Risk Factor Analysis for Proximal Junctional Kyphosis in Neuromuscular Scoliosis: A Single-Center Study
Abstract
1. Introduction
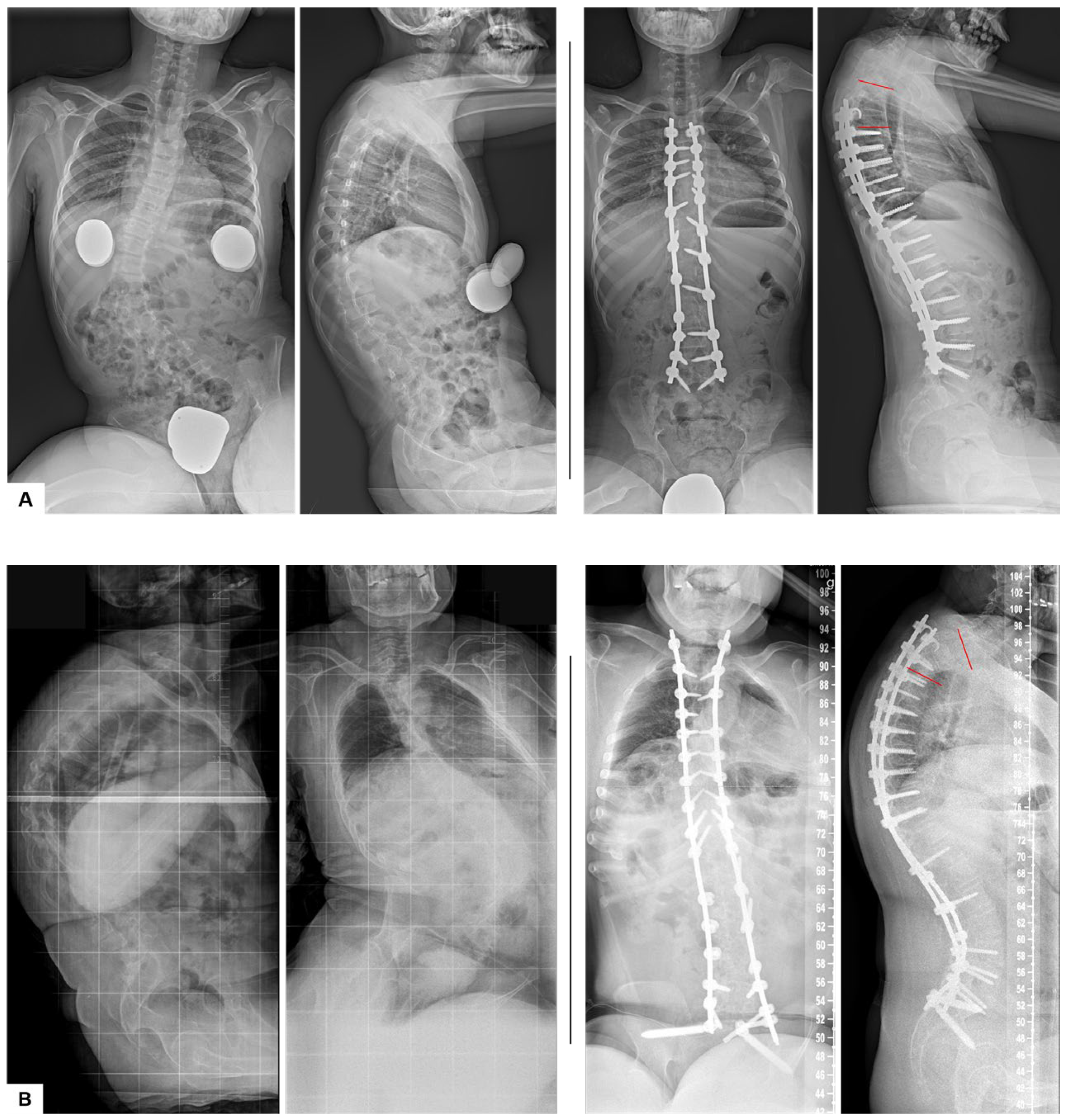
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AIS | Adolescent Idiopathic Scoliosis |
| BMI | Body Mass Index |
| FU | Follow-Up |
| LL | Lumbar Lordosis |
| LIV | Lower Instrumented Vertebra |
| NMS | Neuromuscular Scoliosis |
| OR | Odds Ratio |
| PACS | Picture Archiving and Communication System |
| PI | Pelvic Incidence |
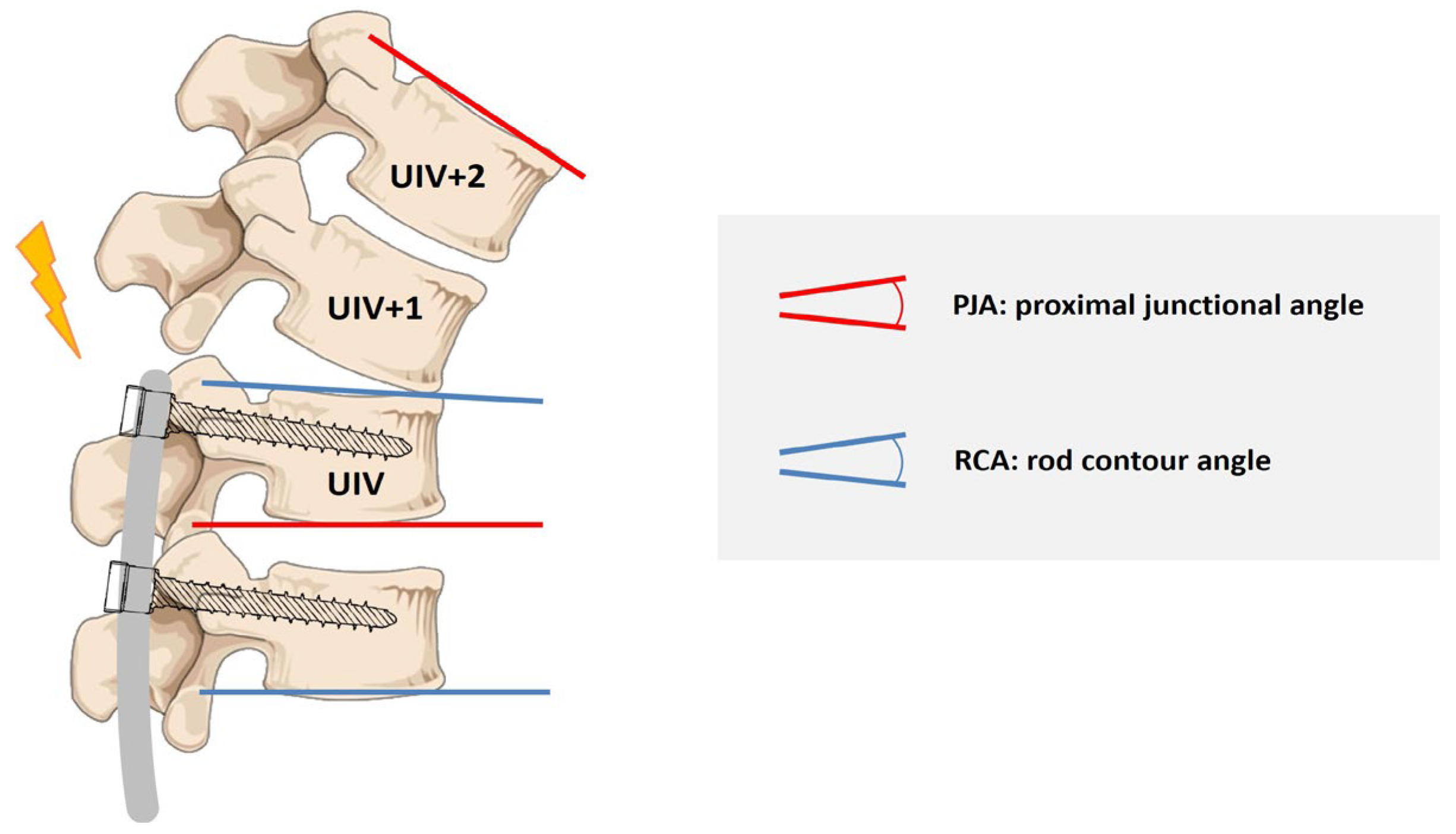
| PJA | Proximal Junctional Angle |
| PJF | Proximal Junctional Failure |
| PJK | Proximal Junctional Kyphosis |
| postOP | Postoperative |
| preOP | Preoperative |
| PT | Pelvic Tilt |
| RCA | Rod Contour Angle |
| SD | Standard Deviation |
| SL | Sacral Slope |
| SPSS | Statistical Package for the Social Sciences |
| SVA | Sagittal Vertical Axis |
| TK | Thoracic Kyphosis |
| UIV | Upper Instrumented Vertebra |
| VEPTR™ | Vertical Expandable Prosthetic Titanium Rib |
| MAGEC™ | MAGnetic Expansion Control Rods |
References
- Yaszay, B.; Coe, K.M.; Scannell, B.P. Neuromuscular Scoliosis: An Overview. In The Growing Spine; Akbarnia, B.A., Thompson, G.H., Yazici, M., El-Hawary, R., Eds.; Springer: Cham, Switzerland, 2022. [Google Scholar] [CrossRef]
- Allam, A.M.; Schwabe, A.L. Neuromuscular scoliosis. PMR 2013, 5, 957–963. [Google Scholar] [CrossRef] [PubMed]
- Duncan, C.; Maenza, S.; Schmid, C.; Segal, E.; Couto, J. Gait Disorders in Patients with Instrumented Neuromuscular Scoliosis. Coluna/Columna 2019, 18, 272–275. [Google Scholar] [CrossRef]
- Modi, H.N.; Suh, S.W.; Song, H.R.; Fernandez, H.M.; Yang, J.H. Treatment of neuromuscular scoliosis with posterior-only pedicle screw fixation. J. Orthop. Surg. Res. 2008, 3, 23. [Google Scholar] [CrossRef] [PubMed]
- Montero, C.; Meneses, D.; Godoy, W.; Alvarado, F.; Acosta, M. Evaluation of the VEPTR (Vertical Expandable Prosthetic Titanium Rib) Device in the Treatment of Patients with Congenital and Neuromuscular Spinal Deformities. Glob. Spine J. 2017, 5, s-0035-1554432. [Google Scholar] [CrossRef]
- White, K.K.; Song, K.M.; Frost, N.; Daines, B.K. VEPTR growing rods for early-onset neuromuscular scoliosis: Feasible and effective. Clin. Orthop. Relat. Res. 2011, 469, 1335–1341. [Google Scholar] [CrossRef]
- Piazzolla, A.; Solarino, G.; De Giorgi, S.; Mori, C.M.; Moretti, L.; De Giorgi, G. Cotrel-Dubousset instrumentation in neuromuscular scoliosis. Eur. Spine J. 2011, 20, S75–S84. [Google Scholar] [CrossRef]
- Lampe, L.P.; Schulze Bovingloh, A.; Gosheger, G.; Schulte, T.L.; Lange, T. Magnetically Controlled Growing Rods in Treatment of Early-Onset Scoliosis: A Single Center Study With a Minimum of 2-Year-Follow up and Preliminary Results After Converting Surgery. Spine 2019, 44, 1201–1210. [Google Scholar] [CrossRef]
- Kim, H.S.; Kwon, J.W.; Park, K.B. Clinical Issues in Indication, Correction, and Outcomes of the Surgery for Neuromuscular Scoliosis: Narrative Review in Pedicle Screw Era. Neurospine 2022, 19, 177–187. [Google Scholar] [CrossRef]
- Protopsaltis, T.S.; Boniello, A.J.; Schwab, F.J. Management of Spinal Deformity in Adult Patients With Neuromuscular Disease. J. Am. Acad. Orthop. Surg. 2016, 24, 634–644. [Google Scholar] [CrossRef]
- Turturro, F.; Montanaro, A.; Calderaro, C.; Labianca, L.; Di Sanzo, V.; Ferretti, A. Rate of complications due to neuromuscular scoliosis spine surgery in a 30-years consecutive series. Eur. Spine J. 2017, 26, 539–545. [Google Scholar] [CrossRef]
- Cognetti, D.; Keeny, H.M.; Samdani, A.F.; Pahys, J.M.; Hanson, D.S.; Blanke, K.; Hwang, S.W. Neuromuscular scoliosis complication rates from 2004 to 2015: A report from the Scoliosis Research Society Morbidity and Mortality database. Neurosurg. Focus 2017, 43, E10. [Google Scholar] [CrossRef] [PubMed]
- Brooks, J.T.; Sponseller, P.D. What’s New in the Management of Neuromuscular Scoliosis. J. Pediatr. Orthop. 2016, 36, 627–633. [Google Scholar] [CrossRef]
- Sharma, S.; Wu, C.; Andersen, T.; Wang, Y.; Hansen, E.S.; Bunger, C.E. Prevalence of complications in neuromuscular scoliosis surgery: A literature meta-analysis from the past 15 years. Eur. Spine J. 2013, 22, 1230–1249. [Google Scholar] [CrossRef]
- Deveza, L.R.; Chhabra, B.N.; Heydemann, J.; Hung, C.; Vanorny, D.; Birhiray, D.; Dahl, B. Comparison of baseline characteristics and postoperative complications in neuromuscular, syndromic and congenital scoliosis. J. Pediatr. Orthop. B 2023, 32, 350–356. [Google Scholar] [CrossRef]
- Beckmann, K.; Lange, T.; Gosheger, G.; Bovingloh, A.S.; Borowski, M.; Bullmann, V.; Liljenqvist, U.; Schulte, T.L. Surgical correction of scoliosis in patients with severe cerebral palsy. Eur. Spine J. 2016, 25, 506–516. [Google Scholar] [CrossRef]
- Ha, Y.; Maruo, K.; Racine, L.; Schairer, W.W.; Hu, S.S.; Deviren, V.; Burch, S.; Tay, B.; Chou, D.; Mummaneni, P.V.; et al. Proximal junctional kyphosis and clinical outcomes in adult spinal deformity surgery with fusion from the thoracic spine to the sacrum: A comparison of proximal and distal upper instrumented vertebrae. J. Neurosurg. Spine 2013, 19, 360–369. [Google Scholar] [CrossRef]
- Cho, S.K.; Kim, Y.J.; Lenke, L.G. Proximal Junctional Kyphosis Following Spinal Deformity Surgery in the Pediatric Patient. J. Am. Acad. Orthop. Surg. 2015, 23, 408–414. [Google Scholar] [CrossRef]
- Passias, P.G.; Krol, O.; Williamson, T.K.; Lafage, V.; Lafage, R.; Smith, J.S.; Line, B.; Vira, S.; Lipa, S.; Daniels, A.; et al. The Benefit of Addressing Malalignment in Revision Surgery for Proximal Junctional Kyphosis Following ASD Surgery. Spine 2023, 48, 1581–1587. [Google Scholar] [CrossRef]
- Lonstein, J.E.; Koop, S.E.; Novachek, T.F.; Perra, J.H. Results and complications after spinal fusion for neuromuscular scoliosis in cerebral palsy and static encephalopathy using luque galveston instrumentation: Experience in 93 patients. Spine 2012, 37, 583–591. [Google Scholar] [CrossRef]
- Toll, B.J.; Gandhi, S.V.; Amanullah, A.; Samdani, A.F.; Janjua, M.B.; Kong, Q.; Pahys, J.M.; Hwang, S.W. Risk Factors for Proximal Junctional Kyphosis Following Surgical Deformity Correction in Pediatric Neuromuscular Scoliosis. Spine 2021, 46, 169–174. [Google Scholar] [CrossRef]
- Kim, H.J.; Iyer, S. Proximal Junctional Kyphosis. J. Am. Acad. Orthop. Surg. 2016, 24, 318–326. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Yang, J.H.; Chang, D.G.; Suk, S.I.; Suh, S.W.; Kim, S.I.; Song, K.S.; Park, J.B.; Cho, W. Proximal Junctional Kyphosis in Adult Spinal Deformity: Definition, Classification, Risk Factors, and Prevention Strategies. Asian Spine J. 2022, 16, 440–450. [Google Scholar] [CrossRef] [PubMed]
- Menger, R.; Park, P.J.; Bixby, E.C.; Marciano, G.; Cerpa, M.; Roye, D.; Roye, B.D.; Vitale, M.; Lenke, L. Complications in ambulatory pediatric patients with nonidiopathic spinal deformity undergoing fusion to the pelvis using the sacral-alar-iliac technique within 2 years of surgery. J. Neurosurg. Pediatr. 2021, 28, 13–20. [Google Scholar] [CrossRef]
- Glassman, S.D.; Coseo, M.P.; Carreon, L.Y. Sagittal balance is more than just alignment: Why PJK remains an unresolved problem. Scoliosis Spinal Disord. 2016, 11, 1. [Google Scholar] [CrossRef]
- Denis, F.; Sun, E.C.; Winter, R.B. Incidence and risk factors for proximal and distal junctional kyphosis following surgical treatment for Scheuermann kyphosis: Minimum five-year follow-up. Spine 2009, 34, E729–E734. [Google Scholar] [CrossRef]
- Lee, G.A.; Betz, R.R.; Clements, D.H., 3rd; Huss, G.K. Proximal kyphosis after posterior spinal fusion in patients with idiopathic scoliosis. Spine 1999, 24, 795–799. [Google Scholar] [CrossRef]
- Wang, J.; Yang, N.; Luo, M.; Xia, L.; Li, N. Large Difference Between Proximal Junctional Angle and Rod Contouring Angle is a Risk Factor for Proximal Junctional Kyphosis. World Neurosurg. 2020, 136, e683–e689. [Google Scholar] [CrossRef]
- Lange, T.; Schmoelz, W.; Gosheger, G.; Eichinger, M.; Heinrichs, C.H.; Boevingloh, A.S.; Schulte, T.L. Is a gradual reduction of stiffness on top of posterior instrumentation possible with a suitable proximal implant? A biomechanical study. Spine J. 2017, 17, 1148–1155. [Google Scholar] [CrossRef]
- Erkilinc, M.; Baldwin, K.D.; Pasha, S.; Mistovich, R.J. Proximal junctional kyphosis in pediatric spinal deformity surgery: A systematic review and critical analysis. Spine Deform. 2022, 10, 257–266. [Google Scholar] [CrossRef]
- Han, S.; Hyun, S.J.; Kim, K.J.; Jahng, T.A.; Kim, H.J. Comparative Study Between Cobalt Chrome and Titanium Alloy Rods for Multilevel Spinal Fusion: Proximal Junctional Kyphosis More Frequently Occurred in Patients Having Cobalt Chrome Rods. World Neurosurg. 2017, 103, 404–409. [Google Scholar] [CrossRef]
- Liu, F.Y.; Wang, T.; Yang, S.D.; Wang, H.; Yang, D.L.; Ding, W.Y. Incidence and risk factors for proximal junctional kyphosis: A meta-analysis. Eur. Spine J. 2016, 25, 2376–2383. [Google Scholar] [CrossRef] [PubMed]
- Yan, P.; Bao, H.; Qiu, Y.; Bao, M.; Varghese, J.J.; Sun, X.; Liu, Z.; Zhu, Z.; Qian, B.; Zheng, M.; et al. Mismatch Between Proximal Rod Contouring and Proximal Junctional Angle: A Predisposed Risk Factor for Proximal Junctional Kyphosis in Degenerative Scoliosis. Spine 2017, 42, E280–E287. [Google Scholar] [CrossRef]
- Yang, B.; Xu, L.; Wang, M.; Wang, B.; Zhu, Z.; Qiu, Y.; Sun, X. Unmatched rod contouring at the proximal end predisposes to occurrence of junctional kyphosis in early-onset scoliosis patients undergoing traditional growing rods treatment. BMC Musculoskelet. Disord. 2022, 23, 624. [Google Scholar] [CrossRef]
- Cao, J.; Zhu, W.; Zhang, X.; Bai, Y.; Guo, D.; Yao, Z.; Gao, R. Benefits of fixing 3 proximal vertebral bodies vs. 2 in the treatment of early-onset scoliosis with growing rods. J. Pediatr. Orthop. B 2023, 32, 342–349. [Google Scholar] [CrossRef]
- Boeckenfoerde, K.; Schulze Boevingloh, A.; Gosheger, G.; Bockholt, S.; Lampe, L.P.; Lange, T. Risk Factors of Proximal Junctional Kyphosis in Adolescent Idiopathic Scoliosis—The Spinous Processes and Proximal Rod Contouring. J. Clin. Med. 2022, 11, 6098. [Google Scholar] [CrossRef]
- Yang, B.; Xu, L.; Qiu, Y.; Wang, M.; Du, C.; Wang, B.; Zhu, Z.; Sun, X. Mismatch Between Proximal Rod Contour Angle and Proximal Junctional Angle: A Risk Factor Associated With Proximal Junctional Kyphosis After Growing Rods Treatment for Early-Onset Scoliosis. Res. Sq. 2020. [Google Scholar] [CrossRef]
- Lange, T.; Schulte, T.L.; Gosheger, G.; Schulze Boevingloh, A.; Mayr, R.; Schmoelz, W. Effects of multilevel posterior ligament dissection after spinal instrumentation on adjacent segment biomechanics as a potential risk factor for proximal junctional kyphosis: A biomechanical study. BMC Musculoskelet. Disord. 2018, 19, 57. [Google Scholar] [CrossRef]
- Glattes, R.C.; Bridwell, K.H.; Lenke, L.G.; Kim, Y.J.; Rinella, A.; Edwards, C., 2nd. Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: Incidence, outcomes, and risk factor analysis. Spine 2005, 30, 1643–1649. [Google Scholar] [CrossRef]
- Mika, A.P.; Mesfin, A.; Rubery, P.T.; Molinari, R.; Kebaish, K.M.; Menga, E.N. Proximal Junctional Kyphosis: A Pediatric and Adult Spinal Deformity Surgery Dilemma. JBJS Rev. 2019, 7, e4. [Google Scholar] [CrossRef]
- Sacramento-Dominguez, C.; Vayas-Diez, R.; Coll-Mesa, L.; Parrilla, A.P.; Machado-Calvo, M.; Pinilla, J.A.; Sosa, A.J.; Lopez Gde, L. Reproducibility measuring the angle of proximal junctional kyphosis using the first or the second vertebra above the upper instrumented vertebrae in patients surgically treated for scoliosis. Spine 2009, 34, 2787–2791. [Google Scholar] [CrossRef]
- Akosman, I.; Hirase, T.; Chow, J.L.; Subramanian, T.; Uzzo, R.; Jones, C.H.; Persaud, S.G.; Demopoulos, B.; Tuma, O.; Cunningham, M.; et al. Heterogeneity in the Definitions of Proximal Junctional Kyphosis and Failure in Spinal Deformity Literature: A Tower of Babel. Spine 2024, 50, 485–492. [Google Scholar] [CrossRef] [PubMed]
- Cammarata, M.; Aubin, C.E.; Wang, X.; Mac-Thiong, J.M. Biomechanical risk factors for proximal junctional kyphosis: A detailed numerical analysis of surgical instrumentation variables. Spine 2014, 39, E500–E507. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.J.; Bridwell, K.H.; Lenke, L.G.; Kim, J.; Cho, S.K. Proximal junctional kyphosis in adolescent idiopathic scoliosis following segmental posterior spinal instrumentation and fusion: Minimum 5-year follow-up. Spine 2005, 30, 2045–2050. [Google Scholar] [CrossRef]
- Kim, Y.J.; Lenke, L.G.; Bridwell, K.H.; Kim, J.; Cho, S.K.; Cheh, G.; Yoon, J. Proximal junctional kyphosis in adolescent idiopathic scoliosis after 3 different types of posterior segmental spinal instrumentation and fusions: Incidence and risk factor analysis of 410 cases. Spine 2007, 32, 2731–2738. [Google Scholar] [CrossRef]
- Lonner, B.S.; Ren, Y.; Newton, P.O.; Shah, S.A.; Samdani, A.F.; Shufflebarger, H.L.; Asghar, J.; Sponseller, P.; Betz, R.R.; Yaszay, B. Risk Factors of Proximal Junctional Kyphosis in Adolescent Idiopathic Scoliosis—The Pelvis and Other Considerations. Spine Deform. 2017, 5, 181–188. [Google Scholar] [CrossRef]
- Rhee, J.M.; Bridwell, K.H.; Won, D.S.; Lenke, L.G.; Chotigavanichaya, C.; Hanson, D.S. Sagittal plane analysis of adolescent idiopathic scoliosis: The effect of anterior versus posterior instrumentation. Spine 2002, 27, 2350–2356. [Google Scholar] [CrossRef]
- Koller, H.; Schulte, T.L.; Meier, O.; Koller, J.; Bullmann, V.; Hitzl, W.; Mayer, M.; Lange, T.; Schmucker, J. The influence of isolated thoracoplasty on the evolution of pulmonary function after treatment of severe thoracic scoliosis. Eur. Spine J. 2017, 26, 1765–1774. [Google Scholar] [CrossRef]
- Korkmaz, M.; Akgul, T.; Sariyilmaz, K.; Ozkunt, O.; Dikici, F.; Yazicioglu, O. Effectiveness of posterior structures in the development of proximal junctional kyphosis following posterior instrumentation: A biomechanical study in a sheep spine model. Acta Orthop. Traumatol. Turc. 2019, 53, 385–389. [Google Scholar] [CrossRef]
- Rodnoi, P.; Le, H.; Hiatt, L.; Wick, J.; Barber, J.; Javidan, Y.; Roberto, R.; Klineberg, E.O. Ligament Augmentation With Mersilene Tape Reduces the Rates of Proximal Junctional Kyphosis and Failure in Adult Spinal Deformity. Neurospine 2021, 18, 580–586. [Google Scholar] [CrossRef]
- Battista, C.; Wild, C.; Kreul, S.; Albert, M. Prevention of Proximal Junctional Kyphosis & Failure Using Sublaminar Bands in a Hybrid Construct in Pediatric Kyphosis Deformity. Int. J. Spine Surg. 2018, 12, 644–649. [Google Scholar] [CrossRef]
- Clement, J.L.; Pesenti, S.; Ilharreborde, B.; Morin, C.; Charles, Y.P.; Parent, H.F.; Violas, P.; Szadkowski, M.; Boissiere, L.; Solla, F. Proximal junctional kyphosis is a rebalancing spinal phenomenon due to insufficient postoperative thoracic kyphosis after adolescent idiopathic scoliosis surgery. Eur. Spine J. 2021, 30, 1988–1997. [Google Scholar] [CrossRef] [PubMed]
- Burton, D.A.; Karkenny, A.J.; Schulz, J.F.; Hanstein, R.; Gomez, J.A. Sagittal spinopelvic changes after posterior spinal fusion in adolescent idiopathic scoliosis. J. Child. Orthop. 2020, 14, 544–553. [Google Scholar] [CrossRef]
- Ha, A.S.; Lee, N.; Blake, R.; Mathew, J.; Cerpa, M.; Lenke, L.G. Can spinal deformity patients maintain proper arm positions while undergoing full-body X-ray? Spine Deform. 2021, 9, 387–394. [Google Scholar] [CrossRef]
- Xue, R.; Liu, D.; Shen, Y. The differences in whole-body sagittal alignment between different postures in young, healthy adults. BMC Musculoskelet. Disord. 2020, 21, 696. [Google Scholar] [CrossRef]
- Shakeri, M.; Mahdavi, S.M.; Rikhtehgar, M.; Soleimani, M.; Ghandhari, H.; Jafari, B.; Daneshmand, S. EOS(R) is reliable to evaluate spinopelvic parameters: A validation study. BMC Med. Imaging 2024, 24, 35. [Google Scholar] [CrossRef]
- Basques, B.A.; Long, W.D., 3rd; Golinvaux, N.S.; Bohl, D.D.; Samuel, A.M.; Lukasiewicz, A.M.; Webb, M.L.; Grauer, J.N. Poor visualization limits diagnosis of proximal junctional kyphosis in adolescent idiopathic scoliosis. Spine J. 2017, 17, 784–789. [Google Scholar] [CrossRef]
- Hart, R.; McCarthy, I.; O‘Brien, M.; Bess, S.; Line, B.; Adjei, O.B.; Burton, D.; Gupta, M.; Ames, C.; Deviren, V.; et al. Identification of decision criteria for revision surgery among patients with proximal junctional failure after surgical treatment of spinal deformity. Spine 2013, 38, E1223–E1227. [Google Scholar] [CrossRef]
- Bridwell, K.H.; Lenke, L.G.; Cho, S.K.; Pahys, J.M.; Zebala, L.P.; Dorward, I.G.; Cho, W.; Baldus, C.; Hill, B.W.; Kang, M.M. Proximal junctional kyphosis in primary adult deformity surgery: Evaluation of 20 degrees as a critical angle. Neurosurgery 2013, 72, 899–906. [Google Scholar] [CrossRef]
| Non-PJK Group | PJK Group | p | |
|---|---|---|---|
| age | 16.6 ± 6.78 | 18.5 ± 9.36 | 0.260 |
| BMI | 18.7 ± 5.18 | 17.4 ± 4.78 | 0.282 |
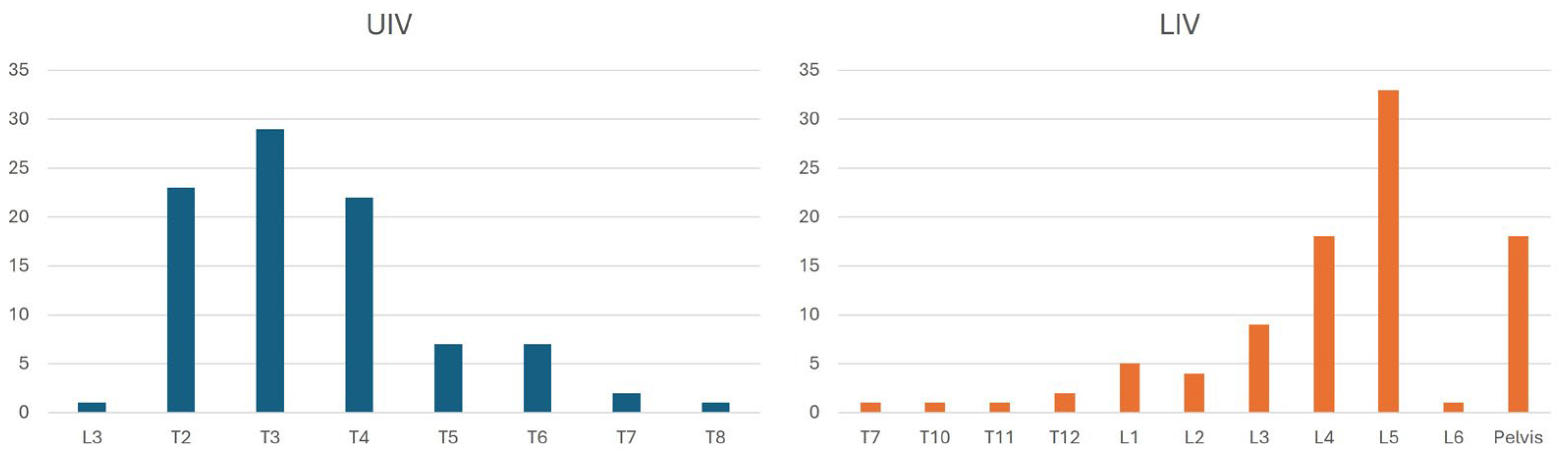
| UIV (median) | T3 | T3 | 0.308 |
| LIV (median) | L5 | L5 | 0.244 |
| instrumented vertebra (n) | 13.8 ± 2.72 | 14.0 ± 2.47 | 0.770 |
| fused segments (n) | 12.7 ± 2.71 | 13.5 ± 2.09 | 0.190 |
| percentage of patients with resected spinous processes | 59.2% | 87.0% | 0.036 |
| resected spinous processes (n) | 7.2 ± 5.65 | 9.4 ± 4.26 | 0.101 |
| Cobb preOP (°) | 81.7 ± 26.38 | 80.7 ± 26.41 | 0.874 |
| Δ Cobb preOP vs. postOP (°) | −42.3 ± 17.84 | −44.3 ± 17.6 | 0.645 |
| TK preOP (°) | 34.5 ± 26.76 | 59.3 ± 29.04 | <0.001 |
| TK postOP (°) | 24.1 ± 14.11 | 38.0 ± 16.48 | <0.001 |
| TK 12 m FU (°) | 24.4 ± 15.15 | 39.2 ± 18.51 | <0.001 |
| Δ TK preOP vs. postOP (°) | −10.7 ± 20.2 | −21.3 ± 19.28 | 0.032 |
| LL preOP (°) | 37.9 ± 28.11 | 41.4 ± 31.91 | 0.625 |
| LL postOP (°) | 37.1 ± 16.59 | 44.0 ± 11.58 | 0.067 |
| LL 12 m FU (°) | 37.7 ± 18.64 | 42.6 ± 17.23 | 0.286 |
| PI (°) | 54.6 ± 22.3 | 48.4 ± 10.55 | 0.486 |
| PT (°) | 10.2 ± 8.76 | 7.3 ± 3.35 | 0.387 |
| SL (°) | 44.4 ± 20.51 | 41.1 ± 11.74 | 0.691 |
| SVA preOP (cm) | 0.4 ± 5.98 | 0.6 ± 2.85 | 0.919 |
| SVA postOP (cm) | 0.1 ± 3.82 | 1.2 ± 5.09 | 0.671 |
| SVA 12 m FU (cm) | 1.0 ± 6.35 | −2.4 ± 2.85 | 0.139 |
| PJA preOP (°) | 3.7 ± 7.93 | 4.2 ± 7.22 | 0.777 |
| PJA postOP (°) | 5.9 ± 6.49 | 14.0 ± 6.31 | <0.001 |
| PJA 12 m FU (°) | 7.3 ± 8.91 | 21.3 ± 10.02 | <0.001 |
| RCA (°) | 7.7 ± 4.34 | 10.2 ± 4.01 | 0.021 |
| postOP PJA-RCA (°) | −1.8 ± 6.55 | 3.78 ± 6.75 | <0.001 |
| 1. | 2. | 3. | 4. | 5. | 6. | |
|---|---|---|---|---|---|---|
| 1 | |||||
| 0.044 | 1 | ||||
| 0.088 | 0.862 ** | 1 | |||
| 0.001 | 0.338 ** | −0.218 * | 1 | ||
| 0.142 | 0.005 | 0.014 | −0.240 * | 1 | |
| 0.224 * | 0.377 ** | −0.235 * | 0.248 * | 0.355 ** | 1 |
| Estimate Coefficient | Odds Ratio (Exp(B)) | p | 95% Confidence Interval | ||
|---|---|---|---|---|---|
| Spinous process resection | 1.848 | 6.346 | 0.036 | 0.769 | 52.396 |
| TK (preOP) | 0.063 | 1.065 | 0.017 | 1.011 | 1.121 |
| ΔTK (pre vs. postOP) | 0.043 | 1.043 | 0.175 | 0.981 | 1.110 |
| RCA (postOP) | 0.137 | 1.147 | 0.094 | 0.977 | 1.346 |
| ΔPJA-RCA (postOP) | 0.174 | 1.190 | 0.002 | 1.065 | 1.331 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lange, T.; Boeckenfoerde, K.; Gosheger, G.; Bockholt, S.; Bövingloh, A.S. Risk Factor Analysis for Proximal Junctional Kyphosis in Neuromuscular Scoliosis: A Single-Center Study. J. Clin. Med. 2025, 14, 3646. https://doi.org/10.3390/jcm14113646
Lange T, Boeckenfoerde K, Gosheger G, Bockholt S, Bövingloh AS. Risk Factor Analysis for Proximal Junctional Kyphosis in Neuromuscular Scoliosis: A Single-Center Study. Journal of Clinical Medicine. 2025; 14(11):3646. https://doi.org/10.3390/jcm14113646
Chicago/Turabian StyleLange, Tobias, Kathrin Boeckenfoerde, Georg Gosheger, Sebastian Bockholt, and Albert Schulze Bövingloh. 2025. "Risk Factor Analysis for Proximal Junctional Kyphosis in Neuromuscular Scoliosis: A Single-Center Study" Journal of Clinical Medicine 14, no. 11: 3646. https://doi.org/10.3390/jcm14113646
APA StyleLange, T., Boeckenfoerde, K., Gosheger, G., Bockholt, S., & Bövingloh, A. S. (2025). Risk Factor Analysis for Proximal Junctional Kyphosis in Neuromuscular Scoliosis: A Single-Center Study. Journal of Clinical Medicine, 14(11), 3646. https://doi.org/10.3390/jcm14113646






