Effects of AMCOP® Elastodontic Devices on Skeletal Divergence and Airway Dimensions in Growing Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample Selection
- Patients who had undergone lateral cephalometric X-rays both before and after treatment.
- Patients with mixed dentition.
- Prepubertal or pubertal stage in skeletal growth at initial observation.
- Previous orthodontic treatment.
- History of adenoidectomy or tonsillectomy.
- Craniofacial syndromes and abnormalities.
2.2. Treatment Protocol
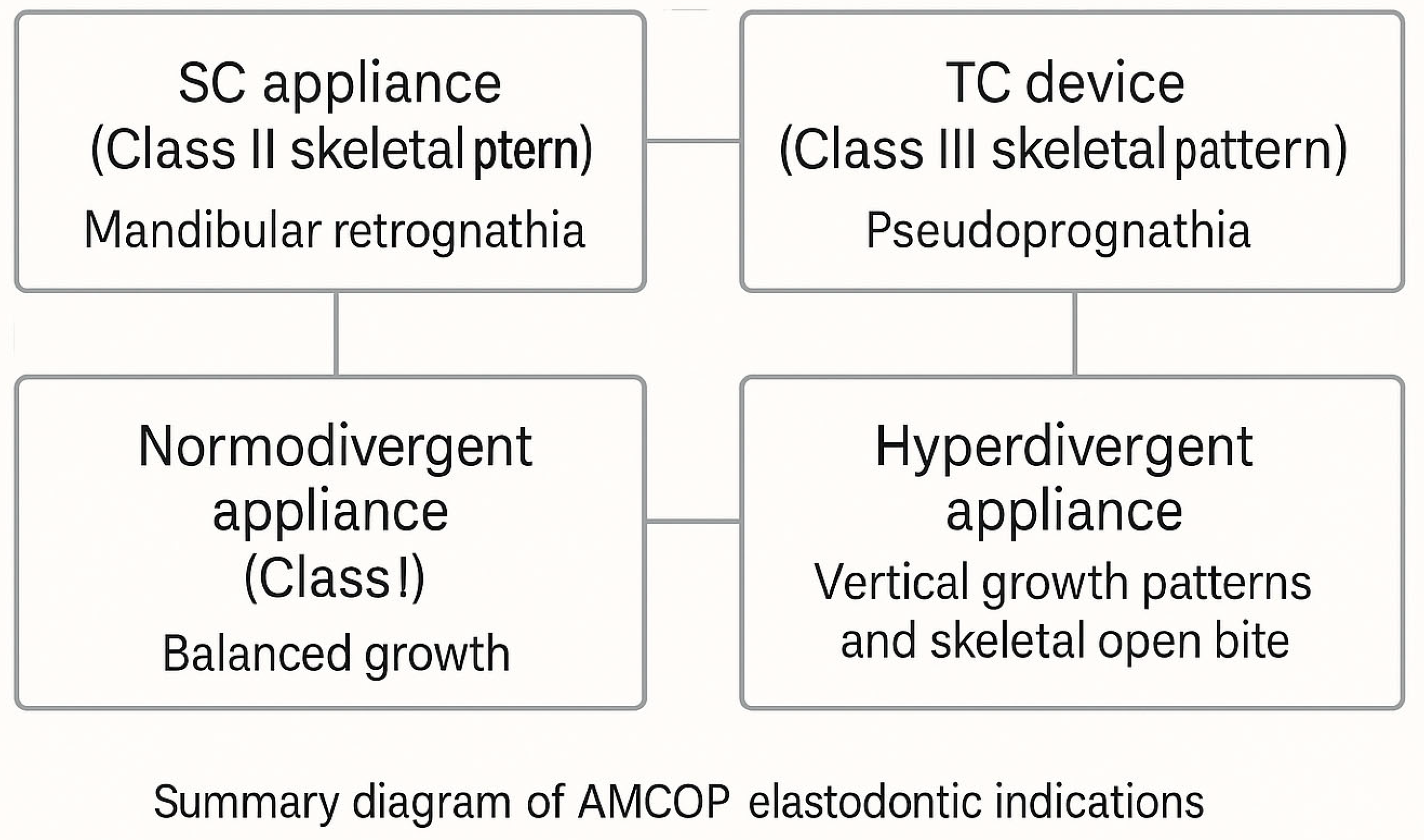
- First class devices.
- Second-class devices.
- Third-class devices.
- OPEN devices.
2.3. Cephalometric Analysis
2.4. Stastistical Analysis
2.5. Sample Size Justification
3. Results
3.1. Regression Analysis: Ans-Pns^Go-Gn Reduction
3.2. Regression Analysis: S-N^Go-Gn Reduction
3.3. Regression Analysis: FMA Reduction
3.4. Regression Analysis: OVB Increase
3.5. Regression Analysis: SPAS Increase
3.6. Regression Analysis: MAS Increase
3.7. Regression Analysis: IAS Increase
3.8. Summary of Multiple Linear Regression Models
4. Discussion
5. Conclusions
6. Patents
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AMCOP® | Armonizzatori Multifunzionali Cranio-Occluso-Posturali |
| ANB | Point A–Nasion–Point B Angle |
| CI | Confidence Interval |
| FMA | Frankfurt Mandibular Plane Angle |
| GN | Gnathion |
| GO | Gonion |
| IAS | Inferior Airway Space |
| MAS | Middle Airway Space |
| OVB | Overbite |
| OVJ | Overjet |
| SD | Standard Deviation |
| SN | Sella–Nasion |
| SNA | Sella–Nasion–Point A Angle |
| SNB | Sella–Nasion–Point B Angle |
| SPAS | Superior Posterior Airway Space |
| T0 | Initial Timepoint (Inizio del Trattamento) |
| T1 | Final Timepoint (Fine del Trattamento) |
References
- Altheer, C.; Papageorgiou, S.N.; Antonarakis, G.S.; Papadopoulou, A.K. Do Patients with Different Craniofacial Patterns Have Differences in Upper Airway Volume? A Systematic Review with Network Meta-Analysis. Eur. J. Orthod. 2024, 46, cjae010. [Google Scholar] [CrossRef]
- Shen, Y.; Li, X.; Feng, X.; Yu, L.; Weng, L.; Zhang, C.; Shang, Y.; Lin, J. Differences in the Effects of Orthodontic Treatment on Airway-Craniocervical Functional Environment in Adult and Adolescent Patients with Skeletal Class II High-Angle: A Retrospective Pilot Study. BMC Oral Health 2023, 23, 605. [Google Scholar] [CrossRef]
- Pirilä-Parkkinen, K.; Löppönen, H.; Nieminen, P.; Tolonen, U.; Pirttiniemi, P. Cephalometric Evaluation of Children with Nocturnal Sleep-Disordered Breathing. Eur. J. Orthod. 2010, 32, 662–671. [Google Scholar] [CrossRef]
- Pereira-Filho, V.A.; Castro-Silva, L.M.; de Moraes, M.; Gabrielli, M.F.R.; Campos, J.A.D.B.; Juergens, P. Cephalometric Evaluation of Pharyngeal Airway Space Changes in Class III Patients Undergoing Orthognathic Surgery. J. Oral Maxillofac. Surg. 2011, 69, e409–e415. [Google Scholar] [CrossRef]
- Inchingolo, F.; Inchingolo, A.D.; Riccaldo, L.; Costa, S.; Palermo, A.; Inchingolo, A.M.; Dipalma, G. Weight and Dental Eruption: The Correlation between BMI and Eruption. Eur. J. Paediatr. Dent. 2025, 1. [Google Scholar] [CrossRef]
- Rogers, K.; Campbell, P.M.; Tadlock, L.; Schneiderman, E.; Buschang, P.H. Treatment Changes of Hypo- and Hyperdivergent Class II Herbst Patients. Angle Orthod. 2017, 88, 3. [Google Scholar] [CrossRef]
- Graber, L.W.; Vanarsdall, R.L.; Vig, K.W.L.; Huang, G.J. (Eds.) Orthodontics: Current Principles and Techniques, 6th ed.; Elsevier: St. Louis, MO, USA, 2017; ISBN 978-0-323-37832-1. [Google Scholar]
- Cantore, S.; Ballini, A.; Farronato, D.; Malcangi, G.; Dipalma, G.; Assandri, F.; Garagiola, U.; Inchingolo, F.; De Vito, D.; Cirulli, N. Evaluation of an Oral Appliance in Patients with Mild to Moderate Obstructive Sleep Apnea Syndrome Intolerant to Continuous Positive Airway Pressure Use: Preliminary Results. Int. J. Immunopathol. Pharmacol. 2016, 29, 267–273. [Google Scholar] [CrossRef]
- Arunachalam, S.; Valiathan, A. Cephalometric Assessment of Dentofacial Vertical Changes in Class I Subjects Treated with and without Extraction. Am. J. Orthod. Dentofac. Orthop. 2008, 133, 869–875. [Google Scholar] [CrossRef]
- Singha Roy, A.; Tandon, P.; Chandna, A.; Sharma, V.; Nagar, A.; Singh, G. Jaw Morphology and Vertical Facial Types: A Cephalometric Appraisal. J. Orofac. Res. 2012, 2, 131–138. [Google Scholar] [CrossRef]
- Riolo, M.L. An Atlas of Craniofacial Growth: Cephalometric Standards from the University School Growth Study, the University of Michigan; University of Michigan: Ann Arbor, MI, USA, 1974; ISBN 978-0-929921-01-3. [Google Scholar]
- Campobasso, A.; Battista, G.; Fiorillo, G.; Caldara, G.; Lo Muzio, E.; Ciavarella, D.; Gastaldi, G.; Muzio, L.L. Transfer Accuracy of 3D-Printed Customized Devices in Digital Indirect Bonding: A Systematic Review and Meta-Analysis. Int. J. Dent. 2023, 2023, 5103991. [Google Scholar] [CrossRef]
- Ahmed, M.; Shaikh, A.; Fida, M. Diagnostic Performance of Various Cephalometric Parameters for the Assessment of Vertical Growth Pattern. Dent. Press J. Orthod. 2016, 21, 41. [Google Scholar] [CrossRef]
- Tweed, C. The Frankfort-Mandibular Incisor Angle (FMIA) in Orthodontic Diagnosis, Treatment Planning and Prognosis. Angle Orthod. 2009, 24, 121–169. [Google Scholar]
- Steiner, C.C. Cephalometrics for You and Me. Am. J. Orthod. 1953, 39, 729–755. [Google Scholar] [CrossRef]
- McNamara, J.A. A Method of Cephalometric Evaluation. Am. J. Orthod. 1984, 86, 449–469. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Ferrara, I.; Viapiano, F.; Netti, A.; Campanelli, M.; Buongiorno, S.; Latini, G.; Carpentiere, V.; Ciocia, A.M.; Ceci, S.; et al. Rapid Maxillary Expansion on the Adolescent Patient: Systematic Review and Case Report. Children 2022, 9, 1046. [Google Scholar] [CrossRef]
- Mangla, R.; Singh, N.; Dua, V.; Padmanabhan, P.; Khanna, M. Evaluation of Mandibular Morphology in Different Facial Types. Contemp. Clin. Dent. 2011, 2, 200. [Google Scholar] [CrossRef]
- McNamara, J.A. Components of Class II Malocclusion in Children 8–10 Years of Age. Angle Orthod. 1981, 51, 177–202. [Google Scholar] [CrossRef]
- Fani, E.; Coli, G.; Messina, A.; Sampalmieri, F.; Bambini, F.; Memè, L. Photobiomodulation and Orthodontic Treatment with Clear Aligners: A Case Report of Severe Crowding and Agenesis. Appl. Sci. 2023, 13, 9198. [Google Scholar] [CrossRef]
- Brezniak, N.; Arad, A.; Heller, M.; Dinbar, A.; Dinte, A.; Wasserstein, A. Pathognomonic Cephalometric Characteristics of Angle Class II Division 2 Malocclusion. Angle Orthod. 2002, 72, 251–257. [Google Scholar] [CrossRef]
- Björk, A. Prediction of Mandibular Growth Rotation. Am. J. Orthod. 1969, 55, 585–599. [Google Scholar] [CrossRef]
- Montenegro, V.; Inchingolo, A.D.; Malcangi, G.; Limongelli, L.; Marinelli, G.; Coloccia, G.; Laudadio, C.; Patano, A.; Inchingolo, F.; Bordea, I.R.; et al. Compliance of Children with Removable Functional Appliance with Microchip Integrated during Covid-19 Pandemic: A Systematic Review. J. Biol. Regul. Homeost. Agents 2021, 35, 365–377. [Google Scholar] [CrossRef]
- Memè, L.; Saccomanno, S.; Strappa, E.M.; Sampalmieri, F.; Bambini, F.; Gallusi, G. Oral Appliances for Severe Positional Obstructive Sleep Apnea Syndrome: A Case Report. Appl. Sci. 2022, 12, 10570. [Google Scholar] [CrossRef]
- Buschang, P.; Jacob, H.; Carrillo, R. The Morphological Characteristics, Growth, and Etiology of the Hyperdivergent Phenotype. Semin. Orthod. 2013, 19, 212–226. [Google Scholar] [CrossRef]
- Schudy, F.F. The rotation of the mandible resulting from growth: Its implications in orthodontic treatment. Angle Orthod. 1965, 35, 36–50. [Google Scholar] [CrossRef]
- Laudadio, C.; Inchingolo, A.D.; Malcangi, G.; Limongelli, L.; Marinelli, G.; Coloccia, G.; Montenegro, V.; Patano, A.; Inchingolo, F.; Bordea, I.R.; et al. Management of Anterior Open-Bite in the Deciduous, Mixed and Permanent Dentition Stage: A Descriptive Review. J. Biol. Regul. Homeost. Agents 2021, 35, 271–281. [Google Scholar] [CrossRef]
- Ciuffolo, F.; Ciavarella, D.; Tepedino, M. Extraction Protocol in Class II Malocclusion with a Straight Profile: Description of Simplified Mechanics in Two Growing Patients. AJO—Clin. Companion 2023, 3, 397–406. [Google Scholar] [CrossRef]
- Kim, J.; Lee, S.; Kim, T.W.; Nahm, D.; Chang, Y. Classification of the Skeletal Variation in Normal Occlusion. Angle Orthod. 2005, 75, 311–319. [Google Scholar]
- Field, H.; Larson, B.; Sarver, D.M.; Proffit, W.R. Contemporary Orthodontics; Elsevier: St. Louis, MO, USA, 2018; ISBN 978-0-323-54387-3. [Google Scholar]
- d’Apuzzo, F.; Nucci, L.; Strangio, B.M.; Inchingolo, A.D.; Dipalma, G.; Minervini, G.; Perillo, L.; Grassia, V. Dento-Skeletal Class III Treatment with Mixed Anchored Palatal Expander: A Systematic Review. Appl. Sci. 2022, 12, 4646. [Google Scholar] [CrossRef]
- Polizzi, A.; Ronsivalle, V.; Lo Giudice, A.; Isola, G.; Bianchi, A.; Santonocito, S.; Leonardi, R.; Mummolo, S. Orthodontic Approaches in the Management of Mandibular Fractures: A Scoping Review. Children 2023, 10, 605. [Google Scholar] [CrossRef]
- Alabdullah, M.; Saltaji, H.; Abou-Hamed, H.; Youssef, M. Association between Facial Growth Pattern and Facial Muscle Activity: A Prospective Cross-Sectional Study. Int. Orthod. 2015, 13, 181–194. [Google Scholar] [CrossRef]
- Moss, M.L. The Functional Matrix Hypothesis Revisited. 1. The Role of Mechanotransduction. Am. J. Orthod. Dentofac. Orthop. 1997, 112, 8–11. [Google Scholar] [CrossRef]
- Pasini, M.; Giuca, M.R.; Ligori, S.; Mummolo, S.; Fiasca, F.; Marzo, G.; Quinzi, V. Association between Anatomical Variations and Maxillary Canine Impaction: A Retrospective Study in Orthodontics. Appl. Sci. 2020, 10, 5638. [Google Scholar] [CrossRef]
- Sonego, C.; Bobrowski, Â.; Chagas Junior, O.; Torriani, M.A. Aesthetic and Functional Implications Following Rotation of the Maxillomandibular Complex in Orthognathic Surgery: A Systematic Review. Int. J. Oral Maxillofac. Surg. 2013, 43, 40–45. [Google Scholar] [CrossRef]
- Tepedino, M.; Iancu-Potrubacz, M.; Ciavarella, D.; Masedu, F.; Marchione, L.; Chimenti, C. Expansion of Permanent First Molars with Rapid Maxillary Expansion Appliance Anchored on Primary Second Molars. J. Clin. Exp. Dent. 2018, 10, e241–e247. [Google Scholar] [CrossRef]
- Cozza, P.; Baccetti, T.; Franchi, L.; Mucedero, M.; Polimeni, A. Sucking Habits and Facial Hyperdivergency as Risk Factors for Anterior Open Bite in the Mixed Dentition. Am. J. Orthod. Dentofac. Orthop. 2005, 128, 517–519. [Google Scholar] [CrossRef]
- Solow, B.; Kreiborg, S. Soft-Tissue Stretching: A Possible Control Factor in Craniofacial Morphogenesis. Scand. J. Dent. Res. 1977, 85, 505–507. [Google Scholar] [CrossRef]
- Sabatucci, A.; Raffaeli, F.; Mastrovincenzo, M.; Luchetta, A.; Giannone, A.; Ciavarella, D. Breathing Pattern and Head Posture: Changes in Craniocervical Angles. Minerva Stomatol. 2015, 64, 59–74. [Google Scholar]
- Quinzi, V.; Caruso, S.; Mummolo, S.; Nota, A.; Angelone, A.M.; Mattei, A.; Gatto, R.; Marzo, G. Evaluation of Lower Dental Arch Crowding and Dimension after Treatment with Lip Bumper versus Schwarz Appliance. A Prospective Pilot Study. Dent. J. 2020, 8, 34. [Google Scholar] [CrossRef]
- Hsu, J.-Y.; Cheng, J.H.-C.; Feng, S.-W.; Lai, P.-C.; Yoshida, N.; Chiang, P.-C. Strategic Treatment Planning for Anterior Open Bite: A Comprehensive Approach. J. Dent. Sci. 2024, 19, 1328. [Google Scholar] [CrossRef]
- Ciavarella, D.; Monsurrò, A.; Padricelli, G.; Battista, G.; Laino, L.; Perillo, L. Unilateral Posterior Crossbite in Adolescents: Surface Electromyographic Evaluation. Eur. J. Paediatr. Dent. 2012, 13, 25–28. [Google Scholar]
- Tecco, S.; Baldini, A.; Mummolo, S.; Marchetti, E.; Giuca, M.R.; Marzo, G.; Gherlone, E.F. Frenulectomy of the Tongue and the Influence of Rehabilitation Exercises on the sEMG Activity of Masticatory Muscles. J. Electromyogr. Kinesiol. Off. J. Int. Soc. Electrophysiol. Kinesiol. 2015, 25, 619–628. [Google Scholar] [CrossRef]
- Dinoi, M.T.; Marchetti, E.; Garagiola, U.; Caruso, S.; Mummolo, S.; Marzo, G. Orthodontic Treatment of an Unerupted Mandibular Canine Tooth in a Patient with Mixed Dentition: A Case Report. J. Med. Case Rep. 2016, 10, 170. [Google Scholar] [CrossRef]
- Ureni, R.; Verdecchia, A.; Suárez-Fernández, C.; Mereu, M.; Schirru, R.; Spinas, E. Effectiveness of Elastodontic Devices for Correcting Sagittal Malocclusions in Mixed Dentition Patients: A Scoping Review. Dent. J. 2024, 12, 247. [Google Scholar] [CrossRef]
- Cardarelli, F.; Drago, S.; Rizzi, L.; Bazzani, M.; Pesce, P.; Menini, M.; Migliorati, M. Effects of Removable Functional Appliances on the Dentoalveolar Unit in Growing Patients. Medicina 2024, 60, 746. [Google Scholar] [CrossRef]
- Lanteri, V.; Abate, A.; Maspero, C.; Farronato, G.; Tessore, E.; Cagetti, M.G. Customized elastodontic therapy during childhood: A pilot study. Dent. Cadmos 2022, 90, 200–210. [Google Scholar] [CrossRef]
- Scandurra, C.; Gasparro, R.; Dolce, P.; Bochicchio, V.; Muzii, B.; Sammartino, G.; Marenzi, G.; Maldonato, N.M. The Role of Cognitive and Non-Cognitive Factors in Dental Anxiety: A Mediation Model. Eur. J. Oral Sci. 2021, 129, e12793. [Google Scholar] [CrossRef]
- Mummolo, S.; Marchetti, E.; Albani, F.; Campanella, V.; Pugliese, F.; Di Martino, S.; Tecco, S.; Marzo, G. Comparison between Rapid and Slow Palatal Expansion: Evaluation of Selected Periodontal Indices. Head Face Med. 2014, 10, 30. [Google Scholar] [CrossRef]
- Fichera, G.; Martina, S.; Palazzo, G.; Musumeci, R.; Leonardi, R.; Isola, G.; Lo Giudice, A. New Materials for Orthodontic Interceptive Treatment in Primary to Late Mixed Dentition. A Retrospective Study Using Elastodontic Devices. Materials 2021, 14, 1695. [Google Scholar] [CrossRef]
- Ronsivalle, V.; Nucci, L.; Bua, N.; Palazzo, G.; Rosa, S.L. Elastodontic Appliances for the Interception of Malocclusion in Children: A Systematic Narrative Hybrid Review. Children 2023, 10, 1821. [Google Scholar] [CrossRef]
- Mohammed, H.; Čirgić, E.; Rizk, M.Z.; Vandevska-Radunovic, V. Effectiveness of Prefabricated Myofunctional Appliances in the Treatment of Class II Division 1 Malocclusion: A Systematic Review. Eur. J. Orthod. 2020, 42, 125–134. [Google Scholar] [CrossRef]
- Patano, A.; Cardarelli, F.; Montenegro, V.; Ceci, S.; Inchingolo, A.D.; Semjonova, A.; Palmieri, G.; Pede, C.D.; Mancini, A.; Maggiore, M.E.; et al. Early Functional Orthodontic Treatment of Bad Oral Habits with AMCOP® Bio-Activators. J. Biol. Regul. Homeost. Agents 2022, 36, 91–110. [Google Scholar] [CrossRef]
- Patano, A.; Inchingolo, A.M.; Cardarelli, F.; Inchingolo, A.D.; Viapiano, F.; Giotta, M.; Bartolomeo, N.; Di Venere, D.; Malcangi, G.; Minetti, E.; et al. Effects of Elastodontic Appliance on the Pharyngeal Airway Space in Class II Malocclusion. J. Clin. Med. 2023, 12, 4280. [Google Scholar] [CrossRef]
- Schievano, D.; Rontani, R.M.; Bérzin, F. Influence of Myofunctional Therapy on the Perioral Muscles. Clinical and Electromyographic Evaluations. J. Oral Rehabil. 1999, 26, 564–569. [Google Scholar] [CrossRef]
- Ming, Y.; Hu, Y.; Li, Y.; Yu, J.; He, H.; Zheng, L. Effects of Maxillary Protraction Appliances on Airway Dimensions in Growing Class III Maxillary Retrognathic Patients: A Systematic Review and Meta-Analysis. Int. J. Pediatr. Otorhinolaryngol. 2018, 105, 138–145. [Google Scholar] [CrossRef]
- Jiang, W.; Xia, S.; Yue, H.; Li, X.-Z. Upper airway changes in patients with skeletal class Ⅲ maxillary retrognathia after rapid maxillary expansion and protraction: A meta-analysis. Shanghai Kou Qiang Yi Xue Shanghai J. Stomatol. 2019, 28, 218–224. [Google Scholar]
- Cannatà, D.; Galdi, M.; Martina, S.; Rongo, R.; D’Antò, V.; Valletta, R.; Bucci, R. Preformed Elastodontic Appliances: Awareness and Attitude of Orthodontists and General Dental Practitioners. Children 2024, 11, 418. [Google Scholar] [CrossRef]
- Cui, Y.; Huang, T.; Yu, Z.; Zhou, S.; Zhang, L.; Han, Y.; Li, S.; Wang, Q.; Tian, Y. Mechanical Characterization and Structural Analysis of Elastodontic Appliances under Intraoral and Artificial Aging Conditions. BMC Oral Health 2024, 24, 1337. [Google Scholar] [CrossRef]
- Ronsivalle, V.; Quinzi, V.; La Rosa, S.; Leonardi, R.; Lo Giudice, A. Comparative Analysis of Skeletal Changes, Occlusal Changes, and Palatal Morphology in Children with Mild Class III Malocclusion Treated with Elastodontic Appliances and Bimaxillary Plates. Children 2023, 10, 1219. [Google Scholar] [CrossRef]
- Zelderloo, A.; Cadenas de Llano-Pérula, M.; Verdonck, A.; Fieuws, S.; Willems, G. Cephalometric Appraisal of Class II Treatment Effects after Functional and Fixed Appliances: A Retrospective Study. Eur. J. Orthod. 2017, 39, 334–341. [Google Scholar] [CrossRef]
- Bhattacharya, A.; Bhatia, A.; Patel, D.; Mehta, N.; Parekh, H.; Trivedi, R. Evaluation of Relationship between Cranial Base Angle and Maxillofacial Morphology in Indian Population: A Cephalometric Study. J. Orthod. Sci. 2014, 3, 74. [Google Scholar] [CrossRef]
- D’Antò, V.; Madariaga, A.C.P.; Rongo, R.; Bucci, R.; Simeon, V.; Franchi, L.; Valletta, R. Distribution of the Condylion-Gonion-Menton (CoGoMe^) Angle in a Population of Patients from Southern Italy. Dent. J. 2019, 7, 104. [Google Scholar] [CrossRef]
- Minervini, G.; Franco, R.; Marrapodi, M.M.; Fiorillo, L.; Cervino, G.; Cicciù, M. Prevalence of Temporomandibular Disorders (TMD) in Pregnancy: A Systematic Review with Meta-Analysis. J. Oral Rehabil. 2023, 50, 627–634. [Google Scholar] [CrossRef]
- Koretsi, V.; Zymperdikas, V.F.; Papageorgiou, S.N.; Papadopoulos, M.A. Treatment Effects of Removable Functional Appliances in Patients with Class II Malocclusion: A Systematic Review and Meta-Analysis. Eur. J. Orthod. 2015, 37, 418–434. [Google Scholar] [CrossRef]
- Ichim, I.; Kieser, J.A.; Swain, M.V. Functional Significance of Strain Distribution in the Human Mandible under Masticatory Load: Numerical Predictions. Arch. Oral Biol. 2007, 52, 465–473. [Google Scholar] [CrossRef]
- Sella-Tunis, T.; Pokhojaev, A.; Sarig, R.; O’Higgins, P.; May, H. Human Mandibular Shape is Associated with Masticatory Muscle Force. Sci. Rep. 2018, 8, 6042. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Inchingolo, A.M.; Piras, F.; Malcangi, G.; Patano, A.; Di Pede, C.; Netti, A.; Ciocia, A.M.; Corriero, A.; Semjonova, A.; et al. A Systematic Review of Positional Plagiocephaly Prevention Methods for Patients in Development. Appl. Sci. 2022, 12, 11172. [Google Scholar] [CrossRef]
- Madurantakam, P. Removable Functional Appliances Effective in Patients with Class II Malocclusions. Evid. Based Dent. 2016, 17, 27–28. [Google Scholar] [CrossRef]
- Ocak, I.; Karsli, N.; Altug, A.T.; Aksu, M. Relationship between Vertical Facial Morphology and Dental Arch Measurements in Class II Malocclusion: A Retrospective Study. PeerJ 2023, 11, e16031. [Google Scholar] [CrossRef]
- Roy, P.; Roy, P.; Koley, S. Comparative Assessment of Various Cephalometric Parameters Used for Determining Vertical Skeletal Dysplasia. Cureus 2024, 16, e55101. [Google Scholar] [CrossRef]
- Lee, Y.-S.; Lee, J.-Y. Orthodontic Diagnosis Rates Based on Panoramic Radiographs in Children Aged 6–8 Years: A Retrospective Study. Korean J. Orthod. 2024, 54, 185–195. [Google Scholar] [CrossRef]
- Asaumi, J.-I.; Hisatomi, M.; Yanagi, Y.; Unetsubo, T.; Maki, Y.; Matsuzaki, H.; Honda, Y.; Konouchi, H. Evaluation of Panoramic Radiographs Taken at the Initial Visit at a Department of Paediatric Dentistry. Dento Maxillo Facial Radiol. 2008, 37, 340–343. [Google Scholar] [CrossRef]
- Mollabashi, V.; Heidari, A.; Ebrahimi Zadeh, H.; Seyed Tabib, M. The Study of Facial Morphology in Patients with Vertical Growth Pattern (Hyperdivergent) Lacking or Showing Temporomandibular Disorders Symptoms. J. Stomatol. Oral Maxillofac. Surg. 2020, 121, 233–237. [Google Scholar] [CrossRef]
- Minervini, G.; Franco, R.; Marrapodi, M.M.; Fiorillo, L.; Cervino, G.; Cicciù, M. The Association between Parent Education Level, Oral Health, and Oral-Related Sleep Disturbance. An Observational Crosssectional Study. Eur. J. Paediatr. Dent. 2023, 24, 218–223. [Google Scholar] [CrossRef]
- Marra, P.M.; Fiorillo, L.; Cervino, G.; Cardarelli, F.; Cicciù, M.; Laino, L. Elastodontic Treatment with Oral Bio-Activators in Young Children. Minerva Dent. Oral Sci. 2022, 71, 270–276. [Google Scholar] [CrossRef]
- Ierardo, G.; Luzzi, V.; Nardacci, G.; Vozza, I.; Polimeni, A. Minimally Invasive Orthodontics: Elastodontic Therapy in a Growing Patient Affected by Dentinogenesis Imperfecta. Ann. Stomatol. 2017, 8, 34–38. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Patano, A.; Coloccia, G.; Ceci, S.; Inchingolo, A.M.; Marinelli, G.; Malcangi, G.; Montenegro, V.; Laudadio, C.; Pede, C.D.; et al. The Efficacy of a New AMCOP® Elastodontic Protocol for Orthodontic Interceptive Treatment: A Case Series and Literature Overview. Int. J. Environ. Res. Public Health 2022, 19, 988. [Google Scholar] [CrossRef]
- Ortu, E.; Di Nicolantonio, S.; Severino, M.; Cova, S.; Pietropaoli, D.; Monaco, A. Effectiveness of Elastodontic Appliances in the Treatment of Malocclusions: A Review of the Literature. Eur. J. Paediatr. Dent. 2024, 25, 57–60. [Google Scholar] [CrossRef]
- Lo Giudice, A.; Ronsivalle, V.; Santonocito, S.; Lucchese, A.; Venezia, P.; Marzo, G.; Leonardi, R.; Quinzi, V. Digital Analysis of the Occlusal Changes and Palatal Morphology Using Elastodontic Devices. A Prospective Clinical Study Including Class II Subjects in Mixed Dentition. Eur. J. Paediatr. Dent. 2022, 23, 275–280. [Google Scholar] [CrossRef]
- Chen, Y.; Hagg, U.; McGrath, C. Elastodontic Appliance Assisted Fixed Appliance Treatment: A New Two-Phase Protocol for Extraction Cases. J. Orthod. 2019, 46, 251–258. [Google Scholar] [CrossRef]
- do Vale, F.; Rodrigues, M.L.; Francisco, I.; Roseiro, A.; Santos, I.; Caramelo, F.; Rodrigues, M.J. Short-Term Pharyngeal Airway Space Changes after Mandibular Advancement Surgery in Class II Patients-a Two-Dimensional Retrospective Study. Orthod. Craniofac. Res. 2019, 22, 81–86. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Dipalma, G.; Ferrara, I.; Viapiano, F.; Netti, A.; Ciocia, A.M.; Mancini, A.; Malcangi, G.; Palermo, A.; Inchingolo, A.M.; et al. Clear Aligners in the Growing Patient: A Systematic Review. Children 2024, 11, 385. [Google Scholar] [CrossRef]
- Cozzani, M.; Mazzotta, L.; Cozzani, P. Early Interceptive Treatment in the Primary Dentition—A Case Report. J. Orthod. 2013, 40, 345–351; quiz 353. [Google Scholar] [CrossRef]
- Ortu, E.; Barrucci, G.; Aprile, G.; Guerrini, L.; Pietropaoli, D.; Monaco, A. Electromyographic Evaluation during Orthodontic Therapy: Comparison of Two Elastodontic Devices. J. Biol. Regul. Homeost. Agents 2020, 34, 1935–1939. [Google Scholar] [CrossRef]
- Lotfi, V.; Ghoneima, A.; Lagravere, M.; Kula, K.; Stewart, K. Three-Dimensional Evaluation of Airway Volume Changes in Two Expansion Activation Protocols. Int. Orthod. 2018, 16, 144–157. [Google Scholar] [CrossRef]
- Chauhan, A.; Autar, R.; Pradhan, K.L.; Yadav, V. Comparison of Pharyngeal Airway Dimension, Tongue and Hyoid Bone Position Based on ANB Angle. Natl. J. Maxillofac. Surg. 2015, 6, 42–51. [Google Scholar] [CrossRef]
- Madian, A.M.; Elfouly, D. Cephalometric Changes in Pharyngeal Airway Dimensions after Functional Treatment with Twin Block versus Myobrace Appliances in Developing Skeletal Class II Patients: A Randomized Clinical Trial. BMC Oral Health 2023, 23, 998. [Google Scholar] [CrossRef]
- Elfouly, D.; Dumu, E.J.; Madian, A.M.; Eid, F.Y. The Effect of Different Functional Appliances on the Sagittal Pharyngeal Airway Dimension in Skeletal Class II: A Retrospective Study. Sci. Rep. 2024, 14, 19410. [Google Scholar] [CrossRef]
- Pradhan, R.; Rajbhandari, A.; Bajracharya, M.; Manandhar, P.; Maharjan, S.; Pant, B.D. Study of Upper Pharyngeal Airway Dimension in Young Adults Visiting Orthodontic Department of a Dental College: A Descriptive Cross-Sectional Study. JNMA J. Nepal Med. Assoc. 2021, 59, 271–275. [Google Scholar] [CrossRef]
- de Oliveira, I.; Pinheiro, R.; Freitas, B.; Reher, P.; Rodrigues, V. Relationship between Craniofacial and Dental Arch Morphology with Pharyngeal Airway Space in Adolescents. J. Orofac. Orthop. 2023, 84, 93–103. [Google Scholar] [CrossRef]
- Mislik, B.; Hänggi, M.P.; Signorelli, L.; Peltomäki, T.A.; Patcas, R. Pharyngeal Airway Dimensions: A Cephalometric, Growth-Study-Based Analysis of Physiological Variations in Children Aged 6–17. Eur. J. Orthod. 2014, 36, 331–339. [Google Scholar] [CrossRef]
- Trenouth, M.J. Cervical Spine Posture and Twin-Block Treatment. Am. J. Orthod. Dentofac. Orthop. 2019, 156, 439. [Google Scholar] [CrossRef]
- Arn, M.-L.; Dritsas, K.; Pandis, N.; Kloukos, D. The Effects of Fixed Orthodontic Retainers on Periodontal Health: A Systematic Review. Am. J. Orthod. Dentofac. Orthop. 2020, 157, 156–164.E17. [Google Scholar] [CrossRef]
- Yıldırım, E.; Karaçay, Ş. Volumetric Evaluation of Pharyngeal Airway after Functional Therapy. Scanning 2021, 2021, 6694992. [Google Scholar] [CrossRef]
- Mehra, P.; Downie, M.; Pita, M.C.; Wolford, L.M. Pharyngeal Airway Space Changes after Counterclockwise Rotation of the Maxillomandibular Complex. Am. J. Orthod. Dentofac. Orthop. 2001, 120, 154–159. [Google Scholar] [CrossRef]
- Okushi, T.; Tonogi, M.; Arisaka, T.; Kobayashi, S.; Tsukamoto, Y.; Morishita, H.; Sato, K.; Sano, C.; Chiba, S.; Yamane, G.-Y.; et al. Effect of Maxillomandibular Advancement on Morphology of Velopharyngeal Space. J. Oral Maxillofac. Surg. 2011, 69, 877–884. [Google Scholar] [CrossRef]
- Zhang, C.; Lu, T.; Wang, L.; Wen, J.; Huang, Z.; Lin, S.; Zhou, Y.; Li, G.; Li, H. Three-Dimensional Analysis of Hard and Soft Tissue Changes in Skeletal Class II Patients with High Mandibular Plane Angle Undergoing Surgery. Sci. Rep. 2024, 14, 2519. [Google Scholar] [CrossRef]





| Parameters | Definitions | Mean Values (SD) |
|---|---|---|
| SNA | Angle between sella–nasion and nasion–point A segments. | 82° (±2°) |
| SNB | Angle between sella–nasion and nasion–point B segments. | 80° (±2°) |
| ANB | Angle between point A–nasion and nasion–point B segments. | 2° (±2°) |
| Ans-Pns^Go-Gn | Intermaxillary angle, between bispinal plane (Ans-Pns) and mandibular plane (Go-Gn). | 28° (±2°) |
| SN^Go-Gn | Mandibular angle between sella–nasion plane (S-N) and mandibular plane. | 32° (±5°) |
| FMA | Angle between Frankfurt plane and mandibular plane. | 25° (±3°) |
| OVJ (mm) | Overjet, distance on the sagittal plane between the upper and lower incisors. | 2.5 (±2.5 mm) |
| OVB (mm) | Overbite, distance on the vertical plane between the upper and lower incisors. | 2.5 (±2.5 mm) |
| SPAS | Superior posterior airway space, the distance along a line parallel to the gonion–menton plane (Go–Me) between the soft palate and the posterior wall of the nasopharynx. | n.d. |
| MAS | Middle airway space, the distance measured along a line parallel to the Go-Me plane between the posterior wall of the oropharynx and the lower tip of the soft palate. | n.d. |
| IAS | Inferior airway space, the distance between the posterior wall of the pharynx and the base of the tongue along the Go-Me plane. | n.d. |
| Qualitative Variables | N. | Percentage | |
| Sex | Male | 29 | 48.33% |
| Female | 31 | 51.67% | |
| Quantitative Variables | CASE | CONTROL | ||||||
|---|---|---|---|---|---|---|---|---|
| T0 | T1 | T0 | T1 | |||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Age (years) | 8.67 | ±1.30 | 15.93 | ±0.83 | 9.17 | ±0.79 | 15.70 | ±0.99 |
| SNA | 83.30 | ±2.84 | 82.15 | ±2.47 | 81.15 | ±3.13 | 81.50 | ±2.99 |
| SNB | 77.13 | ±2.62 | 78.67 | ±2.11 | 81.50 | ±2.99 | 75.26 | ±3.01 |
| ANB | 5.95 | ±1.82 | 3.57 | ±1.18 | 5.94 | ±1.87 | 5.25 | ±2.59 |
| Ans-Pns^Go-Gn | 22.95 | ±4.36 | 21.50 | ±3.54 | 24.80 | ±4.37 | 24.90 | ±4.29 |
| SN^Go-Gn | 31.95 | ±4.06 | 30.20 | ±3.56 | 33.55 | ±4.26 | 33.85 | ±4.39 |
| FMA | 24.75 | ±4.22 | 22.75 | ±3.48 | 24.15 | ±4.54 | 24.40 | ±3.75 |
| OVJ (mm) | 4.95 | ±1.56 | 3.20 | ±0.99 | 5.65 | ±2.13 | 5.60 | ±2.24 |
| OVB (mm) | 1.90 | ±2.38 | 2.65 | ±0.98 | 1.90 | ±1.90 | 3.25 | ±1.49 |
| SPAS | 8.65 | ±2.78 | 12.25 | ±2.80 | 10.60 | ±2.45 | 10.70 | ±2.58 |
| MAS | 9.30 | ±2.59 | 9.45 | ±2.57 | 10.95 | ±2.45 | 10.45 | ±2.03 |
| IAS | 10.85 | ±2.72 | 12.40 | ±2.52 | 11.00 | ±1.82 | 10.35 | ±2.24 |
| Predictor | Unstd. B | Std. β | SE | 95%CI for B | p-Value |
|---|---|---|---|---|---|
| Group (Treated = 1) | −2.12 | −0.38 | 0.69 | [−3.50, −0.74] | 0.003 |
| Sex (Male = 1) | 0.14 | 0.03 | 0.59 | [−1.04, 1.33] | 0.791 |
| Age at T0 | −0.06 | −0.02 | 0.35 | [−0.76, 0.64] | 0.869 |
| FMA at T0 | 0.38 | 0.67 | 0.08 | [0.22, 0.54] | <0.001 |
| Predictor | Unstd. B | Std. β | SE | 95%CI for B | p-Value |
|---|---|---|---|---|---|
| Group (Treated = 1) | 1.92 | 0.34 | 0.63 | [0.62, 3.22] | 0.004 |
| Sex (Male = 1) | −0.11 | −0.02 | 0.56 | [−1.24, 1.02] | 0.848 |
| Age at T0 | 0.03 | 0.01 | 0.31 | [−0.59, 0.65] | 0.919 |
| SPAS at T0 | −0.43 | −0.55 | 0.11 | [−0.66, −0.20] | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dipalma, G.; Inchingolo, A.D.; Cardarelli, F.; Di Lorenzo, A.; Viapiano, F.; Ferrante, L.; Inchingolo, F.; Venere, D.D.; Palermo, A.; Marinelli, G.; et al. Effects of AMCOP® Elastodontic Devices on Skeletal Divergence and Airway Dimensions in Growing Patients. J. Clin. Med. 2025, 14, 5297. https://doi.org/10.3390/jcm14155297
Dipalma G, Inchingolo AD, Cardarelli F, Di Lorenzo A, Viapiano F, Ferrante L, Inchingolo F, Venere DD, Palermo A, Marinelli G, et al. Effects of AMCOP® Elastodontic Devices on Skeletal Divergence and Airway Dimensions in Growing Patients. Journal of Clinical Medicine. 2025; 14(15):5297. https://doi.org/10.3390/jcm14155297
Chicago/Turabian StyleDipalma, Gianna, Alessio Danilo Inchingolo, Filippo Cardarelli, Antonio Di Lorenzo, Fabio Viapiano, Laura Ferrante, Francesco Inchingolo, Daniela Di Venere, Andrea Palermo, Grazia Marinelli, and et al. 2025. "Effects of AMCOP® Elastodontic Devices on Skeletal Divergence and Airway Dimensions in Growing Patients" Journal of Clinical Medicine 14, no. 15: 5297. https://doi.org/10.3390/jcm14155297
APA StyleDipalma, G., Inchingolo, A. D., Cardarelli, F., Di Lorenzo, A., Viapiano, F., Ferrante, L., Inchingolo, F., Venere, D. D., Palermo, A., Marinelli, G., & Inchingolo, A. M. (2025). Effects of AMCOP® Elastodontic Devices on Skeletal Divergence and Airway Dimensions in Growing Patients. Journal of Clinical Medicine, 14(15), 5297. https://doi.org/10.3390/jcm14155297











