Audiological Outcome of the Simultaneous Tumor Resection and Cochlear Implantation in Two Cases of Sporadic and Two Cases of Neurofibromatosis Type 2-Associated Intracochlear Schwannoma
Abstract
1. Introduction
2. Methods
3. Results
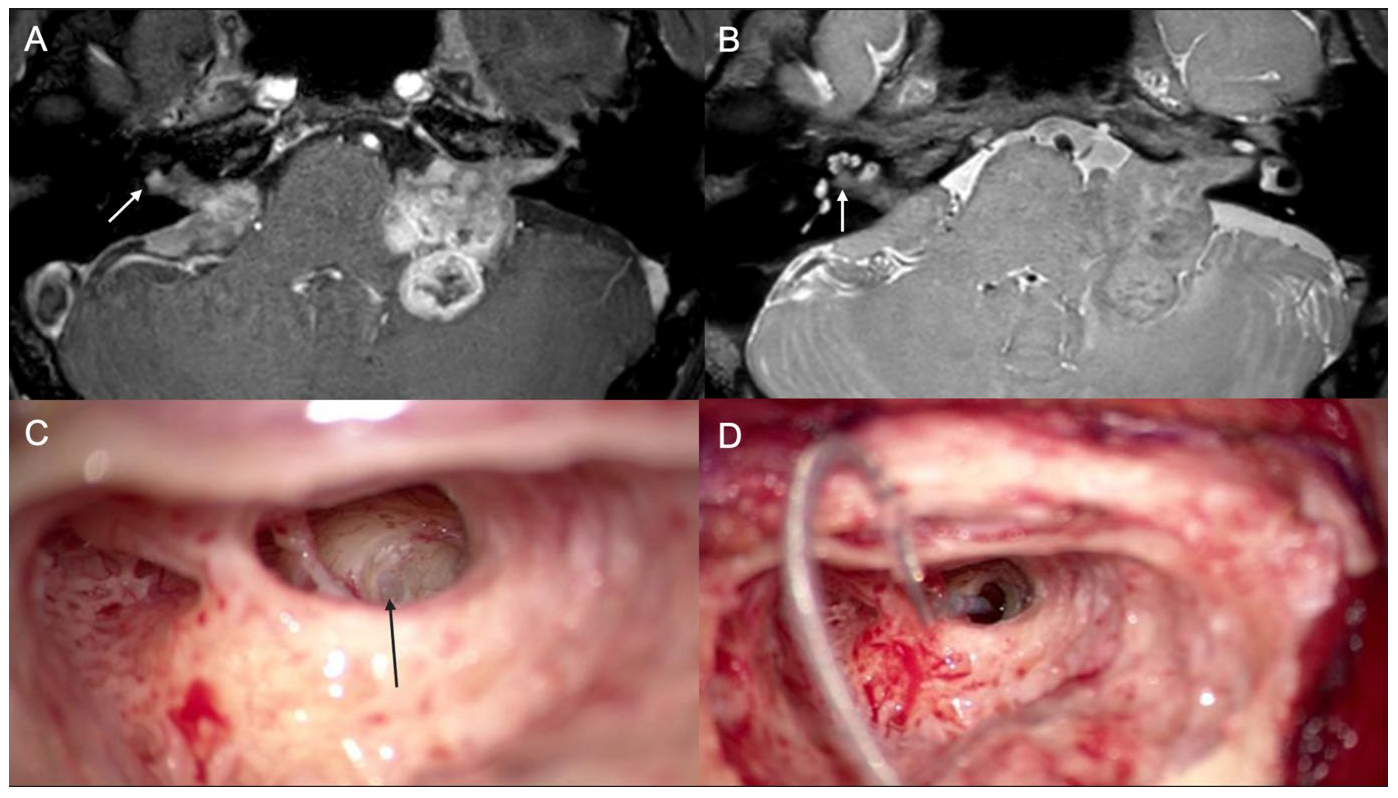
3.1. Case 1
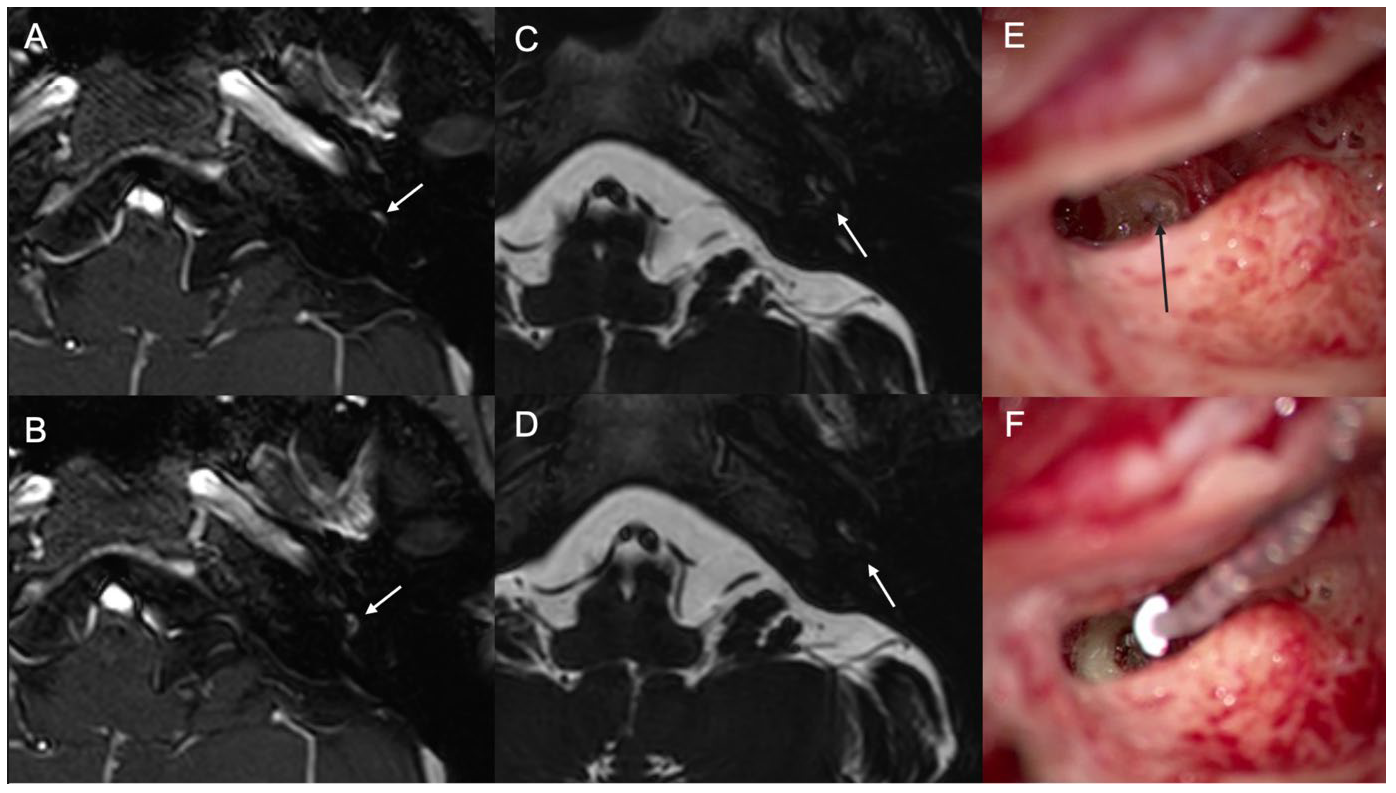
3.2. Case 2
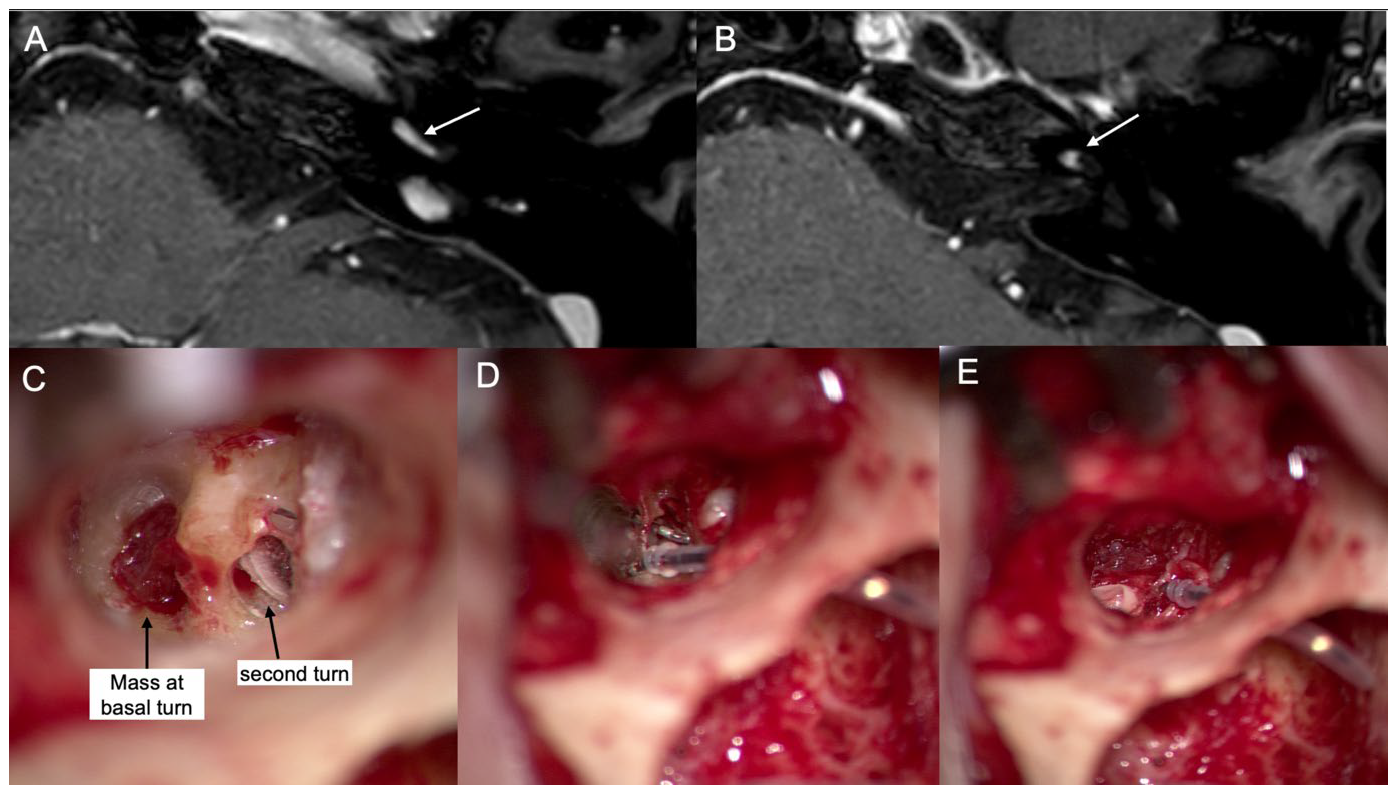
3.3. Case 3
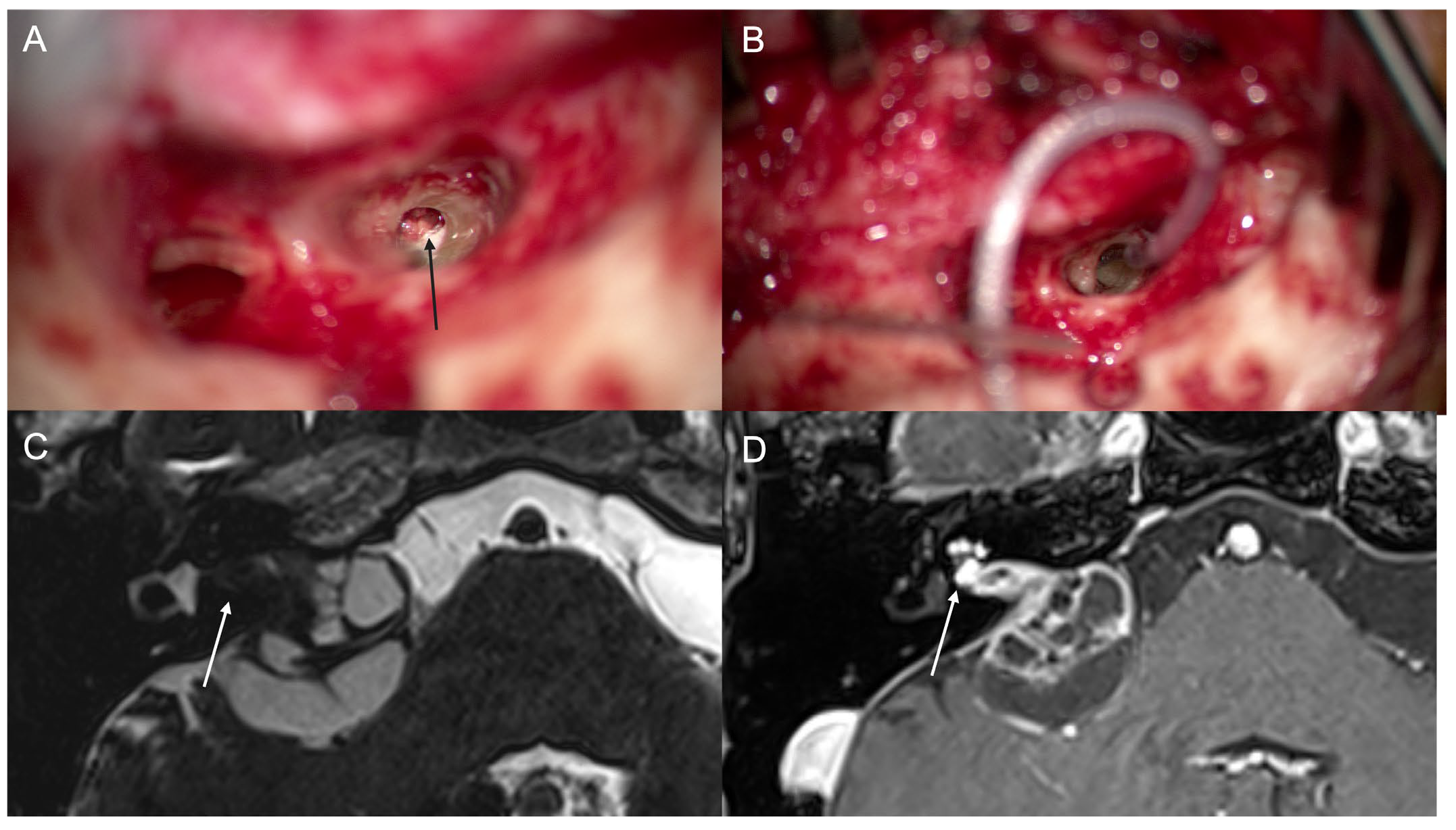
3.4. Case 4
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tadokoro, K.; Bartindale, M.R.; El-Kouri, N.; Moore, D.; Britt, C.; Kircher, M. Cochlear Implantation in Vestibular Schwannoma: A Systematic Literature Review. J. Neurol. Surg. Part B Skull Base 2021, 82, 643–651. [Google Scholar] [CrossRef] [PubMed]
- Gupta, V.K.; Thakker, A.; Gupta, K.K. Vestibular Schwannoma: What We Know and Where We are Heading. Head Neck Pathol. 2020, 14, 1058–1066. [Google Scholar] [CrossRef] [PubMed]
- Goldbrunner, R.; Weller, M.; Regis, J.; Lund-Johansen, M.; Stavrinou, P.; Reuss, D.; Evans, D.G.; Lefranc, F.; Sallabanda, K.; Falini, A.; et al. EANO guideline on the diagnosis and treatment of vestibular schwannoma. Neuro-oncology 2020, 22, 31–45. [Google Scholar] [CrossRef] [PubMed]
- Patel, T.R.; Fleischer, L.; Wiet, R.M.; Michaelides, E.M. Resection of Intracochlear Schwannomas with Immediate Cochlear Implantation. Ann. Otol. Rhinol. Laryngol. 2023, 132, 387–393. [Google Scholar] [CrossRef] [PubMed]
- Kshettry, V.R.; Hsieh, J.K.; Ostrom, Q.T.; Kruchko, C.; Barnholtz-Sloan, J.S. Incidence of vestibular schwannomas in the United States. J. Neurooncol. 2015, 124, 223–228. [Google Scholar] [CrossRef] [PubMed]
- Van Abel, K.M.; Carlson, M.L.; Link, M.J.; Neff, B.A.; Beatty, C.W.; Lohse, C.M.; Eckel, L.J.; Lane, J.I.; Driscoll, C.L. Primary inner ear schwannomas: A case series and systematic review of the literature. Laryngoscope 2013, 123, 1957–1966. [Google Scholar] [CrossRef] [PubMed]
- Di Lullo, A.M.; Paolucci, A.; Motta, S.; Cantone, E.; Barbieri, E.; Cicala, D.; Grassi, R.; Bruno, F.; Splendiani, A.; Tortora, F.; et al. Diagnosis and management of intralabyrinthine schwannoma: Case series and review of the literature. Acta Biomed. 2020, 91 (Suppl. S8), 136–144. [Google Scholar]
- Salzman, K.L.; Childs, A.M.; Davidson, H.C.; Kennedy, R.J.; Shelton, C.; Harnsberger, H.R. Intralabyrinthine schwannomas: Imaging diagnosis and classification. AJNR Am. J. Neuroradiol. 2012, 33, 104–109. [Google Scholar] [CrossRef]
- Carlson, M.L.; Neff, B.A.; Sladen, D.P.; Link, M.J.; Driscoll, C.L. Cochlear Implantation in Patients with Intracochlear and Intralabyrinthine Schwannomas. Otol. Neurotol. 2016, 37, 647–653. [Google Scholar] [CrossRef]
- Plontke, S.K.; Kosling, S.; Rahne, T. Cochlear Implantation after Partial or Subtotal Cochleoectomy for Intracochlear Schwannoma Removal—A Technical Report. Otol. Neurotol. 2018, 39, 365–371. [Google Scholar] [CrossRef]
- Franchella, S.; Ariano, M.; Bevilacqua, F.; Concheri, S.; Zanoletti, E. Cochlear implantation in intralabyrinthine schwannoma: Case series and systematic review of the literature. Audiol. Res. 2023, 13, 169–184. [Google Scholar] [CrossRef] [PubMed]
- Haussler, S.M.; Szczepek, A.J.; Grabel, S.; Olze, H. Challenges of Cochlear Implantation in Intralabyrinthine Schwannoma Patients: Surgical Procedures and Auditory Outcome. J. Clin. Med. 2021, 10, 3899. [Google Scholar] [CrossRef] [PubMed]
- Gosselin, E.; Maniakas, A.; Saliba, I. Meta-analysis on the clinical outcomes in patients with intralabyrinthine schwannomas: Conservative management vs. microsurgery. Eur. Arch. Oto-Rhino-Laryngol. 2016, 273, 1357–1367. [Google Scholar] [CrossRef] [PubMed]
- Wick, C.C.; Butler, M.J.; Yeager, L.H.; Kallogjeri, D.; Durakovic, N.; McJunkin, J.L.; Shew, M.A.; Herzog, J.A.; Buchman, C.A. Cochlear Implant Outcomes following Vestibular Schwannoma Resection: Systematic Review. Otol. Neurotol. 2020, 41, 1190–1197. [Google Scholar] [CrossRef] [PubMed]
- Kronenberg, J.; Horowitz, Z.; Hildesheimer, M. Intracochlear schwannoma and cochlear implantation. Ann. Otol. Rhinol. Laryngol. 1999, 108 Pt 1, 659–660. [Google Scholar] [CrossRef]
- Plontke, S.K.; Fröhlich, L.; Wagner, L.; Kösling, S.; Götze, G.; Siebolts, U.; Liebau, A.; Rahne, T. How much cochlea do you need for cochlear implantation? Otol. Neurotol. 2020, 41, 694–703. [Google Scholar] [CrossRef]
- Ha, J.; Kim, H.; Gu, G.Y.; Song, Y.J.; Jang, J.H.; Park, H.Y.; Choung, Y.H. Surgical Outcomes of Simultaneous Cochlear Implantation and Intracochlear Schwannoma Removal. Otolaryngol. Head Neck Surg. 2023, 169, 660–668. [Google Scholar] [CrossRef]
- Lustig, L.R.; Yeagle, J.; Driscoll, C.L.; Blevins, N.; Francis, H.; Niparko, J.K. Cochlear implantation in patients with neurofibromatosis type 2 and bilateral vestibular schwannoma. Otol. Neurotol. 2006, 27, 512–518. [Google Scholar] [CrossRef] [PubMed]
- Campos Paiva, A.L.; de Salles, A.A.; Diniz, J.M.; Saraiva, C.C.; Ramos, G.R.; Gorgulho, A.A. Gamma Knife Radiosurgery for Transmodiolar Schwannoma. World Neurosurg. 2020, 143, 118–120. [Google Scholar] [CrossRef]
- Plontke, S.K.; Rahne, T.; Curthoys, I.S.; Håkansson, B.; Fröhlich, L. A case series shows independent vestibular labyrinthine function after major surgical trauma to the human cochlea. Commun. Med. 2021, 1, 37. [Google Scholar] [CrossRef]
- Sudhoff, H.; Scholtz, L.U.; Gehl, H.B.; Todt, I. Quality Control after Intracochlear Intralabyrinthine Schwannoma Resection and Cochlear Implantation. Brain Sci. 2021, 11, 1221. [Google Scholar] [CrossRef] [PubMed]
- Edmonson, H.A.; Carlson, M.L.; Patton, A.C.; Watson, R.E. MR imaging and cochlear implants with retained internal magnets: Reducing artifacts near highly inhomogeneous magnetic fields. Radiographics 2018, 38, 94–106. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
AlMutawah, A.A.; Kim, T.; Chung, J.W. Audiological Outcome of the Simultaneous Tumor Resection and Cochlear Implantation in Two Cases of Sporadic and Two Cases of Neurofibromatosis Type 2-Associated Intracochlear Schwannoma. J. Clin. Med. 2024, 13, 3042. https://doi.org/10.3390/jcm13113042
AlMutawah AA, Kim T, Chung JW. Audiological Outcome of the Simultaneous Tumor Resection and Cochlear Implantation in Two Cases of Sporadic and Two Cases of Neurofibromatosis Type 2-Associated Intracochlear Schwannoma. Journal of Clinical Medicine. 2024; 13(11):3042. https://doi.org/10.3390/jcm13113042
Chicago/Turabian StyleAlMutawah, Abdullah A., Taegyeong Kim, and Jong Woo Chung. 2024. "Audiological Outcome of the Simultaneous Tumor Resection and Cochlear Implantation in Two Cases of Sporadic and Two Cases of Neurofibromatosis Type 2-Associated Intracochlear Schwannoma" Journal of Clinical Medicine 13, no. 11: 3042. https://doi.org/10.3390/jcm13113042
APA StyleAlMutawah, A. A., Kim, T., & Chung, J. W. (2024). Audiological Outcome of the Simultaneous Tumor Resection and Cochlear Implantation in Two Cases of Sporadic and Two Cases of Neurofibromatosis Type 2-Associated Intracochlear Schwannoma. Journal of Clinical Medicine, 13(11), 3042. https://doi.org/10.3390/jcm13113042





