Anatomical Risk Patterns for Patellofemoral Instability in Skeletally Immature Patients: A Sex-Stratified MRI Study
Abstract
1. Introduction
2. Materials and Methods
2.1. MRI Measurements
2.2. Statistical Analysis
3. Results
3.1. Patient Demographics
3.2. Trochlea Dysplasia
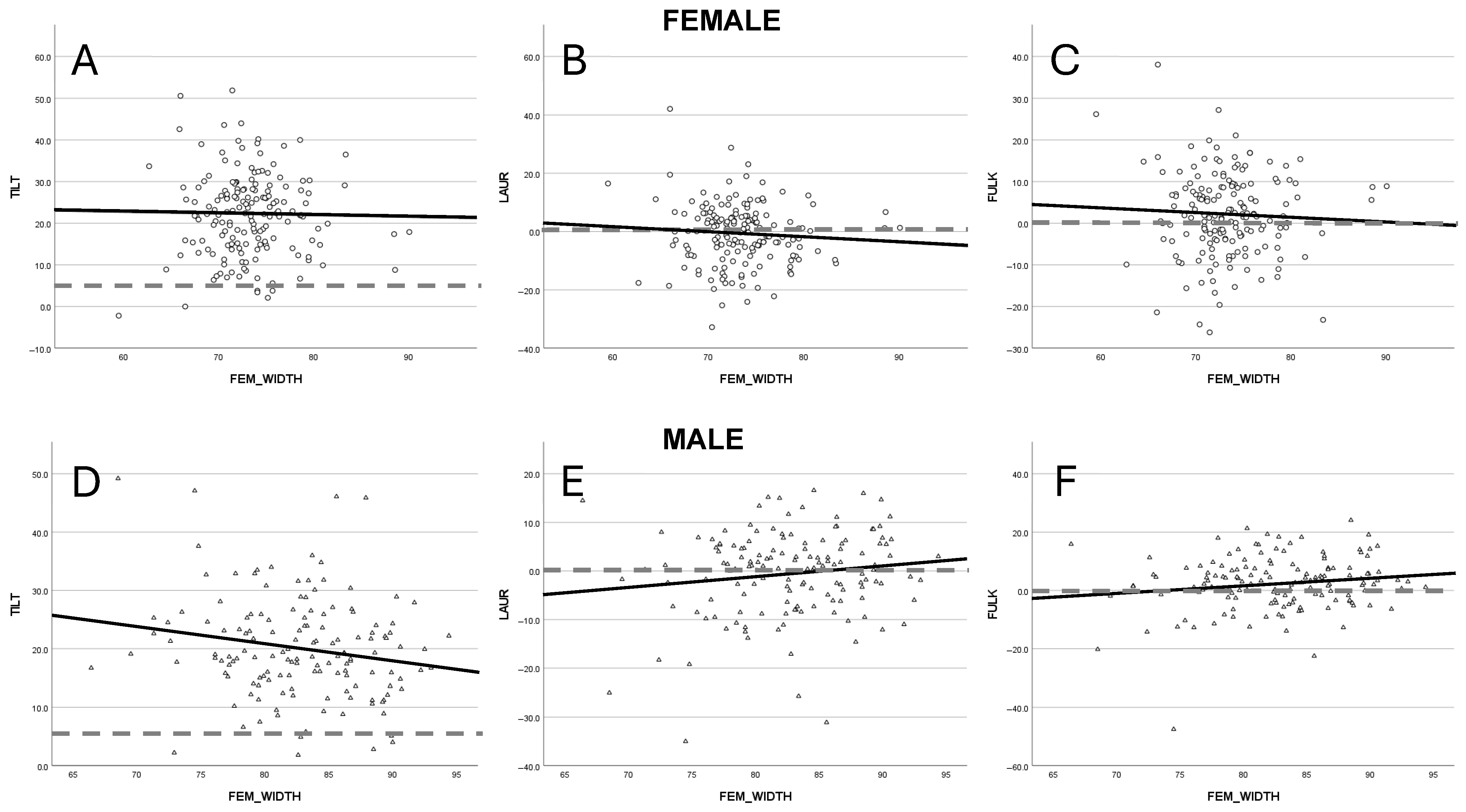
3.3. Patellar Tilt
3.4. Axial Patellar Positioning
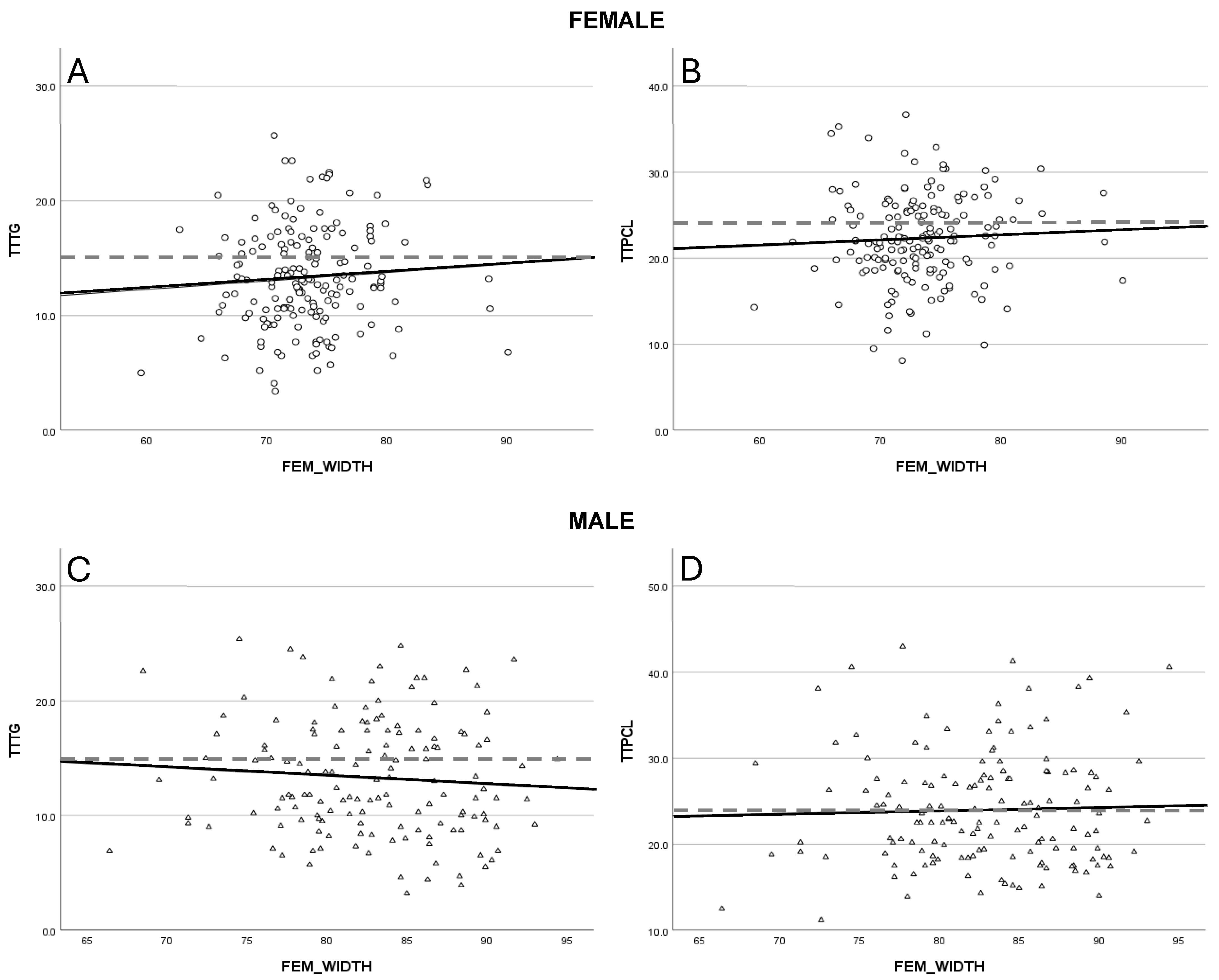
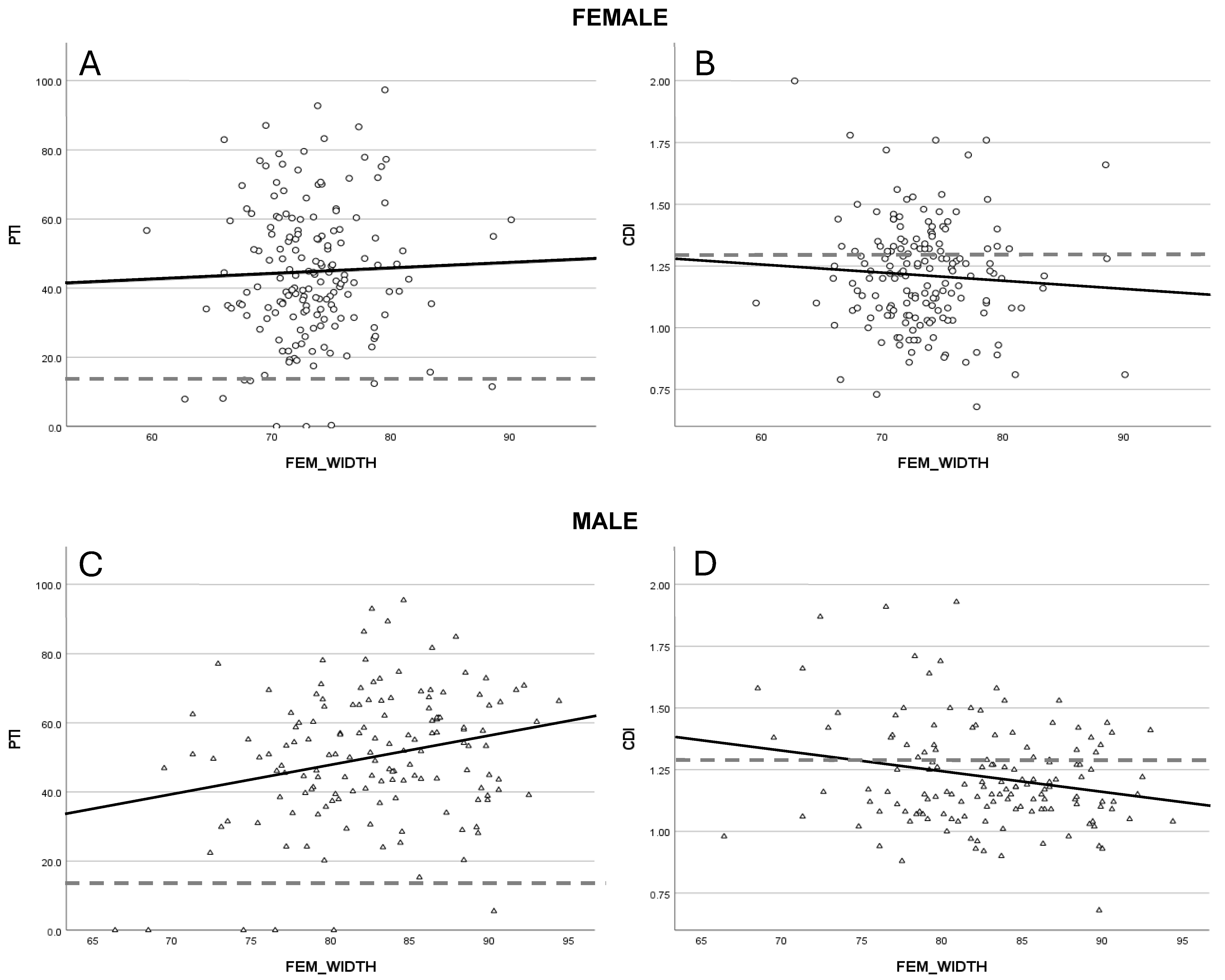
3.5. Sagittal Patellofemoral Alignment
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hasler, C.C.; Studer, D. Patella instability in children and adolescents. EFORT Open Rev. 2017, 1, 160–166. [Google Scholar] [CrossRef] [PubMed]
- Mistovich, R.J.; Urwin, J.W.; Fabricant, P.D.; Lawrence, J.T.R. Patellar tendon–lateral trochlear ridge distance: A novel measurement of patellofemoral instability. Am. J. Sports Med. 2018, 46, 3400–3406. [Google Scholar] [CrossRef] [PubMed]
- Sanders, T.L.; Pareek, A.; Hewett, T.E.; Stuart, M.J.; Dahm, D.L.; Krych, A.J. Incidence of first-time lateral patellar dislocation: A 21-year population-based study. Sports Health 2018, 10, 146–151. [Google Scholar] [CrossRef] [PubMed]
- Sanders, T.L.; Pareek, A.; Johnson, N.R.; Stuart, M.J.; Dahm, D.L.; Krych, A.J. Patellofemoral arthritis after lateral patellar dislocation: A matched population-based analysis. Am. J. Sports Med. 2017, 45, 1012–1017. [Google Scholar] [CrossRef]
- Arendt, E.A.; Dejour, D.; Ntagiopoulos, P.G.; Sillanpää, P.; Feller, J.; Karlsson, J.; Servien, E. An analysis of knee anatomic imaging factors associated with primary lateral patellar dislocations. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 3099–3310. [Google Scholar] [CrossRef]
- Duthon, V.B. Acute traumatic patellar dislocation. Orthop. Traumatol. Surg. Res. 2015, 101 (Suppl. S1), S59–S67. [Google Scholar] [CrossRef]
- Mitchell, J.; Magnussen, R.A.; Collins, C.L.; Best, T.M.; Albright, J.P.; Boden, B.P.; Comstock, R.D. Epidemiology of patellofemoral instability injuries among high school athletes in the United States. Am. J. Sports Med. 2015, 43, 1676–1682. [Google Scholar] [CrossRef]
- Weltsch, D.; Heidenreich, M.J.; Miller, P.E.; Anderson, C.N.; Tompkins, M.A.; Arendt, E.A. Predicting risk of recurrent patellofemoral instability with measurements of extensor mechanism containment. Am. J. Sports Med. 2021, 49, 706–712. [Google Scholar] [CrossRef]
- Zhang, G.; Ding, Y.; Yang, J.; Yu, C.; Yang, J.; Du, X. Incidence of second-time lateral patellar dislocation is associated with anatomic factors, age, and injury patterns of medial patellofemoral ligament in first-time lateral patellar dislocation: A prospective magnetic resonance imaging study with 5-year follow-up. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 197–205. [Google Scholar]
- Zheng, E.T.; Chambers, C.C.; Sanders, T.G.; Lavery, K.P.; Kraeutler, M.J. Descriptive epidemiology of a surgical patellofemoral instability population of 492 patients. Orthop. J. Sports Med. 2022, 10, 23259671221108174. [Google Scholar] [CrossRef]
- Biedert, R.M.; Albrecht, S. The patellotrochlear index: A new index for assessing patellar height. Knee Surg. Sports Traumatol. Arthrosc. 2006, 14, 707–712. [Google Scholar] [CrossRef] [PubMed]
- Charles, M.D.; Haloman, S.; Chen, L.; Ward, S.R.; Fithian, D.; Afra, R. Magnetic resonance imaging-based topographical differences between control and recurrent patellofemoral instability patients. Am. J. Sports Med. 2013, 41, 374–384. [Google Scholar] [CrossRef] [PubMed]
- Jimenez, A.E.; Levy, B.J.; Grimm, N.L.; Andelman, S.M.; Cheng, C.; Hedgecock, J.P.; Cohen, A.; Pace, J.L. Relationship between patellar morphology and known anatomic risk factors for patellofemoral instability. Orthop J Sports Med. 2021, 9, 2325967120988690. [Google Scholar] [CrossRef]
- Kim, H.K.; Shiraj, S.; Kang, C.H.; Anton, C.; Kim, D.H.; Horn, P.S. Patellofemoral instability in children: Correlation between risk factors, injury patterns, and severity of cartilage damage. AJR Am. J. Roentgenol. 2016, 206, 1321–1328. [Google Scholar] [CrossRef]
- Orellana, K.J.; Batley, M.G.; Lawrence, J.T.R.; Nguyen, J.C.; Williams, B.A. Radiographic evaluation of pediatric patients with patellofemoral instability. Curr. Rev. Musculoskelet. Med. 2022, 15, 411–426. [Google Scholar] [CrossRef]
- Paul, R.W.; Brutico, J.M.; Wright, M.L.; Erickson, B.J.; Tjoumakaris, F.P.; Freedman, K.B.; Bishop, M.E. Strong agreement between magnetic resonance imaging and radiographs for Caton-Deschamps index in patients with patellofemoral instability. Arthrosc. Sports Med. Rehabil. 2021, 3, 1621–1628. [Google Scholar] [CrossRef]
- Stepanovich, M.; Bomar, J.D.; Pennock, A.T. Are the current classifications and radiographic measurements for trochlear dysplasia appropriate in the skeletally immature patient? Orthop. J. Sports Med. 2016, 4, 2325967116669490. [Google Scholar] [CrossRef]
- Toms, A.P.; Cahir, J.; Swift, L.; Donell, S.T. Imaging the femoral sulcus with ultrasound, CT, and MRI: Reliability and generalizability in patients with patellar instability. Skelet. Radiol. 2009, 38, 329–338. [Google Scholar] [CrossRef]
- Christensen, T.C.; Sanders, T.L.; Pareek, A.; Mohan, R.; Dahm, D.L.; Krych, A.J. Risk factors and time to recurrent ipsilateral and contralateral patellar dislocations. Am. J. Sports Med. 2017, 45, 2105–2110. [Google Scholar] [CrossRef]
- Dietrich, T.J.; Fucentese, S.F.; Pfirrmann, C.W.A. Imaging of individual anatomical risk factors for patellar instability. Semin. Musculoskelet. Radiol. 2016, 20, 65–73. [Google Scholar] [CrossRef] [PubMed]
- Fithian, D.C.; Paxton, E.W.; Stone, M.L.; Silva, P.; Davis, D.K.; Elias, D.A.; White, L.M. Epidemiology and natural history of acute patellar dislocation. Am. J. Sports Med. 2004, 32, 1114–1121. [Google Scholar] [CrossRef]
- Baxter-Jones, A.D.G.; Jackowski, S.A. Sex differences in bone mineral content and bone geometry accrual: A review of the Paediatric Bone Mineral Accrual Study (1991–2017). Ann. Hum. Biol. 2021, 48, 503–516. [Google Scholar] [CrossRef] [PubMed]
- Degen, N.; Sass, J.; Jalali, J.; Kovacs, L.; Euler, E.; Prall, W.C.; Böcker, W.; Thaller, P.H.; Fürmetz, J. Three-dimensional assessment of lower limb alignment: Reference values and sex-related differences. Knee 2020, 27, 428–435. [Google Scholar] [CrossRef] [PubMed]
- Pringle, L.C.; Tanaka, M.J.; Fayad, L.M. Lady or gentleman? Sex differences in osseous and cartilaginous structures of the knee. Int. J. Sports Exerc. Med. 2019, 5, 153. [Google Scholar] [CrossRef]
- Pruneski, J.; Mara, L.O.; Perrone, G.S.; Kiapour, A.M. Changes in anatomic risk factors for patellar instability during skeletal growth and maturation. Am. J. Sports Med. 2021, 29, 2424–2432. [Google Scholar] [CrossRef]
- Thévenin-Lemoine, C.; Ferrand, M.; Courvoisier, A.; Damsin, J.P.; Le Pointe, H.D.; Vialle, R. Is the Caton-Deschamps index a valuable ratio to investigate patellar height in children? J. Bone Jt. Surg. Am. 2011, 93, e35. [Google Scholar] [CrossRef]
- Nguyen, A.D.; Shultz, S.J. Sex differences in clinical measures of lower extremity alignment. J. Orthop. Sports Phys. Ther. 2007, 37, 389–398. [Google Scholar] [CrossRef]
- Nieves, J.W. Sex differences in skeletal growth and aging. Curr. Osteoporos. Rep. 2017, 15, 70–75. [Google Scholar] [CrossRef]
- Hirschmann, M.T.; Bonnin, M.P. Abandon the mean value thinking: Personalized medicine an intuitive way for improved outcomes in orthopaedics. Knee Surg. Sports Traumatol. Arthrosc. 2024, 32, 3129–3132. [Google Scholar] [CrossRef]
- Choi, W.; Lee, S.; Oh, J.; Baek, H.; Yang, J.; Shin, J. Magnetic resonance imaging of patellofemoral morphometry reveals age and gender variations in the knees of children and adolescents. Diagnostics 2021, 11, 1985. [Google Scholar] [CrossRef]
- Hou, G.; Li, K.; Cao, W.; Tian, W.; Zhang, J.; Wang, Y. Growth charts for children aged 6–17 years in Shanxi, China: Comparison with other cities of China and WHO. BMC Pediatr. 2024, 24, 423. [Google Scholar] [CrossRef]
- Khadilkar, V.; Oza, C.; Khadilkar, A. Relationship between height age, bone age and chronological age in normal children in the context of nutritional and pubertal status. J. Pediatr. Endocrinol. Metab. 2022, 35, 767–775. [Google Scholar] [CrossRef] [PubMed]
- Maloney, E.; Stanescu, A.L.; Ngo, A.V.; Parisi, M.T.; Iyer, R.S. The pediatric patella: Normal development, anatomical variants and malformations, stability, imaging, and injury patterns. Semin. Musculoskelet. Radiol. 2018, 22, 81–94. [Google Scholar] [CrossRef] [PubMed]
- Shelbourne, K.D.; Kerr, B. The relationship of femoral intercondylar notch width to height, weight, and sex in patients with intact anterior cruciate ligaments. Am. J. Knee Surg. 2001, 14, 92–96. [Google Scholar]
- Geraghty, L.; Humphries, D.; Fitzpatrick, J. Assessment of reliability and validity of imaging measurements for patellofemoral instability: An updated systematic review. Skelet. Radiol 2022, 51, 2245–2256. [Google Scholar] [CrossRef]
- Orellana, K.J.; Lee, J.; Yang, D.; Kell, D.; Nguyen, J.; Lawrence, J.T.; Williams, B.A. Trochlear morphological changes in skeletally immature patients across consecutive MRI studies. Am. J. Sports Med. 2025, 53, 690–698. [Google Scholar] [CrossRef]
- Parikh, S.N.; Rajdev, N.; Sun, Q. The growth of trochlear dysplasia during adolescence. J. Pediatr. Orthop. 2018, 38, e318–e324. [Google Scholar] [CrossRef]
- Pagliazzi, G.; Ellermann, J.M.; Carlson, C.S.; Shea, K.G.; Arendt, E.A. Trochlear development in children from 1 month to 10 years of age: A descriptive study utilizing analysis by magnetic resonance imaging. Orthop. J. Sports Med. 2021, 9, 23259671211028269. [Google Scholar] [CrossRef]
- Dong, C.; Zhao, C.; Li, M.; Fan, C.; Feng, X.; Piao, K.; Hao, K.; Wang, F. Accuracy of tibial tuberosity–trochlear groove distance and tibial tuberosity–posterior cruciate ligament distance in terms of the severity of trochlear dysplasia. J. Orthop. Surg. Res. 2021, 16, 383. [Google Scholar] [CrossRef]
- Yao, L.; Gai, N.; Boutin, R.D. Axial scan orientation and the tibial tubercle–trochlear groove distance: Error analysis and correction. AJR Am. J. Roentgenol. 2014, 202, 1291–1296. [Google Scholar] [CrossRef]
- Silvers-Granelli, H.J.; Bizzini, M.; Aurndale, A.; Mandelbaum, B.D.; Snyder-Mackler, L. DOes the FIFIA 11+ injury prevention program reduce the incidence of ACL injury in male soccer players? Clin. Orthop. Relat. Res. 2017, 475, 2447–2455. [Google Scholar] [CrossRef]
- Sanchis, G.J.B.; Lopes, J.M.; Assis, S.J.C.; Catão, R.L.A.; Santos, T.R.T.; Roncalli, A.G.D.C.O. Dynamic knee valgus prevalence in children and its association with pain intensity, foot mobility, and sex—A cross-sectional study. Heliyon 2022, 8, e10984. [Google Scholar] [CrossRef]
- Hodel, S.; Imhoff, F.B.; Strutzenberger, G.; Fitze, D.; Obrist, S.; Vlachopoulos, L.; Scherr, J.; Fucentese, S.F.; Fröhlich, S.; Spörri, J. Greater hip internal rotation range of motion is associated with increased dynamic knee valgus during jump landing, both before and after fatigue. Knee Surg. Sports Traumatol. Arthrosc. 2025, 33, 1560–1568. [Google Scholar] [CrossRef]
- Kernozek, T.W.; Torry, M.R.; Iwasaki, M. Gender differences in lower extremity landing mechanics caused by neuromuscular fatigue. Am. J. Sports Med. 2008, 36, 554–565. [Google Scholar] [CrossRef] [PubMed]
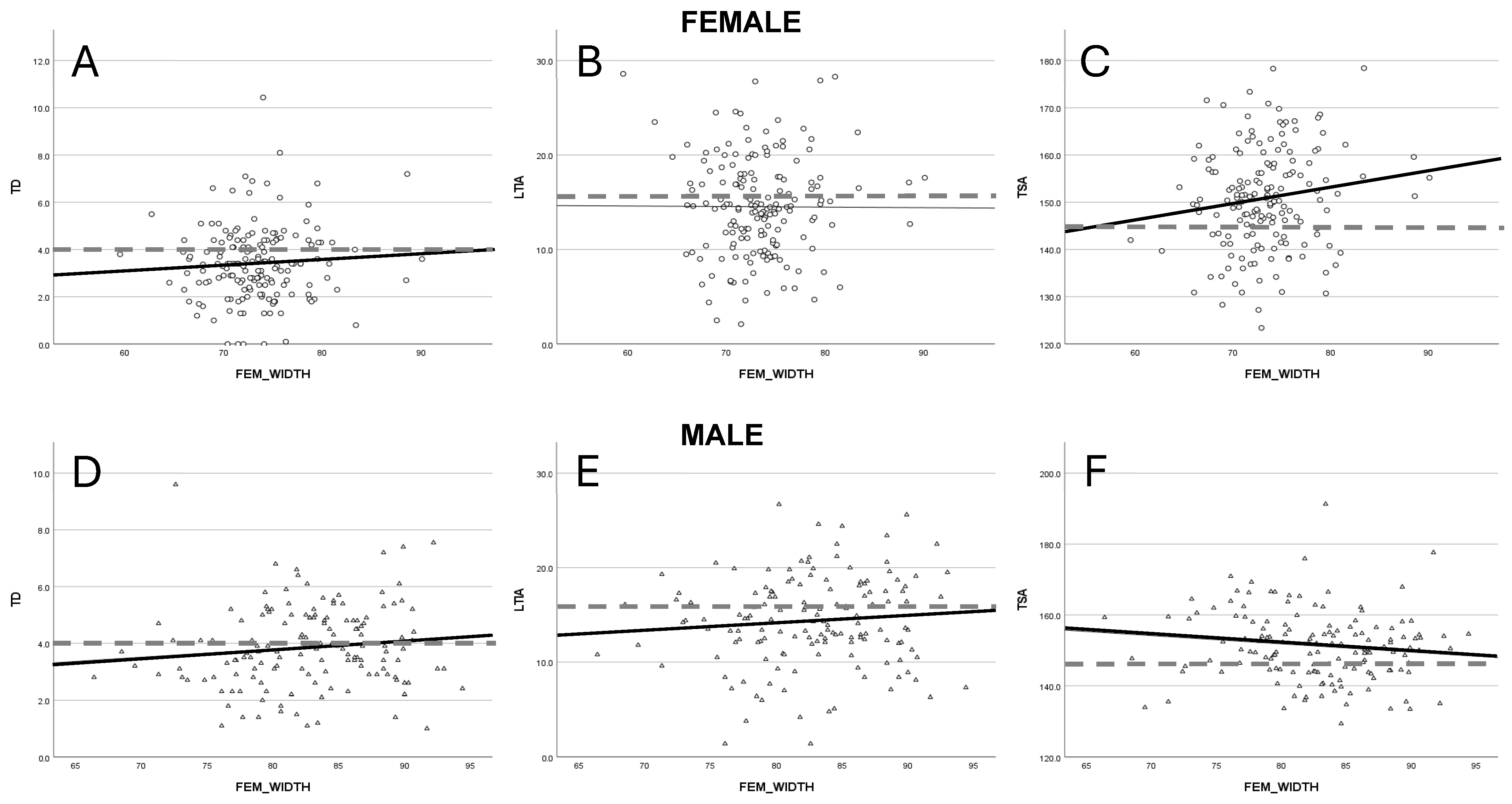
| Measurement | Female | Male | |
|---|---|---|---|
| Group size | 169 | 146 | |
| Age | 14.3 years | 14.7 years | |
| Femoral width | Mean all | 73.3 mm | 82.7 mm |
| Mean ≤ 11 | 71.9 mm | 79.5 mm | |
| Mean 12–14 | 72.9 mm | 81.6 mm | |
| Mean ≥ 15 | 73.9 mm | 83.7 mm |
| Measurement | Male (Mean ± SEM) | Female (Mean ± SEM) | p-Value |
|---|---|---|---|
| TD | 3.9 (±0.34) | 3.4 (±0.45) | <0.05 * |
| LTIA | 14.3 (±0.12) | 14.4 (±0.12) | 0.770 |
| TSA | 151.2 (±0.83) | 150.7 (±0.82) | 0.642 |
| LAUR | −0.6 (±0.73) | −0.8 (±0.81) | 0.818 |
| FULK | 2.4 (±0.77) | 2.1 (±0.77) | 0.757 |
| TILT | 20.1 (±0.71) | 22.1 (±0.76) | 0.064 |
| TTTG | 13.2 (±0.34) | 13.3 (±0.42) | 0.965 |
| TTPCL | 24.1 (±0.55) | 22.3 (±0.39) | <0.05 * |
| PTI | 44.5 (±1.57) | 50.1 (±1.49) | <0.05 * |
| CDI | 1.2 (±0.02) | 1.2 (±0.02) | 0.640 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schroedter, R.; Koutp, A.; Guggenberger, B.; Svehlik, M.; Tschauner, S.; Kraus, T. Anatomical Risk Patterns for Patellofemoral Instability in Skeletally Immature Patients: A Sex-Stratified MRI Study. J. Clin. Med. 2025, 14, 5519. https://doi.org/10.3390/jcm14155519
Schroedter R, Koutp A, Guggenberger B, Svehlik M, Tschauner S, Kraus T. Anatomical Risk Patterns for Patellofemoral Instability in Skeletally Immature Patients: A Sex-Stratified MRI Study. Journal of Clinical Medicine. 2025; 14(15):5519. https://doi.org/10.3390/jcm14155519
Chicago/Turabian StyleSchroedter, René, Amir Koutp, Bernhard Guggenberger, Martin Svehlik, Sebastian Tschauner, and Tanja Kraus. 2025. "Anatomical Risk Patterns for Patellofemoral Instability in Skeletally Immature Patients: A Sex-Stratified MRI Study" Journal of Clinical Medicine 14, no. 15: 5519. https://doi.org/10.3390/jcm14155519
APA StyleSchroedter, R., Koutp, A., Guggenberger, B., Svehlik, M., Tschauner, S., & Kraus, T. (2025). Anatomical Risk Patterns for Patellofemoral Instability in Skeletally Immature Patients: A Sex-Stratified MRI Study. Journal of Clinical Medicine, 14(15), 5519. https://doi.org/10.3390/jcm14155519






