Clinical Applications of Virtual and Augmented Reality in Radiology: A Scoping Review
Abstract
1. Introduction
- What are the target areas of non-educational clinical applications of VR and AR in the pediatric and adult populations?
- Are VR and AR cost-effective strategies in the clinical or surgical management of patients compared with traditional strategies?
- What are the benefits of utilizing these novel technologies in the proposed population, including their impact on the accuracy of diagnostic tests?
2. Methods
2.1. Study Design Framework
2.2. Search and Data Collection Strategies
2.3. Study Selection Process
2.4. Eligibility Criteria for Primary Studies
2.5. Data Extraction, Analysis and Critical Appraisal
2.6. Statistical Analysis
3. Results
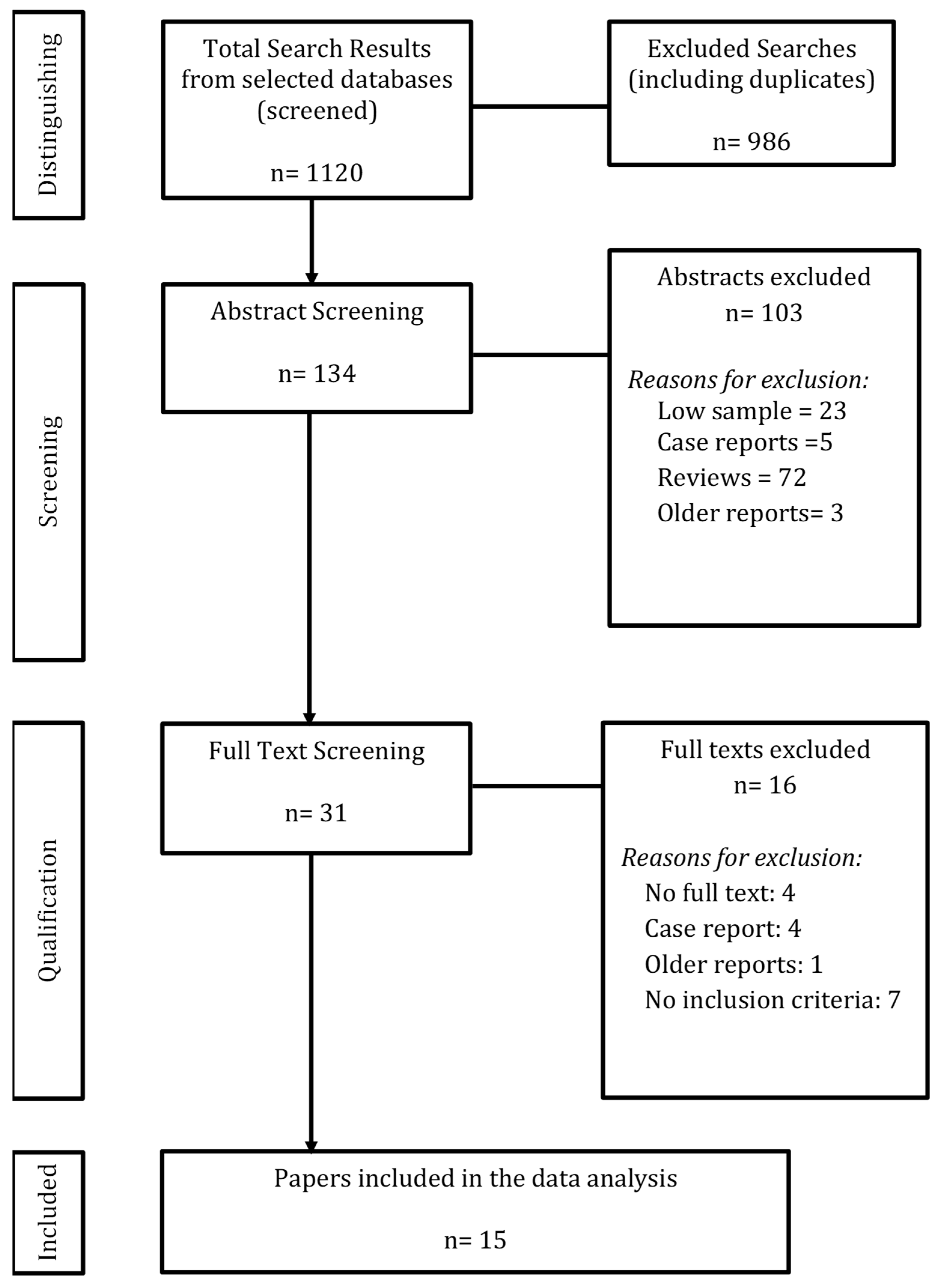
3.1. Study Selection
3.2. Primary Studies’ Research Design
- -
- -
- -
- -
- Non-RCT cross-sectional study with a control group: 1 study (6.7%) [29].
3.3. Reporting Quality of Primary Studies (Using STARD)
- -
- Title or Abstract and Introduction: item 1: identification of the study as a diagnostic accuracy study using at least one measure of accuracy: no papers met this criterion.
- -
- Methods (Study Design, Participants, Test Methods, Analysis): item 6: eligibility criteria: 4/15 studies scored 0; item 8: reporting where and when eligible participants were identified: 3/15 scored 0, and 2/15 scored 0.5; item 9: participant recruitment methods (e.g., consecutive, random, convenience): only 8/15 (53.3%) studies provided details; item 18: intended sample size and determination method: only 5/15 (33.3%) studies provided this information.
- -
- Results (Participants, Tests): item 19: flow diagrams of participant selection: only 6/15 studies (40%) included diagrams; item 20: 10/15 (66.6%) scored 1, 2/15 (13.3%) scored 0.5 for demographic and clinical characteristics.
- -
- Discussion: item 26: 2/15 (13.3%) papers scored zero on consensus for not adequately presenting study limitations.
- -
- Other Information: item 28: 7/15 (46.7%) did not present a registration number or the name of a registry. This may be because only 5 papers (33%) were classified as clinical studies; item 29: only 4/15 (26.7%) studies mentioned where the full protocol could be accessed; item 30: 5/15 papers (33.3%) did not list sources of funding or other forms of support.
- -
- The final STARD scores of the papers are presented in Table 6. Supplementary Table S1 shows the full STARD breakdown of items per study.
3.4. Inter-Reader Reliability of STARD Scoring
3.5. Summary of Data from Primary Studies
4. Discussion
4.1. Summary of Evidence
4.2. Population
4.3. Improvement of Population Health and Experiences of Care
4.4. VR Technology
4.5. Standards for Reporting Diagnostic Accuracy (STARD) of Primary Studies
5. Limitations
6. Future Directions
7. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- University of Toronto, Ontario Institute for Studies in Education. Virtual Reality in the Classroom: What Is VR? Research Guides. Available online: https://guides.library.utoronto.ca/c.php?g=607624&p=4938314 (accessed on 1 September 2021).
- Visualise Creative Limited. Virtual Reality in the Healthcare Industry. VISUALISE. Available online: https://visualise.com/virtual-reality/virtual-reality-healthcare (accessed on 22 September 2017).
- Theingi, S.; Leopold, I.; Ola, T.; Cohen, G.S.; Maresky, H. Virtual Reality as a Non-Pharmacological Adjunct to Reduce the Use of Analgesics in Hospitals. J. Cogn. Enhanc. 2022, 6, 108–113. [Google Scholar] [CrossRef] [PubMed]
- Elsayed, M.; Kadom, N.; Ghobadi, C.; Strauss, B.; Al Dandan, O.; Aggarwal, A.; Anzai, Y.; Griffith, B.; Lazarow, F.; Straus, C.M.; et al. Virtual and augmented reality: Potential applications in radiology. Acta Radiol. 2020, 61, 1258–1265. [Google Scholar] [CrossRef]
- Sutherland, J.; Belec, J.; Sheikh, A.; Chepelev, L.; Althobaity, W.; Chow, B.; Mitsouras, D.; Christensen, A.; Rybicki, F.J.; La Russa, D.J. Applying modern virtual and augmented reality technologies to medical images and models. J. Digit. Imaging 2019, 32, 38–53. [Google Scholar] [CrossRef]
- Moro, C.; Stromberga, Z.; Raikos, A.; Stirling, A. The effectiveness of virtual and augmented reality in health sciences and medical anatomy. Anat. Sci. Educ. 2017, 10, 549–559. [Google Scholar] [CrossRef]
- Plasencia, D.M. One step beyond virtual reality: Connecting past and future developments. XRDS 2015, 22, 18–23. [Google Scholar] [CrossRef]
- Sousa, M.; Mendes, D.; Paulo, S.; Matela, N.; Jorge, J.; Lopes, D. VRRRRoom: Virtual Reality for Radiologists in the Reading Room. In Proceedings of the 2017 CHI Conference on Human Factors in Computing Systems, Denver, CO, USA, 6–11 May 2017; ACM: New York, NY, USA, 2017; pp. 4057–4062. [Google Scholar]
- Lastrucci, A.; Giansanti, D. Radiological Crossroads: Navigating the Intersection of Virtual Reality and Digital Radiology through a Comprehensive Narrative Review of Reviews. Robotics 2024, 13, 69. [Google Scholar] [CrossRef]
- Gelmini, A.; Duarte, M.; de Assis, A.; Guimarães, J.; Carnevale, F. Virtual reality in interventional radiology education: A systematic review. Radiol. Bras. 2021, 54, 254–260. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gelmini, A.; Duarte, M.; Silva, M.; Guimarães, J.; Santos, L. Augmented reality in interventional radiology education: A systematic review of randomized controlled trials. Sao Paulo Med. J. 2022, 140, 604–614. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Shetty, S.; Bhat, S.; Al Bayatti, S.; Al Kawas, S.; Talaat, W.; El-Kishawi, M.; Al Rawi, N.; Narasimhan, S.; Al-Daghestani, H.; Madi, M.; et al. The Scope of Virtual Reality Simulators in Radiology Education: Systematic Literature Review. JMIR Med. Educ. 2024, 10, e52953. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wang, Y.; Tao, J.; Chen, M.; Peng, Y.; Wu, H.; Yan, Z.; Huang, P. Effects of Virtual Reality on Pain, Anxiety and Fear Among Emergency Department Patients: A Meta-Analysis of Randomized Controlled Trials. Pain Manag. Nurs. 2025, 26, e339–e352. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Yu, F.; Shi, D.; Shi, J.; Tian, Z.; Yang, J.; Wang, X.; Jiang, Q. Application of virtual reality technology in clinical medicine. Am. J. Transl. Res. 2017, 9, 3867–3880. [Google Scholar] [PubMed] [PubMed Central]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef] [PubMed]
- Bossuyt, P.M.; Reitsma, J.B.; Bruns, D.E.; Gatsonis, C.A.; Glasziou, P.P.; Irwig, L.; Lijmer, J.G.; Moher, D.; Rennie, D.; de Vet, H.C.W.; et al. STARD 2015: An updated list of essential items for reporting diagnostic accuracy studies. BMJ 2015, 351, h5527. [Google Scholar] [CrossRef] [PubMed]
- Milgram, P.; Takemura, H.; Utsumi, A.; Kishino, F. Augmented reality: A class of displays on the reality–virtuality continuum. Proc. SPIE 1994, 2351, 282–292. [Google Scholar] [CrossRef]
- Altman, D.G. Practical Statistics for Medical Research; Chapman and Hall: London, UK, 1991; pp. 404–408. [Google Scholar]
- Ieiri, S.; Uemura, M.; Konishi, K.; Souzaki, R.; Nagao, Y.; Tsutsumi, N.; Akahoshi, T.; Ohuchida, K.; Ohdaira, T.; Tomikawa, M.; et al. Augmented reality navigation system for laparoscopic splenectomy in children based on preoperative CT image using optical tracking device. Pediatr. Surg. Int. 2012, 28, 341–346. [Google Scholar] [CrossRef] [PubMed]
- Souzaki, R.; Ieiri, S.; Uemura, M.; Ohuchida, K.; Tomikawa, M.; Kinoshita, Y.; Koga, Y.; Suminoe, A.; Kohashi, K.; Oda, Y.; et al. An augmented reality navigation system for pediatric oncologic surgery based on preoperative CT and MRI images. J. Pediatr. Surg. 2013, 48, 2479–2483. [Google Scholar] [CrossRef] [PubMed]
- Zhao, C.; Yang, J.; Gan, Y.; Liu, J.; Tan, Z.; Liang, G.; Meng, X.; Sun, L.; Cao, W. Application of MR virtual endoscopy in children with hydrocephalus. Magn. Reson. Imaging 2015, 33, 1205–1211. [Google Scholar] [CrossRef] [PubMed]
- Han, S.H.; Park, J.W.; Choi, S.I.; Kim, J.Y.; Lee, H.; Yoo, H.J.; Ryu, J.H. Effect of Immersive Virtual Reality Education Before Chest Radiography on Anxiety and Distress Among Pediatric Patients: A Randomized Clinical Trial. JAMA Pediatr. 2019, 173, 1026–1031. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Milano, E.G.; Kostolny, M.; Pajaziti, E.; Marek, J.; Regan, W.; Caputo, M.; Luciani, G.B.; Mortensen, K.H.; Cook, A.C.; Schievano, S.; et al. Enhanced 3D visualization for planning biventricular repair of double outlet right ventricle: A pilot study on the advantages of virtual reality. Eur. Heart J. Digit. Health 2021, 2, 667–675. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Stunden, C.; Stratton, K.; Zakani, S.; Jacob, J. Comparing a Virtual Reality-Based Simulation App (VR-MRI) With a Standard Preparatory Manual and Child Life Program for Improving Success and Reducing Anxiety During Pediatric Medical Imaging: Randomized Clinical Trial. J. Med. Internet Res. 2021, 23, e22942. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ryu, J.H.; Park, J.W.; Choi, S.I.; Kim, J.Y.; Lee, H.; Yoo, H.J.; Han, S.H. Virtual Reality vs. Tablet Video as an Experiential Education Platform for Pediatric Patients Undergoing Chest Radiography: A Randomized Clinical Trial. J. Clin. Med. 2021, 10, 2486. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Simpfendörfer, T.; Gasch, C.; Hatiboglu, G.; Müller, M.; Maier-Hein, L.; Hohenfellner, M.; Teber, D. Intraoperative Computed Tomography Imaging for Navigated Laparoscopic Renal Surgery: First Clinical Experience. J. Endourol. 2016, 30, 1105–1111. [Google Scholar] [CrossRef] [PubMed]
- Nambi, G.; Abdelbasset, W.K.; Alqahatani, B.A. Radiological (Magnetic Resonance Image and Ultrasound) and biochemical effects of virtual reality training on balance training in football players with chronic low back pain: A randomized controlled study. J. Back Musculoskelet. Rehabil. 2021, 34, 269–277. [Google Scholar] [CrossRef] [PubMed]
- Sadri, S.; Loeb, G.J.; Grinshpoon, A.; Elvezio, C.; Sun, S.H.; Ng, V.G.; Khalique, O.; Moses, J.W.; Einstein, A.J.; Patel, A.J.; et al. First Experience With Augmented Reality Guidance for Cerebral Embolic Protection During TAVR. JACC Adv. 2024, 3, 100839. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chuan, A.; Qian, J.; Bogdanovych, A.; Kumar, A.; McKendrick, M.; McLeod, G. Design and validation of a virtual reality trainer for ultrasound-guided regional anaesthesia. Anaesthesia 2023, 78, 739–746. [Google Scholar] [CrossRef] [PubMed]
- Kockro, R.A.; Serra, L.; Tseng-Tsai, Y.; Chan, C.; Yih-Yian, S.; Gim-Guan, C.; Lee, E.; Hoe, L.Y.; Hern, N.; Nowinski, W.L. Planning and simulation of neurosurgery in a virtual reality environment. Neurosurgery 2000, 46, 118–135, discussion 135–137. [Google Scholar] [CrossRef] [PubMed]
- Hohlweg-Majert, B.; Schön, R.; Schmelzeisen, R.; Gellrich, N.C.; Schramm, A. Navigational maxillofacial surgery using virtual models. World J. Surg. 2005, 29, 1530–1538. [Google Scholar] [CrossRef]
- Qiu, T.M.; Zhang, Y.; Wu, J.S.; Tang, W.J.; Zhao, Y.; Pan, Z.G.; Mao, Y.; Zhou, L.F. Virtual reality presurgical planning for cerebral gliomas adjacent to motor pathways in an integrated 3-D stereoscopic visualization of structural MRI and DTI tractography. Acta Neurochir. 2010, 152, 1847–1857. [Google Scholar] [CrossRef]
- Yang, J.H.; Ryu, J.J.; Nam, E.; Lee, H.S.; Lee, J.K. Effects of Preoperative Virtual Reality Magnetic Resonance Imaging on Preoperative Anxiety in Patients Undergoing Arthroscopic Knee Surgery: A Randomized Controlled Study. Arthroscopy 2019, 35, 2394–2399. [Google Scholar] [CrossRef] [PubMed]
- Rieger, M.; Gabl, M.; Gruber, H.; Jaschke, W.R.; Mallouhi, A. CT virtual reality in the preoperative workup of malunited distal radius fractures: Preliminary results. Eur. Radiol. 2005, 15, 792–797. [Google Scholar] [CrossRef]
| Element | Inclusion | Exclusion |
|---|---|---|
| Population | Human patients (all ages) undergoing any clinical or interventional radiology procedure with VR/AR | Non-human studies; healthy-volunteer studies without clinical imaging context |
| Intervention | Virtual reality (fully immersive via head-mounted display) or augmented reality (digital overlays) for clinical purposes (pre-op planning, procedural support, pain/anxiety management) | Educational-only VR/AR without clinical outcomes; 360° video without interactive tracking |
| Comparator | Standard care or preparatory methods (verbal instruction, tablet video, standard imaging) | No-comparator single-arm simulations |
| Outcomes | Clinical outcomes (anxiety/distress scores, procedure time, diagnostic accuracy), reporting quality (STARD score, ICC) | Pure usability metrics or developer-focused performance measures without clinical or reporting outcomes. Clinical outcomes (anxiety/distress scores, procedure time, diagnostic accuracy), reporting quality (STARD score, ICC) |
| Study Design | RCTs, cohort studies, case series with ≥6 participants | Case reports (<6 subjects), editorials, reviews, protocols, letters, conference abstracts |
| Language | English, Spanish, Portuguese, French, German, Korean, Italian | Other languages |
| Date range | January 2000–30 January 2025 | Publications before January 2000 o4-mini-high |
| First Author | Year of Publication | Country of Origin | Number of Patients | Mean Age (SD) Years) | Median Age (Range) Years | % of Male (Rounded) | Prospective vs. Retrospective Design |
|---|---|---|---|---|---|---|---|
| Pediatric only (N = 7) | |||||||
| Ieiri, S. [19] | 2012 | Japan | 6 | n/a | n/a (6–15) | n/a | Prospective |
| Souzaki, R. [20] | 2013 | Japan | 6 | n/a | n/a (1–12) | n/a | Prospective |
| Zhao, C. [21] | 2015 | China | 30 | n/a | n/(0.1–1.7) 1–20 Months | 47% | Prospective |
| Han, S-H [22] | 2019 | Korea | 99 in total Virtual reality group: 49; usual care group: 50 | VR group: Mean 5.8 (SD, 1.3 years); Control group: Mean 5.6 SD, 1.2 year) | 4–8 years | VR group: boys: 32 (65.3%); control group: boys: 26 (52.0%) | Prospective |
| Milano, E.G. [23] | 2021 | UK | 10 | n/a | n/a (0–1.1) 0.1–13 months | n/a | Retrospective |
| Stunden, C. [24] | 2021 | Canada | 92 | n/a | n/a (4–13) | 61% | Prospective |
| Ryu, J-H [25] | 2021 | Korea | 120 in total Virtual reality group: 60 tablet video group: 60 | VR group: Mean 6.0 (4.8–7.0 years); tablet video group: Mean 6.9 (5.0–7.3) | VR group: boys: 25 (41.7%); tablet video group: boys: 32 (53.3%) | Prospective | |
| Adult only (N = 4) | |||||||
| Simpfendorfer, T. [26] | 2016 | Germany | 10 | n/a | n/a (38–69) | 70% | Prospective |
| Nambi, G. [27] | 2020 | Saudi Arabia | 36 | n/a | n/a (18–25) | n/a | Prospective |
| Sadri, S. [28] | 2023 | United States | 24 | n/a | AR guidance group: 84 (79–87), control group: 75(73–85) | AR guidance group: 7 (58%), control group: 8 (66.7%) | Prospective |
| Chuan A [29] | 2023 | Australia, U.K. | 21 novice and 15 experienced participants | Novice: Mean 21 (SD, 1) Experienced: Mean 41 (SD, 6) | Novice: Males 7 (33.3%); Experienced: 10 (66.7%) | Prospective | |
| Pediatric and adult (N = 4) | |||||||
| Kockro, R.A. [30] | 2000 | Singapore | 21 | n/a | n/a (11–66) | 48% | Retrospective |
| Hohlweg-Majert, B. [31] | 2005 | Germany | 107 | n/a | n/a (0.1–80) 0.1 year = 3 weeks | n/a | Prospective |
| Qiu, T.M. [32] | 2010 | China | 45 (baseline); 40 (follow-up) | 46.0 (17.98) | n/a (4–70) | 58% | Prospective |
| Yang, J.H. [33] | 2019 | South Korea | 48 | n/a | n/a Group VR: (15–62); Group Non-VR (20–65). | 0 (all females) | Prospective |
| First Author | Field | Diagnosis | Key Findings |
|---|---|---|---|
| Pediatric only (N = 7) | |||
| Ieiri, S. [19] | Hematology | Hematological disorders: hereditary spherocytosis (HS) and idiopathic thrombocytopenia purpura (ITP)—treated by laparoscopic splenectomy with one patient also requiring a laparoscopic cholecystectomy | The proposed navigation system provides real-time anatomical information that cannot be obtained without the system. Registration accuracies for the study cases were acceptable in clinical operation settings. |
| Souzaki, R. [20] | Oncology | Pediatric malignancy (abdominothoracic) | The proposed AR navigation system was useful for detecting the tumor location during pediatric endoscopic surgery. |
| Zhao, C. [21] | Neurosurgery | Hydrocephalus/Intracranial pathology: clinical manifestation of enlarged head circumference, increased intracranial and growth retardation | “MR virtual endoscopy provides a non-invasive diagnostic modality that can be used as a supplemental approach to ventriculoscopy. Requires future studies to assess sensitivity and specificity of the technique.” |
| Han, S-H [22] | Radiology | Training of experimental group with a 3 min immersive virtual reality experience of the process of chest radiography guided by animation and narration. | During chest radiography, distress scores were lower in the treatment group, with a mean difference of 3.0 (95% CI 1.0 to 5.0). Compared with the control group, the virtual reality group had fewer children classified as distressed (score _5) (risk ratio 0.3, 95% CI 0.1 to 0.7), less need for parent presence (risk ratio 0.3, 95% CI 0.1 to 0.9), higher parental satisfaction scores (MD 20.8, 95% CI 21.5 to 20.1) and reduced procedure time (MD 19.9 s, 95% CI 6.6 to 33.3). |
| Milano, E.G. [23] | Cardiology | DORV and complex interventricular communications | 3D pdf reached only 70%, whereas it was 95% after VR. Virtual reality can enhance understanding of suitability for biventricular repair in patients with complex DORV if compared to cross-sectional images and other 3D modeling techniques. |
| Stunden, C. [24] | Anesthesiology | examine the effectiveness of virtual reality (VR) simulation training in ultrasound-guided regional anesthesia. | VR-based simulation significantly improves clinical performance in ultrasound-guided regional anesthesia compared to standard training methods. |
| Ryu, J-H [25] | Radiology | Evaluated the effect of VR, compared with standard video, on reducing anxiety and distress in pediatric patients undergoing chest radiography. | The number of less distressed children (OSBD score < 5) was significantly higher in the VR group than in the tablet group (49 [81.7%]) vs. 32 [53.3%]) (p = 0.001). The OSBD scores, the need for parental presence, the procedure time, and the number of repeated procedures were all lower in the VR group. |
| Adult only (N = 4) | |||
| Simpfendorfer, T. [26] | Urology | Renal malignancy (with complex or endophytic tumor localization) | Use of CBCT is feasible and safe and allows for direct access to complex or endophytic renal masses. |
| Nambi, G. [27] | Physiatry | Chronic low back pain | Positive effects of VR training on imaging and biochemical aspects of study subjects. |
| Sadri, S. [28] | Anesthesiology | Evaluating the effectiveness of training methods. Specifically, the training of clinicians in performing ultrasound-guided regional anesthesia, assessing whether virtual reality (VR)-based simulation can improve their skills compared to traditional training methods. | VR-based simulation training is as effective as standard training methods, showing no significant difference in the clinical performance outcomes between the two groups. |
| Chuan A [29] | Radiology | Training of an interventional procedure using ultrasound-guidance | The virtual reality trainer was comparable in terms of performance to other high-fidelity virtual reality software, possibility to act and quality of interface subscales (all p > 0.06), but not in the possibility to examine and self-performance subscales (all p < 0.009). It created workloads similar to those reported in real-life procedural medicine (p = 0.53). |
| Pediatric and adult (N = 4) | |||
| Kockro, R.A. [30] | Neurosurgery | Intracranial pathology: complex neurosurgical anatomy of intra- and extra-axial brain tumors and vascular malformations. | The VIVIAN system allows users to work with complex imaging data in a fast, comprehensive, and intuitive manner but still requires a costly operating system. VIVIAN system substantially contributed to surgical planning by (1) providing a quick and better understanding of intracranial anatomic and abnormal spatial relationships, (2) simulating the craniotomy and the required cranial base bone work, and (3) simulating intraoperative views. |
| Hohlweg-Majert, B. [31] | Craniofacial | Craniomaxillofacial malformation | Author’s opinion-based without data analysis: Image-guided treatment improves preoperative planning by visualizing the individual anatomy and outlining the intended reconstructive outcome. Intraoperative navigation makes tumor and reconstructive surgery more reliable by showing safety margins, saving vital structures, and leading the reconstruction to preoperatively planned objectives. |
| Qiu, T.M. [32] | Neurosurgery | Cerebral Glioma | VR-based 3D stereoscopic tractography visualization enhances understanding of anatomic information of intra-axial tumor contours and adjacent PT, and results in surgical trajectory optimization initially and maximal safe tumor resection finally. Surgeons can predict the long-term motor functional outcome based on EPT increasing amplitude. |
| Yang, J.H. [33] | Orthopedics | Knee Pathology: Ligament rupture, Meniscus tear, Chondral lesion | Positive effects of VR experience of 3D reconstructed knee MRIs in patients undergoing arthroscopic knee surgery reducing anxiety around surgical encounters. |
| First Author | Year of Publication | Number of Timepoints | Imaging Modality | Comparators | Key Findings |
|---|---|---|---|---|---|
| Pediatric only (N = 7) | |||||
| Ieiri S [19] | 2012 | Single | Multi-detector low CT (MDCT) (Aquilion 64, Toshiba Medical Co., Ltd., Tokyo, Japan) | n/a | The proposed navigation system provides real-time anatomical information that cannot be obtained without the system. Registration accuracies for the study cases were acceptable in clinical operation settings. |
| Souzaki R [20] | 2013 | Single | MDCT (multi-detector computed tomography) MRI | n/a | The proposed AR navigation system was useful for detecting the tumor location during pediatric endoscopic surgery. |
| Zhao C [21] | 2015 | Single | MRI (3D-T1 weighted, FSPGR; Signa EXCTTE 1.5 T MR machines (GE, USA), processing software (ADW 4.3) CT ventriculography [OPTIMN CT660 (128T) machine (GE, USA)] | Ventriculoscopy or CT imaging reference standard) | “MR virtual endoscopy provides a non-invasive diagnostic modality that can be used as a supplemental approach to ventriculoscopy. Requires future studies to assess sensitivity and specificity of the technique.” |
| Han, S-H. [22] | 2019 | Single (during chest radiography, after VR or verbal instruction intervention). | Chest radiography (x-ray) | Control Group: Received simple verbal instruction before chest radiography. VR Group: Received a 3 min immersive VR education explaining the radiography process. | VR education significantly reduced anxiety and distress in pediatric patients undergoing chest radiography. Lower distress scores in the VR group (OSBD score: 2.0 vs. 5.0 in control, p = 0.004). Lower need for parental presence (16.3% in VR groups vs. 36.0% in control) Shorter procedure time (55.1 s in VR group vs. 75.0 s in control) Higher parental satisfaction (9.4 in VR group vs. 8.6 in control) Fewer repeated procedures in the VR group (8.2% vs. 16.0%) |
| Milano, E.G. [23] | 2021 | Single | CMR, cardiac magnetic resonance; CT, computed tomography | n/a | 3D pdf reached only 70%, whereas it was 95% after VR. Virtual reality can enhance understanding of suitability for biventricular repair in patients with complex DORV if compared to cross-sectional images and other 3D modelling techniques. |
| Stunden, C. [24] | 2021 | Dual | Ultrasound | virtual reality (VR)-based simulation training vs. standard training method | virtual reality (VR)-based simulation training was as effective as standard training methods for ultrasound-guided regional anesthesia. The study found no significant difference in the clinical performance between the two groups, suggesting that VR-based training can be a viable alternative to traditional training methods for developing skills in this area. |
| Ryu, J-H [25] | 2021 | Single (during chest radiography, after the VR or tablet video intervention) | Chest Radiography (X-ray) | Tablet group: watched a 3 min educational video on a tablet explaining chest radiography VR group: received the same educational content in an immersive VR environment using a head-mounted display | VR education significantly reduced distress and anxiety in pediatric patients compared to tablet video education Lower distress scores in the VR group (OSBD score: 1.0 vs. 4.0 in the tablet group, p < 0.001) Lower OSBD scores in the VR group (median 1.0) vs. the tablet group (median 4.0) (p < 0.001) Lower need for parental presence (8.3% in the VR group vs. 31.7% in the tablet group, p = 0.001) Shorter procedure time (48s in the VR group vs. 65s in the tablet group. p < 0.001) Easier procedure for radiology technologists in the VR group (ease-of-procedure rating 10.0 vs. 8.0, p < 0.001) Fewer repeated chest radiographs in the VR group (3.3%) vs. the tablet group (10%) |
| Adult only (N = 4) | |||||
| Simpfendorfer T [26] | 2016 | Single | CB-CT and fluoroscopy infusion | Nephrometry scores of tumors | Use of CBCT is feasible and safe and allows for direct access to complex or endophytic renal masses. |
| Nambi G [27] | 2020 | Dual (Baseline and after 4 weeks) | 3-T MRI Ultrasound Device (Hitachi Ultrasound, Tokyo, Japan) | Immunosor bent assay (ELISA) | Positive effects of VR training on imaging and biochemical aspects of study subjects. |
| Sadri, S [28] | 2023 | Dual | CT and fluoroscopy | AR guidance vs. standard guidance | AR guidance significantly reduced contrast volume used during device deployment without increasing the time required for filter placement or fluoroscopy time. The AR system facilitated easier device placement and increased confidence in navigating the aortic arch during the procedure. |
| Chuan, A [29] | 2023 | Single (within this session, each participant performed 40 needling attempts across four different virtual nerve targets | Ultrasound | Novice group (participants with no prior experience in ultrasound-guided regional anesthesia (UGRA) vs. experienced group: participants with at least 50 ultrasound guided regional anesthesia procedures performed | Experienced participants performed slightly better than novices (p = 0.002) Performance scores remained above 80% for experienced participants from the third attempt onward, while novices showed more variability. VR trainer immersion was comparable to other high-fidelity VR software in realism, quality of interface, and possibility to act (p > 0.06). The VR trainer imposed workloads similar to real-life procedural medicine (p = 0.53) Novices exhibited greater initial learning improvements compared to experienced participants, who had more stable performance. |
| Pediatric and adult (N = 4) | |||||
| Kockro R, A. [30] | 2000 | Single | MRI (Siemens Expert 1.0-T unit, Stuttgart, Germany; General Electric Signa 1.5-T unit, Milwaukee, WI, USA), MRA, MRV venography, CT imaging (GE scanner; Picker 2000 scanner, Picker, Cleveland, OH, USA) | n/a | The VIVIAN system allows users to work with complex imaging data in a fast, comprehensive, and intuitive manner but still requires a costly operating system. VIVIAN system substantially contributed to surgical planning by 1) providing a quick and better understanding of intracranial anatomic and abnormal spatial relationships, 2) simulating the craniotomy and the required cranial base bone work, and 3) simulating intraoperative views. |
| Hohlweg-Majert, B. [31] | 2005 | Dual (Baseline, pre-surgery and post-surgery as clinically indicated | Spiral-CT Contrast-enhanced MRI | n/a | Author’s opinion without data analysis: Image-guided treatment improves preoperative planning by visualizing the individual anatomy, and outlining the intended reconstructive outcome. Intraoperative navigation makes tumor and reconstructive surgery more reliable by showing safety margins, saving vital structures, and leading the reconstruction to preoperatively planned objectives. |
| Qiu TM [32] | 2010 | Dual (Baseline and after 6 months) | 3.0-T whole-body MRI (General Electric Medical Systems, GE Signa VH/i) Diffusion tensor imaging (DTI), T1-weighted 3-D fast spoiled gradient-recalled | n/a | VR-based 3D stereoscopic tractography visualization enhances understanding of anatomic information of intra-axial tumor contours and adjacent PT and results in surgical trajectory optimization initially and maximal safe tumor resection finally. Surgeons can predict the long-term motor functional outcome based on EPT increasing amplitude. |
| Yang, JH [33] | 2019 | Single | MRI | n/a | Positive effects of VR experience of 3D reconstructed knee MRIs in patients undergoing arthroscopic knee surgery reducing anxiety around surgical encounters. |
| First Author | Year of Publication | Measurements | Hardware | Software | Pre-Surgical or Intervention |
|---|---|---|---|---|---|
| Pediatric only (N = 7) | |||||
| Ieiri S [19] | 2012 | Mean +/− SD of fiducial registration error (FRE) and target registration error (TRE) between the lists of markers identified in the CT images for evaluation of registration accuracy | Mean +/− SD of fiducial registration error (FRE) and target registration error (TRE) between the lists of markers identified in the CT images for evaluation of registration accuracy | 3D viewer software (Virtual Place 300, AZE Co., Ltd., Tokyo, Japan | Intervention |
| Souzaki R [20] | 2013 | Descriptive report of success or not of tumor resection using the AR navigation | Descriptive report of success or not of tumor resection using the AR navigation | 3D viewer software program (Virtual Place 300, AZE Co., Ltd. | Pre-surgical |
| Zhao C [21] | 2015 | Descriptive characteristics and degree of obstruction of parts of the ventricular system (complete vs. non-complete obstruction) by MRVE and ventriculoscopy | Descriptive characteristics and degree of obstruction of parts of the ventricular system (complete vs. non-complete obstruction) by MRVE and ventriculoscopy | Processing software (ADW 4.3) for Signa EXCTTE Smooth imaging Navigator software | Intervention |
| Han, S-H. [22] | 2019 | Anxiety and distress: Observational Scale of Behavioral Distress (OSBD) (0–30 scale) Need for parental presence (yes/no) Parental satisfaction score (0–10 scale) Procedure time (seconds from room entry to image capture). Number of repeated radiographs Process difficulty score | Oculus Go VR headset | Custom VR content developed by JSC Games (Seoul, Republic of Korea) Randomization software: Random Allocation Software (version 1.0, Isfahan University of Medical Sciences). Statistical analysis software: SPSS (version 21.0, SPSS Inc). | Pre-intervention: VR was used before chest radiography to educate and prepare pediatric patients |
| Milano, E.G. [23] | 2021 | 3D visualization, LVOT max, RVOT max | Models were printed at 1:1 scale, in rigid white nylon (EOS PA2200 Nylon 12) using selective laser technology (EOS P100). | The 3D reconstructions (as .obj files) were imported into a novel VR environment developed in-house within the Unity engine. The target platform was the Oculus Rift system (comprising a headset, two sensors, and two hand controllers). | Pre-surgical |
| Stunden, C. [24] | 2021 | MoTrak head motion tracking system, Venham picture test, short State-Trait Anxiety Inventory, procedural data (minutes), usability, child reported satisfaction and fun | MERGE VR Headset, Samsung Galaxy S9 | Unity, AirServer Connect | Pre-surgical |
| Ryu, J-H [25] | 2021 | Anxiety and distress: Observational Scale of Behavioral Distress (OSBD) (0–30 scale) Need for parental presence (yes/no) Parental satisfaction score (0–10 scale) Number of repeated radiographs Process difficulty score Ease-of-procedure score (0–10 scale rated by radiology technologists) | VR group: Head-mounted VR display Tablet group: Tablet PC for video education | Custom VR content developed based on a simulated radiology room experience Tablet video was 2D conversion of the same VR material Randomization software: Random allocation software (version 1.0, Isafahan University of Medical Sciences) Statistical analysis software: SPSS (version 21.0, SPSS Inc.) | Pre-intervention: VR was used before chest radiography to educate and prepare pediatric patients |
| Adult only (N = 4) | |||||
| Simpfendorfer T [26] | 2016 | Descriptive feasibility and performance assessed by histopathological results, peri- and postoperative data. | Descriptive feasibility and performance assessed by histopathological results, peri- and postoperative data. | Open-source Medical Imaging Interaction Toolkit (MITK) syngo iPilot; Siemens Health-care, | Intervention |
| Nambi G [27] | 2020 | Imaging (muscle cross-sectional area, muscle thickness) Biochemical (CRP, TNF,-alpha, IL-2, IL-4, IL-6) | Imaging (muscle cross-sectional area, muscle thickness) Biochemical (CRP, TNF,-alpha, IL-2, IL-4, IL-6) | VR: ProKin system (PK 252, N Tecno Body, Italy) | Intervention |
| Sadri, S [28] | 2023 | Primary outcomes measured include iodinated contrast volume, times to filter placement, and fluoroscopy time. Secondary outcomes involve creatinine levels at discharge and clinical adverse events such as stroke and death at 30-day follow-up. | Microsoft HoloLens | Unity, 3mensio | Intervention |
| Chuan, A [29] | 2023 | Needling performance scores, calculated based on needle angulation (ideal in-plane positioning), number of withdrawals (fewer is better), time taken to complete the task Presence Questionnaire (for immersion in the virtual environment) NASA Task Load Index (NASA-TLX) (for cognitive workload) | VR Headset: Oculus Rift S Hand controllers (to manipulate virtual transducer and needle) Motion Capture System: MTw Awinda (Xsens, The Netherlands) Ultrasound Machine: Edge (FujiFilm SonoSite, Bothell, WA, USA) Computer: Gaming laptop with Intel Core i7-8750H processor (2.2 GHz) 16GB RAM NVIDIA GeForce GTX 1060 graphics card | Unity C (for VR trainer development) SPSS version 24 (for statistical analysis) MedCalc version 20.115 Microsoft Excel (2009 version) NASA-TLX software (iOOS version 1.03) for cognitive workload measurement | Pre-surgical (VR trainer was designed for training in ultrasound guided regional anesthesia (UGRA), not for direct intervention on patients |
| Pediatric and adult (N = 4) | |||||
| Kockro R, A. [30] | 2000 | Descriptive analysis: A report was written about each planning session. Each report was divided into two parts. One part recorded the size of the data set, the time needed for fusion and segmentation, the average system performance in frames per second, and the planning and simulation tools used during the session. | Descriptive analysis: A report was written about each planning session. Each report was divided into two parts. One part recorded the size of the data set, the time needed for fusion and segmentation, the average system performance in frames per second, and the planning and simulation tools used during the session. | VIVIAN (Virtual Intracranial Visualization and Navigation) | Pre-surgical |
| Hohlweg-Majert, B. [31] | 2005 | Pre- and postoperative spiral CT/MRI changes between the preceding and actual CT/MRI (e.g., assessment of pre- and post-operative periorbital deformation, optic nerve decompression). | Pre- and postoperative spiral CT/MRI changes between the preceding and actual CT/MRI (e.g., assessment of pre- and post-operative periorbital deformation, optic nerve decompression). | VR surgical navigation tool (Stryker-Leibinger, Germany) | Pre-surgical |
| Qiu TM [32] | 2010 | Karnofsky Performance Scale (KPS): grading functional status at 6-month evaluation, patient questionnaire (at follow-up) | Karnofsky Performance Scale (KPS): grading functional status at 6-month evaluation, patient questionnaire (at follow-up) | VR system (Dextroscope, Volume Interactions Pte. Ltd.)—the Fiber Tracking module of the VR system Volume-One 1.72 (VOLUME-ONE developers group) dTV. II (Image Process and Analysis Laboratory | Pre-surgical |
| Yang, JH [33] | 2019 | Primary: Amsterdam Preoperative Anxiety and Information Scale score to measure level of anxiety; Secondary: visual analog scale (VAS) scores measuring patient pain, preparedness, satisfaction, and stress | Primary: Amsterdam Preoperative Anxiety and Information Scale score to measure level of anxiety; Secondary: visual analog scale (VAS) scores measuring patient pain, preparedness, satisfaction, and stress | Software 3D Slicer 4.6.2 (Brigham and Women’s Hospital and The Slicer Community Autodesk 3ds Max (Autodesk ZBrush (Pixologic) Engine 4 Software (Epic Games) | Intervention |
| Study | Items Reported (Out of 19) | Final Consensus Score (Maximum = 19 *) | % Score ** | Quality |
|---|---|---|---|---|
| Pediatric only (N = 7) | ||||
| Ieiri 2012 [19] | 19 | 10 | 53% | Fair |
| Souzaki 2013 [20] | 19 | 9.5 | 50% | Suboptimal |
| Zhao 2015 [21] | 19 | 12.5 | 66% | Good |
| Han 2019 [22] | 19 | 16 | 84% | Excellent |
| Milano 2021 [23] | 19 | 13 | 68% | Good |
| Stunden 2021 [24] | 18 | 16 | 89% | Excellent |
| Ryu 2021 [25] | 19 | 15 | 79% | Good |
| Adult only (N = 4) | ||||
| Simpfendorfer 2016 [26] | 19 | 10 | 53% | Fair |
| Nambi 2020 [27] | 19 | 16.5 | 87% | Excellent |
| Sadri 2023 [28] | 19 | 13.5 | 71% | Good |
| Chuan 2023 [29] | 19 | 14 | 74% | Good |
| Pediatric and adult (N = 4) | ||||
| Kockro 2000 [30] | 19 | 11.5 | 61% | Fair |
| Hohlweg-Majert 2005 [31] | 19 | 8 | 42% | Suboptimal |
| Qui 2010 [32] | 19 | 15 | 79% | Good |
| Yang 2019 [33] | 19 | 17 | 89% | Excellent |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, S.M.; Coimbra Baffi, H.; Ola, T.; Tsang, B.; Gupta, A.; Faingold, R.; Stimec, J.; Doria, A.S. Clinical Applications of Virtual and Augmented Reality in Radiology: A Scoping Review. J. Clin. Med. 2025, 14, 7438. https://doi.org/10.3390/jcm14207438
Lee SM, Coimbra Baffi H, Ola T, Tsang B, Gupta A, Faingold R, Stimec J, Doria AS. Clinical Applications of Virtual and Augmented Reality in Radiology: A Scoping Review. Journal of Clinical Medicine. 2025; 14(20):7438. https://doi.org/10.3390/jcm14207438
Chicago/Turabian StyleLee, Somin Mindy, Henrique Coimbra Baffi, Tolulope Ola, Brian Tsang, Aaryan Gupta, Ricardo Faingold, Jennifer Stimec, and Andrea S. Doria. 2025. "Clinical Applications of Virtual and Augmented Reality in Radiology: A Scoping Review" Journal of Clinical Medicine 14, no. 20: 7438. https://doi.org/10.3390/jcm14207438
APA StyleLee, S. M., Coimbra Baffi, H., Ola, T., Tsang, B., Gupta, A., Faingold, R., Stimec, J., & Doria, A. S. (2025). Clinical Applications of Virtual and Augmented Reality in Radiology: A Scoping Review. Journal of Clinical Medicine, 14(20), 7438. https://doi.org/10.3390/jcm14207438






