Digital Orthodontic Setups in Orthognathic Surgery: Evaluating Predictability and Precision of the Workflow in Surgical Planning
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Data Acquisition
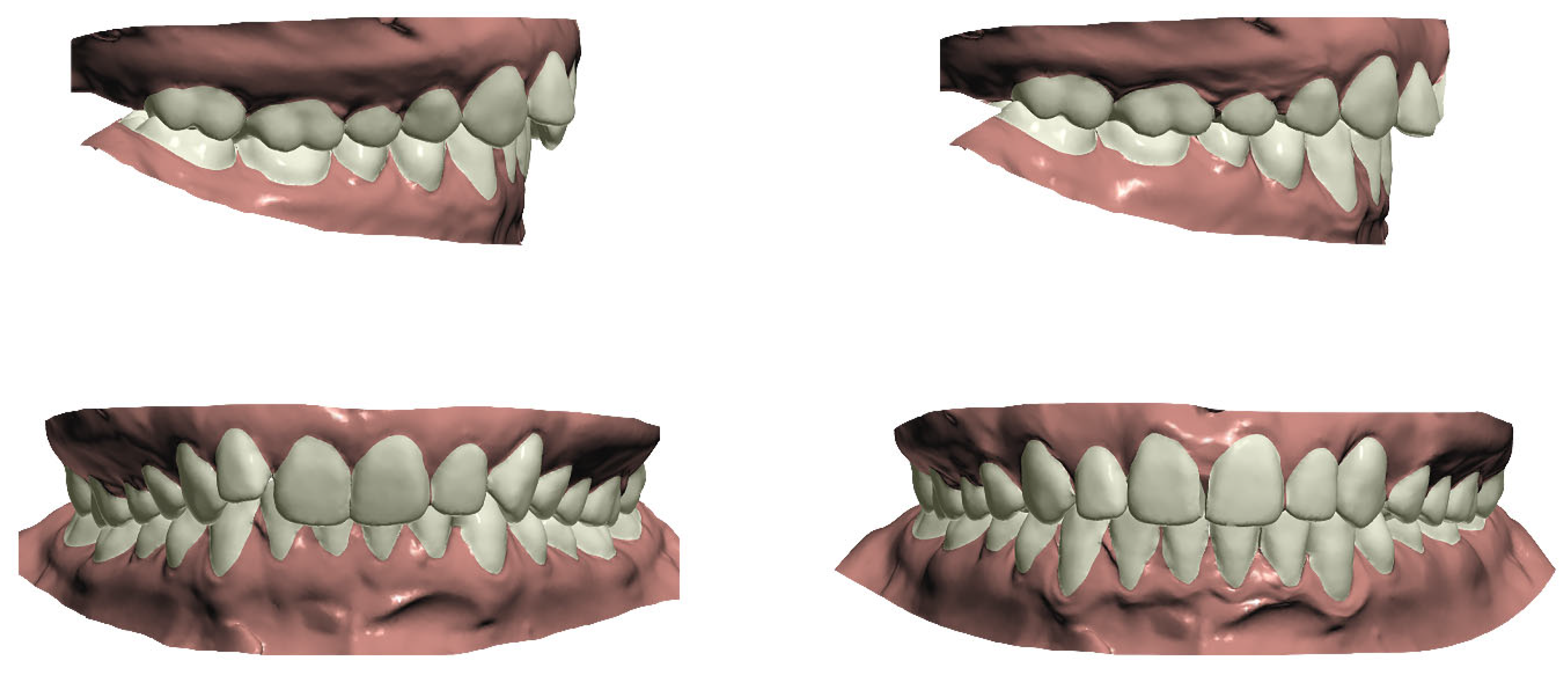
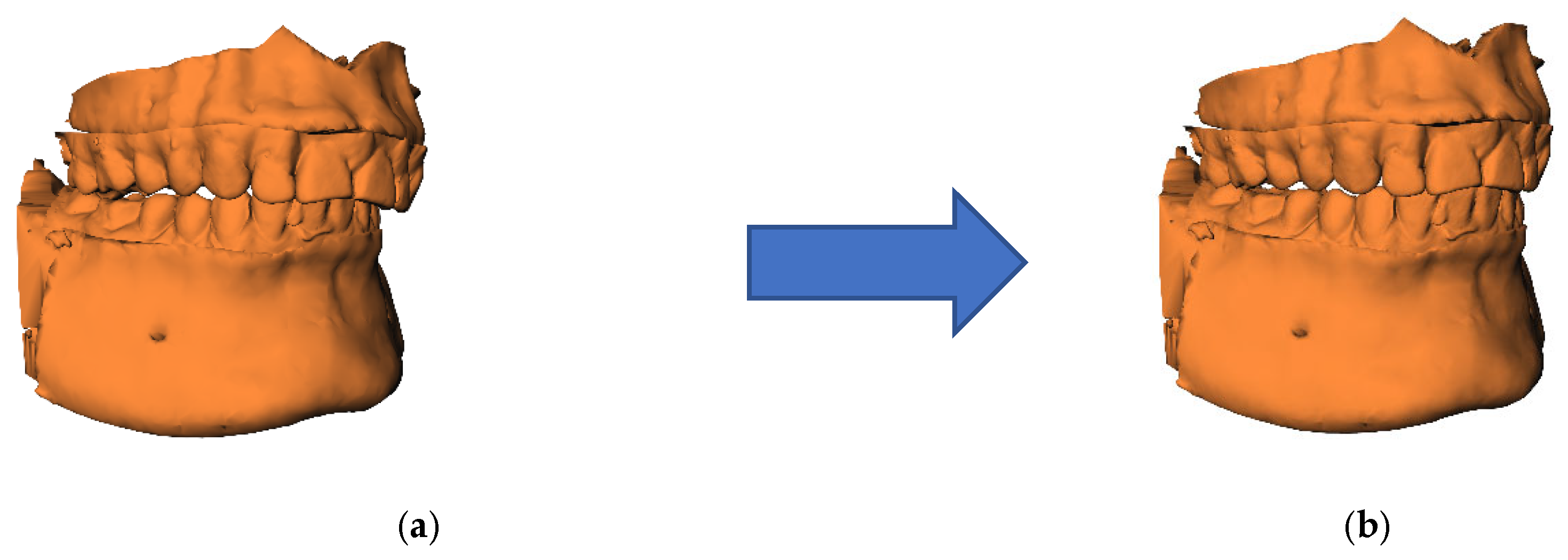
2.3. Orthodontic Setup Production
2.4. Surgical Planning
2.5. Measuring Differences Between Pretreatment and Presurgical Orthognathic Surgical Planning
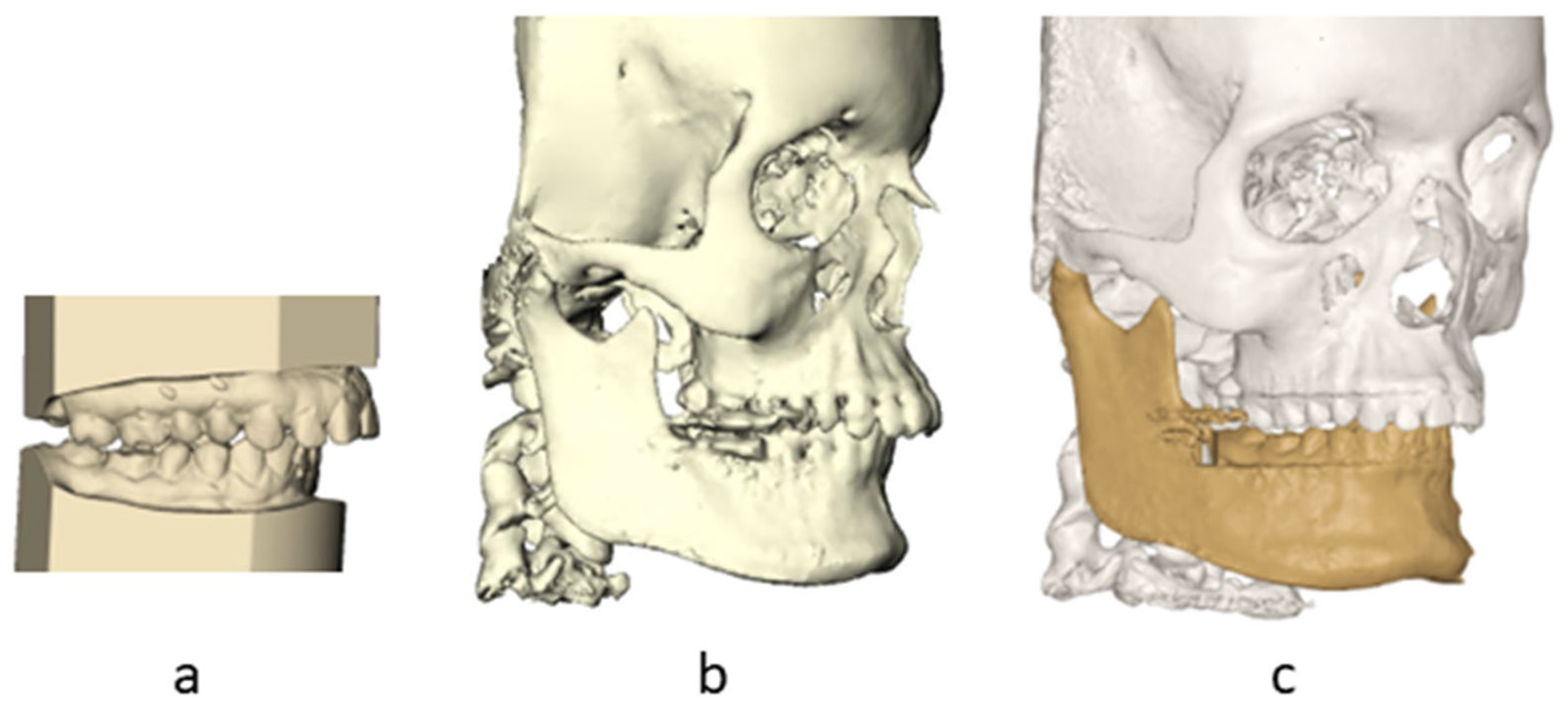
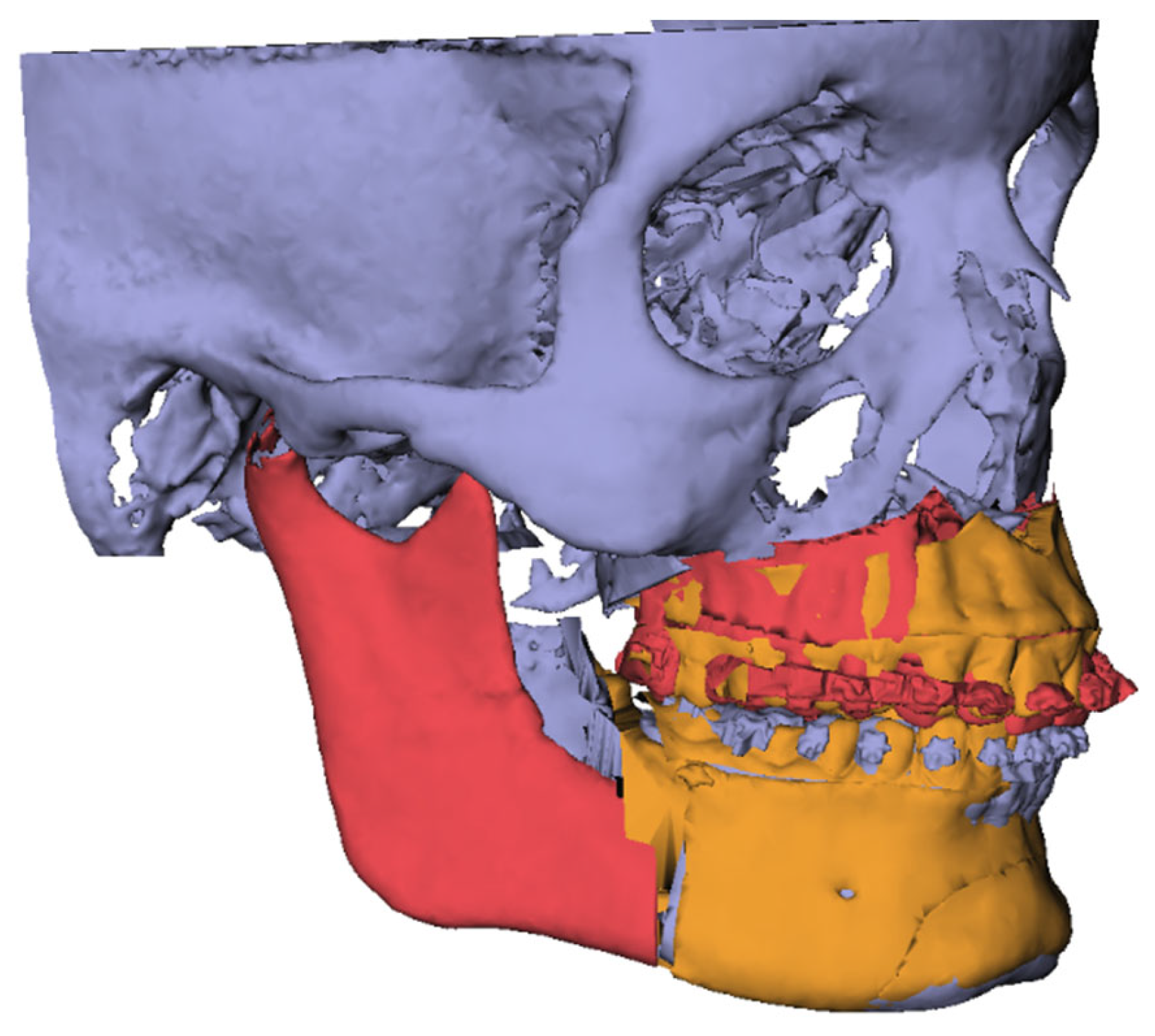
2.5.1. Step 1: Incorporation of Orthodontic Setup with CBCT T0
2.5.2. Step 2: Registration of CBCT T0 Towards Surgery Planning
2.5.3. Step 3: Orthognathic Planning of T0 Model
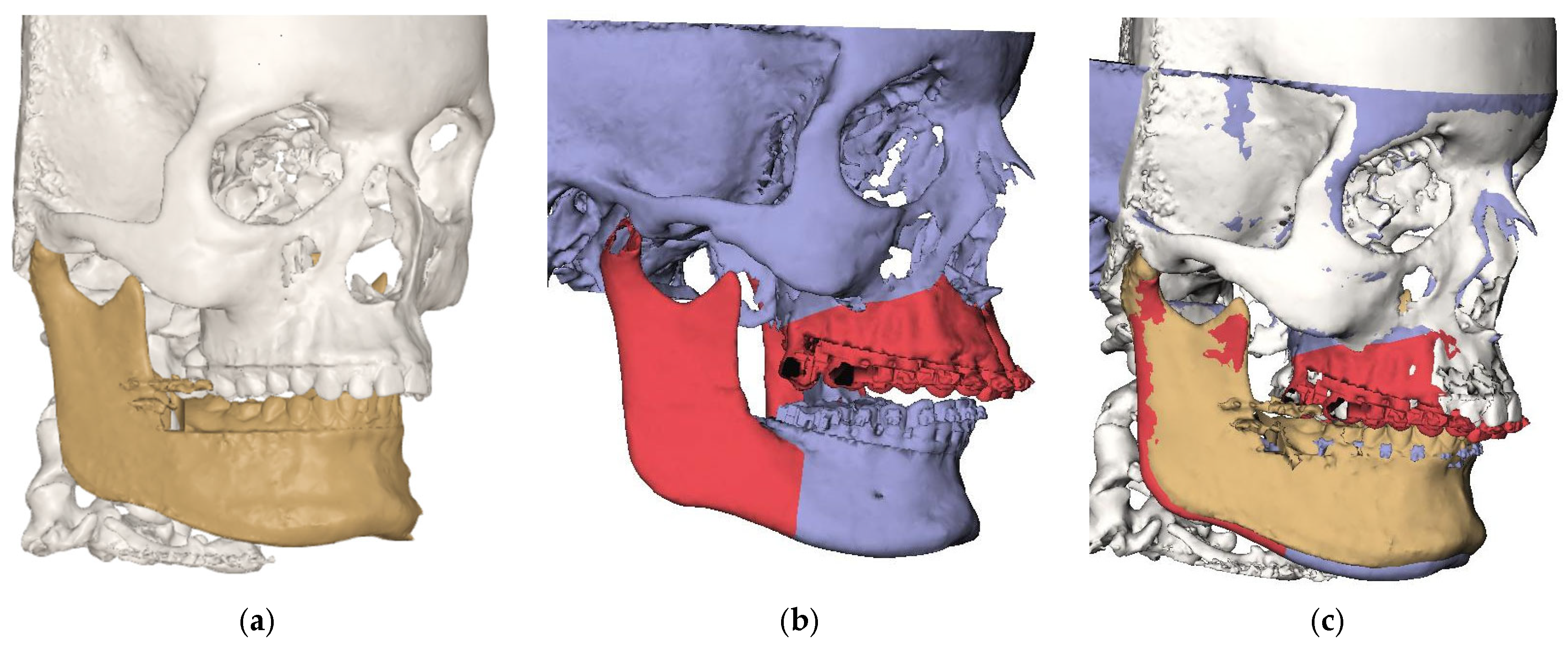
2.5.4. Step 4: Registration of Osteotomized Segments
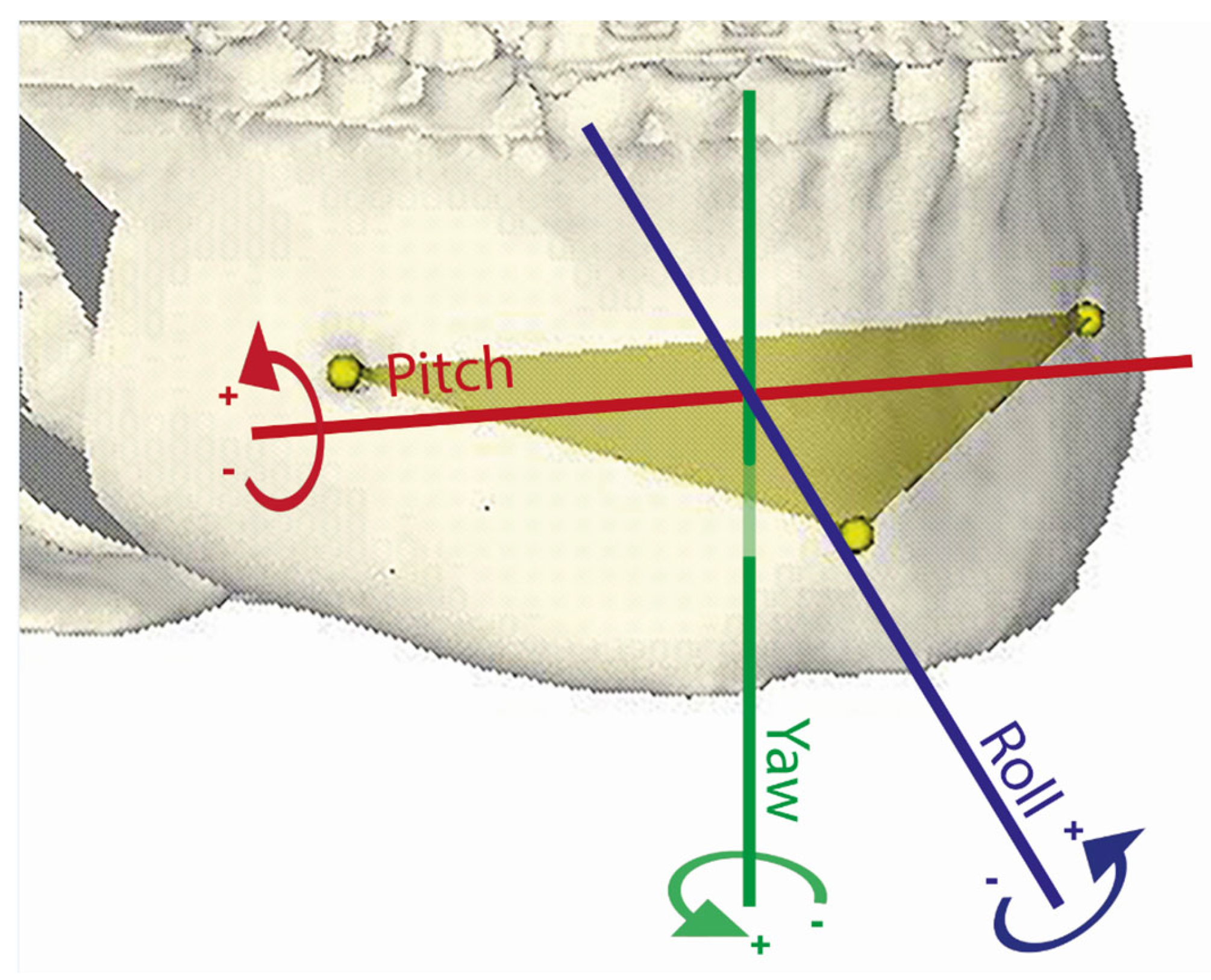
2.5.5. Step 5: Construction of Virtual Triangles
2.5.6. Step 6: Calculation of Rotational and Translational Movements
2.6. Statistical Analyses
3. Results
3.1. T0 Planning Accuracy
3.2. Effect of SARME and Extraction on the Results
4. Discussion
4.1. Interpretation of the Study Results
4.2. Clinical Relevance
4.3. Limitations in Study Design
5. Conclusions
- The accuracy of the presented orthognathic surgical planning workflow prior to orthodontic intervention is limited at the dental level, particularly regarding the torque of the maxillary anterior teeth.
- No significant differences were observed between pretreatment planning and actual orthodontic planning at the level of the bony mandible; however, a noteworthy proportion of rotational and translational discrepancies exceeded clinically acceptable thresholds.
- Although the proposed method demonstrates potential as a simulation tool for predicting mandibular bony outcomes at the start of treatment, the current accuracy is insufficient for reliable routine clinical use. Further refinement and validation in larger, more homogeneous patient groups are necessary to improve its clinical applicability.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CBCT | Cone Beam Computed Tomography |
| 3D | Three-Dimensional |
| STL | Standard Tessellation Language |
| DICOM | Digital Imaging and Communications in Medicine |
| VBM | Voxel-based matching |
| SARME | Surgically Assisted Maxillary Expansion |
| UD | Upward Downward |
| LR | Left Right |
| AP | Anterior Posterior |
References
- Larson, B.E. Orthodontic preparation for orthognathic surgery. Oral Maxillofac. Surg. Clin. N. Am. 2014, 26, 441–458. [Google Scholar] [CrossRef] [PubMed]
- Klein, K.P.; Kaban, L.B.; Masoud, M.I. Orthognathic Surgery and Orthodontics: Inadequate Planning Leading to Complications or Unfavorable Results. Oral Maxillofac. Surg. Clin. N. Am. 2020, 32, 71–82. [Google Scholar] [CrossRef] [PubMed]
- Edler, R.J. Problems in the orthodontic management of orthognathic cases. Eur. J. Orthod. 1990, 12, 420–437. [Google Scholar] [CrossRef] [PubMed]
- Quast, A.; Santander, P.; Leding, J.; Klenke, D.; Moser, N.; Schliephake, H.; Meyer-Marcotty, P. Orthodontic incisor decompensation in orthognathic therapy-success and efficiency in three dimensions. Clin. Oral Investig. 2021, 25, 4001–4010. [Google Scholar] [CrossRef]
- Jacobs, J.D.; Sinclair, P.M. Principles of orthodontic mechanics in orthognathic surgery cases. Am. J. Orthod. 1983, 84, 399–407. [Google Scholar] [CrossRef]
- Ravi, M.S.; Shetty, N.K.; Prasad, R.B. Orthodontics-surgical combination therapy for Class III skeletal malocclusion. Contemp. Clin. Dent. 2012, 3, 78–82. [Google Scholar] [CrossRef]
- Liou, E.J.; Chen, P.H.; Wang, Y.C.; Yu, C.C.; Huang, C.S.; Chen, Y.R. Surgery-first accelerated orthognathic surgery: Orthodontic guidelines and setup for model surgery. J. Oral Maxillofac. Surg. 2011, 69, 771–780. [Google Scholar] [CrossRef]
- Yang, L.; Xiao, Y.D.; Liang, Y.J.; Wang, X.; Li, J.Y.; Liao, G.Q. Does the Surgery-First Approach Produce Better Outcomes in Orthognathic Surgery? A Systematic Review and Meta-Analysis. J. Oral Maxillofac. Surg. 2017, 75, 2422–2429. [Google Scholar] [CrossRef]
- Karatas, O.H.; Toy, E. Three-dimensional imaging techniques: A literature review. Eur. J. Dent. 2014, 8, 132–140. [Google Scholar] [CrossRef]
- Cen, Y.; Huang, X.; Liu, J.; Qin, Y.; Wu, X.; Ye, S.; Du, S.; Liao, W. Application of three-dimensional reconstruction technology in dentistry: A narrative review. BMC Oral Health 2023, 23, 630. [Google Scholar] [CrossRef]
- Alkhayer, A.; Piffko, J.; Lippold, C.; Segatto, E. Accuracy of virtual planning in orthognathic surgery: A systematic review. Head Face Med. 2020, 16, 34. [Google Scholar] [CrossRef]
- Barreto, M.S.; Faber, J.; Vogel, C.J.; Araujo, T.M. Reliability of digital orthodontic setups. Angle Orthod. 2016, 86, 255–259. [Google Scholar] [CrossRef]
- Sereewisai, B.; Chintavalakorn, R.; Santiwong, P.; Nakornnoi, T.; Neoh, S.P.; Sipiyaruk, K. The accuracy of virtual setup in simulating treatment outcomes in orthodontic practice: A systematic review. BDJ Open 2023, 9, 41. [Google Scholar] [CrossRef]
- Luther, F.; Morris, D.O.; Hart, C. Orthodontic preparation for orthognathic surgery: How long does it take and why? A retrospective study. Br. J. Oral Maxillofac. Surg. 2003, 41, 401–406. [Google Scholar] [CrossRef] [PubMed]
- Bonanthaya, K.; Anantanarayanan, P. Unfavourable outcomes in orthognathic surgery. Indian J. Plast. Surg. 2013, 46, 183–193. [Google Scholar] [CrossRef]
- Cunningham, S.J.; Hunt, N.P.; Feinmann, C. Perceptions of outcome following orthognathic surgery. Br. J. Oral Maxillofac. Surg. 1996, 34, 210–213. [Google Scholar] [CrossRef]
- de Waard, O.; Bruggink, R.; Baan, F.; Reukers, H.A.J.; Bronkhorst, E.M.; Kuijpers-Jagtman, A.M.; Ongkosuwito, E.M. Operator Performance of the Digital Setup Fabrication for Orthodontic-Orthognathic Treatment: An Explorative Study. J. Clin. Med. 2021, 11, 145. [Google Scholar] [CrossRef]
- Fabels, L.N.; Nijkamp, P.G. Interexaminer and intraexaminer reliabilities of 3-dimensional orthodontic digital setups. Am. J. Orthod. Dentofac. Orthop. 2014, 146, 806–811. [Google Scholar] [CrossRef]
- Swennen, G.R.; Mollemans, W.; De Clercq, C.; Abeloos, J.; Lamoral, P.; Lippens, F.; Neyt, N.; Casselman, J.; Schutyser, F. A cone-beam computed tomography triple scan procedure to obtain a three-dimensional augmented virtual skull model appropriate for orthognathic surgery planning. J. Craniofacial Surg. 2009, 20, 297–307. [Google Scholar] [CrossRef]
- Baan, F.; Bruggink, R.; Nijsink, J.; Maal, T.J.J.; Ongkosuwito, E.M. Fusion of intra-oral scans in cone-beam computed tomography scans. Clin. Oral Investig. 2021, 25, 77–85. [Google Scholar] [CrossRef]
- Nadjmi, N.; Mollemans, W.; Daelemans, A.; Van Hemelen, G.; Schutyser, F.; Berge, S. Virtual occlusion in planning orthognathic surgical procedures. Int. J. Oral Maxillofac. Surg. 2010, 39, 457–462. [Google Scholar] [CrossRef] [PubMed]
- Papageorgiou, S.N.; Cassina, C.; Vandevska-Radunovic, V.; Eliades, T. Incisor and profile alterations in extraction cases treated with standard Edgewise and pre-adjusted appliances: A controlled before-and-after study. J. World Fed. Orthod. 2021, 10, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Elias, K.G.; Sivamurthy, G.; Bearn, D.R. Extraction vs. nonextraction orthodontic treatment: A systematic review and meta-analysis. Angle Orthod. 2024, 94, 83–106. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.H.; Li, C.; Wong, H.; Chamberland, S.; Le, A.D.; Chung, C.H. Asymmetric Maxillary Expansion Introduced by Surgically Assisted Rapid Palatal Expansion: A Systematic Review. J. Oral Maxillofac. Surg. 2022, 80, 1902–1911. [Google Scholar] [CrossRef]
- Baan, F.; Liebregts, J.; Xi, T.; Schreurs, R.; de Koning, M.; Berge, S.; Maal, T. A New 3D Tool for Assessing the Accuracy of Bimaxillary Surgery: The OrthoGnathicAnalyser. PLoS ONE 2016, 11, e0149625. [Google Scholar] [CrossRef]
- Chen, Z.; Mo, S.; Fan, X.; You, Y.; Ye, G.; Zhou, N. A Meta-analysis and Systematic Review Comparing the Effectiveness of Traditional and Virtual Surgical Planning for Orthognathic Surgery: Based on Randomized Clinical Trials. J. Oral Maxillofac. Surg. 2021, 79, 471.e1–471.e19. [Google Scholar] [CrossRef]
- Baan, F.; de Waard, O.; Bruggink, R.; Xi, T.; Ongkosuwito, E.M.; Maal, T.J.J. Virtual setup in orthodontics: Planning and evaluation. Clin. Oral Investig. 2020, 24, 2385–2393. [Google Scholar] [CrossRef]


| Mean Differences | SEM | Top 10% Value | 95% CI | p-Value | ||
|---|---|---|---|---|---|---|
| Dental maxilla | ||||||
| Pitch a | −2.85 | 0.68 | 7.47 | −4.25 | −1.44 | <0.001 |
| Roll b | 0.05 | 0.21 | 1.47 | −0.39 | 0.49 | 0.804 |
| Yaw c | −0.54 | 0.33 | 2.19 | −1.23 | 0.14 | 0.114 |
| X (LR) d | 0.34 | 0.21 | 1.75 | −0.10 | 0.79 | 0.120 |
| Y (AP) e | −0.74 | 0.54 | 4.44 | −1.84 | 0.37 | 0.181 |
| Z (UD) f | −0.82 | 0.41 | 2.89 | −0.03 | 1.67 | 0.059 |
| Dental mandible | ||||||
| Pitch | −1.63 | 1.30 | 9.75 | −4.31 | 1.05 | 0.222 |
| Roll | 0.51 | 0.72 | 5.51 | −0.98 | 2.00 | 0.485 |
| Yaw | −1.52 | 0.92 | 7.54 | −3.41 | 0.38 | 0.111 |
| X (LR) | 1.19 | 0.51 | 4.49 | 0.15 | 2.24 | 0.027 |
| Y (AP) | 0.72 | 0.45 | 3.70 | −0.21 | 1.64 | 0.124 |
| Z (UD) | 0.02 | 0.51 | 3.88 | −1.03 | 1.07 | 0.970 |
| Bony mandible | ||||||
| Pitch | −0.41 | 0.71 | 5.88 | −1.87 | 1.05 | 0.566 |
| Roll | 0.31 | 0.39 | 2.56 | −0.49 | 1.11 | 0.430 |
| Yaw | −1.21 | 0.49 | 5.06 | −2.23 | −0.20 | 0.121 |
| X (LR) | 0.76 | 0.37 | 3.45 | 0.00 | 1.52 | 0.052 |
| Y (AP) | 0.12 | 0.28 | 2.38 | −0.46 | 0.70 | 0.674 |
| Z (UD) | 0.08 | 0.27 | 1.99 | −0.48 | 0.63 | 0.777 |
| Percentage out of Range (%) | |||
|---|---|---|---|
| Parameter | Dental Maxilla | Dental Mandible | Bony Mandible |
| Pitch | 42.31 | 57.69 | 26.92 |
| Roll | 0.00 | 15.38 | 3.85 |
| Yaw | 3.85 | 26.92 | 15.38 |
| Mean rotations | 15.39 | 33.33 | 15.38 |
| Trans LR | 11.54 | 50.00 | 26.92 |
| Trans FB | 23.08 | 50.00 | 15.38 |
| Trans UD | 30.77 | 34.62 | 11.54 |
| Mean translations | 21.80 | 44.87 | 17.95 |
| Dental Maxilla | Dental Mandible | Bony Mandible | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Parameter | Mean Diff | p | 95% CI | Mean Diff | p | 95% CI | Mean Diff | p | 95% CI | |||
| Effect of SARME (n = 15) | ||||||||||||
| Pitch | −2.39 | 0.084 | −5.13 | 0.35 | −3.15 | 0.247 | −8.62 | 2.34 | −1.33 | 0.358 | −4.27 | 1.62 |
| Roll | −0.10 | 0.826 | −0.99 | 0.80 | 2.23 | 0.100 | −0.46 | 4.92 | 1.58 | 0.028 | 0.18 | 2.98 |
| Yaw | 0.72 | 0.311 | −0.73 | 2.18 | −2.08 | 0.280 | −5.98 | 1.82 | −1.35 | 0.199 | −3.46 | 0.77 |
| Trans LR | −0.39 | 0.381 | −1.30 | 0.52 | 0.89 | 0.378 | −1.16 | 2.94 | 0.97 | 0.191 | −0.52 | 2.47 |
| Trans FB | −0.02 | 0.980 | −2.10 | 2.05 | 0.43 | 0.630 | −1.38 | 2.23 | 0.46 | 0.413 | −0.68 | 1.59 |
| Trans UD | −0.20 | 0.798 | −1.81 | 1.41 | 0.17 | 0.866 | −1.89 | 2.23 | 0.62 | 0.263 | −0.50 | 1.73 |
| Effect extraction in the maxilla (n = 4) | ||||||||||||
| Pitch | −8.30 | 0.020 | −14.71 | −1.89 | −1.98 | 0.409 | −8.02 | 4.06 | −3.57 | 0.038 | −6.88 | −0.27 |
| Roll | −0.23 | 0.543 | −1.05 | 0.59 | −2.69 | 0.164 | −6.94 | 1.55 | −1.29 | 0.110 | −2.96 | 0.37 |
| Yaw | 0.27 | 0.760 | −1.96 | 2.51 | −0.24 | 0.852 | −2.93 | 2.44 | −0.54 | 0.464 | −2.07 | 0.98 |
| Trans LR | 0.13 | 0.763 | −0.89 | 1.16 | 0.37 | 0.678 | −1.58 | 2.32 | −0.11 | 0.871 | −1.63 | 1.40 |
| Trans FB | −0.29 | 0.845 | −3.94 | 3.37 | −0.20 | 0.809 | −1.99 | 1.59 | −0.19 | 0.729 | −1.45 | 1.07 |
| Trans UD | 0.32 | 0.733 | −1.87 | 2.51 | −0.18 | 0.897 | −3.70 | 3.34 | −0.15 | 0.813 | −1.67 | 1.37 |
| Effect extraction in the mandible (n = 13) | ||||||||||||
| Pitch | −0.480 | 0.733 | −3.364 | 2.404 | −1.18 | 0.501 | −4.79 | 2.41 | −1.97 | 0.168 | −4.84 | 0.89 |
| Roll | −0.453 | 0.297 | −1.331 | 0.425 | −0.65 | 0.412 | −2.24 | 0.95 | −0.05 | 0.947 | −1.70 | 1.59 |
| Yaw | 0.356 | 0.604 | −1.046 | 1.758 | −1.12 | 0.300 | −3.32 | 1.07 | −1.61 | 0.103 | −3.57 | 0.35 |
| Trans LR | −0.628 | 0.146 | −1.491 | 0.235 | −0.20 | 0.846 | −2.34 | 1.94 | 0.16 | 0.834 | −1.40 | 1.71 |
| Trans FB | −1.053 | 0.339 | −3.308 | 1.202 | −0.29 | 0.754 | −2.18 | 1.60 | −0.26 | 0.659 | −1.44 | 0.93 |
| Trans UD | −0.122 | 0.886 | −1.878 | 1.634 | −1.51 | 0.141 | −3.56 | 0.54 | −0.20 | 0.717 | −1.35 | 0.94 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Waard, O.d.; Baan, F.; Bruggink, R.; Bronkhorst, E.M.; Kuijpers-Jagtman, A.M.; Ongkosuwito, E.M. Digital Orthodontic Setups in Orthognathic Surgery: Evaluating Predictability and Precision of the Workflow in Surgical Planning. J. Clin. Med. 2025, 14, 5270. https://doi.org/10.3390/jcm14155270
Waard Od, Baan F, Bruggink R, Bronkhorst EM, Kuijpers-Jagtman AM, Ongkosuwito EM. Digital Orthodontic Setups in Orthognathic Surgery: Evaluating Predictability and Precision of the Workflow in Surgical Planning. Journal of Clinical Medicine. 2025; 14(15):5270. https://doi.org/10.3390/jcm14155270
Chicago/Turabian StyleWaard, Olivier de, Frank Baan, Robin Bruggink, Ewald M. Bronkhorst, Anne Marie Kuijpers-Jagtman, and Edwin M. Ongkosuwito. 2025. "Digital Orthodontic Setups in Orthognathic Surgery: Evaluating Predictability and Precision of the Workflow in Surgical Planning" Journal of Clinical Medicine 14, no. 15: 5270. https://doi.org/10.3390/jcm14155270
APA StyleWaard, O. d., Baan, F., Bruggink, R., Bronkhorst, E. M., Kuijpers-Jagtman, A. M., & Ongkosuwito, E. M. (2025). Digital Orthodontic Setups in Orthognathic Surgery: Evaluating Predictability and Precision of the Workflow in Surgical Planning. Journal of Clinical Medicine, 14(15), 5270. https://doi.org/10.3390/jcm14155270










