Earthing as a Supportive Therapy for Post-Spinal Surgery Recovery
Abstract
1. Introduction
2. Materials and Methods
Statistical Analysis
3. Results
3.1. Effect of Earthing on Postoperative Pain (N = 84)
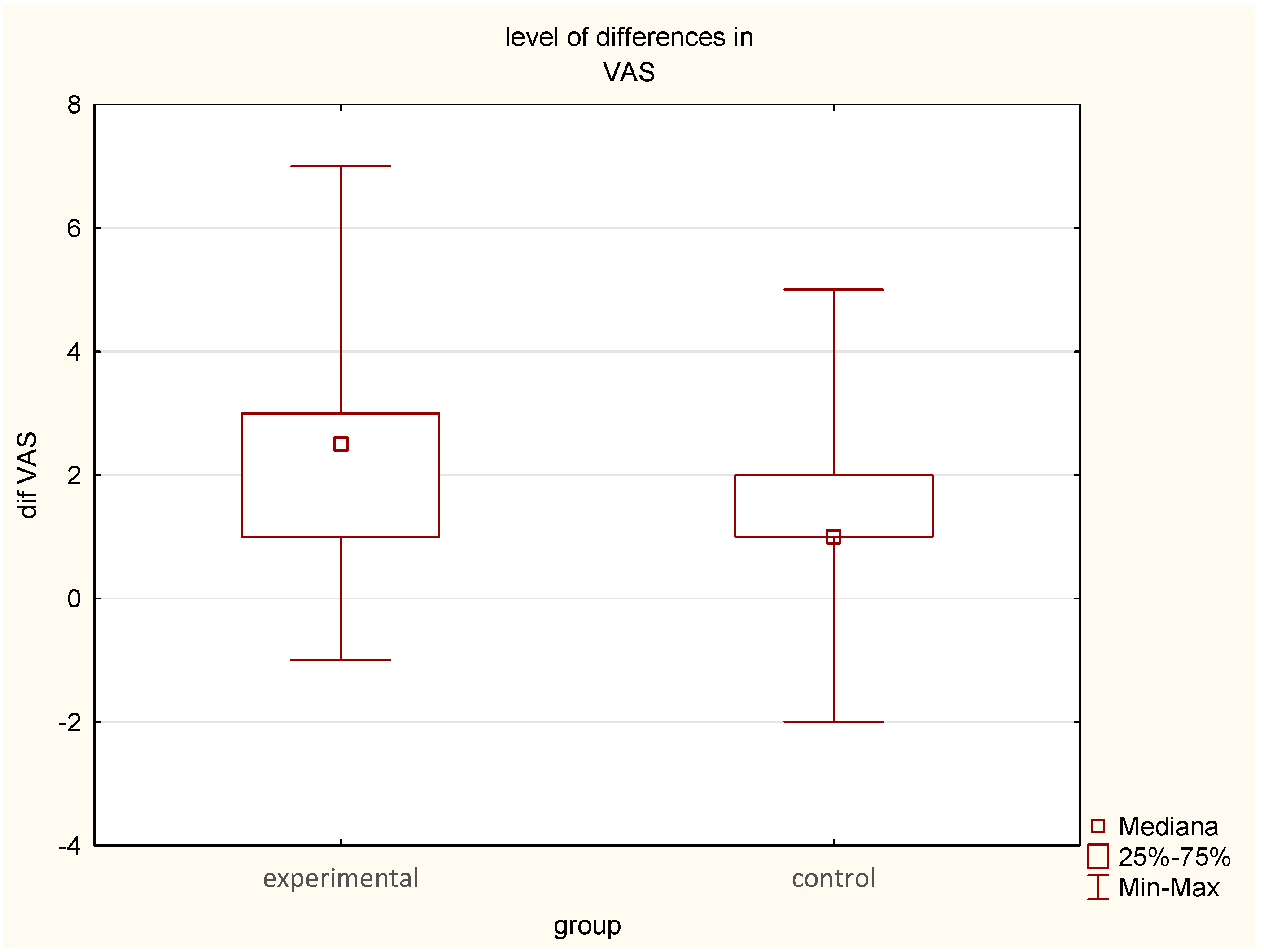
- On postoperative day 1, mean VAS scores were 7.14 ± 1.41 (median = 7) in the EG and 6.6 ± 1.95 (median = 7) in the CG.
- On postoperative day 2, pain significantly decreased in the EG to 4.64 ± 1.29 (median = 5), p < 0.05, compared to 5.26 ± 1.47 (median = 5) in the CG, p < 0.05.
- The mean reduction in pain intensity was greater in the EG (2.50 points) (median = 2.0) compared to the CG (1.59 points) (median = 1.0), suggesting a meaningful analgesic effect of earthing in the experimental group (Figure 2, Table 1, Table 2 and Table 3). The difference in change in pain intensity between the two groups was statistically significant (p < 0.01)
3.2. Effect of Earthing on Postoperative Muscle Injury (N = 84)
- Preoperative CK levels in the EG were 311.97 U/L (median = 208.5), decreasing to 257.36 U/L (median = 182.5) after one night of earthing (p < 0.0001).
- In the CG, CK levels declined from 373.45 U/L (median = 307) to 332.95 U/L (median = 229.5) (p < 0.001).
3.3. Effect of Earthing on Inflammatory Markers (N = 84)
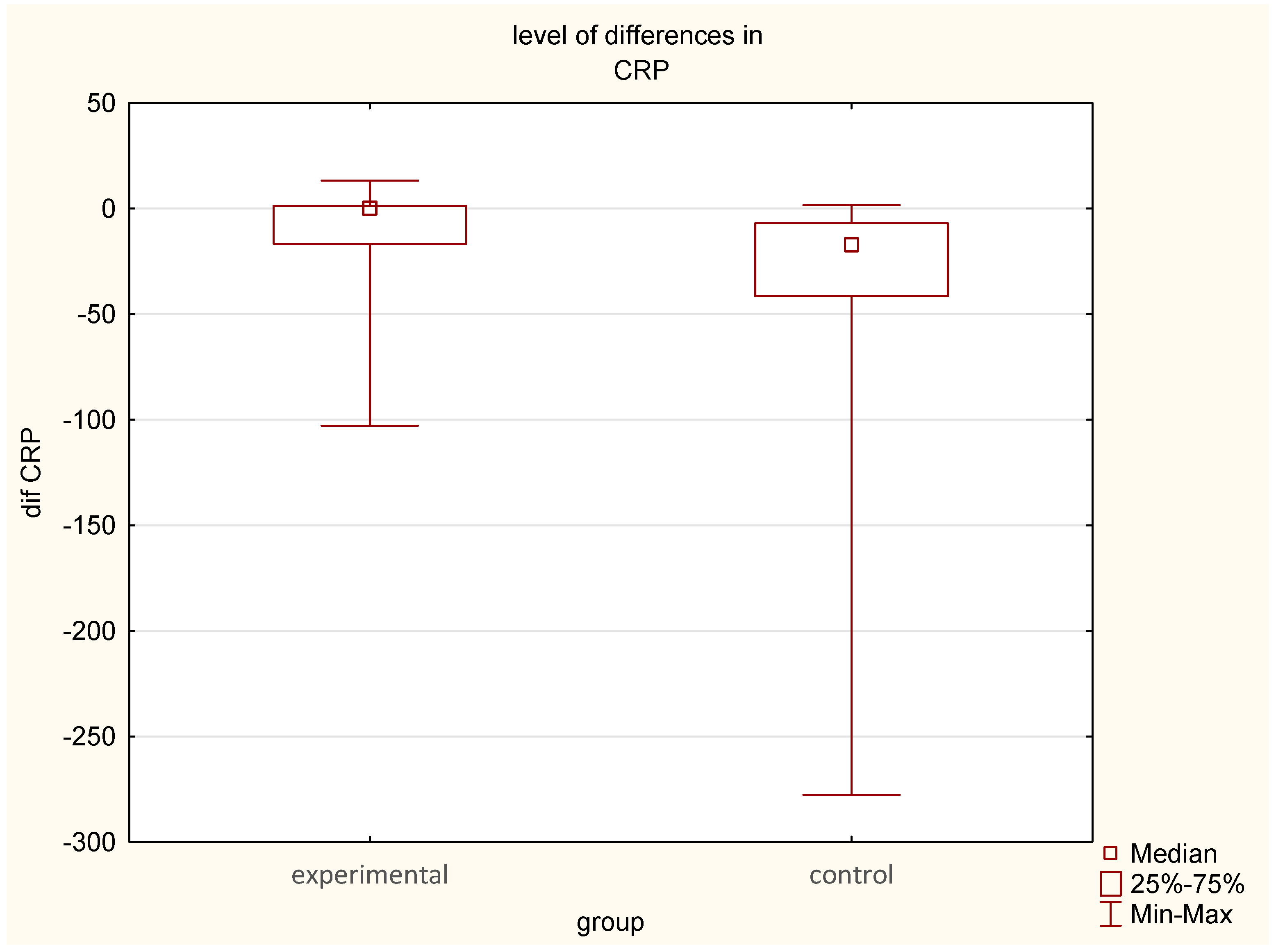
- Postoperative CRP levels increased significantly in both groups, but the rise was lower in the EG (15.34 mg/L to 24.42 mg/L) compared to the CG (24.54 mg/L to 57.42 mg/L).
3.4. Effect of Earthing on Calcium-Phosphate Metabolism (N = 56)
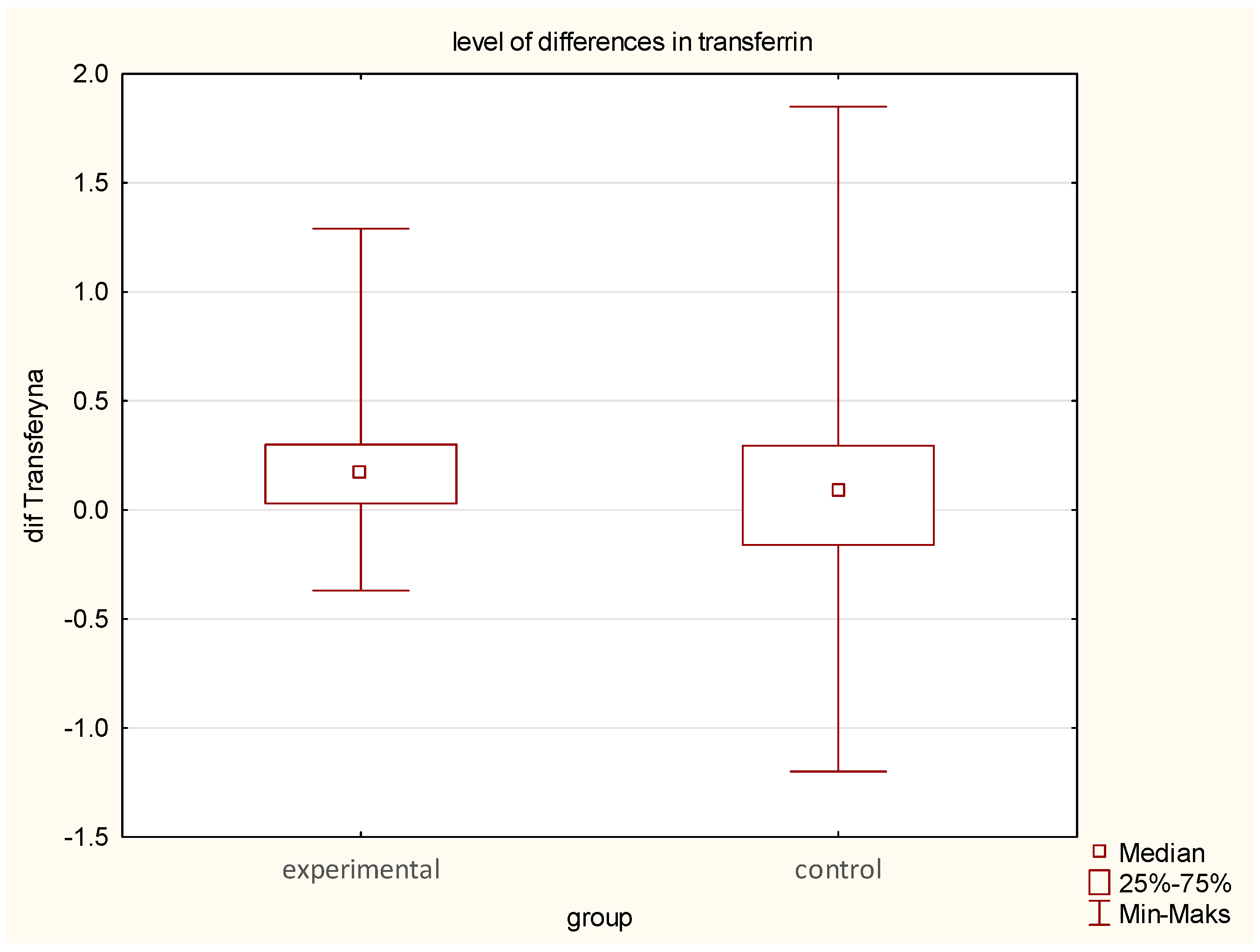
3.5. Effect of Earthing on Iron Metabolism (N = 56)
- Transferrin levels declined more significantly in the EG (from 2.46 to 2.26 g/L) (median difference—0.17, p = 0.02) than in the CG (from 2.28 to 2.24 g/L) (median difference—0.08).
- Ferritin variability was greater in the EG (145 ng/mL—no median change), with both increases and decreases, whereas the CG exhibited a more uniform rise (from 131 to 143 ng/mL) (p = 0.02).
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| DOMS | Delayed onset muscle soreness |
| CK | creatine kinase |
| CRP | C—reactive protein |
References
- Arts, M.; Brand, R.; Kallen, B. Van Der Does Minimally Invasive Lumbar Disc Surgery Result in Less Muscle Injury than Conventional Surgery? A Randomized Controlled Trial. Eur. Spine J. 2011, 20, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Peng, H.; Tang, G.; Zhuang, X.; Lu, S.; Bai, Y.; Xu, L. Minimally Invasive Spine Surgery Decreases Postoperative Pain and Inflammation for Patients with Lumbar Spinal Stenosis. Exp. Ther. Med. 2019, 18, 3032–3036. [Google Scholar] [CrossRef] [PubMed]
- Baird, M.F.; Graham, S.M.; Baker, J.S.; Bickerstaff, G.F. Creatine-Kinase- and Exercise-Related Muscle Damage Implications for Muscle Performance and Recovery. J. Nutr. Metab. 2012, 2012, 960363. [Google Scholar] [CrossRef]
- Sang, P.; Ma, Y.; Chen, B.; Zhang, M. The Role of Serum Creatine Kinase Levels in Anterior Cervical Spinal Surgery: Change Trends and Risk Factors. Medicine 2021, 100, e28300. [Google Scholar] [CrossRef]
- Lombao, D.; Bagó, J.; Vilor, T. Validity of Creatine Kinase as an Indicator of Muscle Injury in Spine Surgery and Its Relation with Postoperative Pain. Acta Orthop. Belg. 2014, 80, 545–550. [Google Scholar] [CrossRef]
- Sokal, K.; Sokal, P. Earthing the Human Organism Influences Bioelectrical Processes. J. Altern. Complement. Med. 2012, 18, 229–234. [Google Scholar] [CrossRef] [PubMed]
- Chevalier, G.; Sinatra, S.T.; Oschman, J.L.; Sokal, K.; Sokal, P. Earthing: Health Implications of Reconnecting the Human Body to the Earth’s Surface Electrons. J. Environ. Public Health 2012, 2012, 291541. [Google Scholar] [CrossRef]
- Chamberlin, K.; Smith, W.; Chirgwin, C.; Appasani, S.; Rioux, P. Analysis of the Charge Exchange between the Human Body and Ground: Evaluation of “Earthing” from an Electrical Perspective. J. Chiropr. Med. 2014, 13, 239–246. [Google Scholar] [CrossRef]
- Chevalier, G.; Brown, R.; Hill, M. Grounding after Moderate Eccentric Contractions Reduces Muscle Damage. Open Access J. Sports Med. 2015, 6, 305–317. [Google Scholar] [CrossRef]
- Sokal, K.; Sokal, P. Earthing the Human Body Influences Physiologic Processes. J. Altern. Complement. Med. 2011, 17, 301–308. [Google Scholar] [CrossRef]
- Sokal, P.; Jastrzębski, Z.; Sokal, K.; Dargiewicz, R.; Jastrzębska, M.; Radzimiński, Ł. Earthing Modulates Glucose and Erythrocytes Metabolism in Exercise. Int. J. Phys. Educ. Sports Health 2016, 3, 6–13. [Google Scholar]
- Sokal, P.; Jastrzȩbski, Z.; Jaskulska, E.; Sokal, K.; Jastrzȩbska, M.; Radzimiński, Ł.; Dargiewicz, R.; Zieliński, P. Differences in Blood Urea and Creatinine Concentrations in Earthed and Unearthed Subjects during Cycling Exercise and Recovery. Evid. -Based Complement. Altern. Med. 2013, 2013, 382643. [Google Scholar] [CrossRef] [PubMed]
- Chevalier, G.; Mori, K.; Oschman, J.L. The Effect of Earthing (Grounding) on Human Physiology. Eur. Biol. Bioelectromagn. 2006, 2, 600–621. [Google Scholar]
- Brown, R.; Chevalier, G. Grounding the Human Body during Yoga Exercise with a Grounded Yoga Mat Reduces Blood Viscosity. Open J. Prev. Med. 2015, 5, 159–168. [Google Scholar] [CrossRef]
- Chevalier, G.; Melvin, G.; Barsotti, T. One-Hour Contact with the Earth’s Surface (Grounding) Improves Inflammation and Blood Flow—A Randomized, Double-Blind, Pilot Study. Health N. Hav. 2015, 7, 1022–1059. [Google Scholar] [CrossRef][Green Version]
- Estiningtyas, E.; Novitayanti, E.; Proborini, C.A.; Cahyaningtyas, A.Y.; Muflikhun, M.A. Earthing Method as a Lifestyle Medicine to Accelerate the Healing of Chronic Diabetic Wounds. J. Health Sci. Prev. 2024, 8, 1–8. [Google Scholar] [CrossRef]
- Chevalier, G.; Sinatra, S.T.; Oschman, J.L.; Delany, R.M. Earthing (Grounding) the Human Body Reduces Blood Viscosity—A Major Factor in Cardiovascular Disease. J. Altern. Complement. Med. 2013, 19, 102–110. [Google Scholar] [CrossRef]
- Abdelmageed Makia, M.; Abdelbary, T.; AlBakry, A. Paraspinal Muscle Damage in Intermuscular and Conventional Lumbar Spinal Fixation: A Comparative Study. Interdiscip. Neurosurg. 2021, 26, 101284. [Google Scholar] [CrossRef]
- Chevalier, G.; Patel, S.; Weiss, L.; Chopra, D.; Mills, P.J. The Effects of Grounding (Earthing) on Bodyworkers’ Pain and Overall Quality of Life: A Randomized Controlled Trial. Explore 2019, 15, 181–190. [Google Scholar] [CrossRef]
- Arts, M.P.; Nieborg, A.; Brand, R.; Peul, W.C. Serum Creatine Phosphokinase as an Indicator of Muscle Injury after Various Spinal and Nonspinal Surgical Procedures. J. Neurosurg. Spine 2007, 7, 282–286. [Google Scholar] [CrossRef]
- Eston, R.G.; Mickleborough, J.; Baltzopoulos, V. Eccentric Activation and Muscle Damage: Biomechanical and Physiological Considerations during Downhill Running. Br. J. Sports Med. 1995, 29, 89–94. [Google Scholar] [CrossRef] [PubMed]
- Müller, E.; Pröller, P.; Ferreira-Briza, F.; Aglas, L.; Stöggl, T. Effectiveness of Grounded Sleeping on Recovery after Intensive Eccentric Muscle Loading. Front. Physiol. 2019, 10, 35. [Google Scholar] [CrossRef] [PubMed]
- Ghaly, M.; Teplitz, D. The Biologic Effects of Grounding the Human Body During Sleep as Measured by Cortisol Levels and Subjective Reporting of Sleep, Pain, and Stress. J. Altern. Complement. Med. 2004, 10, 767–776. [Google Scholar] [CrossRef]
- Brown, D.; Chevalier, G.; Hill, M. Pilot Study on the Effect of Grounding on Delayed-Onset Muscle Soreness. J. Altern. Complement. Med. 2010, 16, 265–273. [Google Scholar] [CrossRef] [PubMed]
- Pantoja, P.; Alberton, C.; Pilla, C.; Vendrusculo, A.; Kruel, L. Effect of Resistive Exercise on Muscle Damage in Water and on Land. J. Strength. Cond. Res. 2009, 23, 1051–1054. [Google Scholar] [CrossRef]
- Sereda, A.P.; Rukina, A.N.; Trusova, Y.V.; Dzhavadov, A.A.; Cherny, A.A.; Bozhkova, S.A.; Shubnyakov, I.I.; Tikhilov, R.M. Dynamics of C-Reactive Protein Level after Orthopedic Surgeries. J. Orthop. 2024, 47, 1–7. [Google Scholar] [CrossRef]
- Schmidt, F.; Ward, M.; Repanos, C. Postoperative Serum C-Reactive Protein Dynamics after Pharyngolaryngectomy with Jejunal Free-Flap Reconstruction. Ann. R. Coll. Surg. Engl. 2023, 105, 263–268. [Google Scholar] [CrossRef]
- Oschman, J.L.; Chevalier, G.; Brown, R. The Effects of Grounding (Earthing) on Inflammation, the Immune Response, Wound Healing, and Prevention and Treatment of Chronic Inflammatory and Autoimmune Diseases. J. Inflamm. Res. 2015, 8, 83–96. [Google Scholar] [CrossRef]
- Sadot, E.; Zheng, J.; Srouji, R.; Strong, V.E.; Gönen, M.; Balachandran, V.P.; D’Angelica, M.I.; Allen, P.J.; DeMatteo, R.P.; Kingham, T.P.; et al. Hypophosphatemia as a Predictor of Organ-Specific Complications Following Gastrointestinal Surgery: Analysis of 8034 Patients. World J. Surg. 2019, 43, 385–394. [Google Scholar] [CrossRef]

| Parameter | U Mann-Whitney Test. Statistical Significance p < 0.05000 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Sum.of Ranks exp EG | Sum of Ranks contr CG | U | Z | p | Z cor | p | N.exp | N.contr | p | |
| VAS before | 1843.5 | 1726.5 | 823.5 | 0.51887 | 0.603851 | 0.53562 | 0.592218 | 42 | 42 | 0.602522 |
| VAS after | 1554 | 2016 | 651 | −2.06207 | 0.039202 | −2.1475 | 0.031755 | 42 | 42 | 0.038749 |
| Na [mmol/L] before | 791.5 | 804.5 | 385.5 | −0.09832 | 0.921677 | −0.09927 | 0.920922 | 28 | 28 | 0.915857 |
| Na [mmol/L] after | 893.5 | 702.5 | 296.5 | 1.55675 | 0.119531 | 1.56704 | 0.117106 | 28 | 28 | 0.118157 |
| K [mmol/L] before | 737 | 859 | 331 | −0.9914 | 0.321489 | −0.99174 | 0.321324 | 28 | 28 | 0.324159 |
| K [mmol/L] after | 726 | 870 | 320 | −1.17166 | 0.241335 | −1.17198 | 0.241206 | 28 | 28 | 0.243438 |
| urea [mg/dL] before | 838.5 | 757.5 | 351.5 | 0.65547 | 0.512163 | 0.65623 | 0.51168 | 28 | 28 | 0.509859 |
| urea [mg/dL] after | 815 | 781 | 375 | 0.27038 | 0.786866 | 0.27067 | 0.786645 | 28 | 28 | 0.788512 |
| glucose [mg/dL] before | 833 | 763 | 357 | 0.56535 | 0.571839 | 0.56552 | 0.571721 | 28 | 28 | 0.574634 |
| glucose [mg/dL] after | 681 | 915 | 275 | −1.90907 | 0.056254 | −1.91103 | 0.056002 | 28 | 28 | 0.05581 |
| CRP [mg/L] before | 1574.5 | 1995.5 | 671.5 | −1.87867 | 0.06029 | −1.8788 | 0.060273 | 42 | 42 | 0.059425 |
| CRP [mg/L] after | 1479.5 | 2090.5 | 576.5 | −2.72855 | 0.006362 | −2.72863 | 0.00636 | 42 | 42 | 0.005849 |
| ALP [U/L] before | 790 | 806 | 384 | −0.1229 | 0.902185 | −0.12294 | 0.902152 | 28 | 28 | 0.90297 |
| ALP [U/L] after | 731.5 | 864.5 | 325.5 | −1.08153 | 0.279462 | −1.08249 | 0.279034 | 28 | 28 | 0.278221 |
| Ca [mmol/L] before | 815.5 | 780.5 | 374.5 | 0.27858 | 0.78057 | 0.2788 | 0.780398 | 28 | 28 | 0.776022 |
| Ca [mmol/L] after | 760.5 | 835.5 | 354.5 | −0.60631 | 0.544307 | −0.60699 | 0.54386 | 28 | 28 | 0.541771 |
| Pi [mmol/L] before | 678.5 | 917.5 | 272.5 | −1.95003 | 0.051173 | −1.95107 | 0.05105 | 28 | 28 | 0.049667 |
| Pi [mmol/L] after | 847 | 749 | 343 | 0.79476 | 0.426753 | 0.79503 | 0.426595 | 28 | 28 | 0.429735 |
| CK [U/L] before | 1612.5 | 1957.5 | 709.5 | −1.53872 | 0.123873 | −1.53878 | 0.12386 | 42 | 42 | 0.123207 |
| CK [U/L] after | 1569 | 2001 | 666 | −1.92788 | 0.053871 | −1.92794 | 0.053863 | 42 | 42 | 0.053555 |
| Fe [ug/dL] before | 821 | 775 | 369 | 0.3687 | 0.712349 | 0.36883 | 0.712255 | 28 | 28 | 0.714479 |
| Fe [ug/dL] after | 882 | 714 | 308 | 1.3683 | 0.171219 | 1.3687 | 0.171094 | 28 | 28 | 0.172551 |
| Ferritin [ng/mL] before | 822.5 | 773.5 | 367.5 | 0.39328 | 0.69411 | 0.3933 | 0.6941 | 28 | 28 | 0.69034 |
| Ferritin [ng/mL] after | 820 | 776 | 370 | 0.35232 | 0.724601 | 0.35234 | 0.724587 | 28 | 28 | 0.726657 |
| Transferin [g/L] before | 814 | 782 | 376 | 0.254 | 0.799499 | 0.25403 | 0.799472 | 28 | 28 | 0.801056 |
| Transferin [g/L] after | 771 | 825 | 365 | −0.43425 | 0.664106 | −0.43435 | 0.664036 | 28 | 28 | 0.666507 |
| Differences | Group | N | Mean | Median | Minimum | Maximum | Std.dev |
|---|---|---|---|---|---|---|---|
| dif VAS | ex | 42 | 2.5 | 2.5 | −1 | 7 | 1.62676 |
| dif Na | ex | 28 | −0.9286 | −100.000 | −8.000 | 40.000 | 272.068 |
| dif K | ex | 28 | 433.214 | 0.00000 | 0.000 | 1010.000 | 5086.806 |
| dif urea | ex | 28 | 40.357 | 450.000 | −7.000 | 190.000 | 600.914 |
| dif GLU | ex | 28 | 372.143 | 3450.000 | −24.000 | 1570.000 | 3660.435 |
| dif CRP | ex | 42 | −10.0762 | 0.05 | −102.9 | 13.2 | 24.16638 |
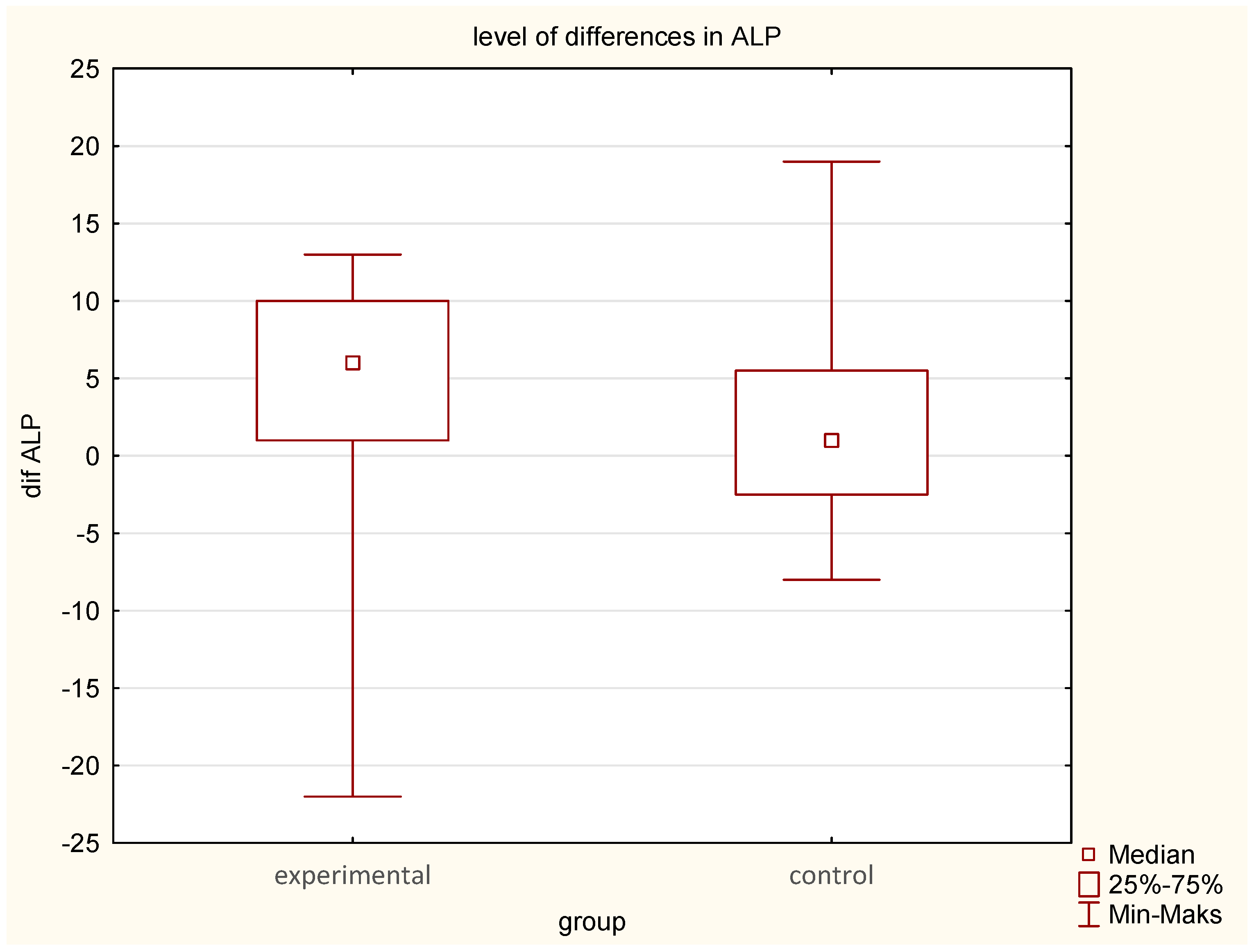
| dif ALP | ex | 28 | 41.429 | 600.000 | −22.000 | 130.000 | 819.085 |
| dif calcium | ex | 28 | 0.0400 | 0.04000 | −0.110 | 0.1800 | 0.07832 |
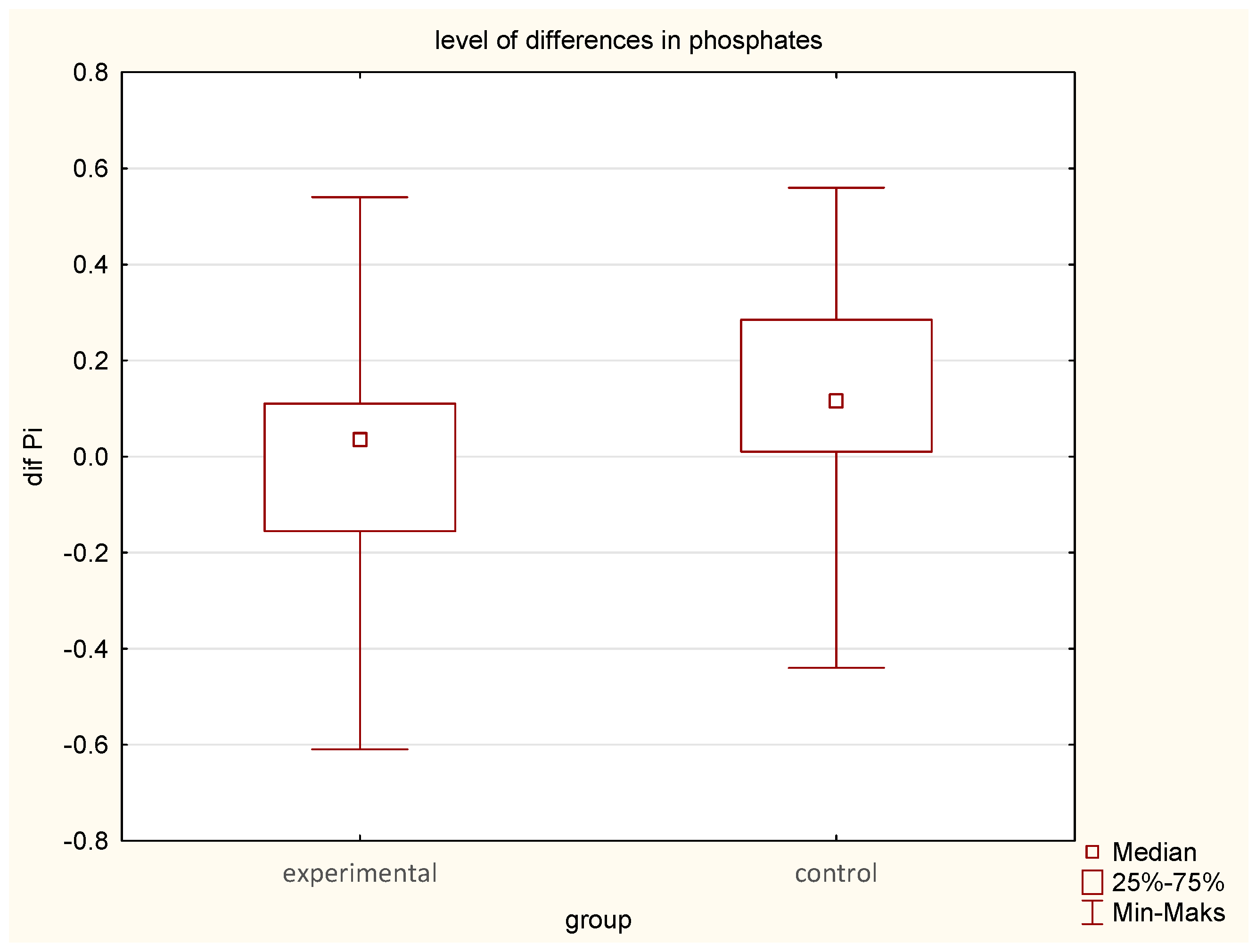
| dif phosphate | ex | 28 | −0.0296 | 0.03500 | −0.610 | 0.5400 | 0.24606 |
| dif CK | ex | 42 | 54.619 | 44.5 | −128 | 250 | 69.79131 |
| dif iron | ex | 28 | −93.571 | −600.000 | −58.000 | 570.000 | 2463.393 |
| dif ferritin | ex | 28 | 39.286 | 350.000 | −85.000 | 1410.000 | 4528.096 |
| dif transferrin | ex | 28 | 0.2046 | 0.17000 | −0.370 | 12,900 | 0.35132 |
| dif VAS | ctr | 42 | 1.5952 | 1 | −2 | 5 | 1.53113 |
| dif NA | ctr | 28 | 0.2500 | 0.0000 | −6.000 | 60.000 | 257.660 |
| dif K | ctr | 28 | 438.571 | 40.000 | 0.000 | 1010.000 | 5,043,640 |
| dif urea | ctr | 28 | 35,357 | 30.000 | −6.000 | 150.000 | 522.446 |
| dif GLU | ctr | 28 | 276.429 | 180.000 | −38.000 | 1340.000 | 3894.366 |
| dif CRP | ctr | 42 | −33.3857 | −17.2 | −277.6 | 1.6 | 48.93226 |
| dif ALP | ctr | 28 | 15.357 | 10.000 | −8.000 | 190.000 | 570.563 |
| dif CA | ctr | 28 | 0.0164 | 0.0200 | −0.130 | 0.2600 | 0.09318 |
| dif phosphate | ctr | 28 | 0.1143 | 0.1150 | −0.440 | 0.5600 | 0.24990 |
| dif CK | ctr | 42 | 40.5 | 26 | −295 | 325 | 96.83661 |
| dif iron | ctr | 28 | −0.4643 | −20.000 | −51.000 | 370.000 | 1778.781 |
| dif ferritin | ctr | 28 | −97.857 | −120.000 | −84.000 | 700.000 | 2725.919 |
| dif transferrin | ctr | 28 | 0.0943 | 0.0850 | −1.200 | 18.500 | 0.55129 |
| Differences in Parameters | Sum of Ranks EG | Sum of Ranks CG | U | Z | p |
|---|---|---|---|---|---|
| dif VAS | 2071.500 | 1498.500 | 595.500 | 2.558574 | 0.010511 |
| dif NA | 705.000 | 891.000 | 299.000 | −1.516 | 0.129575 |
| dif K | 787.500 | 808.500 | 381.500 | −0.164 | 0.889223 |
| dif urea | 819.000 | 777.000 | 371.000 | 0.336 | 0.736924 |
| dif GLU | 867.500 | 728.500 | 322.500 | 1.131 | 0.258186 |
| dif CRP | 2249.500 | 1320.500 | 417.500 | 4.150972 | 0.000033 |
| dif ALP | 936.500 | 659.500 | 253.500 | 2.261 | 0.023736 |
| dif Calcium | 869.000 | 727.000 | 321.000 | 1.155 | 0.247980 |
| dif phosphate | 656.500 | 939.500 | 250.500 | −2.311 | 0.020859 |
| dif CK | 1855.000 | 1715.000 | 812.000 | 0.621751 | 0.534106 |
| dif iron | 703.500 | 892.500 | 297.500 | −1.540 | 0.123473 |
| dif ferritin | 918.500 | 677.500 | 271.500 | 1.966 | 0.049251 |
| dif transferrin | 854.000 | 742.000 | 336.000 | 0.90947 | 0.363103 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sokal, P.; Broda, M.; Zając, M.; Sokal, J. Earthing as a Supportive Therapy for Post-Spinal Surgery Recovery. J. Clin. Med. 2025, 14, 3844. https://doi.org/10.3390/jcm14113844
Sokal P, Broda M, Zając M, Sokal J. Earthing as a Supportive Therapy for Post-Spinal Surgery Recovery. Journal of Clinical Medicine. 2025; 14(11):3844. https://doi.org/10.3390/jcm14113844
Chicago/Turabian StyleSokal, Paweł, Maciej Broda, Magdalena Zając, and Julia Sokal. 2025. "Earthing as a Supportive Therapy for Post-Spinal Surgery Recovery" Journal of Clinical Medicine 14, no. 11: 3844. https://doi.org/10.3390/jcm14113844
APA StyleSokal, P., Broda, M., Zając, M., & Sokal, J. (2025). Earthing as a Supportive Therapy for Post-Spinal Surgery Recovery. Journal of Clinical Medicine, 14(11), 3844. https://doi.org/10.3390/jcm14113844







