Integrative Postural Rehabilitation for Kyphotic Deformity in a Patient with Parkinson’s Disease: A Case Report and Literature Review
Abstract
1. Introduction
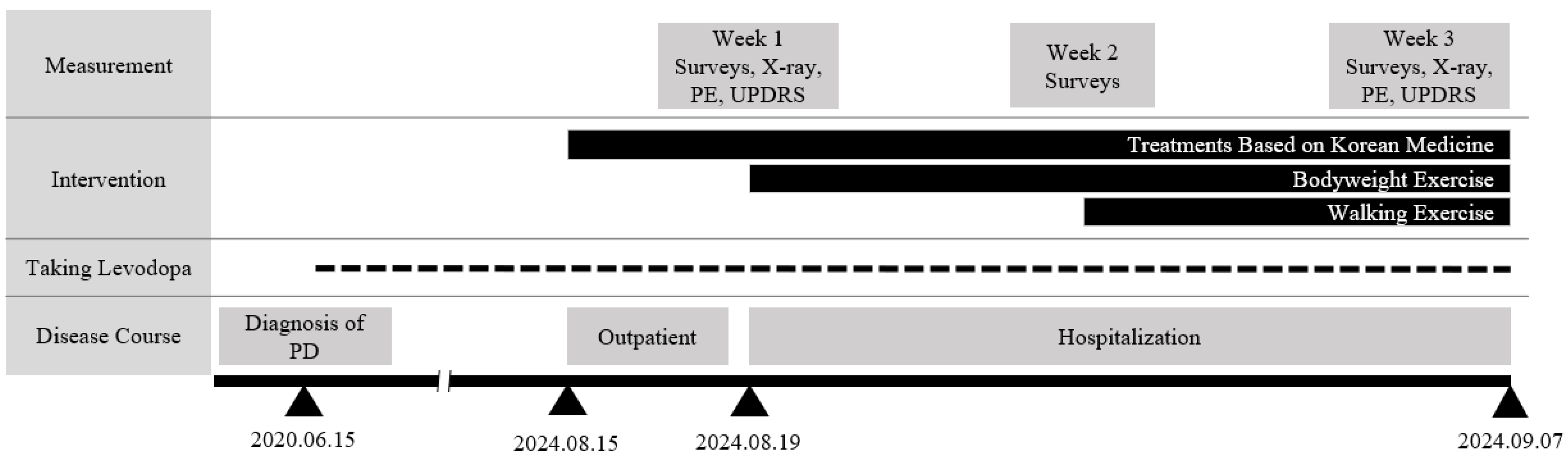
2. Case Presentation
2.1. Patient Characteristics
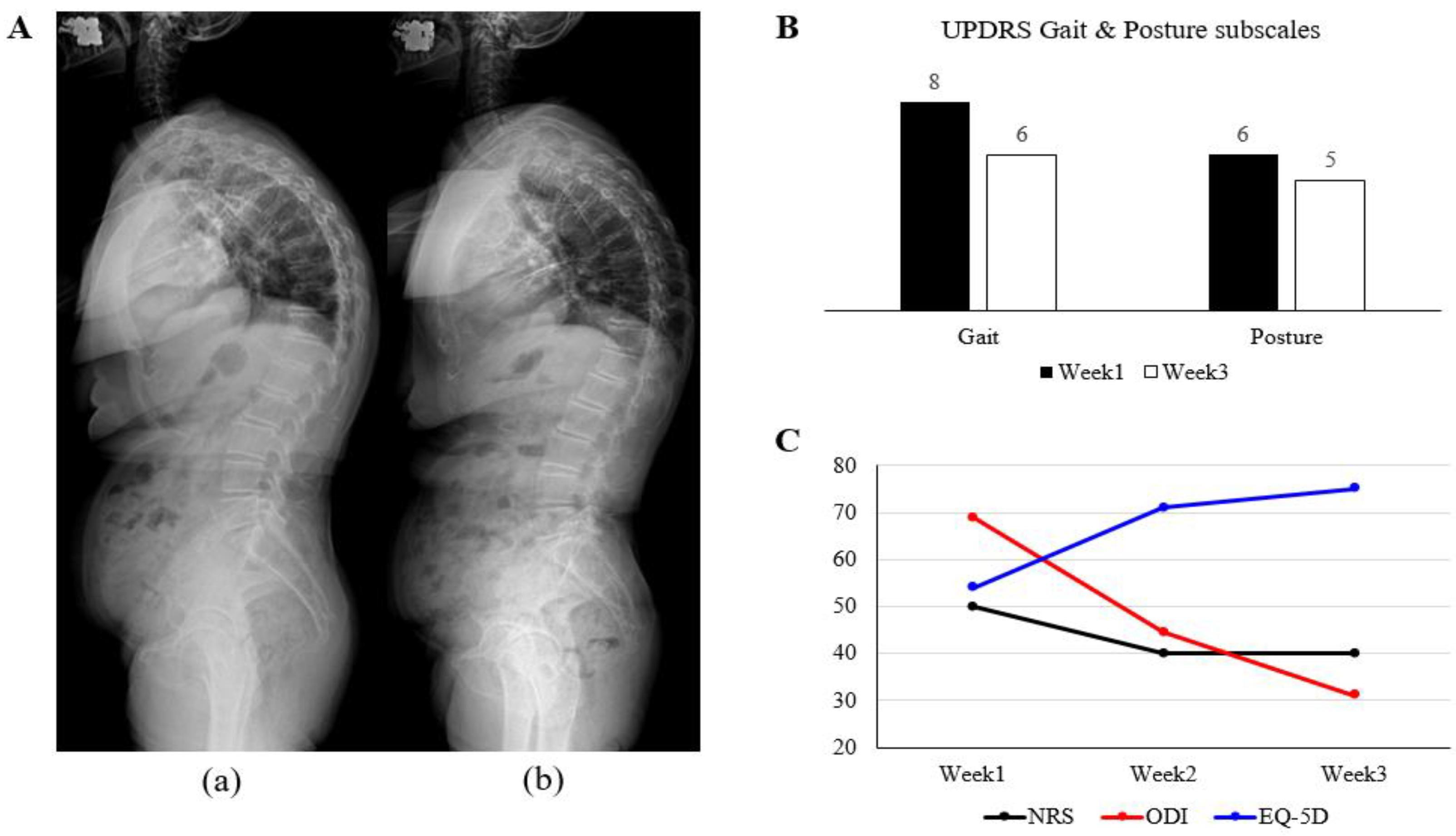
2.2. Diagnosis & Outcome Measurement
2.3. Interventions
2.4. Course of Symptoms and Outcomes
2.5. Review of Literature
3. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| EQ-5D | EuroQol-5 Dimension; |
| MDS-UPDRS | Movement Disorder Society-Unified Parkinson’s Disease Rating Scale |
| NRS | numerical rating scale |
| ODI | Oswestry Disability Index |
| PD | Parkinson disease |
| QoL | quality of life |
| RCT | randomized controlled trial |
| ROM | range of motion |
| SVA | sagittal vertical axis |
| TK | thoracolumbar kyphosis |
Appendix A

| Herbal Medicine | Compositions |
|---|---|
| Jaseng Gongjin-Dan | Cervus nipponT., Aquilaria agallocha, Cornus officinalis, Angelica gigas Nakai |
| Doinseunggi-tang | Rheum palmatum, Cinnamomum cassia Blume, Glycyrrhiza uralensis, Erigeron canadensis L. |
| Medication | Compositions |
| Perkin | 100 mg 4.5T #3 |
| Fosamax | 70 mg 1T #1 |
| Synthyroxine | 1T #1 |
| Tenelia M | 10/500 mg 1T #1 |
| Livalo | 1T #1 |
| Ganakhan | 50 mg 1T #1 (Take PRN) |
| Phazyme | 95 mg 1T #1 (Take PRN) |
| Stogar | 10 mg 1T #1 (Take PRN) |
| Exercise Checklist | |||
|---|---|---|---|
| Exercise | Illustrated Guide | ||
| Core muscle exercises | Supine position | Abdominal breathing exercise |  |
| Prone position | Deep erector spinae strengthening exercise | 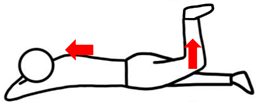 | |
| Gluteus maximus strengthening exercise | |||
| Thoracic mobility exercises | Seated position | External oblique Abdominal muscle strengthening exercise | 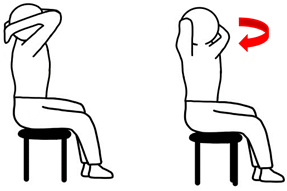 |
| Serratus anterior strengthening exercise | 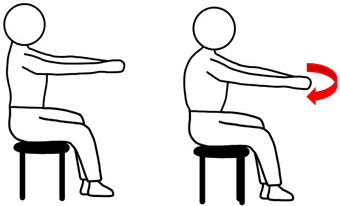 | ||
References
- Ashour, R.; Jankovic, J. Joint and skeletal deformities in Parkinson’s disease, multiple system atrophy, and progressive supranuclear palsy. Mov. Disord. Off. J. Mov. Disord. Soc. 2006, 21, 1856–1863. [Google Scholar] [CrossRef] [PubMed]
- Baik, J.S. Understanding of skeletal deformities in Parkinson’s disease. Indian J. Med. Res. 2016, 144, 650–652. [Google Scholar] [CrossRef] [PubMed]
- Bissolotti, L.; Berjano, P.; Zuccher, P.; Zenorini, A.; Buraschi, R.; Villafañe, J.H.; Negrini, S. Sagittal balance is correlated with Parkinson’s Disease clinical parameters: An overview of spinopelvic alignment on 175 consecutive cases. Eur. Spine J. 2017, 26, 471–478. [Google Scholar] [CrossRef]
- Schrag, A.; Jahanshahi, M.; Quinn, N. What contributes to quality of life in patients with Parkinson’s disease? J. Neurol. Neurosurg. Psychiatry 2000, 69, 308–312. [Google Scholar] [CrossRef] [PubMed]
- Schrag, A.; Ben-Shlomo, Y.; Quinn, N. How common are complications of Parkinson’s disease? J. Neurol. 2002, 249, 419–423. [Google Scholar] [CrossRef]
- Ganz, D.A.; Bao, Y.; Shekelle, P.G.; Rubenstein, L.Z. Will my patient fall? JAMA 2007, 297, 77–86. [Google Scholar] [CrossRef]
- van der Heeden, J.F.; Marinus, J.; Martinez-Martin, P.; Rodriguez-Blazquez, C.; Geraedts, V.J.; van Hilten, J.J. Postural instability and gait are associated with severity and prognosis of Parkinson disease. Neurology 2016, 86, 2243–2250. [Google Scholar] [CrossRef]
- Rizzo, G.; Copetti, M.; Arcuti, S.; Martino, D.; Fontana, A.; Logroscino, G. Accuracy of clinical diagnosis of Parkinson disease: A systematic review and meta-analysis. Neurology 2016, 86, 566–576. [Google Scholar] [CrossRef]
- Palakurthi, B.; Burugupally, S.P. Postural instability in Parkinson’s disease: A review. Brain Sci. 2019, 9, 239. [Google Scholar] [CrossRef]
- Lenoir, T.; Guedj, N.; Boulu, P.; Guigui, P.; Benoist, M. Camptocormia: The bent spine syndrome, an update. Eur. Spine J. 2010, 19, 1229–1237. [Google Scholar] [CrossRef]
- Sakai, W.; Nakane, S.; Urasaki, E.; Toyoda, K.; Sadakata, E.; Nagaishi, A.; Fukudome, T.; Yamakawa, Y.; Matsuo, H. The cross-sectional area of paraspinal muscles predicts the efficacy of deep brain stimulation for camptocormia. J. Park. Dis. 2017, 7, 247–253. [Google Scholar] [CrossRef] [PubMed]
- Babat, L.B.; McLain, R.F.; Bingaman, W.; Kalfas, I.; Young, P.; Rufo-Smith, C. Spinal surgery in patients with Parkinson’s disease: Construct failure and progressive deformity. Spine 2004, 29, 2006–2012. [Google Scholar] [CrossRef]
- Chan, A.K.; Chan, A.Y.; Lau, D.; Durcanova, B.; Miller, C.A.; Larson, P.S.; Starr, P.A.; Mummaneni, P.V. Surgical management of camptocormia in Parkinson’s disease: Systematic review and meta-analysis. J. Neurosurg. 2018, 131, 368–375. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.H.; Lee, J.M.; Lee, E.J.; Oh, M.S. Effects of Daoyin Exercise Therapy Combined with Korean Medicine Treatment on the Pain and Function Improvement of Low Back Pain Patients Diagnosed with Lumbar Disc Herniation: A Retrospective Observational Study. J. Physiol. Pathol. Korean Med. 2017, 31, 238–245. [Google Scholar] [CrossRef]
- Terashi, H.; Endo, K.; Aizawa, H. Characteristics of sagittal spinopelvic alignment in patients with Parkinson’s disease presenting with dropped head syndrome: A case series study. BMC Neurol. 2023, 23, 173. [Google Scholar] [CrossRef]
- Uehara, M.; Takahashi, J.; Ikegami, S.; Tokida, R.; Nishimura, H.; Sakai, N.; Kato, H. Sagittal spinal alignment deviation in the general elderly population: A Japanese cohort survey randomly sampled from a basic resident registry. Spine J. 2019, 19, 349–356. [Google Scholar] [CrossRef]
- Goetz, C.G.; Poewe, W.; Dubois, B.; Schrag, A.; Stern, M.; Lang, A. MDS-Unified Parkinson’s Disease Rating Scale (MDS-UPDRS). 2008. Available online: https://www.movementdisorders.org/MDS/MDS-Rating-Scales/MDS-Unified-Parkinsons-Disease-Rating-Scale-MDS-UPDRS.htm (accessed on 1 August 2024).
- Fairbank, J.C.; Pynsent, P.B. The Oswestry disability index. Spine 2000, 25, 2940–2953. [Google Scholar] [CrossRef]
- Balestroni, G.; Bertolotti, G. EuroQol-5D (EQ-5D): An instrument for measuring quality of life. Monaldi Arch. Chest Dis. 2012, 78, 155–159. [Google Scholar] [CrossRef] [PubMed]
- Seo, B.K. Korean Medicine Clinical Practice Guideline for lumbar disc herniation; National Institute for Korean Medicine Development: Seoul, Republic of Korea, 2020. [Google Scholar]
- Zhao, Y.; Zhang, Z.; Qin, S.; Fan, W.; Li, W.; Liu, J.; Wang, S.; Xu, Z.; Zhao, M. Acupuncture for Parkinson’s disease: Efficacy evaluation and mechanisms in the dopaminergic neural circuit. Neural Plast. 2021, 2021, 9926445. [Google Scholar] [CrossRef]
- Kim, S.-N.; Doo, A.-R.; Park, J.-Y.; Bae, H.; Chae, Y.; Shim, I.; Lee, H.; Moon, W.; Lee, H.; Park, H.-J. Acupuncture enhances the synaptic dopamine availability to improve motor function in a mouse model of Parkinson’s disease. PLoS ONE 2011, 6, e27566. [Google Scholar] [CrossRef]
- Yan, L.; Zhang, J.; Wang, X.; Zhou, Q.; Wen, J.; Zhao, H.; Guo, K.; Zeng, J. Efficacy of acupuncture for lumbar disc herniation: Changes in paravertebral muscle and fat infiltration–a multicenter retrospective cohort study. Front. Endocrinol. 2024, 15, 1467769. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.; Baek, G.G.; Shin, B.-C. An Umbrella Review of Systematic Reviews for Chuna (or Tuina) Manual Therapy on Musculoskeletal Disorders. Perspect. Integr. Med. 2023, 2, 142–154. [Google Scholar] [CrossRef]
- Capecci, M.; Serpicelli, C.; Fiorentini, L.; Censi, G.; Ferretti, M.; Orni, C.; Renzi, R.; Provinciali, L.; Ceravolo, M.G. Postural rehabilitation and Kinesio taping for axial postural disorders in Parkinson’s disease. Arch. Phys. Med. Rehabil. 2014, 95, 1067–1075. [Google Scholar] [CrossRef]
- Morrone, M.; Miccinilli, S.; Bravi, M.; Paolucci, T.; Melgari, J.M.; Salomone, G.; Picelli, A.; Spadini, E.; Ranavolo, A.; Saraceni, V.M. Perceptive rehabilitation and trunk posture alignment in patients with Parkinson disease: A single blind randomized controlled trial. Eur. J. Phys. Rehabil. Med. 2016, 52, 799–809. [Google Scholar]
- Romanato, M.; Guiotto, A.; Spolaor, F.; Bakdounes, L.; Baldassarre, G.; Cucca, A.; Peppe, A.; Volpe, D.; Sawacha, Z. Changes of biomechanics induced by Equistasi® in Parkinson’s disease: Coupling between balance and lower limb joints kinematics. Med. Biol. Eng. Comput. 2021, 59, 1403–1415. [Google Scholar] [CrossRef]
- Doherty, K.M.; Van De Warrenburg, B.P.; Peralta, M.C.; Silveira-Moriyama, L.; Azulay, J.-P.; Gershanik, O.S.; Bloem, B.R. Postural deformities in Parkinson’s disease. Lancet Neurol. 2011, 10, 538–549. [Google Scholar] [CrossRef]
- Schulz-Schaeffer, W.J.; Margraf, N.G.; Munser, S.; Wrede, A.; Buhmann, C.; Deuschl, G.; Oehlwein, C. Effect of neurostimulation on camptocormia in Parkinson’s disease depends on symptom duration. Mov. Disord. 2015, 30, 368–372. [Google Scholar] [CrossRef] [PubMed]
- Schulz-Schaeffer, W.J. Camptocormia in Parkinson’s disease: A muscle disease due to dysregulated proprioceptive polysynaptic reflex arch. Front. Aging Neurosci. 2016, 8, 128. [Google Scholar] [CrossRef]
- Chatilow, L.; DeLany, J. Clinical Application of Neuromuscular Techniques: The Lower Body; Churchill Livingstone: Edinburgh, UK, 2002; Volume 2. [Google Scholar]
- Minakawa, Y.; Miyazaki, S.; Waki, H.; Yoshida, N.; Iimura, K.; Itoh, K. Trigger point acupuncture and exercise for chronic low back pain in older adult: A preliminary randomized clinical trial. J. Acupunct. Meridian Stud. 2022, 15, 143–151. [Google Scholar] [CrossRef]
- Castro-Sánchez, A.M.; Matarán-Penarrocha, G.A.; Arroyo-Morales, M.; Saavedra-Hernández, M.; Fernández-Sola, C.; Moreno-Lorenzo, C. Effects of myofascial release techniques on pain, physical function, and postural stability in patients with fibromyalgia: A randomized controlled trial. Clin. Rehabil. 2011, 25, 800–813. [Google Scholar] [CrossRef]
- Sun, Y.; Li, L.; Chen, Y.; Wang, L.; Zhai, L.; Sheng, J.; Liu, T.; Jin, X. Feasibility and positive effects of scalp acupuncture for modulating motor and cerebral activity in Parkinson’s disease: A pilot study. NeuroRehabilitation 2022, 51, 467–479. [Google Scholar] [CrossRef] [PubMed]
- Yeo, S.; Lim, S.; Choe, I.H.; Choi, Y.G.; Chung, K.C.; Jahng, G.H.; Kim, S.H. Acupuncture Stimulation on GB 34 Activates Neural Responses Associated with P arkinson’s Disease. CNS Neurosci. Ther. 2012, 18, 781–790. [Google Scholar] [CrossRef] [PubMed]
- Chae, Y.; Lee, H.; Kim, H.; Kim, C.H.; Chang, D.I.; Kim, K.M.; Park, H.J. Parsing brain activity associated with acupuncture treatment in Parkinson’s diseases. Mov. Disord. 2009, 24, 1794–1802. [Google Scholar] [CrossRef]
- Gu, H.; Hong, J.; Wang, Z.; Chen, J.; Yuan, F.; Jiang, Y.; Yang, Y.; Luo, M.; Zhang, Z.; He, B. Association of MRI findings with paraspinal muscles fat infiltration at lower lumbar levels in patients with chronic low back pain: A multicenter prospective study. BMC Musculoskelet. Disord. 2024, 25, 549. [Google Scholar]
- Lv, Y.; Dai, D.-C.; Jiang, H.-N.; Wang, L. Effect of electroacupuncture on lumbar disc herniation with different multifidus fatty infiltration rates. Zhongguo Zhen Jiu = Chin. Acupunct. Moxibustion 2021, 41, 593–597. [Google Scholar]
- Yang, Q.; Wang, Y.; Zhao, C.; Pang, S.; Lu, J.; Chan, P. α-Synuclein aggregation causes muscle atrophy through neuromuscular junction degeneration. J. Cachexia Sarcopenia Muscle 2023, 14, 226–242. [Google Scholar] [CrossRef]
- Symons, T.B.; Park, J.; Kim, J.H.; Kwon, E.H.; Delacruz, J.; Lee, J.; Park, Y.; Chung, E.; Lee, S. Attenuation of skeletal muscle atrophy via acupuncture, electro-acupuncture, and electrical stimulation. Integr. Med. Res. 2023, 12, 100949. [Google Scholar] [CrossRef] [PubMed]
- Song, S.Y.; No, J.Y.; Seol, J.Y. A Case Report of Scalp Acupuncture and Chuna Manual Therapy for a Patient with Idiopathic Parkinson’s Disease with Walking Disorders due to Lower Extremity Rigidity. J. Intern. Korean Med. 2023, 44, 894–903. [Google Scholar] [CrossRef]
- Saur, P.M.; Ensink, F.-B.M.; Frese, K.; Seeger, D.; Hildebrandt, J. Lumbar range of motion: Reliability and validity of the inclinometer technique in the clinical measurement of trunk flexibility. Spine 1996, 21, 1332–1338. [Google Scholar] [CrossRef]
- Yao, Y.; Zhenni, Z.; Fengqin, C.; Yufei, L.; Xiangtian, P.; Xiao, X.; Zhiling, S. Effectiveness of moxibustion alone on lumbar disc herniation: A Meta-analysis of randomized controlled trials. J. Tradit. Chin. Med. 2023, 43, 14. [Google Scholar]
- Chen, J.; Xu, J.; Huang, P.; Luo, Y.; Shi, Y.; Ma, P. The potential applications of traditional Chinese medicine in Parkinson’s disease: A new opportunity. Biomed. Pharmacother. 2022, 149, 112866. [Google Scholar] [CrossRef] [PubMed]
- Mazhar, T.; Jameel, A.; Sharif, F.; Asghar, M. Effects of conventional physical therapy with and without proprioceptive neuromuscular facilitation on balance, gait, and function in patients with Parkinson’s disease. J. Pak. Med. Assoc. 2023, 73, 1280–1283. [Google Scholar] [CrossRef] [PubMed]
- Luan, L.; Zhu, M.; Adams, R.; Witchalls, J.; Pranata, A.; Han, J. Effects of acupuncture or similar needling therapy on pain, proprioception, balance, and self-reported function in individuals with chronic ankle instability: A systematic review and meta-analysis. Complement. Ther. Med. 2023, 77, 102983. [Google Scholar] [CrossRef] [PubMed]
- Han, J.; Adams, R.; Waddington, G. “Imposed” and “obtained” ankle proprioception across the life span—Commentary on Djajadikarta et al. J. Appl. Physiol. 2020, 129, 533–534. [Google Scholar] [CrossRef]
| Intervention | Details |
|---|---|
| Acupuncture | GV16, GV20, GB20, GB34 Ashi points in back pain Trigger points of erector spinae (thoracic and lumbar region), sacrotuberous ligament, gluteus maximus, gluteus medius, gluteus minimus, iliopsoas muscle, biceps femoris, gastrocnemius, quadratus lumborum and sternocleidomastoid |
| Pharmacopuncture | Shinbaro2 A intramuscular injections |
| Electroacupuncture | Both sides of GB20 Paraspinal muscles |
| Chuna spinal manual therapy | Joint mobilization therapy Joint distraction therapy Fascia (soft tissue) therapy Joint manipulation therapy Craniosacral therapy |
| Other treatment | Moxibustion, cupping, infrared therapy, hot pack therapy |
| Contents | Details | Intensity | Time | |
|---|---|---|---|---|
| Core muscle exercises | Abdominal breathing | While keeping the knees bent, breathe in deeply, slowly expanding the abdomen without using the chest or neck muscles. Then, exhale slowly, pulling the abdomen in as you fully release the breath. | Without causing pain for 5–10 s | 20 min |
| Deep erector spinae strengthening | While maintaining abdominal breathing in a prone position, move with the feeling of lifting the hips and deep lower back towards the head as you exhale. | |||
| Gluteus maximus strengthening | While lying in a prone position, bend one knee and, using only the glute muscles, lift your leg slightly as you exhale. Hold this position for 5 s. | |||
| Thoracic mobility exercises | External oblique abdominal muscle strengthening | Sit with feet flat on the ground and pelvis in a neutral position. Then, clasp hands behind the head and rotate only the upper body left and right. | Increase intensity by count up to 30 | 20 min |
| Serratus anterior strengthening | Sit with feet flat on the ground and pelvis in a neutral position. Then, extend arms straight in front of the chest, clasp hands together, and rotate only the upper body left and right. | |||
| Radiographic Index | Range of Thoracolumbar motion (degree) | |||||
|---|---|---|---|---|---|---|
| TK (°) | SVA (mm) | Flexion | Extension | Lat. Bending (Rt./Lt.) | Rotation (Rt./Lt.) | |
| Week 1 | 77.7 | 95.55 | 60 | 10 | 10/10 | 45/45 |
| Week 3 | 61.1 | 77.84 | 60 | 20 | 15/15 | 45/45 |
| Target Deformity [reference] | N. of Participants (Female, Mean Age [years]) | Intervention (Control) | Intervention Category (period) | Measurement | Result |
|---|---|---|---|---|---|
| Thoracic bending [25] | 20 (9, 69.1) | (1) GPR (2) GPR + KT (no treatment) | Exercise, sensory stimulation (4 weeks) Bracing (4 weeks) | (1) Angle of anterior and lateral bending of the trunk (2) BBS, TUG | (1) Angle of anterior bending: p < 0.01, angle of lateral bending: NS (2) BBS, TUG: p < 0.01 |
| Thoracic and lumbar bending [26] | 20 (8, 72.5) | Su-Per (physical therapy) | Sensory stimulation (4 weeks) | (1) Kyphosis and lordosis angles (2) Steps cadence, stride length, normalized velocity | (1) Kyphosis angle: p < 0.009, Lordosis angle: NS (2) Gait measurement: NS |
| Thoracic bending [27] | 24 (9, 67.5) | Equistasi® (usual care) | Sensory stimulation (8 weeks) | (1) Postural analysis during the gait cycle (2) UPDRS (gait scale) | (1) Trunk forward Bending: p < 0.05 (2) UPDRS (gait scale): NS |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yun, Y.-R.; Yeom, J.-S.; Lee, J.-S.; Kim, D.; Lee, Y.J.; Ha, I.-H.; Kim, D.-Y. Integrative Postural Rehabilitation for Kyphotic Deformity in a Patient with Parkinson’s Disease: A Case Report and Literature Review. J. Clin. Med. 2025, 14, 3705. https://doi.org/10.3390/jcm14113705
Yun Y-R, Yeom J-S, Lee J-S, Kim D, Lee YJ, Ha I-H, Kim D-Y. Integrative Postural Rehabilitation for Kyphotic Deformity in a Patient with Parkinson’s Disease: A Case Report and Literature Review. Journal of Clinical Medicine. 2025; 14(11):3705. https://doi.org/10.3390/jcm14113705
Chicago/Turabian StyleYun, Ye-Rim, Ji-Sung Yeom, Joon-Seok Lee, Doori Kim, Yoon Jae Lee, In-Hyuk Ha, and Do-Young Kim. 2025. "Integrative Postural Rehabilitation for Kyphotic Deformity in a Patient with Parkinson’s Disease: A Case Report and Literature Review" Journal of Clinical Medicine 14, no. 11: 3705. https://doi.org/10.3390/jcm14113705
APA StyleYun, Y.-R., Yeom, J.-S., Lee, J.-S., Kim, D., Lee, Y. J., Ha, I.-H., & Kim, D.-Y. (2025). Integrative Postural Rehabilitation for Kyphotic Deformity in a Patient with Parkinson’s Disease: A Case Report and Literature Review. Journal of Clinical Medicine, 14(11), 3705. https://doi.org/10.3390/jcm14113705










