Efficacy of Bilateral Cochlear Implantation in Pediatric and Adult Patients with Profound Sensorineural Hearing Loss: A Retrospective Analysis in a Developing European Country
Abstract
1. Introduction
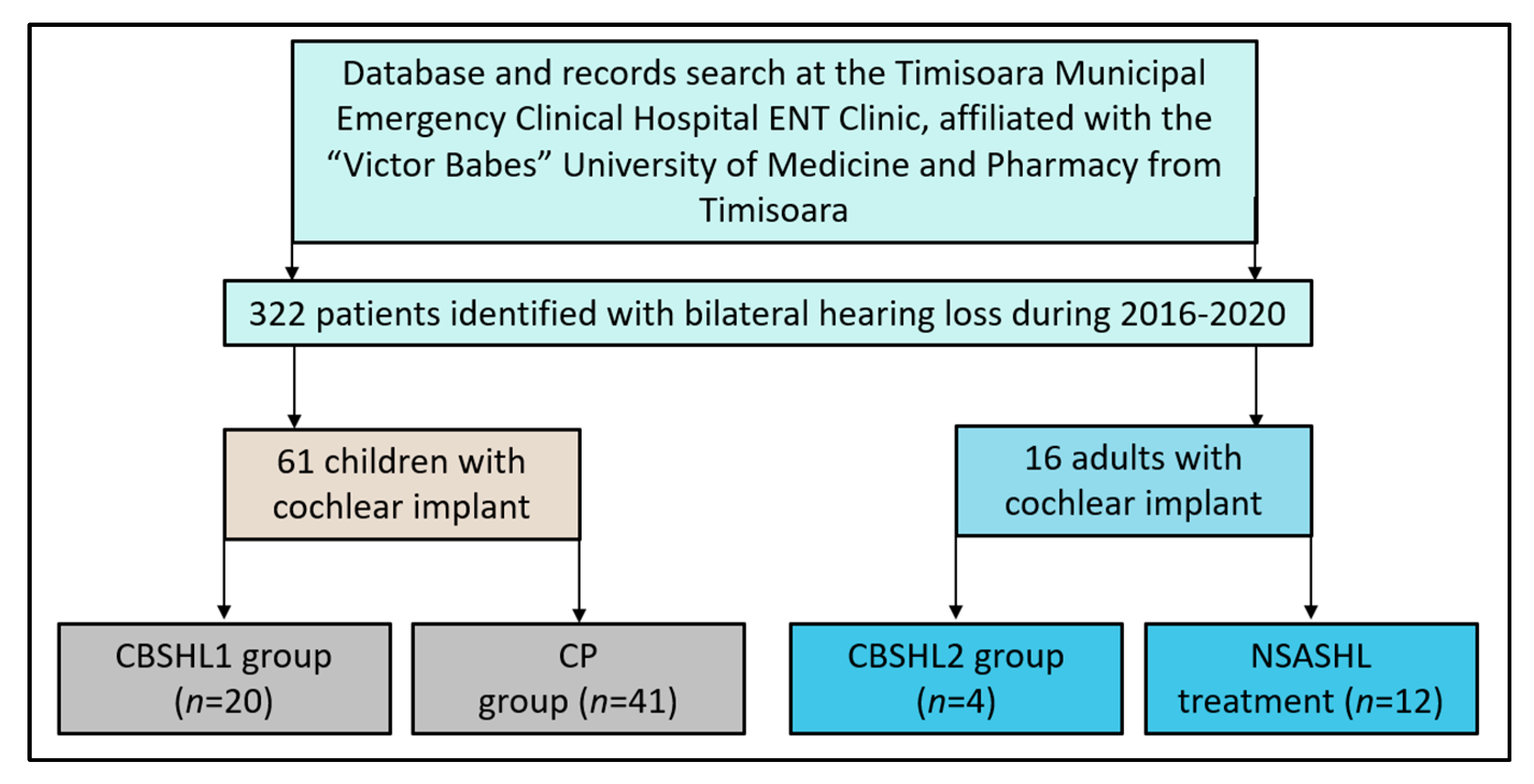
2. Materials and Methods
2.1. Study Design and Variables
2.2. Patient Eligibility and Study Groups
2.3. Statistical Analysis
3. Results
3.1. Patients’ Background
3.2. Audiology Assessment
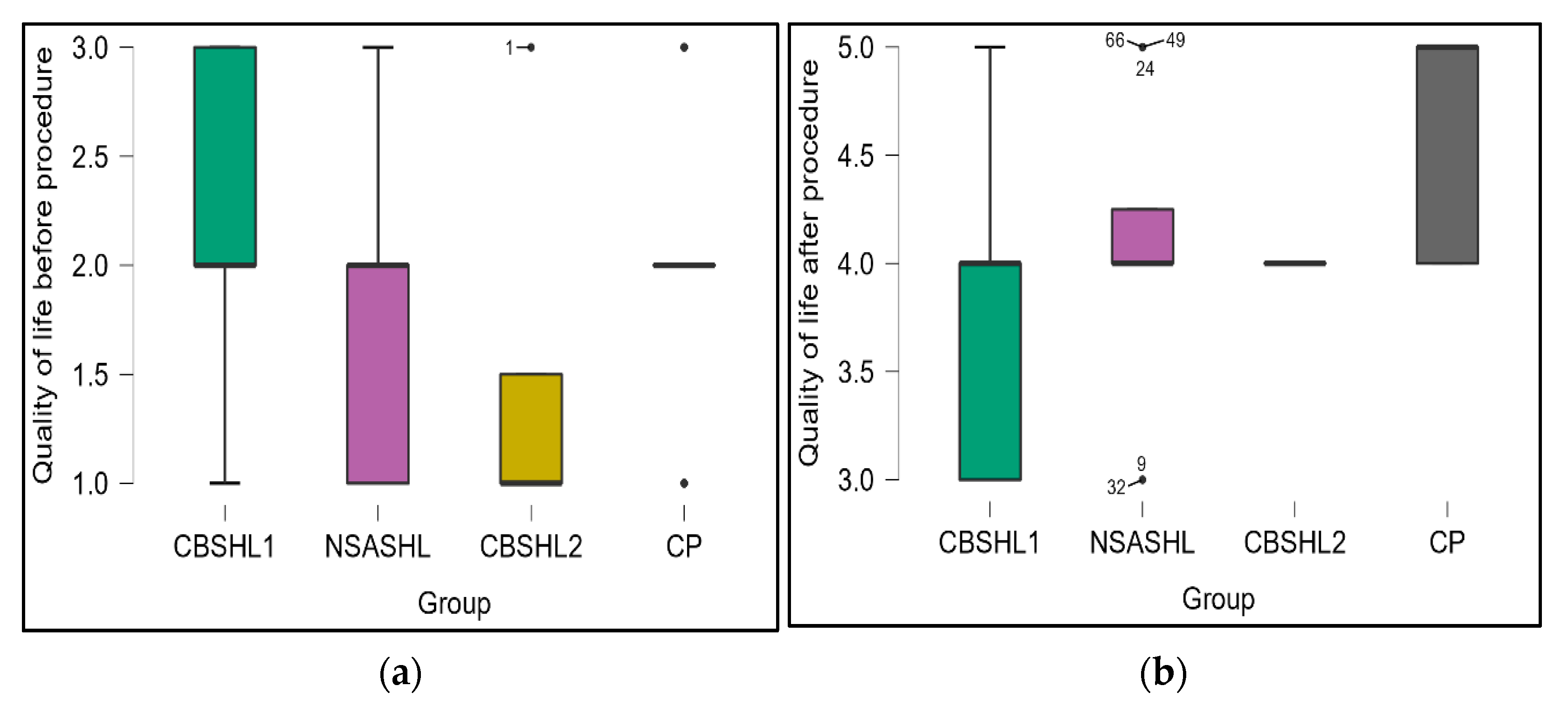
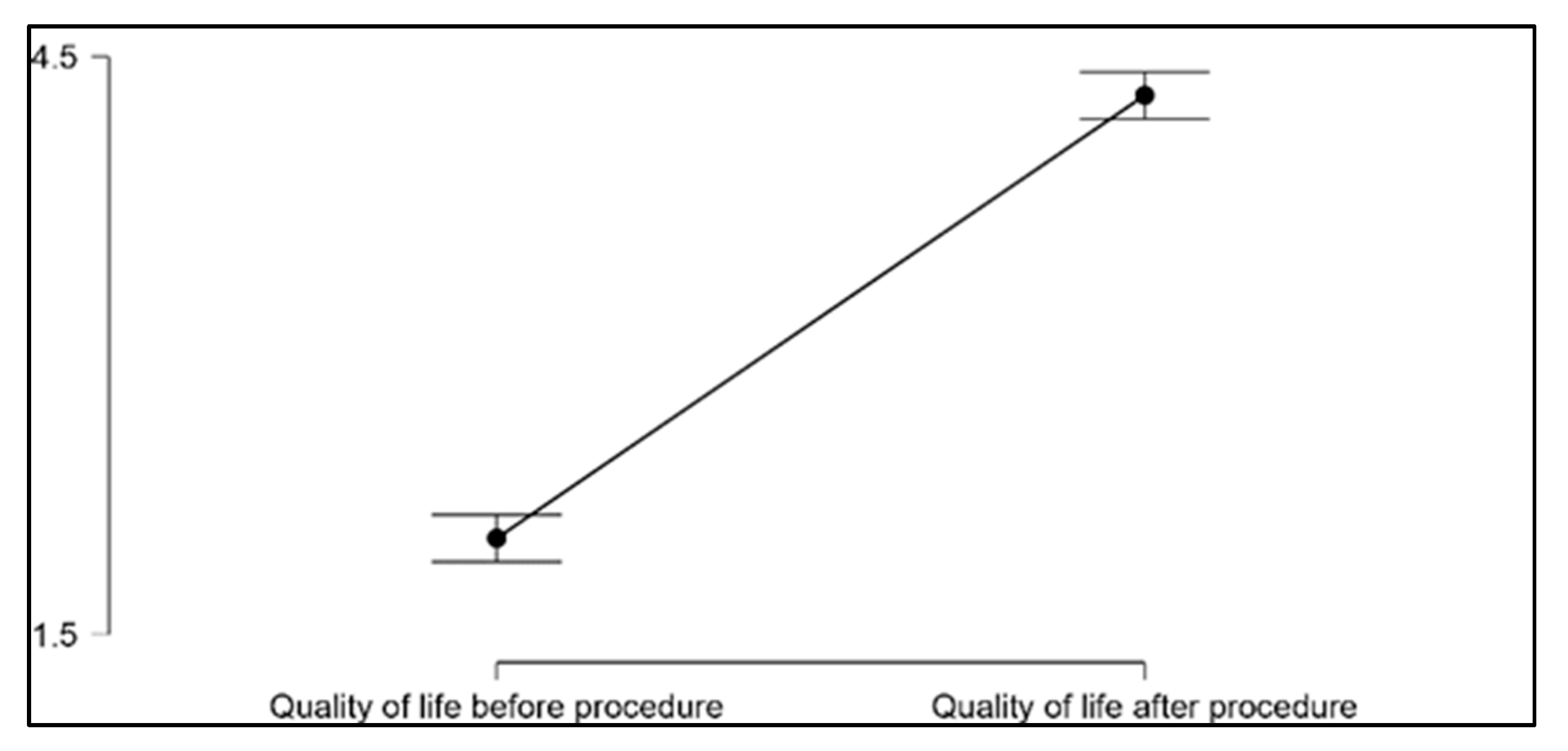
3.3. Quality of Life Assessment
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Carlson, M.L. Cochlear Implantation in Adults. N. Engl. J. Med. 2020, 382, 1531–1542. [Google Scholar] [CrossRef] [PubMed]
- Clinkard, D.; Barbic, S.; Amoodi, H.; Shipp, D.; Lin, V. The Economic and Societal Benefits of Adult Cochlear Implant Implantation: A Pilot Exploratory Study. Cochlear Implant. Int. 2015, 16, 181–185. [Google Scholar] [CrossRef] [PubMed]
- Calháu, C.M.D.F.; Lima Júnior, L.R.P.; Reis, A.M.D.C.D.S.; Capistrano, A.K.B.; Lima, D.D.V.S.P.; Calháu, A.C.D.F.; Rodrigues Júnior, F.D.A. Perfil Etiológico Dos Pacientes Implantados Do Programa de Implante Coclear. Braz. J. Otorhinolaryngol. 2011, 77, 13–18. [Google Scholar] [CrossRef]
- Teagle, H.F.B.; Park, L.R.; Brown, K.D.; Zdanski, C.; Pillsbury, H.C. Pediatric Cochlear Implantation: A Quarter Century in Review. Cochlear Implant. Int. 2019, 20, 288–298. [Google Scholar] [CrossRef]
- Beer, J.; Kronenberger, W.G.; Pisoni, D.B. Executive Function in Everyday Life: Implications for Young Cochlear Implant Users. Cochlear Implant. Int. 2011, 12, S89–S91. [Google Scholar] [CrossRef]
- Vahedi, S. World Health Organization Quality-of-Life Scale (WHOQOL-BREF): Analyses of Their Item Response Theory Properties Based on the Graded Responses Model. Iran J. Psychiatry 2010, 5, 140–153. [Google Scholar]
- De Sousa, A.F.; Couto, M.I.V.; Martinho-Carvalho, A.C. Quality of Life and Cochlear Implant: Results in Adults with Postlingual Hearing Loss. Braz. J. Otorhinolaryngol. 2018, 84, 494–499. [Google Scholar] [CrossRef] [PubMed]
- Aloqaili, Y.; Arafat, A.S.; Almarzoug, A.; Alalula, L.S.; Hakami, A.; Almalki, M.; Alhuwaimel, L. Knowledge about Cochlear Implantation: A Parental Perspective. Cochlear Implants Int. 2019, 20, 74–79. [Google Scholar] [CrossRef] [PubMed]
- Khater, A.; El-Anwar, M. Methods of Hearing Preservation during Cochlear Implantation. Int. Arch. Otorhinolaryngol. 2017, 21, 297–301. [Google Scholar] [CrossRef]
- Vincenti, V.; Bacciu, A.; Guida, M.; Marra, F.; Bertoldi, B.; Bacciu, S.; Pasanisi, E. Pediatric Cochlear Implantation: An Update. Ital. J. Pediatr. 2014, 40, 72. [Google Scholar] [CrossRef] [PubMed]
- McKinney, S. Cochlear Implantation in Children under 12 Months of Age. Curr. Opin. Otolaryngol. Head Neck Surg. 2017, 25, 400–404. [Google Scholar] [CrossRef]
- Firestone, G.M.; McGuire, K.; Liang, C.; Zhang, N.; Blankenship, C.M.; Xiang, J.; Zhang, F. A Preliminary Study of the Effects of Attentive Music Listening on Cochlear Implant Users’ Speech Perception, Quality of Life, and Behavioral and Objective Measures of Frequency Change Detection. Front. Hum. Neurosci. 2020, 14, 110. [Google Scholar] [CrossRef] [PubMed]
- Craddock, L.; Cooper, H.; Riley, A.; Wright, T. Cochlear Implants for Pre-Lingually Profoundly Deaf Adults. Cochlear Implants Int. 2016, 17, 26–30. [Google Scholar] [CrossRef] [PubMed]
- Vieira, S.D.S.; Bevilacqua, M.C.; Ferreira, N.M.L.A.; Dupas, G. Cochlear Implant: The Complexity Involved in the Decision Making Process by the Family. Rev. Lat. Am. Enferm. 2014, 22, 415–424. [Google Scholar] [CrossRef]
- Contrera, K.J.; Choi, J.S.; Blake, C.R.; Betz, J.F.; Niparko, J.K. Rates of Long-Term Cochlear Implant Use in Children. Otol. Neurotol. 2014, 35, 5. [Google Scholar] [CrossRef]
- Chao, T.N.; Levi, J.; O’Reilly, R.C. How Old Is Too Old for Cochlear Implantation for Congenital Bilateral Sensorineural Hearing Loss? Cochlear Implantation Age in Congenital SNHL. Laryngoscope 2018, 128, 2221–2222. [Google Scholar] [CrossRef] [PubMed]
- Rijke, W.J.; Vermeulen, A.M.; Wendrich, K.; Mylanus, E.; Langereis, M.C.; van der Wilt, G.J. Capability of Deaf Children with a Cochlear Implant. Disabil. Rehabil. 2021, 43, 1989–1994. [Google Scholar] [CrossRef] [PubMed]
- Crisan, A.F.; Oancea, C.; Timar, B.; Fira-Mladinescu, O.; Tudorache, V. Falls, an underestimated risk in COPD. Eur. Respir. J. 2015, 46, PA3070. [Google Scholar] [CrossRef]
- Alegre-de la Rosa, O.M.; Villar-Angulo, L.M. Health-Related Quality of Life in Children Who Use Cochlear Implants or Hearing Aids. Heliyon 2020, 6, e03114. [Google Scholar] [CrossRef] [PubMed]
- Bianchin, G.; Tribi, L.; Formigoni, P.; Russo, C.; Polizzi, V. Sequential Pediatric Bilateral Cochlear Implantation: The Effect of Time Interval between Implants. Int. J. Pediatr. Otorhinolaryngol. 2017, 102, 10–14. [Google Scholar] [CrossRef] [PubMed]
- Mosnier, I.; Lahlou, G.; Flament, J.; Mathias, N.; Ferrary, E.; Sterkers, O.; Bernardeschi, D.; Nguyen, Y. Benefits of a Contralateral Routing of Signal Device for Unilateral Naída CI Cochlear Implant Recipients. Eur. Arch. Otorhinolaryngol. 2019, 276, 2205–2213. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.-S.; Hong, S.H.; Kim, E.Y.; Choi, J.E.; Chung, W.-H.; Cho, Y.-S.; Moon, I.J. Benefit and Predictive Factors for Speech Perception Outcomes in Pediatric Bilateral Cochlear Implant Recipients. Braz. J. Otorhinolaryngol. 2019, 85, 571–577. [Google Scholar] [CrossRef] [PubMed]
- Aimoni, C.; Ciorba, A.; Hatzopoulos, S.; Ramacciotti, G.; Mazzoli, M.; Bianchini, C.; Rosignoli, M.; Skarżyński, H.; Skarżyński, P.H. Cochlear Implants in Subjects Over Age 65: Quality of Life and Audiological Outcomes. Med. Sci. Monit. 2016, 22, 3035–3042. [Google Scholar] [CrossRef] [PubMed]
- Vieira, S.D.S.; Dupas, G.; Chiari, B.M. Repercussões Do Implante Coclear Na Vida Adulta. CoDAS 2018, 30, e20180001. [Google Scholar] [CrossRef] [PubMed]
- Barata, P.I.; Crisan, A.F.; Maritescu, A.; Negrean, R.A.; Rosca, O.; Bratosin, F.; Citu, C.; Oancea, C. Evaluating Virtual and Inpatient Pulmonary Rehabilitation Programs for Patients with COPD. J. Pers. Med. 2022, 12, 1764. [Google Scholar] [CrossRef] [PubMed]
- Bourn, S.; Goldstein, M.R.; Jacob, A. Hearing Preservation in Elderly Cochlear Implant Recipients. Otol. Neurotol. 2020, 41, 618–624. [Google Scholar] [CrossRef] [PubMed]
- McKinnon, B.J. Cost Effectiveness of Cochlear Implants. Curr. Opin. Otolaryngol. Head Neck Surg. 2014, 22, 344–348. [Google Scholar] [CrossRef]
- Cheng, L.-J.; Soon, S.S.; Wu, D.B.-C.; Ju, H.; Ng, K. Cost-Effectiveness Analysis of Bilateral Cochlear Implants for Children with Severe-to-Profound Sensorineural Hearing Loss in Both Ears in Singapore. PLoS ONE 2019, 14, e0220439. [Google Scholar] [CrossRef] [PubMed]
- Wachtlin, B.; Turinsky, Y.; Herrmann, F.; Schaefer, B. Phonological Awareness in German-Speaking Preschool Children with Cochlear Implants—3 Case Examples. Int. J. Pediatr. Otorhinolaryngol. 2017, 100, 198–203. [Google Scholar] [CrossRef] [PubMed]
- De Raeve, L.; Archbold, S.; Lehnhardt-Goriany, M.; Kemp, T. Prevalence of cochlear implants in Europe: Trend between 2010 and 2016. Cochlear Implant. Int. 2020, 21, 275–280. [Google Scholar] [CrossRef] [PubMed]
- Sarah, C. The Strobe guidelines. Saudi J. Anaesth. 2019, 13, S31–S34. [Google Scholar] [CrossRef]
- Schindler, A.; Leonardi, M.; Cavallo, M.; Ottaviani, F.; Schindler, O. Comparison between two perception tests in patients with severe and profoundly severe prelingual sensori-neural deafness. Acta Otorhinolaryngol. Ital. 2003, 23, 73–77. [Google Scholar] [PubMed]
- Meyer, T.A.; Pisoni, D.B. Some computational analyses of the PBK test: Effects of frequency and lexical density on spoken word recognition. Ear Hear. 1999, 20, 363–371. [Google Scholar] [CrossRef] [PubMed]
- CADTH. Functional Tests to Assess Speech in Noise. In Audiograms and Functional Auditory Testing to Assess Hearing Speech in Noise: A Review of the Clinical Evidence; Canadian Agency for Drugs and Technologies in Health: Ottawa, ON, Canada, 2015. [Google Scholar]
- Pae, H.K.; Wise, J.C.; Cirino, P.T.; Sevcik, R.A.; Lovett, M.W.; Wolf, M.; Morris, R.D. The woodcock reading mastery test: Impact of normative changes. Assessment 2005, 12, 347–357. [Google Scholar] [CrossRef] [PubMed]
- Wong, F.Y.; Yang, L.; Yuen, J.W.M.; Chang, K.K.P.; Wong, F.K.Y. Assessing quality of life using WHOQOL-BREF: A cross-sectional study on the association between quality of life and neighborhood environmental satisfaction, and the mediating effect of health-related behaviors. BMC Public Health 2018, 18, 1113. [Google Scholar] [CrossRef] [PubMed]
- Pereira, P.J.S.; Souza, N.F.H.D.; Almeida, R.J.D.; Menezes, D.C.; Bom, G.C.; Trettene, A.D.S. Nursing Diagnoses and Interventions in Children Submitted to Cochlear Implantation. Rev. Esc. Enferm. USP 2017, 51, e03238. [Google Scholar] [CrossRef]
- Glennon, E.; Svirsky, M.A.; Froemke, R.C. Auditory Cortical Plasticity in Cochlear Implant Users. Curr. Opin. Neurobiol. 2020, 60, 108–114. [Google Scholar] [CrossRef]
- Fagan, M.K. Cochlear Implantation at 12 Months: Limitations and Benefits for Vocabulary Production. Cochlear Implants Int. 2015, 16, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Hsu, H.-W.; Fang, T.-J.; Lee, L.-A.; Tsou, Y.-T.; Chen, S.H.; Wu, C.-M. Multidimensional Evaluation of Vocal Quality in Children with Cochlear Implants: A Cross-Sectional, Case-Controlled Study. Clin. Otolaryngol. 2014, 39, 32–38. [Google Scholar] [CrossRef] [PubMed]
- Barbosa, M.H.D.M.; Felix, F.; Ribeiro, M.G.; Tomita, S.; Pinheiro, C.; Baptista, M.M. Profile of Patients Assessed for Cochlear Implants. Braz. J. Otorhinolaryngol. 2014, 80, 305–310. [Google Scholar] [CrossRef]
- Sharma, S.D.; Cushing, S.L.; Papsin, B.C.; Gordon, K.A. Hearing and Speech Benefits of Cochlear Implantation in Children: A Review of the Literature. Int. J. Pediatr. Otorhinolaryngol. 2020, 133, 109984. [Google Scholar] [CrossRef] [PubMed]
- AlSanosi, A.; Hassan, S.M. The Effect of Age at Cochlear Implantation Outcomes in Saudi Children. Int. J. Pediatr. Otorhinolaryngol. 2014, 78, 272–276. [Google Scholar] [CrossRef] [PubMed]
- Necula, V.; Cosgarea, M.; Maniu, A.A. Effects of Family Environment Features on Cochlear-Implanted Children. Eur. Arch. Otorhinolaryngol. 2018, 275, 2209–2217. [Google Scholar] [CrossRef] [PubMed]
- Britto, F.D.R.; Samperiz, M.M.F. Communication Difficulties and Strategies Used by the Nurses and Their Team in Caring for the Hearing Impaired. Einstein São Paulo 2010, 8, 80–85. [Google Scholar] [CrossRef] [PubMed]
- McRackan, T.R.; Bauschard, M.; Hatch, J.L.; Franko-Tobin, E.; Droghini, H.R.; Nguyen, S.A.; Dubno, J.R. Meta-Analysis of Quality-of-Life Improvement after Cochlear Implantation and Associations with Speech Recognition Abilities: QOL Improvement After Cochlear Implantation. Laryngoscope 2018, 128, 982–990. [Google Scholar] [CrossRef]
- Crowson, M.G.; Semenov, Y.R.; Tucci, D.L.; Niparko, J.K. Quality of Life and Cost-Effectiveness of Cochlear Implants: A Narrative Review. Audiol. Neurotol. 2017, 22, 236–258. [Google Scholar] [CrossRef] [PubMed]
- Košec, A.; Živko, J.; Marković, S.; Bedeković, V.; Ries, M.; Ajduk, J. Impact of preoperative antibiotic use in preventing complications of cochlear implantation surgery. Cochlear Implants Int. 2022, 23, 134–138. [Google Scholar] [CrossRef] [PubMed]
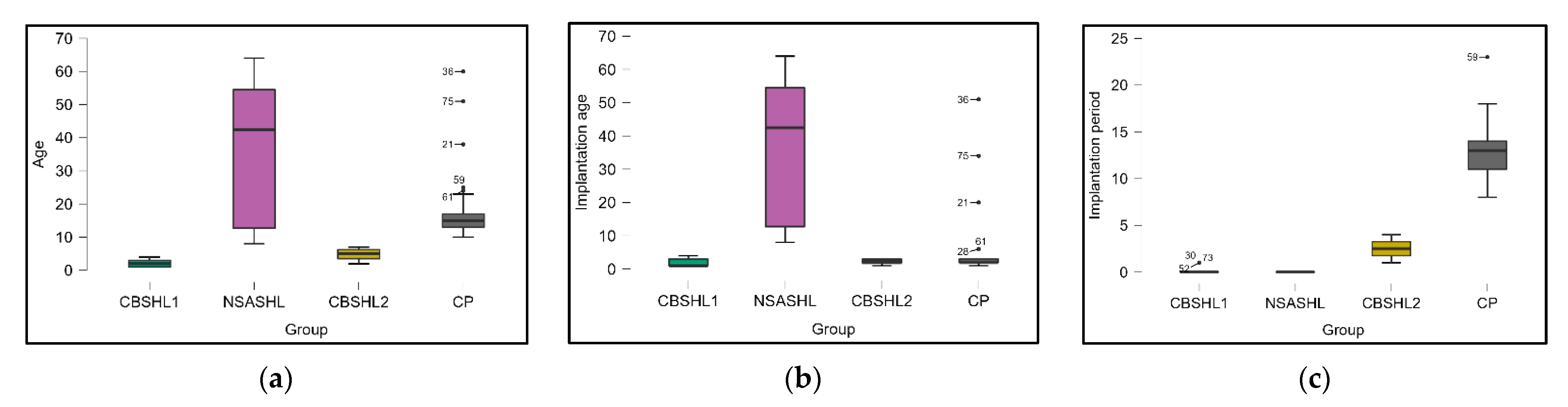
| Variables | CBSHL1 (n = 20) | CBSHL2 (n = 4) | NSASHL (n = 12) | CP (n = 41) | p-Value |
|---|---|---|---|---|---|
| Place of origin | 0.854 | ||||
| Urban | 13 (65.0%) | 3 (75.0%) | 9 (75.0%) | 25 (61.0%) | |
| Rural | 7 (35.0%) | 1 (25.0%) | 3 (25.0%) | 16 (39.0%) | |
| Gender | 0.334 | ||||
| Female | 7 (35.0%) | 2 (50.0%) | 8 (66.7%) | 24 (58.5%) | |
| Male | 13 (65.0%) | 2 (50.0%) | 4 (33.3%) | 17 (41.5%) | |
| Age | |||||
| Mean | 2.1 | 37.3 | 17.8 | 1.9 | 0.003 |
| Median | 2 | 42.5 | 15 | 1 | 0.059 |
| Mode | 1 | 8 | 14 | 1 | 0.798 |
| Range | 3 (4-1) | 56 (64-8) | 5 (7-2) | 50 (60-10) | <0.001 |
| Implantation age | |||||
| Mean | 1.95 | 37.33 | 2.25 | 4.73 | <0.001 |
| Median | 1 | 42.5 | 2.5 | 2 | 0.059 |
| Mode | 1 | 8 | 3 | 2 | 0.272 |
| Range | 3 (4-1) | 56 (64-8) | 2 (3-1) | 50 (51-1) | <0.001 |
| Implantation period | |||||
| Mean | 0.15 | 0 | 2.5 | 13.02 | <0.001 |
| Median | 0 | 0 | 2.5 | 13 | — |
| Mode | 0 | 0 | 1 | 11 | 0.972 |
| Range | 1 (1-0) | 0 | 3 (4-1) | 15 (23-8) | 0.026 |
| Otitis after CI | 15 (75.0%) | 2 (50.0%) | 3 (25.0%) | 10 (24.4%) | 0.001 |
| Variables | CBSHL1 (n = 20) | CBSHL2 (n = 4) | NSASHL (n = 12) | CP (n = 41) | p-Value |
|---|---|---|---|---|---|
| Speech perception | |||||
| WIPI (mean accuracy% ± SD) | — | 13.5 ± 9.2% | 20.2 ± 12.7% | — | 0.351 |
| HINT (mean accuracy% ± SD) | — | 27.4 ± 13.8% | 24.9 ± 15.6% | — | 0.780 |
| PBK (mean accuracy% ± SD) | 19.2 ± 14.4% | — | — | 22.6 ± 12.9% | 0.356 |
| Speech production | |||||
| Correct answers (% ± SD) | — | 33.5 ± 14.2% | 38.1 ± 13.6% | — | 0.570 |
| Reading achievement | |||||
| (mean ± SD) | — | 74.1 ± 7.6 | 71.4 ± 9.2 | — | 0.555 |
| Variables | Before (n = 16) | 3 Months (n = 16) | 6 Months (n = 16) | 12 Months (n = 16) | p-Value | p-Value * |
|---|---|---|---|---|---|---|
| Speech perception | ||||||
| WIPI (mean% ± SD) | 21.3 ± 11.8% | 62.2 ± 16.5% | 69.6 ± 12.3% | 73.4 ± 13.2% | <0.001 | 0.406 |
| HINT (mean% ± SD) | 22.7 ± 13.5% | 55.2 ± 19.1% | 61.0 ± 15.8% | 68.4 ± 11.7% | <0.001 | 0.143 |
| Speech production | ||||||
| Correct answers (% ± SD) | 33.5 ± 14.2% | 68.1 ± 22.8% | 73.5 ± 24.0% | 76.8 ± 19.4% | <0.001 | 0.672 |
| Reading achievement | ||||||
| (mean ± SD) | 76.2 ± 8.1 | 96.5 ± 12.8 | 104.1 ± 17.6 | 106.3 ± 19.2 | <0.001 | 0.737 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Virzob, C.R.B.; Poenaru, M.; Morar, R.; Horhat, I.D.; Balica, N.C.; Prathipati, R.; Moleriu, R.D.; Toma, A.-O.; Juganaru, I.; Bloanca, V.; et al. Efficacy of Bilateral Cochlear Implantation in Pediatric and Adult Patients with Profound Sensorineural Hearing Loss: A Retrospective Analysis in a Developing European Country. J. Clin. Med. 2023, 12, 2948. https://doi.org/10.3390/jcm12082948
Virzob CRB, Poenaru M, Morar R, Horhat ID, Balica NC, Prathipati R, Moleriu RD, Toma A-O, Juganaru I, Bloanca V, et al. Efficacy of Bilateral Cochlear Implantation in Pediatric and Adult Patients with Profound Sensorineural Hearing Loss: A Retrospective Analysis in a Developing European Country. Journal of Clinical Medicine. 2023; 12(8):2948. https://doi.org/10.3390/jcm12082948
Chicago/Turabian StyleVirzob, Claudia Raluca Balasa, Marioara Poenaru, Raluca Morar, Ioana Delia Horhat, Nicolae Constantin Balica, Reshmanth Prathipati, Radu Dumitru Moleriu, Ana-Olivia Toma, Iulius Juganaru, Vlad Bloanca, and et al. 2023. "Efficacy of Bilateral Cochlear Implantation in Pediatric and Adult Patients with Profound Sensorineural Hearing Loss: A Retrospective Analysis in a Developing European Country" Journal of Clinical Medicine 12, no. 8: 2948. https://doi.org/10.3390/jcm12082948
APA StyleVirzob, C. R. B., Poenaru, M., Morar, R., Horhat, I. D., Balica, N. C., Prathipati, R., Moleriu, R. D., Toma, A.-O., Juganaru, I., Bloanca, V., Chicin, G. N., Fericean, R. M., Domuta, E. M., Iurciuc, M., & Iurciuc, S. (2023). Efficacy of Bilateral Cochlear Implantation in Pediatric and Adult Patients with Profound Sensorineural Hearing Loss: A Retrospective Analysis in a Developing European Country. Journal of Clinical Medicine, 12(8), 2948. https://doi.org/10.3390/jcm12082948







