, 305. [Google Scholar] [CrossRef] [PubMed]
- Mantri, S.; Fullard, M.E.; Duda, J.E.; Morley, J.F. Physical Activity in Early Parkinson Disease. J. Parkinsons Dis. 2018, 8, 107–111. [Google Scholar] [CrossRef] [PubMed]
- Hidalgo-Agudo, R.D.; Lucena-Anton, D.; Luque-Moreno, C.; Heredia-Rizo, A.M.; Moral-Munoz, J.A. Additional Physical Interventions to Conventional Physical Therapy in Parkinson’s Disease: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. J. Clin. Med. 2020, 9, 1038. [Google Scholar] [CrossRef] [PubMed]
- Cholewa, J.; Gorzkowska, A.; Nawrocka, A.; Cholewa, J. Quality of life of people with Parkinson’s disease in the context of professional work and physiotherapy. Med. Pr. 2017, 68, 725–734. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Stuart, S.; Vitorio, R.; Morris, R.; Martini, D.N.; Fino, P.C.; Mancini, M. Cortical activity during walking and balance tasks in older adults and in people with Parkinson’s disease: A structured review. Maturitas 2018, 113, 53–72. [Google Scholar] [CrossRef]
- Monteiro-Junior, R.S.; Cevada, T.; Oliveira, B.R.; Lattari, E.; Portugal, E.M.; Carvalho, A.; Deslandes, A.C. We need to move more: Neurobiological hypotheses of physical exercise as a treatment for Parkinson’s disease. Med. Hypotheses 2015, 85, 537–541. [Google Scholar] [CrossRef]
- Schmolesky, M.T.; Webb, D.L.; Hansen, R.A. The effects of aerobic exercise intensity and duration on levels of brain-derived neurotrophic factor in healthy men. J. Sports Sci. Med. 2013, 12, 502–511. [Google Scholar]
- Rodriguez-Nogales, C.; Garbayo, E.; Carmona-Abellán, M.M.; Luquin, M.R.; Blanco-Prieto, M.J. Brain aging and Parkinson’s disease: New therapeutic approaches using drug delivery systems. Maturitas 2016, 84, 25–31. [Google Scholar] [CrossRef]
- Tomlinson, C.L.; Stowe, R.; Patel, S.; Rick, C.; Gray, R.; Clarke, C.E. Systematic review of levodopa dose equivalency reporting in Parkinson’s disease. Mov. Disord. 2010, 25, 2649–2653. [Google Scholar] [CrossRef]
- Hoehn, M.M.; Yahr, M.Y. Parkinsonism: Onset, progression and mortality. Neurology 1967, 17, 427–442. [Google Scholar] [CrossRef] [PubMed]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Hallal, P.C.; Victora, C.G. Reliability and validity of the International Physical Activity Questionnaire (IPAQ). Med. Sci. Sports. Exerc. 2004, 36, 556. [Google Scholar] [CrossRef] [PubMed]
- Folsom, A.R.; Jacobs, D.R.; Caspersen, C.J.; Gomez-Marin, O.; Knudsen, J. Test-retest reliability of the Minnesota Leisure Time Physical Activity Questionnaire. J. Chronic Dis. 1986, 39, 505–511. [Google Scholar] [CrossRef]
- Biernat, E.; Piatkowska, M. Leisure-Time Physical Activity Participation Trends 2014–2018: A Cross-Sectional Study in Poland. Int. J. Environ. Res. Public Health 2020, 17, 208. [Google Scholar] [CrossRef]
- Beck, A.T.; Ward, C.H.; Mendelson, M.; Mock, J.; Erbaugh, J. An inventory for measuring depression. Arch. Gen. Psychiatry 1961, 4, 561–571. [Google Scholar] [CrossRef]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef]
- Starkstein, S.E.; Mayberg, H.S.; Preziosi, T.J.; Andrezejewski, P.; Leiguarda, R.; Robinson, R.G. Reliability, validity, and clinical correlates of apathy in Parkinson’s disease. J. Neuropsychiatry Clin. Neurosci. 1992, 4, 134–139. [Google Scholar]
- Brown, R.G.; Dittner, A.; Findley, L.; Wessely, S.C. The Parkinson fatigue scale. Parkinsonism Relat. Disord. 2005, 11, 49–55. [Google Scholar] [CrossRef]
- Nilsson, M.H.; Bladh, S.; Hagell, P. Fatigue in Parkinson’s Disease: Measurement Properties of a Generic and a Condition-specific Rating Scale. J. Pain Symptom Manag. 2013, 46, 737–746. [Google Scholar] [CrossRef]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Johns, M.W. A new method for measuring daytime sleepiness: The Epworth sleepiness scale. Sleep 1991, 14, 540–545. [Google Scholar] [CrossRef] [PubMed]
- Dontje, M.L.; de Greef, M.H.; Speelman, A.D.; van Nimwegen, M.; Krijnen, W.P.; Stolk, R.P.; Kamsma, Y.P.; Bloem, B.R.; Munneke, M.; van der Schans, C.P. Quantifying daily physical activity and determinants in sedentary patients with Parkinson’s disease. Parkinsonism Relat. Disord. 2013, 19, 878–882. [Google Scholar] [CrossRef] [PubMed]
- Brownlee, K. The Competent Judge Problem. Ratio 2016, 29, 312–326. [Google Scholar] [CrossRef]
- Cusso, M.E.; Donald, K.J.; Khoo, T.K. The Impact of Physical Activity on Non-Motor Symptoms in Parkinson’s Disease: A Systematic Review. Front. Med. 2016, 17, 35. [Google Scholar] [CrossRef]
- Cugusi, L.; Solla, P.; Zedda, F.; Loi, M.; Serpe, R.; Cannas, A.; Marrosu, F.; Mercuro, G. Effects of an adapted physical activity program on motor and non-motor functions and quality of life in patients with Parkinson’s disease. NeuroRehabilitation 2014, 35, 789–794. [Google Scholar] [CrossRef]
- Coe, S.; Franssen, M.; Collett, J.; Boyle, D.; Meaney, A.; Chantry, R.; Esser, P.; Izadi, H.; Dawes, H. Physical Activity, Fatigue, and Sleep in People with Parkinson’s Disease: A Secondary per Protocol Analysis from an Intervention Trial. Parkinsons Dis. 2018, 6, 1517807. [Google Scholar] [CrossRef]
- Cutler, D.M.; Lleras-Muney, A. Understanding differences in health behaviors by education. J. Health Econ. 2010, 29, 1–28. [Google Scholar] [CrossRef]
- Ogwumike, O.O.; Kaka, B.; Adegbemigun, O.; Abiona, T. Health-related and socio-demographic correlates of physical activity level amongst urban menopausal women in Nigeria. Maturitas 2012, 73, 349–353. [Google Scholar] [CrossRef]
- Cai, G.; Huang, Y.; Luo, S.; Lin, Z.; Dai, H.; Ye, Q. Continuous quantitative monitoring of physical activity in Parkinson’s disease patients by using wearable devices: A case-control study. Neurol. Sci. 2017, 38, 1657–1663. [Google Scholar] [CrossRef]
- Vitale, C.; Santangelo, G.; Verde, F.; Amboni, M.; Sorrentino, G.; Grossi, D.; Barone, P. Exercise dependence induced by pramipexole in Parkinson’s Disease-a case report. Mov. Disord. 2010, 25, 2893–2894. [Google Scholar] [CrossRef] [PubMed]
- Hearty, T.M.; Schenkman, M.L.; Kohrt, W.M.; Cress, M.E. Continuous scale physical functional performance test: Appropriateness for middle-aged adults with and without Parkinson’s disease. J. Neurol. Phys. Ther. 2007, 31, 64–70. [Google Scholar] [CrossRef] [PubMed]
| Variable | M (SD) | |
|---|---|---|
| Sex: Women/Men (n) | 61/73 | |
| Age (years) | 65.2 (9.2) | |
| Place of residence (%) | A city with over 100 thousand inhabitants. A city with fewer than 100 thousand inhabitants. | 60.5 39.5 |
| Marital status (%) | Married Single | 83.6 16.4 |
| Education (%) | Basic Professional Medium High | 7.5 20.9 41.0 30.6 |
| Accompanying conditions (%) | 84.3 | |
| The age of the start of symptoms (years) EOPD/MOPD/LOPD (%) | 57.9 (11.1) 21.6/66.4/12.7 | |
| The duration of the disease (years) | 7.3 (4.2) | |
| Hoehn–Yahr scale (degrees) | 2 (0.6) | |
| Time to start treatment (years) | 1.4 (1.5) | |
| Daily levodopa equivalent dose—LED (mg) | 755.4 (418.7) | |
| Levodopa/dopaminergic agonist (%) | 96/52 | |
| Variable | PA-G (n = 55) | PI-G (n = 53) | p Value |
|---|---|---|---|
| Age (years) | 66.3 ± 8.1 | 65.5 ± 10.0 | 0.516 1 |
| Sex (W—women, M—Men) | W—45.5% (n = 25 M—54.5% (n = 30) | W—47.2% (n = 25) M—52.8% (n = 28) | 0.858 2 |
| The duration of the disease (years) | 6.3 ± 4.0 | 8.2 ± 4.2 | p < 0.01 1 |
| Age of onset of (years) | 65.4 ±8.1 | 66.3 ±10.0 | 0.622 1 |
| UPDRS I (points) | 1.3 ± 1.9 | 1.6 ± 1.4 | 0.405 1 |
| UPDRS II (points) | 7.0 ± 5.7 | 9.2 ± 5.5 | p < 0.05 1 |
| UPDRS III (points) | 24.9 ± 12.5 | 27.1 ± 13.0 | 0.246 1 |
| UPDRS IV (points) | 1.8 ± 1.7 | 2.3 ± 2.8 | 0.381 1 |
| Hoehn–Yahr scale (degree) | 2.2 ± 0.6 | 2.4 ± 0.6 | 0.055 1 |
| Dyskinesia (%) | 20.0 (n = 11) | 24.5 (n = 13) | 0.218 |
| Motor fluctuation (%) | 38.2 (n = 21) | 45.3 (n = 24) | 0.946 |
| Treatment: levodopa/DA (%) | 96.4 (n = 53) | 98.1 (n = 52) | 0.580 2 |
| Start of treatment with levodopa (%) | 74.5 (n = 41) | 83.0 (n = 44) | 0.282 2 |
| Start of treatment with DA (%) | 21.8 (n = 12) | 1.9 (n = 1) | p < 0.01 2 |
| Time to initiate treatment (years) | 1.3 ± 1.4 | 1.0 ± 1.5 | 0.212 1 |
| LED (mg) | 730.4 ± 433.4 | 797.6 ± 414.7 | 0.177 1 |
| Current Levodopa dose (mg) | 674.5 ± 410.9 | 746.1 ± 387.3 | 0.710 |
| Depression BDI (M ± SD) (% with depression) | 9.5 ± 6.4 23.6 (n = 13) | 11.9 ± 8.6 35.8 (n = 19) | 0.287 1 |
| Depression HADS (M ± SD) (% with depression) | 4.9 ± 3.7 20.0 (n = 11) | 5.3 ± 3.7 26.4 (n = 14) | 0.462 1 |
| Anxiety HADS (M ± SD) (% with anxiety) | 5.7 ± 3.9 29.1 (n = 16) | 5.1 ± 3.4 24.5 (n = 13) | 0.517 1 |
| Apathy AS (M ± SD) (% with apathy) | 13.2 ± 5.4 49.1 (n = 27) | 15.9 ± 5.6 63.5 (n = 33) | p < 0.05 1 |
| Fatigue PFS−16 (M ± SD) (% with fatigue) | 2.8 ±0.9 27.3 (n = 15) | 3.1 ±1.0 45.3 (n = 24) | 0.078 1 |
| Sleep disorders PSQI (M ± SD) (% with sleep disorders) | 6.4 ± 3.3 56.4 (n = 31) | 6.2 ± 3.6 52.8 (n = 28) | 0.634 1 |
| Excessive daytime sleepiness ESS (M ± SD) (% with excessive daytime sleepiness) | 6.3 ± 4.9 21.8 (n = 12) | 7.7 ± 5.3 39.6 (n = 21) | 0.167 1 |
| Depended Variable | Model | Predictors | R2 | F | p | ϐ | t | p |
|---|---|---|---|---|---|---|---|---|
| ITMWA | Complete model | Sex | R2 = 0.125; F(16,133) = 2.185; p < 0.01 | 0.007 | 0.083 | 0.934 | ||
| Age | 0.041 | 0.452 | 0.652 | |||||
| Professional education | 0.141 | 0.944 | 0.347 | |||||
| Medium education | 0.092 | 0.551 | 0.582 | |||||
| High education | 0.206 | 1.266 | 0.208 | |||||
| Levodopa treatment | 0.138 | 1.493 | 0.138 | |||||
| DA treatment | 0.033 | 0.364 | 0.717 | |||||
| MAOBI treatment | −0.047 | −0.547 | 0.585 | |||||
| Amantadine treatment | 0.010 | 0.119 | 0.905 | |||||
| Anticholinergic treatment | 0.004 | 0.044 | 0.965 | |||||
| Start of treatment with levodopa | 0.157 | 1.483 | 0.141 | |||||
| Start of treatment with DA | 0.420 | 4.068 | 0.000 | |||||
| LED | −0.087 | −0.892 | 0.374 | |||||
| Hoehn–Yahr scale | −0.210 | −1.821 | 0.071 | |||||
| UPDRS part III | 0.352 | 1.181 | 0.240 | |||||
| UPDRS part I + II + III | −0.242 | −0.785 | 0.434 | |||||
| Optimal model highest value R2 | Higher Education | R2 = 0.171; F(6.133) = 5.585; p < 0.001 | 0.105 | 1.261 | 0.210 | |||
| Levodopa treatment | 0.120 | 1.421 | 0.158 | |||||
| Start of treatment with Levodopa | 0.153 | 1.537 | 0.127 | |||||
| Start of treatment with DA | 0.440 | 4.595 | 0.000 | |||||
| Hoehn–Yahr scale | −0.238 | −2.283 | 0.024 | |||||
| UPDRS part III | 0.144 | 1.400 | 0.164 | |||||
| Depended Variable | Model | Predictors | R2 | F | p | ϐ | t | p |
|---|---|---|---|---|---|---|---|---|
| Time spent in the sedentary position | Complete model | Sex | R2 = 0.135; F(16.130) = 2.267; p < 0.01 | −0.013 | −0.149 | 0.882 | ||
| Age | 0.070 | 0.768 | 0.444 | |||||
| Professional education | −0.262 | −1.787 | 0.077 | |||||
| Medium education | −0.339 | −2.026 | 0.045 | |||||
| High education | −0.198 | −1.218 | 0.226 | |||||
| Levodopa treatment | 0.017 | 0.178 | 0.859 | |||||
| DA treatment | 0.007 | 0.077 | 0.939 | |||||
| MAOBI treatment | 0.126 | 1.461 | 0.147 | |||||
| Amantadine treatment | 0.032 | 0.376 | 0.708 | |||||
| Anticholinergic treatment | −0.002 | −0.025 | 0.980 | |||||
| Start of treatment with levodopa | 0.007 | 0.062 | 0.951 | |||||
| Start of treatment with DA | −0.151 | −1.457 | 0.148 | |||||
| LED | −0.029 | −0.290 | 0.772 | |||||
| Hoehn–Yahr scale | −0.006 | −0.052 | 0.958 | |||||
| UPDRS part III | −0.817 | −2.705 | 0.008 | |||||
| UPDRS part. I + II + III | 1.047 | 3.362 | 0.001 | |||||
| Optimal model highest value R2 | Professional education | R2 = 0.171; F(6.133) = 5.585; p < 0.001 | −0.289 | −2.124 | 0.036 | |||
| Medium education | −0.362 | −2.320 | 0.022 | |||||
| Higher education | −0.213 | −1.388 | 0.168 | |||||
| Treatment MAOBI | 0.125 | 1.541 | 0.126 | |||||
| Start of treatment with DA | −0.162 | −1.996 | 0.048 | |||||
| UPDRS part III | −0.813 | −2.849 | 0.005 | |||||
| Optimal Model | Predictors | R2 | F | p | ϐ | t | p |
|---|---|---|---|---|---|---|---|
| ITMWA | Duration of the disease | R2 = 0.151; F(3.133) = 8.85; p < 0.001 | −0.114 | −1.379 | 0.170 | ||
| Start of treatment with DA | 0.348 | 4.306 | 0.000 | ||||
| Hoehn–Yahr scale | −0.105 | −1.273 | 0.205 | ||||
| Time spent in the sedentary position | Medium education | R2 = 0.195; F(7.130) = 5.509; p < 0.001 | −0.375 | −2.407 | 0.018 | ||
| Professional education | −0.294 | −2.172 | 0.032 | ||||
| Higher education | −0.202 | −1.322 | 0.188 | ||||
| UPDRS part. III | −0.589 | −1.939 | 0.055 | ||||
| UPDRS parts I + II + III | 0.787 | 2.535 | 0.013 | ||||
| Start of treatment with DA | −0.177 | −2.190 | 0.030 | ||||
| ESS | 0.147 | 1.677 | 0.096 | ||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gorzkowska, A.; Cholewa, J.; Małecki, A.; Klimkowicz-Mrowiec, A.; Cholewa, J. What Determines Spontaneous Physical Activity in Patients with Parkinson’s Disease? J. Clin. Med. 2020, 9, 1296. https://doi.org/10.3390/jcm9051296
Gorzkowska A, Cholewa J, Małecki A, Klimkowicz-Mrowiec A, Cholewa J. What Determines Spontaneous Physical Activity in Patients with Parkinson’s Disease? Journal of Clinical Medicine. 2020; 9(5):1296. https://doi.org/10.3390/jcm9051296
Chicago/Turabian StyleGorzkowska, Agnieszka, Joanna Cholewa, Andrzej Małecki, Aleksandra Klimkowicz-Mrowiec, and Jarosław Cholewa. 2020. "What Determines Spontaneous Physical Activity in Patients with Parkinson’s Disease?" Journal of Clinical Medicine 9, no. 5: 1296. https://doi.org/10.3390/jcm9051296
APA StyleGorzkowska, A., Cholewa, J., Małecki, A., Klimkowicz-Mrowiec, A., & Cholewa, J. (2020). What Determines Spontaneous Physical Activity in Patients with Parkinson’s Disease? Journal of Clinical Medicine, 9(5), 1296. https://doi.org/10.3390/jcm9051296






