Night-Time Bracing Can Reduce Pain in Adults with Scoliosis: Six-Month Results of a Retrospective Controlled Study
Abstract
1. Introduction
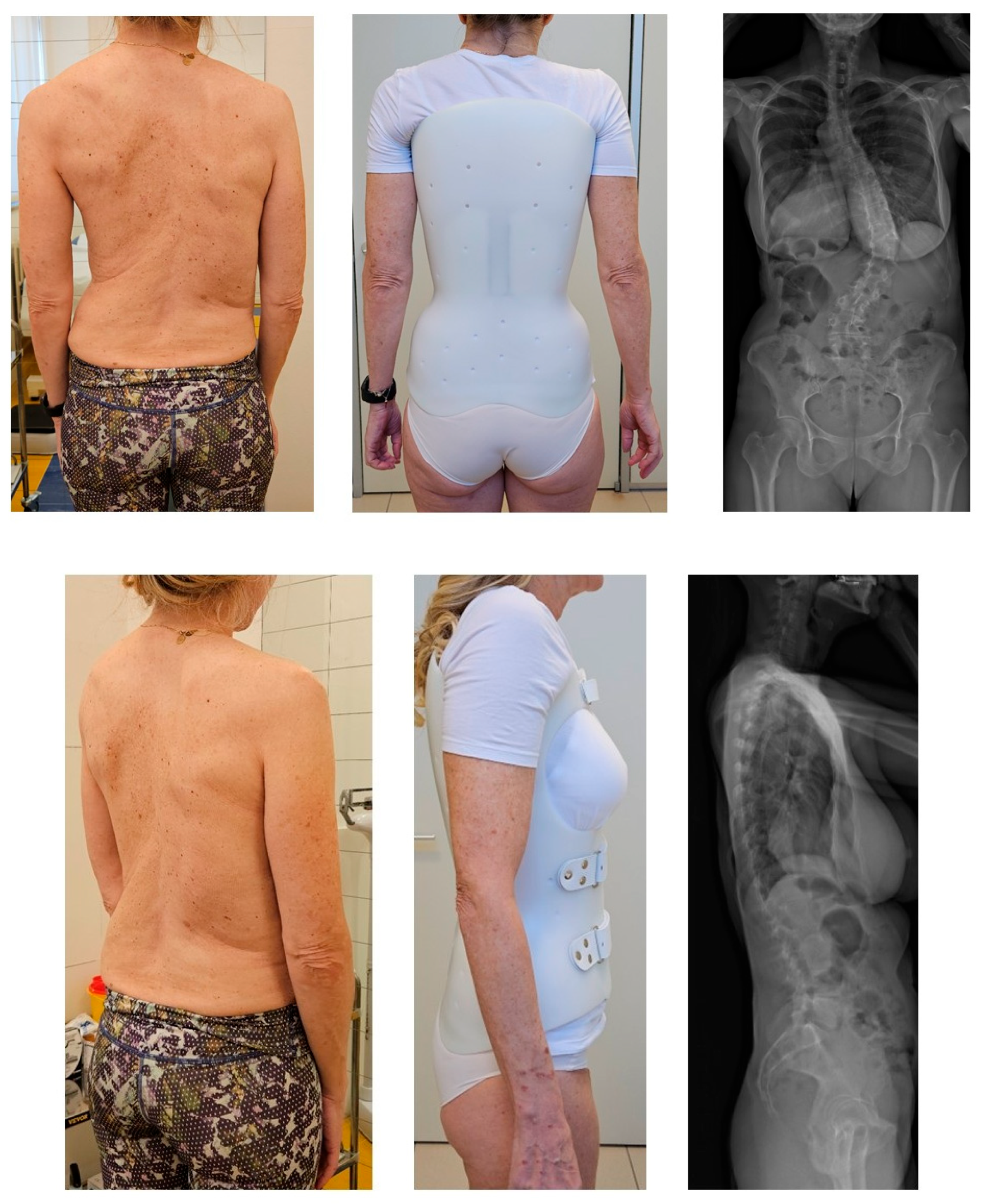
2. Materials and Methods
2.1. Design
2.2. Participants
2.3. Outcome Measures
2.4. Sample Size Calculations
2.5. Protocol
2.6. Statistical Analysis
2.7. Ethical Committee Approval
3. Results
3.1. Population
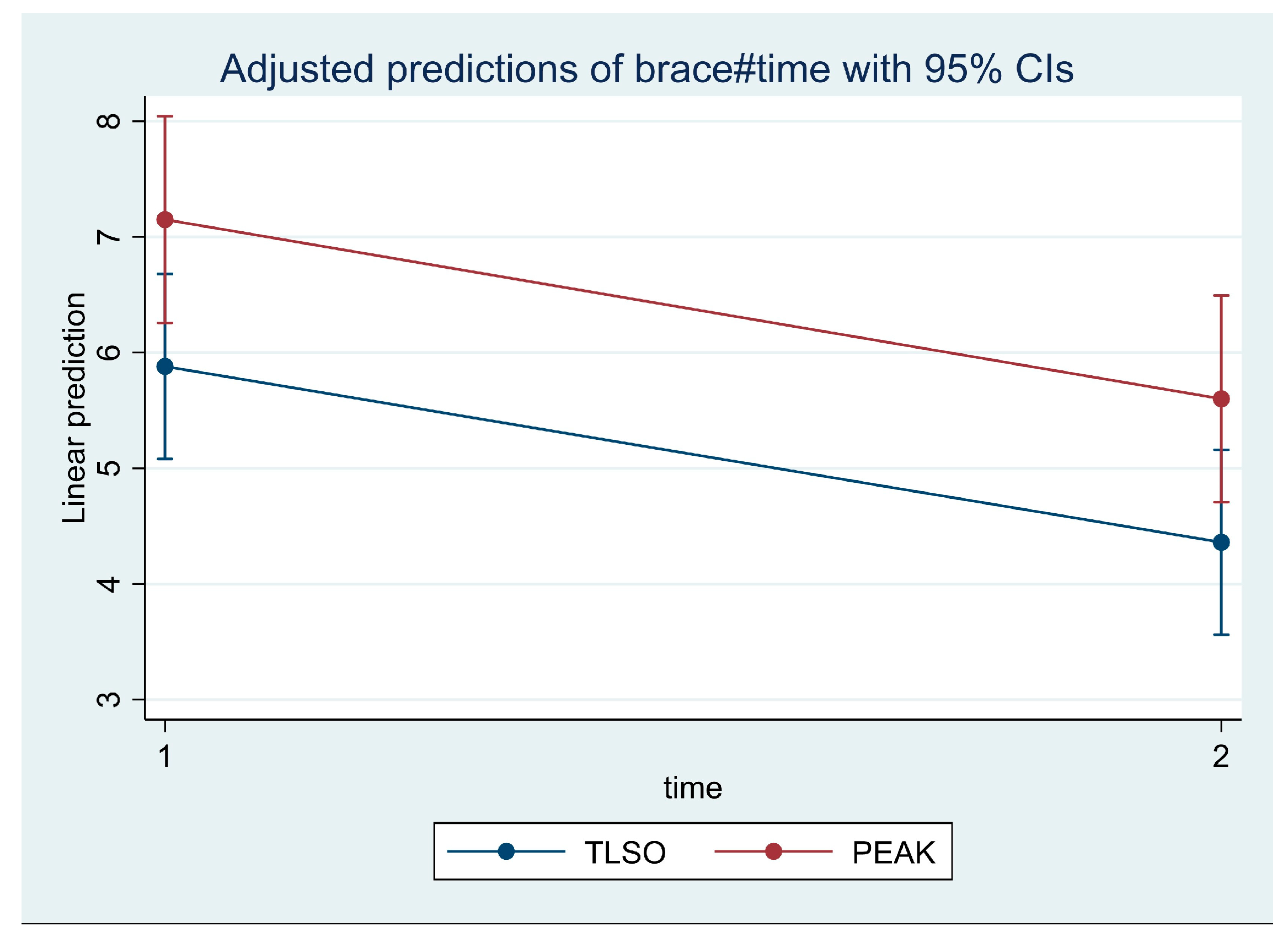
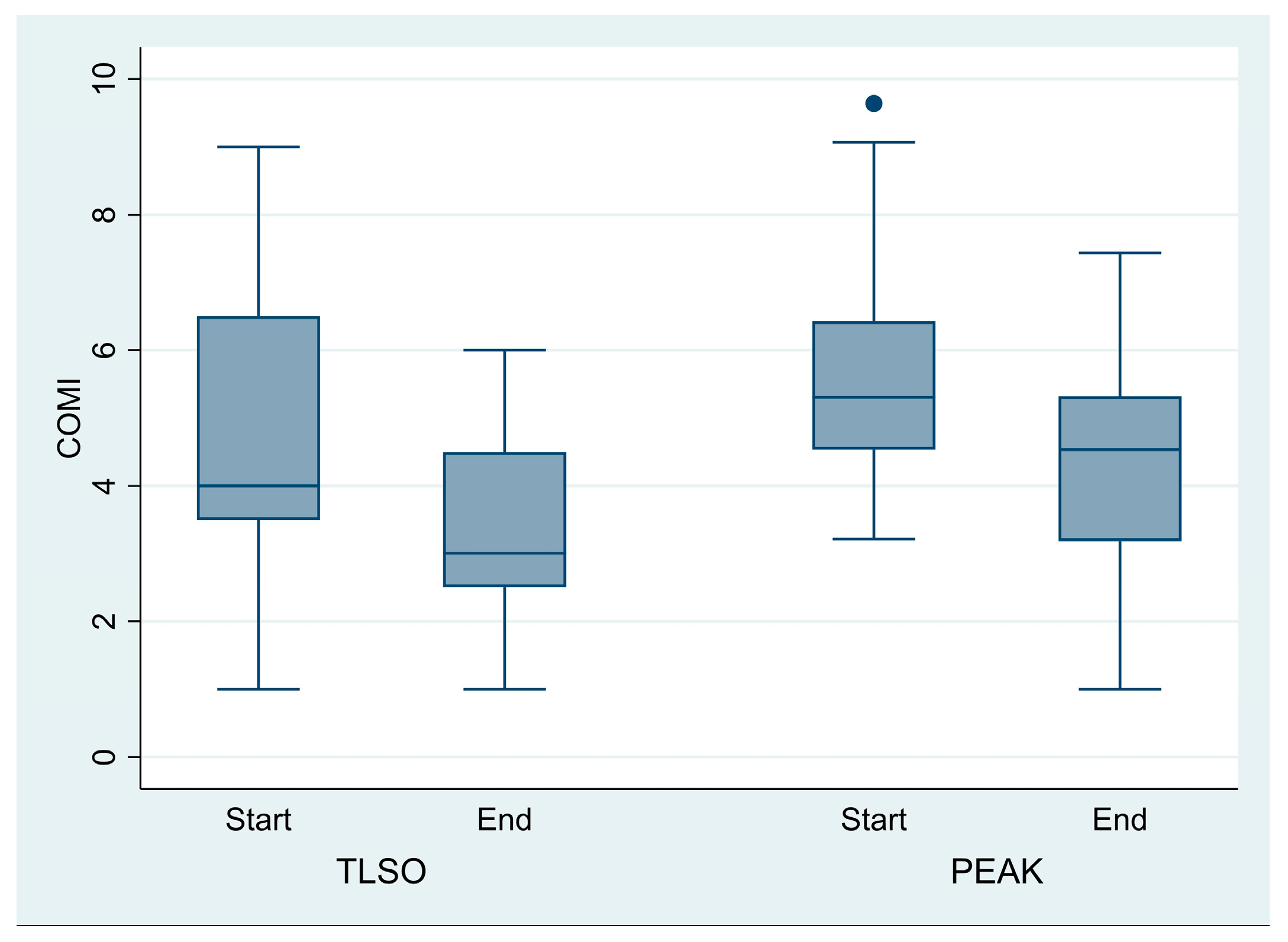
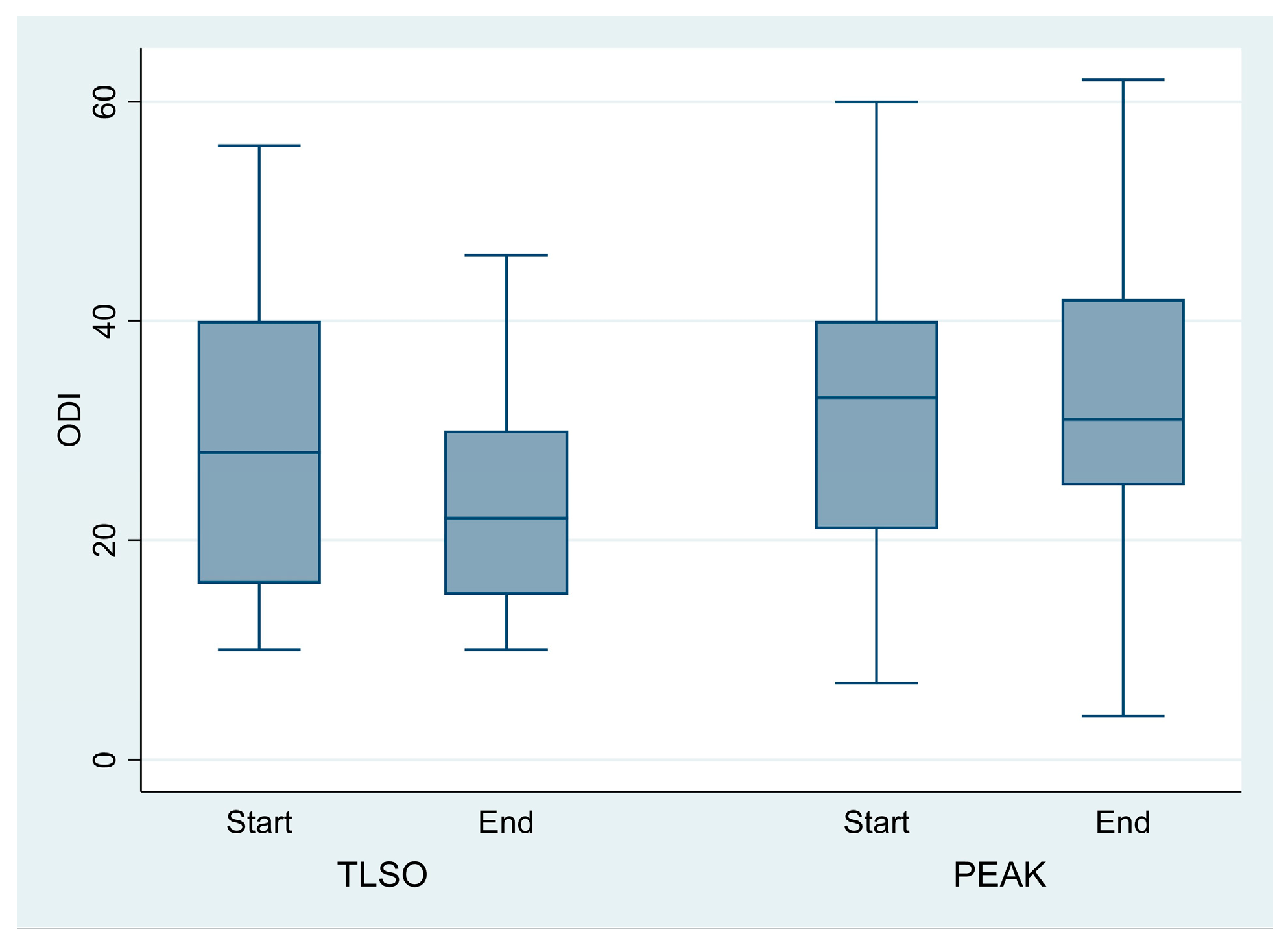
3.2. Pain Improvement
3.3. Logistic Regression Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Negrini, S.; Donzelli, S.; Aulisa, A.G.; Czaprowski, D.; Schreiber, S.; de Mauroy, J.C.; Diers, H.; Grivas, T.B.; Knott, P.; Kotwicki, T.; et al. 2016 SOSORT Guidelines: Orthopaedic and Rehabilitation Treatment of Idiopathic Scoliosis during Growth. Scoliosis Spinal Disord. 2018, 13, 3. [Google Scholar] [CrossRef] [PubMed]
- Schwab, F.; Dubey, A.; Gamez, L.; El Fegoun, A.B.; Hwang, K.; Pagala, M.; Farcy, J.-P. Adult Scoliosis: Prevalence, SF-36, and Nutritional Parameters in an Elderly Volunteer Population. Spine 2005, 30, 1082–1085. [Google Scholar] [CrossRef] [PubMed]
- McAviney, J.; Roberts, C.; Sullivan, B.; Alevras, A.J.; Graham, P.L.; Brown, B.T. The Prevalence of Adult de Novo Scoliosis: A Systematic Review and Meta-Analysis. Eur. Spine J. 2020, 29, 2960–2969. [Google Scholar] [CrossRef]
- Aebi, M. The Adult Scoliosis. Eur. Spine J. 2005, 14, 925–948. [Google Scholar] [CrossRef]
- Marty-Poumarat, C.; Scattin, L.; Marpeau, M.; Garreau de Loubresse, C.; Aegerter, P. Natural History of Progressive Adult Scoliosis. Spine 2007, 32, 1227–1234. [Google Scholar] [CrossRef] [PubMed]
- McAviney, J.; Mee, J.; Fazalbhoy, A.; Du Plessis, J.; Brown, B.T. A Systematic Literature Review of Spinal Brace/Orthosis Treatment for Adults with Scoliosis between 1967 and 2018: Clinical Outcomes and Harms Data. BMC Musculoskelet. Disord. 2020, 21, 87. [Google Scholar] [CrossRef]
- Zaina, F.; Poggio, M.; Di Felice, F.; Donzelli, S.; Negrini, S. Bracing Adults with Chronic Low Back Pain Secondary to Severe Scoliosis: Six Months Results of a Prospective Pilot Study. Eur. Spine J. 2021, 30, 2962–2966. [Google Scholar] [CrossRef]
- Gum, J.L.; Carreon, L.Y.; Glassman, S.D. State-of-the-Art: Outcome Assessment in Adult Spinal Deformity. Spine Deform. 2020, 9, 1–11. [Google Scholar] [CrossRef]
- Zaina, F.; Poggio, M.; Donzelli, S.; Negrini, S. Can Bracing Help Adults with Chronic Back Pain and Scoliosis? Short-Term Results from a Pilot Study. Prosthet. Orthot. Int. 2018, 42, 410–414. [Google Scholar] [CrossRef]
- Negrini, S.; Aulisa, A.G.; Cerny, P.; de Mauroy, J.C.; McAviney, J.; Mills, A.; Donzelli, S.; Grivas, T.B.; Hresko, M.T.; Kotwicki, T.; et al. The Classification of Scoliosis Braces Developed by SOSORT with SRS, ISPO, and POSNA and Approved by ESPRM. Eur. Spine J. 2022, 31, 980–989. [Google Scholar] [CrossRef]
- Gremeaux, V.; Casillas, J.-M.; Fabbro-Peray, P.; Pelissier, J.; Herisson, C.; Perennou, D. Analysis of Low Back Pain in Adults with Scoliosis. Spine 2008, 33, 402–405. [Google Scholar] [CrossRef]
- Weinstein, S.L.; Dolan, L.A.; Spratt, K.F.; Peterson, K.K.; Spoonamore, M.J.; Ponseti, I.V. Health and Function of Patients with Untreated Idiopathic Scoliosis: A 50-Year Natural History Study. JAMA 2003, 289, 559–567. [Google Scholar] [CrossRef]
- Mayo, N.E.; Goldberg, M.S.; Poitras, B.; Scott, S.; Hanley, J. The Ste-Justine Adolescent Idiopathic Scoliosis Cohort Study. Part III: Back Pain. Spine 1994, 19, 1573–1581. [Google Scholar] [CrossRef] [PubMed]
- Jackson, R.P.; Simmons, E.H.; Stripinis, D. Incidence and Severity of Back Pain in Adult Idiopathic Scoliosis. Spine 1983, 8, 749–756. [Google Scholar] [CrossRef]
- Zimmerman, R.M.; Mohamed, A.S.; Skolasky, R.L.; Robinson, M.D.; Kebaish, K.M. Functional Outcomes and Complications after Primary Spinal Surgery for Scoliosis in Adults Aged Forty Years or Older: A Prospective Study with Minimum Two-Year Follow-Up. Spine 2010, 35, 1861–1866. [Google Scholar] [CrossRef] [PubMed]
- Yeramaneni, S.; Robinson, C.; Hostin, R. Impact of Spine Surgery Complications on Costs Associated with Management of Adult Spinal Deformity. Curr. Rev. Musculoskelet. Med. 2016, 9, 327–332. [Google Scholar] [CrossRef] [PubMed]
- Kelly, M.P.; Lurie, J.D.; Yanik, E.L.; Shaffrey, C.I.; Baldus, C.R.; Boachie-Adjei, O.; Buchowski, J.M.; Carreon, L.Y.; Crawford, C.H.; Edwards, C.; et al. Operative Versus Nonoperative Treatment for Adult Symptomatic Lumbar Scoliosis. J. Bone Jt. Surg. Am. 2019, 101, 338–352. [Google Scholar] [CrossRef] [PubMed]
- Monticone, M.; Ambrosini, E.; Cazzaniga, D.; Rocca, B.; Motta, L.; Cerri, C.; Brayda-Bruno, M.; Lovi, A. Adults with Idiopathic Scoliosis Improve Disability after Motor and Cognitive Rehabilitation: Results of a Randomised Controlled Trial. Eur. Spine J. 2016, 25, 3120–3129. [Google Scholar] [CrossRef]
- Weinstein, S.L.; Dolan, L.A.; Wright, J.G.; Dobbs, M.B. Effects of Bracing in Adolescents with Idiopathic Scoliosis. N. Engl. J. Med. 2013, 369, 1512–1521. [Google Scholar] [CrossRef]
- Gallo, D. Case Reports: Orthotic Treatment of Adult Scoliosis Patients with Chronic Back Pain. Scoliosis 2014, 9, 18. [Google Scholar] [CrossRef]
- Polastri, M.; Romano, M. Lumbar Scoliosis: Reducing Lower Back Pain and Improving Function in Adulthood. A Case Report with a 2-Year Follow-Up. J. Bodyw. Mov. Ther. 2017, 21, 81–85. [Google Scholar] [CrossRef]
- De Mauroy, J.C.; Vallèse, P.; Lalain, J.J. Lyon Conservative Treatment of Adult Scoliosis. Minerva Ortop. E Traumatol. 2011, 62, 385–396. [Google Scholar]
- Weiss, H.-R.; Dallmayer, R. Brace Treatment of Spinal Claudication in an Adult with Lumbar Scoliosis—A Case Report. Stud. Health Technol. Inf. 2006, 123, 586–589. [Google Scholar]
- Weiss, H.-R.; Werkmann, M. Treatment of Chronic Low Back Pain in Patients with Spinal Deformities Using a Sagittal Re-Alignment Brace. Scoliosis 2009, 4, 7. [Google Scholar] [CrossRef]
- de Mauroy, J.C.; Lecante, C.; Barral, F.; Pourret, S. Bracing in Adult with Scoliosis: Experience in Diagnosis and Classification from a 15 Year Prospective Study of 739 Patients. Scoliosis Spinal Disord. 2016, 11, 29. [Google Scholar] [CrossRef]
- Janicki, J.A.; Poe-Kochert, C.; Armstrong, D.G.; Thompson, G.H. A Comparison of the Thoracolumbosacral Orthoses and Providence Orthosis in the Treatment of Adolescent Idiopathic Scoliosis: Results Using the New SRS Inclusion and Assessment Criteria for Bracing Studies. J. Pediatr. Orthop. 2007, 27, 369–374. [Google Scholar] [CrossRef] [PubMed]
- Simony, A.; Beuschau, I.; Quisth, L.; Jespersen, S.M.; Carreon, L.Y.; Andersen, M.O. Providence Nighttime Bracing Is Effective in Treatment for Adolescent Idiopathic Scoliosis Even in Curves Larger than 35°. Eur. Spine J. 2019, 28, 2020–2024. [Google Scholar] [CrossRef]
- Charalampidis, A.; Diarbakerli, E.; Dufvenberg, M.; Jalalpour, K.; Ohlin, A.; Ahl, A.A.; Möller, H.; Abbott, A.; Gerdhem, P.; CONTRAIS Study Group. Nighttime Bracing or Exercise in Moderate-Grade Adolescent Idiopathic Scoliosis: A Randomized Clinical Trial. JAMA Netw. Open 2024, 7, e2352492. [Google Scholar] [CrossRef]
- Buyuk, A.F.; Truong, W.H.; Morgan, S.J.; Snyder, A.J.; Miller, D.J.; Nolin, K.K.; Smith, K.J. Is Nighttime Bracing Effective in the Treatment of Adolescent Idiopathic Scoliosis? A Meta-Analysis and Systematic Review Based on Scoliosis Research Society Guidelines. Spine Deform. 2022, 10, 247–256. [Google Scholar] [CrossRef]
- Weiss, H.-R.; Dallmayer, R.; Stephan, C. First Results of Pain Treatment in Scoliosis Patients Using a Sagittal Realignment Brace. Stud. Health Technol. Inf. Inform. 2006, 123, 582–585. [Google Scholar]
- Azadinia, F.; Ebrahimi, E.; Kamyab, M.; Parnianpour, M.; Cholewicki, J.; Maroufi, N. Can Lumbosacral Orthoses Cause Trunk Muscle Weakness? A Systematic Review of Literature. Spine J. 2017, 17, 589–602. [Google Scholar] [CrossRef] [PubMed]
- Takasaki, H.; Miki, T. The Impact of Continuous Use of Lumbosacral Orthoses on Trunk Motor Performance: A Systematic Review with Meta-Analysis. Spine J. 2017, 17, 889–900. [Google Scholar] [CrossRef] [PubMed]
- Palazzo, C.; Montigny, J.-P.; Barbot, F.; Bussel, B.; Vaugier, I.; Fort, D.; Courtois, I.; Marty-Poumarat, C. Effects of Bracing in Adult With Scoliosis: A Retrospective Study. Arch. Phys. Med. Rehabil. 2017, 98, 187–190. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | |
|---|---|
| Age | 62.3 ± 9.5 |
| BMI | 23.1 ± 3.8 |
| Curve (°Cobb) | 60.4 ± 17.7 |
| Single/Double Curve | 18 single (72%) |
| 7 double (28%) | |
| Localization | 9 thoracic (36%) |
| 8 thoraco-lumbar (32%) | |
| 8 lumbar (32%) | |
| Diagnosis | 15 AIS (60%) |
| 3 JIS (12%) | |
| 6 adult scoliosis (24%) | |
| Exercises (Min/week) | 117.9 ± 48 |
| Previous exercises | 12 yes (48%), from 7.3 ± 6.2 months |
| 13 no (52%) | |
| Wearing hours | 7.2 ± 2.2 |
| Age | 62.3 ± 9.5 |
| BMI | 23.1 ± 3.8 |
| LL | 44.0 ± 11.4 |
| PI | 52.2 ± 16.4 |
| PT | 19.2 ± 10.2 |
| PI-LL | 7.2 ± 12.6 |
| TLSO Brace | Peak Brace | |||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | 6 Months | p Value Intragroup | Baseline | 6 Months | p Value Intergroup Post-Treatment | |||
| Mean/Median (SD/95%CI) | Mean/Median (SD/95%CI) | p Value Intergroup Pre-treatment | Mean/Median (SD/95%CI) | Mean/Median (SD/95%CI) | p Value Intragroup | |||
| Worst Pain (back or leg) | 5.9 ± 1.9 | 4. ± 2.5 | 0.01 * | 0.09 | 7.15 ± 2.03 | 5.6 ± 2.13 | 0.007* | 0.06 |
| Back Pain | 5.7 ± 1.9 | 3.6 ± 1.9 | 0.001 * | 0.28 | 6.55 ± 2.37 | 5.25 ± 2.69 | 0.06 | 0.07 |
| Leg Pain | 4.9 ± 2.9 | 3.3 ± 3.4 | 0.22 | 0.01 * | 5.65 ± 3.03 | 4.35 ± 2.66 | 0.04 * | 0.01 * |
| COMI | 4.2 ± 2.0 | 3.1 ± 1.3 | 0.19 | 0.04 * | 5.67 (5.11–6.79) | 4.18 (3.34–5.02) | 0.002 * | 0.11 |
| ODI | 28.7 ± 15.1 | 23.8 ± 10.8 | 0.06 | 0.51 | 33.00 (25.26–38.43) | 33.05 (26.30–39.79) | 0.96 | 0.04 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zaina, F.; Poggio, M.; Donzelli, S.; Castelein, R.; Di Felice, F.; Negrini, S. Night-Time Bracing Can Reduce Pain in Adults with Scoliosis: Six-Month Results of a Retrospective Controlled Study. J. Clin. Med. 2025, 14, 4493. https://doi.org/10.3390/jcm14134493
Zaina F, Poggio M, Donzelli S, Castelein R, Di Felice F, Negrini S. Night-Time Bracing Can Reduce Pain in Adults with Scoliosis: Six-Month Results of a Retrospective Controlled Study. Journal of Clinical Medicine. 2025; 14(13):4493. https://doi.org/10.3390/jcm14134493
Chicago/Turabian StyleZaina, Fabio, Martina Poggio, Sabrina Donzelli, René Castelein, Francesca Di Felice, and Stefano Negrini. 2025. "Night-Time Bracing Can Reduce Pain in Adults with Scoliosis: Six-Month Results of a Retrospective Controlled Study" Journal of Clinical Medicine 14, no. 13: 4493. https://doi.org/10.3390/jcm14134493
APA StyleZaina, F., Poggio, M., Donzelli, S., Castelein, R., Di Felice, F., & Negrini, S. (2025). Night-Time Bracing Can Reduce Pain in Adults with Scoliosis: Six-Month Results of a Retrospective Controlled Study. Journal of Clinical Medicine, 14(13), 4493. https://doi.org/10.3390/jcm14134493










