Hydroceles of the Canal of Nuck in Adults—Diagnostic, Treatment and Results of a Rare Condition in Females
Abstract
:1. Introduction
- Type 1: there is no communication between hydrocele and peritoneal cavity. It mostly appears as an encysted mass without hernia defect in children. Examples for this type are the intra-abdominal protruding forms. In adults, we assume the fascia transversalis along with the ligamentum rotundum is thinned out because of the hydrocele, mimicking a direct hernia [6].
- Type 2: the hydrocele communicates with the peritoneal cavity, thus mostly resulting in an indirect hernia [6].
- Type 3: or combined type has an encysted part that does not communicate with the peritoneal cavity and another that does. Its appearance resembles an hourglass and commonly causes a hernia [6].
2. Methods
3. Results/Case Series Presentation
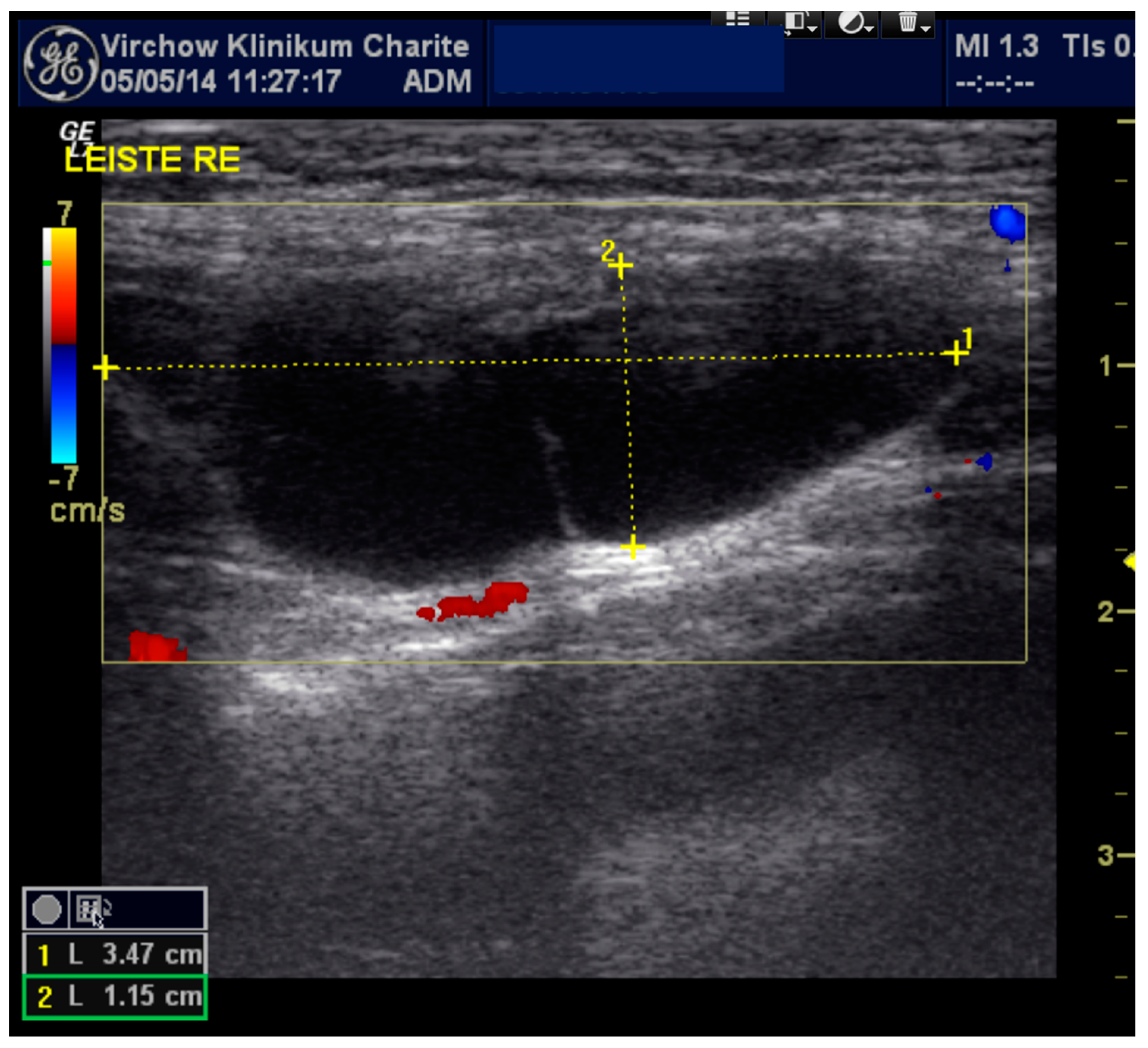
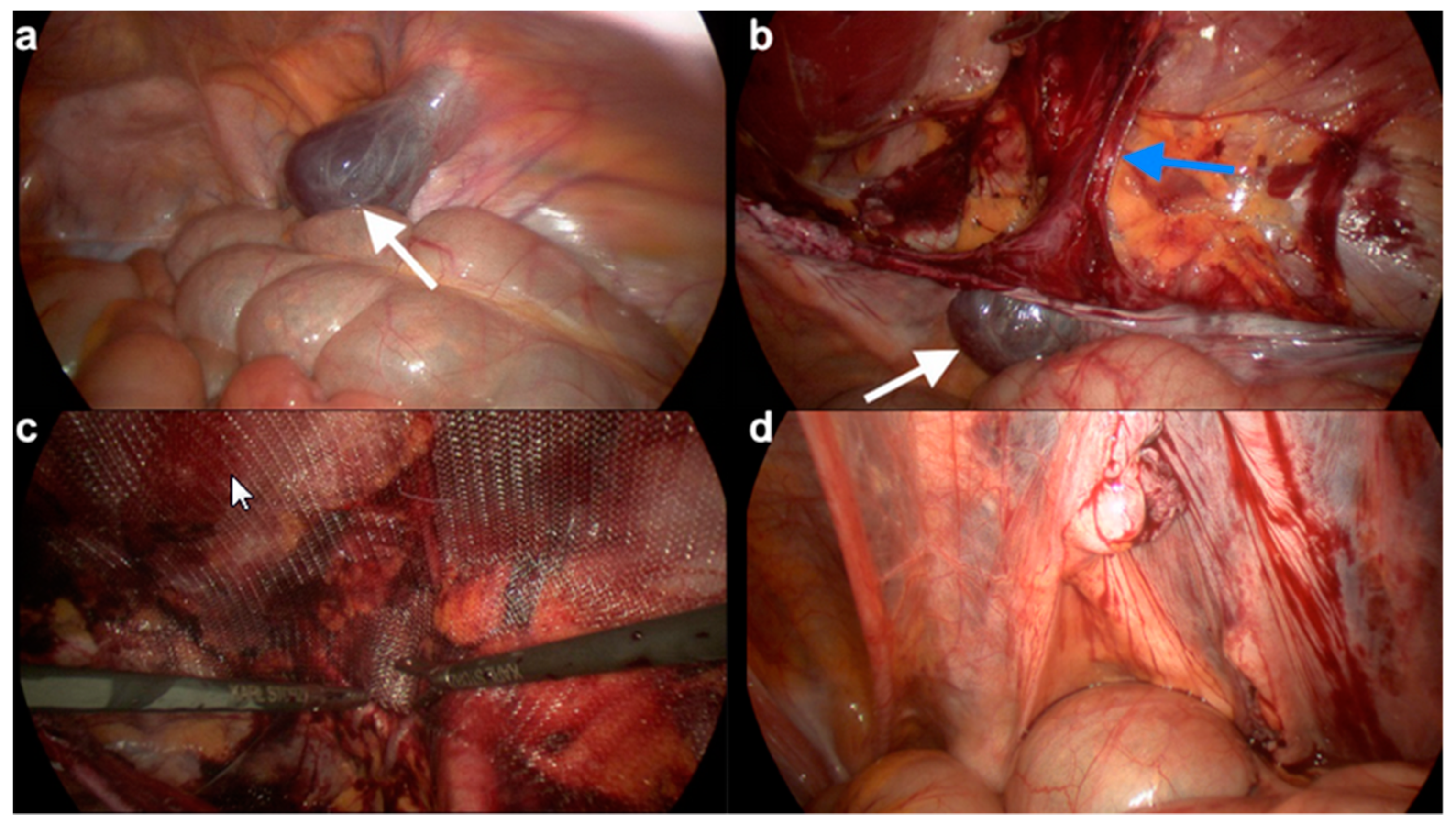
3.1. Case 1
3.2. Case 2
3.3. Case 3
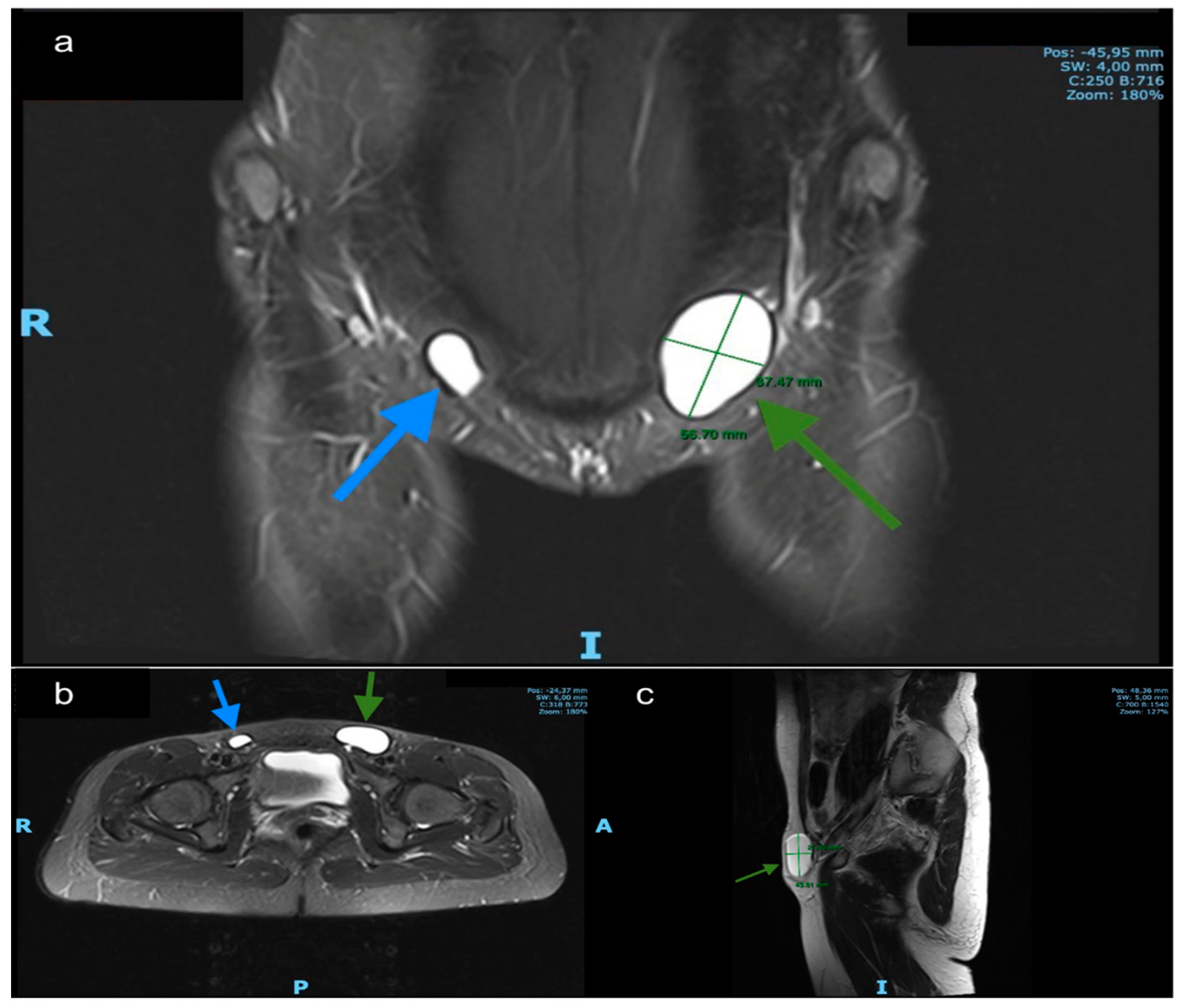
3.4. Case 4
3.5. Case 5
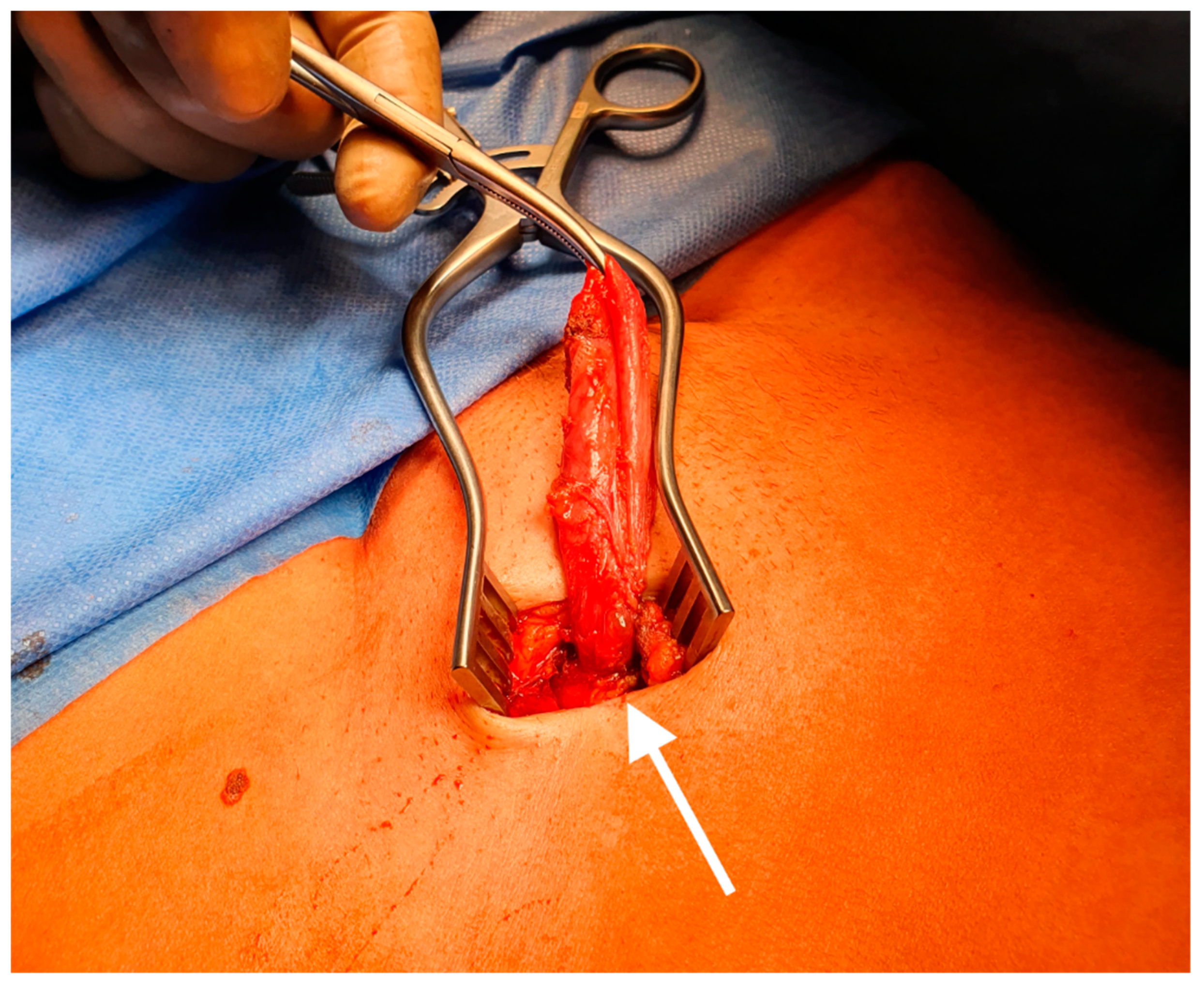
3.6. Case 6
3.7. Review of the Literature
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Rees, M.A.; Squires, J.E.; Tadros, S.; Squires, J.H. Canal of Nuck hernia: A multimodality imaging review. Pediatric Radiol. 2017, 47, 893–898. [Google Scholar] [CrossRef] [PubMed]
- Chan, D.; Kwon, J.K.; Lagomarsino, E.M.; Veltkamp, J.G.; Yang, M.S.; Pfeifer, C.M. Canal of Nuck hernias. Acta Radiol. Open 2019, 8, 2058460119889867. [Google Scholar] [CrossRef] [PubMed]
- Yang, D.M.; Kim, H.C.; Kim, S.W.; Lim, S.J.; Park, S.J.; Lim, J.W. Ultrasonographic diagnosis of ovary-containing hernias of the canal of Nuck. Ultrasonography 2014, 33, 178–183. [Google Scholar] [CrossRef] [PubMed]
- Janssen, K.; Klinkner, D.; Kumar, T. Encysted hydrocele of canal of nuck: A case report with review of literature. J. Surg. Tech. Case Rep. 2011, 3, 97–98. [Google Scholar] [PubMed]
- Grosfeld, J.L. Current concepts in inguinal hernia in infants and children. World J. Surg. 1989, 13, 506–515. [Google Scholar] [CrossRef] [PubMed]
- Counseller, V.S.; Black, B.M. Hydrocele of the Canal of Nuck. Ann. Surg. 1941, 113, 625–630. [Google Scholar] [CrossRef]
- Lee, S.R. Laparoscopic Treatment of Hydrocele of the Canal of Nuck in Pediatric Patients. Eur. J. Pediatric Surg. 2018, 28, 378–382. [Google Scholar] [CrossRef]
- Kim, K.S.; Choi, J.H.; Kim, H.M.; Kim, K.P.; Kwon, Y.J.; Hwang, J.H.; Lee, S.Y. Hydrocele of the Canal of Nuck in a Female Adult. Arch. Plast. Surg. 2016, 43, 476–478. [Google Scholar] [CrossRef] [Green Version]
- Qureshi, N.J.; Lakshman, K. Laparoscopic excision of cyst of canal of Nuck. J. Minim Access Surg. 2014, 10, 87–89. [Google Scholar] [CrossRef]
- Lombardo, V.; Cara, G.D.; Pavone, G.; Turrisi, M.; Cuticone, G.; Iaropoli, F. Surgical Treatment of Cyst of the Canal of Nuck: Report of a case. World J. Surg. Res. 2017, 6. Available online: http://www.npplweb.com/wjsr/fulltext/6/5 (accessed on 22 January 2019).
- Topal, U.; Sarıtaş, A.G.; Ülkü, A.; Akçam, A.T.; Doran, F. Cyst of the canal of Nuck mimicking inguinal hernia. Int. J. Surg. Case Rep. 2018, 52, 117–119. [Google Scholar] [CrossRef]
- Mandhan, P.; Raouf, Z.; Bhatti, K. Infected hydrocele of the canal of nuck. Case Rep. Urol. 2013, 2013, 275257. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matsumoto, T.; Hara, T.; Hirashita, T.; Kubo, N.; Hiroshige, S.; Orita, H. Laparoscopic diagnosis and treatment of a hydrocele of the canal of Nuck extending in the retroperitoneal space: A case report. Int. J. Surg. Case Rep. 2014, 5, 861–864. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sarkar, S.; Panja, S.; Kumar, S. Hydrocele of the Canal of Nuck (Female Hydrocele): A Rare Differential for Inguino-Labial Swelling. J. Clin. Diagn. Res. 2016, 10, PD21–PD22. [Google Scholar] [CrossRef] [PubMed]
- Lucas, J.W.; Shete, K.C.; Schermer, C.; Perosio, P.; Sterious, S. Canal of Nuck hydrocele in an adult female. Urol. Case Rep. 2019, 23, 67–68. [Google Scholar] [CrossRef] [PubMed]
- Caviezel, A.; Montet, X.; Schwartz, J.; Egger, J.-F.; Iselin, C.E. Female hydrocele: The cyst of Nuck. Urol. Int. 2009, 82, 242–245. [Google Scholar] [CrossRef] [PubMed]
- Papparella, A.; Vaccaro, S.; Accardo, M.; De Rosa, L.; Ronchi, A.; Noviello, C. Nuck cyst: A rare cause of inguinal swelling in infancy. Minerva Pediatr. 2018, 23. [Google Scholar] [CrossRef]
- Coley, W.M.B., II. Hydrocele in the Female. Ann. Surg. 1892, 16, 42–59. [Google Scholar] [CrossRef]
- Block, R.E. Hydrocele of the canal of nuck. A report of five cases. Obstet. Gynecol. 1975, 45, 464–466. [Google Scholar]
- Bhosale, P.R.; Patnana, M.; Viswanathan, C.; Szklaruk, J. The inguinal canal: Anatomy and imaging features of common and uncommon masses. Radiographics 2008, 28, 819–835. [Google Scholar] [CrossRef]
- Bagul, A.; Jones, S.; Dundas, S.; Aly, E.H. Endometriosis in the canal of Nuck hydrocele: An unusual presentation. Int. J. Surg. Case Rep. 2011, 2, 288–289. [Google Scholar] [CrossRef] [Green Version]
- Bianchi, A.; Espin, F.; Pulido, L.; Fantova, M.J. Nuck’s duct endometriosis. Med. Clin. 2007, 128, 759. [Google Scholar] [CrossRef] [PubMed]
- Nasser, H.; King, M.; Rosenberg, H.K.; Rosen, A.; Wilck, E.; Simpson, W.L. Anatomy and pathology of the canal of Nuck. Clin. Imaging 2018, 51, 83–92. [Google Scholar] [CrossRef] [PubMed]
- Heer, J.; McPheeters, R.; Atwell, A.E.; Aguiniga, P.; Blake, J. Hydrocele of the Canal of Nuck. West J. Emerg. Med. 2015, 16, 786–787. [Google Scholar] [CrossRef] [PubMed]
- Thomas, A.K.; Thomas, R.L.; Thomas, B. Canal of Nuck Abnormalities. J. Ultrasound Med. 2020, 39, 385–395. [Google Scholar] [CrossRef] [PubMed]
- Ozel, A.; Kirdar, O.; Halefoglu, A.M.; Erturk, S.M.; Karpat, Z.; Lo Russo, G.; Maldur, V.; Cantisani, V. Cysts of the canal of Nuck: Ultrasound and magnetic resonance imaging findings. J Ultrasound 2009, 12, 125–127. [Google Scholar] [CrossRef] [Green Version]
- Choi, Y.M.; Lee, G.M.; Yi, J.B.; Yoon, K.L.; Shim, K.S.; Bae, C.W.; Choi, S.I.; Kim, H.C. Two cases of female hydrocele of the canal of nuck. Korean J. Pediatric 2012, 55, 143–146. [Google Scholar] [CrossRef]
- Lai, I.; Page, A.; Hamidinia, F.; Rahmani, R. Cysts of the canal of Nuck: A rare sonographic diagnosis. J. Clin. Ultrasound 2017, 45, 175–178. [Google Scholar] [CrossRef]
- Jedrzejewski, G.; Osemlak, P.; Wieczorek, A.P.; Nachulewicz, P. Nuck Canal Hernias, Typical and Unusual Ultrasound Findings. Ultrasound Q. 2019, 35, 79–81. [Google Scholar] [CrossRef]
- Thomas, A.K.; Teague, C.T.; Jancelewicz, T. Canal of Nuck hernia containing pelvic structures presenting as a labial mass. Radiol. Case Rep. 2018, 13, 534–536. [Google Scholar] [CrossRef]
- Safak, A.A.; Erdogmus, B.; Yazici, B.; Gokgoz, A.T. Hydrocele of the canal of Nuck: Sonographic and MRI appearances. J. Clin. Ultrasound 2007, 35, 531–532. [Google Scholar] [CrossRef]
- Scheuermann, U.; Niebisch, S.; Lyros, O.; Jansen-Winkeln, B.; Gockel, I. Transabdominal Preperitoneal (TAPP) versus Lichtenstein operation for primary inguinal hernia repair—A systematic review and meta-analysis of randomized controlled trials. BMC Surg. 2017, 17, 55. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Köckerling, F.; Bittner, R.; Kofler, M.; Mayer, F.; Adolf, D.; Kuthe, A.; Weyhe, D. Lichtenstein Versus Total Extraperitoneal Patch Plasty Versus Transabdominal Patch Plasty Technique for Primary Unilateral Inguinal Hernia Repair: A Registry-based, Propensity Score-matched Comparison of 57,906 Patients. Ann. Surg. 2019, 269, 351–357. [Google Scholar] [CrossRef] [PubMed]
- Gass, M.; Banz, V.M.; Rosella, L.; Adamina, M.; Candinas, D.; Güller, U. TAPP or TEP? Population-based analysis of prospective data on 4,552 patients undergoing endoscopic inguinal hernia repair. World J. Surg. 2012, 36, 2782–2786. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gass, M.; Scheiwiller, A.; Sykora, M.; Metzger, J. TAPP or TEP for Recurrent Inguinal Hernia? Population-Based Analysis of Prospective Data on 1309 Patients Undergoing Endoscopic Repair for Recurrent Inguinal Hernia. World J. Surg. 2016, 40, 2348–2352. [Google Scholar] [CrossRef] [PubMed]
- Stickel, W.H.; Manner, M. Female Hydrocele (Cyst of the Canal of Nuck). J. Ultrasound Med. 2004, 23, 429–432. [Google Scholar] [CrossRef] [PubMed]
| Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | Patient 6 | |
|---|---|---|---|---|---|---|
| Age (years) | 29 | 29 | 44 | 35 | 41 | 34 |
| Symptoms/Reason of Presentation | Inguinal pain | Asymptomatic inguinal swelling | Inguinal pain and swelling | Inguinal pain and swelling | Inguinal pain and swelling | Inguinal pain and swelling |
| Diagnostic Study | Ultrasound | Ultrasound | Ultrasound | Ultrasound and magnetic resonance imaging (MRI) | Ultrasound | MRI |
| Elective/Emergent | Elective | Elective | Elective | Elective | Emergent | Elective |
| Procedure | Hydrocelectomy and TAPP hernioplasty | Hydrocelectomy and TAPP hernioplasty | Hydrocelectomy and TAPP hernioplasty | Hydrocelectomy and Lichtenstein hernia repair | Hydrocelectomy and TAPP hernioplasty | Open hydrocelectomy and fascial suture |
| Operating Time (min) | 52 min | 62 min | 62 min | 49 min | 65 min | 27 min |
| Type of Nuck hydrocele | type 2 | type 2 | type 2 | type 1 | type 3 | type 2 |
| Postoperative-Hospital Stay (days) | 2 | 2 | 2 | 2 | 2 | 1 |
| Complication | inguinal seroma | none | inguinal hemato-seroma | none | none | none |
| Recurrence | no | no | no | no | no | no |
| Follow up Period (months) | 1, 3 and 6 | 1, 4 and 6 | 6 | 6 | 3 and 6 | 1 and 6 |
| Year of Publication | Children/Adult | Type of Publication | Diagnostic Study | Elective/Emergent | Procedure | Presence of Hernia | Hospital Stay | Follow-Up | Author’s Conclusion | |
|---|---|---|---|---|---|---|---|---|---|---|
| Kim et al. [8] | 2016 | adult | Single case report | CT and magnetic resonance imaging (MRI) | elective | Open Hydrocelectomy with high ligation | unknown | unknown | unknown | Inclusion in differential diagnosis of inguinal swelling. |
| Janssen et al. [4] | 2011 | child | Single case report | none | elective | Open Hydrocelectomy with high ligation | unknown | unknown | uneventful, no recurrence | Inclusion in differential diagnosis of inguinal swelling. |
| Qureshi et al. [9] | 2013 | adult | Single case report | Ultrasound | elective | Laparoscopic hydrocelectomy and hernia repair with mesh | yes | unknown | uneventful, no recurrence | - |
| Lombardo et al. [10] | 2017 | adult | Single case report | Ultrasound and MRI | elective | Open hydrocelectomy and hernia repair with mesh | yes | unknown | uneventful, no recurrence | - |
| Topal et al. [11] | 2018 | adult | Single case report | Ultrasound and MRI | elective | Open hydrocelectomy and hernia repair with mesh | yes | 1 day | unknown | Inclusion in differential diagnosis of inguinal swelling. |
| Mandhan et al. [12] | 2013 | child | Single case report | Ultrasound | emergent | Open Hydrocelectomy with high ligation | no | unknown | uneventful, no recurrence | Inclusion in differential diagnosis of inguinal swelling. Surgery is mandatory for final diagnosis an treatment. |
| Matsumoto et al. [13] | 2014 | adult | Single case report | Ultrasound and MRI | elective | Hydrocelectomy and hernia repair with mesh (TEP) | yes | 3 days | unknown | TEP approach with its advantage of a shorter recovery period could be useful |
| Sarkar et al. [14] | 2014 | child | Single case report | Ultrasound | emergent | Open Hydrocelectomy with high ligation | no | unknown | uneventful, no recurrence | Inclusion in differential diagnosis for inguinal swelling. U/S and MRI preoperatively. Surgery is the treatment of choice. |
| Lucas et al. [15] | 2019 | adult | Single case report | Ultrasound | elective | Open Hydrocelectomy with high ligation | no | unknown | uneventful, no recurrence | Inclusion in differential diagnosis of inguinal swelling. |
| Lee et al. [7] | 2018 | children | Case series (26 patients) | not enough information | not enough information | Laparoscopic hydrocelectomy with high ligation | none | on average 7.5 h | uneventful, no recurrence | Lap. Hydrocelectomy with high ligation is an effective method for treating Nuck´s hydroceles in pediatric patients |
| Caviezel et al. [16] | 2009 | adult | Case report | MRI | elective | Open Hydrocelectomy | no | unknown | uneventful, no recurrence | Inclusion in differential diagnosis of inguinal swelling, Ultrasound for a first evaluation and MRI for precise information |
| Papparella et al. [17] | 2018 | Children | Case series (353 patients, of whom 3 had a Nuck hydrocele) | Ultrasound | elective | Open Hydrocelectomy with high ligation | no | unknown | uneventful, no recurrence | Surgery with high ligation is considered as therapy of choice for Nuck’s hydroceles |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fikatas, P.; Megas, I.-F.; Mantouvalou, K.; Alkatout, I.; Chopra, S.S.; Biebl, M.; Pratschke, J.; Raakow, J. Hydroceles of the Canal of Nuck in Adults—Diagnostic, Treatment and Results of a Rare Condition in Females. J. Clin. Med. 2020, 9, 4026. https://doi.org/10.3390/jcm9124026
Fikatas P, Megas I-F, Mantouvalou K, Alkatout I, Chopra SS, Biebl M, Pratschke J, Raakow J. Hydroceles of the Canal of Nuck in Adults—Diagnostic, Treatment and Results of a Rare Condition in Females. Journal of Clinical Medicine. 2020; 9(12):4026. https://doi.org/10.3390/jcm9124026
Chicago/Turabian StyleFikatas, Panagiotis, Ioannis-Fivos Megas, Kiriaki Mantouvalou, Ibrahim Alkatout, Sascha S. Chopra, Matthias Biebl, Johann Pratschke, and Jonas Raakow. 2020. "Hydroceles of the Canal of Nuck in Adults—Diagnostic, Treatment and Results of a Rare Condition in Females" Journal of Clinical Medicine 9, no. 12: 4026. https://doi.org/10.3390/jcm9124026
APA StyleFikatas, P., Megas, I.-F., Mantouvalou, K., Alkatout, I., Chopra, S. S., Biebl, M., Pratschke, J., & Raakow, J. (2020). Hydroceles of the Canal of Nuck in Adults—Diagnostic, Treatment and Results of a Rare Condition in Females. Journal of Clinical Medicine, 9(12), 4026. https://doi.org/10.3390/jcm9124026






