The Potential Role of the Ketogenic Diet in Serious Mental Illness: Current Evidence, Safety, and Practical Advice
Abstract
1. Introduction
2. Materials and Methods
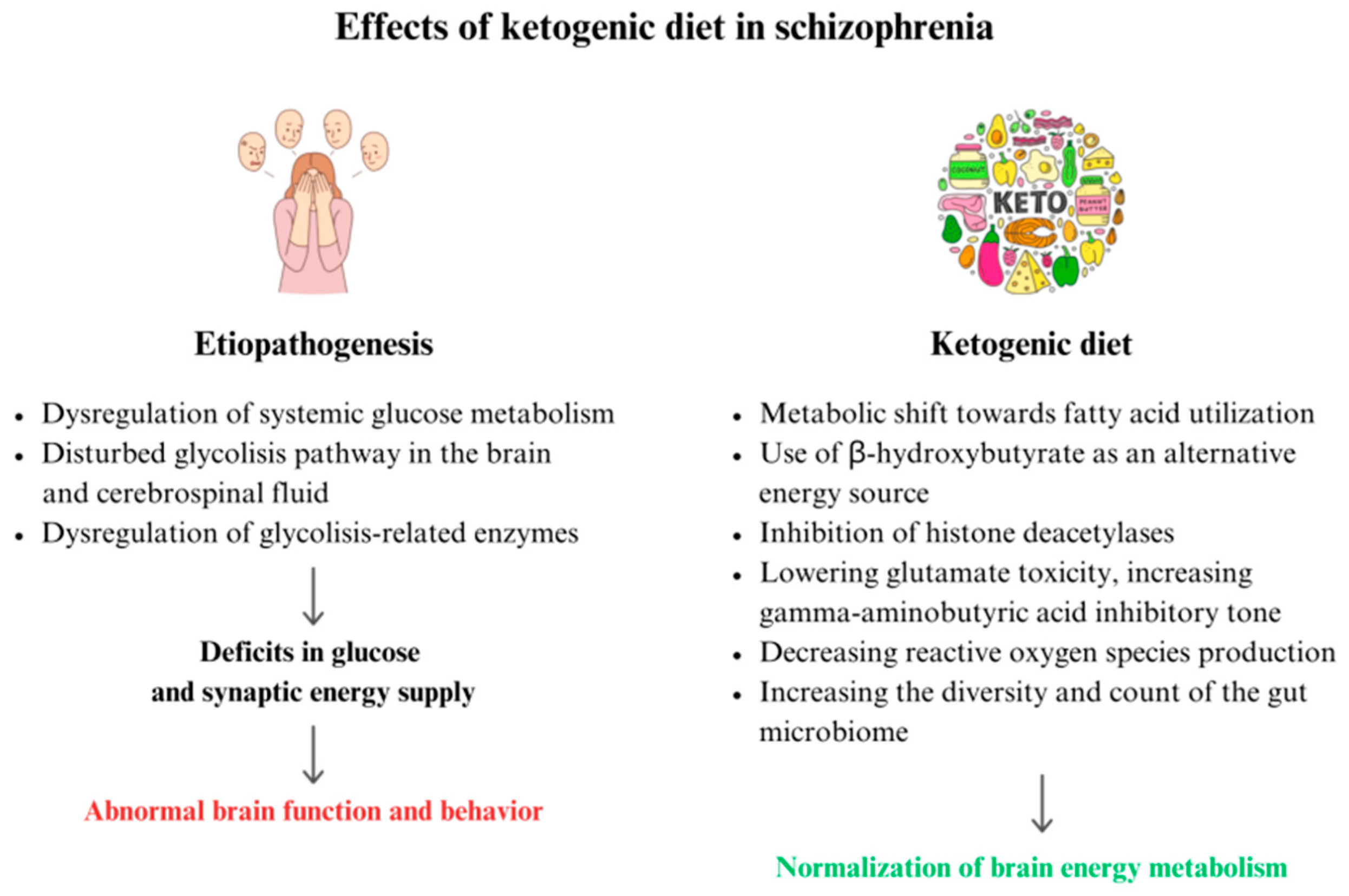
3. Therapeutic Effect of the Ketogenic Diet in Schizophrenia
3.1. Etiopathogenesis and Potential Role of the Ketogenic Diet
3.2. Animal Model Studies
3.3. Clinical Trials and Case Studies
4. Therapeutic Effect of the Ketogenic Diet in Depression
4.1. Etiopathogenesis and Potential Role of the Ketogenic Diet
4.2. Animal Model Studies
4.3. Clinical Trials and Case Studies
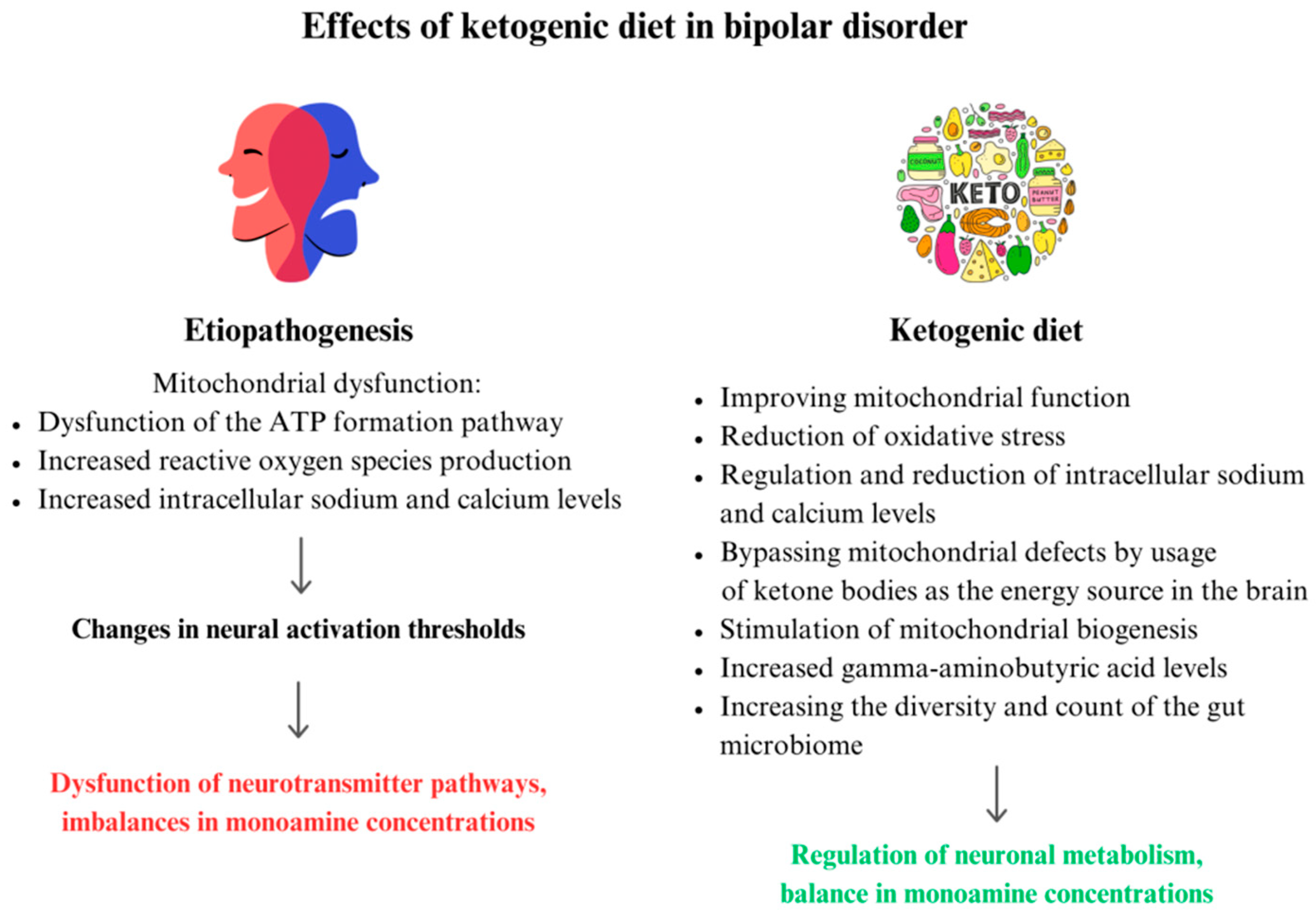
5. Therapeutic Effect of the Ketogenic Diet in Bipolar Disorder
5.1. Etiopathogenesis and Potential Role of the Ketogenic Diet
5.2. Animal Model Studies
5.3. Clinical Trials and Case Studies
6. Health Risks Associated with the Use of the Ketogenic Diet
7. A Practical Guide to Using the KD in Psychiatric Disorders
8. Strengths and Limitations
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pietrzak, D.; Kasperek, K.; Rękawek, P.; Piątkowska-Chmiel, I. The Therapeutic Role of Ketogenic Diet in Neurological Disorders. Nutrients 2022, 14, 1952. [Google Scholar] [CrossRef]
- Hartman, A.L.; Gasior, M.; Vining, E.P.G.; Rogawski, M.A. The Neuropharmacology of the Ketogenic Diet. Pediatr. Neurol. 2007, 36, 281–292. [Google Scholar] [CrossRef]
- Tillery, E.E.; Ellis, K.D.; Threatt, T.B.; Reyes, H.A.; Plummer, C.S.; Barney, L.R. The Use of the Ketogenic Diet in the Treatment of Psychiatric Disorders. Ment. Health Clin. 2021, 11, 211–219. [Google Scholar] [CrossRef]
- Sokoloff, L. Measurement of Local Cerebral Glucose Utilization and Its Relation to Local Functional Activity in the Brain. In Fuel Homeostasis and the Nervous System; Vranic, M., Efendic, S., Hollenberg, C.H., Eds.; Advances in Experimental Medicine and Biology; Springer: Boston, MA, USA, 1991; pp. 21–42. ISBN 9781468459319. [Google Scholar]
- Owen, O.E.; Morgan, A.P.; Kemp, H.G.; Sullivan, J.M.; Herrera, M.G.; Cahill, G.F. Brain Metabolism during Fasting. J. Clin. Investig. 1967, 46, 1589–1595. [Google Scholar] [CrossRef]
- Modified Atkins Diet—An Overview. ScienceDirect Topics. Available online: https://www.sciencedirect.com/topics/medicine-and-dentistry/modified-atkins-diet (accessed on 27 February 2024).
- Huttenlocher, P.R.; Wilbourn, A.J.; Signore, J.M. Medium-chain Triglycerides as a Therapy for Intractable Childhood Epilepsy. Neurology 1971, 21, 1097. [Google Scholar] [CrossRef]
- Hughes, S.D.; Kanabus, M.; Anderson, G.; Hargreaves, I.P.; Rutherford, T.; Donnell, M.O.; Cross, J.H.; Rahman, S.; Eaton, S.; Heales, S.J.R. The Ketogenic Diet Component Decanoic Acid Increases Mitochondrial Citrate Synthase and Complex I Activity in Neuronal Cells. J. Neurochem. 2014, 129, 426–433. [Google Scholar] [CrossRef]
- Feinman, R.D.; Pogozelski, W.K.; Astrup, A.; Bernstein, R.K.; Fine, E.J.; Westman, E.C.; Accurso, A.; Frassetto, L.; Gower, B.A.; McFarlane, S.I.; et al. Dietary Carbohydrate Restriction as the First Approach in Diabetes Management: Critical Review and Evidence Base. Nutrition 2015, 31, 1–13. [Google Scholar] [CrossRef]
- Vega-López, S.; Venn, B.J.; Slavin, J.L. Relevance of the Glycemic Index and Glycemic Load for Body Weight, Diabetes, and Cardiovascular Disease. Nutrients 2018, 10, 1361. [Google Scholar] [CrossRef]
- Kwon, H.E.; Kim, H.D. Recent Aspects of Ketogenic Diet in Neurological Disorders. Acta Epileptol. 2021, 3, 21. [Google Scholar] [CrossRef]
- Kysel, P.; Haluzíková, D.; Doležalová, R.P.; Laňková, I.; Lacinová, Z.; Kasperová, B.J.; Trnovská, J.; Hrádková, V.; Mráz, M.; Vilikus, Z.; et al. The Influence of Cyclical Ketogenic Reduction Diet vs. Nutritionally Balanced Reduction Diet on Body Composition, Strength, and Endurance Performance in Healthy Young Males: A Randomized Controlled Trial. Nutrients 2020, 12, 2832. [Google Scholar] [CrossRef]
- Zou, X.H.; Sun, L.H.; Yang, W.; Li, B.J.; Cui, R.J. Potential Role of Insulin on the Pathogenesis of Depression. Cell Prolif. 2020, 53, e12806. [Google Scholar] [CrossRef]
- Sullivan, P.G.; Rippy, N.A.; Dorenbos, K.; Concepcion, R.C.; Agarwal, A.K.; Rho, J.M. The Ketogenic Diet Increases Mitochondrial Uncoupling Protein Levels and Activity. Ann. Neurol. 2004, 55, 576–580. [Google Scholar] [CrossRef]
- Yu, B.J.; Oz, R.S.; Sethi, S. Ketogenic Diet as a Metabolic Therapy for Bipolar Disorder: Clinical Developments. J. Affect. Disord. Rep. 2023, 11, 100457. [Google Scholar] [CrossRef]
- Maalouf, M.; Sullivan, P.G.; Davis, L.; Kim, D.Y.; Rho, J.M. Ketones Inhibit Mitochondrial Production of Reactive Oxygen Species Production Following Glutamate Excitotoxicity by Increasing NADH Oxidation. Neuroscience 2007, 145, 256–264. [Google Scholar] [CrossRef]
- Sethi, S.; Ford, J.M. The Role of Ketogenic Metabolic Therapy on the Brain in Serious Mental Illness: A Review. J. Psychiatry Brain Sci. 2022, 7, e220009. [Google Scholar] [CrossRef]
- Fu, S.-P.; Wang, J.-F.; Xue, W.-J.; Liu, H.-M.; Liu, B.; Zeng, Y.-L.; Li, S.-N.; Huang, B.-X.; Lv, Q.-K.; Wang, W.; et al. Anti-Inflammatory Effects of BHBA in Both in Vivo and in Vitro Parkinson’s Disease Models Are Mediated by GPR109A-Dependent Mechanisms. J. Neuroinflamm. 2015, 12, 9. [Google Scholar] [CrossRef]
- Shimazu, T.; Hirschey, M.D.; Newman, J.; He, W.; Shirakawa, K.; Le Moan, N.; Grueter, C.A.; Lim, H.; Saunders, L.R.; Stevens, R.D.; et al. Suppression of Oxidative Stress by β-Hydroxybutyrate, an Endogenous Histone Deacetylase Inhibitor. Science 2013, 339, 211–214. [Google Scholar] [CrossRef]
- Huang, C.; Wang, P.; Xu, X.; Zhang, Y.; Gong, Y.; Hu, W.; Gao, M.; Wu, Y.; Ling, Y.; Zhao, X.; et al. The Ketone Body Metabolite β-Hydroxybutyrate Induces an Antidepression-Associated Ramification of Microglia via HDACs Inhibition-Triggered Akt-Small RhoGTPase Activation. Glia 2018, 66, 256–278. [Google Scholar] [CrossRef]
- Qiao, G.; Lv, T.; Zhang, M.; Chen, P.; Sun, Q.; Zhang, J.; Li, Q. β-Hydroxybutyrate (β-HB) Exerts Anti-Inflammatory and Antioxidant Effects in Lipopolysaccharide (LPS)-Stimulated Macrophages in Liza Haematocheila. Fish Shellfish. Immunol. 2020, 107, 444–451. [Google Scholar] [CrossRef]
- Hertz, L.; Peng, L.; Dienel, G.A. Energy Metabolism in Astrocytes: High Rate of Oxidative Metabolism and Spatiotemporal Dependence on Glycolysis/Glycogenolysis. J. Cereb. Blood Flow Metab. 2007, 27, 219–249. [Google Scholar] [CrossRef]
- Hertz, L.; Rothman, D.L. Glucose, Lactate, β-Hydroxybutyrate, Acetate, GABA, and Succinate as Substrates for Synthesis of Glutamate and GABA in the Glutamine—Glutamate/GABA Cycle. In The Glutamate/GABA-Glutamine Cycle: Amino Acid Neurotransmitter Homeostasis; Schousboe, A., Sonnewald, U., Eds.; Advances in Neurobiology; Springer International Publishing: Cham, Switzerland, 2016; pp. 9–42. ISBN 9783319450964. [Google Scholar]
- Zilberter, Y.; Zilberter, T. Glucose-Sparing Action of Ketones Boosts Functions Exclusive to Glucose in the Brain. eNeuro 2020, 7. [Google Scholar] [CrossRef]
- Włodarczyk, A.; Wiglusz, M.S.; Cubała, W.J. Ketogenic Diet for Schizophrenia: Nutritional Approach to Antipsychotic Treatment. Med. Hypotheses 2018, 118, 74–77. [Google Scholar] [CrossRef]
- Włodarczyk, A.; Cubała, W.J.; Stawicki, M. Ketogenic Diet for Depression: A Potential Dietary Regimen to Maintain Euthymia? Prog. Neuropsychopharmacol. Biol. Psychiatry 2021, 109, 110257. [Google Scholar] [CrossRef]
- Srinivasan, K. Editorial: Nutrition and Lifestyle Medicine for Neurodevelopmental and Psychiatric Disorders. Front. Nutr. 2024, 11, 1349690. [Google Scholar] [CrossRef]
- Sarris, J. Nutritional Psychiatry: From Concept to the Clinic. Drugs 2019, 79, 929–934. [Google Scholar] [CrossRef]
- Norwitz, N.G.; Sethi, S.; Palmer, C.M. Ketogenic Diet as a Metabolic Treatment for Mental Illness. Curr. Opin. Endocrinol. Diabetes Obes. 2020, 27, 269. [Google Scholar] [CrossRef]
- Serretti, A.; Mandelli, L. Antidepressants and Body Weight: A Comprehensive Review and Meta-Analysis. J. Clin. Psychiatry 2010, 71, 979. [Google Scholar] [CrossRef]
- Tagliabue, A.; Armeno, M.; Berk, K.A.; Guglielmetti, M.; Ferraris, C.; Olieman, J.; van der Louw, E. Ketogenic Diet for Epilepsy and Obesity: Is It the Same? Nutr. Metab. Cardiovasc. Dis. 2024, 34, 581–589. [Google Scholar] [CrossRef]
- Magistretti, P.J.; Allaman, I. A Cellular Perspective on Brain Energy Metabolism and Functional Imaging. Neuron 2015, 86, 883–901. [Google Scholar] [CrossRef]
- Harris, J.J.; Jolivet, R.; Attwell, D. Synaptic Energy Use and Supply. Neuron 2012, 75, 762–777. [Google Scholar] [CrossRef]
- Kann, O. The Interneuron Energy Hypothesis: Implications for Brain Disease. Neurobiol. Dis. 2016, 90, 75–85. [Google Scholar] [CrossRef]
- Kraeuter, A.-K.; van den Buuse, M.; Sarnyai, Z. Ketogenic Diet Prevents Impaired Prepulse Inhibition of Startle in an Acute NMDA Receptor Hypofunction Model of Schizophrenia. Schizophr. Res. 2019, 206, 244–250. [Google Scholar] [CrossRef] [PubMed]
- Ernst, A.; Ma, D.; Garcia-Perez, I.; Tsang, T.M.; Kluge, W.; Schwarz, E.; Guest, P.C.; Holmes, E.; Sarnyai, Z.; Bahn, S. Molecular Validation of the Acute Phencyclidine Rat Model for Schizophrenia: Identification of Translational Changes in Energy Metabolism and Neurotransmission. J. Proteome Res. 2012, 11, 3704–3714. [Google Scholar] [CrossRef]
- Zuccoli, G.S.; Saia-Cereda, V.M.; Nascimento, J.M.; Martins-de-Souza, D. The Energy Metabolism Dysfunction in Psychiatric Disorders Postmortem Brains: Focus on Proteomic Evidence. Front. Neurosci. 2017, 11, 493. [Google Scholar] [CrossRef]
- Prabakaran, S.; Swatton, J.E.; Ryan, M.M.; Huffaker, S.J.; Huang, J.T.-J.; Griffin, J.L.; Wayland, M.; Freeman, T.; Dudbridge, F.; Lilley, K.S.; et al. Mitochondrial Dysfunction in Schizophrenia: Evidence for Compromised Brain Metabolism and Oxidative Stress. Mol. Psychiatry 2004, 9, 684–697. [Google Scholar] [CrossRef]
- Chouinard, V.A.; Kim, S.Y.; Valeri, L.; Yuksel, C.; Ryan, K.P.; Chouinard, G.; Cohen, B.M.; Du, F.; Öngür, D. Brain bioenergetics and redox state measured by 31P magnetic resonance spectroscopy in unaffected siblings of patients with psychotic disorders. Schizophr. Res. 2017, 187, 11–16. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, C.R.; Koene, R.H.; Hasselfeld, K.; O’Donovan, S.M.; Ramsey, A.; McCullumsmith, R.E. Neuron-Specific Deficits of Bioenergetic Processes in the Dorsolateral Prefrontal Cortex in Schizophrenia. Mol. Psychiatry 2019, 24, 1319–1328. [Google Scholar] [CrossRef]
- Forsyth, J.K.; Lewis, D.A. Mapping the Consequences of Impaired Synaptic Plasticity in Schizophrenia through Development: An Integrative Model for Diverse Clinical Features. Trends Cogn. Sci. 2017, 21, 760–778. [Google Scholar] [CrossRef] [PubMed]
- Wesseling, H.; Chan, M.K.; Tsang, T.M.; Ernst, A.; Peters, F.; Guest, P.C.; Holmes, E.; Bahn, S. A Combined Metabonomic and Proteomic Approach Identifies Frontal Cortex Changes in a Chronic Phencyclidine Rat Model in Relation to Human Schizophrenia Brain Pathology. Neuropsychopharmacology 2013, 38, 2532–2544. [Google Scholar] [CrossRef][Green Version]
- Pillinger, T.; Beck, K.; Gobjila, C.; Donocik, J.G.; Jauhar, S.; Howes, O.D. Impaired Glucose Homeostasis in First-Episode Schizophrenia: A Systematic Review and Meta-Analysis. JAMA Psychiatry 2017, 74, 261–269. [Google Scholar] [CrossRef]
- Steiner, J.; Berger, M.; Guest, P.C.; Dobrowolny, H.; Westphal, S.; Schiltz, K.; Sarnyai, Z. Assessment of Insulin Resistance Among Drug-Naive Patients With First-Episode Schizophrenia in the Context of Hormonal Stress Axis Activation. JAMA Psychiatry 2017, 74, 968–970. [Google Scholar] [CrossRef] [PubMed]
- Chouinard, V.-A.; Henderson, D.C.; Man, C.D.; Valeri, L.; Gray, B.E.; Ryan, K.P.; Cypess, A.M.; Cobelli, C.; Cohen, B.M.; Öngür, D. Impaired Insulin Signaling in Unaffected Siblings and Patients with First Episode Psychosis. Mol. Psychiatry 2019, 24, 1513–1522. [Google Scholar] [CrossRef] [PubMed]
- Koppel, S.J.; Swerdlow, R.H. Neuroketotherapeutics: A Modern Review of a Century-Old Therapy. Neurochem. Int. 2018, 117, 114–125. [Google Scholar] [CrossRef]
- Bough, K. Energy Metabolism as Part of the Anticonvulsant Mechanism of the Ketogenic Diet. Epilepsia 2008, 49 (Suppl. S8), 91–93. [Google Scholar] [CrossRef] [PubMed]
- Branco, A.F.; Ferreira, A.; Simões, R.F.; Magalhães-Novais, S.; Zehowski, C.; Cope, E.; Silva, A.M.; Pereira, D.; Sardão, V.A.; Cunha-Oliveira, T. Ketogenic Diets: From Cancer to Mitochondrial Diseases and Beyond. Eur. J. Clin. Investig. 2016, 46, 285–298. [Google Scholar] [CrossRef] [PubMed]
- Tregellas, J.R.; Smucny, J.; Legget, K.T.; Stevens, K.E. Effects of a Ketogenic Diet on Auditory Gating in DBA/2 Mice: A Proof-of-Concept Study. Schizophr. Res. 2015, 169, 351–354. [Google Scholar] [CrossRef] [PubMed]
- Mujica-Parodi, L.R.; Amgalan, A.; Sultan, S.F.; Antal, B.; Sun, X.; Skiena, S.; Lithen, A.; Adra, N.; Ratai, E.-M.; Weistuch, C.; et al. Diet Modulates Brain Network Stability, a Biomarker for Brain Aging, in Young Adults. Proc. Natl. Acad. Sci. USA 2020, 117, 6170–6177. [Google Scholar] [CrossRef] [PubMed]
- Zhu, F.; Guo, R.; Wang, W.; Ju, Y.; Wang, Q.; Ma, Q.; Sun, Q.; Fan, Y.; Xie, Y.; Yang, Z.; et al. Transplantation of Microbiota from Drug-Free Patients with Schizophrenia Causes Schizophrenia-like Abnormal Behaviors and Dysregulated Kynurenine Metabolism in Mice. Mol. Psychiatry 2020, 25, 2905–2918. [Google Scholar] [CrossRef] [PubMed]
- Munawar, N.; Ahsan, K.; Muhammad, K.; Ahmad, A.; Anwar, M.A.; Shah, I.; Al Ameri, A.K.; Al Mughairbi, F. Hidden Role of Gut Microbiome Dysbiosis in Schizophrenia: Antipsychotics or Psychobiotics as Therapeutics? Int. J. Mol. Sci. 2021, 22, 7671. [Google Scholar] [CrossRef]
- Ma, D.; Wang, A.C.; Parikh, I.; Green, S.J.; Hoffman, J.D.; Chlipala, G.; Murphy, M.P.; Sokola, B.S.; Bauer, B.; Hartz, A.M.S.; et al. Ketogenic Diet Enhances Neurovascular Function with Altered Gut Microbiome in Young Healthy Mice. Sci. Rep. 2018, 8, 6670. [Google Scholar] [CrossRef]
- Shamshoum, H.; Medak, K.D.; McKie, G.L.; Hahn, M.K.; Wright, D.C. Fasting or the Short-Term Consumption of a Ketogenic Diet Protects against Antipsychotic-Induced Hyperglycaemia in Mice. J. Physiol. 2022, 600, 2713–2728. [Google Scholar] [CrossRef] [PubMed]
- Stogios, N.; Smith, E.; Bowden, S.; Tran, V.; Asgariroozbehani, R.; McIntyre, W.B.; Remington, G.; Siskind, D.; Agarwal, S.M.; Hahn, M.K. Metabolic Adverse Effects of Off-Label Use of Second-Generation Antipsychotics in the Adult Population: A Systematic Review and Meta-Analysis. Neuropsychopharmacol. Off. Publ. Am. Coll. Neuropsychopharmacol. 2022, 47, 664–672. [Google Scholar] [CrossRef] [PubMed]
- Huhn, M.; Nikolakopoulou, A.; Schneider-Thoma, J.; Krause, M.; Samara, M.; Peter, N.; Arndt, T.; Bäckers, L.; Rothe, P.; Cipriani, A.; et al. Comparative Efficacy and Tolerability of 32 Oral Antipsychotics for the Acute Treatment of Adults with Multi-Episode Schizophrenia: A Systematic Review and Network Meta-Analysis. Lancet 2019, 394, 939–951. [Google Scholar] [CrossRef]
- Pillinger, T.; McCutcheon, R.A.; Vano, L.; Mizuno, Y.; Arumuham, A.; Hindley, G.; Beck, K.; Natesan, S.; Efthimiou, O.; Cipriani, A.; et al. Comparative Effects of 18 Antipsychotics on Metabolic Function in Patients with Schizophrenia, Predictors of Metabolic Dysregulation, and Association with Psychopathology: A Systematic Review and Network Meta-Analysis. Lancet Psychiatry 2020, 7, 64–77. [Google Scholar] [CrossRef] [PubMed]
- Ranjan, A.; Schmidt, S.; Damm-Frydenberg, C.; Steineck, I.; Clausen, T.R.; Holst, J.J.; Madsbad, S.; Nørgaard, K. Low-Carbohydrate Diet Impairs the Effect of Glucagon in the Treatment of Insulin-Induced Mild Hypoglycemia: A Randomized Crossover Study. Diabetes Care 2017, 40, 132–135. [Google Scholar] [CrossRef]
- Morrison, C.D.; Hill, C.M.; DuVall, M.A.; Coulter, C.E.; Gosey, J.L.; Herrera, M.J.; Maisano, L.E.; Sikaffy, H.X.; McDougal, D.H. Consuming a Ketogenic Diet Leads to Altered Hypoglycemic Counter-Regulation in Mice. J. Diabetes Complicat. 2020, 34, 107557. [Google Scholar] [CrossRef]
- Briant, L.J.B.; Dodd, M.S.; Chibalina, M.V.; Rorsman, N.J.G.; Johnson, P.R.V.; Carmeliet, P.; Rorsman, P.; Knudsen, J.G. CPT1a-Dependent Long-Chain Fatty Acid Oxidation Contributes to Maintaining Glucagon Secretion from Pancreatic Islets. Cell Rep. 2018, 23, 3300–3311. [Google Scholar] [CrossRef]
- Pacheco, A.; Easterling, W.S.; Pryer, M.W. A Pilot Study of the Ketogenic Diet in Schizophrenia. Am. J. Psychiatry 1965, 121, 1110–1111. [Google Scholar] [CrossRef]
- Sethi, S.; Wakeham, D.; Ketter, T.; Hooshmand, F.; Bjorstead, J.; Richards, B.; Westman, E.; Krauss, R.M.; Saslow, L. Ketogenic Diet Intervention on Metabolic and Psychiatric Health in Bipolar and Schizophrenia: A Pilot Trial. Psychiatry Res. 2024, 335, 115866. [Google Scholar] [CrossRef]
- Palmer, C.M.; Gilbert-Jaramillo, J.; Westman, E.C. The Ketogenic Diet and Remission of Psychotic Symptoms in Schizophrenia: Two Case Studies. Schizophr. Res. 2019, 208, 439–440. [Google Scholar] [CrossRef]
- Kraft, B.D.; Westman, E.C. Schizophrenia, Gluten, and Low-Carbohydrate, Ketogenic Diets: A Case Report and Review of the Literature. Nutr. Metab. 2009, 6, 10. [Google Scholar] [CrossRef] [PubMed]
- Guan, Y.-F.; Huang, G.-B.; Xu, M.-D.; Gao, F.; Lin, S.; Huang, J.; Wang, J.; Li, Y.-Q.; Wu, C.-H.; Yao, S.; et al. Anti-Depression Effects of Ketogenic Diet Are Mediated via the Restoration of Microglial Activation and Neuronal Excitability in the Lateral Habenula. Brain Behav. Immun. 2020, 88, 748–762. [Google Scholar] [CrossRef] [PubMed]
- Enache, D.; Pariante, C.M.; Mondelli, V. Markers of Central Inflammation in Major Depressive Disorder: A Systematic Review and Meta-Analysis of Studies Examining Cerebrospinal Fluid, Positron Emission Tomography and Post-Mortem Brain Tissue. Brain Behav. Immun. 2019, 81, 24–40. [Google Scholar] [CrossRef] [PubMed]
- Kern, S.; Skoog, I.; Börjesson-Hanson, A.; Blennow, K.; Zetterberg, H.; Ostling, S.; Kern, J.; Gudmundsson, P.; Marlow, T.; Rosengren, L.; et al. Higher CSF Interleukin-6 and CSF Interleukin-8 in Current Depression in Older Women. Results from a Population-Based Sample. Brain Behav. Immun. 2014, 41, 55–58. [Google Scholar] [CrossRef] [PubMed]
- Hannestad, J.; DellaGioia, N.; Gallezot, J.-D.; Lim, K.; Nabulsi, N.; Esterlis, I.; Pittman, B.; Lee, J.-Y.; O’Connor, K.C.; Pelletier, D.; et al. The Neuroinflammation Marker Translocator Protein Is Not Elevated in Individuals with Mild-to-Moderate Depression: A [11C]PBR28 PET Study. Brain Behav. Immun. 2013, 33, 131–138. [Google Scholar] [CrossRef] [PubMed]
- Holmes, S.E.; Hinz, R.; Conen, S.; Gregory, C.J.; Matthews, J.C.; Anton-Rodriguez, J.M.; Gerhard, A.; Talbot, P.S. Elevated Translocator Protein in Anterior Cingulate in Major Depression and a Role for Inflammation in Suicidal Thinking: A Positron Emission Tomography Study. Biol. Psychiatry 2018, 83, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Walaszek, M.; Kachlik, Z.; Cubała, W.J. Low-Carbohydrate Diet as a Nutritional Intervention in a Major Depression Disorder: Focus on Relapse Prevention. Nutr. Neurosci. 2024, 1–14. [Google Scholar] [CrossRef]
- Newell, C.; Bomhof, M.R.; Reimer, R.A.; Hittel, D.S.; Rho, J.M.; Shearer, J. Ketogenic Diet Modifies the Gut Microbiota in a Murine Model of Autism Spectrum Disorder. Mol. Autism 2016, 7, 37. [Google Scholar] [CrossRef]
- Bailey, M.T.; Dowd, S.E.; Galley, J.D.; Hufnagle, A.R.; Allen, R.G.; Lyte, M. Exposure to a Social Stressor Alters the Structure of the Intestinal Microbiota: Implications for Stressor-Induced Immunomodulation. Brain Behav. Immun. 2011, 25, 397–407. [Google Scholar] [CrossRef]
- Ruskin, D.N.; Kawamura, M.; Masino, S.A. Reduced Pain and Inflammation in Juvenile and Adult Rats Fed a Ketogenic Diet. PLoS ONE 2009, 4, e8349. [Google Scholar] [CrossRef]
- Pieklik, A.; Pawlaczyk, M.; Rog, J.; Karakula-Juchnowicz, H. The Ketogenic Diet: A Co-Therapy in the Treatment of Mood Disorders and Obesity—A Case Report. Curr. Probl. Psychiatry 2021, 22, 000010247820210002. [Google Scholar] [CrossRef]
- Dahlin, M.; Månsson, J.-E.; Åmark, P. CSF Levels of Dopamine and Serotonin, but Not Norepinephrine, Metabolites Are Influenced by the Ketogenic Diet in Children with Epilepsy. Epilepsy Res. 2012, 99, 132–138. [Google Scholar] [CrossRef]
- Juge, N.; Gray, J.A.; Omote, H.; Miyaji, T.; Inoue, T.; Hara, C.; Uneyama, H.; Edwards, R.H.; Nicoll, R.A.; Moriyama, Y. Metabolic Control of Vesicular Glutamate Transport and Release. Neuron 2010, 68, 99–112. [Google Scholar] [CrossRef] [PubMed]
- Murphy, P.; Likhodii, S.; Nylen, K.; Burnham, W.M. The Antidepressant Properties of the Ketogenic Diet. Biol. Psychiatry 2004, 56, 981–983. [Google Scholar] [CrossRef] [PubMed]
- Sussman, D.; Germann, J.; Henkelman, M. Gestational Ketogenic Diet Programs Brain Structure and Susceptibility to Depression & Anxiety in the Adult Mouse Offspring. Brain Behav. 2015, 5, e00300. [Google Scholar] [CrossRef] [PubMed]
- Gumus, H.; Ilgin, R.; Koc, B.; Yuksel, O.; Kizildag, S.; Guvendi, G.; Karakilic, A.; Kandis, S.; Hosgorler, F.; Ates, M.; et al. A Combination of Ketogenic Diet and Voluntary Exercise Ameliorates Anxiety and Depression-like Behaviors in Balb/c Mice. Neurosci. Lett. 2022, 770, 136443. [Google Scholar] [CrossRef]
- Kasprowska-Liśkiewicz, D.; Liśkiewicz, A.D.; Nowacka-Chmielewska, M.M.; Nowicka, J.; Małecki, A.; Barski, J.J. The Ketogenic Diet Affects the Social Behavior of Young Male Rats. Physiol. Behav. 2017, 179, 168–177. [Google Scholar] [CrossRef] [PubMed]
- de Almeida Rabello Oliveira, M.; da Rocha Ataíde, T.; de Oliveira, S.L.; de Melo Lucena, A.L.; de Lira, C.E.P.R.; Soares, A.A.; de Almeida, C.B.S.; Ximenes-da-Silva, A. Effects of Short-Term and Long-Term Treatment with Medium- and Long-Chain Triglycerides Ketogenic Diet on Cortical Spreading Depression in Young Rats. Neurosci. Lett. 2008, 434, 66–70. [Google Scholar] [CrossRef] [PubMed]
- Danan, A.; Westman, E.C.; Saslow, L.R.; Ede, G. The Ketogenic Diet for Refractory Mental Illness: A Retrospective Analysis of 31 Inpatients. Front. Psychiatry 2022, 13, 951376. [Google Scholar] [CrossRef] [PubMed]
- Cox, N.; Gibas, S.; Salisbury, M.; Gomer, J.; Gibas, K. Ketogenic Diets Potentially Reverse Type II Diabetes and Ameliorate Clinical Depression: A Case Study. Diabetes Metab. Syndr. Clin. Res. Rev. 2019, 13, 1475–1479. [Google Scholar] [CrossRef]
- Adams, R.N.; Athinarayanan, S.J.; McKenzie, A.L.; Hallberg, S.J.; McCarter, J.P.; Phinney, S.D.; Gonzalez, J.S. Depressive Symptoms Improve over 2 Years of Type 2 Diabetes Treatment via a Digital Continuous Remote Care Intervention Focused on Carbohydrate Restriction. J. Behav. Med. 2022, 45, 416–427. [Google Scholar] [CrossRef] [PubMed]
- Brietzke, D.E.M. Effects and Mechanistic Aspects of Ketogenic Diet in Individuals with Major Depressive Disorder: A Pilot Study. Available online: https://clinicaltrials.gov/study/NCT05558995?id=NCT05558995&rank=1 (accessed on 19 March 2024).
- Alves, T.; Ata, F.; Campos-Cuellar, C.; Diaz, D.; Gomes, W.; Parente, J.; Schmidt, M.; Serrano, N.; Tay, A.; Vasudevan-Nampoothiri, R.; et al. The KDEP Trial: Protocol for a Phase II, Multicenter, Open Label, Randomized Controlled Trial to Evaluate the Efficacy of Ketogenic Diet for Symptomatic Improvement of Moderate to Severe Major Depressive Disorder. Princ. Pract. Clin. Res. J. 2022, 8, 77–83. [Google Scholar] [CrossRef]
- Phillips, M.L.; Kupfer, D.J. Bipolar Disorder Diagnosis: Challenges and Future Directions. Lancet 2013, 381, 1663–1671. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Santos, R.; Gage, F.H.; Marchetto, M.C. Molecular Mechanisms of Bipolar Disorder: Progress Made and Future Challenges. Front. Cell. Neurosci. 2017, 11, 30. [Google Scholar] [CrossRef] [PubMed]
- Andreazza, A.C.; Shao, L.; Wang, J.-F.; Young, L.T. Mitochondrial Complex I Activity and Oxidative Damage to Mitochondrial Proteins in the Prefrontal Cortex of Patients With Bipolar Disorder. Arch. Gen. Psychiatry 2010, 67, 360–368. [Google Scholar] [CrossRef] [PubMed]
- Das, S.C.; Hjelm, B.E.; Rollins, B.L.; Sequeira, A.; Morgan, L.; Omidsalar, A.A.; Schatzberg, A.F.; Barchas, J.D.; Lee, F.S.; Myers, R.M.; et al. Mitochondria DNA Copy Number, Mitochondria DNA Total Somatic Deletions, Complex I Activity, Synapse Number, and Synaptic Mitochondria Number Are Altered in Schizophrenia and Bipolar Disorder. Transl. Psychiatry 2022, 12, 353. [Google Scholar] [CrossRef] [PubMed]
- Scaini, G.; Rezin, G.T.; Carvalho, A.F.; Streck, E.L.; Berk, M.; Quevedo, J. Mitochondrial Dysfunction in Bipolar Disorder: Evidence, Pathophysiology and Translational Implications. Neurosci. Biobehav. Rev. 2016, 68, 694–713. [Google Scholar] [CrossRef]
- Berk, M.; Kapczinski, F.; Andreazza, A.C.; Dean, O.M.; Giorlando, F.; Maes, M.; Yücel, M.; Gama, C.S.; Dodd, S.; Dean, B.; et al. Pathways Underlying Neuroprogression in Bipolar Disorder: Focus on Inflammation, Oxidative Stress and Neurotrophic Factors. Neurosci. Biobehav. Rev. 2011, 35, 804–817. [Google Scholar] [CrossRef]
- Mertens, J.; Wang, Q.-W.; Kim, Y.; Yu, D.X.; Pham, S.; Yang, B.; Zheng, Y.; Diffenderfer, K.E.; Zhang, J.; Soltani, S.; et al. Differential Responses to Lithium in Hyperexcitable Neurons from Patients with Bipolar Disorder. Nature 2015, 527, 95–99. [Google Scholar] [CrossRef] [PubMed]
- Jiménez-Fernández, S.; Gurpegui, M.; Garrote-Rojas, D.; Gutiérrez-Rojas, L.; Carretero, M.D.; Correll, C.U. Oxidative Stress Parameters and Antioxidants in Patients with Bipolar Disorder: Results from a Meta-Analysis Comparing Patients, Including Stratification by Polarity and Euthymic Status, with Healthy Controls. Bipolar Disord. 2021, 23, 117–129. [Google Scholar] [CrossRef]
- Harrison, P.J.; Hall, N.; Mould, A.; Al-Juffali, N.; Tunbridge, E.M. Cellular Calcium in Bipolar Disorder: Systematic Review and Meta-Analysis. Mol. Psychiatry 2021, 26, 4106–4116. [Google Scholar] [CrossRef] [PubMed]
- Giorgio, V.; Guo, L.; Bassot, C.; Petronilli, V.; Bernardi, P. Calcium and Regulation of the Mitochondrial Permeability Transition. Cell Calcium 2018, 70, 56–63. [Google Scholar] [CrossRef] [PubMed]
- Marchi, S.; Patergnani, S.; Missiroli, S.; Morciano, G.; Rimessi, A.; Wieckowski, M.R.; Giorgi, C.; Pinton, P. Mitochondrial and Endoplasmic Reticulum Calcium Homeostasis and Cell Death. Cell Calcium 2018, 69, 62–72. [Google Scholar] [CrossRef] [PubMed]
- Belosludtsev, K.N.; Dubinin, M.V.; Belosludtseva, N.V.; Mironova, G.D. Mitochondrial Ca2+ Transport: Mechanisms, Molecular Structures, and Role in Cells. Biochemistry 2019, 84, 593–607. [Google Scholar] [CrossRef] [PubMed]
- Campbell, I.; Campbell, H. A Pyruvate Dehydrogenase Complex Disorder Hypothesis for Bipolar Disorder. Med. Hypotheses 2019, 130, 109263. [Google Scholar] [CrossRef] [PubMed]
- el-Mallakh, R.S.; Wyatt, R.J. The Na,K-ATPase Hypothesis for Bipolar Illness. Biol. Psychiatry 1995, 37, 235–244. [Google Scholar] [CrossRef] [PubMed]
- El-Mallakh, R.S.; Barrett, J.L.; Jed Wyatt, R. The Na,K-ATPase Hypothesis for Bipolar Disorder: Implications of Normal Development. J. Child Adolesc. Psychopharmacol. 1993, 3, 37–52. [Google Scholar] [CrossRef] [PubMed]
- Wang, F.; Yang, J.; Pan, F.; Ho, R.C.; Huang, J.H. Editorial: Neurotransmitters and Emotions. Front. Psychol. 2020, 11, 21. [Google Scholar] [CrossRef] [PubMed]
- Campbell, I.; Campbell, H. Mechanisms of Insulin Resistance, Mitochondrial Dysfunction and the Action of the Ketogenic Diet in Bipolar Disorder. Focus on the PI3K/AKT/HIF1-a Pathway. Med. Hypotheses 2020, 145, 110299. [Google Scholar] [CrossRef]
- Church, W.H.; Adams, R.E.; Wyss, L.S. Ketogenic Diet Alters Dopaminergic Activity in the Mouse Cortex. Neurosci. Lett. 2014, 571, 1–4. [Google Scholar] [CrossRef]
- Ari, C.; Kovács, Z.; Juhasz, G.; Murdun, C.; Goldhagen, C.R.; Koutnik, A.P.; Poff, A.M.; Kesl, S.L.; D’Agostino, D.P. Exogenous Ketone Supplements Reduce Anxiety-Related Behavior in Sprague-Dawley and Wistar Albino Glaxo/Rijswijk Rats. Front. Mol. Neurosci. 2016, 9, 137. [Google Scholar] [CrossRef]
- MacDonald, K.; Krishnan, A.; Cervenka, E.; Hu, G.; Guadagno, E.; Trakadis, Y. Biomarkers for Major Depressive and Bipolar Disorders Using Metabolomics: A Systematic Review. Am. J. Med. Genet. Part B Neuropsychiatr. Genet. Off. Publ. Int. Soc. Psychiatr. Genet. 2019, 180, 122–137. [Google Scholar] [CrossRef]
- Evans, S.J.; Bassis, C.M.; Hein, R.; Assari, S.; Flowers, S.A.; Kelly, M.B.; Young, V.B.; Ellingrod, V.E.; McInnis, M.G. The Gut Microbiome Composition Associates with Bipolar Disorder and Illness Severity. J. Psychiatr. Res. 2017, 87, 23–29. [Google Scholar] [CrossRef]
- Flowers, S.A.; Evans, S.J.; Ward, K.M.; McInnis, M.G.; Ellingrod, V.L. Interaction Between Atypical Antipsychotics and the Gut Microbiome in a Bipolar Disease Cohort. Pharmacotherapy 2017, 37, 261–267. [Google Scholar] [CrossRef]
- Coello, K.; Hansen, T.H.; Sørensen, N.; Munkholm, K.; Kessing, L.V.; Pedersen, O.; Vinberg, M. Gut Microbiota Composition in Patients with Newly Diagnosed Bipolar Disorder and Their Unaffected First-Degree Relatives. Brain Behav. Immun. 2019, 75, 112–118. [Google Scholar] [CrossRef]
- Dickerson, F.; Adamos, M.; Katsafanas, E.; Khushalani, S.; Origoni, A.; Savage, C.; Schweinfurth, L.; Stallings, C.; Sweeney, K.; Goga, J.; et al. Adjunctive Probiotic Microorganisms to Prevent Rehospitalization in Patients with Acute Mania: A Randomized Controlled Trial. Bipolar Disord. 2018, 20, 614–621. [Google Scholar] [CrossRef]
- Janssen, A.W.F.; Kersten, S. The Role of the Gut Microbiota in Metabolic Health. FASEB J. Off. Publ. Fed. Am. Soc. Exp. Biol. 2015, 29, 3111–3123. [Google Scholar] [CrossRef]
- Ding, Y.; Bu, F.; Chen, T.; Shi, G.; Yuan, X.; Feng, Z.; Duan, Z.; Wang, R.; Zhang, S.; Wang, Q.; et al. A Next-Generation Probiotic: Akkermansia Muciniphila Ameliorates Chronic Stress-Induced Depressive-like Behavior in Mice by Regulating Gut Microbiota and Metabolites. Appl. Microbiol. Biotechnol. 2021, 105, 8411–8426. [Google Scholar] [CrossRef]
- Needham, N.; Campbell, I.H.; Grossi, H.; Kamenska, I.; Rigby, B.P.; Simpson, S.A.; McIntosh, E.; Bahuguna, P.; Meadowcroft, B.; Creasy, F.; et al. Pilot Study of a Ketogenic Diet in Bipolar Disorder. BJPsych Open 2023, 9, e176. [Google Scholar] [CrossRef]
- Phelps, J.R.; Siemers, S.V.; El-Mallakh, R.S. The Ketogenic Diet for Type II Bipolar Disorder. Neurocase 2013, 19, 423–426. [Google Scholar] [CrossRef]
- Chmiel, I. Ketogenic Diet in Therapy of Bipolar Affective Disorder—Case Report and Literature Review. Psychiatr. Pol. 2022, 56, 1345–1363. [Google Scholar] [CrossRef]
- Campbell, I.H.; Campbell, H. Ketosis and Bipolar Disorder: Controlled Analytic Study of Online Reports. BJPsych Open 2019, 5, e58. [Google Scholar] [CrossRef]
- Campbell, I.H.; Needham, N.; Grossi, H.; Kamenska, I.; Luz, S.; Sheehan, S.; Thompson, G.; Thrippleton, M.J.; Gibbs, M.C.; Leitao, J.; et al. A Pilot Study of a Ketogenic Diet in Bipolar Disorder: Clinical, Metabolomic and Magnetic Resonance Spectroscopy Outcomes. Available online: https://www.medrxiv.org/content/10.1101/2023.10.23.23297391v1 (accessed on 19 March 2024).
- Kuopio University Hospital. Ketogenic Diet for Psychotic Disorders (PsyDiet). Available online: https://clinicaltrials.gov/study/NCT03873922?term=NCT03873922&rank=1 (accessed on 19 March 2024).
- Kelly, D. Ketogenic Diet in People with Schizophrenia. Available online: https://clinicaltrials.gov/study/NCT05968638?term=NCT05968638&rank=1 (accessed on 19 March 2024).
- Northern California Institute of Research and Education. Can Neural Network Instability in Schizophrenia Be Improved with a Very Low Carbohydrate Ketogenic Diet? Available online: https://clinicaltrials.gov/study/NCT05268809?term=NCT05268809&rank=1 (accessed on 19 March 2024).
- Chouinard, V.-A. Ketogenic and Nutritional Interventions for First Episode Bipolar Disorder. Available online: https://clinicaltrials.gov/study/NCT06221852?term=NCT06221852&rank=1 (accessed on 19 March 2024).
- Phillips, M. Examining Neurobiological Mechanisms Underlying the Therapeutic Effect of the Ketogenic Diet in Bipolar Disorder (BD). Available online: https://clinicaltrials.gov/study/NCT06081426?term=NCT06081426&rank=1 (accessed on 19 March 2024).
- Sethi, S. Impact of a Ketogenic Diet on Metabolic and Psychiatric Health in Patients with Bipolar Illness. Available online: https://clinicaltrials.gov/study/NCT05705063?term=NCT05705063&rank=1 (accessed on 19 March 2024).
- Liwinski, T. Ketogenic Diet for Depression (KETO-MOOD). Available online: https://clinicaltrials.gov/study/NCT06105762?term=NCT06105762&rank=1 (accessed on 19 March 2024).
- University of Oxford. Ketogenic Diet for Treatment-Resistant Depression: Dietary Interventions for MEntal Health Study (DIME). Available online: https://clinicaltrials.gov/study/NCT06091163?term=NCT06091163&rank=1 (accessed on 19 March 2024).
- Ohio State University. Ketogenic Intervention in Depression (KIND). Available online: https://clinicaltrials.gov/study/NCT06080932?term=NCT06080932&rank=1 (accessed on 19 March 2024).
- Bostock, E.C.S.; Kirkby, K.C.; Taylor, B.V.; Hawrelak, J.A. Consumer Reports of “Keto Flu” Associated With the Ketogenic Diet. Front. Nutr. 2020, 7, 20. [Google Scholar] [CrossRef]
- Bergqvist, A.G.C. Long-Term Monitoring of the Ketogenic Diet: Do’s and Don’ts. Epilepsy Res. 2012, 100, 261–266. [Google Scholar] [CrossRef]
- Armeno, M.; Araujo, C.; Sotomontesano, B.; Caraballo, R.H. Update on the adverse effects during therapy with a ketogenic diet in paediatric refractory epilepsy. Rev. Neurol. 2018, 66, 193–200. [Google Scholar]
- Włodarek, D. Role of Ketogenic Diets in Neurodegenerative Diseases (Alzheimer’s Disease and Parkinson’s Disease). Nutrients 2019, 11, 169. [Google Scholar] [CrossRef]
- Crosby, L.; Davis, B.; Joshi, S.; Jardine, M.; Paul, J.; Neola, M.; Barnard, N.D. Ketogenic Diets and Chronic Disease: Weighing the Benefits Against the Risks. Front. Nutr. 2021, 8, 702802. [Google Scholar] [CrossRef]
- Masood, W.; Annamaraju, P.; Suheb, M.Z.K.; Uppaluri, K.R. Ketogenic Diet. Available online: https://www.ncbi.nlm.nih.gov/books/NBK499830/ (accessed on 19 March 2024).
- Yancy, W.S.; Olsen, M.K.; Guyton, J.R.; Bakst, R.P.; Westman, E.C. A Low-Carbohydrate, Ketogenic Diet versus a Low-Fat Diet to Treat Obesity and Hyperlipidemia: A Randomized, Controlled Trial. Ann. Intern. Med. 2004, 140, 769–777. [Google Scholar] [CrossRef]
- Westman, E.C.; Yancy, W.S.; Edman, J.S.; Tomlin, K.F.; Perkins, C.E. Effect of 6-Month Adherence to a Very Low Carbohydrate Diet Program. Am. J. Med. 2002, 113, 30–36. [Google Scholar] [CrossRef] [PubMed]
- Kanikarla-Marie, P.; Jain, S.K. Hyperketonemia and Ketosis Increase the Risk of Complications in Type 1 Diabetes. Free Radic. Biol. Med. 2016, 95, 268–277. [Google Scholar] [CrossRef]
- Leow, Z.Z.X.; Guelfi, K.J.; Davis, E.A.; Jones, T.W.; Fournier, P.A. The Glycaemic Benefits of a Very-Low-Carbohydrate Ketogenic Diet in Adults with Type 1 Diabetes Mellitus May Be Opposed by Increased Hypoglycaemia Risk and Dyslipidaemia. Diabet. Med. J. Br. Diabet. Assoc. 2018, 35, 1258–1263. [Google Scholar] [CrossRef] [PubMed]
- McClean, A.-M.; Montorio, L.; McLaughlin, D.; McGovern, S.; Flanagan, N. Can a Ketogenic Diet Be Safely Used to Improve Glycaemic Control in a Child with Type 1 Diabetes? Arch. Dis. Child. 2019, 104, 501–504. [Google Scholar] [CrossRef] [PubMed]
- Desrosiers, T.A.; Siega-Riz, A.M.; Mosley, B.S.; Meyer, R.E. National Birth Defects Prevention Study Low Carbohydrate Diets May Increase Risk of Neural Tube Defects. Birth Defects Res. 2018, 110, 901–909. [Google Scholar] [CrossRef] [PubMed]
- Grotto, D.; Zied, E. The Standard American Diet and Its Relationship to the Health Status of Americans. Nutr. Clin. Pract. Off. Publ. Am. Soc. Parenter. Enter. Nutr. 2010, 25, 603–612. [Google Scholar] [CrossRef] [PubMed]
- Magrath, G.; MacDonald, A.; Whitehouse, W. Dietary Practices and Use of the Ketogenic Diet in the UK. Seizure 2000, 9, 128–130. [Google Scholar] [CrossRef] [PubMed]
- Kossoff, E.H.; Turner, Z.; Adams, J.; Bessone, S.K.; Avallone, J.; McDonald, T.J.W.; Diaz-Arias, L.; Barron, B.J.; Vizthum, D.; Cervenka, M.C. Ketogenic Diet Therapy Provision in the COVID-19 Pandemic: Dual-Center Experience and Recommendations. Epilepsy Behav. 2020, 111, 107181. [Google Scholar] [CrossRef] [PubMed]
- Whiteley, V.J.; Martin-McGill, K.J.; Carroll, J.H.; Taylor, H.; Schoeler, N.E. Ketogenic Dietitians Research Network (KDRN) Nice to Know: Impact of NICE Guidelines on Ketogenic Diet Services Nationwide. J. Hum. Nutr. Diet. Off. J. Br. Diet. Assoc. 2020, 33, 98–105. [Google Scholar] [CrossRef] [PubMed]
- Cervenka, M.C.; Wood, S.; Bagary, M.; Balabanov, A.; Bercovici, E.; Brown, M.-G.; Devinsky, O.; Di Lorenzo, C.; Doherty, C.P.; Felton, E.; et al. International Recommendations for the Management of Adults Treated With Ketogenic Diet Therapies. Neurol. Clin. Pract. 2021, 11, 385–397. [Google Scholar] [CrossRef]
- Sabé, M.; Pallis, K.; Solmi, M.; Crippa, A.; Sentissi, O.; Kaiser, S. Comparative Effects of 11 Antipsychotics on Weight Gain and Metabolic Function in Patients With Acute Schizophrenia: A Dose-Response Meta-Analysis. J. Clin. Psychiatry 2023, 84, 22r14490. [Google Scholar] [CrossRef]
- Correll, C.U.; Højlund, M.; Graham, C.; Todtenkopf, M.S.; McDonnell, D.; Simmons, A. Weight Gain and Metabolic Changes in Patients With First-Episode Psychosis or Early-Phase Schizophrenia Treated With Olanzapine: A Meta-Analysis. Int. J. Neuropsychopharmacol. 2023, 26, 451–464. [Google Scholar] [CrossRef]
- Ferrell, M.C.; Ernst, Z.; Ferrell, S.C.; Jaiswal, D.D.; Vassar, M. Effects of Statin Therapies on Individuals Taking Antipsychotics: A Systematic Review. J. Cardiovasc. Med. 2023, 24, 481–487. [Google Scholar] [CrossRef]
- Çağıran, İ.H.; Yılmaz, D.A. Ketogenic Diet in Clinical Practices. Hum. Nutr. Metab. 2024, 36, 200250. [Google Scholar] [CrossRef]
- Dauriac-Le Masson, V.; Bornes, C.; Hadjedj, L.; Montariol, P.; Nguyen-Machet, S.; Hallouche, N. Constipation in Hospitalized Psychiatric Patients: An Underestimated Common Phenomenon. Retrospective Epidemiological Study in an Adult Psychiatric Hospital Setting. L’Encephale 2024, in press. [Google Scholar] [CrossRef]
- Garofalo, V.; Barbagallo, F.; Cannarella, R.; Calogero, A.E.; La Vignera, S.; Condorelli, R.A. Effects of the Ketogenic Diet on Bone Health: A Systematic Review. Front. Endocrinol. 2023, 14, 1042744. [Google Scholar] [CrossRef] [PubMed]
- Holick, M.F. Optimal Vitamin D Status for the Prevention and Treatment of Osteoporosis. Drugs Aging 2007, 24, 1017–1029. [Google Scholar] [CrossRef] [PubMed]
- Ferraris, C.; Guglielmetti, M.; Neri, L.d.C.L.; Allehdan, S.; Mohsin Albasara, J.M.; Fareed Alawadhi, H.H.; Trentani, C.; Perna, S.; Tagliabue, A. A Review of Ketogenic Dietary Therapies for Epilepsy and Neurological Diseases: A Proposal to Implement an Adapted Model to Include Healthy Mediterranean Products. Foods 2023, 12, 1743. [Google Scholar] [CrossRef]
- Erkent, I.; Ilgaz, F.; Dericioglu, N. Difficulties in the Implementation of the Ketogenic Diet in Adult Patients with Refractory Epilepsy. Epilepsy Behav. 2023, 144, 109234. [Google Scholar] [CrossRef]
- Burrows, T.; Teasdale, S.; Rocks, T.; Whatnall, M.; Schindlmayr, J.; Plain, J.; Latimer, G.; Roberton, M.; Harris, D.; Forsyth, A. Effectiveness of Dietary Interventions in Mental Health Treatment: A Rapid Review of Reviews. Nutr. Diet. 2022, 79, 279–290. [Google Scholar] [CrossRef]
- Barrett, S.; Begg, S.; O’Halloran, P.; Kingsley, M. Integrated Motivational Interviewing and Cognitive Behaviour Therapy for Lifestyle Mediators of Overweight and Obesity in Community-Dwelling Adults: A Systematic Review and Meta-Analyses. BMC Public Health 2018, 18, 1160. [Google Scholar] [CrossRef]
- Teasdale, S.B.; Ward, P.B.; Samaras, K.; Firth, J.; Stubbs, B.; Tripodi, E.; Burrows, T.L. Dietary Intake of People with Severe Mental Illness: Systematic Review and Meta-Analysis. Br. J. Psychiatry 2019, 214, 251–259. [Google Scholar] [CrossRef]
- Tabele Składu i Wartości Odżywczej Żywności. Available online: https://pzwl.pl/Tabele-skladu-i-wartosci-odzywczej-zywnosci,145994761,p.html (accessed on 18 March 2024).

| Author(s), Year | Study Design | Number of Participants (Intervention/Control) | Range Age of Participants (Years) | Dietary Intervention/ Assessment of Ketosis | Control Intervention | Duration | Outcome Measures | Main Findings |
|---|---|---|---|---|---|---|---|---|
| Pacheco et al., 1965 [61] | Pilot study | I: 10 (F) | 19–63 | KD, lack of detailed information | none | 2 weeks | A nursing checklist for ward behavior ratings, The Minimal Social Behavior Scale, The Beckomberga Rating Scale for the S-Factor | ↓symptomatology, ↑symptomatology after discontinuing the KD |
| Kraft et al., 2009 [64] | Case study | I: 1 (F) | 70 | gluten and low-carbohydrate KD, (<20 g carbohydrates per day), ketosis was not confirmed | none | 1 year | Patients’ and physicians’ observations | ↓symptomatology (visual and auditory hallucinations), ↓body weight, ↑energy level |
| Palmer et al., 2019 [63] | Two case studies | I: 2 (F) | 82 and 39 | KD, lack of detailed information | none | 5 years and 12 years | Patients’ and physicians’ observations | ↓symptomatology, ↓body weight, ↓the amount of taken medications |
| Sethi et al., 2024 [62] | Pilot study | I: 5 | 18–75 | KD, 10% carbohydrate, 30% protein, 60% fat; ≥5040 kJ, <20 g carbohydrates per day; blood ketone meter at least once a week | none | 4 months | Generalized Anxiety Disorder (GAD–7), Patient Health Questionnaire Depression Scale (PHQ–9), Pittsburgh Sleep Quality Index (PSQI), Clinical Mood Monitoring Forms (CMF), Clinical Global Impression–Schizophrenia (CGI–SCH) Scale, Global Assessment of Functioning (GAF), Manchester Short Assessment of Quality of Life (MANSA), Brief Psychiatric Rating Scale (BPRS) for Schizophrenia and screening for suicidality; HbA1c, fatty acid profile, hsCRP, HOMA-IR, HOMA2-IR, advanced lipid testing, body weight, blood pressure, HR, waist circumference, body composition analysis | 32% reduction in Brief Psychiatric Rating Scale, ↑proportion of participants who were in the recovery state at baseline *, ↑sleep quality *, improvement in cognition and mood, ↓anxiety, ↓depressive symptoms *, improvement in CGI scale, ↑life quality and satisfaction *, ↓body weight, waist circumference, systolic blood pressure, FMI, BMI *, ↓visceral adipose tissue, HbA1c, triglycerides, HOMA-IR * |
| Author(s), Year | Study Design | Number of Participants (Intervention/ Control) | Range Age of Participants (Years) | Dietary Intervention/ Assessment of Ketosis | Control Intervention | Duration | Outcome Measures | Main Findings |
|---|---|---|---|---|---|---|---|---|
| Cox et al., 2019 [83] | Case study | I: 1 (F) | 65 | KD, 65% fat, 25% protein, 10% carbohydrates with a time restricted feeding window; Nutritional education; High-intensity interval training; blood ketones pre/post intervention | none | 12 weeks | The Patient Health Questionnaire 9 (PHQ-9), The General Self-Efficacy Scale (GSE), MetS Compliance Questionnaire (MSC), blood: HgA1C, glucose, ketones, HOMA-IR, the triglyceride/HDL cardiac risk ratio | Improvement in PHQ-9, GSE, and MSC scales; ↓HgA1C, glucose ketones, HOMA-IR, and triglycerides/HDL cardiac list ratio; ↓body weight; ↓amount of taken medications; ↑self-confidence, self-efficacy, energy, mood stability and cognition; sleep improvement |
| Pieklik et al., 2021 [74] | Case study | I: 1 (F) | 21 | KD, the Kalibra medical protocol diet; the urine ketone strip test | none | 4 weeks | Body Image Questionnaire (KWCO), Scale of satisfaction with parts and parameters of the body, The Scale for the Using of Methods for Correcting Appearance, Scale of Perception of Peer Messages, Scale of Self Constructs and Beck Depression Inventory Scale (BDI) | ↓body weight, mood stabilization, stabilization of daily rhythm, ↓anxiety, Improvement in BDI scale, a lack of suicidal thoughts |
| Danan et al., 2022 [82] | Retrospective analysis | I: 31; bipolar disorder type two (n = 13), schizoaffective disorder (n = 12), major depressive disorder (n = 7) | 27–73 | KD, <20 g (5%) carbohydrates per day, 15–20% protein, 75–80% fat; measurement of urine acetoacetate at least one time during the intervention period | none | 6–248 days | Hamilton Depression Rating Scale (HAM-D), Montgomery–Åsberg Depression Rating Scale (MADRS), Positive and Negative Syndrome Scale (PANSS), Clinical Global Impressions Scale (CGI-S), metabolic health measures | improvement in HAM-D, MADRS and CGI-S scales; ↓the amount of taken medications; ↓body weight, blood pressure, blood glucose, and triglycerides |
| Author(s), Year | Study Design | Number of Participants (Intervention/ Control) | Range Age of Participants (Years) | Dietary Intervention/ Assessment of Ketosis | Control Intervention | Duration | Outcome Measures | Main Findings |
|---|---|---|---|---|---|---|---|---|
| Phelps et al., 2013 [114] | Two case studies | I: 2 (F) | 69 and 30 | KD, 8% carbohydrates, 22% protein, 70% fat (second case), the urine ketone strip test (first case) | none | 2 years, 3 years | Patients’ and physicians’ observations | significant subjective reduction in symptoms, ↓the amount of taken medications, ↓depressive symptoms mood stabilization, ↑calm and confidence, comfort |
| Chmiel et al., 2022 [115] | Case study | I: 1 (M) | 32 | KD; 5% carbohydrate, 15% protein, 80% fat; ≥5040 kJ, <30 g carbohydrates per day; cyclic one-day fast introduced every 7–10 days, blood concentration of β-hydroxybutyrate | none | 2 years | Body mass index (BMI), blood: CBC, lipid profile, glucose, liver tests, creatinine, uric acid | mood stabilization, elimination of anxiety, shorter and milder depressive states till complete remission, ↑mood, ↑energy, ↑cognitive functions and concentration, ↑periods of total remission of symptoms, ↓amount of taken medications, ↑HDL, ↓triglycerides |
| Needham et al., 2023 [113] | Pilot study | I: 27 | 26–54 | A modified KD, 60–75% fat, 5–7% carbohydrates, additionally calories from protein, blood ketones | none | 6–8 weeks | Medical and medication history, blood pressure and body mass index (BMI), Affective Lability Scale 18, Beck’s Depression Inventory, Young Mania Rating Scale, Within Trial Resource Use Questionnaire, EuroQol 5D quality of life instrument and the Work Productivity and Activity Impairment Questionnaire (tailored), Fasting venepuncture and MR brain scans, measurement of glucose and ketones on a KetoMojo device, daily ecological momentary assessments (EMAs) of anxiety, mood, energy, impulsivity and speed of thought, Visual Analogue Scale (VAS) | ↓body weight, normalization of total cholesterol, LDL, and triglyceride levels EQ5D-5L at baseline and follow-up, respectively, were: mobility, 90 and 85%; self-care, 90 and 85%; usual activities, 65 and 55%; pain and discomfort, 45 and 45%; and anxiety and depression, 45 and 50% The visual analogue scale (VAS) utility scores at baseline and follow up were 66.7 and 64.2, ↓mean expenditure, ↑mean productivity loss |
| Sethi et al., 2024 [62] | Pilot study | I: 16 | 18–75 | KD, 10% carbohydrate, 30% protein, 60% fat; ≥5040 kJ, <20 g carbohydrates per day; blood ketone meter at least once a week | none | 4 months | Generalized Anxiety Disorder (GAD–7), Patient Health Questionnaire Depression Scale (PHQ–9), Pittsburgh Sleep Quality Index (PSQI), Clinical Mood Monitoring Forms (CMF), Clinical Global Impression–Schizophrenia (CGI–SCH) Scale, Global Assessment of Functioning (GAF), Manchester Short Assessment of Quality of Life (MANSA), Brief Psychiatric Rating Scale (BPRS) for Schizophrenia and screening for suicidality; HbA1c, fatty acid profile, hsCRP, HOMA-IR, HOMA2-IR, advanced lipid testing, body weight, blood pressure, HR, waist circumference, body composition analysis | improvement in CGI scale: severity of mental illness showed improvement of >1 point in 69% of participants, ↑proportion of participants who were in the recovery state at baseline *, ↑sleep quality *, ↓anxiety *, ↓depressive symptoms, ↑life quality and satisfaction *, ↓body weight, waist and circumference and systolic blood pressure and FMI and BMI * ↓visceral adipose tissue, HbA1c, triglycerides, HOMA-IR * |
| Identifier | Study Title | Status | Locations | Conditions | Hospitalized/ Amulatory Patients | Age of Participants | Enrollment | Intervention | Control | Timeframe | Primary Outcome and Timeframe |
|---|---|---|---|---|---|---|---|---|---|---|---|
| NCT03873922 [118] | Dietary Intervention for Psychotic Disorders: a Pilot Intervention Study of Ketogenic Diet for Psychotic Symptoms—PsyDiet Pilot Study | Recruiting | Kuopio, Finland | Patients with psychotic symptoms (ICD-10 diagnosis F20-29) | Hospitalized | ≥18 | 40 | Ketogenic diet (15–20 g CHO/d) | Conventional hospital meals | 6 weeks | Changes in PANSS and diet feasibility |
| NCT05968638 [119] | Single-Blind Randomized Ketogenic Diet vs. Control Diet in People With Schizophrenia | Recruiting | Catonsville, Maryland, United States | Schizophrenia/Schizoaffective disorder (DSM-IV/DSM-5) | N/A | 18–64 | 50 | Ketogenic diet | Standard diet | 3 months | Changes in BPRS |
| NCT05268809 [120] | Can Neural Network Instability in Schizophrenia be Improved With a Very Low Carbohydrate Ketogenic Diet? | Recruiting | San Francisco, California, United States | Schizophrenia/Schizoaffective disorder/Bipolar disorder (SCID-5) | Ambulatory | 18–65 | 70 | Ketogenic diet (70% F; 10% CHO; 20% PRO); 3 meals + snak/d | The diet as usual | 4 weeks | Changes in network stabilization, cognition, waist to hip ratio, HOMA-IR, blood: CRP |
| NCT06221852 [121] | A Randomized Controlled Clinical Trial of Ketogenic and Nutritional Interventions for Brain Energy Metabolism and Psychiatric Symptoms in First Episode Bipolar Disorder | Not yet recruiting | Belmont, Massachusetts, United States | Bipolar disorder/Schizoaffective disorder, onset of illness in the last 7 years (DSM-5) | N/A | 18–45 | 50 | Ketogenic diet (75–80% F; 7% CHO; 13–18% PRO); 3 meals + snak/d; normocaloric | Dietary Guidelines for Americans; 3 meals + snak/d; normocaloric | 12 weeks | Changes in PANSS, HAM-D, YMRS, CGI, insulin resistance, brain NAD+/NADH ratio and creatine kinase forward reaction rate |
| NCT06081426 [122] | Elucidating Neurobiological Mechanisms Underlying the Therapeutic Effect of the Ketogenic Diet in Bipolar Disorder (BD): a Multidisciplinary Mechanistic Study | Recruiting | Pittsburgh, Pennsylvania, United States | Bipolar disorder I/Bipolar disorder II, hypomanic/euthymic (DSM-5) | N/A | 18–30 | 107 | Ketogenic diet | Non-ketogenic diet/No diet | 8–10 weeks | Changes in YMRS, brain activity and connectivity, brain concentration of GABA, glutamate, lactate, blood: glucose, lipids, bilirubin, total protein, albumin, liver enzymes |
| NCT05705063 [123] | Impact of A Low-Carbohydrate, High-Fat, Ketogenic Diet on Obesity, Metabolic Abnormalities, and Psychiatric Symptoms on Patients With Bipolar Disorder (BPD) | Not yet recruiting | Stanford, California, United States | Bipolar disorder (DSM-5) | N/A | 18–75 | 30 | Ketogenic diet | No control group | 6 weeks | Changes in weight, waist circumference, visceral fat mass, body fat mass, heart rate, blood pressure, HOMA-IR, blood: HbA1c, hs-CRP, lipids |
| NCT06105762 [124] | KETO-MOOD: Ketogenic Diet for Microbiome Optimization and Overcoming Depression | Not yet recruiting | Basel, Switzerland | Major Depressive Disorder/Bipolar Depression (ICD-10/ICD-11) | N/A | 18–70 | 120 | Ketogenic diet (MAD, <20 g CHO/d) | Mixed diet following the recommendations for healthy nutrition by the Schweizerische Gesellschaft für Ernährung (Société Suisse de Nutrition) (45–60% CHO) | 8 weeks | Changes in HAM-D17 |
| NCT05558995 [85] | Effects and Mechanistic Aspects of Ketogenic Diet in Individuals With Major Depressive Disorder: A Pilot Study | Recruiting | Kingston, Ontario, Canada | Major Depressive Disorder (DSM-5) | Ambulatory | 18–55 | 10 | Ketogenic diet (20–30 g CHO/d; 80–100 g PRO/d; PUFA; MUFA) + vitamins, minerals in caps | No control group | 12 weeks | Adherence to diet |
| NCT06091163 [125] | A Randomised Controlled Trial Evaluating the Efficacy and Mechanisms of a Ketogenic Diet as an Adjunctive Treatment for People With Treatment-resistant Depression | Recruiting | Oxford, United Kingdom | Depression | Ambulatory | 18–65 | 100 | Ketogenic diet (20–50 g CHO estimated on a 2000 kcal/d); 3 meals + snacks | Modified fat and phytonutrient diet | 6 weeks | Changes in PHQ-9 |
| NCT06080932 [126] | Ketogenic Intervention in Depression | Recruiting | Columbus, Ohio, United States | Major Depressive Disorder (DSM-5) | Ambulatory | 18–30 | 30 | Ketogenic diet (<50 g CHO/d, ~1.5 g PRO/kg reference weight) | No control group | ~up to 12 weeks | Changes in HAM-D17, WHO-5, blood: ketones and glucose |
| Potential Risk | Risk Group | Advice |
|---|---|---|
| Dyslipidemia | Patients treated with atypical antipsychotic medication. Overweight or obese individuals. | Replace foods with high SFA and trans unsaturated fatty acid with sources of PUFA and MUFA. Less: meat with high-fat content, lard, butter, eggs, coconut/palm oil More: olive oil, rapeseed oil, flax oil, avocado, fatty fish, allowed amounts of nuts and seeds Supplementation of omega-3 fatty acids (>1 g EPA or EPA/DHA ratio 1:1) could be helpful |
| Constipation | Patients treated with medication with anticholinergic effects (clozapine, olanzapine, phenothiazine derivatives, TCA72). | Choose vegetables, nuts, and seeds with more fiber and less carbohydrate content; the examples of the ratio of fiber to carbohydrate in some foods are presented below: Spinach 1:1.15 Sesame 1:1.27 Desiccated coconut 1:1.28 Mushrooms 1:1.3 Chives 1:1.56 Celery tuber 1:1.57 Almonds 1:1.59 Kale 1:1.6 Brussels sprout 1:1.6 Hazelnut 1:1.67 Chinese cabbage 1:1.68 Horseradish 1:1.76 Green beans 1:1.95 Lettuce 1:2.07 Broccoli 1:2.08 Cauliflower 1:2.08 Parsley, root 1:2.14 Peanuts 1:2.63 Red cabbage 1:2.68 Walnuts 1:2.77 Tomatoes 1:3 Zucchini 1:3.2 Red pepper 1:3.3 Cucumber, pickled 1:3.8 Onion 1:4.05 Cucumber 1:5.8 * |
| Calcium deficiency, osteoporosis risk | Patients treated with SSRI, valproic acid and with high prolactin levels after pharmacotherapy. | Supplementation of vitamin D according to guidelines. Monitoring vitamin D status. Intake of foods rich in Ca allowed on KD, such as: cheese (hard cheese, feta, mozzarella), Greek yoghurt, cream, or vegetables with a high ratio of Ca to P. The ratio of Ca to P in some foods is presented below; 1:1 or higher Ca is recommended. Kale 1:0.36 Parsley, leaves 1:0.44 Cabbage, white 1:0.49 Cheese, Emmentaler 1:0.5 Sauerkraut 1:0.5 Chives 1:0.54 Onion 1:0.56 Brussels, sprout 1:0.58 Cheese, parmesan 1:0.59 Cheese, brie 1:0.63 Pumpkin 1:0.65 Cabbage, red 1:0.67 Cheese, camembert 1:0.8 Cabbage, Chinese 1:0.82 Broccoli 1:1.38 Cucumber, pickled 1:1.5 Cucumber 1:1.53 Almonds 1:1.9 Cauliflower 1:2.15 Walnuts 1:3.82 Sunflower seeds 1:5.98 Peanuts 1:6.64 Egg, white 1:8.5 Cod 1:92 Roast beef 1:95.5 Chicken, leg 1:98 Egg 1:102 Breast, chicken 1:120 Salmon 1:133 Egg, yolk 1:293 ** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rog, J.; Wingralek, Z.; Nowak, K.; Grudzień, M.; Grunwald, A.; Banaszek, A.; Karakula-Juchnowicz, H. The Potential Role of the Ketogenic Diet in Serious Mental Illness: Current Evidence, Safety, and Practical Advice. J. Clin. Med. 2024, 13, 2819. https://doi.org/10.3390/jcm13102819
Rog J, Wingralek Z, Nowak K, Grudzień M, Grunwald A, Banaszek A, Karakula-Juchnowicz H. The Potential Role of the Ketogenic Diet in Serious Mental Illness: Current Evidence, Safety, and Practical Advice. Journal of Clinical Medicine. 2024; 13(10):2819. https://doi.org/10.3390/jcm13102819
Chicago/Turabian StyleRog, Joanna, Zuzanna Wingralek, Katarzyna Nowak, Monika Grudzień, Arkadiusz Grunwald, Agnieszka Banaszek, and Hanna Karakula-Juchnowicz. 2024. "The Potential Role of the Ketogenic Diet in Serious Mental Illness: Current Evidence, Safety, and Practical Advice" Journal of Clinical Medicine 13, no. 10: 2819. https://doi.org/10.3390/jcm13102819
APA StyleRog, J., Wingralek, Z., Nowak, K., Grudzień, M., Grunwald, A., Banaszek, A., & Karakula-Juchnowicz, H. (2024). The Potential Role of the Ketogenic Diet in Serious Mental Illness: Current Evidence, Safety, and Practical Advice. Journal of Clinical Medicine, 13(10), 2819. https://doi.org/10.3390/jcm13102819









