Endocarditis: Rising Incidence in the Post-COVID-19 Pandemic Era: A Narrative Review
Abstract
1. Introduction
2. Methodology
3. Incidence and Epidemiology
4. Non-Bacterial Thrombotic Endocarditis (NBTE)
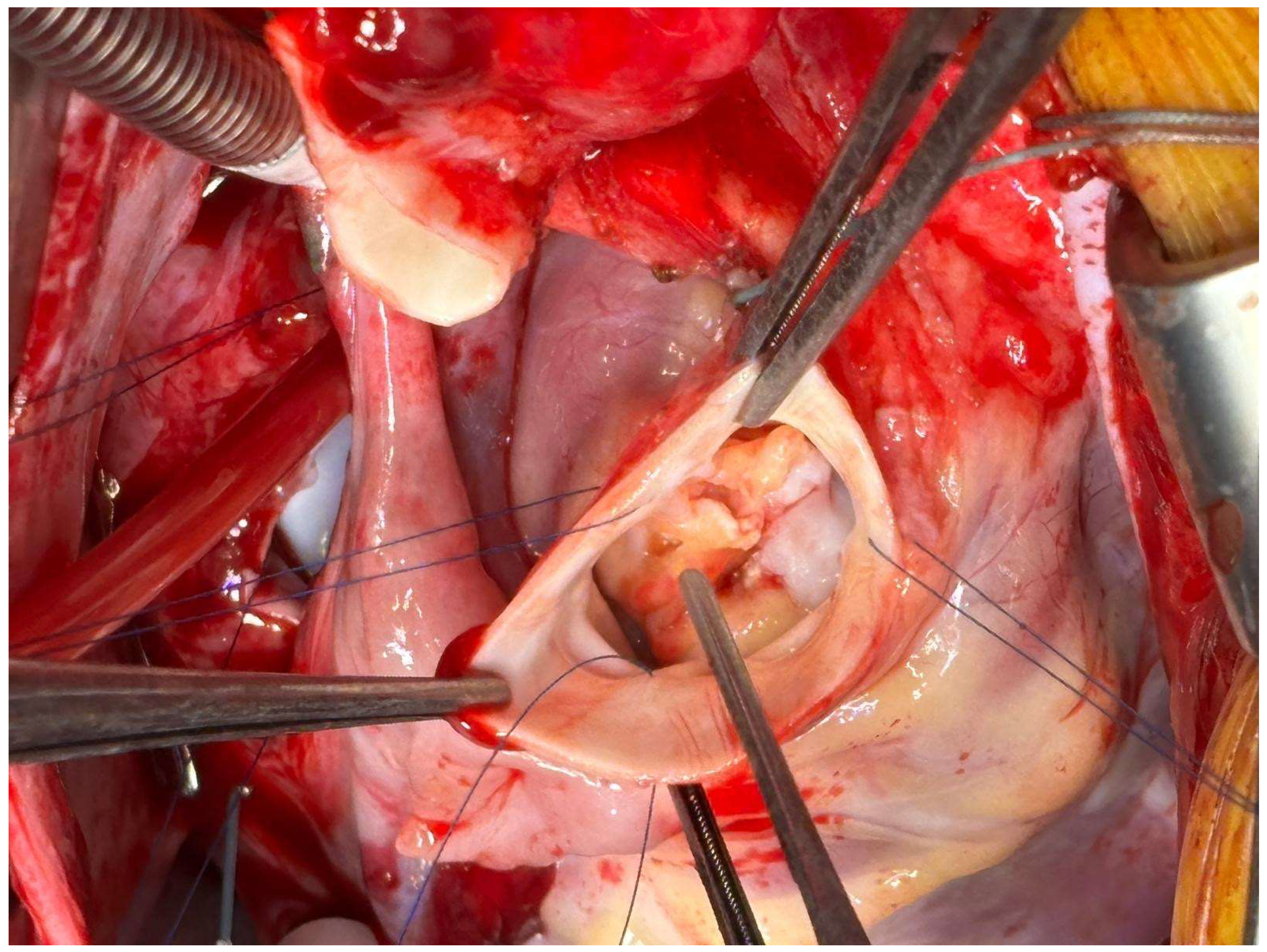
5. Infective Endocarditis After COVID-19
| Authors, Year | Title | Study Design and Size | Findings | Limitations |
|---|---|---|---|---|
| Quintero-Martinez et al., 2022 [31] | A clinical profile of infective endocarditis in patients with recent COVID-19: A systematic review | Systematic Review 21 cases | Systemic and endothelial inflammation could lead to IE Avoidance of echocardiography may underdiagnosed IE | Sample Size Retrospective Study |
| Bele et al., 2023 [32] | A Comprehensive Review on Cardiovascular Complications of COVID-19: Unraveling the Link to Bacterial Endocarditis | Review | Convergence of viral-induced endothelial dysfunction, immune dysregulation, and microbial translocation creates a conducive environment for bacterial colonization Early recognition of IE can significantly influence patient outcomes | Narrative Review |
| Taghizadeh-Waghefi et al., 2023 [37] | Cardiac Surgery for Treatment of COVID-19-Associated Infectious Endocarditis | Systematic Review 12 cases | Inflammatory response caused by SARS-CoV-2 may result in damage to the endocardium of native heart valves, a convenient site for bacterial infection Avoid delays in diagnosis and treatment to decrease mortality in patients with IE | Sample Size Retrospective Study |
| Mikus et al., 2024 [42] | Surgical Treatment of Active Endocarditis Pre- and Post-COVID-19 Pandemic Onset | Single Center Cohort Study 535 cases | Incidence of surgically treated IE significantly increases after COVID-19 Higher incidence of mitral valve involvement Mortality and outcomes unaffected | Retrospective Study |
| Novelli et al., 2023 [43] | Impact of the COVID-19 Pandemic on Infective Endocarditis Management and Outcomes: Analysis of a National Clinical Database | National Cohort Study 128,539 cases | Patients with IE after COVID-19 were more complex with worsened outcomes Patients who underwent surgery had stable outcomes and improved mortality despite the pandemic COVID-19 may predispose toward IE | Retrospective Study |
| Wang et al., 2022 [44] | Association of COVID-19 with endocarditis in patients with cocaine or opioid use disorders in the US | National Cohort Study 1,116,125 cases | COVID-19 associated with significantly increased risk for IE in patients with opioid or cocaine use disorders | Retrospective Study |
6. Diagnosis, Imaging, Current Challenges
7. Discussion
7.1. Rising Incidence and Changing Epidemiology
7.2. Personalized Antibiotic Prophylaxis
7.3. NBTE: Rule out in High-Risk Population
7.4. COVID-19 and IE: Never Postpone Diagnostic Process
8. Limitations
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| APLAS | Antiphospholipid Antibody Syndrome |
| ARDS | Acute Respiratory Distress Syndrome |
| BD | Behçet’s disease |
| CCT | Cardiac Computed Tomography |
| CHD | Congenital Heart Disease |
| CIED | Cardiac Implantable Electronic Device |
| FISH | Fluorescence In Situ Hybridization |
| HACEK | Haemophilus, Aggregatibacter, Cardiobacterium, Eikenella, Kingella |
| HCV | Hepatitis C Virus |
| IE | Infective Endocarditis |
| IDU | Intravenous Drug Use |
| MRI | Magnetic Resonance |
| MEET | Multidisciplinary Endocarditis Evaluation Team |
| MRSA | Methicillin-Resistant Staphylococcus Aureus |
| NBTE | Non-Bacterial Thrombotic Endocarditis |
| PET/CT | Positron Emission Tomography/Computed Tomography |
| PWID | People Who Inject Drugs |
| PCR | Polymerase Chain Reaction |
| SDI | Socio-Demographic Index |
| SLE | Systemic Lupus Erythematosus |
| TEE | Trans-Esophageal Echocardiogram |
| TTE | Trans-Thoracic Echocardiography |
| TAVI | Transcatheter Aortic Valve Implantation |
References
- Thuny, F.; Grisoli, D.; Cautela, J.; Riberi, A.; Raoult, D.; Habib, G. Infective Endocarditis: Prevention, Diagnosis, and Management. Can. J. Cardiol. 2014, 30, 1046–1057. [Google Scholar] [CrossRef]
- Rajani, R.; Klein, J.L. Infective Endocarditis: A Contemporary Update. Clin. Med. Lond. Engl. 2020, 20, 31–35. [Google Scholar] [CrossRef] [PubMed]
- Momtazmanesh, S.; Moghaddam, S.S.; Rad, E.M.; Azadnajafabad, S.; Ebrahimi, N.; Mohammadi, E.; Rouhifard, M.; Rezaei, N.; Masinaei, M.; Rezaei, N.; et al. Global, regional, and national burden and quality of care index of endocarditis: The global burden of disease study 1990–2019. Eur. J. Prev. Cardiol. 2022, 29, 1287–1297. [Google Scholar] [CrossRef]
- Hammond-Haley, M.; Hartley, A.; Al-Khayatt, B.M.; Delago, A.J.; Ghajar, A.; Ojha, U.; Marshall, D.C.; Salciccioli, J.D.; Prendergast, B.D.; Shalhoub, J. Trends in the Incidence and Mortality of Infective Endocarditis in High-Income Countries between 1990 and 2019. Int. J. Cardiol. 2023, 371, 441–451. [Google Scholar] [CrossRef]
- Arslan, M.; Kaleli, İ.; Kutlu, M. Prospective Clinical Follow-Up Results of Infective Endocarditis. Infect. Dis. Clin. Microbiol. 2024, 6, 133–140. [Google Scholar] [CrossRef]
- Carvajal, V.; Reyes, F.B.; Gonzalez, D.; Schwartz, M.; Whitlow, A.; Alegria, J.R. Endocarditis in Adult Congenital Heart Disease Patients: Prevention, Recognition, and Management. Curr. Cardiol. Rep. 2024, 26, 1031–1045. [Google Scholar] [CrossRef] [PubMed]
- Elgharably, H.; Sarhan, H.; Poddi, S.; Fraser, T.; Xu, B.; Pettersson, G.B. Sutureless and Trans-Catheter Valve Use in Aortic Valve Endocarditis: A Review. Heart Surg. Forum 2025, 28, E452–E461. [Google Scholar] [CrossRef]
- Pant, S.; Patel, N.J.; Deshmukh, A.; Golwala, H.; Patel, N.; Badheka, A.; Hirsch, G.A.; Mehta, J.L. Trends in Infective Endocarditis Incidence, Microbiology, and Valve Replacement in the United States from 2000 to 2011. J. Am. Coll. Cardiol. 2015, 65, 2070–2076. [Google Scholar] [CrossRef]
- Habib, G.; Erba, P.A.; Iung, B.; Donal, E.; Cosyns, B.; Laroche, C.; Popescu, B.A.; Prendergast, B.; Tornos, P.; Sadeghpour, A.; et al. Clinical Presentation, Aetiology and Outcome of Infective Endocarditis. Results of the ESC-EORP EURO-ENDO (European Infective Endocarditis) Registry: A Prospective Cohort Study. Eur. Heart J. 2019, 40, 3222–3232. [Google Scholar] [CrossRef] [PubMed]
- Iung, B.; Duval, X. Infective Endocarditis: Innovations in the Management of an Old Disease. Nat. Rev. Cardiol. 2019, 16, 623–635. [Google Scholar] [CrossRef] [PubMed]
- Comeaux, S.; Jamison, K.; Voeltz, M. Contemporary Features and Management of Endocarditis. Diagnostics 2023, 13, 3086. [Google Scholar] [CrossRef]
- Andreß, S.; Reischmann, K.; Markovic, S.; Rohlmann, F.; Hay, B.; Rottbauer, W.; Buckert, D.; d’Almeida, S. Men’s More Frequent Predisposing Factors in Infectious Endocarditis Facilitate Improvement of Outcomes by Shortening of Diagnostic Delay. Front. Cardiovasc. Med. 2025, 11, 1517288. [Google Scholar] [CrossRef]
- Bhandari, R.; Tiwari, S.; Alexander, T.; Annie, F.H.; Kaleem, U.; Irfan, A.; Balla, S.; Wiener, R.C.; Cook, C.; Nanjundappa, A.; et al. Sex Differences in Characteristics of Patients with Infective Endocarditis: A Multicenter Study. J. Clin. Med. 2022, 11, 3514. [Google Scholar] [CrossRef]
- Rudasill, S.E.; Sanaiha, Y.; Mardock, A.L.; Khoury, H.; Xing, H.; Antonios, J.W.; McKinnell, J.A.; Benharash, P. Clinical Outcomes of Infective Endocarditis in Injection Drug Users. J. Am. Coll. Cardiol. 2019, 73, 559–570. [Google Scholar] [CrossRef]
- Cahill, T.J.; Baddour, L.M.; Habib, G.; Hoen, B.; Salaun, E.; Pettersson, G.B.; Schäfers, H.J.; Prendergast, B.D. Challenges in Infective Endocarditis. J. Am. Coll. Cardiol. 2017, 69, 325–344. [Google Scholar] [CrossRef]
- Thornhill, M.H.; Crum, A.; Campbell, R.; Stone, T.; Lee, E.C.; Bradburn, M.; Fibisan, V.; Dayer, M.; Prendergast, B.D.; Lockhart, P.; et al. Temporal Association between Invasive Procedures and Infective Endocarditis. Heart Br. Card. Soc. 2023, 109, 223–231. [Google Scholar] [CrossRef] [PubMed]
- Hubers, S.A.; DeSimone, D.C.; Gersh, B.J.; Anavekar, N.S. Infective Endocarditis: A Contemporary Review. Mayo Clin. Proc. 2020, 95, 982–997. [Google Scholar] [CrossRef]
- Havers-Borgersen, E.; Butt, J.H.; Østergaard, L.; Petersen, J.K.; Torp-Pedersen, C.; Køber, L.; Fosbøl, E.L. Long-Term Incidence of Infective Endocarditis among Patients with Congenital Heart Disease. Am. Heart J. 2023, 259, 9–20. [Google Scholar] [CrossRef] [PubMed]
- Fedchenko, M.; Giang, K.W.; Snygg-Martin, U.; Dellborg, M.; Mandalenakis, Z. Risk and Predictors of First-Time Infective Endocarditis in Adult Patients with Congenital Heart Disease-A Nationwide, Register-Based Study. Int. J. Cardiol. 2025, 426, 133081. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, O.; King, N.E.; Qureshi, M.A.; Choudhry, A.A.; Osama, M.; Zehner, C.; Ali, A.; Hamzeh, I.R.; Palaskas, N.L.; Thompson, K.A.; et al. Non-Bacterial Thrombotic Endocarditis: A Clinical and Pathophysiological Reappraisal. Eur. Heart J. 2025, 46, 236–249. [Google Scholar] [CrossRef]
- Zmaili, M.; Alzubi, J.; Lo Presti Vega, S.; Ababneh, E.; Xu, B. Non-Bacterial Thrombotic Endocarditis: A State-of-the-Art Contemporary Review. Prog. Cardiovasc. Dis. 2022, 74, 99–110. [Google Scholar] [CrossRef]
- Al Chalaby, S.; Makhija, R.R.; Sharma, A.N.; Majid, M.; Aman, E.; Venugopal, S.; Amsterdam, E.A. Nonbacterial Thrombotic Endocarditis: Presentation, Pathophysiology, Diagnosis and Management. Rev. Cardiovasc. Med. 2022, 23, 137. [Google Scholar] [CrossRef] [PubMed]
- Kuipers, R.S.; Berghuis, M.A.T.; Ogilvie, A.C.; van Wissen, S.A.; Riezebos, R.K. Non-Bacterial Thrombotic Endocarditis Manifested by Ventricular Fibrillation in a Patient with Low Grade Ovarian Carcinoma: Case Report and Literature Review. Eur. Heart J. Case Rep. 2021, 5, ytab120. [Google Scholar] [CrossRef] [PubMed]
- Kania, B.; Mekheal, E.; Veeraballi, S.; Bondili, L.; Maroules, M. A Rare Case of Metastatic Pancreatic Adenocarcinoma Presenting as a Pulmonary Embolism from Nonbacterial Thrombotic Endocarditis. Radiol. Case Rep. 2022, 17, 3097–3102. [Google Scholar] [CrossRef]
- Dietrich, M.; Bois, M.; Ferrufino, R.; Cobey, F.; Mankad, R. A Tale of Two Valves: Bioprosthetic Aortic Valve Obstruction in Systemic Lupus Erythematosus and Antiphospholipid Antibody Syndrome. J. Cardiothorac. Vasc. Anesth. 2020, 34, 3462–3466. [Google Scholar] [CrossRef] [PubMed]
- Zmaili, M.A.; Alzubi, J.M.; Kocyigit, D.; Bansal, A.; Samra, G.S.; Grimm, R.; Griffin, B.P.; Xu, B. A Contemporary 20-Year Cleveland Clinic Experience of Nonbacterial Thrombotic Endocarditis: Etiology, Echocardiographic Imaging, Management, and Outcomes. Am. J. Med. 2021, 134, 361–369. [Google Scholar] [CrossRef]
- Mazzoni, C.; Scheggi, V.; Mariani, T. Cardiac Involvement in Behçet Disease Presenting as Non-Bacterial Thrombotic Endocarditis: A Case Report. J. Cardiol. Cases 2021, 24, 157–160. [Google Scholar] [CrossRef]
- Patrzałek, P.; Zawada, T.; Stolarski, Ł.; Kamińska, M.; Kaczmarek, W. Non-bacterial Thrombotic Endocarditis (NBTE) in the Absence of Malignancy or Lupus Anticoagulant/Antiphospholipid Antibodies: A Case Report. Cureus 2024, 16, e59336. [Google Scholar] [CrossRef]
- Chan, K.H.; Joseph, O.; Ahmed, E.; Kommidi, A.; Suleiman, A.; Szabela, M.E.; Slim, J. Marantic Endocarditis Associated with COVID-19: A Rare Case Report of a Potentially Deadly Disease. Eur. J. Case Rep. Intern. Med. 2021, 8, 002409. [Google Scholar] [CrossRef]
- Raisi-Estabragh, Z.; Mamas, M.A. Cardiovascular Health Care Implications of the COVID-19 Pandemic. Cardiol. Clin. 2022, 40, 389–396. [Google Scholar] [CrossRef]
- Quintero-Martinez, J.A.; Hindy, J.-R.; Mahmood, M.; Gerberi, D.J.; DeSimone, D.C.; Baddour, L.M. A Clinical Profile of Infective Endocarditis in Patients with Recent COVID-19: A Systematic Review. Am. J. Med. Sci. 2022, 364, 16–22. [Google Scholar] [CrossRef]
- Bele, A.; Wagh, V.; Munjewar, P.K. A Comprehensive Review on Cardiovascular Complications of COVID-19: Unraveling the Link to Bacterial Endocarditis. Cureus 2023, 15, e44019. [Google Scholar] [CrossRef]
- George, A.; Venkataramanan, S.V.A.; John, K.J.; Mishra, A.K. Infective endocarditis and COVID-19 coinfection: An updated review. Acta Biomed. 2022, 93, e2022030. [Google Scholar] [CrossRef]
- Milovančev, A.; Miljković, T.; Petrović, M.; Kovačević, M.; Ilić, A.; Bjelobrk, M.; Lozanov-Crvenković, Z.; Milosavljević, A.S.; Tadić, S.; Bulatović, T. Impact of the COVID-19 Pandemic on Cardiology Emergency Department Visits. Int. Heart J. 2022, 63, 749–754. [Google Scholar] [CrossRef] [PubMed]
- Khan, Y.; Verhaeghe, N.; Devleesschauwer, B.; Cavillot, L.; Gadeyne, S.; Pauwels, N.; Van den Borre, L.; De Smedt, D. The Impact of the COVID-19 Pandemic on Delayed Care of Cardiovascular Diseases in Europe: A Systematic Review. Eur. Heart J. Qual. Care Clin. Outcomes 2023, 9, 647–661. [Google Scholar] [CrossRef] [PubMed]
- Lorusso, R.; Calafiore, A.M.; Di Mauro, M. Acute Infective Endocarditis during COVID-19 Pandemic Time: The Dark Side of the Moon. J. Card. Surg. 2022, 37, 1168–1170. [Google Scholar] [CrossRef]
- Taghizadeh-Waghefi, A.; Petrov, A.; Wilbring, M.; Alexiou, K.; Kappert, U.; Matschke, K.; Tugtekin, S.M. Cardiac Surgery for Treatment of COVID-19-Associated Infectious Endocarditis. Tex. Heart Inst. J. 2023, 50, e227884. [Google Scholar] [CrossRef]
- Pommier, T.; Benzenine, E.; Bernard, C.; Mariet, A.-S.; Béjot, Y.; Giroud, M.; Morgant, M.-C.; Steinmetz, E.; Guenancia, C.; Bouchot, O.; et al. Trends of Myocarditis and Endocarditis Cases before, during, and after the First Complete COVID-19-Related Lockdown in 2020 in France. Biomedicines 2022, 10, 1231. [Google Scholar] [CrossRef]
- Spinoni, E.G.; Degiovanni, A.; Della Corte, F.; Patti, G. Infective Endocarditis Complicating COVID-19 Pneumonia: A Case Report. Eur. Heart J. Case Rep. 2020, 4, 1–5. [Google Scholar] [CrossRef]
- Sawada, K.; Kawaji, T.; Yamana, K.; Matsuhashi, K.; Hara, Y.; Kuriyama, N.; Nakamura, T.; Maekawa, A.; Takagi, Y.; Nishida, O. Veno-Venous Extracorporeal Membrane Oxygenation for Perioperative Management of Infective Endocarditis after COVID-19 with Acute Respiratory Distress Syndrome: A Case Report. J. Cardiothorac. Surg. 2024, 19, 358. [Google Scholar] [CrossRef]
- Kraiem, S.; Amor, H.I.H. Bi-Valvular Endocarditis Occurring 2 Months after COVID-19 Infection. Pan Afr. Med. J. 2021, 39, 37. [Google Scholar] [CrossRef]
- Mikus, E.; Fiorentino, M.; Sangiorgi, D.; Fiaschini, C.; Tenti, E.; Tremoli, E.; Calvi, S.; Costantino, A.; Tripodi, A.; Zucchetta, F.; et al. Surgical Treatment of Active Endocarditis Pre- and Post-COVID-19 Pandemic Onset. Biomedicines 2024, 12, 233. [Google Scholar] [CrossRef]
- Novelli, A.; Ingason, A.B.; Jirka, C.; Callas, P.; Hirashima, F.; Lovoulos, C.; Dauerman, H.L.; Polomsky, M. Impact of the COVID-19 Pandemic on Infective Endocarditis Management and Outcomes: Analysis of a National Clinical Database. Am. J. Cardiol. 2023, 209, 224–231. [Google Scholar] [CrossRef]
- Wang, L.; Volkow, N.D.; Berger, N.A.; Davis, P.B.; Kaelber, D.C.; Xu, R. Association of COVID-19 with endocarditis in patients with cocaine or opioid use disorders in the US. Mol. Psychiatry 2023, 28, 543–552. [Google Scholar] [CrossRef]
- Sebastian, S.A.; Co, E.L.; Mehendale, M.; Sudan, S.; Manchanda, K.; Khan, S. Challenges and Updates in the Diagnosis and Treatment of Infective Endocarditis. Curr. Probl. Cardiol. 2022, 47, 101267. [Google Scholar] [CrossRef] [PubMed]
- Kirk, F.; Vaselli, N.M. Blood Culture-Negative Infective Endocarditis: Are We Looking Hard Enough? Infection 2023, 51, 1629–1631. [Google Scholar] [CrossRef]
- Fowler, V.G.; Durack, D.T.; Selton-Suty, C.; Athan, E.; Bayer, A.S.; Chamis, A.L.; Dahl, A.; DiBernardo, L.; Durante-Mangoni, E.; Duval, X.; et al. The 2023 Duke-International Society for Cardiovascular Infectious Diseases Criteria for Infective Endocarditis: Updating the Modified Duke Criteria. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2023, 77, 518–526. [Google Scholar] [CrossRef]
- Jain, V.; Wang, T.K.M.; Bansal, A.; Farwati, M.; Gad, M.; Montane, B.; Kaur, S.; Bolen, M.A.; Grimm, R.; Griffin, B.; et al. Diagnostic Performance of Cardiac Computed Tomography versus Transesophageal Echocardiography in Infective Endocarditis: A Contemporary Comparative Meta-Analysis. J. Cardiovasc. Comput. Tomogr. 2021, 15, 313–321. [Google Scholar] [CrossRef] [PubMed]
- Tonutti, A.; Scarfò, I.; La Canna, G.; Selmi, C.; De Santis, M. Diagnostic Work-Up in Patients with Nonbacterial Thrombotic Endocarditis. J. Clin. Med. 2023, 12, 5819. [Google Scholar] [CrossRef]
- Lo Presti, S.; Elajami, T.K.; Zmaili, M.; Reyaldeen, R.; Xu, B. Multimodality Imaging in the Diagnosis and Management of Prosthetic Valve Endocarditis: A Contemporary Narrative Review. World J. Cardiol. 2021, 13, 254–270. [Google Scholar] [CrossRef] [PubMed]
- Wahadat, A.R.; Tanis, W.; Galema, T.W.; Swart, L.E.; van Leeuwen, W.J.; Verkaik, N.J.; Schurink, C.A.M.; van Dalen, B.; Zoet-Nugteren, S.; Gurlek, C.; et al. The Impact of the Multidisciplinary Endocarditis Team on the Management of Infective Endocarditis. Neth. Heart J. 2023, 31, 29–35. [Google Scholar] [CrossRef]
- Diab, M.; Franz, M.; Hagel, S.; Guenther, A.; Struve, A.; Musleh, R.; Penzel, A.; Sponholz, C.; Lehmann, T.; Kuehn, H.; et al. Impact of an In-Hospital Endocarditis Team and a State-Wide Endocarditis Network on Perioperative Outcomes. J. Clin. Med. 2021, 10, 4734. [Google Scholar] [CrossRef] [PubMed]
- Cimmino, G.; Bottino, R.; Formisano, T.; Orlandi, M.; Molinari, D.; Sperlongano, S.; Castaldo, P.; D’Elia, S.; Carbone, A.; Palladino, A.; et al. Current Views on Infective Endocarditis: Changing Epidemiology, Improving Diagnostic Tools and Centering the Patient for Up-to-Date Management. Life 2023, 13, 377. [Google Scholar] [CrossRef]
- Nappi, F.; Martuscelli, G.; Bellomo, F.; Avtaar Singh, S.S.; Moon, M.R. Infective Endocarditis in High-Income Countries. Metabolites 2022, 12, 682. [Google Scholar] [CrossRef]
- Miao, H.; Zhang, Y.; Zhang, Y.; Zhang, J. Update on the Epidemiology, Diagnosis, and Management of Infective Endocarditis: A Review. Trends Cardiovasc. Med. 2024, 34, 499–506. [Google Scholar] [CrossRef]
- Barocas, J.A.; Morgan, J.R.; Wang, J.; McLoone, D.; Wurcel, A.; Stein, M.D. Outcomes Associated With Medications for Opioid Use Disorder Among Persons Hospitalized for Infective Endocarditis. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2021, 72, 472–478. [Google Scholar] [CrossRef]
- Weimer, M.B.; Falker, C.G.; Seval, N.; Golden, M.; Hull, S.C.; Geirsson, A.; Vallabhajosyula, P. The Need for Multidisciplinary Hospital Teams for Injection Drug Use-Related Infective Endocarditis. J. Addict. Med. 2022, 16, 375–378. [Google Scholar] [CrossRef]
- Delgado, V.; Marsan, N.A.; de Waha, S.; Bonaros, N.; Brida, M.; Burri, H.; Caselli, S.; Doenst, T.; Ederhy, S.; Erba, P.A.; et al. ESC Scientific Document Group. 2023 ESC Guidelines for the management of endocarditis. Eur. Heart J. 2023, 44, 3948–4042, Erratum in Eur. Heart J. 2023, 44, 4780; Erratum in Eur. Heart J. 2024, 45, 56; Erratum in Eur. Heart J. 2025, 46, 1082. [Google Scholar] [CrossRef]
- Santarpino, G.; Lofrumento, F.; Zito, C.; Trio, O.; Restelli, D.; Piccione, M.C.; Manganaro, R.; Carerj, S.; Cardetta, F.; Fiore, C.; et al. Exploring the Complexities of Non-Bacterial Thrombotic Endocarditis: Highlights from Literature and Case Studies. J. Clin. Med. 2024, 13, 4904. [Google Scholar] [CrossRef] [PubMed]
- Petkovic, A.; Menkovic, N.; Petrovic, O.; Bilbija, I.; Nisevic, M.; Radovanovic, N.N. Imaging in Infective Endocarditis-Current Opinions and Trends in Cardiac Computed Tomography. Diagnostics 2024, 14, 1355. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lefter, C.L.; Poddi, S.; Rungatscher, A. Endocarditis: Rising Incidence in the Post-COVID-19 Pandemic Era: A Narrative Review. J. Clin. Med. 2025, 14, 7274. https://doi.org/10.3390/jcm14207274
Lefter CL, Poddi S, Rungatscher A. Endocarditis: Rising Incidence in the Post-COVID-19 Pandemic Era: A Narrative Review. Journal of Clinical Medicine. 2025; 14(20):7274. https://doi.org/10.3390/jcm14207274
Chicago/Turabian StyleLefter, Cynthia L., Salvatore Poddi, and Alessio Rungatscher. 2025. "Endocarditis: Rising Incidence in the Post-COVID-19 Pandemic Era: A Narrative Review" Journal of Clinical Medicine 14, no. 20: 7274. https://doi.org/10.3390/jcm14207274
APA StyleLefter, C. L., Poddi, S., & Rungatscher, A. (2025). Endocarditis: Rising Incidence in the Post-COVID-19 Pandemic Era: A Narrative Review. Journal of Clinical Medicine, 14(20), 7274. https://doi.org/10.3390/jcm14207274





