Characteristics of and Public Health Responses to the Coronavirus Disease 2019 Outbreak in China
Abstract
1. Introduction
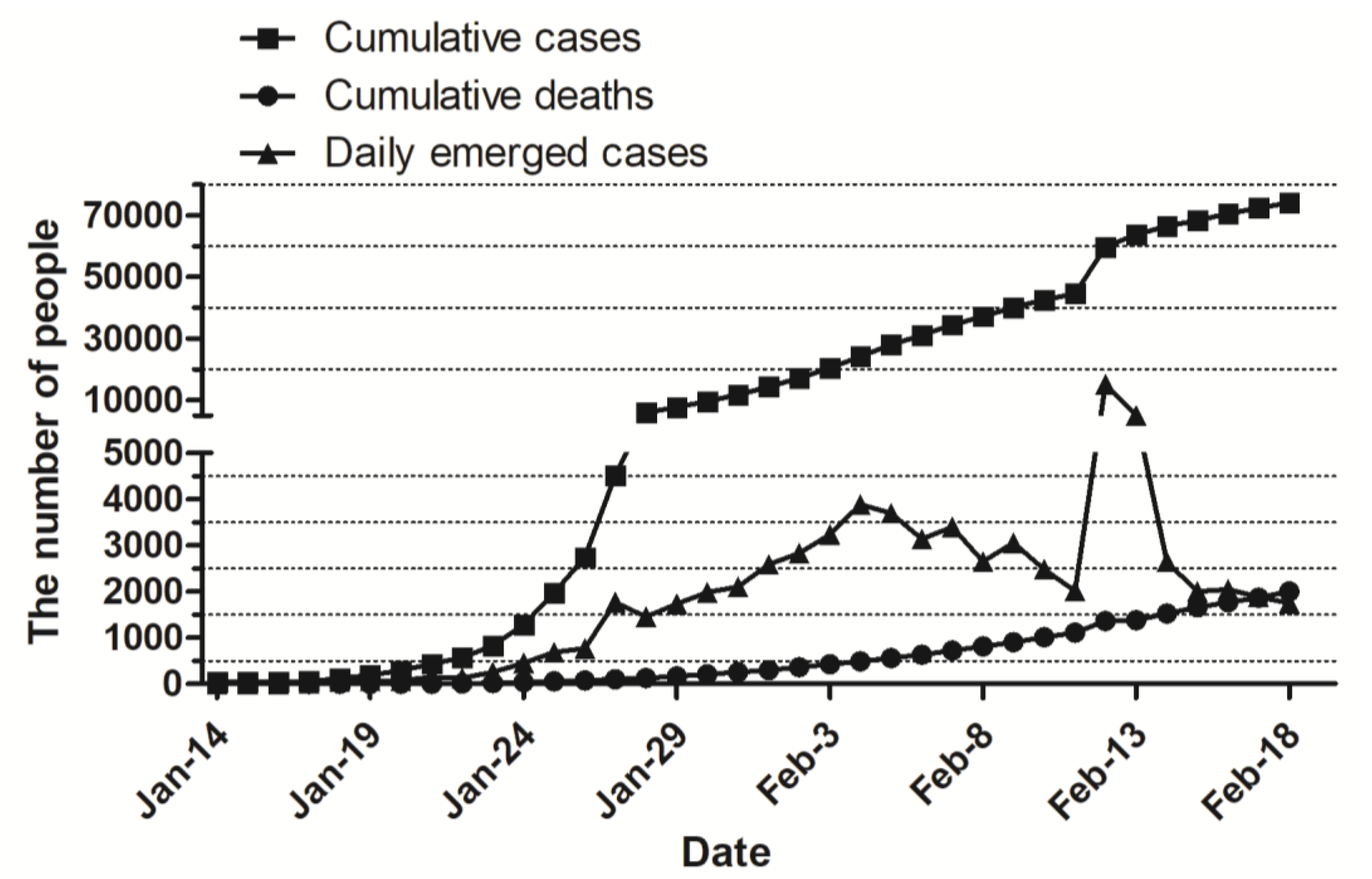
2. The Epidemiology of COVID-19
3. Pathogenic Characteristics of Coronavirus
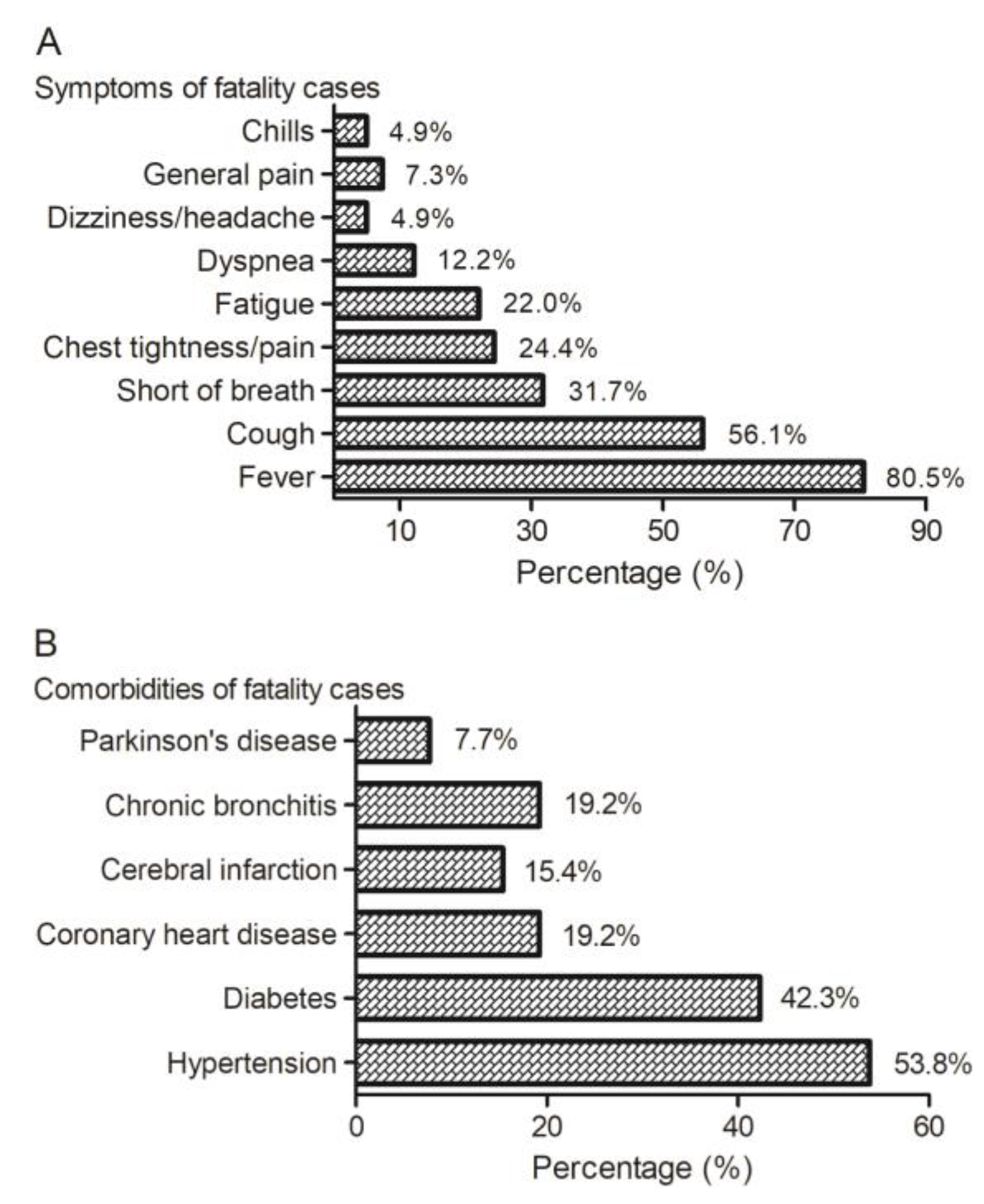
4. Clinical Characteristics of COVID-19
4.1. Clinical Manifestations
4.2. Laboratory Examination
4.3. Chest Imaging
5. Diagnosis of COVID-19
5.1. Suspected Cases
5.2. Confirmed Cases
5.3. Clinical Typing of the Confirmed Cases
6. Treatment of COVID-19
6.1. Treatment Area Decision According to the Disease Severity
6.2. General Treatment
- Bed rest, strengthen supportive treatment, ensure sufficient energy; pay attention to water-electrolytes balance and maintain the stability of the internal environment; closely monitor vital signs and finger oxygen saturation, and so on.
- Monitor the blood routine, urine routine, C-reactive protein (CRP) and health indications (liver enzyme, myocardial enzyme, renal function, etc.), coagulation function, arterial blood gas analysis if necessary, and recheck chest imaging.
- According to the change of oxygen saturation, give effective oxygen therapy in time, including oxygen given by nasal catheter or mask. If necessary, apply high flow oxygen therapy via the nose, noninvasive or invasive mechanical ventilation, and so on.
- Antiviral treatment: no effective antiviral drug at present. Treat with IFN-α aerosol inhalation (five million U per time for adults, two times per day), and/or Lopinavir/Ritonavir oral administration (two tablets per time, two times per day).
- Antibiotic treatment: avoid blind and improper use of antibiotics, especially the combination use of broad-spectrum antibiotics. Strengthen bacteriological monitoring. Antibiotics should be used in time in secondary bacterial infection.
6.3. Treatment of Severe and Critical Cases
- Treatment principle: based on symptomatic treatment, actively prevent and treat complications, treat basic diseases, prevent secondary infection, and timely apply organ function support.
- Respiratory support: apply noninvasive mechanical ventilation for two hours, if the condition is not improved, or the patient is intolerable to noninvasive ventilation, accompanied with increased airway secretions, severe coughing, or unstable hemodynamics, the patient should be transferred to invasive mechanical ventilation in time. The “lung-protective ventilation strategy” with low tidal volume should be adopted in invasive mechanical ventilation to reduce ventilator-associated lung injury. If necessary, ventilation in the prone position, recruitment maneuver, or extracorporeal membrane oxygenation (ECMO) can be used.
- Circulation support: improve microcirculation based on full fluid resuscitation, use vasoactive drugs, and apply hemodynamic monitoring if necessary.
- Others: according to the degree of dyspnea and the progress of chest imaging, use glucocorticoids appropriately for a short time (3–5 days) with the recommended dose no more than what is equivalent to methylprednisolone 1–2 mg/kg·day.
7. Prevention and Control
8. Discussion
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Wuhan Municipal Health Commission. Report on the Current Situation of Pneumonia in Wuhan (2019-12-31). Available online: http://wjw.wuhan.gov.cn/front/web/showDetail/2019123108989 (accessed on 19 February 2020).
- Health Emergency Office. National Health Commission and Relevant Departments Jointly Prevent and Control New Coronavirus Infected Pneumonia. Available online: http://www.nhc.gov.cn/yjb/s7860/202001/d9570f3a52614113ae0093df51509684.shtml (accessed on 19 February 2020).
- Chan, J.F.; Yuan, S.; Kok, K.H.; To, K.K.; Chu, H.; Yang, J.; Xing, F.; Liu, J.; Yip, C.C.Y.; Poon, R.W.S.; et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: A study of a family cluster. Lancet 2020, 395, 514–523. [Google Scholar] [CrossRef]
- Chen, N.; Zhou, M.; Dong, X.; Qu, J.; Gong, F.; Han, Y.; Qiu, Y.; Wang, J.; Liu, Y.; Wei, Y.; et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet 2020, 395, 507–513. [Google Scholar] [CrossRef]
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A novel coronavirus from patients with pneumonia in China. N. Engl. J. Med. 2019. [Google Scholar] [CrossRef]
- Alexander, E. Gorbalenya. Severe acute respiratory syndrome-related coronavirus—The species and its viruses, a statement of the Coronavirus Study Group. bioRxiv 2020. [Google Scholar] [CrossRef]
- World Health Organization. Coronavirus disease 2019 (COVID-19) Situation Reports. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports (accessed on 19 February 2020).
- Wuhan Municipal Health Commission. Report on the Current Situation of Pneumonia in Wuhan (2020-01-05). Available online: http://wjw.wuhan.gov.cn/front/web/showDetail/2020010509020 (accessed on 19 February 2020).
- Wuhan Municipal Health Commission. Report on the Current Situation of Pneumonia in Wuhan (2020-01-11). Available online: http://wjw.wuhan.gov.cn/front/web/showDetail/2020011109035 (accessed on 19 February 2020).
- National Health Commission of the People’s Republic of China. The Latest Situation of Pneumonia Caused by Novel Corona Virus. Available online: http://www.nhc.gov.cn/xcs/yqtb/list_gzbd.shtml. (accessed on 19 February 2020).
- World Health Organization Report. Available online: https://www.who.int/csr/sars/country/table2003_09_23/en/ (accessed on 19 February 2020).
- World Health Organization. Middle East Respiratory Syndrome Coronavirus (MERS-CoV). Available online: https://www.who.int/emergencies/mers-cov/en/ (accessed on 19 February 2020).
- Cui, J.; Li, F.; Shi, Z.L. Origin and evolution of pathogenic coronaviruses. Nat. Rev. Microbiol. 2019, 17, 181–192. [Google Scholar] [CrossRef] [PubMed]
- Wong, A.C.P.; Li, X.; Lau, S.K.P.; Woo, P.C.Y. Global epidemiology of bat coronaviruses. Viruses 2019, 11, 174. [Google Scholar] [CrossRef] [PubMed]
- Kolb, A.F.; Hegyi, A.; Siddell, S.G. Identification of residues critical for the human coronavirus 229E receptor function of human aminopeptidase N. J. Gen. Virol. 1997, 78, 2795–2802. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Sui, J.; Huang, I.C.; Kuhn, J.H.; Radoshitzky, S.R.; Marasco, W.A.; Choe, H.; Farzan, M. The S proteins of human coronavirus NL63 and severe acute respiratory syndrome coronavirus bind overlapping regions of ACE2. Virology 2007, 367, 367–374. [Google Scholar] [CrossRef] [PubMed]
- Hulswit, R.J.G.; Lang, Y.; Bakkers, M.J.G.; Li, W.; Li, Z.; Schouten, A.; Ophorst, B.; van Kuppeveld, F.J.; Boons, G.J.; Bosch, B.J.; et al. Human coronaviruses OC43 and HKU1 bind to 9-O-acetylated sialic acids via a conserved receptor-binding site in spike protein domain A. Proc. Nat. Acad. Sci. USA 2019, 116, 2681–2690. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.T.; Chen, P.; Wang, J.F.; Feng, J.N.; Zhou, H.; Li, X.; Zhong, W.; Hao, P. Evolution of the novel coronavirus from the ongoing Wuhan outbreak and modeling of its spike protein for risk of human transmission. Sci. China Life Sci. 2020. [Google Scholar] [CrossRef] [PubMed]
- Knoops, K.; Kikkert, M.; Worm, S.H.; Zevenhoven-Dobbe, J.C.; van der Meer, Y.; Koster, A.J.; Mommaas, A.M.; Snijder, E.J. SARS-coronavirus replication is supported by a reticulovesicular network of modified endoplasmic reticulum. PLoS Biol. 2008, 6, e226. [Google Scholar] [CrossRef] [PubMed]
- National Health Commission of the People’s Republic of China and National Administration of Traditional Chinese Medicine. Diagnosis & Treatment Scheme for Novel Coronavirus Pneumonia (Trial) 6th Edition. Available online: http://www.nhc.gov.cn/xcs/zhengcwj/202002/8334a8326dd94d329df351d7da8aefc2.shtml (accessed on 19 February 2020).
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef]
- Global Network Report. Available online: https://baijiahao.baidu.com/s?id=1656696048015939580&wfr=spider&for=pc (accessed on 19 February 2020).
- National Health Commission of the People’s Republic of China. Technical Guide for Prevention and Control of New Coronavirus Infection in Medical Institutions (Second Edition) (2020-01-22). Available online: http://www.nhc.gov.cn/jkj/s3577/202001/c67cfe29ecf1470e8c7fc47d3b751e88.shtml (accessed on 19 February 2020).
- Zhong, N.S.; Zheng, B.J.; Li, Y.M.; Poon, L.L.M.; Xie, Z.H.; Chan, K.H.; Li, P.H.; Tan, S.Y.; Chang, Q.; Xie, J.P.; et al. Epidemiology and cause of severe acute respiratory syndrome (SARS) in Guangdong, People’s Republic of China, in February 2003. Lancet 2003, 362, 1353–1358. [Google Scholar] [CrossRef]
- Drosten, C.; Gunther, S.; Preiser, W.; van der Werf, S.; Brodt, H.R.; Becker, S.; Rabenau, H.; Panning, M.; Kolesnikova, L.; Fouchier, R.A.; et al. Identification of a novel coronavirus in patients with severe acute respiratory syndrome. N. Engl. J. Med. 2003, 348, 1967–1976. [Google Scholar] [CrossRef] [PubMed]
| Coronavirus Infection Outbreak | Total Confirm Cases | Median Age (Years Old) | Number of Deaths | Case-Fatality Rate (%) | Countries Reported Cases | References | |
|---|---|---|---|---|---|---|---|
| Female (%) | Male (%) | ||||||
| COVID-19 (November 2019–18 February 2020) | 75,199 | 55.5 * | 2009 | 2.67 11.0 * | 26 | [10] [4] | |
| 32 * | 67 * | ||||||
| SARS (November 2002–July 2003) | 8098 | 41.3 | 774 | 9.60 | 26 | WHO [11] | |
| 53.1 | 46.9 | ||||||
| MERS (April 2012–November 2019) | 2494 | 52.8 | 858 | 34.4 | 27 | WHO [12] | |
| 26.3 | 73.7 | ||||||
| Organization at all Levels | Health Administration Department | Center for Diseases Control | Medical Institutions |
|---|---|---|---|
| Objectives | To timely find and report the COVID-19 cases, understand the disease characteristics and possible sources of infection, standardize the management of close contacts, and prevent the spread of the epidemic. | ||
| Responsibilities | Overall guidance of epidemic control, organizing a technical expert group for prevention and control; formulation and improvement of relevant work and technical schemes, and implementation of funds and materials for disease prevention and control; tracking and management of close contacts. | Organization, coordination, supervision, and evaluation of the monitoring work; collection, analysis, report, and feedback of the monitoring data; epidemiological investigation; strengthening laboratory testing ability, bio-safety protection awareness, and technical training; carrying out health education and publicity and risk communication to the public. | Case detection and report, isolation, diagnosis, and treatment; clinical management and prevention and control of nosocomial infections; sample collection and detection, and training of medical staff in the institution. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Deng, S.-Q.; Peng, H.-J. Characteristics of and Public Health Responses to the Coronavirus Disease 2019 Outbreak in China. J. Clin. Med. 2020, 9, 575. https://doi.org/10.3390/jcm9020575
Deng S-Q, Peng H-J. Characteristics of and Public Health Responses to the Coronavirus Disease 2019 Outbreak in China. Journal of Clinical Medicine. 2020; 9(2):575. https://doi.org/10.3390/jcm9020575
Chicago/Turabian StyleDeng, Sheng-Qun, and Hong-Juan Peng. 2020. "Characteristics of and Public Health Responses to the Coronavirus Disease 2019 Outbreak in China" Journal of Clinical Medicine 9, no. 2: 575. https://doi.org/10.3390/jcm9020575
APA StyleDeng, S.-Q., & Peng, H.-J. (2020). Characteristics of and Public Health Responses to the Coronavirus Disease 2019 Outbreak in China. Journal of Clinical Medicine, 9(2), 575. https://doi.org/10.3390/jcm9020575





