Evaluation of the Possible Correlation Between Dental Occlusion and Craniomandibular Disorders by Means of Teethan® Electromyography: Clinical-Observational Study on 20 Patients
Abstract
1. Introduction
- Traumas (macro traumas such as a car accident, a fight or a fall; microtraumas such as titillophagia and onychophagia);
- Occlusal factors (second/third classes, unilateral crossbite, open bite);
- Hormonal factors (possible role of estrogens in the excessive laxity of the ligaments);
- Psychological causes (increased emotional tension and excess stress);
- Wakeful or sleeping bruxism;
- Genetic background (XX) [18].
- -
- It allows analysis of the shape, amplitude, duration and frequency of action potentials of individual motor units, providing detailed information on the integrity of the peripheral nerve and muscle.
- -
- It can detect abnormal electrical activity at rest (such as fibrillations or positive waves), which is indicative of muscle denervation (nerve damage).
- -
- It evaluates how motor units are activated during voluntary contraction, which is useful for distinguishing between neurogenic (nerve damage) and myogenic (muscle damage) disorders.
- -
- It is essential for distinguishing between a wide range of neuromuscular disorders, including peripheral nerve damage (carpal tunnel syndrome, diabetic neuropathies, radiculopathies from herniated discs, traumatic nerve injuries); myopathies (muscular dystrophies, myositis); diseases that alter nerve-to-muscle signal transmission (myasthenia gravis); diseases that affect motor neurons in the brain and spinal cord (amyotrophic lateral sclerosis).
- -
- Invasiveness and Patient Discomfort
- -
- Pain/Discomfort: Inserting the needle into the muscle can be painful or uncomfortable for the patient. Although the needles are thin and disposable, pain tolerance varies from person to person.
- -
- Anxiety: Many patients experience anxiety at the thought of needle insertion, which can make the examination more difficult.
- -
- Bruising/Bleeding: Minor bruising or slight bleeding may occur at the puncture sites, especially in patients with coagulation disorders or who are on anticoagulant therapy.
- -
- Risk of Complications (Rare): Infections, although rare with sterile, disposable needles, there is a minimal risk of infection at the puncture site: pneumothorax—extremely rare, but theoretically possible when examining deep chest muscles with pleural penetration; nerve/muscle injuries—although the risk is low when performed by experienced personnel, there is a minimal risk of direct injury to nerves or blood vessels.
- -
- Relative Contraindications: anticoagulant/antiplatelet therapy—requires caution and a risk/benefit assessment; pacemakers/defibrillators—although there are no absolute contraindications, caution and communication with the attending physician are necessary; local skin infections—avoid inserting the needle into areas with active infections.
2. Materials and Methods
- Inclusion criteria were:
- -
- age between 18 and 30 years old;
- -
- full dental arches (from 7 to 7);
- -
- Caucasian ethnic group.
- Exclusion criteria were:
- -
- partially or totally edentulous dental arches;
- -
- previous facial trauma,
- -
- maxillofacial surgery.
2.1. Patient’s History
2.2. Clinical Examination
2.2.1. Morphological Occlusion
- -
- 1 open bite;
- -
- 1 posterior cross-bite;
- -
- 3 deep-bites.
2.2.2. Functional Occlusion
2.3. Teethan®
2.3.1. Advantages of Teethan Method
2.3.2. Limits of Teethan Method
2.3.3. Teethan Protocol
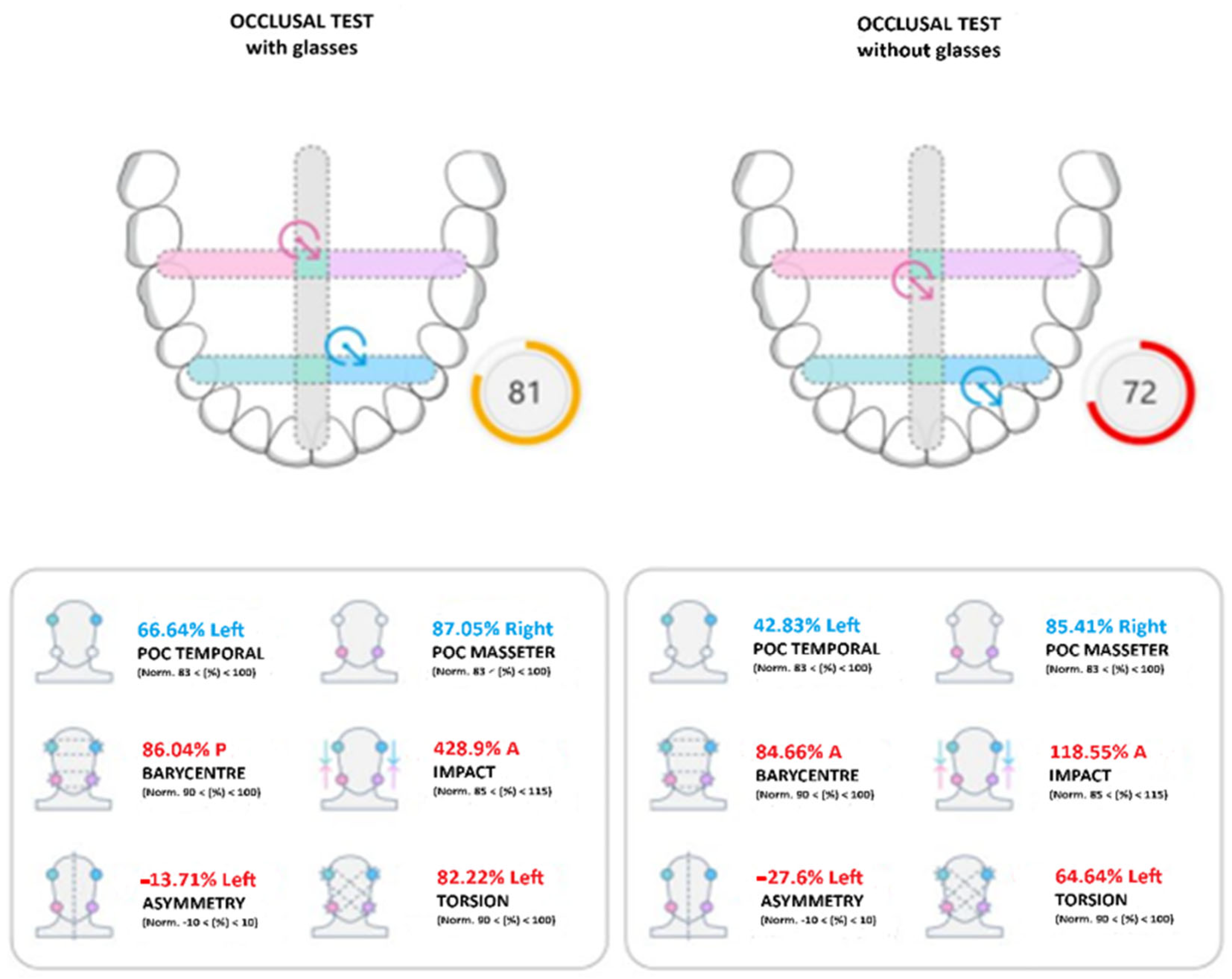
- OCCLUSAL-STATIC TEST: protocol for measuring the balance of dental occlusion.
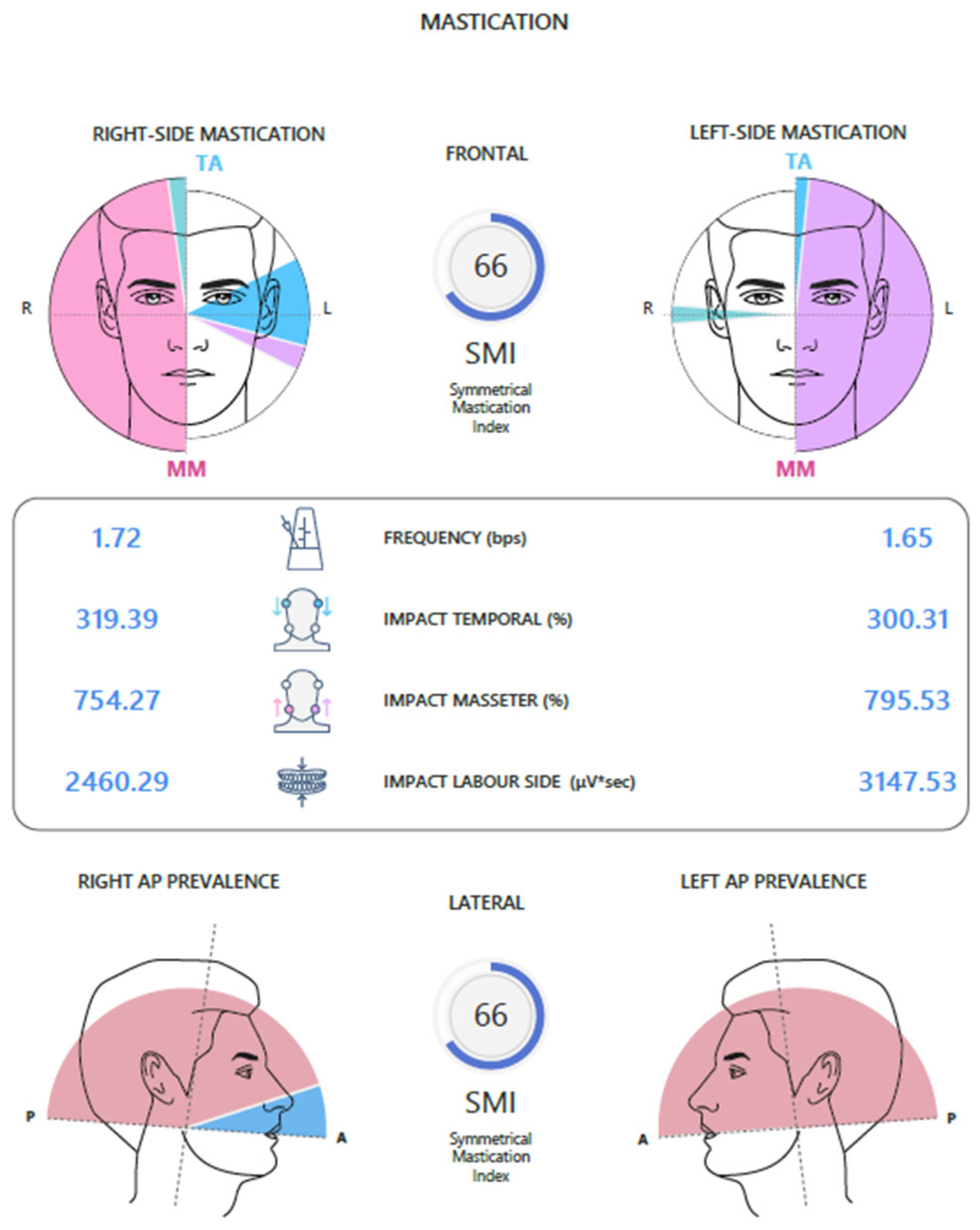
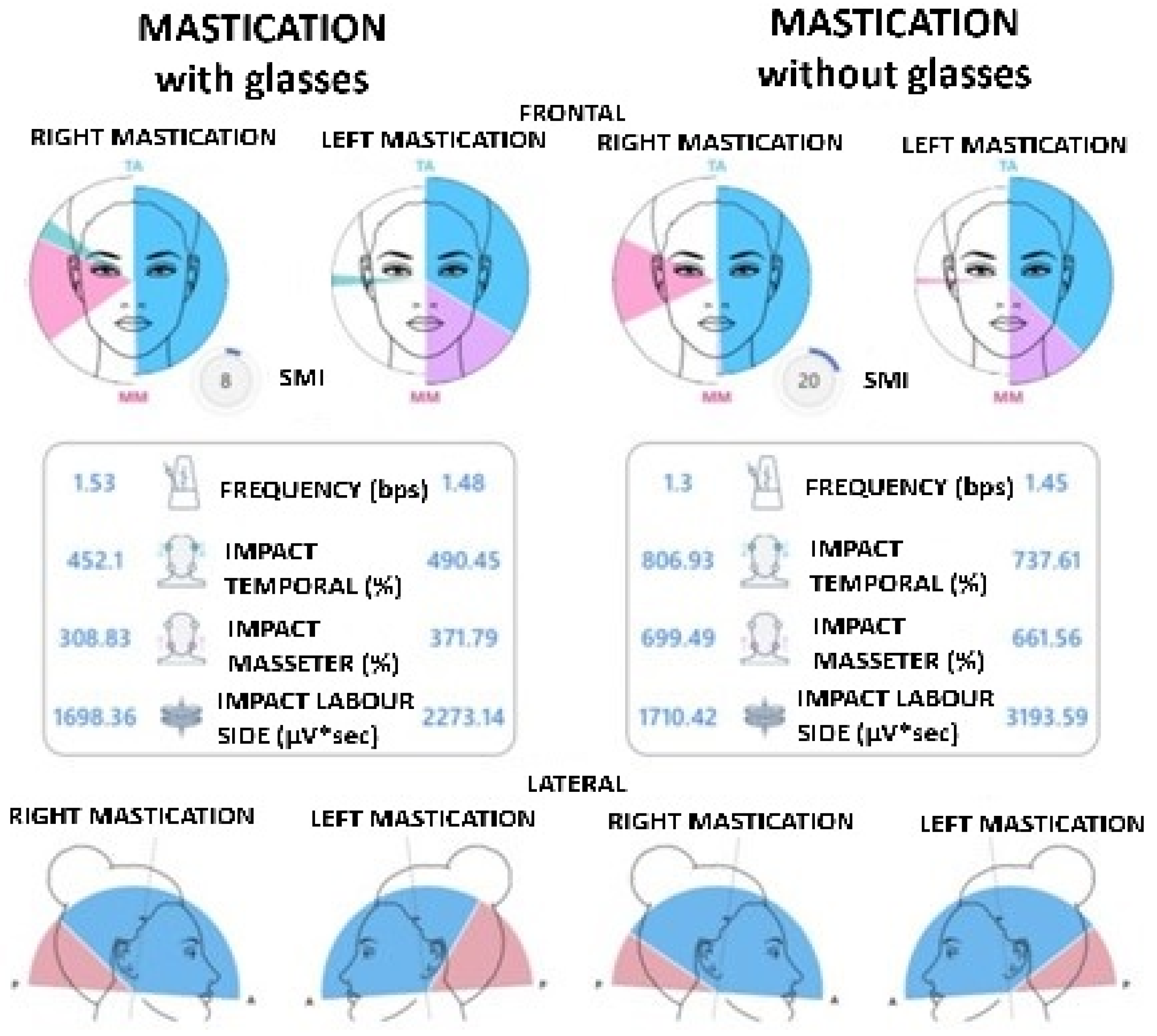
- DYNAMIC CHEWING TEST: protocol for the evaluation of neuromuscular coordination during the chewing act.
- OCCLUSAL TEST.
Parameters and Indices of the Occlusal Plane
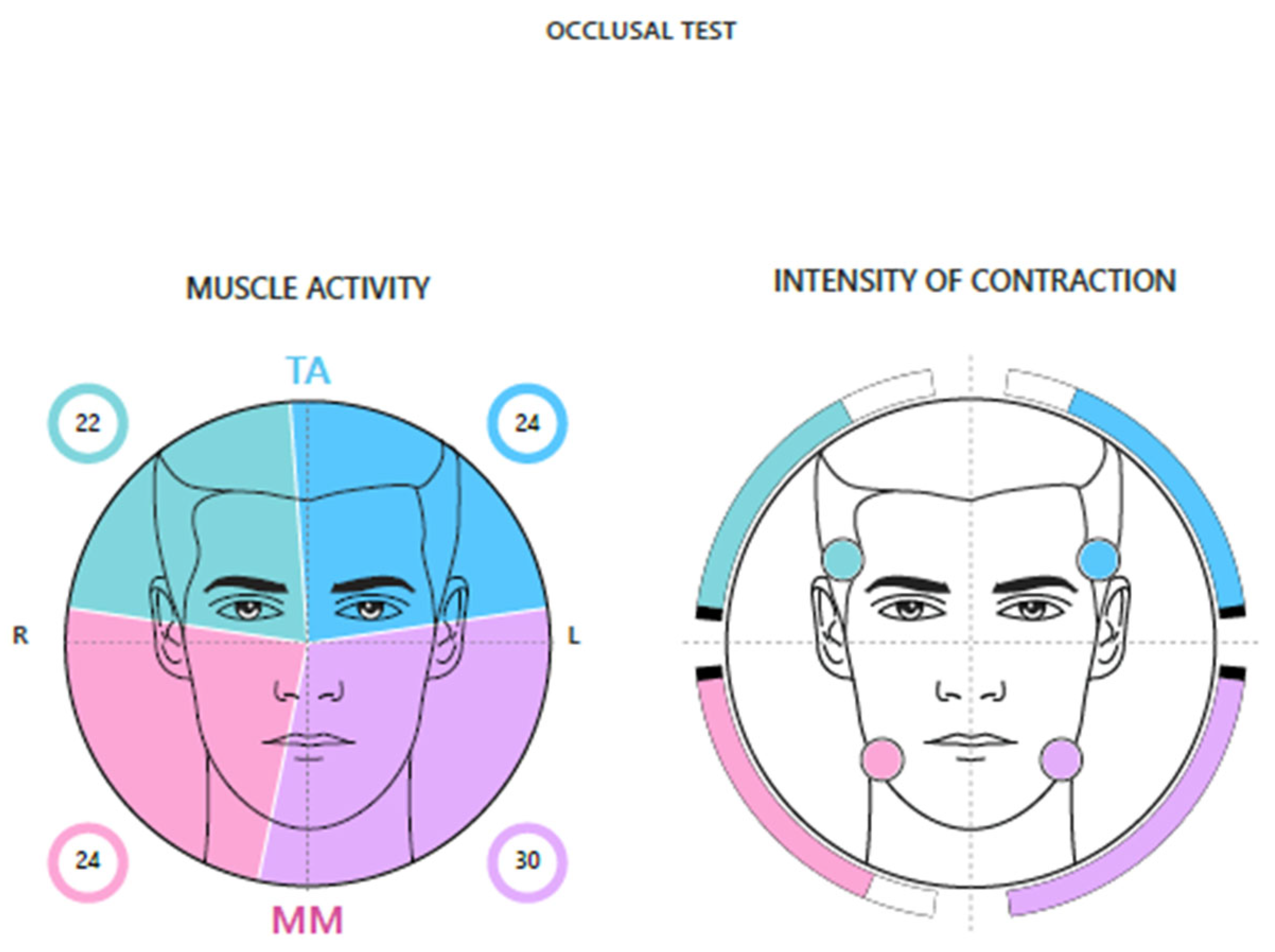
- The blue target refers to the activity of the temporalis muscles (which govern the front part of the mouth);
- The pink target refers to the activity of the masseter muscles (which govern the back of the mouth).
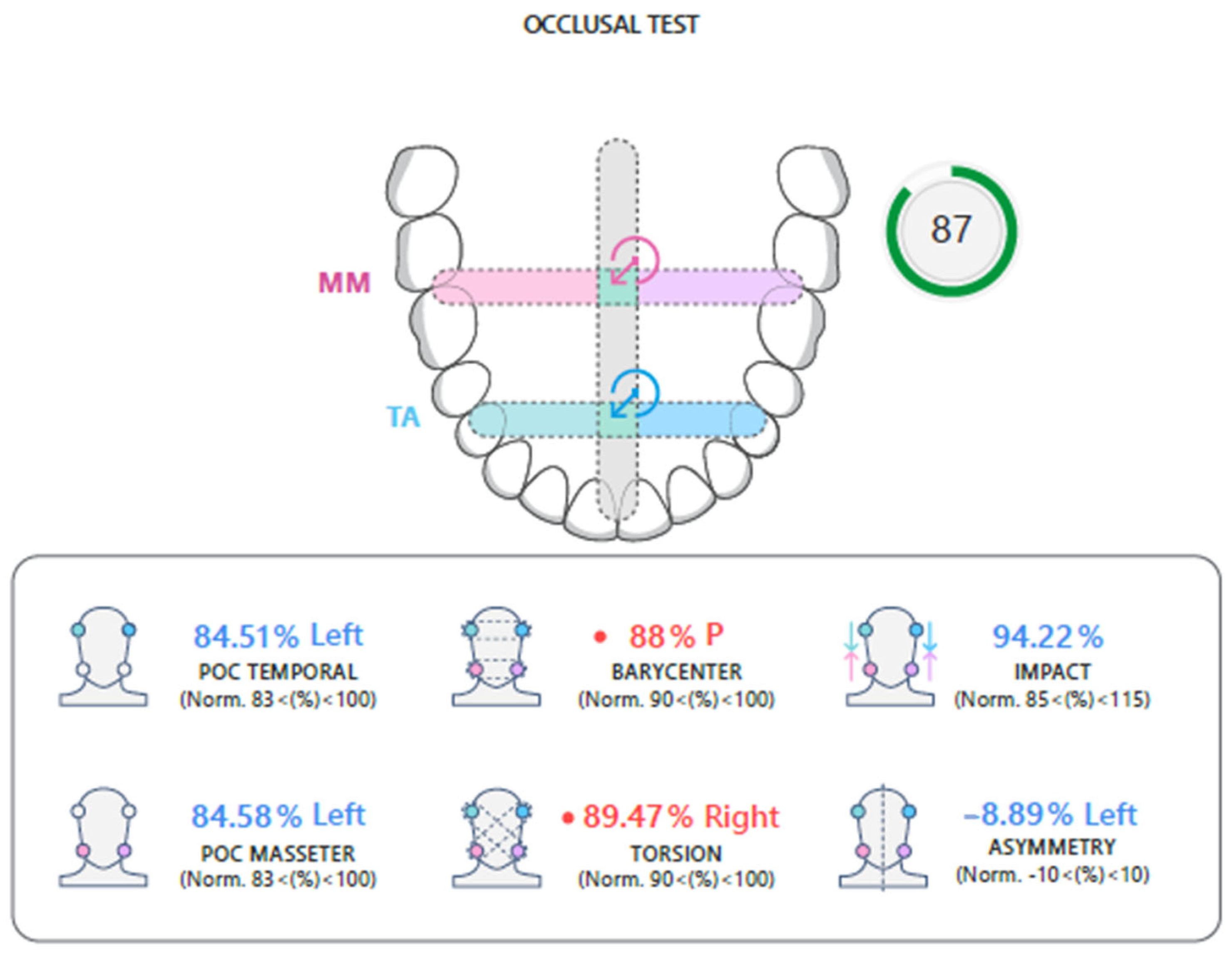
- Muscle Activity and Intensity of Muscle Contraction (Figure 3).
Muscle Electrical Activity
Normality Values and Notes
- Chewing Report;
- Notes page.
- -
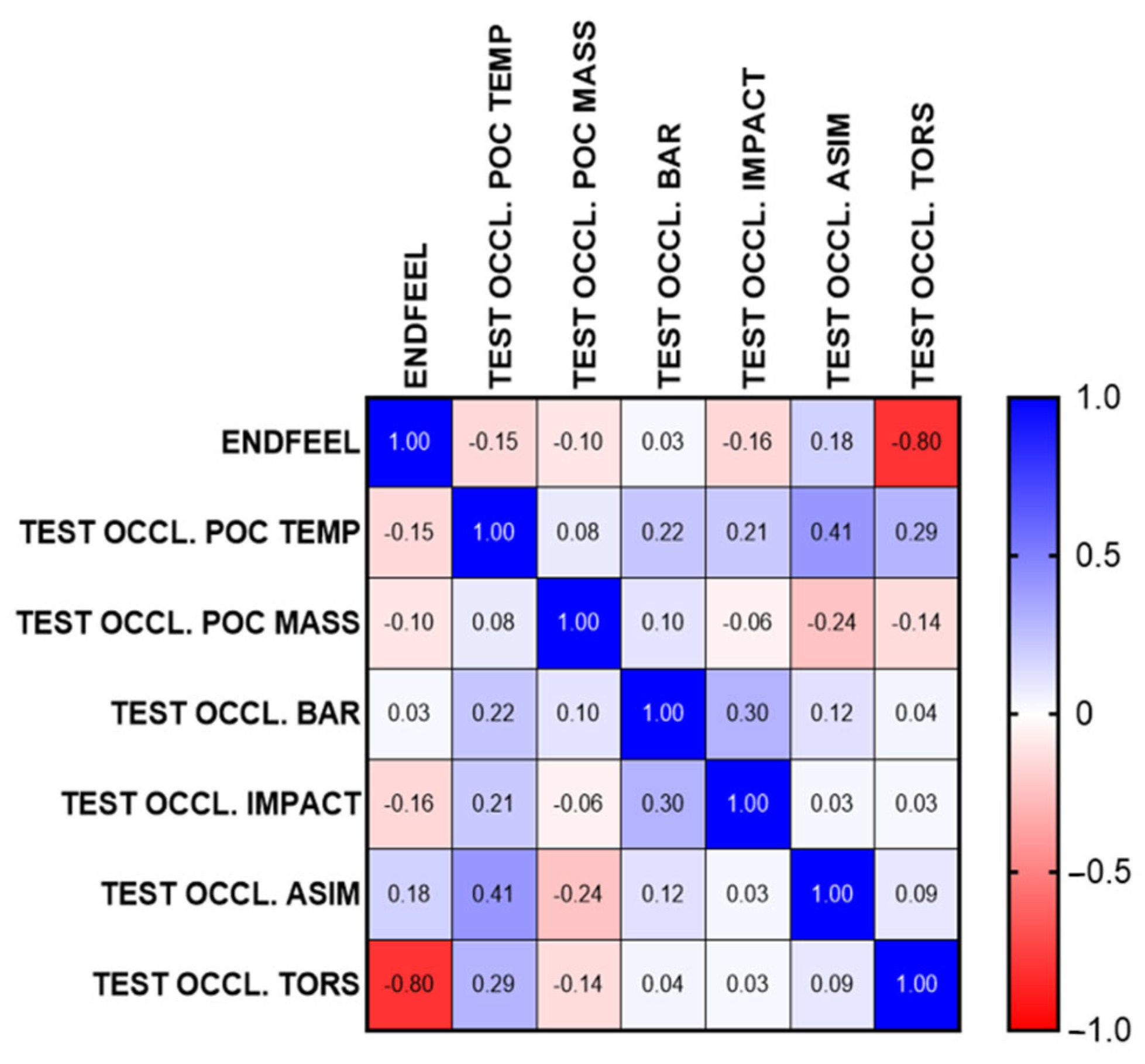
- Percentage Overlap Coefficient (POC): refers to the overall activity of the temporal and masseter muscles, specifying which muscle of each pair prevails.
- -
- Normal values are between 83% and 100%.
- -
- Center of gravity (BAR): compares the activity of the temporal muscles and the masseter muscles; physiologically, a posterior center of gravity is preferable, that is, with prevalent activity of the masseters compared to the temporals.
- -
- Normal values are between 90% and 100%.
- -
- Torsion (TORS): evaluates the crossed activity of the temporal muscles and the masseter muscles, revealing the torsion of the mandible on the horizontal plane.
- -
- Normal values are between 90% and 100%.
- -
- Muscle Work (IMPACT): refers to the intensity of the muscular work of the temporalis muscles and masseter muscles. A high intensity reveals a tightening patient, while a low intensity reveals the presence of nociceptive pain. Normal values are between 85% and 115%.
- -
- Asymmetry (ASIM): compares the activity of the temporal and masseter muscles on the right side and the activity of the temporal and masseter muscles on the left side, allowing identification of any asymmetry and the dominant side on the occlusal plane. Normal values are between −10% and 10%.
- -
- Global Symmetry Index (SMI): compares neuromuscular coordination during right and left chewing. The optimal value is 100%.
- -
- Chewing y: refers to the number of chewing acts per second.
- -
- Work Produced: evaluates the work produced by the temporalis and masseter muscles during the chewing cycles performed, as well as the work of the involved side, not normalized (Figure 6).
2.4. Statistical Analysis
3. Results
3.1. Occlusal Test Results (Static Condition)
3.2. Dynamic Test Results (Chewing)
3.3. Correlations Between Clinical Variables and EMG Parameters
3.4. Muscle Symmetry Analysis
3.5. Distribution of the Muscle Center of Gravity
3.6. Chewing Frequency and Lateral Preference
3.7. Subjective Results and Clinical Observations
4. Discussion
5. Conclusions
6. Patents
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| Abbreviation | Definition |
| AAOP | American Academy of Orofacial Pain |
| ASIM | Asymmetry |
| BAR | Center of Gravity |
| DC/TMD | Diagnostic Criteria for Temporomandibular Disorders |
| EMG | Electromyography |
| ENG | Electroneurography |
| IHS | International Headache Society |
| IMPACT | Muscle Work |
| MASS | Masseter |
| MI | Maximum Intercuspidation |
| MM | Masseter Muscle |
| OD | Oral Stage Dysphagia |
| OPT | Orthopantomography |
| POC | Percentage Overlapping Coefficient |
| RCD | Research Diagnostic Criteria |
| sEMG | Surface Electromyography |
| SMI | Global Symmetry Index |
| TA | Anterior Temporal |
| TENS | Transcutaneous Neural Electrical Stimulation |
| TMJ | Temporomandibular Joint |
| TORS | Torsion |
References
- Calabria, E.; Adamo, D.; Leuci, S.; Pecoraro, G.; Coppola, N.; Aria, M.; Mignogna, M.D. The health-related quality of life and psychological profile in patients with oropharyngeal Pemphigus Vulgaris in complete clinical remission: A case-control study. J. Oral Pathol. Med. 2021, 50, 510–519. [Google Scholar] [CrossRef]
- Canfora, F.; Calabria, E.; Pecoraro, G.; D’Aniello, L.; Aria, M.; Marenzi, G.; Sammartino, P.; Mignogna, M.D.; Adamo, D. The use of self-report questionnaires in an analysis of the multidimensional aspects of pain and a correlation with the psychological profile and quality of life in patients with burning mouth syndrome: A case-control study. J. Oral Rehabil. 2022, 49, 890–914. [Google Scholar] [CrossRef] [PubMed]
- Adamo, D.; Calabria, E.; Coppola, N.; Pecoraro, G.; Mignogna, M.D. Vortioxetine as a new frontier in the treatment of chronic neuropathic pain: A review and update. Ther. Adv. Psychopharmacol. 2021, 11, 20451253211034320. [Google Scholar] [CrossRef] [PubMed]
- Adamo, D.; Canfora, F.; Calabria, E.; Coppola, N.; Leuci, S.; Pecoraro, G.; Cuocolo, R.; Ugga, L.; D’Aniello, L.; Aria, M.; et al. White matter hyperintensities in Burning Mouth Syndrome assessed according to the Age-Related White Matter Changes scale. Front. Aging Neurosci. 2022, 14, 923720. [Google Scholar] [CrossRef]
- Ciavarella, D.; Mastrovincenzo, M.; D’Onofrio, V.; Chimenti, C.; Parziale, V.; Barbato, E.; Muzio, L.L. Saliva analysis by surface-enhanced laser desorption/ionization time-of-flight mass spectrometry (SELDI-TOF-MS) in orthodontic treatment: First pilot study. Prog. Orthod. 2011, 12, 126–131. [Google Scholar] [CrossRef]
- Kitagawa, K.; Kodama, N.; Manda, Y.; Mori, K.; Furutera, H.; Minagi, S. Effect of masseter muscle activity during wake-fulness and sleep on tooth wear. J. Prosthodont. Res. 2022, 66, 551–556. [Google Scholar] [CrossRef] [PubMed]
- Campobasso, A.; Lo Muzio, E.; Battista, G.; Ciavarella, D.; Crincoli, V.; Lo Muzio, L. Taxonomic Analysis of Oral Microbiome during Orthodontic Treatment. Int. J. Dent. 2021, 2021, 8275181. [Google Scholar] [CrossRef]
- Ciavarella, D.; Monsurrò, A.; Padricelli, G.; Battista, G.; Laino, L.; Perillo, L. Unilateral posterior crossbite in adolescents: Surface electromyographic evaluation. Eur. J. Paediatr. Dent. 2012, 13, 25–28. [Google Scholar]
- Inchingolo, F.; Inchingolo, A.M.; Latini, G.; Pezzolla, C.; Trilli, I.; Sardano, R.; Palermo, A.; Inchingolo, A.D.; Dipalma, G. Analysis of microbiota in black stain of children and its impact on caries risk. A systematic review. Eur. J. Paediatr. Dent. 2024, 1. [Google Scholar] [CrossRef]
- Pelo, S.; Correra, P.; Gasparini, G.; Marianetti, T.M.; Cervelli, D.; Grippaudo, C.; Boniello, R.; Azzuni, C.; Deli, R.; Moro, A. Three-dimensional analysis and treatment planning of hemimandibular hyperplasia. J. Craniofac. Surg. 2011, 22, 2227–2234. [Google Scholar] [CrossRef]
- Oliva, B.; Sferra, S.; Greco, A.L.; Valente, F.; Grippaudo, C. Three-dimensional analysis of dental arch forms in Italian population. Prog. Orthod. 2018, 19, 34. [Google Scholar] [CrossRef]
- Grippaudo, C.; D’Apolito, I.; Cafiero, C.; Re, A.; Chiurazzi, P.; Frazier-Bowers, S.A. Validating clinical characteristic of primary failure of eruption (PFE) associated with PTH1R variants. Prog. Orthod. 2021, 22, 43. [Google Scholar] [CrossRef]
- Grippaudo, C.; Paolantonio, E.G.; Deli, R.; La Torre, G. Validation of the Risk Of Malocclusion Assessment (ROMA) index. Eur. J. Paediatr. Dent. 2007, 8, 136–142. [Google Scholar] [PubMed]
- Al-Dboush, R.; Al-Zawawi, E.; El-Bialy, T. Does short-term treatment with clear aligner therapy induce changes in muscular activity? Evid.-Based Dent. 2024, 25, 6–8. [Google Scholar] [CrossRef] [PubMed]
- Al-Saleh, M.A.Q.; Jaremko, J.L.; Alsufyani, N.; Jibri, Z.; Lai, H.; Major, P.W. Assessing the reliability of MRI-CBCT image registration to visualize temporomandibular joints. Dentomaxillofac. Radiol. 2015, 44, 20140244. [Google Scholar] [CrossRef] [PubMed]
- Anderson, D.J.; Hannam, A.G.; Mathews, B. Sensory mechanisms in mammalian teeth and their supporting structures. Physiol. Rev. 1970, 50, 171–195. [Google Scholar] [CrossRef]
- Asano, T.; Zeredo, J.L.; Toda, K.; Soma, K. Periodontal Masseteric Reflex is Changed by Periodontal Sensory Modification during Occlusal Hypofunction in Rats. J. Med. Dent. Sci. 2007, 54, 31–37. [Google Scholar] [CrossRef]
- Wieckiewicz, M.; Boening, K.; Wiland, P.; Shiau, Y.-Y.; Paradowska-Stolarz, A. Reported concepts for the treatment modalities and pain management of temporomandibular disorders. J. Headache Pain 2015, 16, 106. [Google Scholar] [CrossRef]
- Bakke, M.; Michler, L.; Möller, E. Occlusal control of mandibular elevator muscles. Eur. J. Oral Sci. 1992, 100, 284–291. [Google Scholar] [CrossRef]
- Balkhi, K.M.; Tallents, R.H.; Katzberg, R.W.; Murphy, W.; Proskin, H. Activity of anterior temporalis and masseter muscles during deliberate unilateral mastication. J. Orofac. Pain 1993, 7, 89–97. [Google Scholar]
- Behr, M.; Held, P.; Leibrock, A.; Fellner, C.; Handel, G. Diagnostic potential of pseudo-dynamic MRI (CINE mode) for evaluation of internal derangement of the TMJ. Eur. J. Radiol. 1996, 23, 212–215. [Google Scholar] [CrossRef]
- Bezuur, J.N.; Hansson, T.L.; Wilkinson, T.M. The recognition of craniomandibular disorders—an evaluation of the most reliable signs and symptoms when screening for CMD. J. Oral Rehabil. 1989, 16, 367–372. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, F.; Inchingolo, A.D.; Riccaldo, L.; Costa, S.; Palermo, A.; Inchingolo, A.M.; Dipalma, G. Weight and dental eruption: The correlation between BMI and eruption. Eur. J. Paediatr. Dent. 2025, 1. [Google Scholar] [CrossRef]
- Tecco, S.; Crincoli, V.; Di Bisceglie, B.; Caputi, S.; Festa, F. Relation between facial morphology on lateral skull radiographs and sEMG activity of head, neck, and trunk muscles in Caucasian adult females. J. Electromyogr. Kinesiol. 2011, 21, 298–310. [Google Scholar] [CrossRef] [PubMed]
- Crincoli, V.; Piancino, M.G.; Iannone, F.; Errede, M.; Di Comite, M. Temporomandibular Disorders and Oral Features in Systemic Lupus Erythematosus Patients: An Observational Study of Symptoms and Signs. Int. J. Med. Sci. 2020, 17, 153–160. [Google Scholar] [CrossRef]
- Crincoli, V.; Favia, G.; LImongelli, L.; Tempesta, A.; Brienza, N. The Effectiveness of Ropivacaine and Mepivacaine in the Postoperative Pain after Third Lower Molar Surgery. Int. J. Med. Sci. 2015, 12, 862–866. [Google Scholar] [CrossRef]
- Achmad, H.; Areni, I.S.; Sumintarti, S.; Ramadhany, S.; Ardiansya, R.; Edy, S.; Kuandinata, W. Detection of Lip, Tongue, Masseter, and Temporalis Muscle Contractions with Electromyography Tools as an Early Diagnostic Medium for Dentoalveolar Malocclusion. Eur. J. Dent. 2024. [Google Scholar] [CrossRef] [PubMed]
- Pumklin, J.; Sowithayasakul, T.; Thaweemonkongsap, C.; Saptasevee, P.; Sangprasert, P. Effects of occlusal conditions on masseter and temporalis muscle activity: An electromyographic evaluation. Saudi Dent. J. 2023, 35, 946–952. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bogdanov, V. Repeatability of the Calibration Protocol for Emg Evaluation of the Occlusion with the Teethan Device. Acta Medica Bulg. 2024, 51, 95–101. [Google Scholar] [CrossRef]
- Bogdanov, V.; Chakalov, I. Evaluation of the occlusion with two different methods: A T-scan II occlusal analysis and the teethan synchromyography recording system. J. IMAB—Annu. Proceeding Sci. Pap. 2025, 31, 5956–5961. [Google Scholar] [CrossRef]
- Bogdanov, V.; Petrunov, V. EMG evaluation of the occlusion with teethan device: Effect of the muscles. J. IMAB 2024, 30, 5460–5465. [Google Scholar] [CrossRef]
- Bonjardim, L.R.; Lopes-Filho, R.J.; Amado, G.; Albuquerque, R.L.; Goncalves, S.R. Association between symptoms of temporomandibular disorders. Indian J. Dent. Res. 2009, 20, 190–194. [Google Scholar] [CrossRef] [PubMed]
- Hellmann, D.; Brüstle, F.; Terebesi, S.; Giannakopoulos, N.N.; Eberhard, L.; Rammelsberg, P.; Schindler, H.J. Static balancing behaviour of the mandible. Eur. J. Oral Sci. 2015, 123, 439–446. [Google Scholar] [CrossRef] [PubMed]
- Ciavarella, D.; Tepedino, M.; Gallo, C.; Montaruli, G.; Zhurakivska, K.; Coppola, L.; Troiano, G.; Chimenti, C.; Laurenziello, M.; Lo Russo, L. Post-orthodontic position of lower incisors and gingival recession: A retrospective study. J. Clin. Exp. Dent. 2017, 9, e1425–e1430. [Google Scholar] [CrossRef]
- Gallo, C.; Ciavarella, D.; Santarelli, A.; Ranieri, E.; Colella, G.; Muzio, L.L.; Russo, L.L. Potential Salivary Proteomic Markers of Oral Squamous Cell Carcinoma. Cancer Genom. Proteom. 2016, 13, 55–61. [Google Scholar]
- Cazzolla, A.P.; Zhurakivska, K.; Ciavarella, D.; Lacaita, M.G.; Favia, G.; Testa, N.F.; Marzo, G.; La Carbonara, V.; Troiano, G.; Muzio, L.L. Primary hyperoxaluria: Orthodontic management in a pediatric patient: A case report. Spec. Care Dent. 2018, 38, 259–265. [Google Scholar] [CrossRef]
- Laforgia, A.; Dipalma, G.; Inchingolo, A.D.; Chieppa, S.; Colonna, V.; Tartaglia, F.C.; Tari, S.R.; Bugea, C.; Corsalini, M.; Palermo, A.; et al. Dental issues following the placement of orthodontic mini-screws. Eur. J. Musculoskelet. Dis. 2024, 13, 28–36. [Google Scholar]
- Adamo, D.; Gasparro, R.; Marenzi, G.; Mascolo, M.; Cervasio, M.; Cerciello, G.; De Novellis, D.; Mignogna, M.D. Amyloidoma of the Tongue: Case Report, Surgical Management, and Review of the Literature. J. Oral Maxillofac. Surg. 2020, 78, 1572–1582. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Ceci, S.; Patano, A.; Inchingolo, A.M.; Montenegro, V.; Di Pede, C.; Malcangi, G.; Marinelli, G.; Coloccia, G.; Garibaldi, M.; et al. Elastodontic Therapy of Hyperdivergent Class II Patients Using AMCOP® Devices: A Retrospective Study. Appl. Sci. 2022, 12, 3259. [Google Scholar] [CrossRef]
- Almeida, L.E.; Cicciù, M.; Doetzer, A.; Beck, M.L.; Cervino, G.; Minervini, G. Mandibular condylar hyperplasia and its correlation with vascular endothelial growth factor. J. Oral Rehabil. 2023, 50, 845–851. [Google Scholar] [CrossRef]
- Alshadidi, A.A.F.; Alshahrani, A.A.; Aldosari, L.I.N.; Chaturvedi, S.; Saini, R.S.; Hassan, S.A.B.; Cicciù, M.; Minervini, G. Investigation on the Application of Artificial Intelligence in Prosthodontics. Appl. Sci. 2023, 13, 5004. [Google Scholar] [CrossRef]
- Saccomanno, S.; Martini, C.; D’Alatri, L.; Farina, S.; Grippaudo, C. A specific protocol of myo-functional therapy in children with Down syndrome. A pilot study. Eur. J. Paediatr. Dent. 2018, 19, 243–246. [Google Scholar] [CrossRef] [PubMed]
- Saccomanno, S.; Antonini, G.; D’Alatri, L.; D’Angeloantonio, M.; Fiorita, A.; Deli, R. Case report of patients treated with an orthodontic and myofunctional protocol. Eur. J. Paediatr. Dent. 2014, 15, 184–186. [Google Scholar] [PubMed]
- Saccomanno, S.; Passarelli, P.C.; Oliva, B.; Grippaudo, C. Comparison between Two Radiological Methods for Assessment of Tooth Root Resorption: An In Vitro Study. BioMed Res. Int. 2018, 2018, 5152172. [Google Scholar] [CrossRef]
- Saccomanno, S.; Ieria, I.; Manenti, R.J.; Giancaspro, S.; Pirelli, P. Complications of oral piercing: A review of the literature and two case reports. J. Biol. Regul. Homeost. Agents 2021, 35, 167–178. [Google Scholar] [CrossRef]
- Quinzi, V.; Paskay, L.C.; D’Andrea, N.; Albani, A.; Monaco, A.; Saccomanno, S. Evaluation of the Nasolabial Angle in Orthodontic Diagnosis: A Systematic Review. Appl. Sci. 2021, 11, 2531. [Google Scholar] [CrossRef]
- Angelelli, G.; Moschetta, M.; Limongelli, L.; Albergo, A.; Lacalendola, E.; Brindicci, F.; Favia, G.; Maiorano, E. Endocavitary sonography of early oral cavity malignant tumors. Head Neck 2017, 39, 1349–1356. [Google Scholar] [CrossRef]
- Annibali, S.; Cristalli, M.P.; Solidani, M.; Ciavarella, D.; La Monaca, G.; Suriano, M.M.; Muzio, L.L.; Russo, L.L. Langerhans cell histiocytosis: Oral/periodontal involvement in adult patients. Oral Dis. 2009, 15, 596–601. [Google Scholar] [CrossRef]
- Antonelli, A.; Bennardo, F.; Brancaccio, Y.; Barone, S.; Femiano, F.; Nucci, L.; Minervini, G.; Fortunato, L.; Attanasio, F.; Giudice, A. Can Bone Compaction Improve Primary Implant Stability? An In Vitro Comparative Study with Osseodensification Technique. Appl. Sci. 2020, 10, 8623. [Google Scholar] [CrossRef]
- Aquilanti, L.; Alia, S.; Pugnaloni, S.; Coccia, E.; Mascitti, M.; Santarelli, A.; Limongelli, L.; Favia, G.; Mancini, M.; Vignini, A.; et al. Impact of Elderly Masticatory Performance on Nutritional Status: An Observational Study. Medicina 2020, 56, 130. [Google Scholar] [CrossRef]
- Arezzo, F.; Cormio, G.; La Forgia, D.; Santarsiero, C.M.; Mongelli, M.; Lombardi, C.; Cazzato, G.; Cicinelli, E.; Loizzi, V. A machine learning approach applied to gynecological ultrasound to predict progression-free survival in ovarian cancer patients. Arch. Gynecol. Obstet. 2022, 306, 2143–2154. [Google Scholar] [CrossRef] [PubMed]
- Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Headache Classification Committee of the International Headache Society. Cephalalgia 1988, 8 (Suppl. 7), 1–96. [Google Scholar]
- Zieliński, G.; Matysik-Woźniak, A.; Baszczowski, M.; Rapa, M.; Ginszt, M.; Zawadka, M.; Szkutnik, J.; Rejdak, R.; Gawda, P. Effects of visual input on changes in the bioelectrical activity of the cervical and masticatory muscles in myopic subjects. Sci. Rep. 2022, 12, 9435. [Google Scholar] [CrossRef] [PubMed]
- Williams, W.N.; Low, S.B.; Cooper, W.R.; Cornell, C.E. The effect of periodontal bone loss on bite force discrimination. J. Periodontol. 1987, 58, 236–239. [Google Scholar] [CrossRef]
- Wieczorek, A.; Loster, J.; Loster, B.W. Relationship between occlusal force distribution and the activity of masseter and anterior temporalis muscles in asymptomatic young adults. BioMed Res. Int. 2013, 2013, 354017. [Google Scholar] [CrossRef]
- Widmalm, S.E.; Hedegard, B. Reflex activity in the masseter muscle of young individuals: I. Experimental procedure—Results. J. Oral Rehabil. 1976, 3, 41–55. [Google Scholar] [CrossRef]
- Weinberg, L.A. Vertical dimension: A research and clinical analysis. J. Prosthet. Dent. 1982, 47, 290–302. [Google Scholar] [CrossRef]
- Watanabe, K. The relationship between dentofacial morphology and the isometric jaw-opening and closing muscle function as evaluated by electromyography. J. Oral Rehabil. 2000, 27, 639–645. [Google Scholar] [CrossRef]
- Giacomini, P.S. Electromyography and Neuromuscular Disorders: Clinical Electrophysiologic Correlations. McGill J. Med. MJM 2006, 9, 173. [Google Scholar]
- Saracutu, O.I.; Pollis, M.; Cagidiaco, E.F.; Ferrari, M.; Manfredini, D. Repeatability of Teethan® indexes analysis of the masseter and anterior temporalis muscles during maximum clenching: A pilot study. Clin. Oral Investig. 2023, 27, 5309–5316. [Google Scholar] [CrossRef]
- Vogl, T.J.; Lauer, H.-C.; Lehnert, T.; Naguib, N.N.N.; Ottl, P.; Filmann, N.; Soekamto, H.; Nour-Eldin, N.-E.A. The value of MRI in patients with temporomandibular joint dysfunction: Correlation of MRI and clinical findings. Eur. J. Radiol. 2016, 85, 714–719. [Google Scholar] [CrossRef]
- Valenti, C.; Di Pasquale, F.; Pancrazi, G.P.; Falocci, N.; Nanussi, A.; Biscarini, A.; Pagano, S. Evaluation of different electromyographic parameters of temporomandibular dysfunction in athletes. J. Bodyw. Mov. Ther. 2025, 42, 56–63. [Google Scholar] [CrossRef]
- Tuller, B.; Harris, K.S.; Gross, B. Electromyographic study of the jaw muscles during speech. J. Phon. 1981, 9, 175–188. [Google Scholar] [CrossRef]
- Bambini, F.; Greci, L.; Memè, L.; Santarelli, A.; Carinci, F.; Pezzetti, F.; Procaccini, M.; Muzio, L.L. Raloxifene covalently bonded to titanium implants by interfacing with (3-aminopropyl)-triethoxysilane affects osteoblast-like cell gene expression. Int. J. Immunopathol. Pharmacol. 2006, 19, 905–914. [Google Scholar] [CrossRef] [PubMed]
- Rossi, R.; Memè, L.; Strappa, E.M.; Bambini, F. Restoration of Severe Bone and Soft Tissue Atrophy by Means of a Xenogenic Bone Sheet (Flex Cortical Sheet): A Case Report. Appl. Sci. 2023, 13, 692. [Google Scholar] [CrossRef]
- Memè, L.; Strappa, E.M.; Monterubbianesi, R.; Bambini, F.; Mummolo, S. SEM and FT-MIR Analysis of Human Demineralized Dentin Matrix: An In Vitro Study. Appl. Sci. 2022, 12, 1480. [Google Scholar] [CrossRef]
- Memè, L.; Bambini, F.; Gallusi, G.; Sartini, D.; Pozzi, V.; Emanuelli, M.; Strappa, E.M.; Mummolo, S. The Effect and the Potential Use of Magnetic–Dam Barrier in Guided Bone Regeneration: A Laboratory Study. Appl. Sci. 2023, 13, 1625. [Google Scholar] [CrossRef]
- Alghadir, A.H.; Zafar, H.; Iqbal, Z.A.; Al-Eisa, E.S. Effect of voluntary teeth clenching and sitting posture on maximal static force of limb muscles. J. Sports Med. Phys. Fit. 2019, 59, 774–778. [Google Scholar] [CrossRef] [PubMed]
- Crincoli, V.; Ballini, A.; Fatone, L.; Di Bisceglie, M.B.; Nardi, G.M.; Grassi, F.R. Cytokine genotype distribution in patients with periodontal disease and rheumatoid arthritis or diabetes mellitus. J. Biol. Regul. Homeost. Agents 2016, 30, 863–866. [Google Scholar]
- Dioguardi, M.; Cantore, S.; Scacco, S.; Quarta, C.; Sovereto, D.; Spirito, F.; Alovisi, M.; Troiano, G.; Aiuto, R.; Garcovich, D.; et al. From Bench to Bedside in Precision Medicine: Diabetes Mellitus and Peri-Implantitis Clinical Indices with a Short-Term Follow-Up: A Systematic Review and Meta-Analysis. J. Pers. Med. 2022, 12, 235. [Google Scholar] [CrossRef]
- Manfredini, D.; Lombardo, L.; Visentin, A.; Arreghini, A.; Siciliani, G. Correlation Between Sleep-Time Masseter Muscle Activity and Tooth Wear: An Electromyographic Study. J. Oral Facial Pain Headache 2019, 33, 199–204. [Google Scholar] [CrossRef] [PubMed]
- Tecco, S.; Quinzi, V.; Nota, A.; Giovannozzi, A.; Abed, M.R.; Marzo, G. Electromyography-Guided Adjustment of an Occlusal Appliance: Effect on Pain Perceptions Related with Temporomandibular Disorders. A Controlled Clinical Study. Diagnostics 2021, 11, 667. [Google Scholar] [CrossRef] [PubMed]
- Talley, R.L.; Murphy, G.J.; Smith, S.D.; Baylin, M.A.; Haden, J.L. Standards for the history, examination, diagnosis, and treatment of temporomandibular disorders (TMD): A position paper. CRANIO® 1990, 8, 60–77. [Google Scholar] [CrossRef] [PubMed]
- Tallents, R.H.; Macher, D.J.; Kyrkanides, S.; Katzberg, R.W.; Moss, M.E. Prevalence of missing posterior teeth and intraarticular temporomandibular disorders. J. Prosthet. Dent. 2002, 87, 45–50. [Google Scholar] [CrossRef]
- Szyszka-Sommerfeld, L.; Sycińska-Dziarnowska, M.; Cernera, M.; Esposito, L.; Woźniak, K.; Spagnuolo, G. Electromyographic Assessment of Muscle Activity in Children Undergoing Orthodontic Treatment-A Systematic Review. J. Clin. Med. 2024, 13, 2051. [Google Scholar] [CrossRef]
- Hobo, S.; Ichida, E.; Garcia, L. Osteointegrazione e Riabilitazione Occlusale; Utet: Turin, Italy, 1993; Available online: https://www.unilibro.it/libro/hobo-sumiya-ichida-eiji-garcia-lily/osteointegrazione-riabilitazione-occlusale/961199?srsltid=AfmBOoptw9gD7De7VwIt8rVZaB7Nt3NPXYbyh2QkOb5KMCdaT-MK2sod (accessed on 4 July 2025).
- Inchingolo, F.; Inchingolo, A.M.; Ferrante, L.; de Ruvo, E.; Di Noia, A.; Palermo, A.; Inchingolo, A.D.; Dipalma, G. Pharmacological Sedation in Paediatric Dentistry. Eur. J. Paediatr. Dent. 2024, 25, 230–237. [Google Scholar] [CrossRef]
- Marchetti, E.; Tecco, S.; Caterini, E.; Casalena, F.; Quinzi, V.; Mattei, A.; Marzo, G. Alcohol-free essential oils containing mouthrinse efficacy on three-day supragingival plaque regrowth: A randomized crossover clinical trial. Trials 2017, 18, 154. [Google Scholar] [CrossRef]
- Pasini, M.; Giuca, M.R.; Ligori, S.; Mummolo, S.; Fiasca, F.; Marzo, G.; Quinzi, V. Association between Anatomical Variations and Maxillary Canine Impaction: A Retrospective Study in Orthodontics. Appl. Sci. 2020, 10, 5638. [Google Scholar] [CrossRef]
- Campanella, V.; Gallusi, G.; Nardi, R.; Mea, A.; Di Taranto, V.; Montemurro, E.; Marzo, G.; Libonati, A. Dentinal substrate variability and bonding effectiveness: SEM investigation. J. Biol. Regul. Homeost. Agents 2020, 34, 49–54. [Google Scholar]
- Stegenga, B.; de Bont, L.G.; Boering, G.; van Willigen, J.D. Tissue responses to degenerative changes in the temporomandibular joint: A review. J. Oral Maxillofac. Surg. 1991, 49, 1079–1088. [Google Scholar] [CrossRef]
- SCHROEDER, D.K.; SCHROEDER, M.A.; VASCONCELOS, V. Agenesis of maxillary lateral incisors: Diagnosis and treatment options. Dent. Press J. Orthod. 2022, 27, e22spe1. [Google Scholar] [CrossRef]
- Rugh, J.D.; Drago, C.J. Vertical dimension: A study of clinical rest position and jaw muscle activity. J. Prosthet. Dent. 1981, 45, 670–675. [Google Scholar] [CrossRef]
- Robinson, P.D. Articular cartilage of the temporomandibular joint: Can it regenerate? Ann. R. Coll. Surg. Engl. 1993, 75, 231–236. [Google Scholar] [PubMed]
- Memè, L.; Pizzolante, T.; Saggiomo, A.P.; Plaku, D.; Inchingolo, A.D.; Inchingolo, F.; Rastelli, S. The use of ozone therapy for the treatment and post-surgical management of patients treated with bilateral extraction of the included third mandibular molars. Oral Implantol. J. Innov. Adv. Tech. Oral Health 2024, 16, 124–132. [Google Scholar] [CrossRef]
- Inchingolo, A.M.; Malcangi, G.; Costa, S.; Fatone, M.C.; Avantario, P.; Campanelli, M.; Piras, F.; Patano, A.; Ferrara, I.; Di Pede, C.; et al. Tooth Complications after Orthodontic Miniscrews Insertion. Int. J. Environ. Res. Public Health 2023, 20, 1562. [Google Scholar] [CrossRef] [PubMed]
- Tortarolo, A.; Rotolo, R.; Nucci, L.; Tepedino, M.; Crincoli, V.; Piancino, M.G. Condylar Asymmetry in Children with Unilateral Posterior Crossbite Malocclusion: A Comparative Cross-Sectional Study. Children 2022, 9, 1772. [Google Scholar] [CrossRef]
- Tagore, S.; Reche, A.; Paul, P.; Deshpande, M. Electromyography: Processing, Muscles’ Electric Signal Analysis, and Use in Myofunctional Orthodontics. Cureus 2023, 15, e50773. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pröschel, P.; Hofmann, M. Frontal chewing patterns of the incisor point and their dependence on resistance of food and type of occlusion. J. Prosthet. Dent. 1988, 59, 617–624. [Google Scholar] [CrossRef]
- Piancino, M.G.; Tortarolo, A.; Di Benedetto, L.; Crincoli, V.; Falla, D. Chewing Patterns and Muscular Activation in Deep Bite Malocclusion. J. Clin. Med. 2022, 11, 1702. [Google Scholar] [CrossRef]
- Orthlieb, J.D.; Re, J.P.; Rerez, C.; Darmouni, L.; Mantout, B.; Gossin, G.; Giraudeau, A. La Relation Centrée Myostabilisée un Concept Simple, Physiologique et Consensual; CDP: London, UK, 2008; Available online: https://www.researchgate.net/publication/353175091_La_relation_centree_myostabilisee_Un_concept_simple_physiologique_et_consensuel (accessed on 4 July 2025).
- Mongini, F. L’Apparato Stomatognatico—Funzione, Disfunzione e Riabilitazione; Scienza Tecnica Dentistica: Milano, Italy, 1989; Available online: https://www.medicalinformation.it/l-apparato-stomatognatico-funzione-disfunzione-e-riabilitazione-mongini-franco.html (accessed on 20 May 2025).
- Monaco, A.; Ortu, E.; Giannoni, M.; D’Andrea, P.; Cattaneo, R.; Mummolo, A.; Pietropaoli, D. Standard Correction of Vision Worsens EMG Activity of Pericranial Muscles in Chronic TMD Subjects. Pain Res. Manag. 2020, 2020, 3932476. [Google Scholar] [CrossRef]
- Moller, E. The chewing apparatus. An electromyographic study of the action of the muscles of mastication and its correlation to facial morphology. Acta Physiol. Scand. 1966, 280, 1–229. [Google Scholar]
- Sammartino, G.; Gasparro, R.; Marenzi, G.; Trosino, O.; Mariniello, M.; Riccitiello, F. Extraction of mandibular third molars: Proposal of a new scale of difficulty. Br. J. Oral Maxillofac. Surg. 2017, 55, 952–957. [Google Scholar] [CrossRef]
- Marenzi, G.; Spagnuolo, G.; Sammartino, J.C.; Gasparro, R.; Rebaudi, A.; Salerno, M. Micro-Scale Surface Patterning of Titanium Dental Implants by Anodization in the Presence of Modifying Salts. Materials 2019, 12, 1753. [Google Scholar] [CrossRef] [PubMed]
- Mortellaro, C.; Dall’Oca, S.; Lucchina, A.G.; Castiglia, A.; Farronato, G.; Fenini, E.; Marenzi, G.; Trosino, O.; Cafiero, C.; Sammartino, G. Sublingual ranula: A closer look to its surgical management. J. Craniofac. Surg. 2008, 19, 286–290. [Google Scholar] [CrossRef] [PubMed]
- Scandurra, C.; Gasparro, R.; Dolce, P.; Bochicchio, V.; Muzii, B.; Sammartino, G.; Marenzi, G.; Maldonato, N.M. The role of cognitive and non-cognitive factors in dental anxiety: A mediation model. Eur. J. Oral Sci. 2021, 129, e12793. [Google Scholar] [CrossRef] [PubMed]
- McNamara, J.A. The independent functions of the two heads of the lateral pterygoid muscle. Am. J. Anat. 1973, 138, 197–205. [Google Scholar] [CrossRef]
- Ming, X.; Cheng, X.; Tian, C.; Li, W.; Wang, R.; Qian, C.; Zeng, X. Evaluation of condylar osseous changes using a wireless detector with proton density–weighted imaging sequences. Quant. Imaging Med. Surg. 2023, 13, 17–26. [Google Scholar] [CrossRef]
- McNeill, C. Science and Practice of Occlusion; Quintessence Pub. Co.: Batvia, IL, USA, 1997; ISBN 978-0-86715-304-0. [Google Scholar]
- Maruyama, T. Esthetics: Occlusion and function. J. Esthet. Restor. Dent. 1994, 6, 295–299. [Google Scholar] [CrossRef]
- Marklund, S.; Wänman, A. Incidence and prevalence of temporomandibular joint pain and dysfunction. A one-year prospective study of university students. Acta Odontol. Scand. 2007, 65, 119–127. [Google Scholar] [CrossRef]
- Manni, A.; Brunori, P.; Ursini, R.; Deli, R. L’occlusione neuromuscolare nella terapia ortodontica del paziente con disordini craniomandibolari. Caso clinic. Minerva Stomatol. 2002, 51, 95–102. Available online: https://www.minervamedica.it/it/riviste/minerva-dental-and-oralscience/articolo.php?cod=R18Y2002N03A0095 (accessed on 27 May 2025).
- D‘Ettorre, G.; Farronato, M.; Candida, E.; Quinzi, V.; Grippaudo, C. A comparison between stereophotogrammetry and smartphone structured light technology for three-dimensional face scanning. Angle Orthod. 2022, 92, 358–363. [Google Scholar] [CrossRef] [PubMed]
- Quinzi, V.; Orilisi, G.; Vitiello, F.; Notarstefano, V.; Marzo, G.; Orsini, G. A spectroscopic study on orthodontic aligners: First evidence of secondary microplastic detachment after seven days of artificial saliva exposure. Sci. Total Environ. 2023, 866, 161356. [Google Scholar] [CrossRef] [PubMed]
- Memè, L.; Notarstefano, V.; Sampalmieri, F.; Orilisi, G.; Quinzi, V. ATR-FTIR Analysis of Orthodontic Invisalign® Aligners Subjected to Various In Vitro Aging Treatments. Materials 2021, 14, 818. [Google Scholar] [CrossRef] [PubMed]
- Quinzi, V.; Panetta, G.; Filippi, P.; Rizzo, F.A.; Mancini, L.; Mummolo, S. Autotransplatation of immature third molars as substitutes for congenitally missing second premolars: An alternative solution in a young patient with oligodontia. J. Biol. Regul. Homeost. Agents 2020, 34, 155–163. [Google Scholar]
- Saccomanno, S.; Mummolo, S.; Giancaspro, S.; Manenti, R.J.; Mastrapasqua, R.F.; Marzo, G.; Quinzi, V. Catering Work Profession and Medico-Oral Health: A Study on 603 Subjects. Healthcare 2021, 9, 582. [Google Scholar] [CrossRef]
- Manni, A.; Brunori, P.; Ursini, R.; Deli, R. Neuromuscular occlusion in the orthodontic treatment of craniomandibular disorders. A clinical case. Minerva Stomatol. 2002, 51, 95–101. [Google Scholar]
- Manfredini, D.; Castroflorio, T.; Perinetti, G.; Guarda-Nardini, L. Dental occlusion, body posture and temporomandibular disorders: Where we are now and where we are heading for. J. Oral Rehabil. 2012, 39, 463–471. [Google Scholar] [CrossRef]
- Nanussi, A.; Costa, G.; Baldoni, M. Treatment of Temporomandibular Disorders of Muscular Origin with a Silicon Oral Device (Alifix®): Electromyographic Analysis. J. Contemp. Dent. Pract. 2019, 20, 1367–1374. [Google Scholar]
- MacDonald, J.W.; Hannam, A.G. Relationship between occlusal contacts and jaw-closing muscle activity during tooth clenching: Part I. J. Prosthet. Dent. 1984, 52, 718–728. [Google Scholar] [CrossRef]
- Liu, Z.J.; Yamagata, K.; Kasahara, Y.; Ito, G. Electromyographic examination of jaw muscles in relation to symptoms and occlusion of patients with temporomandibular joint disorders. J. Oral Rehabil. 1999, 26, 33–47. [Google Scholar] [CrossRef]
- Lauriti, L.; Motta, L.J.; de Godoy, C.H.L.; Biasotto-Gonzalez, D.A.; Politti, F.; Mesquita-Ferrari, R.A.; Fernandes, K.P.S.; Bussadori, S.K. Influence of temporomandibular disorder on temporal and masseter muscles and occlusal contacts in adolescents: An electromyographic study. BMC Musculoskelet. Disord. 2014, 15, 123. [Google Scholar] [CrossRef] [PubMed]
- Di Stasio, D.; Romano, A.; Paparella, R.S.; Gentile, C.; Serpico, R.; Minervini, G.; Candotto, V.; Laino, L. How social media meet patients’ questions: YouTube™ review for mouth sores in children. J. Biol. Regul. Homeost. Agents 2018, 32, 117–121. [Google Scholar] [PubMed]
- Di Stasio, D.; Lauritano, D.; Romano, A.; Salerno, C.; Minervini, G.; Minervini, G.; Gentile, E.; Serpico, R.; Lucchese, A. In vivo characterization of oral pemphigus vulgaris by optical coherence tomography. J. Biol. Regul. Homeost. Agents 2015, 29, 39–41. [Google Scholar] [PubMed]
- Temelci, A.; Yılmaz, H.G.; Ünsal, G.; Uyanik, L.O.; Yazman, D.; Ayali, A.; Minervini, G. Investigation of the Wetting Properties of Thalassemia Patients’ Blood Samples on Grade 5 Titanium Implant Surfaces: A Pilot Study. Biomimimetics 2023, 8, 25. [Google Scholar] [CrossRef]
- Kuhn, F.P.; Spinner, G.; Del Grande, F.; Wyss, M.; Piccirelli, M.; Erni, S.; Pfister, P.; Ho, M.; Sah, B.-R.; Filli, L.; et al. MR imaging of the temporomandibular joint: Comparison between acquisitions at 7.0 T using dielectric pads and 3.0 T. Dentomaxillofac. Radiol. 2017, 46, 20160280. [Google Scholar] [CrossRef]
- Hannam, A.G.; Matthews, B.; Yemm, R. Receptors involved in the response of the masseter muscle to tooth contact in man. Arch. Oral Biol. 1970, 15, 17–24. [Google Scholar] [CrossRef]
- Gibbs, C.H.; Mahan, P.E.; Wilkinson, T.M.; Mauderli, A. EMG activity of the superior belly of the lateral pterygoid muscle in relation to other jaw muscles. J. Prosthet. Dent. 1984, 51, 691–702. [Google Scholar] [CrossRef]
- Gaudy, J.F.; Zouaoui, A.; Bri, P.; Charrier, J.L.; Laison, F. Functional anatomy of the human temporal muscle. Surg. Radiol. Anat. 2002, 23, 389–398. [Google Scholar] [CrossRef]
- Ferrario, V.F.; Serrao, G.; Dellavia, C.; Caruso, E.; Sforza, C. Relationship between the number of occlusal contacts and masticatory muscle activity in healthy young adults. CRANIO® 2002, 20, 91–98. [Google Scholar] [CrossRef]
- Felício, C.M.D.; Melchior, M.D.O.; Silva, M.A.M.R.D.; Celeghini, R.M.D.S. Masticatory performance in adults related to temporomandibular disorder and dental occlusion. Pró-Fono Rev. Atualização Cient. 2007, 19, 151–158. [Google Scholar] [CrossRef]
- Federici, E. Mandibular movements. Mondo Odontostomatol. 1979, 21, 33–49. [Google Scholar]
- Ballini, A.; Cantore, S.; Fotopoulou, E.A.; Georgakopoulos, I.P.; Athanasiou, E.; Bellos, D.; Paduanelli, G.; Saini, R.; Dipalma, G.; Inchingolo, F. Combined sea salt-based oral rinse with xylitol in orthodontic patients: Clinical and microbiological study. J. Biol. Regul. Homeost. Agents 2019, 33, 263–268. [Google Scholar]
- Khubchandani, S.R.; Bhoyar, A.; Sathe, S. Evaluation and Correlation of Bite Force with Electromyography (EMG) Activity Before and After Rehabilitation of the First Molar with an Implant-Supported Prosthesis. Cureus 2022, 14, e31085. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Inchingolo, A.D.; Cosola, M.D.; Inchingolo, A.M.; Lucchina, A.G.; Malcangi, G.; Pettini, F.; Scarano, A.; Bordea, I.R.; Hazballa, D.; Lorusso, F.; et al. Correlation between occlusal trauma and oral microbiota: A microbiological investigation. J. Biol. Regul. Homeost. Agents 2021, 35, 295–302. [Google Scholar] [CrossRef] [PubMed]
- Pasciuti, E.; Coloccia, G.; Inchingolo, A.D.; Patano, A.; Ceci, S.; Bordea, I.R.; Cardarelli, F.; Di Venere, D.; Inchingolo, F.; Dipalma, G. Deep Bite Treatment with Aligners: A New Protocol. Appl. Sci. 2022, 12, 6709. [Google Scholar] [CrossRef]
- Dworkin, S.F.; LeResche, L. Research diagnostic criteria for temporomandibular disorders: Review, criteria, examinations and specifications, critique. J. Orofac. Pain 1992, 6, 302–355. [Google Scholar]
- Ekberg, O.; Hillarp, B. Radiologic evaluation of the oral stage of swallowing. Acta Radiol. Diagn. 1986, 27, 533–537. [Google Scholar] [CrossRef]
- Ebadian, B.; Abbasi, M.; Nazarifar, A.M. Frequency distribution of temporomandibular disorders according to occlusal factors: A cross-sectional study. Dent. Res. J. 2020, 17, 186–192. [Google Scholar] [CrossRef]
- Dzingutė, A.; Pileičikienė, G.; Baltrušaitytė, A.; Skirbutis, G. Evaluation of the relationship between the occlusion parameters and symptoms of the temporomandibular joint disorder. Acta Medica Litu. 2017, 24, 167–175. [Google Scholar] [CrossRef]
- Davies, P.L. Electromyographic study of superficial neck muscles in mandibular function. J. Dent. Res. 1979, 58, 537–538. [Google Scholar] [CrossRef]
- Catapano, S.; Ferrari, M.; Mobilio, N.; Montanari, M.; Corsalini, M.; Grande, F. Comparative Analysis of the Stability of Prosthetic Screws under Cyclic Loading in Implant Prosthodontics: An In Vitro Study. Appl. Sci. 2021, 11, 622. [Google Scholar] [CrossRef]
- de Tommaso, M.; Lavolpe, V.; Di Venere, D.; Corsalini, M.; Vecchio, E.; Favia, G.; Sardaro, M.; Livrea, P.; Nolano, M. A case of unilateral burning mouth syndrome of neuropathic origin. Headache J. Head Face Pain 2011, 51, 441–443. [Google Scholar] [CrossRef] [PubMed]
- Grippaudo, C.; Cancellieri, D.; Grecolini, M.E.; Deli, R. Comparison between different interdental stripping methods and evaluation of abrasive strips: SEM analysis. Prog. Orthod. 2010, 11, 127–137. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, A.D.; Pezzolla, C.; Patano, A.; Ceci, S.; Ciocia, A.M.; Marinelli, G.; Malcangi, G.; Montenegro, V.; Cardarelli, F.; Piras, F.; et al. Experimental Analysis of the Use of Cranial Electromyography in Athletes and Clinical Implications. Int. J. Environ. Res. Public Health 2022, 19, 7975. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Inchingolo, F.; Patano, A.; Inchingolo, A.M.; Riccaldo, L.; Morolla, R.; Netti, A.; Azzollini, D.; Inchingolo, A.D.; Palermo, A.; Lucchese, A.; et al. Analysis of Mandibular Muscle Variations Following Condylar Fractures: A Systematic Review. J. Clin. Med. 2023, 12, 5925. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dipalma, G.; Inchingolo, A.D.; Inchingolo, A.M.; Piras, F.; Carpentiere, V.; Garofoli, G.; Azzollini, D.; Campanelli, M.; Paduanelli, G.; Palermo, A.; et al. Artificial Intelligence and Its Clinical Applications in Orthodontics: A Systematic Review. Diagnostics 2023, 13, 3677. [Google Scholar] [CrossRef]
- Dipalma, G.; Inchingolo, A.M.; Colonna, V.; Marotti, P.; Carone, C.; Ferrante, L.; Inchingolo, F.; Palermo, A.; Inchingolo, A.D. Autologous and Heterologous Minor and Major Bone Regeneration with Platelet-Derived Growth Factors. J. Funct. Biomater. 2025, 16, 16. [Google Scholar] [CrossRef]
- Compilato, D.; Cirillo, N.; Termine, N.; Kerr, A.R.; Paderni, C.; Ciavarella, D.; Campisi, G. Long-standing oral ulcers: Proposal for a new “S-C-D classification system”. J. Oral Pathol. Med. 2009, 38, 241–253. [Google Scholar] [CrossRef]
- Cianci, C.; Pappalettera, G.; Renna, G.; Casavola, C.; Laurenziello, M.; Battista, G.; Pappalettere, C.; Ciavarella, D. Mechanical Behavior of PET-G Tooth Aligners Under Cyclic Loading. Front. Mater. 2020, 7, 104. [Google Scholar] [CrossRef]
- Cassano, M.; Russo, G.; Granieri, C.; Ciavarella, D. Modification of growth, immunologic and feeding parameters in children with OSAS after adenotonsillectomy. Acta Otorhinolaryngol. Ital. 2018, 38, 124–130. [Google Scholar] [CrossRef]
- Muzio, L.L.; Santarelli, A.; Panzarella, V.; Campisi, G.; Carella, M.; Ciavarella, D.; Di Cosola, M.; Giannone, N.; Bascones, A. Oral squamous cell carcinoma and biological markers: An update on the molecules mainly involved in oral carcinogenesis. Minerva Stomatol. 2007, 56, 341–347. [Google Scholar]
- Tepedino, M.; Illuzzi, G.; Laurenziello, M.; Perillo, L.; Taurino, A.M.; Cassano, M.; Guida, L.; Burlon, G.; Ciavarella, D. Craniofacial morphology in patients with obstructive sleep apnea: Cephalometric evaluation. Braz. J. Otorhinolaryngol. 2022, 88, 228–234. [Google Scholar] [CrossRef]
- Ciavarella, D.; Parziale, V.; Mastrovincenzo, M.; Palazzo, A.; Sabatucci, A.; Suriano, M.M.; Bossù, M.; Cazzolla, A.P.; Muzio, L.L.; Chimenti, C. Condylar position indicator and T-scan system II in clinical evaluation of temporomandibular intracapsular disease. J. Cranio-Maxillofac. Surg. 2012, 40, 449–455. [Google Scholar] [CrossRef]
- Tepedino, M.; Iancu-Potrubacz, M.; Ciavarella, D.; Masedu, F.; Marchione, L.; Chimenti, C. Expansion of permanent first molars with rapid maxillary expansion appliance anchored on primary second molars. J. Clin. Exp. Dent. 2018, 10, e241–e247. [Google Scholar] [CrossRef] [PubMed]
- Mignogna, M.D.; Leuci, S.; Fedele, S.; Ruoppo, E.; Adamo, D.; Russo, G.; Pagliuca, R. Adjuvant high-dose intravenous immunoglobulin therapy can be easily and safely introduced as an alternative treatment in patients with severe pemphigus vulgaris: A retrospective preliminary study. Am. J. Clin. Dermatol. 2008, 9, 323–331. [Google Scholar] [CrossRef] [PubMed]
- Mignogna, M.D.; Fortuna, G.; Leuci, S.; Ruoppo, E.; Adamo, D.; Fedele, S. Analysis of thromboembolic risk related to high-dose intravenous immunoglobulin treatment: A preliminary clinical study of 10 patients with autoimmune mucocutaneous blistering diseases. Clin. Exp. Dermatol. 2009, 34, 145–150. [Google Scholar] [CrossRef]
- Adamo, D.; Spagnuolo, G. Burning Mouth Syndrome: An Overview and Future Perspectives. Int. J. Environ. Res. Public. Health 2022, 20, 682. [Google Scholar] [CrossRef]
- Meme’, L.; Bambini, F.; Dipalma, G.; Sampalmieri, F.; Laforgia, A.; Inchingolo, A.D.; Pennacchio, B.F.P.; Giorgio, R.V.; Corsalini, M.; Paduanelli, G.; et al. The key role of the palatal expander in orthodontics. Eur. J. Musculoskelet. Dis. 2024, 13, S175–S182. [Google Scholar]
- Minetti, E.; Dipalma, G.; Palermo, A.; Inchingolo, A.D.; Viapiano, F.; Inchingolo, A.M.; Inchingolo, F. The most suitable system to grind the whole tooth to use it as graft material. Explor. Med. 2024, 5, 1–16. [Google Scholar] [CrossRef]
- Inchingolo, F.; Inchingolo, A.D.; Latini, G.; Trilli, I.; Ferrante, L.; Nardelli, P.; Malcangi, G.; Inchingolo, A.M.; Mancini, A.; Palermo, A.; et al. The Role of Curcumin in Oral Health and Diseases: A Systematic Review. Antioxidants 2024, 13, 660. [Google Scholar] [CrossRef]
- Cerkezi, S.; Nakova, M.; Gorgoski, I.; Ferati, K.; Bexheti-Ferati, A.; Palermo, A.; Inchingolo, A.D.; Ferrante, L.; Inchingolo, A.M.; Inchingolo, F.; et al. The Role of Sulfhydryl (Thiols) Groups in Oral and Periodontal Diseases. Biomedicines 2024, 12, 882. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, A.D.; Laforgia, A.; Inchingolo, A.M.; Latini, G.; Pezzolla, C.; Nardelli, P.; Palermo, A.; Inchingolo, F.; Malcangi, G.; Dipalma, G. Rapid palate expansion’s impact on nasal breathing: A systematic review. Int. J. Pediatr. Otorhinolaryngol. 2025, 190, 112248. [Google Scholar] [CrossRef] [PubMed]
- Tatullo, M.; Marrelli, M.; Scacco, S.; Lorusso, M.; Doria, S.; Sabatini, R.; Auteri, P.; Cagiano, R.; Inchingolo, F. Relationship between oxidative stress and “burning mouth syndrome” in female patients: A scientific hypothesis. Eur. Rev. Med. Pharmacol. Sci. 2012, 16, 1218–1221. [Google Scholar] [PubMed]
- Minetti, E.; Palermo, A.; Savadori, P.; Patano, A.; Inchingolo, A.D.; Rapone, B.; Malcangi, G.; Inchingolo, F.; Dipalma, G.; Tartaglia, F.C.; et al. Socket Preservation Using Dentin Mixed with Xenograft Materials: A Pilot Study. Materials 2023, 16, 4945. [Google Scholar] [CrossRef]
- Inchingolo, A.M.; Inchingolo, A.D.; Nardelli, P.; Latini, G.; Trilli, I.; Ferrante, L.; Malcangi, G.; Palermo, A.; Inchingolo, F.; Dipalma, G. Stem Cells: Present Understanding and Prospects for Regenerative Dentistry. J. Funct. Biomater. 2024, 15, 308. [Google Scholar] [CrossRef]
- D’oria, V.; Bettocchi, S.; De Cosmi, V.; Paglia, M.; Colombo, S.; Scaglioni, S.; Agostoni, C.; Beretta, M.; Braiotta, F.; Berti, C.; et al. Risk factors for Early Childhood Caries in Italian preschoolers: A cross-sectional analysis. Eur. J. Paediatr. Dent. 2024, 25, 271–276. [Google Scholar] [CrossRef]
- Moscati, M.; Caruso, S.; De Felice, M.E.; Di Fabio, G.; Gatto, R.; Botticelli, G. Selective excavation and ozone therapy: New frontier of mini-invasive caries treatment in MIH paediatric patients. A case report. Eur. J. Paediatr. Dent. 2024, 25, 6–10. [Google Scholar] [CrossRef]
- Salerno, C.; Allam, A.; Cirio, S.; Malerba, A.; Ionescu, A.C.; Tartaglia, G.M.; Campus, G.; Cagetti, M.G. Survival of different caries managements in children with autism and unaffected peers: A retrospective cohort study. Eur. J. Paediatr. Dent. 2024, 25, 214–223. [Google Scholar] [CrossRef]
- Izzetti, R.; Giuca, M.R.; Lardani, L.; Nisi, M.; Carli, E. Treatment options of periapical cysts of deciduous teeth: Report of a case and systematic review of the literature. Eur. J. Paediatr. Dent. 2024, 25, 113–119. [Google Scholar] [CrossRef]
- Memè, L.; Quinzi, V.; Coli, G.; Caciari, E.; Sampalmieri, F.; Gallusi, G. Unconventional use of Invisalign® in the treatment of ectopic palatal maxillary canines. Eur. J. Paediatr. Dent. 2024, 25, 61–68. [Google Scholar] [CrossRef]
- Luigi, P. A lifelong smile: A journey that begins during pregnancy! Eur. J. Paediatr. Dent. 2024, 25, 89. [Google Scholar] [CrossRef]
- Vasakova, J.; Borovec, J.; Polackova, P.; Duskova, J. Are there any limits to the dental treatment of children? Eur. J. Paediatr. Dent. 2024, 25, 178–182. [Google Scholar] [CrossRef] [PubMed]
- Walia, T.; Shetty, R.M.; Osman, O.T.S. Attitude and Practices of Paediatric Dentists towards Parental Guidance on Dental Trauma. A cross-sectional survey. Eur. J. Paediatr. Dent. 2023, 25, 98–107. [Google Scholar] [CrossRef] [PubMed]
- Cenzato, N.; Cazzaniga, F.; Masserini, F.; Baldini, B.; Colombo, L.; Fumagalli, M.; Maspero, C. Comparison of facial features in fetuses and newborns following natural delivery with cephalic presentation: A pilot study. Eur. J. Paediatr. Dent. 2024, 25, 284–289. [Google Scholar] [CrossRef] [PubMed]
- Garrocho-Rangel, A.; Rosales-Bérber, M.; Ríos-Méndez, D.; Flores-Velázquez, J.; Trejo-Herbert, D.; Pozos-Guillén, F.; Pozos-Guillén, A. Dog-Assisted Therapy (DAT) for the management of anxiety during paediatric dental care. A scoping review. Eur. J. Paediatr. Dent. 2024, 25, 120–125. [Google Scholar] [CrossRef]
- Ortu, E.; Di Nicolantonio, S.; Severino, M.; Cova, S.; Pietropaoli, D.; Monaco, A. Effectiveness of elastodontic appliances in the treatment of malocclusions: A review of the literature. Eur. J. Paediatr. Dent. 2024, 25, 57–60. [Google Scholar] [CrossRef]
- Bayrak, G.D.; Yaman-Dosdogru, E.; Selvi-Kuvvetli, S. Effects of maternal anxiety and sociodemographic factors on fluoride knowledge and opinions about fluoride-containing oral products. A cross-sectional study. Eur. J. Paediatr. Dent. 2024, 25, 50–56. [Google Scholar] [CrossRef]
- Cots, E.; Casas, M.; Gregoriano, M.; Busquet-Dura, X.; Bielsa, J.; Chacon, C.; Kragt, L.; Torán, P.; Guinot, F. Ethnic disparities in the prevalence of Molar-Incisor-Hypomineralisation (MIH) and caries among 6-12-year-old children in Catalonia, Spain. Eur. J. Paediatr. Dent. 2024, 25, 188–199. [Google Scholar] [CrossRef]
- Aktaş, N.; Atabek, D. Fracture Resistance of Space Maintainers Produced Using 3D Printable Materials. Eur. J. Paediatr. Dent. 2024, 25, 266–270. [Google Scholar] [CrossRef]
- Zerman, N.; Zangani, A.; Maffeis, C.; Pietrobelli, A.; Piacentini, G.; Zotti, F.; De Manzoni, R.; Silva, R.; Cordiano, A.; Spinas, E.; et al. Interdisciplinary management of orofacial lesions in early childhood: Paediatric alert system at University of Verona. Eur. J. Paediatr. Dent. 2024, 25, 149–154. [Google Scholar] [CrossRef]
- Spinas, E.; Carboni, L.; Mallus, T.; Zerman, N. Intrusive Luxation Injuries in deciduous teeth: Literature Review and Treatment Complications Update. Eur. J. Paediatr. Dent. 2024, 25, 77–80. [Google Scholar] [CrossRef]
- Rosa, M.; Manti, G.; Lucchi, P.; Mutinelli, S. Nasal bone modification compared to normal growth after rapid maxillary expansion anchored onto deciduous teeth: A CBCT retrospective study. Eur. J. Paediatr. Dent. 2024, 25, 310–317. [Google Scholar] [CrossRef]
- Signoriello, A.G.; Stellini, E.; Bertolini, R.; Pezzato, L.; Positello, P.; Gracco, A.; Mazzoleni, S.; Ludovichetti, F.S. Paedodontic preformed crowns in primary teeth and relative degree of dental wear. Eur. J. Paediatr. Dent. 2025, 26, 19–23. [Google Scholar] [CrossRef]
- Cenzato, N.; Crispino, R.; Galbiati, G.; Giannini, L.; Bolognesi, L.; Lanteri, V.; Maspero, C. Premature loss of primary molars in children: Space recovery through molar distalisation. A literature review. Eur. J. Paediatr. Dent. 2024, 25, 72–76. [Google Scholar] [CrossRef]
- Giuca, M.R. Rare diseases: A challenge in paediatric dentistry. Eur. J. Paediatr. Dent. 2024, 25, 171. [Google Scholar] [CrossRef]


| Table Analyzed | Occlusal Test POC MASS | |||
| Column B | POC MASS OCCH. | |||
| VS. | VS. | |||
| Column A | POC MASS | |||
| Paired t test | ||||
| p value | 0.0042 | |||
| p value summary | ** | |||
| Significantly different (p < 0.05)? | Yes | |||
| One- or two-tailed p value? | Two-tailed | |||
| t, df | t = 3.810, df = 9 | |||
| Number of pairs | 10 | |||
| How big is the difference? | ||||
| Mean of differences (B-A) | 5.064 | |||
| SD of differences | 4.203 | |||
| SEM of differences | 1.329 | |||
| 95% confidence interval | 2.057 to 8.071 | |||
| R squared (partial eta squared) | 0.6173 | |||
| How effective was the pairing? | ||||
| Correlation coefficient (r) | 0.9501 | |||
| p value (one tailed) | <0.0001 | |||
| p value summary | **** | |||
| Was the pairing significantly effective? | Yes | |||
| Normality of Residuals | ||||
| Test name | Statistics | p value | Passed normality test | p value summary |
| Anderson–Darling (A2 *) | 0.6024 | 0.0844 | Yes | ns |
| D’Agostino–Pearson omnibus (K2) | 6.806 | 0.0333 | No | * |
| Shapiro–Wilk (W) | 0.8501 | 0.0583 | Yes | ns |
| Kolmogorov–Smirnov (distance) | 0.2222 | >0.1000 | Yes | ns |
| POC MASS | POC MASS OCCH. | POC MASS OCCH.—POC MASS | ||
| Number of values | 10 | 10 | 10 | |
| Minimum | 49.57 | 51.53 | 1.03 | |
| 25% Percentile | 61.77 | 69.05 | 1.843 | |
| Median | 75.56 | 80.78 | 3.835 | |
| 75% Percentile | 82.37 | 85.41 | 8.018 | |
| Maximum | 85.41 | 87.05 | 14.69 | |
| Mean | 71.74 | 76.8 | 5.064 | |
| Std. Deviation | 13.12 | 11.52 | 4.203 | |
| Std. Error of Mean | 4.15 | 3.642 | 1.329 | |
| Lower 95% CI | 62.35 | 68.56 | 2.057 | |
| Upper 95% CI | 81.12 | 85.04 | 8.071 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Crincoli, V.; Inchingolo, A.D.; Marinelli, G.; Lagioia, R.; Bassi, P.; Ciocia, C.; Calò, F.; Deodato, R.; Marsella, G.; Inchingolo, F.; et al. Evaluation of the Possible Correlation Between Dental Occlusion and Craniomandibular Disorders by Means of Teethan® Electromyography: Clinical-Observational Study on 20 Patients. J. Clin. Med. 2025, 14, 5508. https://doi.org/10.3390/jcm14155508
Crincoli V, Inchingolo AD, Marinelli G, Lagioia R, Bassi P, Ciocia C, Calò F, Deodato R, Marsella G, Inchingolo F, et al. Evaluation of the Possible Correlation Between Dental Occlusion and Craniomandibular Disorders by Means of Teethan® Electromyography: Clinical-Observational Study on 20 Patients. Journal of Clinical Medicine. 2025; 14(15):5508. https://doi.org/10.3390/jcm14155508
Chicago/Turabian StyleCrincoli, Vito, Alessio Danilo Inchingolo, Grazia Marinelli, Rosalba Lagioia, Paola Bassi, Claudia Ciocia, Francesca Calò, Roberta Deodato, Giulia Marsella, Francesco Inchingolo, and et al. 2025. "Evaluation of the Possible Correlation Between Dental Occlusion and Craniomandibular Disorders by Means of Teethan® Electromyography: Clinical-Observational Study on 20 Patients" Journal of Clinical Medicine 14, no. 15: 5508. https://doi.org/10.3390/jcm14155508
APA StyleCrincoli, V., Inchingolo, A. D., Marinelli, G., Lagioia, R., Bassi, P., Ciocia, C., Calò, F., Deodato, R., Marsella, G., Inchingolo, F., Palermo, A., Dioguardi, M., Cazzolla, A. P., Di Comite, M. S., Piancino, M. G., Inchingolo, A. M., & Dipalma, G. (2025). Evaluation of the Possible Correlation Between Dental Occlusion and Craniomandibular Disorders by Means of Teethan® Electromyography: Clinical-Observational Study on 20 Patients. Journal of Clinical Medicine, 14(15), 5508. https://doi.org/10.3390/jcm14155508












