Lipoprotein(a) and Risk of Ischemic Stroke in Atrial Fibrillation: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Eligibility Criteria
- Population: adults (≥18 years old) with atrial fibrillation, whether or not they have had an ischemic stroke in the past, as determined by neuroimaging (CT or MRI).
- Exposure: measurement of circulating Lp(a) concentration, either as a continuous or categorical variable.
- Comparator: AF patients without ischemic stroke or systemic embolism served as a comparator.
- Outcomes: Results include either enough raw data to enable computation, or effect estimates, with corresponding confidence intervals that show relationships between Lp(a) concentration and the risk or prevalence of ischemic stroke and/or systemic embolism.
- Study designs: Cross-sectional analyses published in peer-reviewed journals, case–control studies, or observational cohort studies (prospective or retrospective) are examples of study designs.
2.3. Data Sources and Search Strategy
2.4. Study Selection and Data Extraction
2.5. Assessment of Risk of Bias
2.6. Statistical Analysis
3. Results
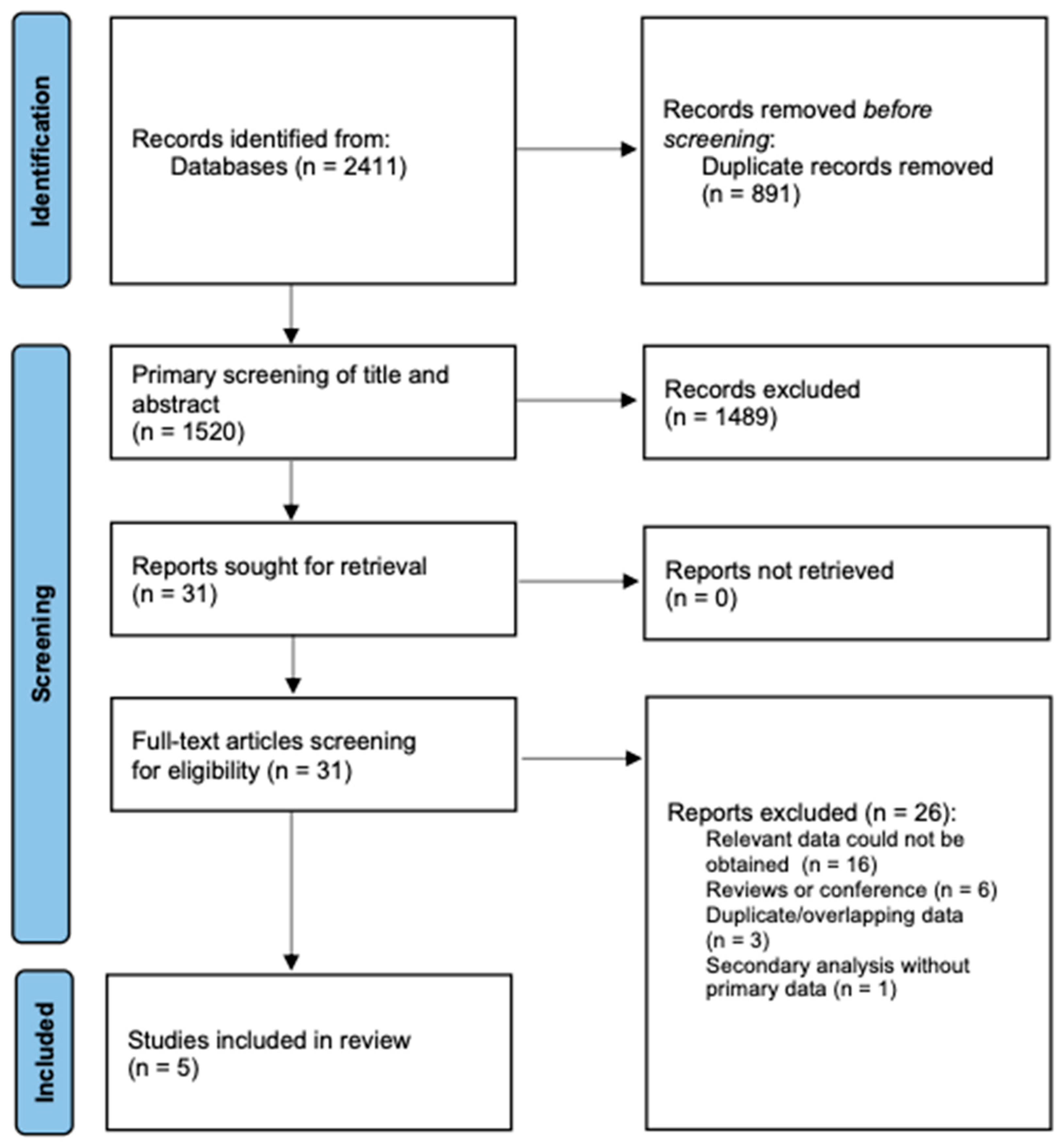
3.1. Study Selection
3.2. Study Characteristics
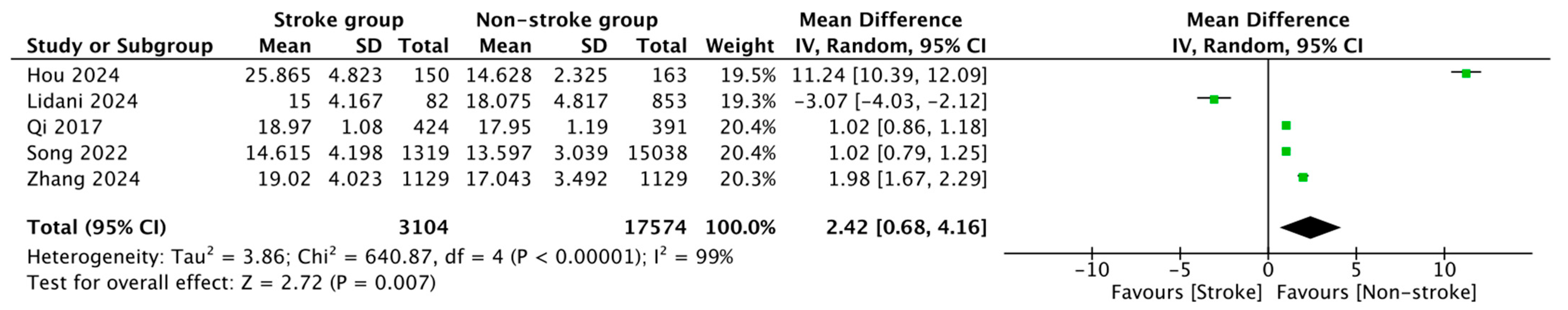
3.3. Meta-Analysis Results
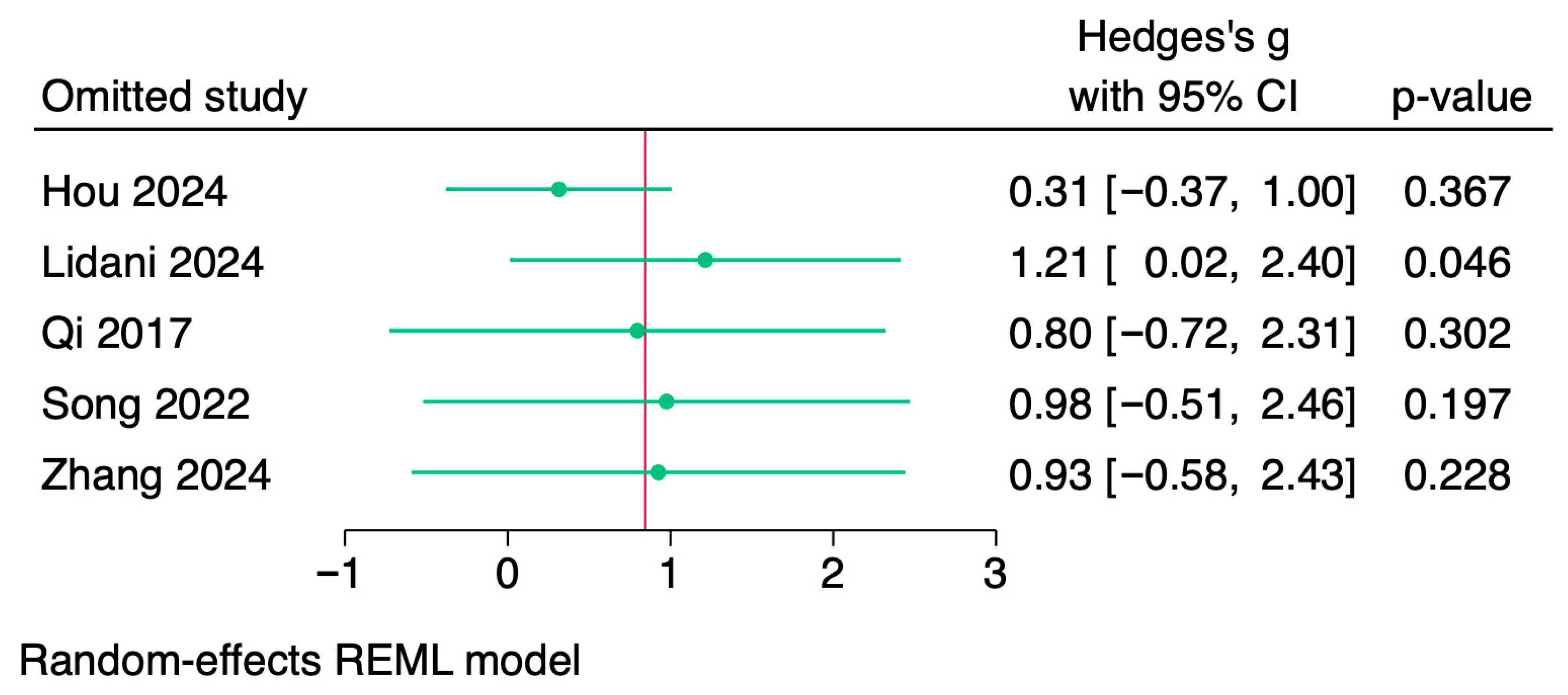
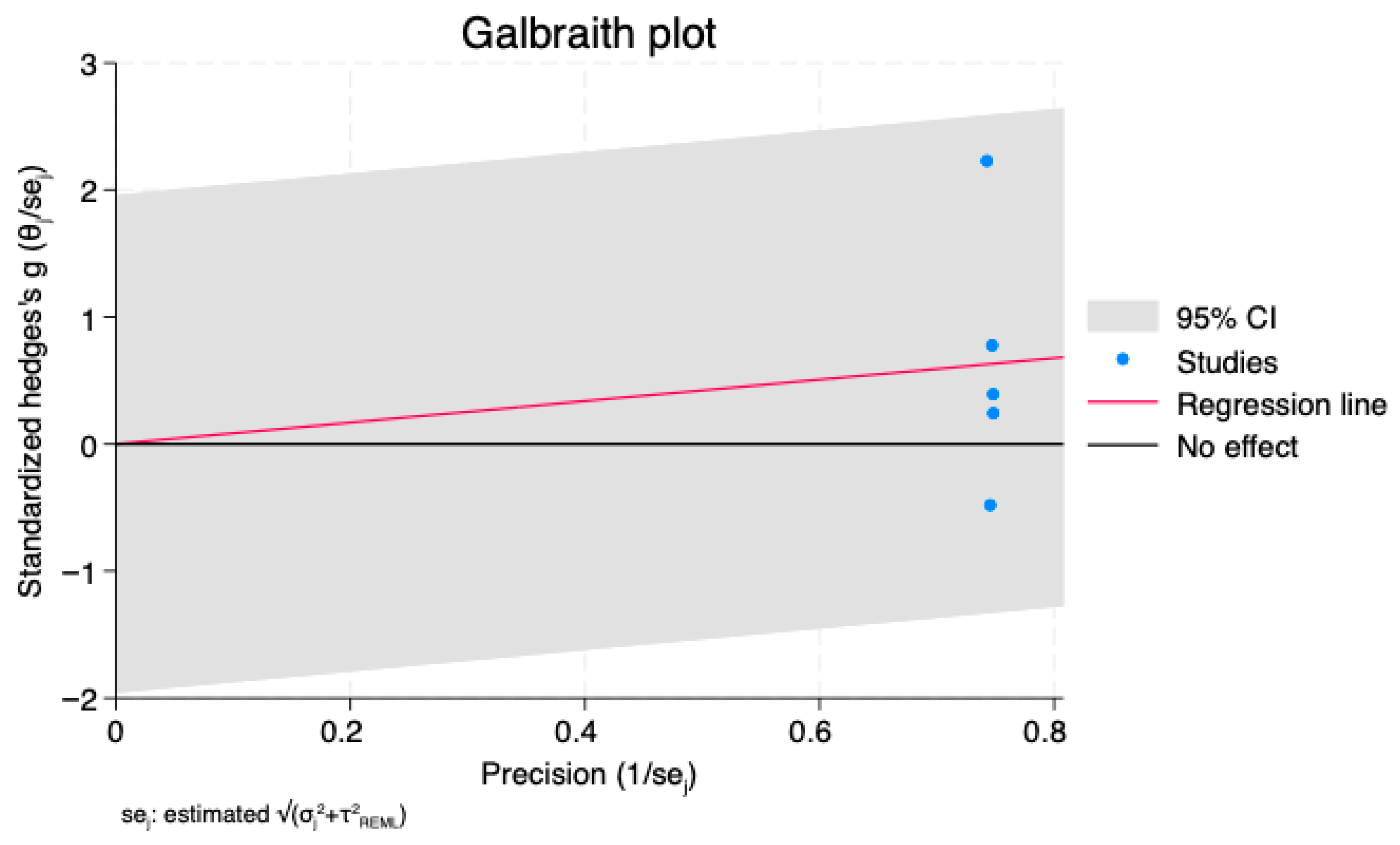
3.4. Sensitivity Analysis
3.5. Exploratory Analyses
3.6. Certainty of Evidence
4. Discussion
4.1. Strengths and Clinical Implications
4.2. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AF | Atrial fibrillation |
| BMI | Body Mass Index |
| CI | Confidence interval |
| CT | Computer tomography |
| GRADE | Grading of Recommendations, Assessment, Development, and Evaluation |
| HDL | High-Density Lipoprotein |
| HTN | Hypertension |
| I2 | Inconsistency Index |
| LDL | Low-Density Lipoprotein |
| Lp(a) | Lipoprotein(a) |
| MD | Mean difference |
| MRI | Magnetic Resonance Imaging |
| NS | Not specified |
| PECOS | Population, Exposure, Comparator, Outcomes, Study design |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| PROSPERO | International Prospective Register of Systematic Reviews |
| Q | Cochran’s Q Statistic |
| QUADAS-2 | Quality Assessment of Diagnostic Accuracy Studies–version 2 |
| REML | Restricted Maximum Likelihood Estimation |
| SD | Standard deviation |
| SE | Standard error |
| SMD | Standardized Mean Difference |
| TIA | Transient Ischemic Attack |
References
- Cheng, S.; He, J.; Han, Y.; Han, S.; Li, P.; Liao, H.; Guo, J. Global burden of atrial fibrillation/atrial flutter and its attributable risk factors from 1990 to 2021. Europace 2024, 26, euae195. [Google Scholar] [CrossRef]
- Van Gelder, I.C.; Rienstra, M.; Bunting, K.V.; Casado-Arroyo, R.; Caso, V.; Crijns, H.J.; De Potter, T.J.; Dwight, J.; Guasti, L.; Hanke, T.; et al. 2024 ESC Guidelines for the management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). Eur. Heart J. 2024, 45, 3314–3414. [Google Scholar] [CrossRef]
- Bassand, J.P.; Accetta, G.; Al Mahmeed, W.; Corbalan, R.; Eikelboom, J.; Fitzmaurice, D.A.; Fox, K.A.A.; Gao, H.; Goldhaber, S.Z.; Goto, S.; et al. Risk factors for death, stroke, and bleeding in 28,628 patients from the GARFIELD-AF registry: Rationale for comprehensive management of atrial fibrillation. PLoS ONE 2018, 13, e0191592. [Google Scholar] [CrossRef]
- Ruddox, V.; Sandven, I.; Munkhaugen, J.; Skattebu, J.; Edvardsen, T.; Otterstad, J.E. Atrial fibrillation and the risk for myocardial infarction, all-cause mortality and heart failure: A systematic review and meta-analysis. Eur. J. Prev. Cardiol. 2017, 24, 1555–1566. [Google Scholar] [CrossRef] [PubMed]
- Bassand, J.P.; Accetta, G.; Camm, A.J.; Cools, F.; Fitzmaurice, D.A.; Fox, K.A.; Goldhaber, S.Z.; Goto, S.; Haas, S.; Hacke, W.; et al. Two-year outcomes of patients with newly diagnosed atrial fibrillation: Results from GARFIELD-AF. Eur. Heart J. 2016, 37, 2882–2889. [Google Scholar] [CrossRef] [PubMed]
- Diener, H.C.; Hart, R.G.; Koudstaal, P.J.; Lane, D.A.; Lip, G.Y.H. Atrial Fibrillation and Cognitive Function: JACC Review Topic of the Week. J. Am. Coll. Cardiol. 2019, 73, 612–619. [Google Scholar] [CrossRef]
- Vinding, N.E.; Kristensen, S.L.; Rørth, R.; Butt, J.H.; Østergaard, L.; Olesen, J.B.; Torp-Pedersen, C.; Gislason, G.H.; Køber, L.; Kruuse, C.; et al. Ischemic Stroke Severity and Mortality in Patients With and Without Atrial Fibrillation. J. Am. Heart Assoc. 2022, 11, e022638. [Google Scholar] [CrossRef] [PubMed]
- Benz, A.P.; Hijazi, Z.; Lindbäck, J.; Connolly, S.J.; Eikelboom, J.W.; Oldgren, J.; Siegbahn, A.; Wallentin, L. Biomarker-Based Risk Prediction With the ABC-AF Scores in Patients With Atrial Fibrillation Not Receiving Oral Anticoagulation. Circulation 2021, 143, 1863–1873. [Google Scholar] [CrossRef]
- Tsimikas, S. A Test in Context: Lipoprotein(a): Diagnosis, Prognosis, Controversies, and Emerging Therapies. J. Am. Coll. Cardiol. 2017, 69, 692–711. [Google Scholar] [CrossRef]
- Clarke, R.; Peden, J.F.; Hopewell, J.C.; Kyriakou, T.; Goel, A.; Heath, S.C.; Parish, S.; Barlera, S.; Franzosi, M.G.; Rust, S.; et al. Genetic variants associated with Lp(a) lipoprotein level and coronary disease. N. Engl. J. Med. 2009, 361, 2518–2528. [Google Scholar] [CrossRef]
- Kamstrup, P.R.; Tybjaerg-Hansen, A.; Steffensen, R.; Nordestgaard, B.G. Genetically elevated lipoprotein(a) and increased risk of myocardial infarction. JAMA 2009, 301, 2331–2339. [Google Scholar] [CrossRef]
- Rath, M.; Niendorf, A.; Reblin, T.; Dietel, M.; Krebber, H.J.; Beisiegel, U. Detection and quantification of lipoprotein(a) in the arterial wall of 107 coronary bypass patients. Arteriosclerosis 1989, 9, 579–592. [Google Scholar] [CrossRef]
- Lampsas, S.; Xenou, M.; Oikonomou, E.; Pantelidis, P.; Lysandrou, A.; Sarantos, S.; Goliopoulou, A.; Kalogeras, K.; Tsigkou, V.; Kalpis, A.; et al. Lipoprotein(a) in Atherosclerotic Diseases: From Pathophysiology to Diagnosis and Treatment. Molecules 2023, 28, 969. [Google Scholar] [CrossRef]
- Etingin, O.R.; Hajjar, D.P.; Hajjar, K.A.; Harpel, P.C.; Nachman, R.L. Lipoprotein (a) regulates plasminogen activator inhibitor-1 expression in endothelial cells. A potential mechanism in thrombogenesis. J. Biol. Chem. 1991, 266, 2459–2465. [Google Scholar] [CrossRef]
- Menke, J.; Lüthje, L.; Kastrup, A.; Larsen, J. Thromboembolism in atrial fibrillation. Am. J. Cardiol. 2010, 105, 502–510. [Google Scholar] [CrossRef]
- Safavi-Naeini, P.; Rasekh, A. Thromboembolism in Atrial Fibrillation: Role of the Left Atrial Appendage. Card. Electrophysiol Clin. 2020, 12, 13–20. [Google Scholar] [CrossRef]
- Arboix, A.; Alió, J. Cardioembolic stroke: Clinical features, specific cardiac disorders and prognosis. Curr. Cardiol. Rev. 2010, 6, 150–161. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Deeks, J.J.; Higgins, J.P.T.; Altman, D.G. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions. Version 6.3. Cochrane. 2022. Available online: https://training.cochrane.org/handbook/current (accessed on 1 October 2025).
- Whiting, P.F.; Rutjes, A.W.; Westwood, M.E.; Mallett, S.; Deeks, J.J.; Reitsma, J.B.; Leeflang, M.M.; Sterne, J.A.; Bossuyt, P.M.; QUADAS-2 Group. QUADAS-2: A revised tool for the quality assessment of diagnostic accuracy studies. Ann. Intern. Med. 2011, 155, 529–536. [Google Scholar] [CrossRef]
- Guyatt, G.; Oxman, A.D.; Akl, E.A.; Kunz, R.; Vist, G.; Brozek, J.; Norris, S.; Falck-Ytter, Y.; Glasziou, P.; DeBeer, H.; et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J. Clin. Epidemiol. 2011, 64, 383–394. [Google Scholar] [CrossRef]
- Hozo, S.P.; Djulbegovic, B.; Hozo, I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med. Res. Methodol. 2005, 5, 13. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. Br. Med. J. 2003, 327, 557–560. [Google Scholar] [CrossRef]
- Meng, Z.; Wang, J.; Lin, L.; Wu, C. Sensitivity analysis with iterative outlier detection for systematic reviews and meta-analyses. Stat. Med. 2024, 43, 1549–1563. [Google Scholar] [CrossRef]
- Korevaar, E.; Turner, S.L.; Forbes, A.B.; Karahalios, A.; Taljaard, M.; McKenzie, J.E. Comparison of statistical methods used to meta-analyse results from interrupted time series studies: An empirical study. BMC Med. Res. Methodol. 2024, 24, 31. [Google Scholar] [CrossRef]
- Hou, X.; Zhang, X. Enhancing the evaluation of acute ischemic stroke risk in individuals with non-valvular atrial fibrillation by including laboratory indicators. Sci. Rep. 2024, 14, 6844. [Google Scholar] [CrossRef]
- Lidani, K.C.F.; Trainor, P.J.; Buscaglia, R.; Foster, K.; Jaramillo, S.; Michael, K.; Landry, A.P.; Michos, E.D.; Ouyang, P.; Morgan, E.S.; et al. Circulating Levels of Angiotensinogen, Sex Hormones, and Hormone Therapy-The Multi-Ethnic Study of Atherosclerosis (MESA). J. Clin. Hypertens. 2025, 27, e70083. [Google Scholar] [CrossRef]
- Qi, Z.; Chen, H.; Wen, Z.; Yuan, F.; Ni, H.; Gao, W.; Shen, J.; Li, J.; Lin, Y.; Shan, Y.; et al. Relation of Low-Density Lipoprotein Cholesterol to Ischemic Stroke in Patients With Nonvalvular Atrial Fibrillation. Am. J. Cardiol. 2017, 119, 1224–1228. [Google Scholar] [CrossRef]
- Song, J.; Zhang, X.; Wei, M.; Bo, Y.; Zhou, X.; Tang, B. Association between lipoprotein(a) and thromboembolism in patients with non-valvular atrial fibrillation: A cross-sectional study. Lipids Health Dis. 2022, 21, 78. [Google Scholar] [CrossRef]
- Zhang, S.; Zhou, Y.; Wang, J.; Fu, Q.; Shen, T.; Pan, G.; Luo, R.; Yang, X.; Jiang, L.; Hu, H. The Association of High Lipoprotein(a) Concentration and Risk of Ischaemic Stroke in Atrial Fibrillation Patients. Int. J. Gen. Med. 2024, 17, 2001–2009. [Google Scholar] [CrossRef]
- Koh, M.Y.; Toh, K.Z.; Loh, E.D.; Teo, Y.N.; Joon, K.C.; Tan, Q.X.; Sharma, V.K.; Yeo, L.L.; Sia, C.H.; Loh, W.J.; et al. Association of elevated lipoprotein(a) levels with ischemic stroke in young patients—A systematic review and meta-analysis. J. Stroke Cerebrovasc. Dis. 2024, 33, 107960. [Google Scholar] [CrossRef]
- Emerging Risk Factors Collaboration; Erqou, S.; Kaptoge, S.; Perry, P.L.; Di Angelantonio, E.; Thompson, A.; White, I.R.; Marcovina, S.M.; Collins, R.; Thompson, S.G.; et al. Lipoprotein(a) concentration and the risk of coronary heart disease, stroke, and nonvascular mortality. JAMA, 2009; 302, 412–423. [Google Scholar]
- Boffa, M.B.; Koschinsky, M.L. Lipoprotein(a): Truly a direct prothrombotic factor in cardiovascular disease? J. Lipid Res. 2016, 57, 745–757. [Google Scholar] [CrossRef]
- Zhang, Z.; Peng, B.; Nuranmubieke, A.; Xu, Y.; Liu, Y.; Tu, T.; Lin, Q.; Wang, C.; Liu, Q.; Xiao, Y. Lipoprotein(a) and Atrial Fibrillation: Mechanistic Insights and Therapeutic Approaches. Int. J. Med. Sci. 2025, 22, 357–370. [Google Scholar] [CrossRef]
- Aronis, K.N.; Zhao, D.; Hoogeveen, R.C.; Alonso, A.; Ballantyne, C.M.; Guallar, E.; Jones, S.R.; Martin, S.S.; Nazarian, S.; Steffen, B.T.; et al. Associations of lipoprotein(a) levels with incident atrial fibrillation and ischemic stroke: The ARIC study. J. Am. Heart Assoc. 2017, 6, e007372. [Google Scholar] [CrossRef]
- Mohammadi-Shemirani, P.; Chong, M.; Narula, S.; Perrot, N.; Conen, D.; Roberts, J.D.; Thériault, S.; Bossé, Y.; Lanktree, M.B.; Pigeyre, M.; et al. Elevated lipoprotein(a) and risk of atrial fibrillation: An observational and Mendelian randomization study. J. Am. Coll. Cardiol. 2022, 79, 1579–1590. [Google Scholar] [CrossRef]
- Langsted, A.; Nordestgaard, B.G.; Kamstrup, P.R. Lipoprotein(a) and cerebrovascular disease: Dose–response relationship in the general population. Stroke 2021, 52, 3306–3314. [Google Scholar]
- Pujadas Capmany, R.; Arboix, A.; Casañas-Muñoz, R.; Anguera-Ferrando, N. Specific cardiac disorders in 402 consecutive patients with ischaemic cardioembolic stroke. Int. J. Cardiol. 2004, 95, 129–134. [Google Scholar] [CrossRef]
- Bejarano-Arosemena, R.; Martínez-Sellés, M. Interatrial Block, Bayés Syndrome, Left Atrial Enlargement, and Atrial Failure. J. Clin. Med. 2023, 12, 7331. [Google Scholar] [CrossRef]
- Escobar-Robledo, L.A.; Bayés-de-Luna, A.; Lupón, J.; Baranchuk, A.; Moliner, P.; Martínez-Sellés, M.; Zamora, E.; de Antonio, M.; Domingo, M.; Cediel, G.; et al. Advanced interatrial block predicts new-onset atrial fibrillation and ischemic stroke in patients with heart failure: The “Bayes’ Syndrome-HF” study. Int. J. Cardiol. 2018, 271, 74–180. [Google Scholar] [CrossRef]
- Inogés, M.; Arboix, A.; García-Eroles, L.; Sánchez-López, M.J. Gender Predicts Differences in Acute Ischemic Cardioembolic Stroke Profile: Emphasis on Woman-Specific Clinical Data and Early Outcome-The Experience of Sagrat Cor Hospital of Barcelona Stroke Registry. Medicina 2024, 60, 101. [Google Scholar] [CrossRef]
| Study | Country | Study Desing | Study Group | Population | Age (Years) | Male (%) | BMI | HTN (%) | Diabetes (%) |
|---|---|---|---|---|---|---|---|---|---|
| Hou et al., 2024 [26] | China | Retrospective observational study | Stroke | 150 | 78.4 (9.1) | 73 (48.7) | NS | 113 (75.3) | 43 (28.7) |
| Non-stroke | 163 | 73.28 (12.42) | 80 (49.1) | NS | 105 (64.4) | 35 (21.5) | |||
| Lidani et al., 2024 [27] | USA | Prospective cohort study | Stroke | 82 | 75.3 (8.2) | 42 (51.2) | 28.8 (5.7) | 63 (76.7) | 15 (18.3) |
| Non-stroke | 853 | 74.7 (8.2) | 394 (46.2) | 28.2 (5.7) | 693 (69.0) | 208 (20.7) | |||
| Qi et al., 2017 [28] | China | Retrospective case–control study | Stroke | 424 | 74.5 (11.6) | 240 (56.6) | NS | 312 (73.6) | 145 (34.2) |
| Non-stroke | 391 | 72.7 (11.9) | 250 (63.9) | NS | 251 (64.2) | 105 (26.9) | |||
| Song et al., 2022 [29] | China | Cross-sectional study | Stroke | 1319 | NS | NS | NS | NS | NS |
| Non-stroke | 15,038 | NS | NS | NS | NS | NS | |||
| Zhang et al., 2024 [30] | China | Retrospective cohort study | Stroke | 1129 | 73 (65, 79) | 611 (54.12) | 23.44 (21.47, 25.43) | 754 (66.78) | 230 (20.37) |
| Non-stroke | 1129 | 73 (66, 80) | 582 (51.55) | 23.42 (21.37, 25.52) | 753 (66.70) | 224 (19.84) |
| Omitted Study | Pooled MD | 95% CI | τ2 | I2 (%) | Significance (p) |
|---|---|---|---|---|---|
| None (baseline) | 2.42 | 0.67–4.17 | 3.89 | 99.4 | p < 0.05 |
| Hou et al., 2024 [26] | 0.45 | −0.37–1.28 | 0.66 | 97.2 | p > 0.05 |
| Lidani et al., 2024 [27] | 3.73 | 1.87–5.58 | 3.52 | 99.5 | p < 0.05 |
| Qi et al., 2017 [28] | 2.79 | −0.23–5.81 | 9.36 | 99.5 | p > 0.05 |
| Song et al., 2022 [29] | 2.79 | −0.01–5.59 | 8.04 | 99.5 | p ≈ 0.05 |
| Zhang et al., 2024 [30] | 2.54 | 0.22–4.86 | 5.49 | 99.5 | p < 0.05 |
| Outcome | № of Participants (Studies) | Study Design | Effect (95% CI) | Relative/ Absolute Effect | Certainty of the Evidence (GRADE) | Comments |
|---|---|---|---|---|---|---|
| Mean Lp(a) difference between AF patients with and without ischemic stroke | 20,678 (5) | Observational (case–control/cohort, mostly single-center) | MD = 2.42 mg/dL (95% CI 0.68 to 4.16) | Continuous outcome–absolute MD reported (no meaningful relative measure) | ⬤◯◯◯ Very low | Downgraded for serious risk of bias, very serious inconsistency (I2 = 100%), and indirectness (predominantly Asian cohorts). No upgrading despite biological plausibility, as heterogeneity remains unexplained. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maj, B.; Pruc, M.; Momot, K.; Krauz, K.; Kozak, J.; Golczyk, H.; Uminska, J.; Kotfis, K.; Szpinda, Ł.; Lis, M.; et al. Lipoprotein(a) and Risk of Ischemic Stroke in Atrial Fibrillation: A Systematic Review and Meta-Analysis. J. Clin. Med. 2025, 14, 7851. https://doi.org/10.3390/jcm14217851
Maj B, Pruc M, Momot K, Krauz K, Kozak J, Golczyk H, Uminska J, Kotfis K, Szpinda Ł, Lis M, et al. Lipoprotein(a) and Risk of Ischemic Stroke in Atrial Fibrillation: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2025; 14(21):7851. https://doi.org/10.3390/jcm14217851
Chicago/Turabian StyleMaj, Bartosz, Michal Pruc, Karol Momot, Kamil Krauz, Joanna Kozak, Hieronim Golczyk, Julia Uminska, Katarzyna Kotfis, Łukasz Szpinda, Michal Lis, and et al. 2025. "Lipoprotein(a) and Risk of Ischemic Stroke in Atrial Fibrillation: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 14, no. 21: 7851. https://doi.org/10.3390/jcm14217851
APA StyleMaj, B., Pruc, M., Momot, K., Krauz, K., Kozak, J., Golczyk, H., Uminska, J., Kotfis, K., Szpinda, Ł., Lis, M., Peacock, F. W., & Szarpak, L. (2025). Lipoprotein(a) and Risk of Ischemic Stroke in Atrial Fibrillation: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 14(21), 7851. https://doi.org/10.3390/jcm14217851






