A Retrospective Analysis of the American Thrombosis and Hemostasis Network Dataset Describing Outcomes of Dental Extractions in Persons with Hemophilia
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Measures
3. Results
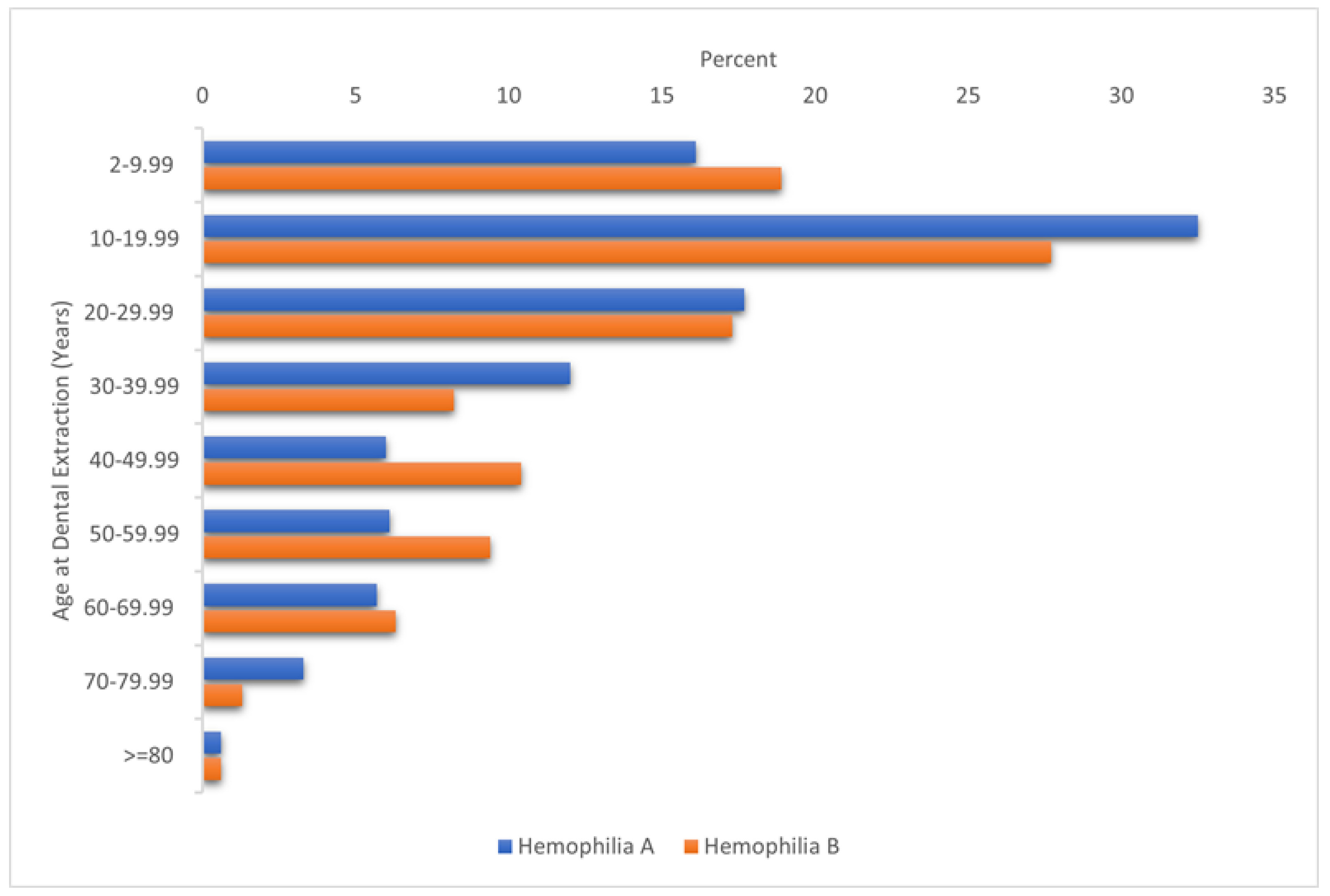
3.1. Sociodemographic and Clinical Characteristics
3.2. Dental Extraction Clinical Outcomes and Related Treatments
3.3. Factors Associated with Dental Extraction Bleeding
4. Discussion
4.1. Further Research
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bajkin, B.; Dougall, A. Current State of Play Regarding Dental Extractions in Patients with Haemophilia: Consensus or Evidence-Based Practice? A Review of the Literature. Haemophilia 2020, 26, 183–199. [Google Scholar] [CrossRef] [PubMed]
- ATHN. Available online: https://Athn.Org/What-We-Do/for-Researchers/Athndataset-Core-Data-Elements.Html (accessed on 1 April 2019).
- Basta, M.; Pandya, A.M. Genetics, X-Linked Inheritance; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Srivastava, A.; Santagostino, E.; Dougall, A.; Kitchen, S.; Sutherland, M.; Pipe, S.W.; Carcao, M.; Mahlangu, J.; Ragni, M.V.; Windyga, J.; et al. WFH Guidelines for the Management of Hemophilia, 3rd Edition. Haemophilia 2020, 26. [Google Scholar] [CrossRef] [PubMed]
- Ivastava, A.S.; Rewer, A.K.B.; Mauser-Bunsc Hoten, E.P.; Ey, N.S.K.; Kitc He, N.S.; Llin As, A.; Udlam, C.A.L.; Mah La, N.G.U.N.; Mulder, K.; Poon, M.C.; et al. WFH GUIDELINES Guidelines for the Management of Hemophilia. Haemophilia 2013, 19, 1–47. [Google Scholar] [CrossRef] [PubMed]
- van Galen, K.P.M.; Engelen, E.T.; Mauser-Bunschoten, E.P.; van Es, R.J.J.; Schutgens, R.E.G. Antifibrinolytic Therapy for Preventing Oral Bleeding in Patients with Haemophilia or Von Willebrand Disease Undergoing Minor Oral Surgery or Dental Extractions. Cochrane Database Syst. Rev. 2015, 2015, 2134. [Google Scholar] [CrossRef] [PubMed]
- Champagne, P.A.; Bourassa, M.; Desjardins, M.P.; Cloutier, S.; Demers, C.; Singbo, N.U.; Néron, H.P.-M.M.C. Post-Procedural Bleeding Rate and Haemostatic Treatment Use for Dental Procedures before and after the Implementation of a Standardized Protocol for People with Inherited Bleeding Disorders. Haemophilia 2022, 4, 4609. [Google Scholar] [CrossRef] [PubMed]
- Santagostino, E.; Oldenburg, J.; Chang, T.; Chebon, S.; Doral, M.; Jimenez-Yuste, V.; Liesner, R.; Croteau, S.; Tones, L.; Circe, K.; et al. Surgical Experience from Four Phase III Studies (Haven 1–4) of Emicizumab in Persons with Haemophilia a (PWHA) with or without FVIII Inhibitors. Res. Pract. Thromb. Haemost. 2019, 3, 299. [Google Scholar]
- Pell, G. Tranexamic Acid-Its Use in Controlling Dental Postoperative Bleeding in Patients with Defective Clotting Mechanisms. Br. J. Oral Surg. 1973, 11, 35. [Google Scholar] [CrossRef] [PubMed]
- Franchini, M.; Rossetti, G.; Tagliaferri, A.; Pattacini, C.; Pozzoli, D.; Lorenz, C.; del Dot, L.; Ugolotti, G.; Dell’Aringa, C.; Gandini, G. Dental Procedures in Adult Patients with Hereditary Bleeding Disorders: 10 Years Experience in Three Italian Hemophilia Centers. Haemophilia 2005, 11, 504–509. [Google Scholar] [CrossRef] [PubMed]
- Reich, W.; Kriwalsky, M.S.; Wolf, H.H.; Schubert, J. Bleeding Complications after Oral Surgery in Outpatients with Compromised Haemostasis: Incidence and Management. Oral Maxillofac. Surg. 2009, 13, 73–77. [Google Scholar] [CrossRef] [PubMed]
- Yagyuu, T.; Yata, S.; Imada, M.; Funayama, N.; Imai, Y.; Yada, K.; Nogami, K.; Kirita, T. Risk Factors for Post-Extraction Bleeding in Patients with Haemophilia: A Retrospective Cohort Study. Br. J. Oral Maxillofac. Surg. 2021, 59, 121. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, J.T.; Klein, K.; Batstone, M. Ten-Year Study of Postoperative Complications Following Dental Extractions in Patients with Inherited Bleeding Disorders. Int. J. Oral Maxillofac. Surg. 2017, 46, 1147–1150. [Google Scholar] [CrossRef] [PubMed]
- Hikmat, R.; Maposa, W.; Hart, D.P.; Nanayakkara, L. Patient Reported Outcomes of Post-Operative Bleeding Following Dental Treatment. Haemophilia 2018, 24, 68. [Google Scholar]
- Frachon, X.; Pommereuil, M.; Berthier, A.M.; Lejeune, S.; Hourdin-Eude, S.; Quéro, J.; Mézière, X.; de Mello, G.; Garnier, J. Management Options for Dental Extraction in Hemophiliacs: A Study of 55 Extractions (2000–2002). Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2005, 99, 71. [Google Scholar] [CrossRef] [PubMed]
- Hewson, I.; Makhmalbaf, P.; Street, A.; Mccarthy, P.; Walsh, M. Dental Surgery with Minimal Factor Support in the Inherited Bleeding Disorder Population at the Alfred Hospital. Haemophilia 2011, 17, 2346. [Google Scholar] [CrossRef] [PubMed]
- Peisker, A.; Raschke, G.F.; Schultze-Mosgau, S. Management of Dental Extraction in Patients with Haemophilia A and B: A Report of 58 Extractions. Med. Oral Patol. Oral Cir. Bucal. 2014, 19, 9191. [Google Scholar] [CrossRef] [PubMed]
- Sindet-Pedersen, S.; Stenbjerg, S. Effect of Local Antifibrinolytic Treatment with Tranexamic Acid in Hemophiliacs Undergoing Oral Surgery. J. Oral Maxillofac. Surg. 1986, 44, 39. [Google Scholar] [CrossRef] [PubMed]
- Piot, B.; Sigaud-Fiks, M.; Huet, P.; Fressinaud, E.; Trossaërt, M.; Mercier, J. Management of Dental Extractions in Patients with Bleeding Disorders. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2002, 93, 431. [Google Scholar] [CrossRef] [PubMed]
- Givol, N.; Hirschhorn, A.; Lubetsky, A.; Bashari, D.; Kenet, G. Oral Surgery-Associated Postoperative Bleeding in Haemophilia Patients—A Tertiary Centre’s Two Decade Experience. Haemophilia 2015, 21, 2573. [Google Scholar] [CrossRef] [PubMed]
- Zanon, E.; Martinelli, F.; Bacci, C.; Zerbinati, P.; Girolami, A. Proposal of a Standard Approach to Dental Extraction in Haemophilia Patients. A Case-Control Study with Good Results. Haemophilia 2000, 6, 423. [Google Scholar] [CrossRef] [PubMed]
- Stajčić, Z. The Combined Local/Systemic Use of Antifibrinolytics in Hemophiliacs Undergoing Dental Extractions. Int. J. Oral Surg. 1985, 14, 23. [Google Scholar] [CrossRef] [PubMed]

| Variable | Dental Extraction (%) | No Dental Extraction (%) | OR (95% CI) |
|---|---|---|---|
| Most recent biological age | |||
| 2–9.99 years | 103 (8.9) | 2542 (14.2) | Reference |
| 10–19.99 years | 311 (26.9) | 4230 (23.6) | 1.81 (1.44–2.28) |
| 20–29.99 years | 324 (28.0) | 3610 (20.2) | 2.22 (1.76–2.78) |
| 30–39.99 years | 137 (11.8) | 2802 (15.7) | 1.21 (0.92–1.57) |
| 40–49.99 years | 89 (7.7) | 1602 (9.0) | 1.37 (1.03–1.83) |
| 50–59.99 years | 73 (6.3) | 1365 (7.6) | 1.32 (0.97–1.79) |
| 60–69.99 years | 72 (6.2) | 1006 (5.6) | 1.77 (1.30–2.41) |
| 70–79.99 years | 35 (3.0) | 550 (3.1) | 1.57 (1.06–2.33) |
| ≥80 years | 13 (1.1) | 184 (1.0) | 1.74 (0.96–3.16) |
| Gender | |||
| Female | 65 (5.6) | 2302 (12.9) | Reference |
| Male | 1092 (94.4) | 15,588 (87.1) | 2.48 (1.93–3.20) |
| Race a | |||
| White | 955 (84.1) | 14,421 (82.8) | Reference |
| Black or African American | 118 (10.4) | 1870 (10.7) | 0.95 (0.78–1.16) |
| Asian | 43 (3.8) | 634 (3.6) | 1.02 (0.75–1.40) |
| Other races | 20 (1.8) | 488 (2.8) | 0.62 (0.39–0.97) |
| Diagnosis | |||
| Hemophilia A | 866 (74.9) | 13,797 (77.1) | Reference |
| Hemophilia B | 291 (25.2) | 4094 (22.9) | 1.13 (0.99–1.30) |
| Severity a | |||
| Mild | 386 (34.5) | 5146 (31.6) | Reference |
| Moderate | 263 (23.5) | 3582 (22.0) | 0.98 (0.83–1.15) |
| Severe | 470 (42.0) | 7572 (46.5) | 0.83 (0.72–0.95) |
| Ever inhibitor a | |||
| No | 920 (85.0) | 11,891 (86.0) | Reference |
| Yes | 162 (15.0) | 1934 (14.0) | 1.08 (0.91–1.29) |
| Education b | |||
| Advanced degree | 44 (9.6) | 724 (10.8) | Reference |
| College | 67 (14.7) | 1072 (16.0) | 1.03 (0.70–1.52) |
| Some college | 155 (33.9) | 2097 (31.2) | 1.22 (0.86–1.72) |
| GED or equivalent | 32 (7.0) | 441 (6.6) | 1.19 (0.75–1.91) |
| Secondary or under | 159 (34.8) | 2381 (35.5) | 1.10 (0.78–1.55) |
| Employment b | |||
| Full-time | 258 (51.8) | 4089 (52.9) | Reference |
| Part-time | 52 (10.4) | 631 (8.2) | 1.31 (0.96–1.78) |
| Not employed | 188 (27.8) | 3013 (39.0) | 0.99 (0.82–1.20) |
| Variable | Hemophilia A (n = 983) | Hemophilia B (n = 318) | All Patients (n = 1301) |
|---|---|---|---|
| Dental-extraction-related bleeds, n (%) | 50 (5.1) | 16 (5.0) | 66 (5.1) |
| ≥2 dental extractions | 14 (28.0) | 2 (12.5) | 16 (24.2) |
| Treated dental-extraction-related bleeds a | 17 (34.0) | 8 (50.0) | 25 (37.8) |
| Hospitalization b, n (%) | 74 (7.4) | 28 (8.8) | 102 (7.8) |
| Emergency visit b, n (%) | 13 (1.3) | 3 (0.9) | 16 (1.2) |
| Health insurance, n (%) | |||
| Insured | 849 (86.4) | 251 (78.9) | 1100 (84.6) |
| Uninsured | 27 (2.8) | 35 (11.0) | 62 (4.8) |
| Unknown | 107 (10.2) | 32 (10.1) | 139 (10.7) |
| General bleeding treatment one week post dental extraction c | |||
| On-demand d, n (%) | 182 (18.5) | 58 (18.2) | 240 (18.4) |
| EHL products | 5 (0.5) | 2 (0.6) | 7 (0.5) |
| SHL products | 82 (8.3) | 26 (8.2) | 108 (8.3) |
| Plasma-derived products | 7 (0.7) | 3 (0.9) | 10 (0.8) |
| Bypassing agents | 5 (0.5) | 2 (0.6) | 7 (0.5) |
| Other hemostasis medications | 109 (11.1) | 33 (10.4) | 142 (10.9) |
| Prophylaxis | 367 (37.3) | 80 (25.2) | 447 (34.3) |
| EHL products, n (%) | 71 (7.2) | 35 (11.0) | 106 (8.1) |
| Dose per Kg (IU/Kg), median (IQR) | 50 (42–60) | 76 (53–100) | 51 (50–70) |
| Dose frequency, median (IQR) | 3.5 (3.5–4.0) | 7.0 (7.0–7.0) | 3.5 (3.5–7.0) |
| SHL products, n (%) | 221 (22.5) | 36 (11.3) | 257 (19.8) |
| Dose per Kg (IU/Kg), median (IQR) | 40 (32–49) | 66 (55–76) | 40 (35–50) |
| Dose frequency, median (IQR) | 2.3 (2.0–3.5) | 3.5 (2.3–3.5) | 2.3 (2.0–3.5) |
| Plasma-derived products, n (%) | 28 (2.8) | 6 (1.9%) | 34 (2.6) |
| Dose per Kg (IU/Kg), median (IQR) | 40 (31–85) | 75 (74–90) | 74 (38–89) |
| Dose frequency, median (IQR) | 2.3 (2.0–2.3) | 3.5 (3.5–7.0) | 2.3 (2.0–3.5) |
| Bypassing agents, n (%) | 10 (1.0) | 2 (0.6) | 12 (0.9) |
| Non-factor molecules, n (%) | 24 (2.4) | NA | 24 (1.8) |
| Other hemostasis medications, n (%) | 2 (0.2) | 1 (0.3) | 3 (0.2) |
| Dental extraction without hemostatic treatment, n (%) | 496 (50.5) | 190 (59.7) | 686 (52.7) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Messenger, H.; Kulkarni, R.; Recht, M.; He, C. A Retrospective Analysis of the American Thrombosis and Hemostasis Network Dataset Describing Outcomes of Dental Extractions in Persons with Hemophilia. J. Clin. Med. 2023, 12, 1839. https://doi.org/10.3390/jcm12051839
Messenger H, Kulkarni R, Recht M, He C. A Retrospective Analysis of the American Thrombosis and Hemostasis Network Dataset Describing Outcomes of Dental Extractions in Persons with Hemophilia. Journal of Clinical Medicine. 2023; 12(5):1839. https://doi.org/10.3390/jcm12051839
Chicago/Turabian StyleMessenger, Heather, Roshni Kulkarni, Michael Recht, and Chunla He. 2023. "A Retrospective Analysis of the American Thrombosis and Hemostasis Network Dataset Describing Outcomes of Dental Extractions in Persons with Hemophilia" Journal of Clinical Medicine 12, no. 5: 1839. https://doi.org/10.3390/jcm12051839
APA StyleMessenger, H., Kulkarni, R., Recht, M., & He, C. (2023). A Retrospective Analysis of the American Thrombosis and Hemostasis Network Dataset Describing Outcomes of Dental Extractions in Persons with Hemophilia. Journal of Clinical Medicine, 12(5), 1839. https://doi.org/10.3390/jcm12051839





